Pimples on babies cheeks
Is that acne on my baby’s face?
Diseases & conditions
- Coronavirus Resource Center
- Acne
- Eczema
- Hair loss
- Psoriasis
- Rosacea
- Skin cancer
- A to Z diseases
- A to Z videos
- DIY acne treatment
- How dermatologists treat
- Skin care: Acne-prone skin
- Causes
- Is it really acne?
- Types & treatments
- Childhood eczema
- Adult eczema
- Insider secrets
- Types of hair loss
- Treatment for hair loss
- Causes of hair loss
- Hair care matters
- Insider secrets
- What is psoriasis
- Diagnosis & treatment
- Skin, hair & nail care
- Triggers
- Insider secrets
- What is rosacea
- Treatment
- Skin care & triggers
- Insider secrets
- Types and treatment
- Find skin cancer
- Prevent skin cancer
- Raise awareness
- Español
Featured
How Natalie cleared her adult acneNatalie tried many acne products without success. Find out how a board-certified dermatologist helped Natalie see clear skin before her wedding.
JAK inhibitors are helping patients with alopecia areata, eczema/atopic dermatitis, psoriasis, and vitiligo. Here’s what you need to know.
Everyday care
- Skin care basics
- Skin care secrets
- Injured skin
- Itchy skin
- Sun protection
- Hair & scalp care
- Nail care secrets
- Basic skin care
- Dry, oily skin
- Hair removal
- Tattoos and piercings
- Anti-aging skin care
- For your face
- For your skin routine
- Preventing skin problems
- Bites & stings
- Burns, cuts, & other wounds
- Itch relief
- Poison ivy, oak & sumac
- Rashes
- Shade, clothing, and sunscreen
- Sun damage and your skin
- Aprenda a proteger su piel del sol
- Your hair
- Your scalp
- Nail care basics
- Manicures & pedicures
Featured
Practice Safe SunEveryone's at risk for skin cancer.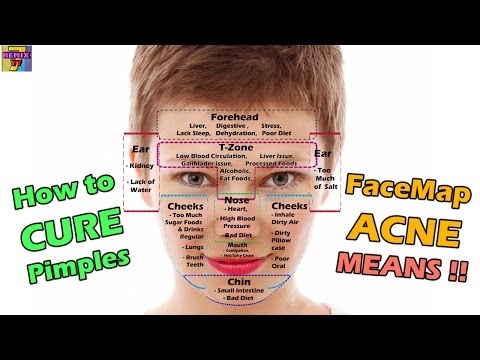 These dermatologists' tips tell you how to protect your skin.
These dermatologists' tips tell you how to protect your skin.
Find out what may be causing the itch and what can bring relief.
Darker Skin Tones
- Skin care secrets
- Hair care
- Hair loss
- Diseases & Conditions
- Acne
- Dark spots
- Dry skin
- Light spots
- Razor bumps
- Caring for Black hair
- Scalp psoriasis
- Weaves & extensions
- Central centrifugal cicatricial alopecia
- Frontal fibrosing alopecia
- Hairstyles that pull can cause hair loss
- Acanthosis nigricans
- Acne keloidalis nuchae
- Hidradenitis suppurativa
- Keloid scars
- Lupus and your skin
- Sarcoidosis and your skin
- Skin cancer
- Vitiligo
- More diseases & conditions
Featured
Fade dark spotsFind out why dark spots appear and what can fade them.
If you have what feels like razor bumps or acne on the back of your neck or scalp, you may have acne keloidalis nuchae. Find out what can help.
Cosmetic treatments
- Your safety
- Age spots & dark marks
- Cellulite & fat removal
- Hair removal
- Scars & stretch marks
- Wrinkles
- Younger-looking skin
Featured
Laser hair removalYou can expect permanent results in all but one area.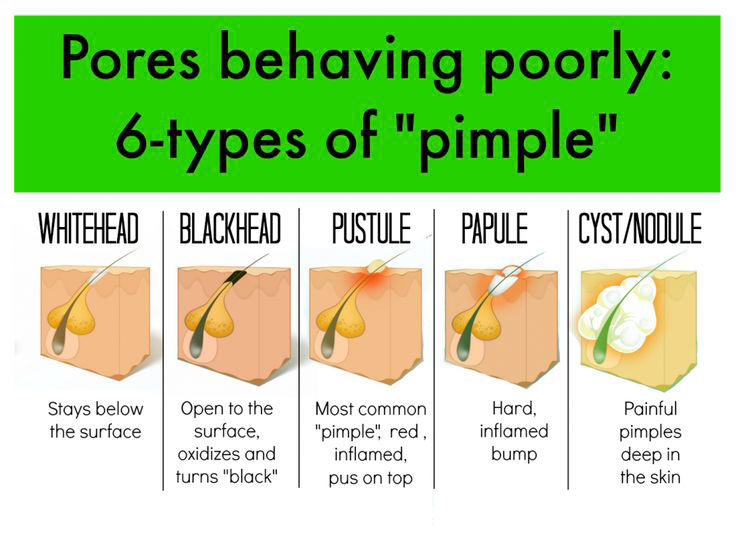 Do you know which one?
Do you know which one?
If you want to diminish a noticeable scar, know these 10 things before having laser treatment.
BotoxIt can smooth out deep wrinkles and lines, but the results aren’t permanent. Here’s how long botox tends to last.
Public health programs
- Skin cancer awareness
- Free skin cancer screenings
- Kids' camp
- Good Skin Knowledge
- Shade Structure grants
- Skin Cancer, Take a Hike!™
- Awareness campaigns
- Flyers & posters
- Get involved
- Lesson plans and activities
- Community grants
Featured
Free materials to help raise skin cancer awarenessUse these professionally produced online infographics, posters, and videos to help others find and prevent skin cancer.
Free to everyone, these materials teach young people about common skin conditions, which can prevent misunderstanding and bullying.
Find a dermatologist
- Find a dermatologist
- What is a dermatologist?
- FAAD: What it means
- How to select a dermatologist
- Telemedicine appointments
- Prior authorization
- Dermatologists team up to improve patient care
Featured
Find a DermatologistYou can search by location, condition, and procedure to find the dermatologist that’s right for you.
A dermatologist is a medical doctor who specializes in treating the skin, hair, and nails. Dermatologists care for people of all ages.
Baby Acne: What Causes It and How to Treat It
Your beautiful newborn has made their long-awaited entrance into the world, but a few weeks later you notice pimple-like spots on their face. Don’t worry—your little one isn’t heading into their teens particularly early! It’s likely they have baby acne, a condition that’s common in newborns. Find out more about it and what you can do to care for your baby's delicate skin during a bout of baby acne.
What Is Baby Acne and What Are the Symptoms?
You may see your newborn baby with small pimples on their face, usually on their cheeks, nose, eyelids, chin, and/or forehead. This may be baby acne, which is also referred to as neonatal acne. It’s common in newborns and appears in 3 out of 10 babies.
It’s common in newborns and appears in 3 out of 10 babies.
When Does Baby Acne Start and How Long Does It Last?
Baby acne may first appear on your newborn at around 2 to 5 weeks old. So, when does baby acne go away? It's a temporary condition that typically clears up after about three to four months and leaves no scars.
What Causes Baby Acne?
There is no way to prevent baby acne. Experts are not exactly sure what causes baby acne, but it could be due to one of the following:
Inflammation caused by yeast on your baby's skin
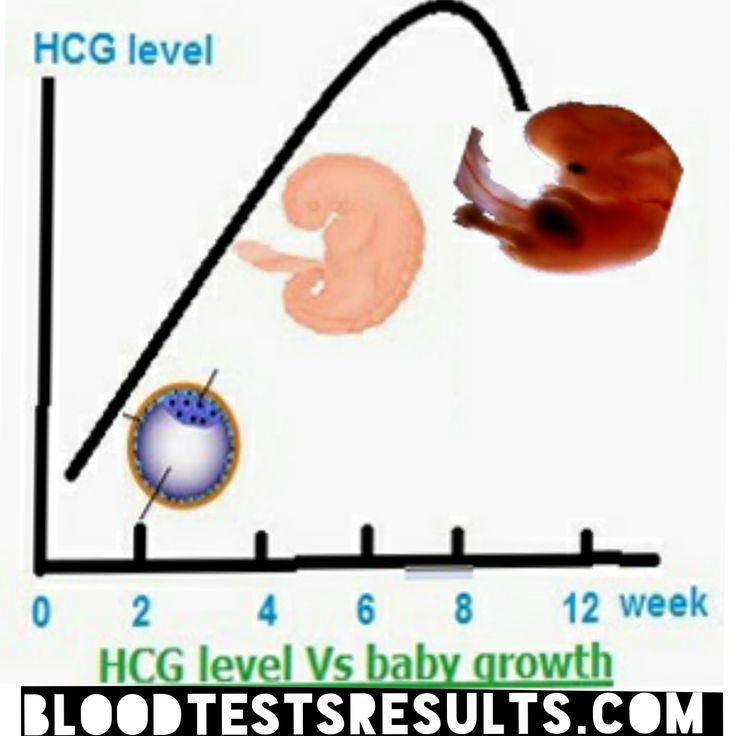
Overstimulated oil glands in your baby's skin caused by encountering hormones in the placenta during your pregnancy.
Baby acne has nothing to do with the type of acne that a teenager may experience.
What Does Baby Acne Look Like?
Baby acne looks like tiny red or white bumps (a. k.a. milia) or pustules that appear on your infant's cheeks, nose, eyelids, chin, and/or forehead. Sometimes the acne can also appear on your baby’s scalp or on their neck or upper trunk. Unlike acne that teens and adults can experience, baby acne does not have blackheads or whiteheads.
k.a. milia) or pustules that appear on your infant's cheeks, nose, eyelids, chin, and/or forehead. Sometimes the acne can also appear on your baby’s scalp or on their neck or upper trunk. Unlike acne that teens and adults can experience, baby acne does not have blackheads or whiteheads.
How to Treat Baby Acne
There are no treatments or natural, at-home remedies for clearing up baby acne—you will just have to wait for it to go away on its own.
In the meantime, here’s how you can care for your baby's delicate skin:
Place a soft, clean blanket under your baby’s head when they’re awake to shield their skin from any laundry detergent residue on sheets or clothing
Ensure that your baby's bed sheets and clothing haven't been washed with harsh laundry detergents (use one designed specifically for babies)
Maintain proper hygiene by gently washing your little one's face every day with warm water and a mild baby soap and pat it dry
Avoid irritating the acne by pinching or scrubbing the pimples as this may cause more harm or even lead to an infection.
 Avoid moisturizing their face with lotions or oils.
Avoid moisturizing their face with lotions or oils.
When Should You See Your Baby’s Healthcare Provider?
So, when is baby acne a concern? If anything about your baby's complexion seems out of the ordinary, or if the condition isn't getting better after three to four months, consult your baby's healthcare provider. Also, contact your baby's provider if you ever notice any of the following:
Skin blisters
Peeling skin
Irritability
Fever
Your baby isn't feeding well.
How Is Baby Acne Diagnosed?
Your baby’s healthcare provider will be able to determine if it's baby acne or some other form of baby rash such as heat rash or eczema after examining your little one.
The healthcare provider may prescribe a medicated ointment or some other treatment for the baby acne.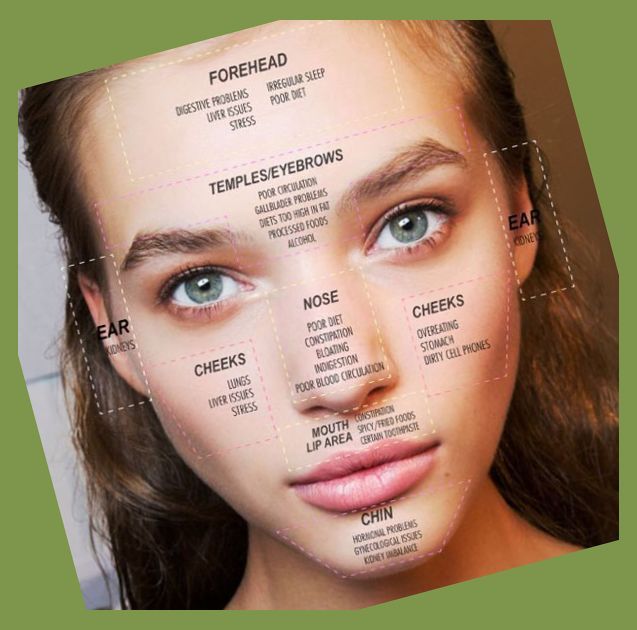 But be sure not to use any over-the-counter creams or medications without consulting the healthcare provider first, as these can damage your baby's delicate skin.
But be sure not to use any over-the-counter creams or medications without consulting the healthcare provider first, as these can damage your baby's delicate skin.
The Bottom Line
A little baby acne will not diminish how absolutely adorable your newborn is. Like teenage acne, baby acne is just something that can happen as a part of growing up. Take care of your little one's skin as best as you can, wait for it to pass, and keep giving those little cheeks plenty of kisses.
Did you know that you can get rewarded for all the baby wipes and diapers you buy from Pampers? Simply download the Pampers Club app, scan your Pampers purchases, and watch your Pampers Cash balance grow.
Red pimples on the face of a newborn: symptoms, causes and treatment
A rash on the face of a newborn is a common occurrence, which is considered a sign of the baby's adaptation to the environment. In most cases, rashes go away on their own and require only competent care without the use of drugs.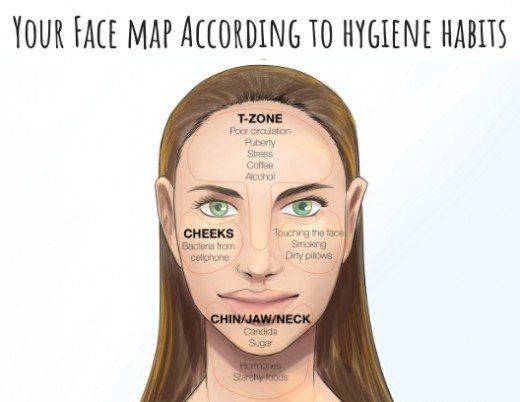 How to distinguish harmless red pimples from dermatological diseases and allergies? How to understand that the rash will pass by itself, and what signs are a reason to see a doctor?
How to distinguish harmless red pimples from dermatological diseases and allergies? How to understand that the rash will pass by itself, and what signs are a reason to see a doctor?
Allergic rash in a newborn
An allergy in an infant is an unfavorable immune response of a child's body to a potentially dangerous substance. Most often, an allergic rash occurs against the background of the use by a nursing mother of products that can act as an irritant. This group includes:
- cow's milk;
- soy [1] and egg white;
- fish;
- strawberries;
- nuts.
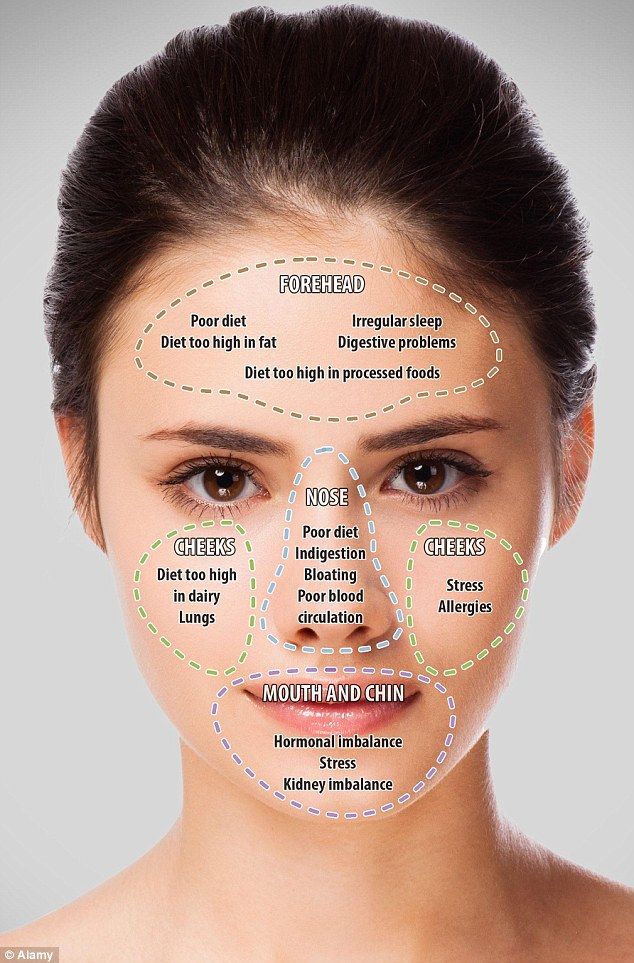
The first sign of developing allergic rash is peeling. Pathological foci with dry skin on the face of a newborn are formed symmetrically, localized on the cheeks and on the forehead.
It is necessary to consult a doctor if the appearance of rashes affects the general condition of the baby. Irritability, restless sleep, disorders of the gastrointestinal tract, fever and vomiting are dangerous symptoms that should be stopped immediately under the supervision of a pediatrician.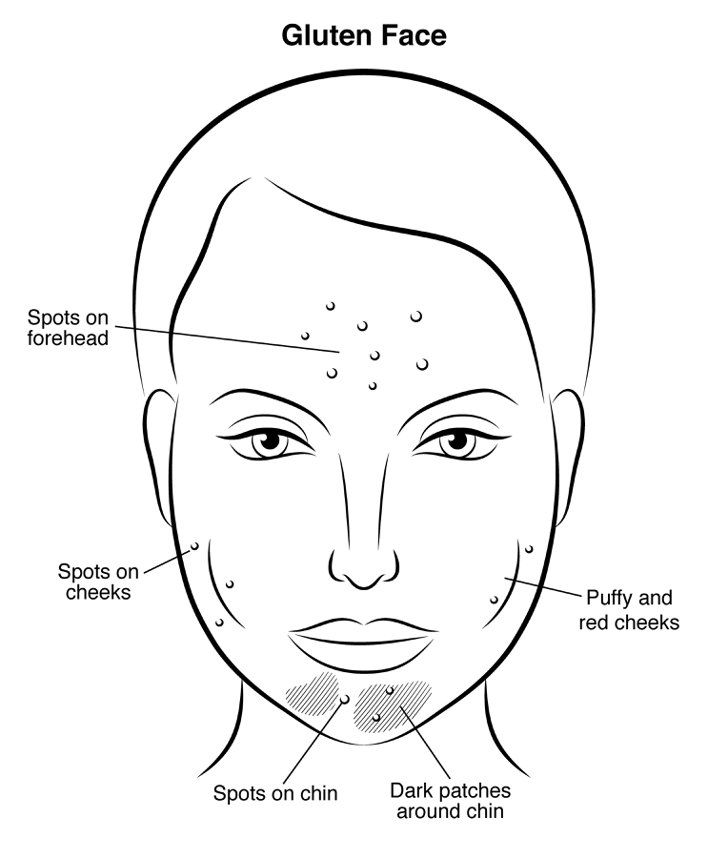
Neonatal acne
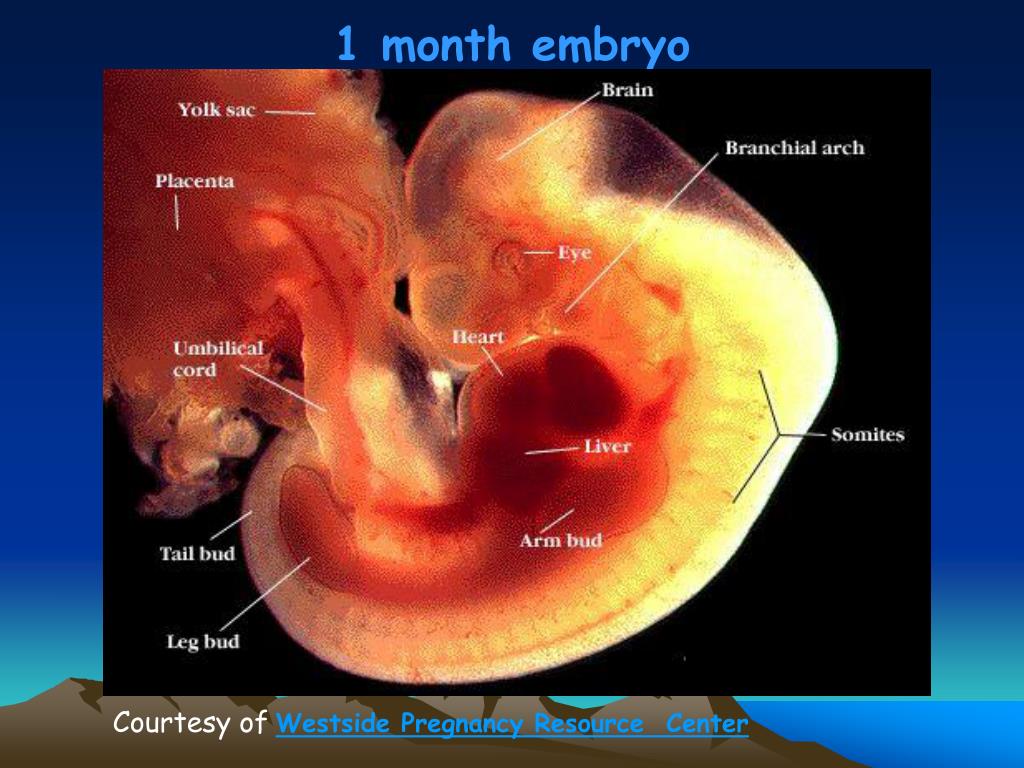
Neonatal acne may appear in the first weeks of a child's life on the forehead, nose and cheeks. In appearance, they resemble acne with purulent heads, characteristic of a teenage rash. It is assumed that the reason for the appearance of acne is increased production of sebum, which clogs the ducts of the sebaceous glands and provokes an inflammatory reaction.
The pathogenesis of the appearance of small pimples in newborns is also associated with the processes of the formation of the hormonal system. The body gets rid of the transplacental influence of maternal androgens [2], adrenal hormones begin to be produced more intensively, which affect the condition of the skin.
Neonatal acne does not require treatment [9] - standard daily care using delicate soap or baby cosmetics is sufficient. In most cases, pimples that appear on the face go away on their own by 4 months of age.
Sweating
Sweating is a skin lesion that is associated with hyperfunction of the sweat glands and irritation of the excretory ducts . The disease can develop due to improper skin care newborn, with a long stay in hot rooms and the wrong choice of clothing (the child is heavily wrapped up).
Miliaria resembles an allergic rash, but differs from it in localization. Signs of allergy most often appear on the skin of the child's face, and with miliaria, rashes form throughout the body - most often in natural folds, on the neck, lower abdomen and upper chest.
What prickly heat looks like:
- small vesicles with clear contents, prone to burning and itching;
- in difficult cases, reddish nodules with an inflamed rim;
- with extensive skin lesions - weeping areas.
Prickly heat in itself is not dangerous for the health of the child. But damage to the skin is fraught with the addition of a bacterial or fungal infection.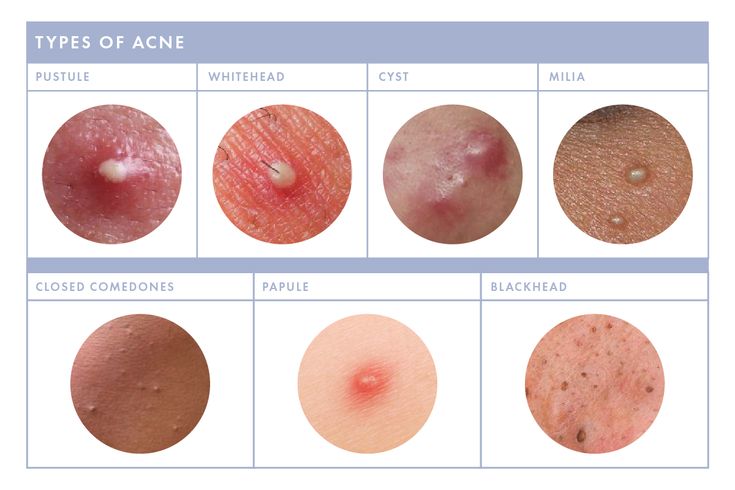 In this case, purulent processes develop, the skin becomes edematous, a putrid odor appears. Red pimples with prickly heat cause discomfort in the child - he becomes capricious and irritable, refuses to eat and sleeps poorly.
In this case, purulent processes develop, the skin becomes edematous, a putrid odor appears. Red pimples with prickly heat cause discomfort in the child - he becomes capricious and irritable, refuses to eat and sleeps poorly.
Seborrheic dermatitis
In addition to red pimples, yellowish scales may appear on the skin of a newborn. These are signs of seborrheic dermatitis, a disease associated with increased secretion of sebum. Scales are formed in the first month of life in areas of the body with a large accumulation of sebaceous glands - on the scalp, upper third of the back, on the face, chest and in the area of the auricles. Seborrheic dermatitis is sometimes called "milky crusts", which may be associated with the use of unsuitable cosmetic products for baby skin care.
In fact, the disease is caused by a high content of maternal hormones in the blood or a change in the biochemical composition of lipids on the surface of the skin [4].
Most childhood seborrheic dermatitis resolves on its own. Parents need only to take care of proper care , but diligently removing the crusts is not recommended - you risk damaging delicate skin and causing infection. It is better to use specially designed products - such as Shampoo-foam from "milk crusts" for newborns. He facilitates the removal of scales in 90% of cases and soothes the scalp in 95% of babies [5.2]. The product contains 99% ingredients of natural origin. The shampoo is fragrance-free and has a tear-free formula.
In the presence of thick, dense scales, which are located not only on the scalp, but also in other areas, a good helper will be Milk crust cream which helps to completely remove milk crusts in an average of 7 days [5.3].
Atopic dermatitis
Atopic dermatitis is an allergic disease accompanied by chronic skin inflammation .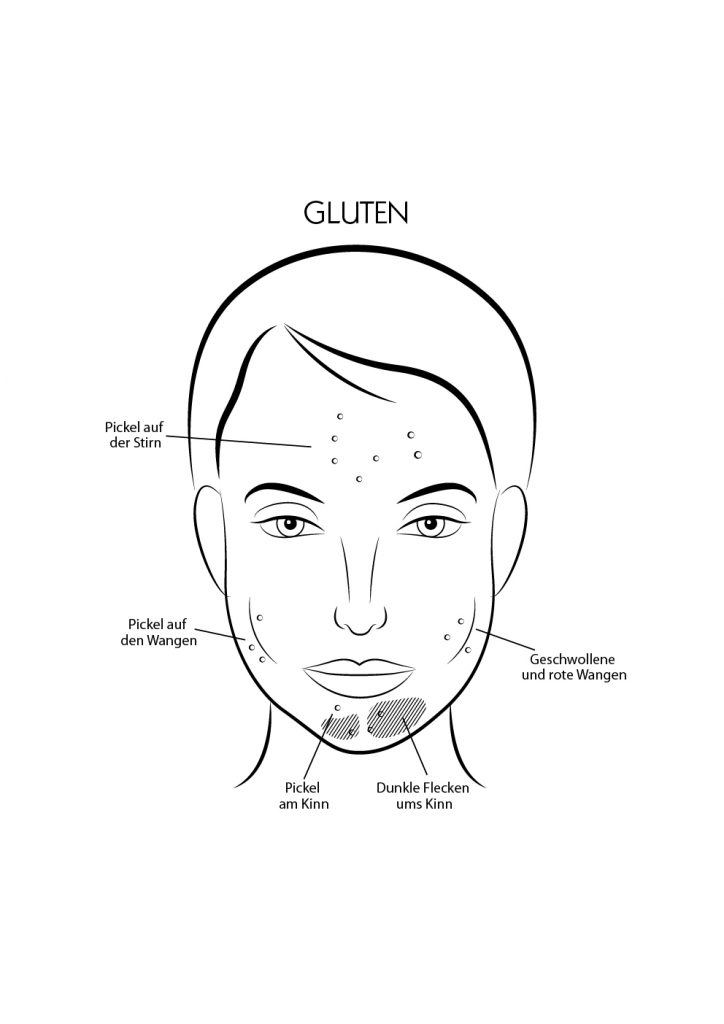 The causes of uncontrolled allergic reactions in infants are:
The causes of uncontrolled allergic reactions in infants are:
- food allergens - animal protein, soy products, some types of vegetables;
- airborne allergens - household dust, pollen, pet hair, tobacco smoke, etc.;
- pathogenic microflora - fungi, viruses, bacteria.
Newborns are most often diagnosed with erythematous-squamous form of atopic dermatitis with signs of an acute inflammatory reaction:
- hyperemia of the skin;
- peeling;
- flat small papules.
Red spots are localized on the arms and legs in the area of the folds , on the sides of the neck, on the back of the hands and on the cheeks.
Children with atopic dermatitis are advised to regularly cleanse and moisturize their skin [6]. Anti-inflammatory drugs are prescribed only for extensive skin lesions that impair the quality of life of the baby - in this case, you should contact your pediatrician.
For daily care it is recommended to use STELATOPIA Emollient Cream . Studies [5.1] have shown that emollient:
- In 90% of cases reduces increased dryness of the skin [5.1] and reduces the likelihood of clinical signs of AD by 51% [10]
- Soothes itching in 91% of cases [5.1]
- Reduces inflammation after 32 hours [11]
Diaper dermatitis
This disease is better known as diaper rash and is accompanied by inflammation of the skin in the diaper area zone in infants. The rash appears as a result of prolonged contact of the body with wet diapers - the skin becomes excessively moist and defenseless against damaging factors (chemical, physical, infectious). The situation is aggravated by the simultaneous effect on the skin of children's feces that remain in a diaper or diaper.
Diaper dermatitis is not localized on the face - pimples in newborns appear on the lower abdomen, on the convex surfaces of the thighs and buttocks.
For non-drug treatment of pathology, air baths [7], bathing in a decoction of string and celandine [8], and thorough hygiene procedures are indicated. For the prevention of diaper dermatitis and redness, it is recommended to use Diaper Cream 1 2 3.
Useful properties of the product:
- reduces redness and irritation by 80% from the first application [5];
- does not interfere with skin breathing;
- reduces the risk of exacerbations by 74% [5];
- protects, repairs and soothes inflamed skin.
A number of dermatological diseases of newborns develop as a result of improper care, so parents should pay special attention to children's hygiene, and if the baby's condition worsens, immediately consult a doctor.
____________________________________________________________________________________________
Literature:
1. Bhatia J, Greer F, for the Committee on Nutrition of the American Academy of Pediatrics. The use of mixtures based on soy protein in infant feeding.// Pediatrics, 2008; 121:1062–1068.
The use of mixtures based on soy protein in infant feeding.// Pediatrics, 2008; 121:1062–1068.
2. Herani M.I., Ando I. Acne in infancy and acne genetics // Dermatology 2003. Volume 206. Number 1. pp. 24-28. DOI: 10.1159/000067819
3. Zanko NI Efficiency of new technologies for skin care in young children: Abstract of the thesis. dis. ... cand. honey. Sciences, M., 2000
4. Naldi L., Rebora A. Clinical practice. Seborrheic dermatitis.
N Engle Gee Med. 360(4):387-96 (2009 January).
5. Results of the study 1035 F4.
5.1 Study results 1016F10.01.02
5.2 Study results 1008F4.01.16
5.3 Study results 1042F3.01.24
Dermatol. 2005; 53: S214-S219.
7. Galliamova Yu.A. Diaper dermatitis and skin trauma in children. Attending doctor. – 2013; 9: 42-6.
8. Zverkova F.A. Skin diseases in young children. SPb.: Sotis, 1994.
9. Tamrazova OB, Zaslavsky DV Diseases of the sebaceous glands in infants. Medical advice. 2019; 2:152-160.
10. Atopic-prone skin: latest discoveries (Laboratoire Expansion Center for Development and Research)
Atopic-prone skin: latest discoveries (Laboratoire Expansion Center for Development and Research)
11. Inhibits the synthesis of inflammatory mediators. “A study of the activity of sunflower oil distillate on inflammatory mediators. June 2010»
Acne on the face and skin of a child - causes, symptoms and treatment of acne
Acne in children is one of the most common skin conditions, especially in adolescence. This is a violation of the hair follicles and sebaceous glands, which are clogged, leading to the formation of acne and cysts.
Acne or Acne vulgaris, by its medical name, is defined as an inflammation of the sebaceous glands. Most often this occurs during puberty, as a result of hormonal activity. In addition to pain and discomfort, acne in boys and girls is fraught with social isolation, the constant need to hide damage, low self-esteem, and in some cases even the development of anxiety and depression. That's why it's so important to understand what acne is and what are the most effective ways to treat it.
Acne is caused by overactivity of the sebaceous glands in the skin, which is caused by a natural increase in hormone synthesis during adolescence. Most often they appear in the face, back and chest.
About 70-80% of adolescents suffer from this problem with varying degrees of severity. Although acne is considered a disease of adolescents, it also appears in young children or adults as a reaction to hormonal changes.
When classified by age group, there are basically two types of acne:
-
In newborns and young children. The belief that acne only affects teenagers and adults is wrong. Babies, preschoolers and early schoolers, although not often, also suffer from acne. Newborns face this problem because their mothers pass hormones on to them shortly before birth. Acne also occurs when the stress of childbirth causes the baby's body to release these hormones.
-
Teenagers and adults. Acne affects 80% of people between the ages of 11 and 30.
 Usually occur during pubertal hormonal changes. The increased production of sex hormones during puberty makes the sebaceous glands more active.
Usually occur during pubertal hormonal changes. The increased production of sex hormones during puberty makes the sebaceous glands more active.
Table - Classification of childhood acne by age
| Form | Child's age |
|---|---|
| Neonatal | from birth to 6 weeks |
| Infantile (early childhood) | from 6 weeks to 12 months |
| Middle childhood | from one year to 7 years |
| Preadolescent | 7 to 12 years (in girls before menarche) |
Neonatal acne develops during a period of hormonal changes. In all forms of acne, additional provoking exogenous factors play a significant role.
Acne develops around the hair follicles and is formed from excessive sebum production. Increased secretion of sebum, combined with the presence of dead skin cells on the epidermis, leads to clogging of the hair shaft follicles, which is accompanied by the appearance of comedones.
Comedones are the same tiny sores with a white tip that turn black when exposed to oxygen. The exacerbation of the condition of acne is caused by the involvement of an infectious process. A moist and oily environment is a favorable substrate for the reproduction of acne bacilli (Propionibacterium acnes).
In the presence of bacteria, an inflammatory reaction develops, from pimples that form a red plaque on the top of the skin. The final sign of acne is called nodular acne, characterized by large inflammatory foci that can hurt and even leave scars after recovery.
There are several factors that increase the likelihood that a child will develop acne:
-
use of skin and hair care products containing chemicals that irritate the skin;
-
using alkaline soap and very hot water;
-
squeezing acne and combing the affected areas of the skin;
-
frequent stressful situations or constant nervous tension;
-
excessive sweating and dandruff.

Studying what causes acne in children helps find ways to prevent and treat the disease. This allows the child to overcome the stress and depression that he experiences due to acne on his skin.
Doctor's expert opinion
The cause of childhood acne can be endocrinopathies. That is why, if you have acne, you should definitely consult a doctor to exclude such severe pathologies as congenital adrenal hyperplasia, malignant testicular tumors, and polycystic ovary syndrome.
Kovaleva Natalia Vladimirovna Dermatologist, cosmetologist, trichologist
Pimples appear on any part of the body. However, most often they appear in places where there is a high concentration of sebaceous glands.
The most commonly affected areas in children with acne include:
-
Ears. Acne in the ears of a child is localized behind the auricle, along the edge and on the lobe, closer to the temporal region at the upper base.
 Pimples look like black dots or inflamed papules.
Pimples look like black dots or inflamed papules. -
Face. Acne on the face of a child is characterized by a few separate closed or open comedones. Closed ones are represented by yellowish or pearly white papules, the size of which varies from 1 to 2 mm. Over time, they turn into open comedones, which look like black dots.
-
Nose. Acne on the nose of a child acts as isolated pustules or papules - surrounded by a pink rim. They are characterized by rapid (1-2 weeks) spontaneous resolution.
Also, acne in children can be localized on the chest, upper back and neck. After the disappearance of acne on the skin, as a rule, there are no traces left. The situation is complicated by infection - the appearance of signs of inflammation (edema, redness around the periphery). The elements are transformed into pustules with a purulent discharge that has a yellow color. In this case, it is quite difficult to avoid marks on the skin.
Traditional medical treatment includes the use of topical ointments as prescribed by a doctor, along with oral antibiotic therapy or drugs intended for internal treatment.
External therapy most often involves the use of retinoid ointments, which reduce inflammation and help exfoliate the top layer of skin. Topical ointments can be used without a prescription. These preparations contain a small amount of active substance, therefore they are safe.
In addition to medical attention, it is important to remember that acne develops on moist areas of the skin, so maintaining proper hygiene is essential. Timely and thorough cleansing of the skin can significantly reduce inflammation. It is important to give preference to the prescribed care products, do not rub or scratch the wounds, as this will cause additional irritation and exacerbation of the inflammatory process.
You can use antibacterial drugs that will help eliminate the inflammatory reaction. Under no circumstances should you pop a blackhead, as this will spread a bacterial infection and can also lead to scarring of the skin.
Under no circumstances should you pop a blackhead, as this will spread a bacterial infection and can also lead to scarring of the skin.
Extra moisture and protection
Many people make the mistake of thinking that acne-prone skin doesn't need extra hydration. The truth is that adjusting the moisturizing emulsion can help balance sebum production throughout the day. Moisturizing emulsions are easily absorbed to help balance moisture levels and prevent flare-ups or irritation.
Acne-affected skin needs constant protection from solar radiation, as exposure to direct ultraviolet rays promotes sebum production. Choose sunscreen according to your age and skin type. It is recommended to give preference to products that do not contain parabens.
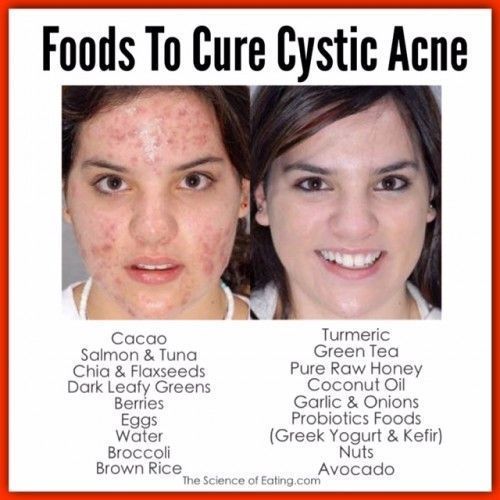
Nutrition and lifestyle
The process of acne is also affected by lifestyle. Nutrition, stress and hours of sleep also negatively affect the condition of the skin. It used to be that certain foods contributed to acne. Personalized diet is being promoted today:
Personalized diet is being promoted today:
-
it is recommended to reduce the consumption of sweet or spicy foods;
-
cutting down on foods that don't do any good mitigate the damage.
In addition to nutritional advice, omega-3 supplements should also be used. These are polyunsaturated fatty acids that the body cannot produce on its own, and they are found in marine fish oil or plant products. Their presence will help mitigate inflammation in the body, which means it will have a beneficial effect on all skin diseases and acne in particular.
If the problem disappears over time, no treatment is needed. Seek medical attention as soon as possible if acne scars or if there is a family history of skin disease.
At the RebenOK clinic in Moscow, competent dermatologists conduct appointments. If there are signs of infection, separable acne is taken for bacteriological examination. Treatment for acne in children mainly depends on the severity of the skin problem.
Because prevention is better than cure, there are a few habits you should teach your child to promote healthy skin and keep acne under control:
-
Wash your face with a mild cleanser every day.
-
Wash your hair regularly and braid it so it doesn't touch your face.
-
Wear loose, breathable and light cotton clothing.
Remember that a healthy lifestyle contributes greatly to the health of the child. Encourage adherence to a sleep-wake schedule and regular exercise. Also, an excellent prevention of acne is a balanced diet and personal hygiene.
If acne appears, contact the RebenOK clinic in Moscow, where pediatricians and dermatologists with extensive practical experience work. The medical center uses expert-class equipment, which greatly simplifies diagnostics. Contact our administrator at the number listed on the site to make an appointment and receive additional recommendations regarding the preparation for laboratory tests.