Injury at birth
Birth Injuries in Newborns - Children's Health Issues
By
Arcangela Lattari Balest
, MD, University of Pittsburgh, School of Medicine
Full review/revision Oct 2022
VIEW PROFESSIONAL VERSION
Topic Resources
Birth injury is damage that occurs as a result of physical pressure during the birthing process, usually during transit through the birth canal.
Many newborns have minor injuries during birth.
Infrequently, nerves are damaged or bones are broken.
Most injuries resolve without treatment.
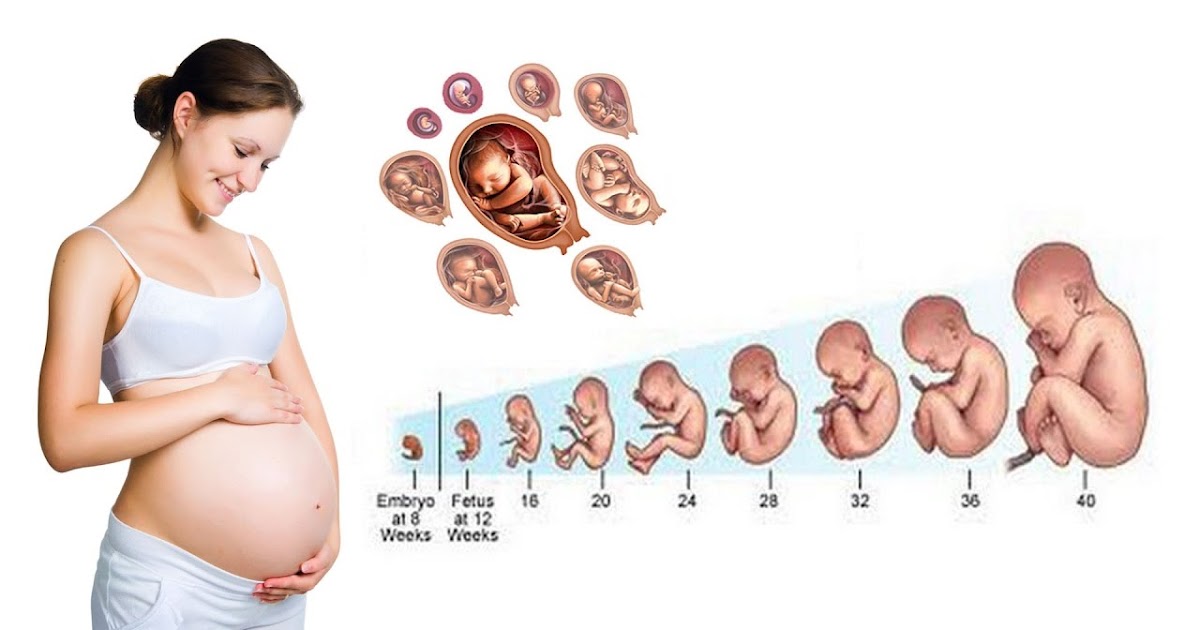
A difficult delivery, with the risk of injury to the baby, may occur with extremely large fetuses. Doctors recommend cesarean delivery Cesarean Delivery Cesarean delivery is surgical delivery of a baby by incision through a woman’s abdomen and uterus. In the United States, up to 30% of deliveries are cesarean. Doctors use a cesarean delivery... read more (C-section) when they estimate the baby weighs more than 11 pounds (more than 10 pounds when the mother has diabetes). Injury is also more likely when the fetus is lying in an abnormal position in the uterus before birth ( see Figure: Position and Presentation of the Fetus Position and Presentation of the Fetus ).
Birth injuries are most commonly due to the natural forces of labor and delivery. In the past, when risks of cesarean delivery were high, doctors did difficult deliveries by pulling the fetus out using forceps Operative Vaginal Delivery Operative vaginal delivery is delivery using a vacuum extractor or forceps. A vacuum extractor consists of a small cup made of a rubberlike material that is connected to a vacuum. It is inserted... read more (a surgical instrument with rounded edges that fit around the fetus's head). However, bringing the fetus down from high in the birth canal with forceps had a high risk of causing birth injury.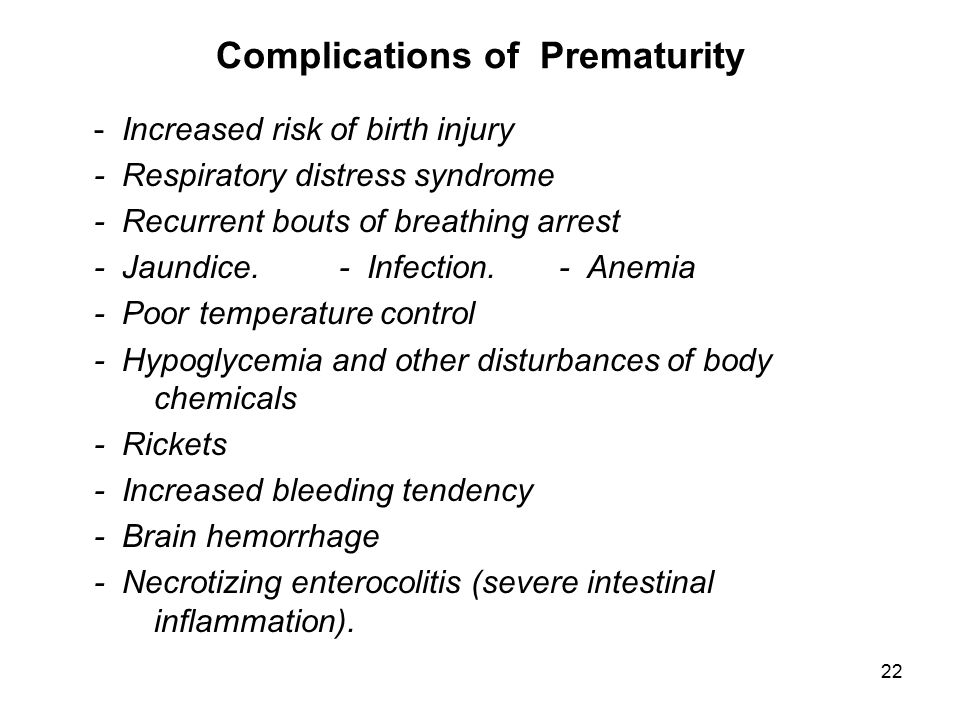 Today, forceps are used only in the final stages of delivery and rarely cause injury. Overall, the rate of birth injuries is much lower now than in previous decades because of improved prenatal assessment with ultrasonography Overview of General Problems in Newborns Problems in newborns may develop Before birth while the fetus is growing During labor and delivery After birth About 9% of newborns need special care after birth due to prematurity, problems... read more , the limited use of forceps, and because doctors often do cesarean delivery if they foresee an increased risk of birth injury.
Today, forceps are used only in the final stages of delivery and rarely cause injury. Overall, the rate of birth injuries is much lower now than in previous decades because of improved prenatal assessment with ultrasonography Overview of General Problems in Newborns Problems in newborns may develop Before birth while the fetus is growing During labor and delivery After birth About 9% of newborns need special care after birth due to prematurity, problems... read more , the limited use of forceps, and because doctors often do cesarean delivery if they foresee an increased risk of birth injury.
(See also Overview of General Problems in Newborns Overview of General Problems in Newborns Problems in newborns may develop Before birth while the fetus is growing During labor and delivery After birth About 9% of newborns need special care after birth due to prematurity, problems... read more .)
Position and Presentation of the Fetus
Toward the end of pregnancy, the fetus moves into position for delivery. An abnormal position is facing forward, and abnormal presentations include face, brow, breech, and shoulder. | |
Did You Know...
Head injury is the most common birth-related injury.
Head molding is not an injury. Molding refers to the normal change in shape of the baby's head that results from pressure on the head during delivery. In most births, the head is the first part to enter the birth canal. Because a fetus's skull bones are not rigidly fixed in position, the head elongates as it is pushed through the birth canal, which allows the fetus to pass through more easily. Molding does not affect the brain and does not cause problems or require treatment. The head shape gradually becomes more rounded over several days.
Swelling and bruising of the scalp is common but not serious and generally resolves within a few days.
Scalp scratches can occur when instruments (such as monitor leads attached to the scalp, forceps, or vacuum extractors Operative Vaginal Delivery Operative vaginal delivery is delivery using a vacuum extractor or forceps. A vacuum extractor consists of a small cup made of a rubberlike material that is connected to a vacuum. It is inserted... read more ) are used during a vaginal delivery.
Bleeding outside of the skull bones can lead to an accumulation of blood either above or below the thick fibrous covering (periosteum) of one of the skull bones.
A cephalhematoma is blood accumulation below the periosteum. Cephalohematomas feel soft and can increase in size after birth. Cephalohematomas disappear on their own over weeks to months and almost never require any treatment. However, they should be evaluated by the pediatrician if they become red or start to drain liquid. Sometimes some of the blood calcifies and leaves a hard lump in the scalp. The lump is not dangerous, is usually hidden by hair, and requires no treatment.
The lump is not dangerous, is usually hidden by hair, and requires no treatment.
A subgaleal hemorrhage is bleeding directly under the scalp above the periosteum covering the skull bones. Blood in this area can spread and is not confined to one area like a cephalohematoma. It can cause significant blood loss and shock Shock Shock is a life-threatening condition in which blood flow to the organs is low, decreasing delivery of oxygen and thus causing organ damage and sometimes death. Blood pressure is usually low... read more , which may even require a blood transfusion Overview of Blood Transfusion A blood transfusion is the transfer of blood or a blood component from one healthy person (a donor) to a sick person (a recipient). Transfusions are given to increase the blood's ability to... read more . A subgaleal hemorrhage may result from the use of forceps or a vacuum extractor, or may result from a blood clotting problem Overview of Blood Clotting Disorders Blood clotting (coagulation) disorders are dysfunctions in the body's ability to control the formation of blood clots. These dysfunctions may result in Too little clotting, leading to abnormal... read more .
These dysfunctions may result in Too little clotting, leading to abnormal... read more .
Fracture of one of the bones of the skull may occur before or during the birth process. Unless the skull fracture forms an indentation (depressed fracture), it generally heals rapidly without treatment.
Did You Know...
Bleeding in and around the brain (intracranial hemorrhage) is caused by the rupture of blood vessels and may be caused by
Prematurity Preterm (Premature) Newborns A preterm newborn is a baby delivered before 37 weeks of gestation. Depending on when they are born, preterm newborns have underdeveloped organs, which may not be ready to function outside of... read more increases the risk of intracranial hemorrhage.
Sometimes, intracranial hemorrhage occurs after a normal delivery in an otherwise well newborn. The cause of bleeding in these cases is unknown.
Bleeding in the brain is much more common among very preterm infants. Newborns who have bleeding disorders (such as hemophilia Hemophilia Hemophilia is a hereditary bleeding disorder caused by a deficiency in one of two blood clotting factors: factor VIII or factor IX. Several different gene abnormalities can cause the disorder... read more ) are also at increased risk of bleeding in the brain.
Newborns who have bleeding disorders (such as hemophilia Hemophilia Hemophilia is a hereditary bleeding disorder caused by a deficiency in one of two blood clotting factors: factor VIII or factor IX. Several different gene abnormalities can cause the disorder... read more ) are also at increased risk of bleeding in the brain.
Most infants with bleeding do not have symptoms, whereas others can be sluggish (lethargic), feed poorly, and/or have seizures.
Bleeding can occur in several places in and around the brain:
Subarachnoid hemorrhage is bleeding below the innermost of the two membranes that cover the brain. This is the most common type of intracranial hemorrhage in newborns, usually occurring in full-term newborns. Newborns with a subarachnoid hemorrhage may occasionally have apnea (periods when they stop breathing), seizures Seizures in Children Seizures are a periodic disturbance of the brain’s electrical activity, resulting in some degree of temporary brain dysfunction.
 When older infants or young children have seizures, they often... read more , or lethargy during the first 2 to 3 days of life but usually ultimately do well.
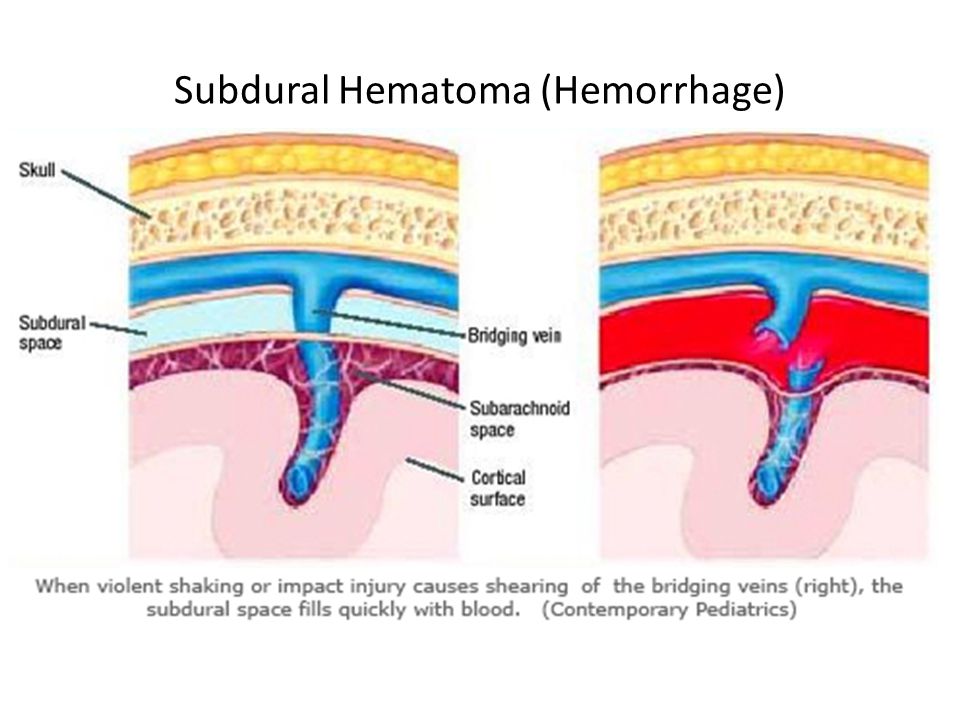
When older infants or young children have seizures, they often... read more , or lethargy during the first 2 to 3 days of life but usually ultimately do well.Subdural hemorrhage is bleeding between the outer and the inner layers of the brain covering. It is now much less common because of improved childbirth techniques. A subdural hemorrhage can put increased pressure on the surface of the brain. Newborns with a subdural hemorrhage may develop problems such as seizures.
Epidural hematoma is bleeding between the outer layer (dura mater) of tissue covering the brain (meninges) and the skull. An epidural hematoma may be caused by a skull fracture. If the hematoma increases the pressure in the brain, the soft spots between skull bones (fontanelles) may bulge. Newborns with an epidural hematoma may have apnea or seizures.
Intraventricular hemorrhage is bleeding into the normal fluid-filled spaces (ventricles) in the brain.
Intraparenchymal hemorrhage occurs into the brain tissue itself. Intraventricular hemorrhages and intraparenchymal hemorrhages usually occur in very preterm newborns Preterm (Premature) Newborns A preterm newborn is a baby delivered before 37 weeks of gestation. Depending on when they are born, preterm newborns have underdeveloped organs, which may not be ready to function outside of... read more and occur more typically as a result of an underdeveloped brain rather than a birth injury. Most of these hemorrhages do not cause symptoms, but large ones may cause apnea or a bluish gray discoloration to the skin, or the newborn's entire body may suddenly stop functioning normally. Newborns who have large hemorrhages have a poor prognosis, but those with small hemorrhages usually survive and do well.
Newborns who have a hemorrhage may be admitted to a neonatal intensive care unit Neonatal intensive care unit (NICU) Problems in newborns may develop Before birth while the fetus is growing During labor and delivery After birth About 9% of newborns need special care after birth due to prematurity, problems. .. read more (NICU) for imaging tests (such as a CT scan or MRI) and monitoring, supportive care (such as warmth), fluids given by vein (intravenously), and other treatments to maintain body function.
.. read more (NICU) for imaging tests (such as a CT scan or MRI) and monitoring, supportive care (such as warmth), fluids given by vein (intravenously), and other treatments to maintain body function.
Bleeding Around the Brain
Bleeding may occur in several areas in and around the brain. |
Nerve injuries may occur before or during delivery. These injuries usually cause weakness of the muscles controlled by the affected nerve. Nerve injuries may involve the
Facial nerve: Lopsided facial expression
Brachial plexus: Arm and/or hand weakness
Phrenic nerve (rare): Difficulty breathing
Spinal cord (rare): Paralysis
Facial nerve injury is evident when the newborn cries and the face appears lopsided (asymmetric). The facial nerve is the nerve injured most often. This injury is caused by pressure against the nerve due to
The way the fetus was positioned in the uterus before birth
The nerve being pressed against the mother's pelvis during delivery
Forceps used to assist the delivery
No treatment of facial nerve injury is needed, and the muscle weakness usually resolves by 2 to 3 months of age. However, sometimes facial nerve weakness is caused by a congenital disorder rather than an injury and does not resolve.
However, sometimes facial nerve weakness is caused by a congenital disorder rather than an injury and does not resolve.
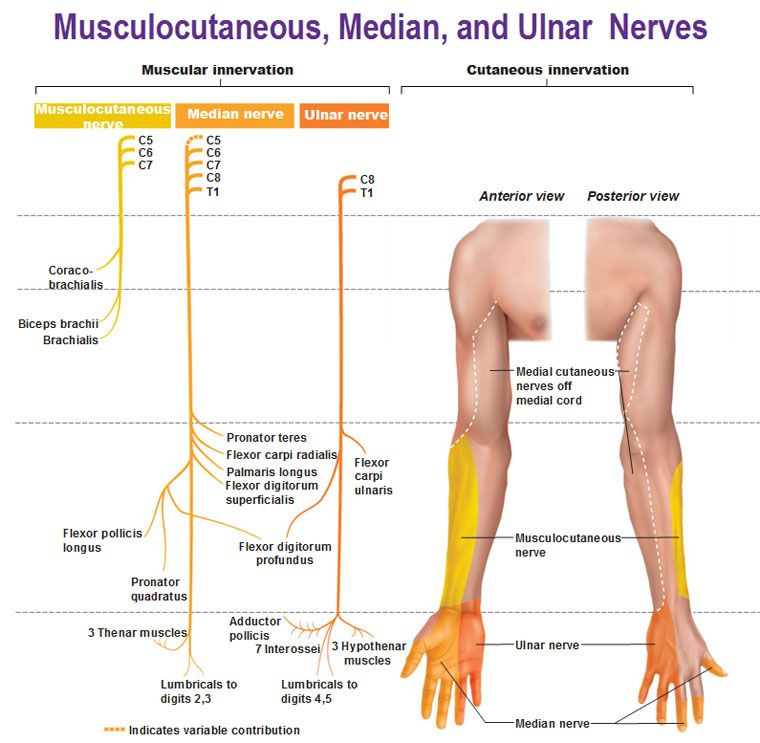
The brachial plexus is a group of large nerves located between the neck and shoulder, leading to each arm. During a difficult delivery, one or both of the baby's arms can be stretched and injure the nerves of the brachial plexus ( see Plexus Disorders Plexus Disorders Plexuses (networks of interwoven nerve fibers from different spinal nerves) may be damaged by injury, tumors, pockets of blood (hematomas), or autoimmune reactions. Pain, weakness, and loss... read more ) and cause weakness or paralysis of part or all of the baby's arm and hand. Weakness of the shoulder and elbow is called Erb palsy, and weakness of the hand and wrist is called Klumpke palsy. About half of the cases of brachial plexus injuries are related to difficult deliveries, typically involving large babies, and about half occur in babies with normal deliveries. Brachial plexus injury is less frequent in babies delivered by cesarean delivery. Extreme movements at the shoulder should be avoided to allow the nerves to heal. Many milder injuries resolve over a few days. If the abnormality is more severe or lasts for more than 1 or 2 weeks, physical therapy or occupational therapy for proper positioning and gentle movement of the arm are recommended. If there is no improvement over 1 or 2 months, doctors typically recommend the baby be evaluated by a pediatric neurologist and/or orthopedist at a pediatric specialty hospital to see whether surgery may be beneficial.
Extreme movements at the shoulder should be avoided to allow the nerves to heal. Many milder injuries resolve over a few days. If the abnormality is more severe or lasts for more than 1 or 2 weeks, physical therapy or occupational therapy for proper positioning and gentle movement of the arm are recommended. If there is no improvement over 1 or 2 months, doctors typically recommend the baby be evaluated by a pediatric neurologist and/or orthopedist at a pediatric specialty hospital to see whether surgery may be beneficial.
The phrenic nerve, which is the nerve going to the diaphragm (the muscular wall that separates the organs of the chest from those of the abdomen and assists in breathing), is occasionally damaged, resulting in paralysis of the diaphragm on the same side. In this case, the newborn may have difficulty breathing and sometimes requires assistance with breathing. Injury of the phrenic nerve usually resolves completely within a few weeks.
Spinal cord injuries due to overstretching during delivery are extremely rare. These injuries can result in paralysis below the site of the injury. Damage to the spinal cord is often permanent. Some spinal cord injuries that occur high up in the neck are fatal because they prevent the newborn from breathing properly.
These injuries can result in paralysis below the site of the injury. Damage to the spinal cord is often permanent. Some spinal cord injuries that occur high up in the neck are fatal because they prevent the newborn from breathing properly.
Other nerves, such as the radial nerve in the arm, the sciatic nerve in the lower back, or the obturator nerve in the leg, also may be injured during delivery.
Bones may be broken (fractured) before or during delivery even when the delivery is normal.
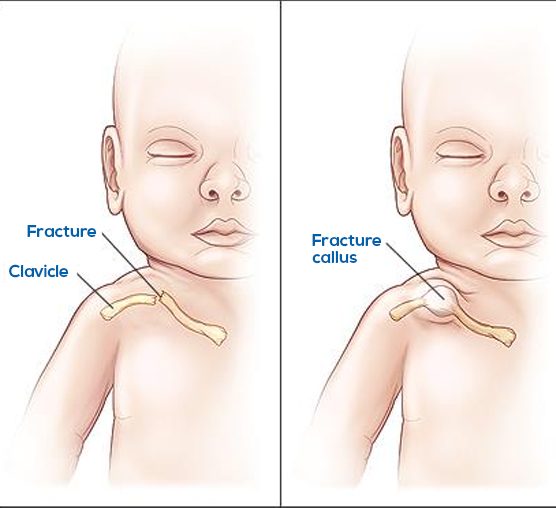
A fracture of the collarbone (clavicle) is relatively common, occurring in 1 to 2% of newborns. Sometimes these fractures are not recognized until several days after birth when a lump of tissue forms around the fracture. Clavicle fractures do not seem to bother newborns and need no treatment. Healing is complete over a few weeks.
Fractures of the upper arm bone (humerus) or upper leg bone (femur) sometimes occur. Doctors usually apply a loose splint to limit movement.
 These fractures may cause pain with movement in the first few days. These fractures usually heal well unless the head of the bone (where growth occurs) is involved.
These fractures may cause pain with movement in the first few days. These fractures usually heal well unless the head of the bone (where growth occurs) is involved.Fractures of multiple bones can occur in newborns with certain genetic conditions in which the bones are very fragile.
The newborn’s skin may have minor injuries after delivery, especially areas that receive pressure during contractions or that first emerge from the birth canal during delivery. Instruments needed for delivery, such as forceps Operative Vaginal Delivery Operative vaginal delivery is delivery using a vacuum extractor or forceps. A vacuum extractor consists of a small cup made of a rubberlike material that is connected to a vacuum. It is inserted... read more , can injure the skin. Swelling and bruising may occur around the eyes and on the face during face-first deliveries and on the genitals after breech deliveries (see Abnormal Presentations Abnormal Presentations Position refers to whether the fetus is facing rearward (toward the woman’s back—that is, face down when the woman lies on her back) or forward (face up).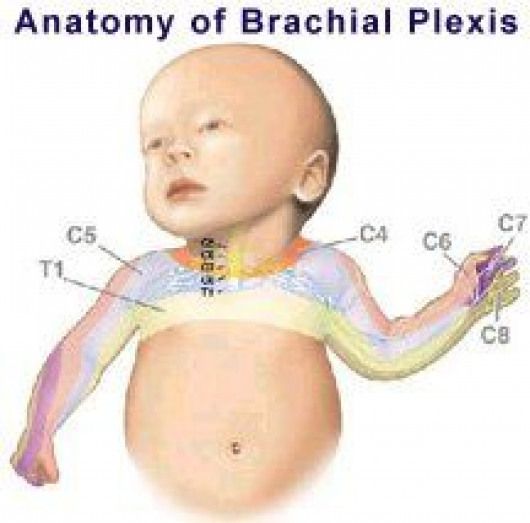 It’s important to check the baby’s... read more ). No treatment for these bruises is needed.
It’s important to check the baby’s... read more ). No treatment for these bruises is needed.
Use of instruments during delivery and stress on the newborn (such as caused by asphyxia) can injure the fat under the skin (called subcutaneous fat necrosis of the newborn). This skin injury can look like red, firm, raised areas on the trunk, arms, thighs, or buttocks. This type of injury usually resolves on its own over weeks to months.
Perinatal asphyxia is a decrease in blood flow to the baby's tissues or a decrease in oxygen in the baby's blood before, during, or just after delivery. Some common causes include the following:
Separation of the placenta from the uterus before delivery (placental abruption Placental Abruption Placental abruption is the premature detachment of the placenta from the wall of the uterus, usually after 20 weeks of pregnancy. Women may have abdominal pain and tenderness and vaginal bleeding... read more )
Obstruction of umbilical cord blood flow
Abnormal development of the fetus (for example, when there is a genetic abnormality)
Severe infection in the fetus
Exposure to certain drugs or medications before birth
Severe maternal hemorrhage
Severe maternal illness
Sometimes the exact cause of perinatal asphyxia cannot be identified.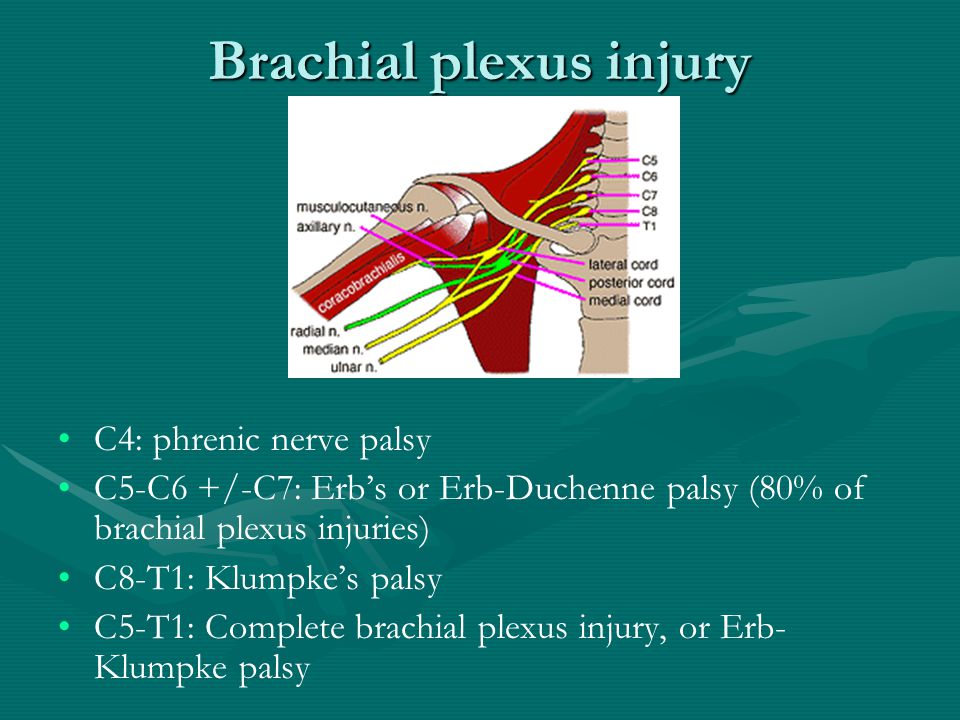
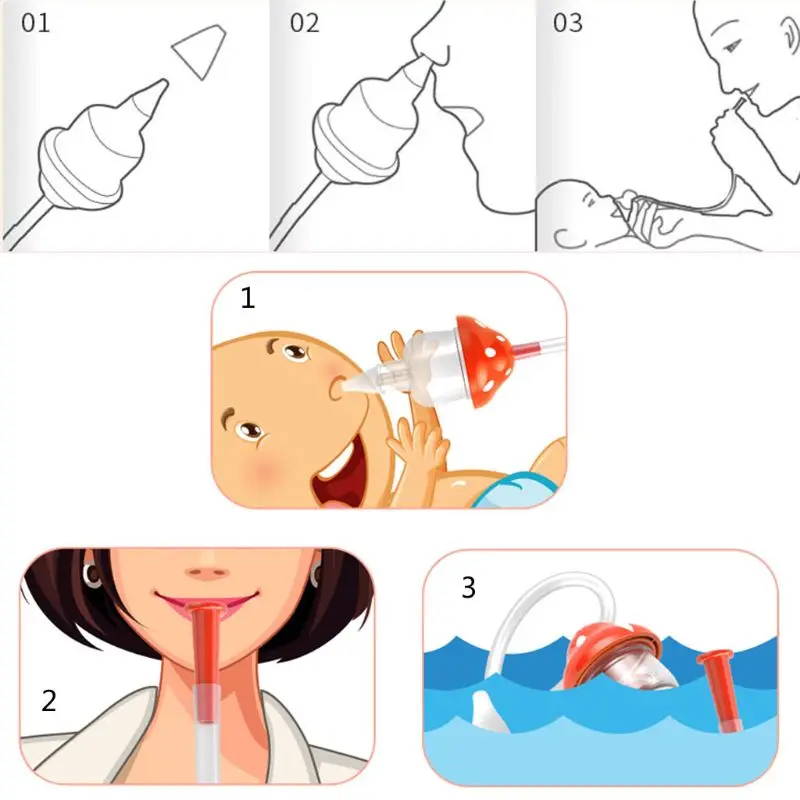
Regardless of the cause, affected newborns appear pale and lifeless at birth. They breathe weakly or not at all and have a very slow heart rate. They need to be revived (resuscitated) after delivery. Resuscitation may include use of a resuscitation bag and mask to push air into the lungs or insertion of a breathing tube in the newborn's throat (endotracheal intubation). If asphyxia resulted from rapid blood loss, the newborn may be in shock Shock Shock is a life-threatening condition in which blood flow to the organs is low, decreasing delivery of oxygen and thus causing organ damage and sometimes death. Blood pressure is usually low... read more . They are immediately given fluids by vein, and sometimes a blood transfusion Overview of Blood Transfusion A blood transfusion is the transfer of blood or a blood component from one healthy person (a donor) to a sick person (a recipient). Transfusions are given to increase the blood's ability to... read more .
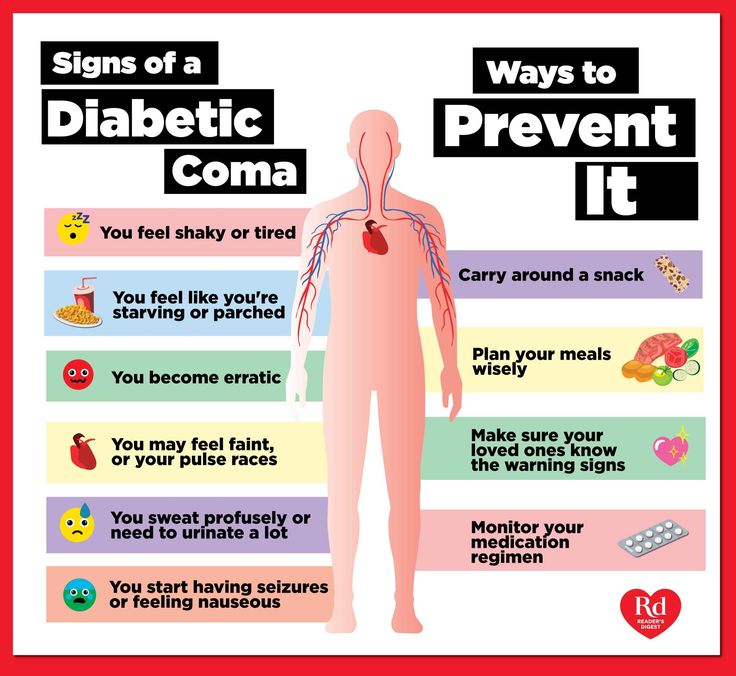
Newborns with asphyxia may show signs of injury to one or more organ systems, including the following:
Heart: Poor color, low blood pressure
Lungs: Difficulty breathing and low oxygen levels
Brain: Lethargy, seizures, or even coma
Kidneys: Reduced output of urine
Liver: Difficulty making proteins that are needed for blood to clot normally
Intestines: Difficulty digesting milk
Blood forming system: Low platelet count and bleeding
Newborns may need medications to help their heart function and a mechanical ventilator Mechanical Ventilation Mechanical ventilation is use of a machine to aid the movement of air into and out of the lungs.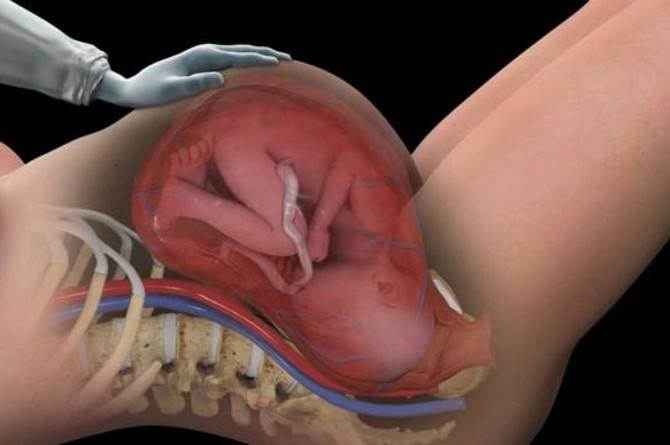 Some people with respiratory failure need a mechanical ventilator (a machine that helps air get... read more to support their breathing. Some newborns who have been revived may benefit from having their body temperature lowered below the normal temperature of 98.6° F (37° C) for 72 hours. Blood cell transfusions and plasma may be necessary to manage problems with the blood forming system. Most of the organs damaged by perinatal asphyxia recover over a week, but brain damage may persist.
Some people with respiratory failure need a mechanical ventilator (a machine that helps air get... read more to support their breathing. Some newborns who have been revived may benefit from having their body temperature lowered below the normal temperature of 98.6° F (37° C) for 72 hours. Blood cell transfusions and plasma may be necessary to manage problems with the blood forming system. Most of the organs damaged by perinatal asphyxia recover over a week, but brain damage may persist.
Survivors who have minimal injury to the brain may be completely normal. Survivors who have moderate to severe injury to the brain may have permanent signs of damage, ranging from mild learning disorders Learning Disorders Learning disorders involve an inability to acquire, retain, or broadly use specific skills or information, resulting from deficiencies in attention, memory, or reasoning and affecting academic... read more to delayed development to cerebral palsy Cerebral Palsy (CP) Cerebral palsy refers to a group of conditions that involve difficulty moving and muscle stiffness (spasticity). It results from brain malformations that occur before birth as the brain is developing... read more . Some severely asphyxiated infants do not survive.
It results from brain malformations that occur before birth as the brain is developing... read more . Some severely asphyxiated infants do not survive.
VIEW PROFESSIONAL VERSION
Copyright © 2023 Merck & Co., Inc., Rahway, NJ, USA and its affiliates. All rights reserved.
Test your knowledge
Take a Quiz!Birth injury (to the mother)
Birth injury (to the mother) | Pregnancy Birth and Baby beginning of content4-minute read
Listen
What is birth injury?
Birth injuries are physical injuries experienced during childbirth, and can affect either the mother or the baby.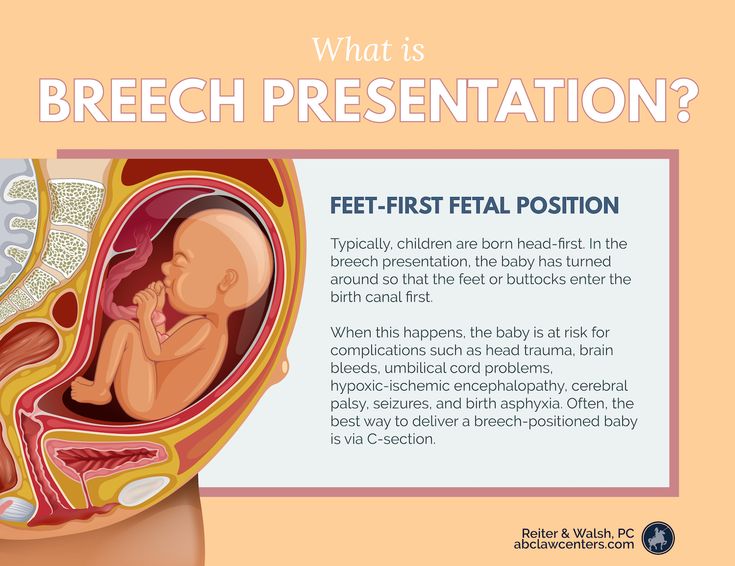 In newborn babies, a birth injury (often called 'neonatal birth trauma') can include many things, from bruising to a broken bone.
In newborn babies, a birth injury (often called 'neonatal birth trauma') can include many things, from bruising to a broken bone.
In mothers, birth injuries range from tearing in the vaginal area to damage to the pelvic floor.
Birth injuries in mothers typically fall into 2 main categories:
Injuries to the perineal area
- Perineal tears and episiotomy — around 3 in 4 women who give birth vaginally experience 'perineal trauma' (a tear or surgical cut to the area between the vagina and anus).
- Nerve damage — occasionally, nerves in the perineal area can get damaged during childbirth, which can lead to a painful condition called pudendal neuralgia.
- Haemorrhoids (piles) — these are swollen veins around the anus that you might feel as lumps. While they can be painful or itchy, they are usually not serious.
Injuries to the pelvic floor
- Muscle damage — the 'pelvic floor' is a group of muscles inside the pelvis that helps hold the uterus, bladder and bowel in place.
 In up to half of all women who give birth vaginally, there are permanent changes to the pelvic floor due to over-stretching or tearing (avulsion).
In up to half of all women who give birth vaginally, there are permanent changes to the pelvic floor due to over-stretching or tearing (avulsion). - Pelvic organ prolapse — if the pelvic muscles are damaged or weakened, the organs inside the pelvis can drop down towards the vagina, causing bladder and bowel problems.
While these birth injuries are physical, many mothers can experience emotional or psychological distress — before, during or after the birth. This is known as birth trauma. There are ways to decrease your risk of birth trauma, and both treatment and support are available.
What causes birth injury?
If you suffer a birth injury, the cause was most likely something out of your control.
Some of the main risk factors for birth injury include:
- the position of the baby, such as in a breech birth
- having a large baby (over 4kg)
- having a very quick or very long labour
- labour complications
- assisted delivery using forceps or ventouse (vacuum)
- having a small or unusually shaped pelvis
Can birth injury be prevented?
Although it's often not possible to prevent birth injury, there are some things you can do during pregnancy to reduce your risk:
- Exercise regularly (make sure you do pregnancy safe exercise).
- Strengthen your pelvic muscles with daily pelvic floor exercises.
- Avoid getting constipated or straining on the toilet, as this can weaken your pelvic muscles.
- Giving birth by caesarean could prevent some birth injuries, but this is major surgery so carries health risks of its own.
How is birth injury treated?
Some birth injuries are minor and may heal on their own — for example, a minor perineal tear or graze. Other injuries need treatment at the time, such as a deeper tear that needs stitches. You may also need some pain relief.
If you had a more serious birth injury, such as a significant tear or damage to the muscles of the pelvic floor, treatment may include physiotherapy and exercises to strengthen your pelvic floor muscles. Some women may need to use pessaries in their vagina or surgery to repair a prolapse.
Sometimes, signs of pelvic floor damage or prolapse are not detected and treated until much later.
If you have had a birth injury, you may be at more risk of it happening again with your next baby. Your doctor will talk to you about whether you should consider a planned caesarean section next time.
Your doctor will talk to you about whether you should consider a planned caesarean section next time.
If you experience any ongoing symptoms, such as pelvic pain or bladder and bowel problems, you should see your doctor.
Resources and support
- Talk to your doctor, midwife or obstetrician.
- You can call Pregnancy, Birth and Baby on 1800 882 436 to speak with a maternal child health nurse (7 days a week, 7am to midnight AET).
- The Continence Foundation of Australia offers information and support to people with bowel and bladder problems. You can call the helpline on 1800 33 00 66 between 8am and 8pm (AEST), Monday to Friday.
- Visit the Australasian Birth Trauma Association website for information and support, including peer-to-peer support.
- Visit the PANDA (Perinatal Anxiety & Depression Australia) website for information and support after a traumatic birth. You can call the PANDA national helpline on 1300 726 306 ((Mon to Fri, 9am to 7.
 30pm AEST).
30pm AEST).
Sources:
Mater Mothers Hospital (Labour and birth - assisted vaginal birth), Medical Hypotheses (The significance of incomplete skull fracture in the birth injury), Stanford Children's Health (Birth injury), Australian Commission on Safety and Quality in Health Care (Neonatal birth trauma), Medscape (Birth trauma), Merck Manual (Birth injuries in newborns), Australian Institute of Health and Welfare (Australia's mothers and babies data visualisations perineal status), PANDA (Childbirth trauma), Cerebral Palsy Alliance Research Foundation (What causes cerebral palsy)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: May 2021
Back To Top
Related pages
- Birth trauma (emotional)
- Birth injury (to the baby)
- When birth doesn't go to plan
Need more information?
Psychological Trauma - Birth Trauma
Read more on Australasian Birth Trauma Association website
What is Birth Trauma? - Birth Trauma
The delivery of a baby is a positive event for many women, but for some it can be a mixed experience or even very negative, resulting in physical and/or
Read more on Australasian Birth Trauma Association website
Birth trauma (emotional)
Birth trauma affects many women.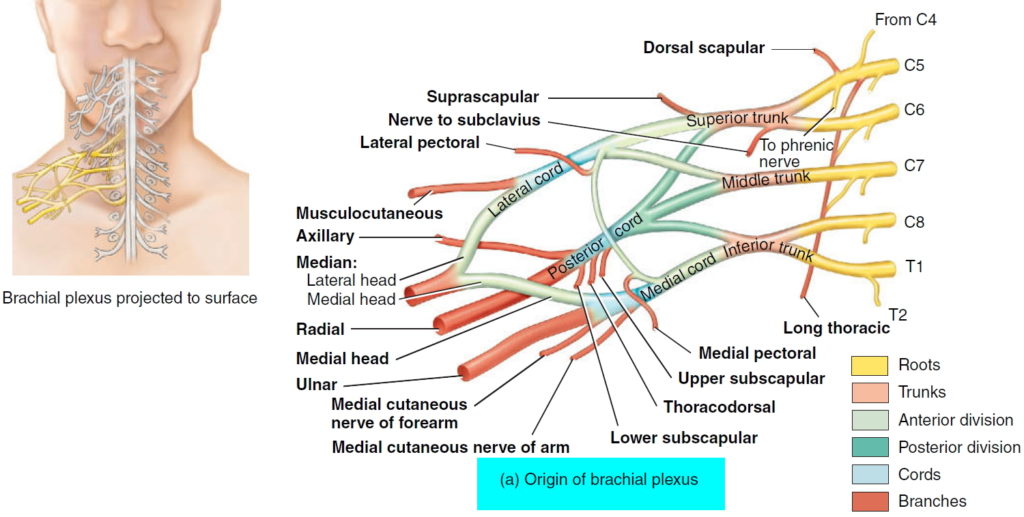 But there are ways to reduce your risk of an emotionally traumatic childbirth, while support and treatment are available if you experience symptoms.
But there are ways to reduce your risk of an emotionally traumatic childbirth, while support and treatment are available if you experience symptoms.
Read more on Pregnancy, Birth & Baby website
Early Postnatal - Birth Trauma
The early postnatal period is a time of emotional change for most women. Some women may experience distress or symptoms of depression at this time if they
Read more on Australasian Birth Trauma Association website
Family & Friends - Birth Trauma
If you are reading this then you may have someone close to you that has been impacted by a difficult birth experience, be it a partner, loved one or someone
Read more on Australasian Birth Trauma Association website
Placental abruption - Better Health Channel
Placental abruption means the placenta has detached from the wall of the uterus, starving the baby of oxygen and nutrients.
Read more on Better Health Channel website
Birth and beyond - Ngala
Exciting times are ahead!Birth comes after lots of anticipation and preparation
Read more on Ngala website
Looking after your body after having a baby
Over the last 9 months, your body has had to change to accommodate your growing baby and preparing to give birth.
Read more on Pregnancy, Birth & Baby website
Bladder weakness after birth
Leaking urine after childbirth is very common. It can be embarrassing and inconvenient, but there are ways to improve bladder weakness.
Read more on Pregnancy, Birth & Baby website
Birth injury (to the baby)
While some babies do experience birth injury, giving birth in Australia is very safe. Most birth injuries to babies are temporary, and in many cases treatment is available.
Most birth injuries to babies are temporary, and in many cases treatment is available.
Read more on Pregnancy, Birth & Baby website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Subscribe to newsletters
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.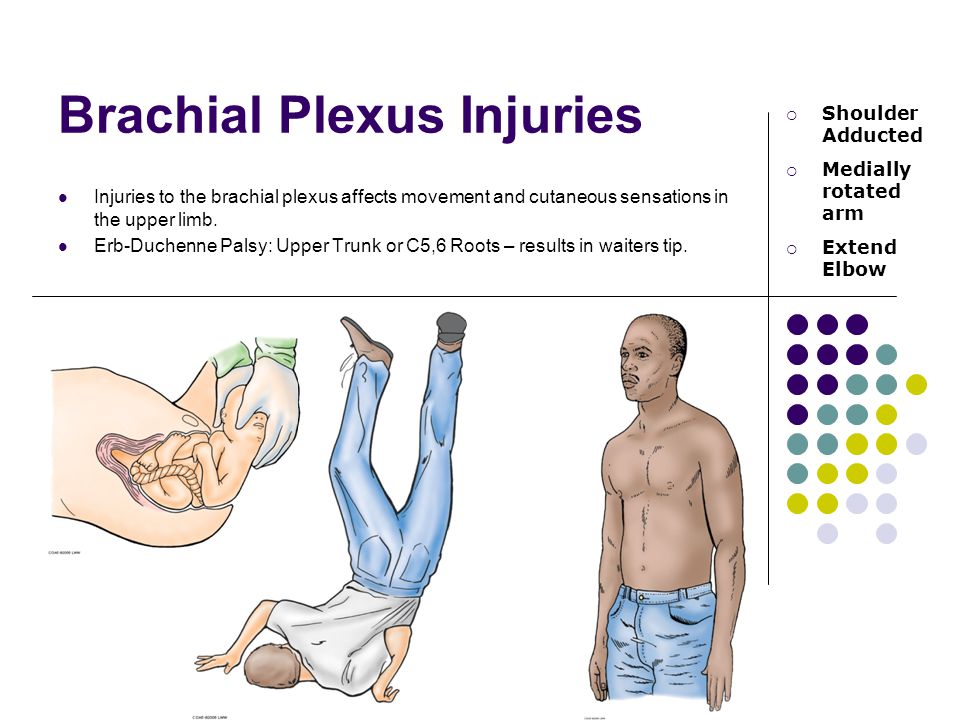
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
Healthdirect Australia acknowledges the Traditional Owners of Country throughout Australia and their continuing connection to land, sea and community. We pay our respects to the Traditional Owners and to Elders both past and present.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Birth trauma of newborns.
 What is birth trauma in newborns?
What is birth trauma in newborns? IMPORTANT
The information in this section should not be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
Birth trauma of newborns - various injuries to the fetus that occur during the birth act. Among the birth injuries of newborns, there are injuries to soft tissues (skin, subcutaneous tissue, muscles), the skeletal system, internal organs, and the central and peripheral nervous systems. Birth trauma in newborns is diagnosed taking into account the mother's obstetric and gynecological history, characteristics of the course of labor, examination data of the newborn and additional studies (EEG, ultrasound, radiography, ophthalmoscopy, etc.). Treatment of birth injuries of newborns is carried out differentially, taking into account the type and severity of the injury.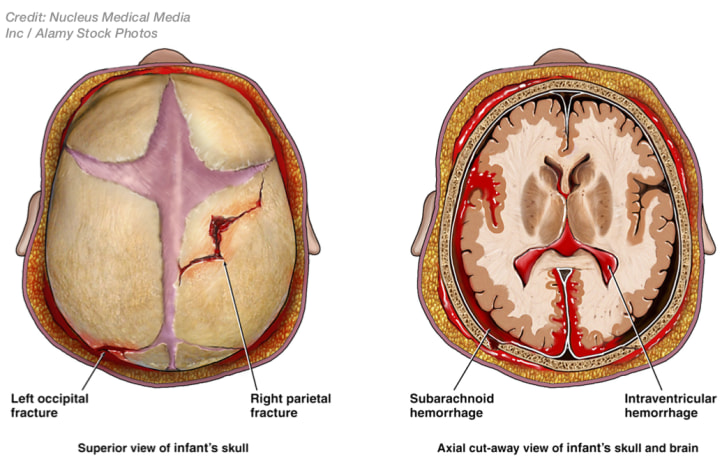
- Classification of birth injuries of newborns
- Causes
- Different types of neonatal injuries
- Birth injuries of soft tissues
- Birth injuries of the skeletal system
- Birth injuries of internal organs
- Birth injuries of the central and peripheral nervous system
- Prophylaxis
- Prices for treatment
General
Under the birth trauma of newborns understand the violation of the integrity of the tissues or organs of the child, due to the mechanical forces acting in the process of childbirth. Birth injuries are diagnosed in 8-11% of newborns. Birth injuries of newborns are often combined with birth injuries of the mother (ruptures of the vulva, vagina, perineum, uterus, urogenital and vagina-rectal fistulas, etc.). Birth injuries of newborns can have a serious impact on the further physical health and intellectual development of the child. All this makes birth traumatism one of the most urgent problems of obstetrics and gynecology, neonatology and pediatrics, pediatric neurology and traumatology.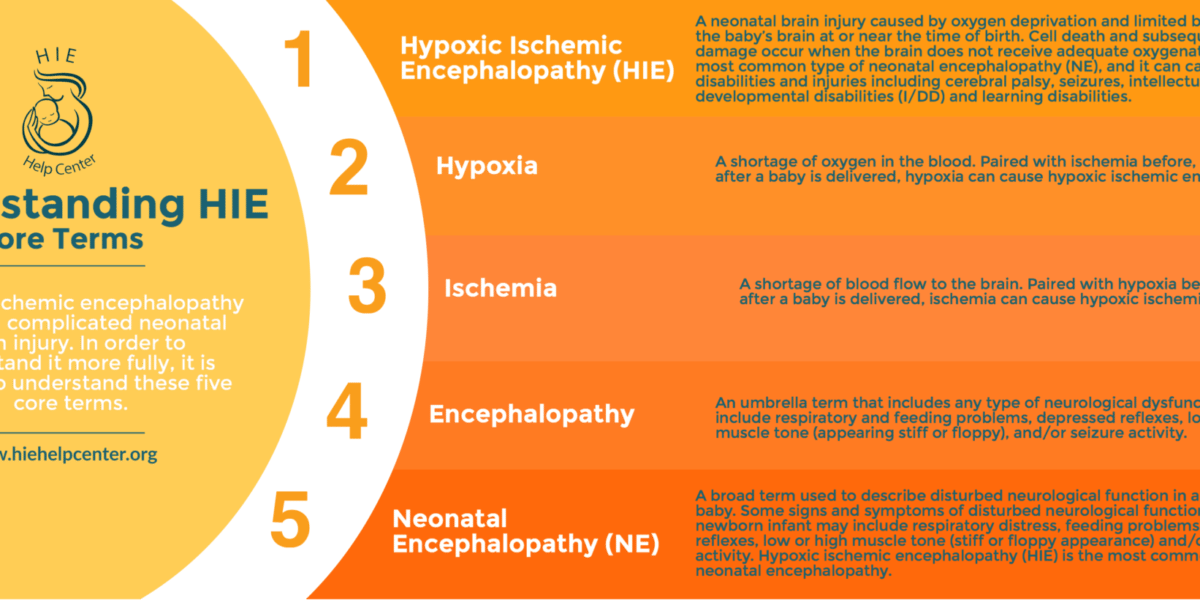
Birth trauma in newborns
Classification of birth injuries of newborns
Depending on the location of the damage and the predominant dysfunction, the following types of birth trauma of newborns are distinguished:
1. Birth injuries of soft tissues (skin, subcutaneous tissue, muscles, birth tumor, cephalohematoma).
2. Birth injuries of the osteoarticular system (cracks and fractures of the clavicle, humerus and femurs; traumatic epiphyseolysis of the humerus, subluxation of the C1 and C2 joints, damage to the bones of the skull, etc.).
3. Birth injuries of internal organs (hemorrhages in internal organs: liver, spleen, adrenal glands).
4. Birth injuries of the central and peripheral nervous system in newborns:
- intracranial birth trauma (epidural, subdural, subarachnoid, intraventricular hemorrhages)
- birth injury of the spinal cord (bleeding into the spinal cord and its membranes)
- birth injury of the peripheral nervous system (damage to the brachial plexus - Duchenne-Erb paresis/paralysis or Dejerine-Klumpke palsy, total paralysis, paresis of the diaphragm, damage to the facial nerve, etc.
 ).
).
Causes
An analysis of the causes of birth trauma in newborns allows us to identify three groups of factors that increase the likelihood of its occurrence: those related to the mother, to the fetus, as well as to the course and management of childbirth.
Predisposing "maternal" factors may be early or late reproductive age, gestosis, narrow pelvis, hypoplasia or hyperanteflexia of the uterus, diseases of the pregnant woman (cardiovascular, endocrine, gynecological, etc.), post-term pregnancy, occupational hazards, etc.
The most extensive group of causes leading to birth trauma in newborns is the circumstances associated with the fetus. Birth injury can be provoked by breech presentation of the fetus, oligohydramnios, incorrect (asynclitic or extensor insertion of the head), prematurity, large fetal size, fetal abnormalities, intrauterine hypoxia and asphyxia, etc.
Anomalies of labor activity can lead to the birth trauma of a newborn: prolonged or rapid labor, labor stimulation with weak labor activity, discoordinated or excessively strong labor activity. A serious group of causes of birth injuries in newborns is the incorrect or unreasonable use of obstetric aids (turning the fetus on a leg, applying obstetric forceps, using a vacuum extractor, performing a caesarean section, etc.).
A serious group of causes of birth injuries in newborns is the incorrect or unreasonable use of obstetric aids (turning the fetus on a leg, applying obstetric forceps, using a vacuum extractor, performing a caesarean section, etc.).
As a rule, when birth injuries occur in newborns, there is a combination of a number of adverse factors that disrupt the normal biomechanics of childbirth.
Various types of neonatal injuries
Birth injuries of soft tissues
The most common manifestations of birth trauma in newborns are damage to the skin and subcutaneous tissue. These include scratches, abrasions, petechiae, ecchymosis in various parts of the body. Such damage is detected during a visual examination of the newborn by a neonatologist; usually they are not dangerous and require only local antiseptic treatment and the application of an aseptic dressing. Minor birth injuries of soft tissues disappear by the end of the first week of a newborn's life.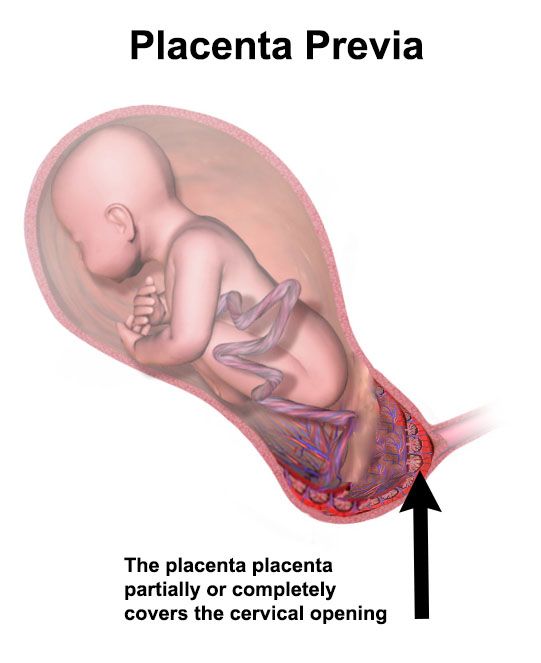
A type of birth trauma in newborns is a birth tumor, which is characterized by local swelling of the soft tissues of the head. The birth tumor has a soft elastic consistency, cyanotic color with multiple petechiae and ecchymosis. Its occurrence is usually associated with prolonged labor in the cephalic presentation or the imposition of obstetric forceps. The birth tumor does not require treatment, it disappears on its own after 1-3 days.
A more severe type of birth injury in newborns is damage (hemorrhage, rupture) of the sternocleidomastoid muscle, usually its lower third. In this case, a small tumor of moderately dense or doughy consistency is determined at the site of damage. Damage to the sternocleidomastoid muscle may not be detected immediately, but after about a week, when the child develops torticollis. In the treatment of a birth injury of the sternocleidomastoid muscle in newborns, a corrective head position is used with the help of rollers, dry heat, potassium iodide electrophoresis, massage; in case of inefficiency - surgical correction.
Cephalhematoma, as a kind of birth trauma of newborns, is characterized by hemorrhage under the periosteum of the parietal or occipital bones of the skull. Typical signs of cephalohematoma are an elastic consistency, absence of pulsation, painlessness, fluctuation, and the presence of a roller along the periphery. In the future, newborns with cephalohematoma may experience jaundice caused by increased extravascular production of bilirubin. Cephalhematoma decreases in size by 2-3 weeks of life, and completely resolves by the end of 6-8 weeks. Complications of subperiosteal birth trauma of newborns include anemia, calcification and suppuration of cephalohematoma. Children with large (more than 6 cm in diameter) cephalohematomas need an X-ray of the skull to rule out bone fractures. Since cephalohematomas in premature babies are often associated with intrauterine mycoplasmosis, PCR or ELISA diagnostics is required.
In most cases, birth injuries of soft tissues in newborns pass without consequences.
Birth injuries of the skeletal system
Among birth injuries of the osteoarticular system in newborns, injuries of the clavicle and bones of the extremities are more common. They always refer to purely obstetric types of damage. Subperiosteal fractures of the clavicle without displacement are usually detected 3-4 days after delivery by the presence of a fusiform dense swelling - forming callus. A fracture of the clavicle with displacement is accompanied by the inability to perform active movements, pain, crying with passive movement of the arm, swelling and crepitus over the fracture site.
With a fracture of the humerus or femur, there are no active movements in the limbs, there is a pain reaction to passive movements, there is swelling, deformity and shortening of the damaged limb. For all types of fractures, newborns need to consult a pediatric traumatologist, conduct x-ray diagnostics (radiography of the collarbone, radiography of tubular bones). In case of a clavicle fracture, a short-term immobilization of the arm is performed by applying a Dezo bandage or tight swaddling. In case of fractures of the humerus and femur, the bones of the upper or lower limb are repositioned and a plaster cast is applied (if necessary, traction).
In case of a clavicle fracture, a short-term immobilization of the arm is performed by applying a Dezo bandage or tight swaddling. In case of fractures of the humerus and femur, the bones of the upper or lower limb are repositioned and a plaster cast is applied (if necessary, traction).
A type of birth trauma of the skeletal system of newborns is traumatic epiphysiolysis of the humerus. Its manifestations are pain, swelling and crepitus in the area of the shoulder or elbow joints, limited range of motion in the affected arm. The outcome of such an injury may be paresis of the radial nerve, the formation of flexion contracture in the joints. Treatment consists of immobilization of the limb, physiotherapy, massage.
Birth injuries of internal organs
Damage to internal organs occurs as a result of mechanical impact on the fetus during an abnormal course of childbirth. The most common hemorrhages are in the liver, spleen and adrenal glands. Clinical manifestations of birth trauma of internal organs in newborns develop on the 3rd-5th day due to internal bleeding. When a hematoma ruptures, abdominal distention occurs, intestinal paresis develops, muscular hypotension (or atony), inhibition of physiological reflexes, arterial hypotension, persistent regurgitation and vomiting.
Clinical manifestations of birth trauma of internal organs in newborns develop on the 3rd-5th day due to internal bleeding. When a hematoma ruptures, abdominal distention occurs, intestinal paresis develops, muscular hypotension (or atony), inhibition of physiological reflexes, arterial hypotension, persistent regurgitation and vomiting.
If a birth injury of the internal organs is suspected, the newborn is given a survey radiography of the abdominal cavity, ultrasound of the abdominal organs and ultrasound of the adrenal glands. Treatment consists in carrying out hemostatic and symptomatic therapy; if necessary - laparoscopy or laparotomy with revision of internal organs.
With a hemorrhage in the adrenal glands, the child may develop acute or chronic adrenal insufficiency. The prognosis for birth trauma of internal organs in newborns is determined by the volume and severity of the lesion, the timeliness of detection of damage.
Birth injuries of the central and peripheral nervous system
Damage to the nervous system in newborns is the most extensive group of birth injuries. As part of this review, we will focus on birth trauma of the spinal cord and peripheral nervous system; a detailed description of intracranial birth injuries of newborns will be given in the corresponding article.
As part of this review, we will focus on birth trauma of the spinal cord and peripheral nervous system; a detailed description of intracranial birth injuries of newborns will be given in the corresponding article.
Birth injuries of the spinal cord in newborns may include hemorrhage, sprain, compression, or rupture of the spinal cord at various levels, associated with or without a spinal fracture. Severe injuries are characterized by the clinic of spinal shock: lethargy, muscular hypotension, areflexia, weak cry, diaphragmatic breathing. The death of children can come from respiratory failure. In more favorable cases, there is a gradual regression of the phenomena of spinal shock; hypotension is replaced by spasticity; autonomic disorders develop (vasomotor reactions, sweating), trophic changes in muscle and bone tissue. Mild birth injuries in newborns are accompanied by transient neurological symptoms: changes in muscle tone, reflex and motor reactions.
Diagnosis is facilitated by examination of the child by a pediatric neurologist, X-ray or MRI of the spine, electromyography, lumbar puncture, and examination of cerebrospinal fluid. Treatment of a birth injury of the spinal cord in newborns includes immobilization of the damaged area, dehydration and antihemorrhagic therapy, restorative measures (orthopedic massage, exercise therapy, electrical stimulation, physiotherapy).
Treatment of a birth injury of the spinal cord in newborns includes immobilization of the damaged area, dehydration and antihemorrhagic therapy, restorative measures (orthopedic massage, exercise therapy, electrical stimulation, physiotherapy).
Birth injuries of the peripheral nervous system in newborns combine damage to the roots, plexuses, peripheral and cranial nerves.
Given the localization, the paresis of the brachial plexus (obstetric paresis) can be upper (proximal), lower (distal) or total. Upper Duchenne-Erb paresis is associated with damage to the plexuses and roots originating in the C5-C6 segments, which is accompanied by dysfunction of the proximal upper limb. In this case, the child takes a characteristic position with the arm brought to the body, extended at the elbow joint, turned inward at the shoulder and pronated at the forearm; with a hand bent in the palm and a head tilted to the sore shoulder.
With lower obstetric paresis of Dejerine-Klumpke, plexuses or roots originating from C7-T1 are affected, resulting in dysfunction of the distal arm. Manifestations include muscle hypotonia, hypesthesia, limitation of movements in the wrist and elbow joints, fingers, a symptom of "clawed paw". With a total type of obstetric paresis, the arm is completely inactive, muscle hypotension is pronounced, and muscle atrophy develops early.
Manifestations include muscle hypotonia, hypesthesia, limitation of movements in the wrist and elbow joints, fingers, a symptom of "clawed paw". With a total type of obstetric paresis, the arm is completely inactive, muscle hypotension is pronounced, and muscle atrophy develops early.
Diagnosis and localization of damage is specified using electromyography. Treatment of a birth injury of the brachial plexus in newborns consists in immobilizing the arm with a splint, performing massage, exercise therapy, physiotherapy (ozocerite, paraffin, electrical stimulation, electrophoresis), and drug therapy.
With paresis of the diaphragm, the newborn develops shortness of breath, paradoxical breathing, cyanosis, bulging of the chest on the affected side. The detection of paresis is facilitated by fluoroscopy and chest x-ray, which determine the high standing and inactivity of the dome of the diaphragm. Against this background, congestive pneumonia can develop in children. Treatment of birth trauma consists of transcutaneous stimulation of the phrenic nerve; if necessary - mechanical ventilation until adequate spontaneous breathing is restored.
Treatment of birth trauma consists of transcutaneous stimulation of the phrenic nerve; if necessary - mechanical ventilation until adequate spontaneous breathing is restored.
Paresis of the facial nerve is associated with damage to the trunk or branches of the facial nerve. In this case, the child has facial asymmetry, lagophthalmos, upward displacement of the eyeball when crying, asymmetry of the mouth, and difficulty in sucking. Birth trauma in newborns is diagnosed on the basis of clinical signs, electroneurography, registration of evoked potentials. Often, paresis of the facial nerve resolves without special treatment; in other cases, thermotherapy, drug therapy is carried out.
Rare types of birth injuries of newborns include injuries of the pharyngeal, median, radial, sciatic, peroneal nerve, lumbosacral plexus.
Prophylaxis
Prevention of birth injuries in newborns involves an assessment of the degree of risk of their occurrence even at the stage of pregnancy, the most careful attitude towards the child during childbirth, the rejection of unreasonable use of benefits for the extraction of the fetus and operative delivery.
Sources
- In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
Birth injuries: types, symptoms, complications
Birth injuries: types, symptoms, complications
Sometimes babies get injured during childbirth - according to statistics, about 10% of newborns need medical care. Birth injuries are not always easy to spot at a glance. They are easy to identify by characteristic signs that indicate the need for medical intervention. The sooner the child gets help, the less likely complications are.
Sometimes during childbirth, children are injured - according to statistics, about 10% of newborns require medical care. Birth injuries are not always easy to spot at a glance. They are easy to identify by characteristic signs that indicate the need for medical intervention. The sooner the child gets help, the less likely complications are.

Most common birth injuries
Medicine knows many of their types. The following deviations occur most frequently:
- injuries of cranial bones;
- damage to duplications of the dura mater;
- epidural hemorrhages;
- cephalohematomas;
- birth tumors.
They are also fraught with serious consequences that can greatly affect the child's quality of life. It is impossible to avoid complications without qualified medical care. Injuries received by the child during childbirth lead to the following complications:
- general developmental delay;
- delayed speech development;
- sleep disorders;
- epileptic syndrome;
- autism;
- clubfoot;
- cerebral palsy;
- hyperactivity;
- as well as a number of other diseases.
Damage affects the development of internal organs, the brain, the central nervous system, the spine, and the skeletal system.
 In the future, they can cause serious complications.
In the future, they can cause serious complications. How to recognize a birth injury?
The consequences, as a rule, are not immediately noticeable - the problem worsens gradually, in some cases the process is delayed for 2-3 years. There are characteristic signs that indicate the need to show the baby to a specialist:
- Restless behavior of the child;
- frequent regurgitation;
- hand or foot movement disorders;
- skull asymmetry;
- reflex disorders;
- sleep disorders.
These signs are expressed to a greater or lesser extent - sometimes violations are visible immediately, but in most cases only a specialist can determine them
Risk group
Children at risk must be examined by a specialist. How do you know if your baby is in this group? It includes children who have had a hard time coming into the world. This can be judged by the following signs:
- cesarean section;
- large fetal weight - over 4 kg;
- state of hypoxia;
- cephalohematoma - swelling on the skull of a newborn;
- induction of labor and obstetric manipulations.

 Normally, the position of a fetus is facing rearward (toward the woman’s back) with the face and body angled to one side and the neck flexed, and presentation is head first.
Normally, the position of a fetus is facing rearward (toward the woman’s back) with the face and body angled to one side and the neck flexed, and presentation is head first.