Oxytocin milk production
Oxytocin - Drugs and Lactation Database (LactMed)
Summary of Use during Lactation
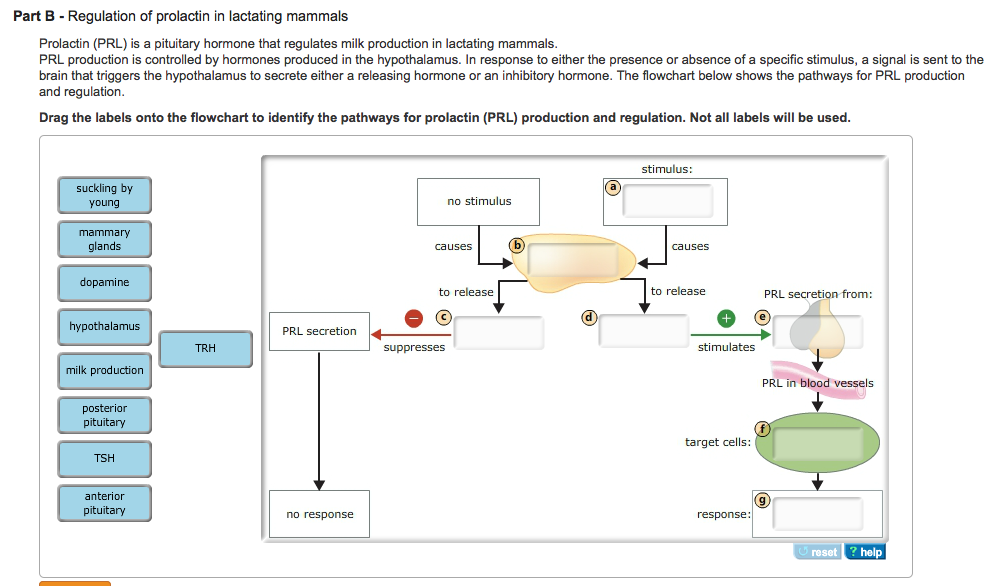
Oxytocin is an essential lactation hormone released during breastfeeding that causes milk ejection and appears to have calming effect on the mother.[1] Administration of exogenous oxytocin to mothers having difficulty in breastfeeding has not been clearly shown to have a beneficial effect on lactation success or in the treatment of breast engorgement. It might be of benefit in women who have lost the neuronal connection between the breast and hypothalamus. Effects on the infant are unlikely when given during breastfeeding.
Numerous studies suggest that oxytocin given during labor can negatively affect breastfeeding, possibly by reducing sucking behavior in the newborn in a dose-dependent manner, or by decreasing postpartum oxytocin release although study methodology and consistency has varied considerably.[2-15] This effect might be most important during the initiation of breastfeeding, but may not persist after lactation is established. [16] One study found that only oxytocin in conjunction with epidural analgesia reduced breastfeeding, but not oxytocin alone.[17] Another study found that all rhythmic reflexes, the antigravity reflex, and total primitive neonatal reflexes were inhibited by intrapartum oxytocin administration, unrelated to dose, which could adversely affect breastfeeding.[18] Some evidence exists that peripartum oxytocin administration might increase the risk of postpartum depression.[15]
Drug Levels
Maternal Levels. Relevant published information was not found as of the revision date.
Infant Levels. Relevant published information was not found as of the revision date.
Effects in Breastfed Infants
Relevant published information was not found as of the revision date.
Effects on Lactation and Breastmilk
Intranasal oxytocin is reportedly used by some midwives in Switzerland as a galactogogue.[19] It has been used as part of regimens used by adoptive mothers who wish to breastfeed. [20]
[20]
A small study found no difference in symptoms between subcutaneous oxytocin 2.5 international units daily and placebo after 3 days of treatment for breast engorgement.[21,22]
An early randomized, placebo-controlled trial used oxytocin nasal spray in the mothers of newborns, but lactation management fell far short of what is considered acceptable nowadays. The study found that the spray might be useful in decreasing breast engorgement slightly in the mothers of fullterm infants, but no difference was found in the average infant weight loss between birth and day 4 in the oxytocin and placebo groups.[23]
Two similarly designed trials studied oxytocin nasal spray in mothers of preterm newborns who were pumping milk for their infants. The first studied mothers of infants born before 38 weeks and used a total of 3 units of intranasal oxytocin (Syntocinon-Sandoz, 40 units/mL) before pumping each breast for10 minutes a breast pump four times daily. Among primiparous mothers, milk production during days 2 to 5 days postpartum was 1964 mL in those who used oxytocin and 510 mL in those who received placebo spray.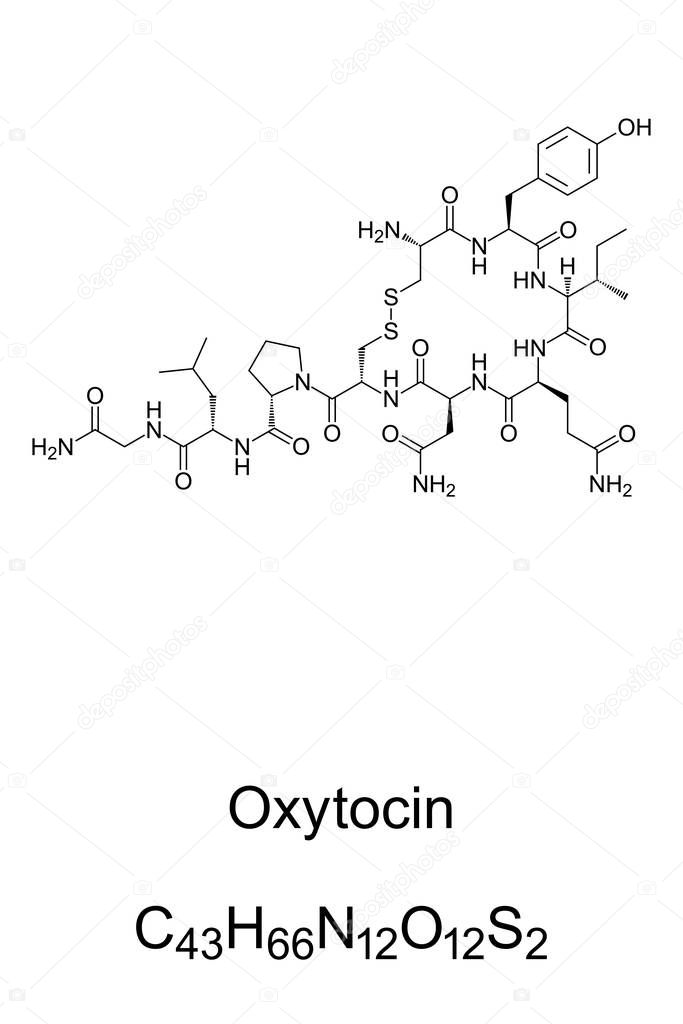 Because of the large and statistically significant effect of oxytocin among primiparous women, the trial was stopped after only 8 primiparous mothers had been studied. No statistically significant difference was found between oxytocin and placebo among 4 multiparous women who were attempting to breastfeed for the first time. The paper did not report giving the mothers any instructions in lactation technique.[24]
Because of the large and statistically significant effect of oxytocin among primiparous women, the trial was stopped after only 8 primiparous mothers had been studied. No statistically significant difference was found between oxytocin and placebo among 4 multiparous women who were attempting to breastfeed for the first time. The paper did not report giving the mothers any instructions in lactation technique.[24]
Fifty-one mothers who delivered an infant of less than 35 weeks gestation were studied. Twenty-seven mothers used 4 units of intranasal oxytocin (Syntocinon-Novartis, 40 units/mL), and 24 mothers received an identical placebo spray before pumping with a breast pump. All mothers were given instructions on using hand massage before pumping and advised to pump every 3 hours. No difference in milk production over the first 5 days postpartum was found between mothers who received oxytocin (median 667 mL) and placebo (median 530 mL), although women receiving oxytocin produced slightly more milk on day 2 of the study.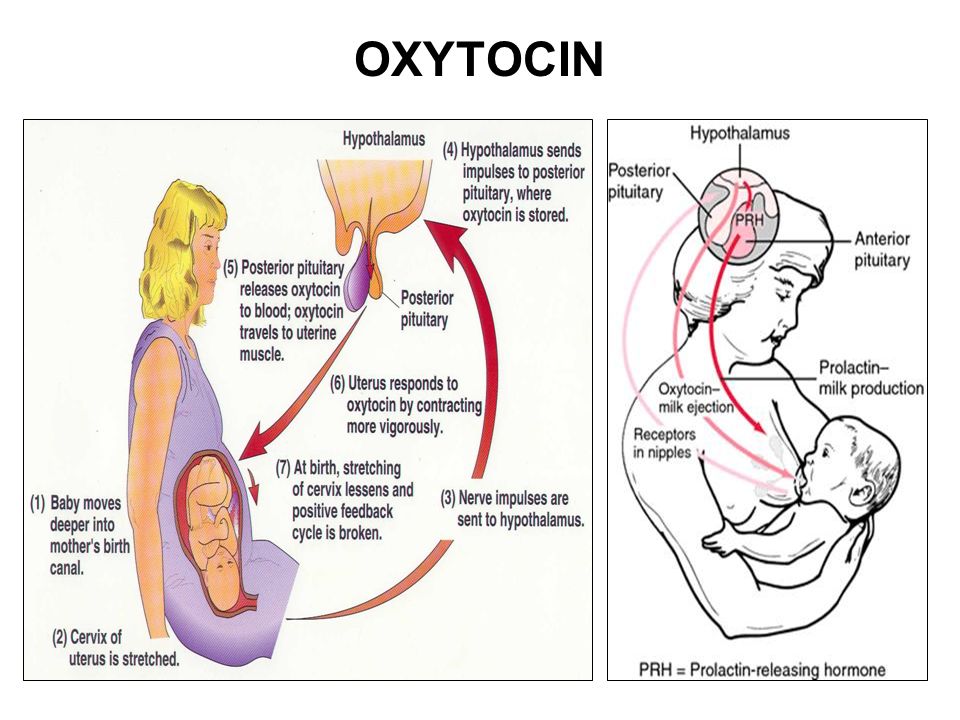 Parity had no effect in this study.[25]
Parity had no effect in this study.[25]
Several factors might explain the differences in findings between the studies. Because of the great interpatient variability in milk production documented in the recent study and the small number of patients in the first study, the finding in the earlier study may have been due to chance. A 50% higher dose of oxytocin was used in the first study, which may have caused a greater effect. Another plausible explanation is the good lactation support given to mothers in the recent larger study that seemed to be lacking in the early study.
Two case reports indicate that oxytocin nasal spray may facilitate letdown in tetraplegic women who have lost the neuronal connection between the nipple and the hypothalamus.[26]
A study of mothers who received oxytocin during labor found that on the second day postpartum, oxytocin infusion decreased endogenous oxytocin levels dose-dependently. Epidural analgesia in combination with oxytocin infusion influenced endogenous oxytocin levels negatively. Oxytocin infusion also increased serum prolactin.[14]
Oxytocin infusion also increased serum prolactin.[14]
Logistic regression of data from 585 mothers who had epidural analgesia during labor found that mothers who had received exogenous oxytocin had a 3.3 times greater risk of delayed onset of lactation than women who did not.[7]
An observational study of 20 primiparous women found that those who were exclusively breastfeeding at 3 months (63%) had received a lower dose of oxytocin during labor (mean total dosage 1363 milliIunits) than those who were not exclusively breastfeeding (mean total dosage 3088 milliIunits). This result was attributed to an inhibitory effect on neonatal sucking by the infant caused by oxytocin.[2]
A small, nonrandomized cohort study found that the newborn infants whose mothers received synthetic oxytocin to induce or maintain labor had a decreased level of prefeeding organization one hour after birth.[6]
A retrospective cohort study in Spain compared breastfeeding outcomes between mothers who received oxytocin during labor (n = 189) and mothers who did not, including those who delivered via elective Cesarean section (n = 127).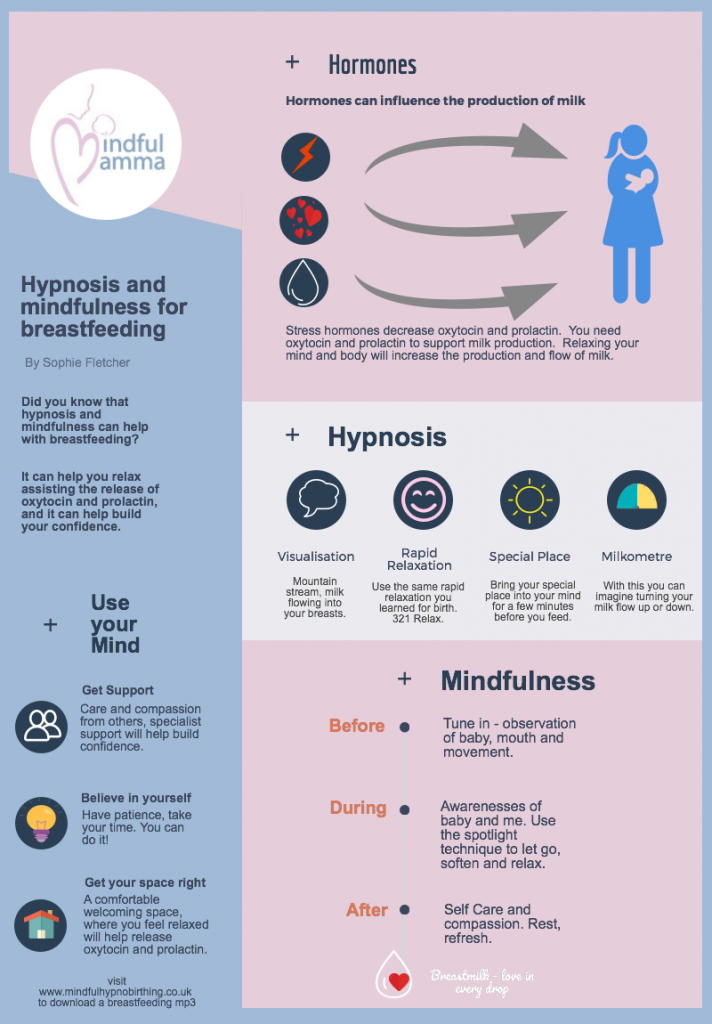 Mothers who received oxytocin during the first and second stages of labor had a 45% increased risk of bottle feeding and a 129% increased risk of breastfeeding discontinuation by 3 months of age. Effects were most pronounced in women under 27 years of age.[5]
Mothers who received oxytocin during the first and second stages of labor had a 45% increased risk of bottle feeding and a 129% increased risk of breastfeeding discontinuation by 3 months of age. Effects were most pronounced in women under 27 years of age.[5]
A small prospective study in California compared women who received an epidural infusion of fentanyl and ropivacaine to mothers who did not receive an epidermal during labor. All mothers had normal vaginal deliveries and their infants had 1 uninterrupted hour of skin-to-skin contact immediately postpartum. The study found inverse relationships between the amount of fentanyl and the amount of oxytocin received during labor and the time of the first suckling. Because women who received more fentanyl also tended to receive more oxytocin, the study could not clearly separate the effects of the two drugs.[9]
A small prospective cohort study in Spain followed mothers by telephone postpartum to determine their breastfeeding status. Mothers who had received oxytocin during labor were breastfeeding at a similar rate as those who had not at 1, 3 and 6 months postpartum.[27]
Mothers who had received oxytocin during labor were breastfeeding at a similar rate as those who had not at 1, 3 and 6 months postpartum.[27]
A nonblinded, nonrandomized study compared breastfeeding among the infants of mothers who received oxytocin during delivery (n = 70) and those who did not (n = 90) in two Iranian hospitals. Mothers were primiparous and infants were full term. Infant breastfeeding behavior was assessed to be either successful or unsuccessful within 2 hours of delivery. Infants whose mothers received oxytocin were judged to successfully breastfeed 48.6% compared to 82.2% among the infants of mothers who did not receive oxytocin. Use of opiate pain relievers in the two groups was not stated.[28]
A retrospective cohort study compared breastfeeding results between women who did and did not receive oxytocin during labor. After correcting for confounding factors, the study found that exogenous oxytocin impaired breastfeeding during the first hour postpartum, but not at 3 months postpartum. High pregestational body mass index was the best predictor of an impaired third month's postpartum breastfeeding.[12]
High pregestational body mass index was the best predictor of an impaired third month's postpartum breastfeeding.[12]
A retrospective case-control study conducted in two hospitals in central Iran compared breastfeeding behaviors in the first 2 hours postdelivery by infants of 4 groups of primiparous women with healthy, full-term singleton births who had vaginal deliveries. The groups were those who received no medications during labor, those who received oxytocin plus scopolamine, those who received oxytocin plus meperidine, and those who received oxytocin, scopolamine and meperidine. The infants in the no medication group performed better than those in all other groups, and the oxytocin plus scopolamine group performed better than the groups that had received meperidine.[13]
A prospective cohort study in Spain found no relationship between oxytocin dose during labor or postpartum with the duration of breastfeeding. However, elective cesarean section without oxytocin resulted in the greatest risk of stopping exclusive breastfeeding. [29]
[29]
An observational study in Sweden compared nursing behaviors of the infants of mothers who received intravenous oxytocin or intramuscular oxytocin with or without receiving epidural analgesia with sufentanil and bupivacaine. Infants of mothers who received oxytocin infusions alone during labor breastfed as well as those of mothers who had no interventions during labor. Mothers who received oxytocin plus epidural analgesia had reduced breastfeeding behaviors and more weight loss at 2 days postpartum than those who did not receive epidural analgesia. The mothers of infants who breastfed well had greater variability in serum oxytocin than those whose infants did not breastfeed well.[17]
References
- 1.
Niwayama R, Nishitani S, Takamura T, et al. Oxytocin mediates a calming effect on postpartum mood in primiparous mothers. Breastfeed Med. 2017;12:103–9. [PubMed: 28103103]
- 2.
Olza Fernández I, Marin Gabriel M, Malalana Martínez A, et al.
 Newborn feeding behaviour depressed by intrapartum oxytocin: A pilot study. Acta Paediatr. 2012;101:749–54. [PubMed: 22452314]
Newborn feeding behaviour depressed by intrapartum oxytocin: A pilot study. Acta Paediatr. 2012;101:749–54. [PubMed: 22452314]- 3.
Jonas W, Nissen E, Ransjö-Arvidson AB, et al. Influence of oxytocin or epidural analgesia on personality profile in breastfeeding women: a comparative study. Arch Womens Ment Health. 2008;11:335–45. [PubMed: 18726143]
- 4.
Jordan S, Emery S, Watkins A, et al. Associations of drugs routinely given in labour with breastfeeding at 48 hours: Analysis of the Cardiff births survey. BJOG. 2009;116:1622–9. [PubMed: 19735379]
- 5.
García-Fortea P, González-Mesa E, Blasco M, et al. Oxytocin administered during labor and breast-feeding: A retrospective cohort study. J Matern Fetal Neonatal Med. 2014;27:1598–603. [PubMed: 24289796]
- 6.
Bell AF, White-Traut R, Rankin K. Fetal exposure to synthetic oxytocin and the relationship with prefeeding cues within one hour postbirth. Early Hum Dev.
 2013;89:137–43. [PubMed: 23084698]
2013;89:137–43. [PubMed: 23084698]- 7.
Wiklund I, Norman M, Uvnäs-Moberg K, et al. Epidural analgesia: breast-feeding success and related factors. Midwifery. 2009;25:e31–8. [PubMed: 17980469]
- 8.
Davey MA, Gibson KL. Intervention in labour and early breastfeeding outcomes. Arch Dis Child Fetal Neonatal Ed 2014;99:A81. Abstract. doi:10.1136/archdischild-2014-306576.231. [CrossRef]
- 9.
Brimdyr K, Cadwell K, Widstrom AM, et al. The association between common labor drugs and suckling when skin-to-skin during the first hour after birth. Birth. 2015;42:319–28. [PMC free article: PMC5057303] [PubMed: 26463582]
- 10.
Gu V, Feeley N, Gold I, et al. Intrapartum synthetic oxytocin and its effects on maternal well-being at 2 months postpartum. Birth. 2016;43:28–35. [PubMed: 26554749]
- 11.
Erickson EN, Emeis CL. Breastfeeding outcomes after oxytocin use during childbirth: An integrative review.
 J Midwifery Womens Health. 2017;62:397–417. [PubMed: 28759177]
J Midwifery Womens Health. 2017;62:397–417. [PubMed: 28759177]- 12.
Gomes M, Trocado V, Carlos-Alves M, et al. Intrapartum synthetic oxytocin and breastfeeding: A retrospective cohort study. J Obstet Gynaecol. 2018;38:745–9. [PubMed: 29523035]
- 13.
Hemati Z, Abdollahi M, Broumand S, et al. Association between newborns' breastfeeding behaviors in the first two hours after birth and drugs used for their mothers in labor. Iran J Child Neurol. 2018;12:33–40. [PMC free article: PMC5904736] [PubMed: 29696044]
- 14.
Jonas W, Johansson LM, Nissen E, et al. Effects of intrapartum oxytocin administration and epidural analgesia on the concentration of plasma oxytocin and prolactin, in response to suckling during the second day postpartum. Breastfeed Med. 2009;4:71–82. [PubMed: 19210132]
- 15.
Monks DT, Palanisamy A. Oxytocin: At birth and beyond. A systematic review of the long-term effects of peripartum oxytocin.
 Anaesthesia. 2021;76:1526–37. [PubMed: 34389972]
Anaesthesia. 2021;76:1526–37. [PubMed: 34389972]- 16.
Takács L, Bartoš F, Čepický P, et al. The effects of intrapartum administration of synthetic oxytocin on breastfeeding in the first 9 months postpartum: A longitudinal prospective study. Breastfeed Med. 2021;16:965–70. [PubMed: 34463162]
- 17.
Takahashi Y, Uvnäs-Moberg K, Nissen E, et al. Epidural analgesia with or without oxytocin, but not oxytocin alone, administered during birth disturbs infant pre-feeding and sucking behaviors and maternal oxytocin levels in connection with a breastfeed two days later. Front Neurosci. 2021;15:673184. [PMC free article: PMC8276259] [PubMed: 34267623]
- 18.
Marín Gabriel MA, Olza Fernández I, Malalana Martínez AM, et al. Intrapartum synthetic oxytocin reduce the expression of primitive reflexes associated with breastfeeding. Breastfeed Med. 2015;10:209–13. [PMC free article: PMC4410763] [PubMed: 25785487]
- 19.
Winterfeld U, Meyer Y, Panchaud A, et al.
 Management of deficient lactation in Switzerland and Canada: A survey of midwives' current practices. Breastfeed Med. 2012;7:317–8. [PubMed: 22224508]
Management of deficient lactation in Switzerland and Canada: A survey of midwives' current practices. Breastfeed Med. 2012;7:317–8. [PubMed: 22224508]- 20.
Cazorla-Ortiz G, Obregón-Guitérrez N, Rozas-Garcia MR, et al. Methods and success factors of induced lactation: A scoping review. J Hum Lact. 2020;36:739–49. [PubMed: 32926655]
- 21.
Ingelman-Sundberg A. Early puerpereal breast engorgement. Acta Obstet Gynecol Scand. 1953;32:399–402. [PubMed: 13138066]
- 22.
Mangesi L, Zakarija-Grkovic I. Treatments for breast engorgement during lactation. Cochrane Database Syst Rev. 2016;6:CD006946. [PMC free article: PMC7388926] [PubMed: 27351423]
- 23.
Luhman LA. The effect of intranasal oxytocin on lactation. Obstet Gynecol. 1963;21:713–7. [PubMed: 13931578]
- 24.
Ruis H, Rolland R, Doesburg W, et al. Oxytocin enhances onset of lactation among mothers delivering prematurely. Br Med J (Clin Res Ed).
 1981;283:340–2. [PMC free article: PMC1506140] [PubMed: 6788318]
1981;283:340–2. [PMC free article: PMC1506140] [PubMed: 6788318]- 25.
Fewtrell MS, Loh K, Blake A, et al. Randomised, double-blind trial of oxytocin nasal spray in mothers expressing breast milk for preterm infants. Arch Dis Child Fetal Neonatal Ed. 2006;91:F169–74. [PMC free article: PMC2672698] [PubMed: 16223754]
- 26.
Cowley KC. Psychogenic and pharmacologic induction of the let-down reflex can facilitate breastfeeding by tetraplegic women: A report of 3 cases. Arch Phys Med Rehabil. 2005;86:1261–4. [PubMed: 15954070]
- 27.
Fernández-Cañadas Morillo A, Marin Gabriel MA, Olza Fernández I, et al. The relationship of the administration of intrapartum synthetic oxytocin and breastfeeding initiation and duration rates. Breastfeed Med. 2017;12:98–102. [PubMed: 28165755]
- 28.
Abdoulahi M, Hemati Z, Asl FS, et al. Association of using oxytocin during labor and breastfeeding behaviors of infants within two hours after birth.
 Iran J Neonatol. 2017;8:48–52. [CrossRef]
Iran J Neonatol. 2017;8:48–52. [CrossRef]- 29.
Fernández-Cañadas Morillo A, Duran Duque M, Hernandez López AB, et al. Cessation of breastfeeding in association with oxytocin administration and type of birth. A prospective cohort study. Women Birth. 2019;32:e43–e8. [PubMed: 29754970]
Oxytocin Administration and Breastfeeding - The Institute for Breastfeeding and Lactation Education (IABLE)
You are here: Home / Questions / Oxytocin Administration and Breastfeeding
CQ #62 -
by Anne Eglash MD, IBCLC, FABM
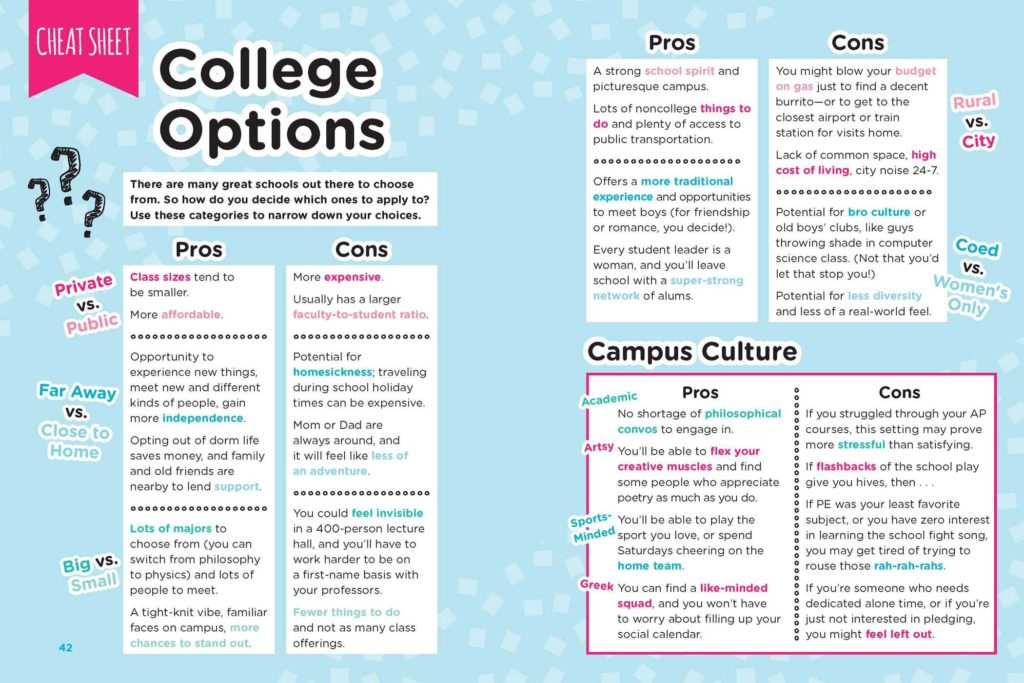
Does administration of oxytocin (Pitocin) effect breastfeeding? Oxytocin plays a central role in the management of labor and delivery in the USA and in many other countries. It is used to induce labor, augment a slow or stalled labor, and given after birth to prevent or control postpartum bleeding.
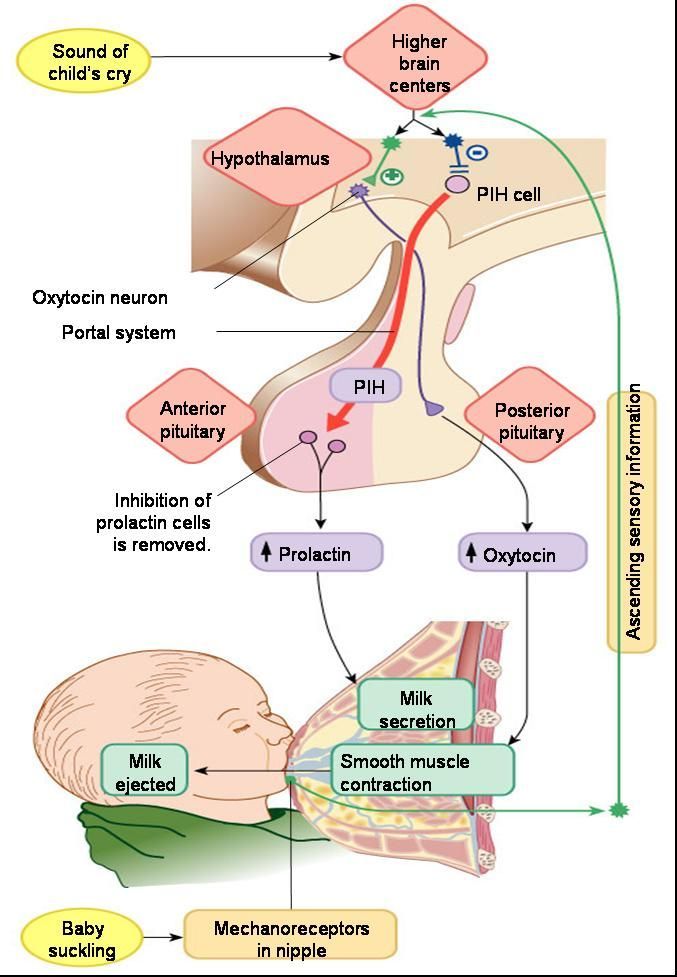
Oxytocin is a crucial hormone secreted from a breastfeeding mother’s pituitary gland, responsible for milk ejection. All sorts of stimuli initiate an oxytocin surge in breastfeeding women, such as hearing, seeing, feeling, smelling, or thinking about the baby. The question is whether the oxytocin given during labor and delivery messes with the mother’s ability to create her own oxytocin surges in the first few days postpartum, and whether this in turn has an overall effect on the success of lactation.
All sorts of stimuli initiate an oxytocin surge in breastfeeding women, such as hearing, seeing, feeling, smelling, or thinking about the baby. The question is whether the oxytocin given during labor and delivery messes with the mother’s ability to create her own oxytocin surges in the first few days postpartum, and whether this in turn has an overall effect on the success of lactation.
The authors of a 2017 study compiled the evidence to date on the effect of administrating oxytocin during labor and after delivery on breastfeeding.
What do you think they found? Choose 1 or more:
- Some studies have found that oxytocin during labor and delivery benefits the breastfeeding outcome.
- Studies consistently show that administrating oxytocin is associated with a delay in lactation (taking longer for the milk to ‘come in’).
- Administrating oxytocin intrapartum is strongly associated with a shorter duration of breastfeeding.
- Giving oxytocin during labor causes infants to not nurse as well during the first week postpartum.

- All of the above are true.
- None of the above are true
See the Answer
The correct answer - F
Read the ABSTRACT
J Midwifery Womens Health. 2017 Jul;62(4):397-417. doi: 10.1111/jmwh.12601.
Breastfeeding Outcomes After Oxytocin Use During Childbirth: An Integrative Review.
Erickson EN, Emeis CL.
INTRODUCTION:
Despite widespread use of exogenous synthetic oxytocin during the birth process, few studies have examined the effect of this drug on breastfeeding. Based on neuroscience research, endogenous oxytocin may be altered or manipulated by exogenous administration or by blocking normal function of the hormone or receptor. Women commonly cite insufficient milk production as their reason for early supplementation, jeopardizing breastfeeding goals. Researchers need to consider the role of birth-related medications and interventions on the production of milk. This article examines the literature on the role of exogenous oxytocin on breastfeeding in humans.
This article examines the literature on the role of exogenous oxytocin on breastfeeding in humans.
METHODS:
Using the method described by Whittemore and Knafl, this integrative review of literature included broad search criteria within the PubMed, Cumulative Index to Nursing and Allied Health Literature (CINAHL), Cochrane, and Scopus databases. Studies published in English associating a breastfeeding outcome in relation to oxytocin use during the birth process were included. Twenty-six studies from 1978 to 2015 met the criteria.
RESULTS:
Studies were analyzed according to the purpose of the research, measures and methods used, results, and confounding variables. The 26 studies reported 34 measures of breastfeeding. Outcomes included initiation and duration of breastfeeding, infant behavior, and physiologic markers of lactation. Timing of administration of oxytocin varied. Some studies reported on low-risk birth, while others included higher-risk experiences. Fifty percent of the results (17 of 34 measures) demonstrated an association between exogenous oxytocin and less optimal breastfeeding outcomes, while 8 of 34 measures (23%) reported no association. The remaining 9 measures (26%) had mixed findings. Breastfeeding intentions, parity, birth setting, obstetric risk, and indications for oxytocin use were inconsistently controlled among the studies.
Fifty percent of the results (17 of 34 measures) demonstrated an association between exogenous oxytocin and less optimal breastfeeding outcomes, while 8 of 34 measures (23%) reported no association. The remaining 9 measures (26%) had mixed findings. Breastfeeding intentions, parity, birth setting, obstetric risk, and indications for oxytocin use were inconsistently controlled among the studies.
DISCUSSION:
Research on breastfeeding and lactation following exogenous oxytocin exposure is limited by few studies and heterogeneous methods. Despite the limitations, researchers and clinicians may benefit from awareness of this body of literature. Continued investigation is recommended given the prevalence of oxytocin use in clinical practice.
Milk Mob Comment by Anne Eglash MD, IBCLC, FABM
The research on the effect of oxytocin during labor and delivery is not strong enough to make any of the above statements above. Overall, the studies on this topic are each designed so differently, that they are hard to compare in order to determine any real conclusions. For example, some studies separate out primiparous women from multiparous women, and others don’t. Some studies made sure to report the mothers’ intent to breastfeeding, while others did not. Even the definition of breastfeeding varied between the studies. Nearly all of the studies were done in high income countries, making any conclusions not valid for lower income countries.
For example, some studies separate out primiparous women from multiparous women, and others don’t. Some studies made sure to report the mothers’ intent to breastfeeding, while others did not. Even the definition of breastfeeding varied between the studies. Nearly all of the studies were done in high income countries, making any conclusions not valid for lower income countries.
The bottom line is that there are many studies that hint at the possibility that administering oxytocin during labor and delivery may have an impact on breastfeeding outcome. It is important that we not ‘hang our hat’ on one particular study until we have larger, better designed and replicated outcomes on this topic. For now, we can simply shrug our shoulders.
Oxytocin - what it is, functions and production of the hormone
Oxytocin is both a hormone that acts on various organs (including the breast and uterus) and a neurotransmitter (chemical messenger in the brain). It controls key aspects of the reproductive system, including childbirth and lactation, as well as human behavior.
English name:
Oxytocin
Synonyms:
synthocinone and pitocin (synthetic variants of oxytocin), carbetocin (an analogue of oxytocin with a similar structure), “love hormone”
See also:
What is oxytocin: main functions
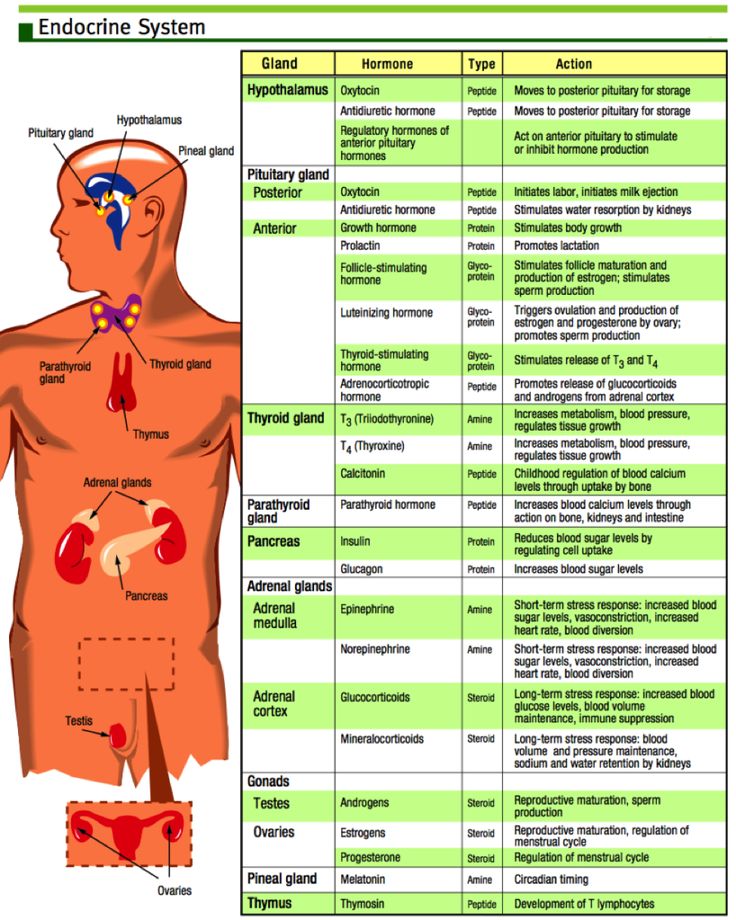
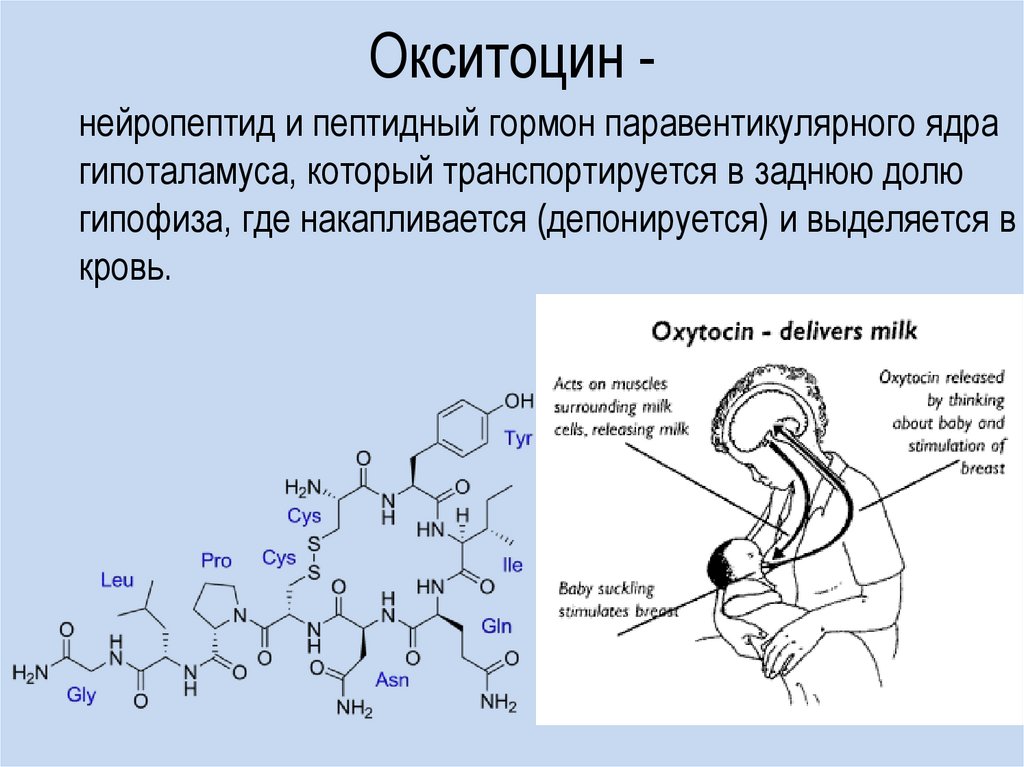
Oxytocin is produced in the hypothalamus and secreted into the bloodstream by the posterior pituitary gland. For example, the ability of the uterus to contract during childbirth and breastfeeding depends on it.
Artificial oxytocin is sometimes prescribed to induce labor if it hasn't started naturally. It is also used to increase contractions during weak labor and to reduce the risk of severe bleeding after the birth of a child. During breastfeeding, oxytocin promotes the movement of milk through the ducts in the breast, allowing it to exit through the nipples.
In the male body, oxytocin is responsible for the movement of spermatozoa and the production of testosterone by the testicles.
In the brain, oxytocin acts as a chemical messenger and influences the behavior and emotions of people, namely:
-
For sexual arousal;
-
Confession;
-
Confidence;
-
romantic affection;
-
The bond between mother and baby.
Therefore, oxytocin is often referred to as the “love hormone” or “cuddle hormone.”
How is oxytocin controlled?
The production and secretion of oxytocin is controlled by a positive feedback mechanism, where the release of the hormone triggers an action that stimulates its own production. For example, when uterine contractions begin during childbirth, oxytocin is released. This stimulates contraction activity and the release of more oxytocin. Thus, contractions increase in intensity and frequency.
Another example of positive feedback: nipple stimulation during breastfeeding leads to increased production of oxytocin and its secretion into the bloodstream, resulting in milk being delivered to the breast.
What happens with an excess of oxytocin?
To date, there is no clear answer to this question. However, it is known that high levels of oxytocin are associated with benign prostatic hyperplasia, a disease that affects more than half of men over 60 years of age. It usually causes difficulty urinating.
This condition can be cured by adjusting the level of oxytocin. However, more research is needed.
What happens if there is a lack of oxytocin?
The consequences of insufficient levels of oxytocin in the body are also under study.
So far, it is known that a deficiency of the “love hormone” in a nursing mother can interfere with breastfeeding.
In addition, low levels of oxytocin have been linked to autism and autism spectrum disorders (such as Asperger's syndrome). The main symptom of these disorders is difficulties with interaction in society. Some scientists believe that oxytocin can be used to treat these diseases.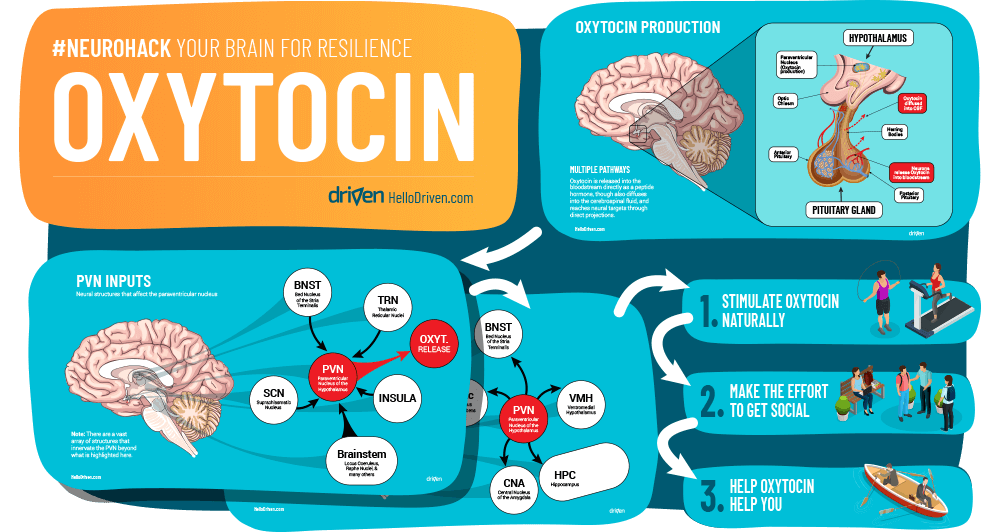
In addition, a low level of oxytocin is detected in depressive states. And, probably, it can be used to correct them.
Interested in anti-aging
and preventive medicine?
Learn more at
Anti-Age Expert Tutorials
To be the best - learn
at the best!
Experts from all over the world will be your mentors
on the way learning Anti-Age Expert. More
How to Succeed in Milk Production
Dairy owners understand that this task involves constant struggle. The growth of the global dairy market and the concerns of buyers around the world about food quality and safety issues will continue to put increasing pressure on farmers in the future, forcing them to produce healthy, high quality and safe dairy products. These processes take place against the backdrop of significant economic pressure on dairy producers. In this regard, today's dairy farmers are looking for production management strategies that would allow them to use materials and labor more efficiently to remain competitive and profitable.
More than 50 percent of the labor force and an equally high proportion of the dairy farm's fixed costs are used to milk cows. It is easy to see why lean dairy farmers seek to achieve greater profitability in the use of labour, equipment and milking materials while also trying to meet the unwavering need of customers for quality. The “good news” is that the farming practices that produce high quality milk also lead to good livestock health and efficient dairy production.
Herd management technology has been greatly improved. Achievements in the field of genetics, nutrition and 3-time milking of cows have made it possible to increase the pace of dairy production. At the same time, there are improvements related to the power, performance and automation of milking equipment. These are examples of technical improvements that have influenced how cows are milked.
Today's dairy farms are more dependent on the skills to use high performance technologies and products. However, it is also a good idea to keep in mind that new farm management approaches should take into account the basic biological needs of cows.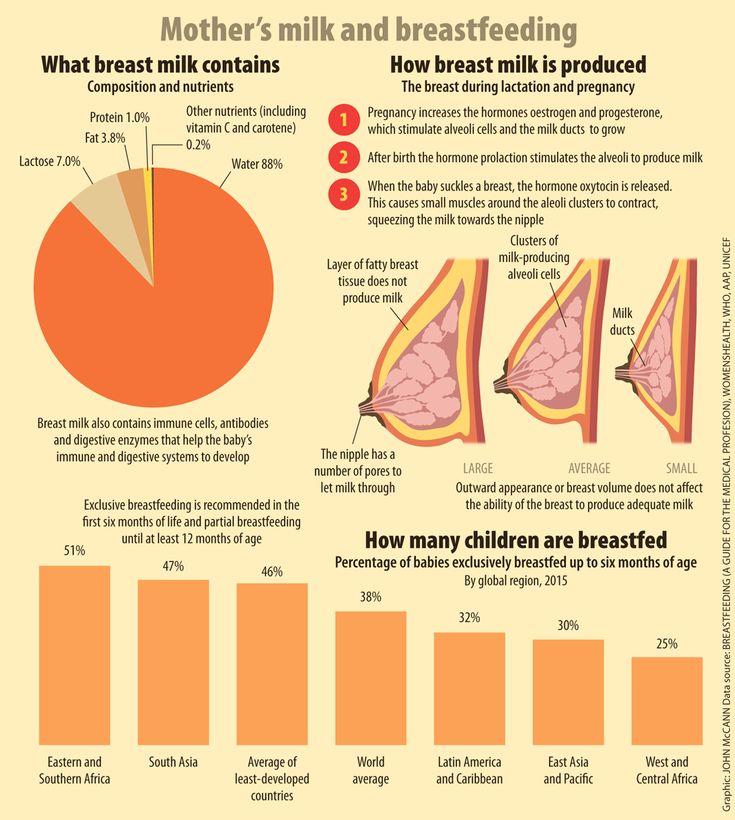 The milking procedure should be designed taking into account the physiology of cows in order to optimize cow health, milk quality, human health, and the process of practical and efficient use of labor and materials. The purpose of this [article] is to describe the facts known to date about the procedure for preparing cows, as well as the most effective principles for carrying out this procedure, taking into account the need to optimize cow health, milk quality, health of the milker and maintain the profitability of the farm.
The milking procedure should be designed taking into account the physiology of cows in order to optimize cow health, milk quality, human health, and the process of practical and efficient use of labor and materials. The purpose of this [article] is to describe the facts known to date about the procedure for preparing cows, as well as the most effective principles for carrying out this procedure, taking into account the need to optimize cow health, milk quality, health of the milker and maintain the profitability of the farm.
Despite the existence of basic scientific principles that govern the procedure for preparing cows, the operation of each farm is unique. Thus, there is no single procedure for preparing cows that would meet the needs of any dairy farm. We hope that an overview of these principles will help you find the best solution for your farm.
Cow physiology
Milk production is mandatory. Lactation in dairy cows depends on the process of milk transfer (milk secretion).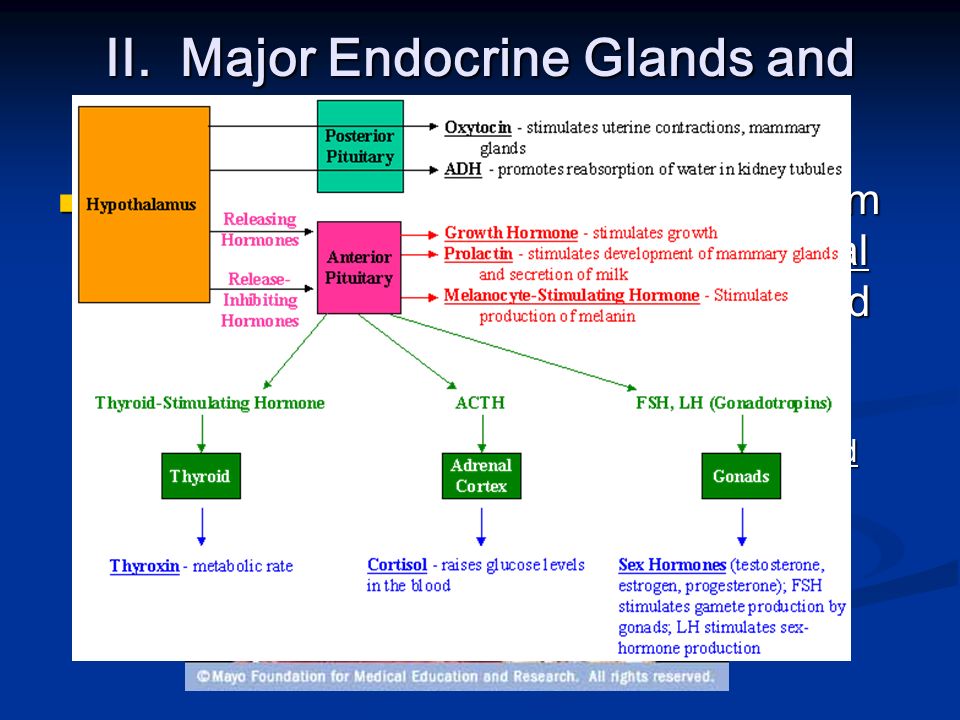 While this statement is not true for goats, it does apply to dairy cows. The requirements for the process of milk secretion depend on the ratio of the volume of the alveolar tissue (they secrete milk) and the capacity of the cistern (the ducts of the mammary gland and the cistern). The udder tank capacity is 80 percent for goats and 30 percent for cows.
While this statement is not true for goats, it does apply to dairy cows. The requirements for the process of milk secretion depend on the ratio of the volume of the alveolar tissue (they secrete milk) and the capacity of the cistern (the ducts of the mammary gland and the cistern). The udder tank capacity is 80 percent for goats and 30 percent for cows.
In general, the higher the percentage of alveoli compared to the capacity of the tank, the more significant the process of milk transfer will be. First lactating cows have lower cistern capacity than older cows. This fact explains the greater need for the development of a qualitative reaction of lactation in these cows for efficient milking, as well as a proportionally higher level of milk production in response to more frequent milking.
- The role of oxytocin
The role of oxytocin in milk production has been well studied. However, the process of milk release is more complex than a simple reaction to the action of oxytocin.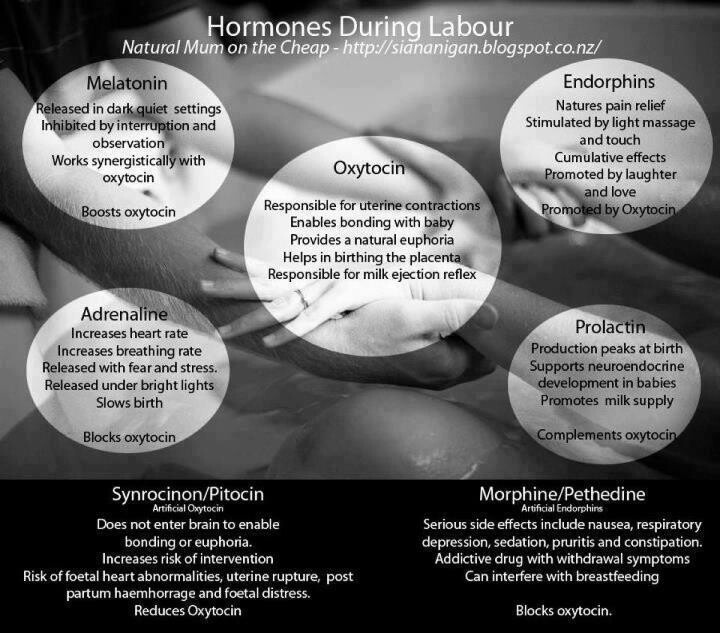 The results of studies have shown that the process of secretion of milk in the alveolar tissue is not fully dependent on the action of oxytocin, while there are many other factors that affect the effectiveness of the response to oxytocin.
The results of studies have shown that the process of secretion of milk in the alveolar tissue is not fully dependent on the action of oxytocin, while there are many other factors that affect the effectiveness of the response to oxytocin.
- Local nervous system reaction
The effect of nipple stimulation on the tone of the sympathetic part of the nervous system, which is part of the mammary gland, is to form a secondary mechanism of milk secretion. The process of stimulation of the nipples triggers a local automatic reflex, which leads to a decrease in the tone of the smooth muscles around the milk ducts and nipple sphincters. There is also an increase in blood flow to the mammary gland and a decrease in the sensitivity threshold of myoepithelial cells to the action of oxytocin. Despite the fact that the mechanism of milk ejection caused by the local autonomic reflex does not depend on the action of oxytocin, this mechanism stimulates the development of a response to oxytocin.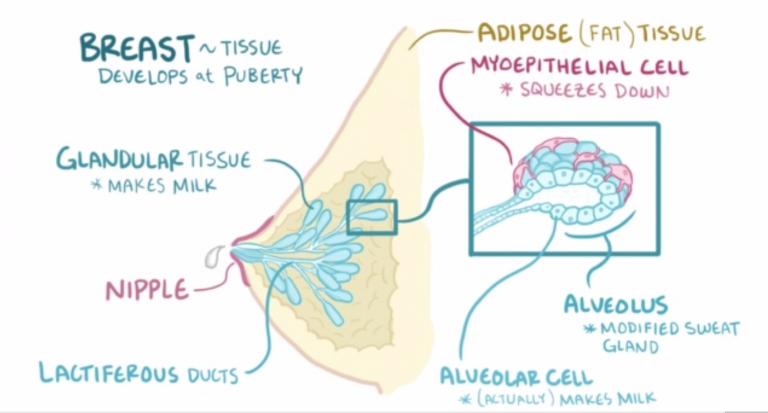 These two mechanisms contribute to the efficient secretion of milk.
These two mechanisms contribute to the efficient secretion of milk.
- Other factors
The effect of oxytocin on breast myoepithelial cells and uterine smooth muscle cells is similar and depends on the action of oxytocin receptors. Progesterone and estrogen levels affect the activity of oxytocin receptors in uterine smooth muscle cells and are thought to have a similar effect on breast myoepithelial cells. Sufficient calcium content in the composition of the diet is necessary to ensure normal contraction of smooth muscle cells, including myoepithelial cells of the mammary gland.
Magnesium is involved in the activation of oxytocin receptors and smooth muscle contraction. This means that magnesium supplementation has a direct effect on the milk fat content of milk. Cobalt and manganese also affect the efficiency of the oxytocin response. It is obvious that the process of milk secretion is a complex mechanism.
- Possible effects on the reproductive cycle
In general, it is noted that the reaction of milk flow depends on the stage of lactation and the level of milk production.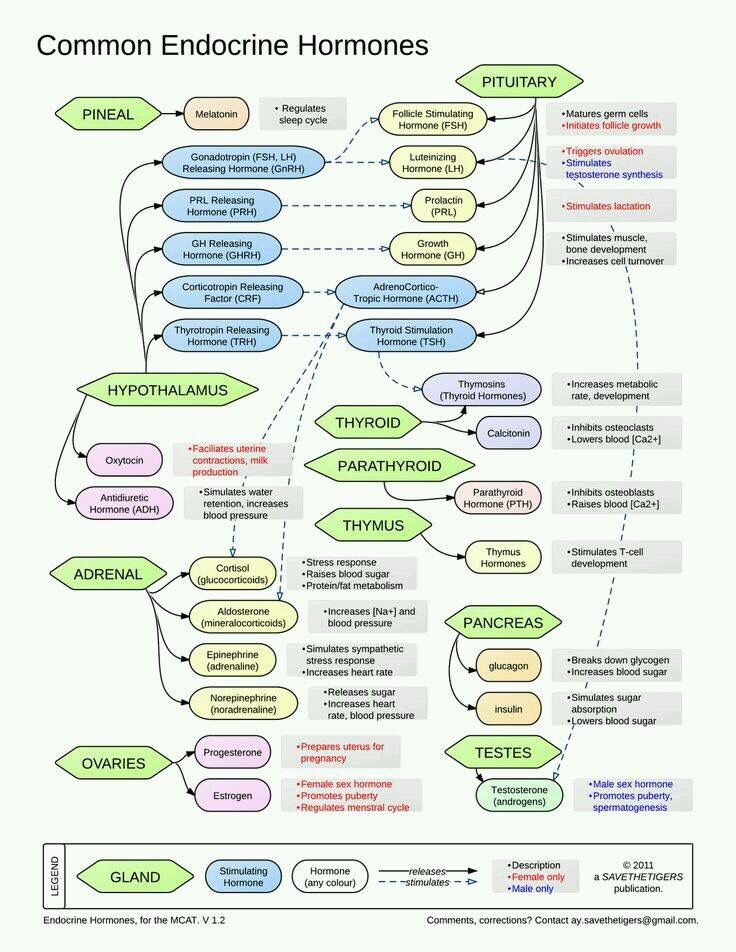 Late lactating cows generally need more stimulation to achieve efficient milk release than early lactating cows. It may be reasonable to conclude that at the stage of early lactation, especially in highly productive cows, the process of milk secretion is more pronounced, since the more myoepithelial cells are loosened, the more forcefully they will contract, while the cyclic effect of estrogen at the stage of early lactation maintains the sensitivity of oxytocin receptor sites to oxytocin, which allows for a more pronounced response to oxytocin.
Late lactating cows generally need more stimulation to achieve efficient milk release than early lactating cows. It may be reasonable to conclude that at the stage of early lactation, especially in highly productive cows, the process of milk secretion is more pronounced, since the more myoepithelial cells are loosened, the more forcefully they will contract, while the cyclic effect of estrogen at the stage of early lactation maintains the sensitivity of oxytocin receptor sites to oxytocin, which allows for a more pronounced response to oxytocin.
During pregnancy, the body of the cow is under the influence of the hormone progesterone, while the affinity of oxytocin receptor sites for oxytocin decreases, and smooth muscle cells become less sensitive. It can be assumed that the hormonal changes accompanying pregnancy shift the dependence of the milk secretion process on the mechanism of action of oxytocin towards the mechanism caused by the local automatic reflex. It is assumed (but this fact has not yet been proven) that nipple stimulation plays a more important role in the development of the local autonomous milk flow reflex than the mechanism mediated by the action of oxytocin.
- Incentive before milking
The preparation period is defined as the time spent manually cleaning and drying the surface of the nipples. The operator must be sure that the surface of the teats is perfectly clean and dry before attaching the milking cluster to them and that a proper teat massage has been performed to stimulate milk flow. Regarding the preparation of the cow for milking, the Mein source states the following: “Modern high-yielding Holstein cows require little stimulation for normal milk production. In this regard, the basis of high-quality preparation of a cow before milking is to fix the teat cups:
- On visually clean and dry teat surfaces, with special attention to detail to reduce the risk of mastitis and maintain high milk quality
- During milk ejection or immediately afterwards when the udder is full of milk
- With minimal time and effort for stimulation.
Some interpret the phrase "with a minimum investment of time and effort" to mean no preparation required. However, a careful analysis of Main's statement (see above) and published data on the subject does not support this conclusion.
However, a careful analysis of Main's statement (see above) and published data on the subject does not support this conclusion.
Recent studies have shown that pacing of less than 10 seconds is not sufficient to achieve a sustained milk ejection response in different types of cows. Despite the fact that manual stimulation of 10 seconds ensures the development of a qualitative reaction of milk flow in American Holsteins at an early stage of lactation, this measure is insufficient for cows of the American Holstein breed at a later stage of lactation, European Friesian and Jersey breeds. Manual stimulation (washing, drying, pre-milking) of 10 to 20 seconds is sufficient for most types of cows, regardless of the stage of lactation or lactation.
It is often difficult to convince some milkers that the time spent preparing a cow's udder before milking to ensure sufficient teat cleaning and a good milk flow response does not significantly increase the overall duration of the milking process.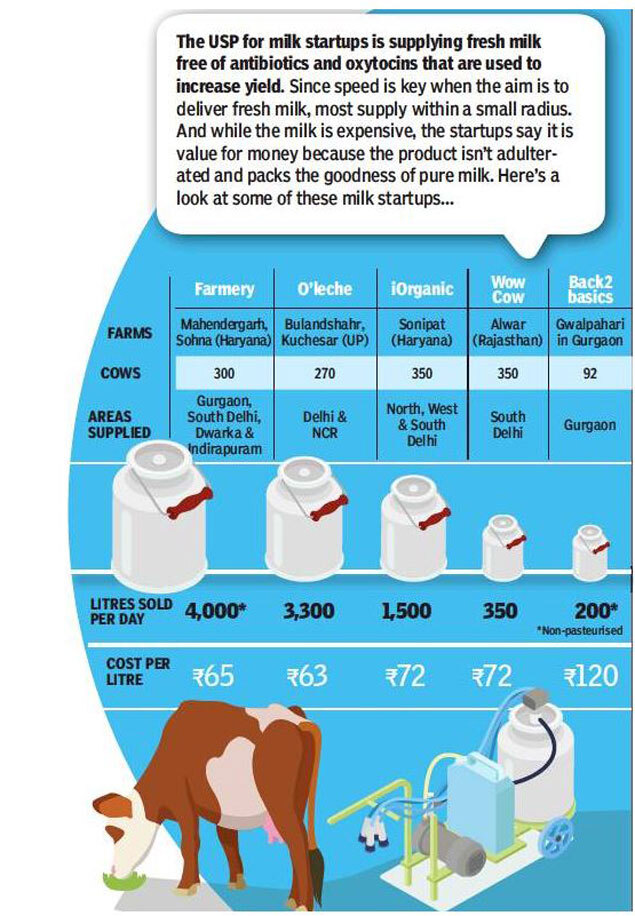 Data from a number of studies indicate that the optimization of the udder process can reduce milking time and increase the productivity of a cow, however, in accordance with other data, the absence of a preparatory stage allows an increase in productivity in a two-row milking parlor for 8 machines from 75 cows per hour to 90.
Data from a number of studies indicate that the optimization of the udder process can reduce milking time and increase the productivity of a cow, however, in accordance with other data, the absence of a preparatory stage allows an increase in productivity in a two-row milking parlor for 8 machines from 75 cows per hour to 90.
Difference in labor costs for milking 300 cows three times with optimal preparation (75 cows per person per day) and without this preparation (90 cows per person per day) is 200 pounds of milk per cow per year . Thus, if spending extra time on properly preparing cows results in more than 200 pounds of milk, or higher quality milk, it makes economic sense to prepare cows well for milking.
- Pre-flaking
Pre-milking to check for clinical signs of mastitis is the recommended procedure for preparing a cow for milking. Currently, many milkers refuse to perform pre-milking due to the fact that this procedure is physically difficult and laborious. However, the pre-milking procedure is a powerful stimulation of the lactation response, and therefore it is best done at the initial stage, during the preparation of the cow. However, if it takes more than 20 seconds to prepare a cow for milking, the use of a pre-milking technique can slightly improve milking efficiency. Thus, in a situation where a procedure for preparing cows with a minimum duration (10 seconds) is used, the inclusion of a preliminary milking process in the framework of this procedure allows achieving a high-quality reaction of milk ejection.
However, the pre-milking procedure is a powerful stimulation of the lactation response, and therefore it is best done at the initial stage, during the preparation of the cow. However, if it takes more than 20 seconds to prepare a cow for milking, the use of a pre-milking technique can slightly improve milking efficiency. Thus, in a situation where a procedure for preparing cows with a minimum duration (10 seconds) is used, the inclusion of a preliminary milking process in the framework of this procedure allows achieving a high-quality reaction of milk ejection.
- Effect of more frequent milking
More frequent milking means better udder handling before milking. Cows that are milked more than 2 times a day do not have the same effective milk supply. It is hypothesized that pressure on the udder may be a factor in stimulating the release of oxytocin, or, as previously mentioned, pressure on the udder may alter the sensitivity of myoepithelial cells to oxytocin.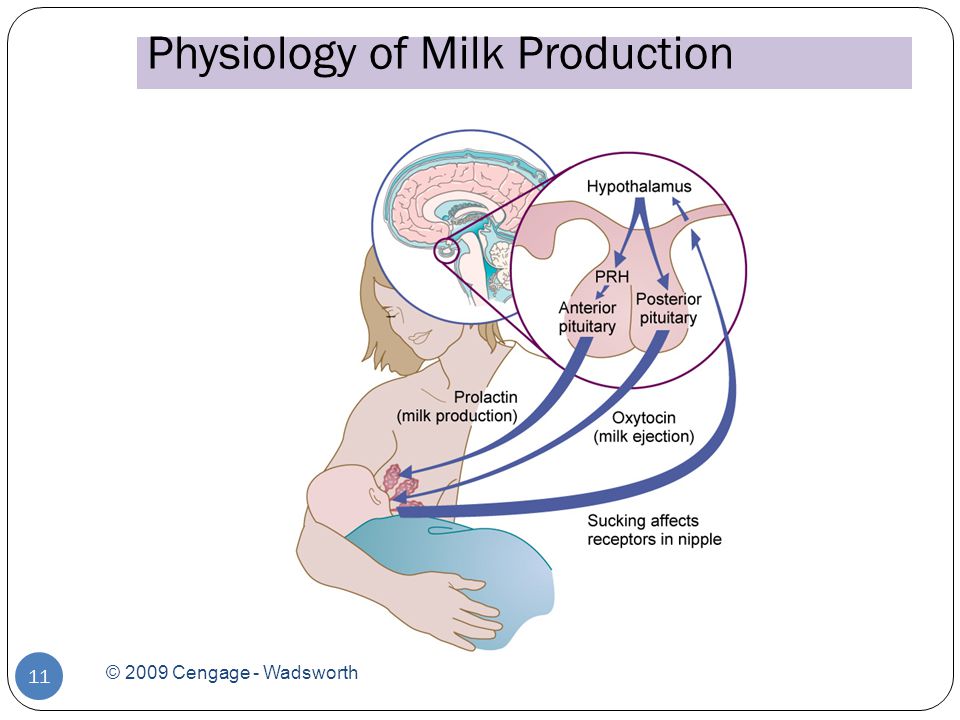
Thus, a high quality cow preparation procedure may be relatively more important in a herd that uses three milkings instead of two milkings.
- Fixing time
The preparation downtime is the period of time between the start of teat treatment and the attachment of the milking cluster. In the Rasmussen spring, optimal milk production is defined as the maximum milk yield obtained without the need to milk non-milk teats. Recent studies in the US and Denmark have shown that downtime spent on preparation is the most important factor in optimizing milk production. Based on these studies, the ideal prep downtime is 1.3 minutes (1 minute and 18 seconds).
A range of one to two minutes is considered optimal downtime for preparation at all stages of lactation. If the downtime during preparation exceeds three minutes, this leads to an increase in the proportion of residual milk and a decrease in milk yield, regardless of the stage of lactation. Excessive downtime during preparation is more common in stall barns and can limit herd productivity.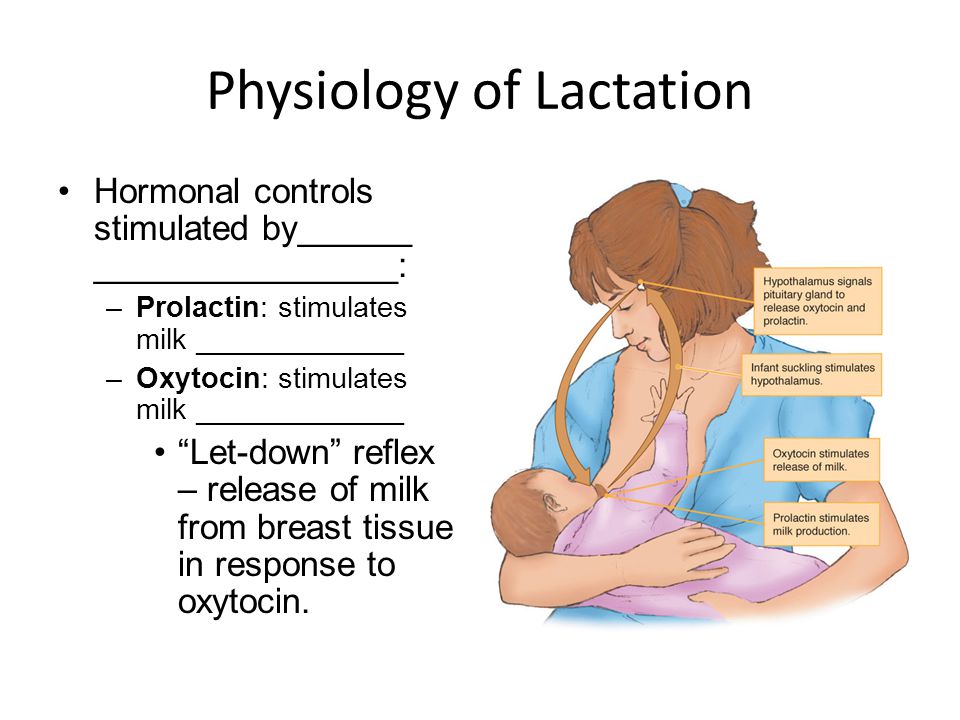 It seems clear that more effort needs to be put into developing those procedures that will optimize the downtime in preparation.
It seems clear that more effort needs to be put into developing those procedures that will optimize the downtime in preparation.
- Condition of nipples
Although the use of a milking cluster can stimulate a prolonged milk ejection response, it is not recommended to attach the milking cluster before milk has begun to flow. Attaching the milking cluster before the milk is released results in milking of non-milk teats, longer machine life and increased risk of backflow due to air leakage. It also causes excessive wear on the nipples. The use of a milking machine is the main cause of the development of hyperkeratosis at the top of the nipples. Thus, it is advisable, as far as possible, to minimize the duration of contact of the device with the udder.
Given that the milking process of today's high yielding cows takes longer due to the increased milk production (10 pounds per minute), and the fact that cows are often milked 3 times a day, it is reasonable to calculate the time spent on the attachment of the equipment, in order to maximize the milk flow rate and minimize the contact time of this equipment with the cow's body.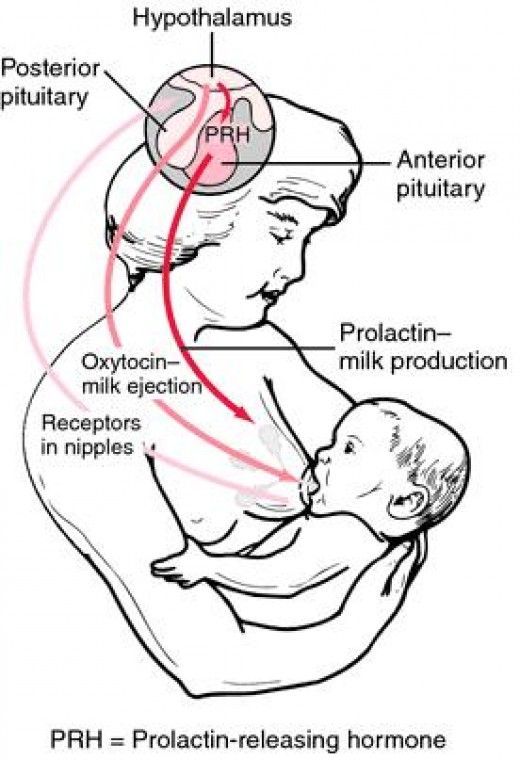 This measure reduces the risk of new infections and excessive wear on the nipples.
This measure reduces the risk of new infections and excessive wear on the nipples.
Rasmussen's source suggested the need to use automatic detachment devices for faster removal of the device when cows are milked 3 times a day. By increasing the thresholds in the automatic disconnect settings from 0.44 to 0.9 pounds per minute, the average duration of contact between the milking cluster and the cow's udder is reduced by 0.5 minutes, and the condition of the teats is improved. At the same time, there is no change in the level of milk yield or quality of milk. Adjusting idle time from 20-30 seconds to 10 seconds after the threshold has been reached also reduces the total cluster-to-udder contact time and improves parlor productivity.
It is recommended to be careful with insufficient milking for several days, as this can reduce milk production. However, under conditions of full milk supply, it is acceptable to leave a small amount of milk (1-2 pounds) in the mammary gland and tank, as this will not reduce milk production or increase the risk of mastitis in any areas, except for those quarters of the udder that are infected with the most dangerous pathogens.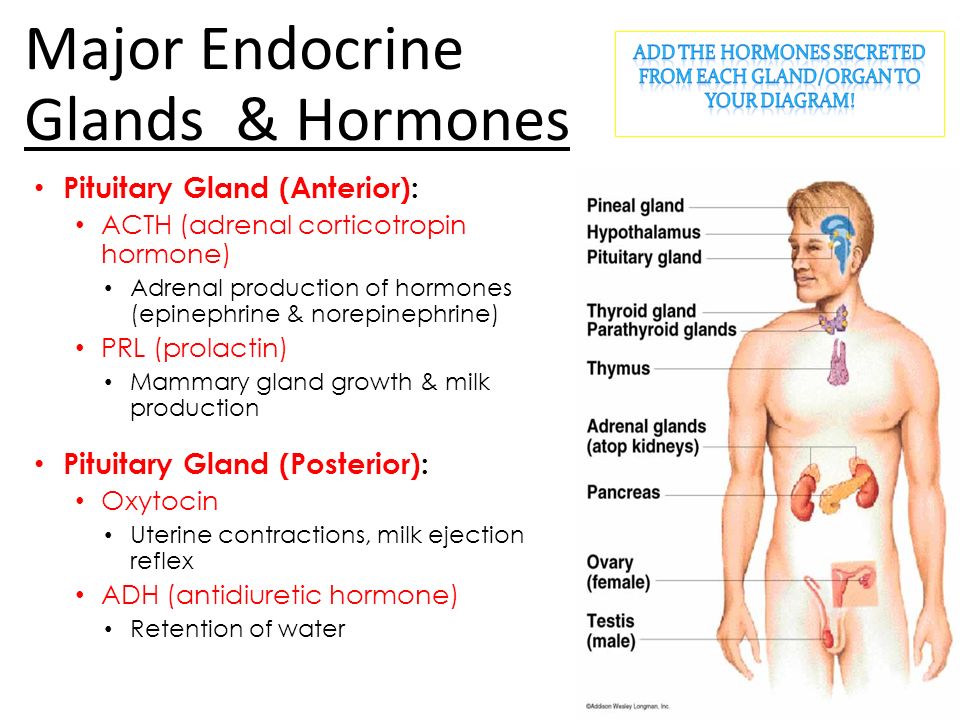
Standardization
Cows love a strict daily routine. They are at their most productive when they are fed, milked, or otherwise treated at fixed times every day. Full cycle lactation studies have shown that standardized milking yields 5.5 percent more milk production than irregular milking. This fact confirms the opinion about the need to develop a regime that provides milking of cows strictly at a certain time, regardless of the stage of lactation or the personality of the milker.
Teat cleanliness, milk quality and udder health
Studies have shown that good cleaning and drying with separate towels can reduce the bacterial population on teat surfaces by 75 percent. Data on nipple pretreatment indicate that increased nipple cleanliness reduces the incidence of breast infections. The level of cleanliness of the cow has a significant impact on the efficiency of preparing the cow for milking. It is estimated that when working with uncleaned udders, the duration of the cow preparation period is doubled, which leads to an unnecessary decrease in the productivity of the milking parlour.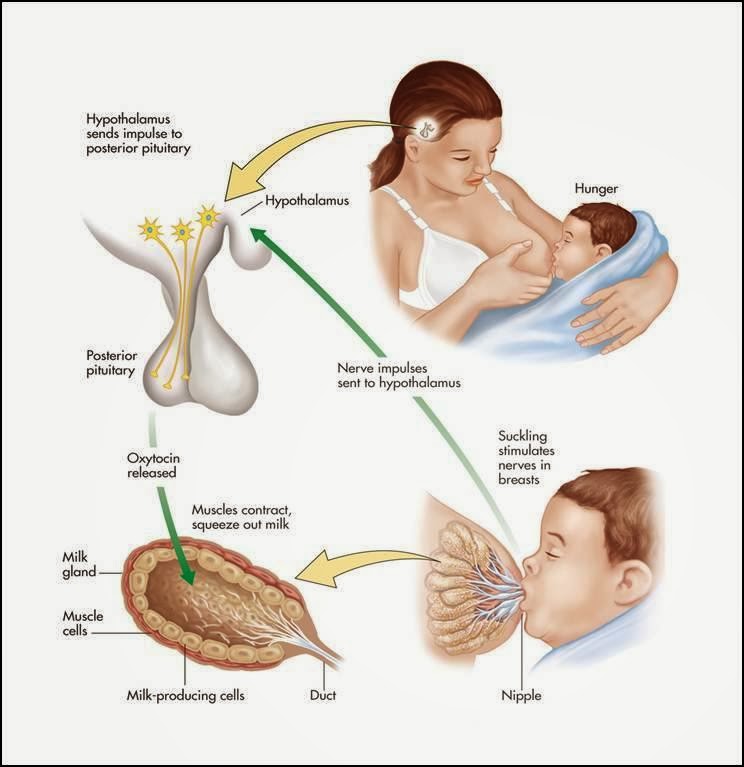 Processing methods such as trimming or “scorching” udder hairs, docking tails, as well as lining the stall with fresh hay, organizing clean, dry and comfortable stall areas, can achieve efficiency in preparing a cow for milking and at the same time improve milk quality and reduce risk development of mastitis.
Processing methods such as trimming or “scorching” udder hairs, docking tails, as well as lining the stall with fresh hay, organizing clean, dry and comfortable stall areas, can achieve efficiency in preparing a cow for milking and at the same time improve milk quality and reduce risk development of mastitis.
Any bacteria not removed from the teat surface before attaching the milking cluster will pass into the milk. In the past, we were more concerned about the pathogens that cause mastitis and the risk of developing mastitis, but now there is a growing concern about bacteria that affect milk quality and food safety. Some time ago, psychrophilic bacteria and milk quality were a concern. Psychrophilic bacteria are usually present in the body of a cow. The surface of the nipples is usually colonized by these bacteria. The presence of these bacteria in milk is undesirable, as they continue to thrive at sub-zero temperatures and can survive pasteurization. Research conducted in Wisconsin has shown that these bacteria are a source of proteolytic enzymes or plasminogen activators that shorten the shelf life of dairy products and milk yield.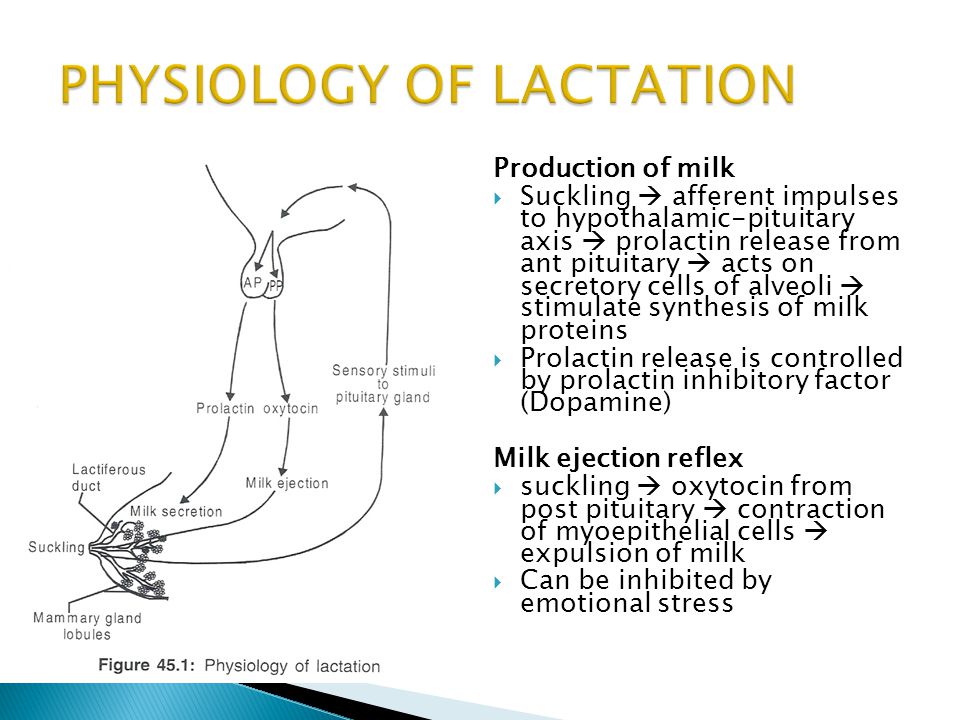
Plasminogen is usually present in milk. In the presence of plasminogen activators, it is converted into an active enzyme necessary for the formation of plasmin. Plasmin breaks down the casein found in milk. Plasmin remains active at low temperatures and withstands high temperatures during milk processing. This fact is of high concern among dairy producers.
Bacteria of the genus Salmonella and Listeria pose a threat to human health. They may also be present in the body of the cow and easily colonize the surface of the teats. In light of the growing concern, it is doubtful that the current PMO (Milk Pasteurization Rules) requirements for cleaning teat surfaces before milking will be reduced. Dairy owners should develop practical methods for incorporating pre-milking teat cleaning into their daily milking schedule to ensure milk quality and safety.
Ergonomics and milking routine
What about the milker's health? It is not difficult to determine the most beneficial milking rules in terms of human health and safety.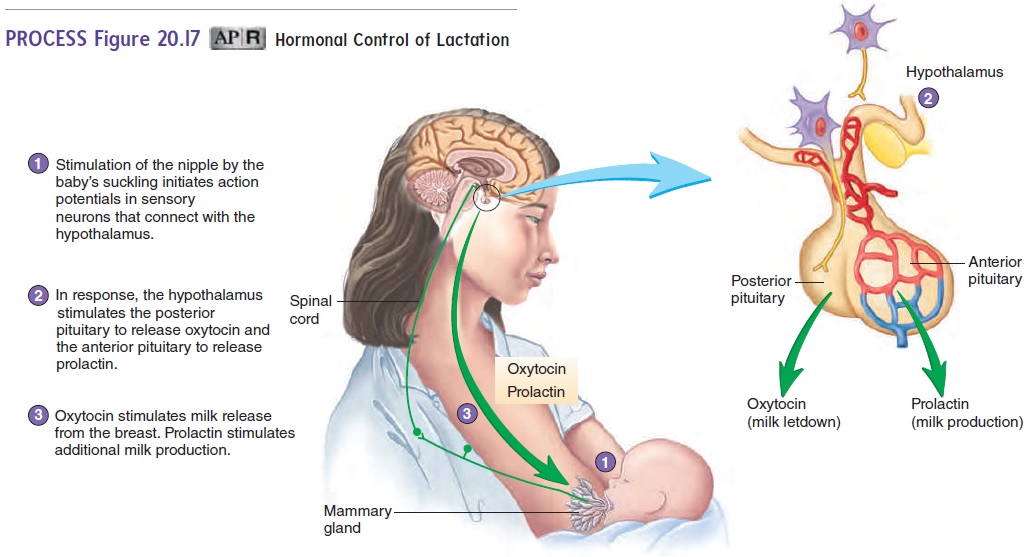 It seems clear that when cows are milked in a stall barn, farm workers are at risk of chronic knee and back injuries. However, we do not know much about the ergonomic requirements for long shifts in milking parlors. Studies in other industries have shown that workers who perform high-intensity, repetitive, manual tasks (such as pre-flaking) have a higher prevalence of carpal tunnel syndrome over a long period of time. However, there are many factors that need to be taken into account before drawing conclusions about the prevalence of chronic musculoskeletal diseases in relation to the milking regimen. It is undeniable that as the average herd size and duration of milking shifts increases, the need for research in this area increases.
It seems clear that when cows are milked in a stall barn, farm workers are at risk of chronic knee and back injuries. However, we do not know much about the ergonomic requirements for long shifts in milking parlors. Studies in other industries have shown that workers who perform high-intensity, repetitive, manual tasks (such as pre-flaking) have a higher prevalence of carpal tunnel syndrome over a long period of time. However, there are many factors that need to be taken into account before drawing conclusions about the prevalence of chronic musculoskeletal diseases in relation to the milking regimen. It is undeniable that as the average herd size and duration of milking shifts increases, the need for research in this area increases.
Conclusions
Given what we know about milk quality, udder condition and physiology of cows, it seems clear that there is a need to incorporate minimal udder handling before milking into the daily routine. This pre-milking udder treatment procedure should effectively remove bacterial contamination from the teat surface as well as effectively stimulate milk flow in 20 seconds or less.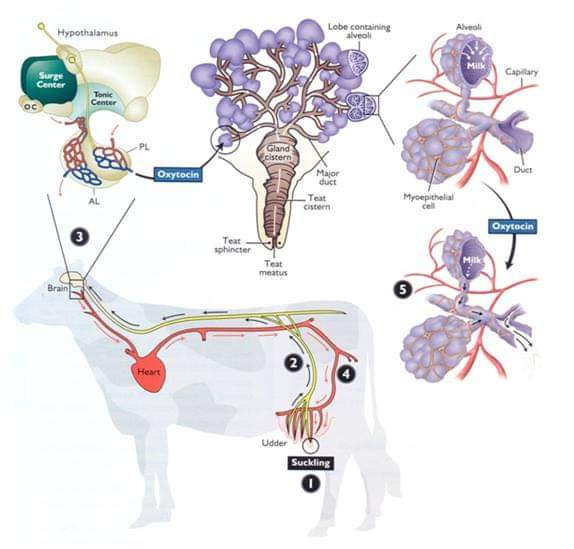 The duration of attachment of machinery is the most decisive factor in efficient milking. The milking cluster is attached one or two minutes after the start of udder preparation. The milking schedule should be standardized to ensure that cows are milked at the same time throughout the lactation period, regardless of the stage of lactation or the identity of the milker.
The duration of attachment of machinery is the most decisive factor in efficient milking. The milking cluster is attached one or two minutes after the start of udder preparation. The milking schedule should be standardized to ensure that cows are milked at the same time throughout the lactation period, regardless of the stage of lactation or the identity of the milker.
What do you need to do on your farm?
- Conduct a full analysis of the milking regimen you use on the farm, taking into account the above principles.
- Design a practical milking plan that takes into account the characteristics of the premises, milking equipment and staff. Develop a written milking protocol that can be used as a job description and when training new employees.
- Organize standard dairy farm meetings to educate employees, raise morale and solve problems. Use the available training videos on how to manage your milking routine as a learning tool.
- Establish specific performance standards (e.