Cerebral palsy tests
Screening and Diagnosis of Cerebral Palsy
Diagnosing cerebral palsy (CP) at an early age is important to the well-being of children and their families. Diagnosing CP can take several steps:
- Developmental Monitoring
- Developmental Screening
- Developmental and Medical Evaluations
Developmental Monitoring
Developmental monitoring (also called surveillance) means tracking a child’s growth and development over time. At each well-child office visit, the doctor monitors the child’s development. The doctor does this by asking parents if they have any concerns about their child’s development, taking or updating the child’s developmental history, and watching the child during the exam to see how he or she moves.
It is important for doctors to monitor the development of all children, but especially those who are at a higher risk for developmental problems due to preterm birth or low birthweight.
If any concerns about the child’s development are raised during monitoring, then a developmental screening test should be given as soon as possible.
Developmental Screening
During developmental screening a short test is given to see if the child has specific developmental delays, such as motor or movement delays. Some developmental screening tests are in the form of interviews or questionnaires completed by parents, others are tests that the doctor gives to the child. The American Academy of Pediatrics recommends that all children be screened for developmental delays during regular well-child office visits at:
- 9 months
- 18 months
- 24 or 30 months
When a child is 9 months of age, many issues involving movement can be seen easily. However, mild movement delays that were not found at the 9-month screening might be easier to see when the child is 18 months of age. By the time the child is 30 months of age, most movement delays can be found.
A developmental screening test also can be given whenever the child’s parents or doctor or others involved in the care of the child have concerns about the child’s development. If the results of the screening test are cause for concern, then the doctor will make referrals for:
If the results of the screening test are cause for concern, then the doctor will make referrals for:
- Developmental and medical evaluations
AND
- Early intervention or early childhood services
Developmental and Medical Evaluations
The goal of a developmental evaluation is to diagnose the specific type of disorder that affects a child. To evaluate movement or motor delays, the doctor will look closely at the child’s motor skills, muscle tone, reflexes, and posture, and take a careful medical history from the parents. The doctor will try to rule out other disorders that could cause similar problems.
Because many children with CP also have related developmental conditions such as intellectual disability; seizures; or vision, hearing, or speech problems, it is important to evaluate the child to find these disorders as well.
The developmental evaluation can be performed by the primary care doctor or by a specialist. Specialists who can do this type of developmental evaluation include:
- Developmental pediatricians or neurodevelopment pediatricians (doctors with special training in child development and in evaluating children developmental problems).

- Child neurologists (doctors with special training in childhood diseases of the brain, spine, and nerves).
- Pediatric physiatrists or pediatric rehabilitation doctors (doctors with special training in physical medicine and rehabilitation for children).
In addition to the developmental evaluation, additional tests can be done to look for a cause of CP. Specialists might suggest brain imaging tests, such as x-ray computed tomography (CT scan) or magnetic resonance imaging (MRI). An electroencephalogram (EEG), genetic testing, or metabolic testing, or a combination of these, also might be done.
CP generally is diagnosed during the first or second year after birth. But if a child’s symptoms are mild, it is sometimes difficult to make a diagnosis until the child is a few years older.
Visit the National Institute of Neurological Disorders and Stroke (NINDS) Cerebral Palsy Information Page to learn more about how CP is diagnosed external icon
If You’re Concerned
If you think your child is not meeting movement milestones or might have CP, contact your doctor or nurse and share your concerns.
If you or your doctor is still concerned, ask for a referral to a specialist who can do a more in-depth evaluation of your child and assist in making a diagnosis.
At the same time, call your state’s public early childhood system to request a free evaluation to find out if your child qualifies for intervention services. This is sometimes called a Child Find evaluation. You do not need to wait for a doctor’s referral or a medical diagnosis to make this call.
Where to call for a free evaluation from the state depends on your child’s age:
- If your child is not yet 3 years old, contact your local early intervention system.
You can find the right contact information for your state by calling the Early Childhood Technical Assistance Center (ECTA) at 919-962-2001 or visit the ECTA websiteexternal icon. - If your child is 3 years of age or older, contact your local public school system.
Even if your child is not yet old enough for kindergarten or enrolled in a public school, call your local elementary school or board of education and ask to speak with someone who can help you have your child evaluated.
If you’re not sure who to contact, call the Early Childhood Technical Assistance Center (ECTA) at 919-962-2001 or visit the ECTA websiteexternal icon.
Learn more about early intervention
Cerebral palsy - Diagnosis and treatment
Diagnosis
Signs and symptoms of cerebral palsy can become more apparent over time, so a diagnosis might not be made until a few months to a year after birth. In some cases where the signs and symptoms are mild, diagnosis may be delayed longer.
If your family doctor or pediatrician suspects your child has cerebral palsy, he or she will evaluate your child's signs and symptoms, monitor growth and development, review your child's medical history, and conduct a physical exam. Your doctor might refer you to specialists trained in treating children with brain and nervous system conditions, such as a pediatric neurologist, pediatric physical medicine and rehabilitation specialist, and child developmental specialist.
Your doctor might also order a series of tests to make a diagnosis and rule out other possible causes.
Brain scans
Brain-imaging technologies can reveal areas of damage or abnormal development in the brain. These tests might include the following:
- MRI. An MRI uses radio waves and a magnetic field to produce detailed 3D or cross-sectional images of the brain. An MRI can often identify lesions or abnormalities in your child's brain. This test is painless, but it's noisy and can take up to an hour to complete. Your child will likely receive a sedative or light general anesthesia beforehand.
- Cranial ultrasound. This can be performed during infancy. A cranial ultrasound uses high-frequency sound waves to produce images of the brain. An ultrasound doesn't produce a detailed image, but it may be used because it's quick and it can provide a valuable preliminary assessment of the brain.

Electroencephalogram (EEG)
If your child is suspected of having seizures, an EEG can evaluate the condition further. Seizures can develop in a child with epilepsy. In an EEG test, a series of electrodes are attached to your child's scalp. The EEG records the electrical activity of your child's brain. It's common for there to be changes in normal brain wave patterns in epilepsy.
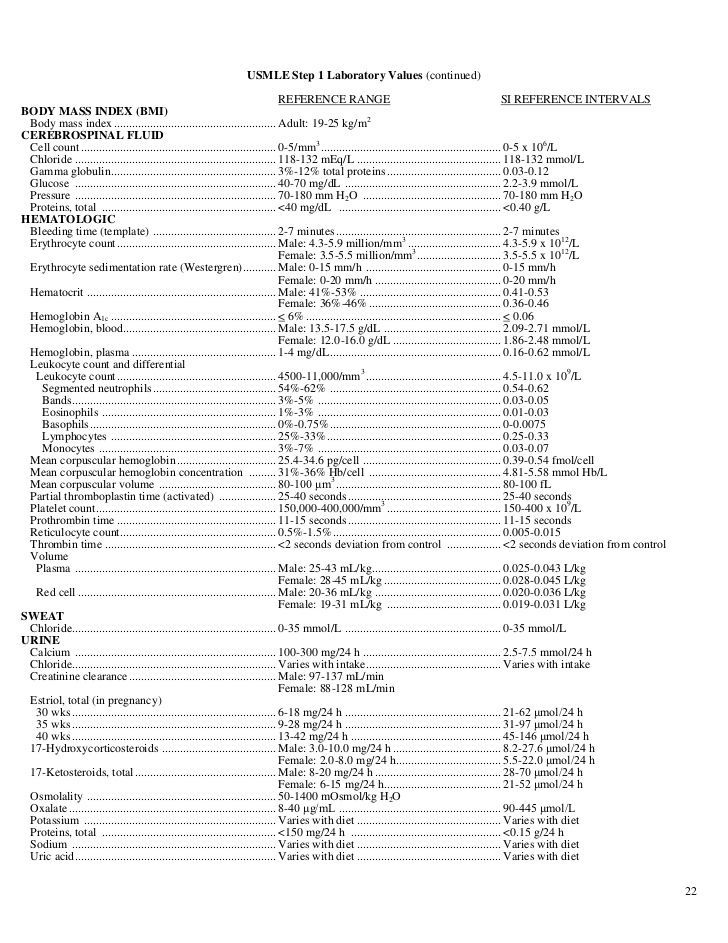
Laboratory tests
Tests of the blood, urine or skin might be used to screen for genetic or metabolic problems.
Additional tests
If your child is diagnosed with cerebral palsy, you'll likely be referred to specialists to test your child for other conditions often associated with the disorder. These tests can identify problems with:
- Vision
- Hearing
- Speech
- Intellect
- Development
- Movement
- Other medical conditions
The type of cerebral palsy is determined by the main movement disorder experienced, but several movement disorders can occur together. The most common type of cerebral palsy is spastic cerebral palsy, which includes stiff muscles and exaggerated reflexes. Other types of cerebral palsy include movement disorders involving poor balance and coordination (ataxic) and difficulty controlling voluntary muscles (dyskinetic).
The most common type of cerebral palsy is spastic cerebral palsy, which includes stiff muscles and exaggerated reflexes. Other types of cerebral palsy include movement disorders involving poor balance and coordination (ataxic) and difficulty controlling voluntary muscles (dyskinetic).
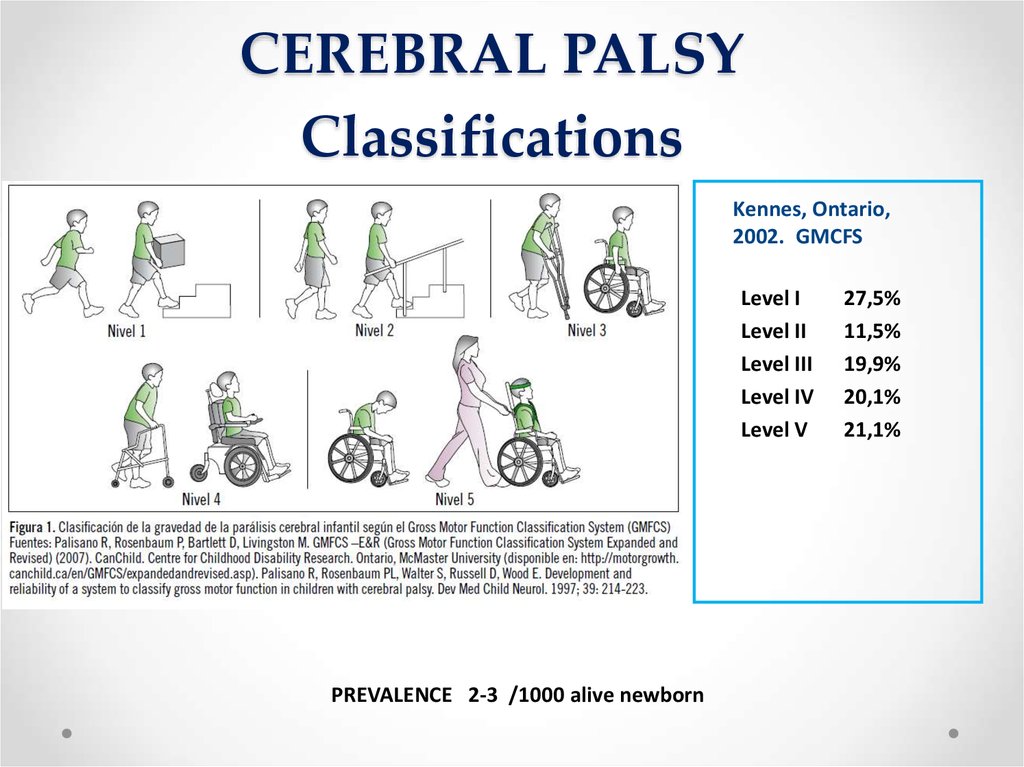
After making the diagnosis of cerebral palsy, your doctor may use a rating scale tool, such as the Gross Motor Function Classification System, to determine function and severity of mobility, posture and balance. This information can help in selecting treatments.
Care at Mayo Clinic
Our caring team of Mayo Clinic experts can help you with your cerebral palsy-related health concerns Start Here
More Information
- Cerebral palsy care at Mayo Clinic
- CT scan
- EEG (electroencephalogram)
- Genetic testing
- MRI
- Ultrasound
Treatment
Children and adults with cerebral palsy may require lifelong care with a medical care team. Besides a pediatrician or physical medicine and rehabilitation specialist (physiatrist) and possibly a pediatric neurologist to oversee your child's medical care, the team might include a variety of therapists and mental health specialists. These experts give special attention to needs and issues that are more common in people with cerebral palsy and can work together with your primary care provider. Together you can develop a treatment plan.
Besides a pediatrician or physical medicine and rehabilitation specialist (physiatrist) and possibly a pediatric neurologist to oversee your child's medical care, the team might include a variety of therapists and mental health specialists. These experts give special attention to needs and issues that are more common in people with cerebral palsy and can work together with your primary care provider. Together you can develop a treatment plan.
There is no cure for cerebral palsy. However, there are many treatments options that may help improve your child's daily functioning. Selecting care will depend on his or her specific symptoms and needs, and needs may change over time. Early intervention can improve outcomes.
Treatment options can include medications, therapies, surgical procedures and other treatments as needed.
Medications
Medications that can lessen muscle tightness might be used to improve functional abilities, treat pain and manage complications related to spasticity or other cerebral palsy symptoms.
-
Muscle or nerve injections. To treat tightening of a specific muscle, your doctor might recommend injections of onabotulinumtoxinA (Botox), or another agent. The injections will need to be repeated about every three months.
Side effects can include pain at the injection site and mild flu-like symptoms. Other more-serious side effects include difficulty breathing and swallowing.
-
Oral muscle relaxants. Drugs such as baclofen, tizanidine (Zanaflex), diazepam (Valium) or dantrolene (Dantrium) are often used to relax muscles.
In some cases, baclofen is pumped into the spinal cord with a tube (intrathecal baclofen). The pump is surgically implanted under the skin of the abdomen.
- Medications to reduce drooling. One option is Botox injections into the salivary glands.
Talk to your doctor about benefits and risks and possible side effects of recommended medication options.
Therapies
A variety of therapies play an important role in treating cerebral palsy:
-
Physical therapy. Muscle training and exercises can help your child's strength, flexibility, balance, motor development and mobility. You'll also learn how to safely care for your child's everyday needs at home, such as bathing and feeding your child. Your therapist can provide guidance on how you can continue muscle training and exercise at home between therapy visits.
For the first 1 to 2 years after birth, both physical and occupational therapists work on issues such as head and trunk control, rolling, and grasping. Later, both types of therapists are involved in wheelchair assessments.
Braces, splints or other supportive devices might be recommended for your child to help with function, such as improved walking, and stretching stiff muscles.
- Occupational therapy. Occupational therapists work to help your child gain independence in daily activities and routines at home and school and in the community.
 Adaptive equipment recommended for your child can include walkers, wide-based canes, standing and seating systems, or electric wheelchairs.
Adaptive equipment recommended for your child can include walkers, wide-based canes, standing and seating systems, or electric wheelchairs. - Speech and language therapy. Speech-language pathologists can help improve your child's ability to speak clearly or to communicate using sign language. They can also teach the use of communication devices, such as a computer and voice synthesizer, if communication is difficult. Speech therapists can also address difficulties with eating and swallowing.
- Recreational therapy. Some children benefit from regular or adaptive recreational or competitive sports, such as therapeutic horseback riding or skiing. This type of therapy can help improve your child's motor skills, speech and emotional well-being. Both adults and children benefit from regular physical activity and exercise for general health and fitness.
Surgical procedures
Surgery may be needed to lessen muscle tightness or correct bone abnormalities caused by spasticity. These treatments include:
These treatments include:
- Orthopedic surgery. Children with severe contractures or deformities might need surgery on bones or joints to place their arms, spine, hips or legs in their correct positions. Surgical procedures can also lengthen muscles and lengthen or reposition tendons that are shortened by contractures. These corrections can lessen pain and improve mobility. The procedures can also make it easier to use a walker, braces or crutches.
- Cutting nerve fibers (selective dorsal rhizotomy). In some severe cases, when other treatments haven't helped, surgeons might cut the nerves serving specific spastic muscles in a procedure called selective dorsal rhizotomy. This relaxes the muscle in the legs and reduces pain, but can cause numbness.
Other treatments
As needed, medications and other treatments may be recommended for seizures, pain, osteoporosis, mental health conditions, and problems with sleep, oral health, feeding and nutrition, bladder incontinence, vision, or hearing.
Adults with cerebral palsy
As your child with cerebral palsy becomes an adult, his or her health care needs can change. In addition to general health screenings recommended for all adults, ongoing health care includes evaluation and treatment for conditions that are more common in adults with cerebral palsy. These can include:
- Vision and hearing problems
- Maintenance of muscle tone
- Seizure management
- Problems with pain and fatigue
- Dental issues
- Orthopedic problems, such as contractures, arthritis and osteoporosis
- Heart and lung disease
- Mental health issues, such as depression
Request an Appointment at Mayo Clinic
Alternative medicine
Some children and adolescents with cerebral palsy use some form of complementary or alternative medicine. These are therapies that are unproved and have not been adopted into routine clinical practice. If you're considering a complementary or alternative medicine or therapy, talk with your doctor about potential risks and benefits.
Coping and support
When a child is diagnosed with a disabling condition, the whole family faces new challenges. Here are a few tips for caring for your child and yourself:
- Foster your child's independence. Encourage any effort at independence, no matter how small. At any age, your child's participation in social, educational, employment, recreational and other community activities can help them participate in society and have a positive effect on quality of life.
- Be an advocate for your child. You're an important part of your child's health care team. Don't be afraid to speak out on your child's behalf or to ask tough questions of your physicians, therapists and teachers.
- Find support. A circle of support can make a big difference in helping you and your family cope with cerebral palsy and its effects. As a parent, you might feel grief and guilt over your child's disability. Your doctor can help you locate support groups, organizations and counseling services in your community.
 Your child might also benefit from family support programs, school programs and counseling.
Your child might also benefit from family support programs, school programs and counseling. - Access services. Early intervention and special education services are available for children under 21 years of age through the Individuals with Disabilities Education Act. Services for adults with disabilities are also available. Talk with your health care team about how to access programs and services in your area.
Community resources and support for adults
In addition to addressing health needs, caring for your adult loved one with cerebral palsy may include planning for current and future lifestyle needs, such as:
- Guardianship
- Living arrangements
- Social and recreational participation
- Employment
- Financial support
Preparing for your appointment
If your child has cerebral palsy, how you learn about your child's condition can depend on the severity of the disabilities, when signs and symptoms started, and whether there were risk factors during pregnancy or delivery.
Here's some information to help you get ready for your child's appointment with his or her doctor.
What you can do
Before your appointment make a list of:
- Symptoms that concern you and when they began
- All medications, vitamins and other supplements your child takes, including doses
- Your child's medical history, including other conditions with which he or she has been diagnosed
- Information about your pregnancy and delivery, including any problems
- Questions to ask your doctor
Take a relative or friend with you, if possible, to help you remember the information you receive.
Questions to ask your doctor can include:
- What tests will my child need?
- When will we know the results of the tests?
- What specialists will we need to see?
- How will you monitor my child's health and development?
- Can you suggest educational materials and local support services regarding cerebral palsy?
- Can my child be followed through a multidisciplinary program that addresses all of his or her needs on the same visit, such as a cerebral palsy clinic?
Don't hesitate to ask other questions during your appointment.
What to expect from your doctor
Your doctor is likely to ask you questions, including:
- What concerns do you have about your child's growth or development?
- How well does your child eat?
- How does your child respond to touch?
- Do you observe favoring of one side of the body?
- Is your child reaching certain milestones in development, such as rolling over, pushing up, sitting up, crawling, walking or speaking?
- Did you have any problems during your pregnancy or delivery?
By Mayo Clinic Staff
Related
Associated Procedures
News from Mayo Clinic
Products & Services
Childhood Cerebral Palsy Answer Test (According to Approved Clinical Guidelines)
Magnetic resonance imaging (MRI) is a more sensitive diagnostic tool for diagnosing early brain damage.
- free
- children
- Children
- CCP
- Clinical
- Medical
- NMO
- Paralya
- s
- topic
- Test
- y
- approved
- cerebral
005 recommendations
Magnetic resonance imaging (MRI) is more sensitive for early diagnosis of brain lesions.
1. What form of cerebral palsy is hemiplegia?
1) ataxic form;
2) atonic-astatic form;
3) dystonic form;
4) spastic form.+
2. What form of cerebral palsy is diplegia?
1) atonic-astatic form;
2) hypotonic form;
3) dystonic form;
4) spastic form.+
3. What is the time interval for the development of cerebral palsy in the initial residual stage?
1) up to 1 year;
2) up to 4-5 months;
3) from 6 months to 3 years; +
4) over 3 years old.
4. According to the functional classification, what level of development of large motor functions does walking with the use of hand-held devices for movement belong to?
1) level II;
2) level III;+
3) level IV;
4) level V.
5. What is the level of confidence in the treatment of local spasticity with antispastic drugs?
1) D;
2) A;+
3) B;
4) С.
6. What level of reliability is the performance of physical rehabilitation methods?
1) D;
2) A;
3) B;
4) С.+
7. What is the level of reliability of generalized spasticity with antispastic drugs?
1) D;
2) A;
3) B;+
4) C.
8. According to the functional classification, what level of development of large motor functions does limited walking belong to?
1) level II;+
2) level III;
3) level IV;
4) level V.
9. What is the time interval for the development of cerebral palsy in the late residual stage?
1) up to 1 year;
2) up to 4-5 months;
3) from 6 months to 3 years;
4) over 3 years old.+
10. What is the maximum total dose of Botox per procedure to reduce local spasticity in cerebral palsy?
1) 100 units;
2) 200 U;+
3) 300 U;
4) 400 units
11. What neurosurgical treatments for spasticity are used in cerebral palsy?
What neurosurgical treatments for spasticity are used in cerebral palsy?
1) selective dorsal rhizotomy; +
2) stimulation of the cerebral cortex;
3) installation of an intrathecal baclofen pump; +
4) chronic epidural spinal cord stimulation.
1) cephalohematoma;
2) hemorrhages in the membranes and substance of the brain;+
3) crushing and necrosis of the medulla;+
4) compression of the brain.+
13. What are the stages of development of cerebral palsy?
1) initial residual stage; +
2) late residual; +
3) premature;
4) early.+
14. What are the risk factors for developing cerebral palsy?
1) anomalies of placental circulation;+
2) immunological compatibility of maternal and fetal blood;
3) uterine bleeding; +
4) placenta previa or placenta abruption.
1) deformities and shortening of limbs; +
2) brachial plexopathy;
3) scoliosis;+
4) articular-muscular contractures.+
16. What are the alternative treatments for cerebral palsy?
1) acupuncture; +
2) botulinum therapy;
3) hippotherapy;+
4) osteopathy.+
17. What methods of physical rehabilitation are used for cerebral palsy?
1) acupuncture;
2) kinesiotherapy;+
3) therapeutic exercises;+
4) massage.+
18. What disorders are related to the mixed form of cerebral palsy?
1) atactico-hyperkinetic;+
2) hypotonic;
3) spastic-ataxic;+
4) spastic-hyperkinetic.+
19. What complications during childbirth are risk factors for developing cerebral palsy?
What complications during childbirth are risk factors for developing cerebral palsy?
1) a long period of standing of the head in the birth canal; +
2) instrumental obstetrics;+
3) 1st degree vaginal rupture;
4) breech and pelvic presentation of the fetus. +
20. Which drugs are centrally acting muscle relaxants?
1) Baclofenage;+
2) Tizanidine;+
3) Tolperisone;+
4) Botulinic toxin type A.
21. What are the additional drugs in the treatment of children's cerebral paralysis?
1) M- and N-cholinolytics; +
2) angioprotectors; +
3) dopaminomimetics; +
4) centrally acting muscle relaxants.
22. What symptoms can occur in all forms of cerebral palsy?
1) pathological synkinetic activity; +
2) pathological tonic reflexes; +
3) increased general reflex excitability; +
4) decrease in general reflex excitability.
23. What are the symptoms of spastic diplegia?
1) bilateral limb lesions; +
2) legs are affected to a greater extent; +
3) early formation of deformities and contractures; +
4) hands are affected to a greater extent.
24. What are the symptoms of spasticity?
1) hyperexcitability of stretch receptors; +
2) increase in tendon reflexes; +
3) increase in muscle tone; +
4) decrease in muscle tone.
25. What factors are "alarming" in the differential diagnosis of cerebral palsy?
1) multiple developmental anomalies in a child; +
2) repeated cases of cerebral palsy or early death of children in the family without an established cause; +
3) the presence of perinatal risk factors in the patient;
4) loss of previously acquired skills. +
+
Badalyan?
1) ataxic form;
2) hypotonic form;+
3) dystonic form;+
4) spastic forms.+
Badalyan?
1) atonic-astatic form; +
2) hypotonic form;
3) hyperkinetic form;+
4) spastic forms.+
1) atonic-astatic form;+
2) hemiplegic form;+
3) hyperkinetic form;+
4) double hemiplegia;+ 9004;+ 0050 5) choreoathetosis.
29. What stages are included in the pathogenesis of structural disorders of embryonic development as a risk factor for cerebral palsy?
1) intrauterine fetal hypoxia; +
2) impaired uteroplacental circulation; +
3) inhibition of the synthesis of nucleic acids and proteins; +
4) inhibition of the synthesis of carbohydrates.
30. Which diagnostic method is more sensitive for diagnosing brain damage in the early stages?
1) computed tomography;
2) magnetic resonance imaging; +
3) ultrasound;
4) electroencephalogram.
31. What method allows you to determine the functional activity of the brain?
1) video-EEG monitoring; +
2) computed tomography;
3) magnetic resonance imaging;
4) ultrasound.
32. When is a genetic consultation indicated for cerebral palsy?
1) with a clinical picture of "sluggish child syndrome"; +
2) with dysembryogenesis stigmas; +
3) with severe birth asphyxia;
4) with burdened perinatal history.
33. When is neurosurgical treatment recommended?
1) if alternative methods of treatment are ineffective;
2) Botulinum toxin type A injections fail;+
3) with ineffectiveness of oral antispastic drugs; +
4) immediately after the diagnosis of cerebral palsy.
34. What is the basis for calculating the dose of botulinum toxin type A?
1) the number of units of the drug per kilogram of body weight per muscle;+
2) the number of units of the drug per injection point;+
3) per surface area;
4) total dose per kilogram of body weight +
35. What determines the duration of continuous stay of a child with cerebral palsy in a medical institution?
1) disease duration;
2) concomitant pathology; +
3) severity of movement disorders; +
4) forms of the disease.
36. List the leading causes of cerebral palsy:
1) anomalies in the development of the brain of the fetus and newborn; +
2) caesarean section;
3) obesity before pregnancy; +
4) damage to the brain of the fetus and newborn +
3) acute or chronic extragenital diseases of the mother; +
4) medication during pregnancy. +
+
38. List the main points of the pathophysiology of cerebral palsy:
1) brain damage; +
2) muscle hypotonia develops predominantly;
3) The preservation of gate reflexes and related disorders of the formation of chain installation rectifier reflexes;+
4) Formation of pathological muscle tone.+
39. List the common symptoms of spastic duplia: 9004 speech development; +
2) presence of pseudobulbar syndrome; +
3) hearing impairment; +
4) low muscle tone.
40. At what level of development of large motor functions, according to the functional classification, motorized vehicles can be used?
1) level II;
2) level III;
3) level IV;+
4) level V.
41. How many age groups does the functional classification of cerebral palsy include?
1) two groups;
2) five groups;+
3) three groups;
4) four groups.
42. How many units per kilogram of body weight of a child is the dose of Botox to reduce local spasticity in cerebral palsy?
1) 2-4 U/kg;
2) 4-6 U/kg; +
3) 6-8 U/kg;
4) 8-10 U/kg.
43. What does the functional classification of cerebral palsy evaluate?
1) degree of physical development;
2) degree of restriction of movements;+
3) degree of mental retardation;
4) the degree of development of motor skills. +
← Test with answers on the topic "Topical issues in the work of a dental technician"↑ Tests NMO Test with answers on the topic "Actual issues of preventive dentistry" →
Test with answers on the topic " Cerebral palsy in children (according to approved clinical guidelines)
psycholog 0 Comments cerebral palsy, classification, methods, brain, preparations, development, spasticity, test with answers, level, form
guidelines)” (2 SG) with alphabetical answers. This test with answers on topic "Cerebral palsy in children (according to approved clinical guidelines)" (2 ZET) will allow you to successfully prepare for the final certification in the direction "Pediatrics" .
This test with answers on topic "Cerebral palsy in children (according to approved clinical guidelines)" (2 ZET) will allow you to successfully prepare for the final certification in the direction "Pediatrics" .
Hemiplegia refers to the spastic form of cerebral palsy. The initial residual stage refers to the interval of development of cerebral palsy, starting from 6 months to 3 years. Neurosurgical methods for the treatment of spasticity in cerebral palsy include selective dorsal rhizotomy, intrathecal baclofen pumps, and chronic epidural spinal cord stimulation.
1. What form of cerebral palsy is hemiplegia?
1) ataxic form;
2) atonic-astatic form;
3) dystonic form;
4) spastic form. +
2. What form of cerebral palsy is diplegia?
1) atonic-astatic form;
2) hypotonic form;
3) dystonic form;
4) spastic form. +
+
3. What is the time interval for the development of cerebral palsy in the initial residual stage?
1) up to 1 year;
2) up to 4-5 months;
3) from 6 months to 3 years; +
4) over 3 years old.
4. According to the functional classification, what level of development of large motor functions does walking with the use of hand-held mobility aids belong to?
1) level II;
2) level III; +
3) level IV;
4) level V.
5. What is the level of confidence in the treatment of local spasticity with antispastic drugs?
1) D;
2) A; +
3) B;
4) С.
6. What level of reliability is the performance of physical rehabilitation methods?
1) D;
2) A;
3) B;
4) C. +
7. What is the level of confidence in the treatment of generalized spasticity with antispastic drugs?
1) D;
2) A;
3) B; +
4) С.
8. According to the functional classification, what level of development of large motor functions does limited walking belong to?
1) level II; +
2) level III;
3) level IV;
4) level V.
9. What is the time interval for the development of cerebral palsy in the late residual stage?
1) up to 1 year;
2) up to 4-5 months;
3) from 6 months to 3 years;
4) over 3 years old. +
10. What is the maximum total dose of Botox per procedure to reduce local spasticity in cerebral palsy?
1) 100 units;
2) 200 U; +
3) 300 units;
4) 400 units
11. What neurosurgical treatments for spasticity are used in cerebral palsy?
1) selective dorsal rhizotomy; +
2) stimulation of the cerebral cortex;
3) installation of an intrathecal baclofen pump; +
4) chronic epidural stimulation of the spinal cord. +
+
12. What types of birth trauma are the cause of cerebral palsy?
1) cephalohematoma;
2) hemorrhages in the membranes and substance of the brain; +
3) crushing and necrosis of the medulla; +
4) compression of the brain. +
13. What are the stages of development of cerebral palsy?
1) initial residual stage; +
2) late residual; +
3) premature;
4) early. +
14. What are the risk factors for developing cerebral palsy?
1) anomalies of the placental circulation; +
2) immunological compatibility of maternal and fetal blood;
3) uterine bleeding; +
4) placenta previa or placental abruption. +
15. What changes are typical for orthopedic pathology in cerebral palsy?
1) deformities and shortening of the limbs; +
2) brachial plexopathy;
3) scoliosis; +
4) articular-muscular contractures. +
+
16. What are the alternative treatments for cerebral palsy?
1) acupuncture; +
2) botulinum therapy;
3) hippotherapy; +
4) osteopathy. +
17. What methods of physical rehabilitation are used for cerebral palsy?
1) acupuncture;
2) kinesiotherapy; +
3) therapeutic exercises; +
4) massage. +
18. What disorders are related to the mixed form of cerebral palsy?
1) atactico-hyperkinetic; +
2) hypotonic;
3) spastic-ataxic; +
4) spastic-hyperkinetic. +
19. Which birth complications are risk factors for developing cerebral palsy?
1) a long period of standing of the head in the birth canal; +
2) instrumental obstetrics; +
3) 1st degree vaginal rupture;
4) breech and breech presentation of the fetus. +
+
20. Which drugs are centrally acting muscle relaxants?
1) Baclofenage; +
2) Tizaniding; +
3) Tolperisone; +
4) botulinum toxin type A.
21. What drugs are additional in the treatment of cerebral palsy?
1) M- and N-cholinolytics; +
2) angioprotectors; +
3) dopaminomimetics; +
4) muscle relaxants of central action.
22. What symptoms can occur in all forms of cerebral palsy?
1) pathological synkinetic activity; +
2) pathological tonic reflexes; +
3) increase in general reflex excitability; +
4) decrease in general reflex excitability.
23. What are the symptoms of spastic diplegia?
1) bilateral limb lesion; +
2) the legs are affected to a greater extent; +
3) early formation of deformities and contractures; +
4) hands are affected to a greater extent.
24. What are the symptoms of spasticity?
1) hyperexcitability of stretch receptors; +
2) increased tendon reflexes; +
3) increased muscle tone; +
4) decrease in muscle tone.
25. What factors are "alarming" in the differential diagnosis of cerebral palsy?
1) multiple developmental anomalies in a child; +
2) repeated cases of cerebral palsy or early death of children in the family without an established cause; +
3) the patient has perinatal risk factors;
4) loss of previously acquired skills. +
26. What forms of cerebral palsy occur at an early age according to L.O. Badalyan?
1) ataxic form;
2) hypotonic form; +
3) dystonic form; +
4) spastic forms. +
27. What forms of cerebral palsy occur in older age according to L.O. Badalyan?
1) atonic-astatic form; +
2) hypotonic form;
3) hyperkinetic form; +
4) spastic forms. +
+
28. What forms of cerebral palsy are included in the classification of Semenova K.A.
1) atonic-astatic form; +
2) hemiplegic form; +
3) hyperkinetic form; +
4) double hemiplegia; +
5) choreoathetosis.
29. What stages are included in the pathogenesis of structural disorders of embryonic development as a risk factor for cerebral palsy?
1) intrauterine fetal hypoxia; +
2) violation of uteroplacental circulation; +
3) inhibition of the synthesis of nucleic acids and proteins; +
4) inhibition of carbohydrate synthesis.
30. Which diagnostic method is more sensitive for diagnosing brain damage in the early stages?
1) computed tomography;
2) magnetic resonance imaging; +
3) ultrasound examination;
4) electroencephalogram.
31. What method allows you to determine the functional activity of the brain?
1) video EEG monitoring; +
2) computed tomography;
3) magnetic resonance imaging;
4) ultrasound.
32. When is a genetic consultation indicated for cerebral palsy?
1) with the clinical picture of "sluggish child syndrome"; +
2) in the presence of disembryogenesis stigmas; +
3) in the presence of severe birth asphyxia;
4) with burdened perinatal history.
33. When is neurosurgical treatment recommended?
1) if alternative methods of treatment are ineffective;
2) Botulinum toxin type A injections fail; +
3) in case of ineffectiveness of oral antispastic drugs; +
4) immediately after the diagnosis of cerebral palsy.
34. What is the basis for calculating the dose of botulinum toxin type A?
1) the number of units of the drug per kilogram of body weight per muscle; +
2) the number of units of the drug per injection point; +
3) per surface area;
4) total dose per kilogram of body weight.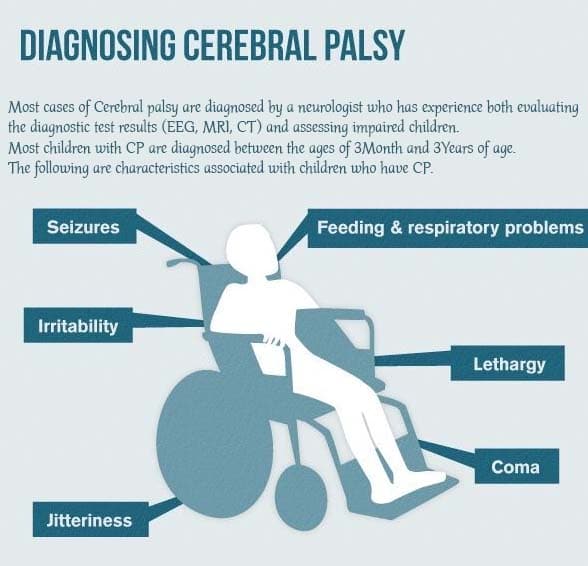 +
+
35. What determines the length of continuous stay of a child with cerebral palsy in a medical institution?
1) disease duration;
2) concomitant pathology; +
3) severity of movement disorders; +
4) forms of the disease.
36. List the leading causes of cerebral palsy:
1) anomalies in the development of the brain of the fetus and newborn; +
2) cesarean section;
3) obesity before pregnancy;
4) damage to the brain of the fetus and newborn. +
37. List the intrauterine causes of cerebral palsy:
1) parental alcoholism; +
2) overweight before pregnancy;
3) acute or chronic extragenital diseases of the mother; +
4) medication during pregnancy. +
38. List the main points of the pathophysiology of cerebral palsy:
1) brain damage; +
2) muscle hypotonia develops predominantly;
3) preservation of postural reflexes and concomitant disorders in the formation of chain adjusting rectifying reflexes; +
4) formation of pathological muscle tone.