Normal lab values in pregnancy
Pregnancy: laboratory measurements
Home / ABA Keyword Categories / Obstetric Anesthesia / Pregnancy: laboratory measurements
Definition
Pregnancy is known to be a state of “physiologic anemia” due to the disproportionate increase in plasma volume relative to red blood cell volume. This increase in blood volume is necessary to supply the fetus and placenta and begins very early in pregnancy. The plasma volume is already increased by 10-15% at 6 weeks of gestation and increases to 30-50% greater than pre-pregnancy volume by term. The red cell volume, in contrast to this, is only increased by 20-30% at term. This increase is prompted by a higher level of erythropoietin. Thus, despite a higher red cell volume, the hematocrit will fall during pregnancy. The greatest time of disproportion between the plasma volume and red cell volume changes will be at 28-36 weeks. Anemia during pregnancy is defined differently than someone who is not pregnant. To be considered anemic during pregnancy the hemoglobin needs to be less than 11g/dL in the 1st or 3rd trimesters.
Other hematologic changes in pregnancy include an increase in white blood cells, particularly neutrophils, and a slight decrease in platelet count. The average white cell count during pregnancy is about 9-15k. It increases up to term, and can go as high as 25k during labor. Platelets, on the other hand, remain in the normal non-pregnant range but mean platelet counts may be slightly lower than in healthy non-pregnant women. The “low normal” range is considered to be about 106-120k.
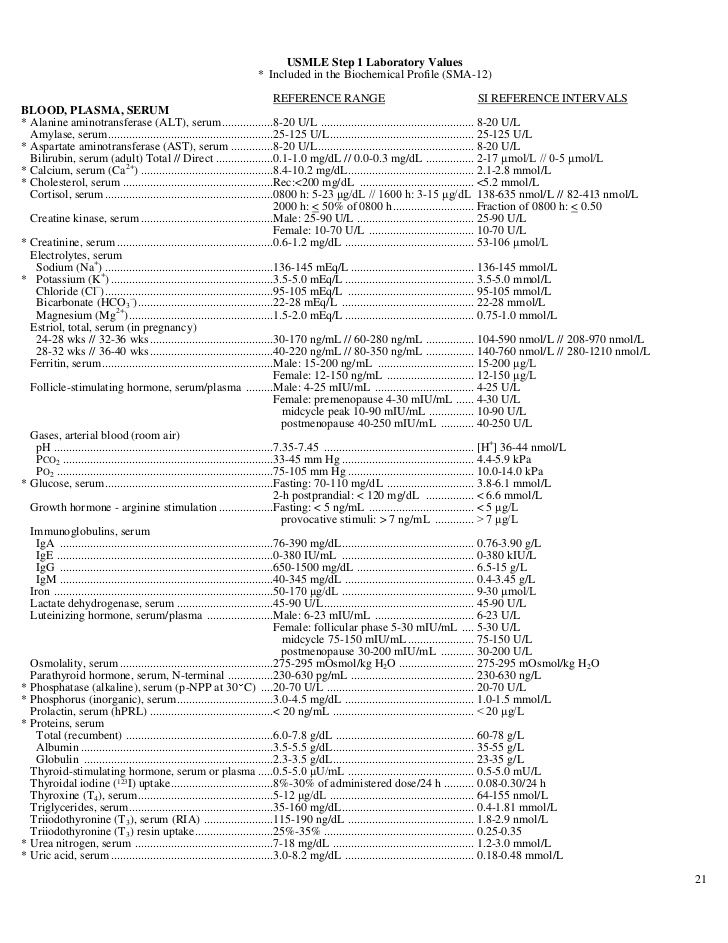
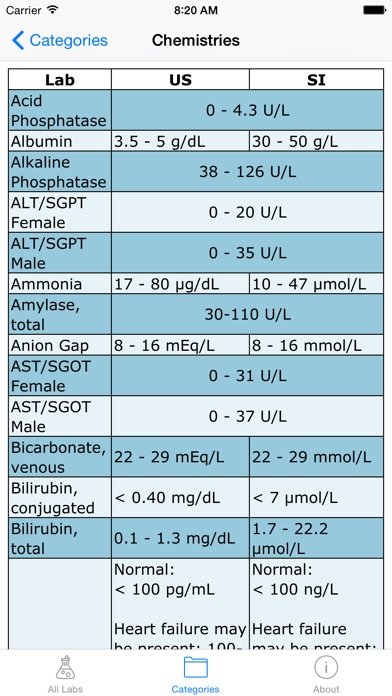
There are also many changes in blood chemistries during pregnancy as well, mostly by the same dilutional mechanism as the hematocrit. Important among these are albumin, total protein and creatinine. Both albumin and total protein decrease by about 1g/dL by mid-pregnancy and creatinine decreases by about 0.3mg/dL. For other chemistry changes, see chart (below).
| Blood Chemistry | |||
| Albumin | 3.5-4.8 g/dL | 1 g/dL decrease | By midpregnancy |
| Calcium | 9.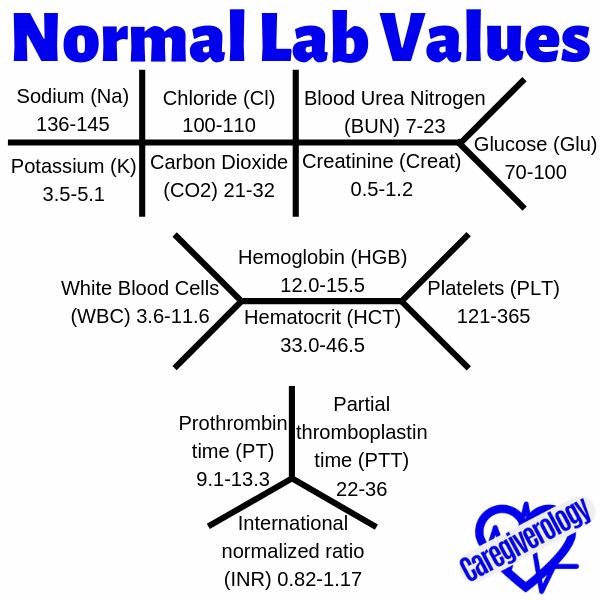 0-10.3 mg/dL 0-10.3 mg/dL | 10% decrease | Falls gradually |
| Chloride | 95-105 mEq/L | No change | |
| Cholesterol | 200-240 mg/dL | 50% increase | Rises steadily |
| Creatinine | 0.6–1.1 mg/dL | 0.3 mg/dL increase | By midpregnancy |
| Fibrinogen | 200–400 mg/dL | 1.5-3x increase | By term |
| Glucose, fasting | 65–105 mg/dL | 10% decrease | Gradual fall |
| Potassium (plasma) | 3.5–4.5 mEq/L | 0.2–0.3 mEq/L decrease | By midpregnancy |
| Protein (total) | 6.5–8.5 g/dL | 1 g/dL decrease | By midpregnancy |
| Sodium | 135–145 mEq/L | 2–4 mEq/L decrease | By midpregnancy |
| Urea nitrogen | 12–30 mg/dL | 50% decrease | First trimester |
| Uric acid | 3.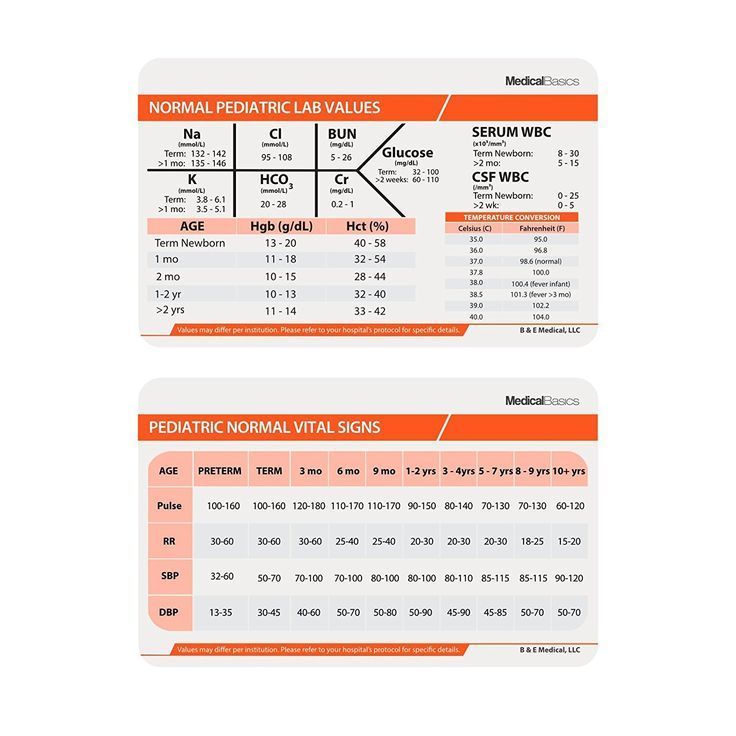 5–8 mg/dL 5–8 mg/dL | 33% decrease | First trimester |
| Urine Chemistry | |||
| Creatinine | 15–25 mg/kg/d | No change | |
| Protein | Up to 150 mg/d | Up to 250–300 mg/day | By midpregnancy |
| Creatinine clearance | 90–130 mL/min/1.73 m2 | 40–50% increase | By 16 weeks |
| Serum Enzymes | |||
| Alkaline phosphatase | 30–120 U/L | 2x to 4x increase | By 20 weeks |
| Amylase | 60–180 U/L | Controversial | |
| Creatinine phosphokinase | 26–140 U/L | 2- to 4-fold increase | After labor (MB bands as well) |
| Lipase | 10–140 U/L | No change | |
| Aspartate aminotransferase (AST) | 5–35 mU/mL | No change | |
| Alanine Aminotransferase (ALT) | 5–35 mU/mL | No change | |
| Formed Elements of Blood | |||
| Hematocrit | 36–46% | 4–7 point decrease | Nadir at 30–34 weeks |
| Hemoglobin | 12–16 g/dL | 1.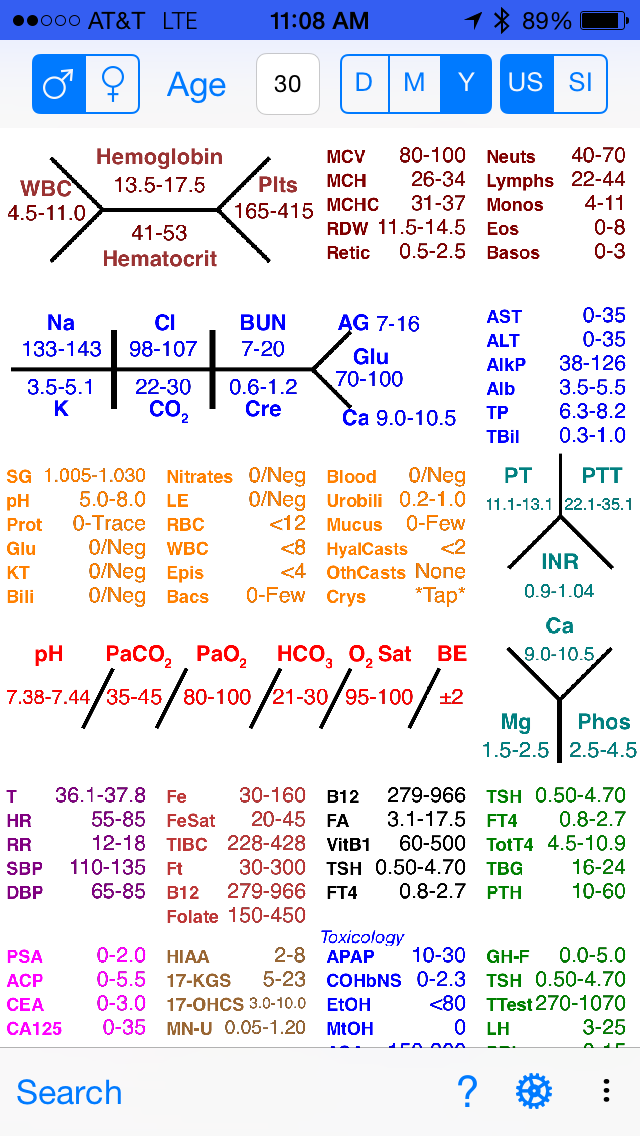 4–2.0 g/dL decrease 4–2.0 g/dL decrease | Nadir at 30–34 weeks |
| Leukocyte count | 4.8–10.8 x 103/mm3 | 3.5 x 103/mm3 increase | Gradual increase to term, as high as 25 x 103/mm3 in labor |
| Platelets | 150–400 x 103/mm3 | Slight decrease | Gradual |
Subspecialty
Obstetric Anesthesia
Related Media
Keyword history
71%/2008
See Also:
Pregnancy: Heme and electrolyte changes
Sources
PubMed
Filed Under: Obstetric Anesthesia, Obstetric Anesthesia, P
Laboratory Tests, Results and Normal Values In Pregnancy
Skip to main content
Pregnancy » Prenatal Testing
By:
Amos Grünebaum
Updated on February 18, 2022
Pregnancy is a special time of a woman's life that affects many different parts of the body. Most laboratory tests remain the same whether you are pregnant or not, while other laboratory tests that may be considered abnormal when not pregnant, can be considered normal during pregnancy. Below are the normal ranges for various lab tests whether you are pregnant or not.
Most laboratory tests remain the same whether you are pregnant or not, while other laboratory tests that may be considered abnormal when not pregnant, can be considered normal during pregnancy. Below are the normal ranges for various lab tests whether you are pregnant or not.
Track your pregnancy
Blood tests during and outside pregnancy
- ALT, SGPT
- Albumin
- Aldosterone (Serum or Plasma)
- Alpha-Fetoprotein
- Alkaline Phosphatase
- Amylase
- APTT
- Alpha-1 Antitrypsin
- Alpha-Fetoprotein
- Angiotensin Converting Enzyme
- Anion Gap (Plasma, Serum)
- Antithrombin III, functional
- Apolipoprotein A-1
- Apolipoprotein B
- Aspartate Aminotransferase AST, SGOT
- Basophil Count
- Bicarbonate
- Bile Acids
- Bilirubin - Conjugated, Direct
- Bilirubin - Total
- Bilirubin - Unconjugated, Indirect
- Calcium - Ionized (Serum)
- Calcium - Total (Serum)
- Cancer Antigen - 125 (Serum CA)
- Cell-Free DNA Blood Test
- Ceruloplasmin (Serum)
- Chloride (Plasma, Serum)
- Cholesterol - HDL (Plasma, Serum)
- Cholesterol - LDL (Plasma, Serum)
- Cholesterol - Total (Plasma, Serum)
- Cholesterol - VLDL (Plasma, Serum)
- Complement - C3 (Serum)
- Complement - C4 (Serum)
- Copper (Serum)
- Cortisol (Plasma, Serum)
- C-reactive Protein (Serum)
- Creatinine (Plasma, Serum)
- Creatine Kinase - Total (Serum)
- D-dimer (Plasma)
- Dehydroepiandrosterone Sulfate - DHEA-S (Serum)
- Eosinophil Count (Whole Blood)
- Erythrocyte Sedimentation Rate - ESR (Whole Blood)
- Erythropoietin (Serum)
- Estradiol (Serum)
- Factor V (Plasma)
- Factor VII (Plasma)
- Factor VIII (Plasma)
- Folate (Serum)
- Folate - Red Cell (Whole blood)
- Follicle Stimulating Hormone (FSH)
- Gamma Glutamyl Transferase - Gamma Glutamyl Transpeptidase - GGT (Serum)
- Glomerular Filtration Rate (GFR)
- Glucose - Fasting (Plasma)
- Hepatitis A
- Hepatitis B
- Hepatitis C
- Homocysteine (Plasma)
- Hemoglobin (Whole Blood)
- Hemoglobin A1c - Glycated Hemoglobin (Whole Blood)
- Hemoglobin Electrophoresis
- Hematocrit (Whole Blood)
- Immunoglobulin A (IgA) - Quantitative (Serum)
- Immunoglobulin G (IgG) (Serum)
- Immunoglobulin M (IgM) (Serum)
- Iron (Serum)
- Lactate Dehydrogenase LDH (Serum)
- Lipase (Serum)
- Mean Corpuscular Hemoglobin Concentration (MCHC) (Whole Blood)
- Luteinizing Hormone (LH)
- Mean Corpuscular Hemoglobin (MCH) (Whole Blood)
- Magnesium (Serum)
- Lymphocyte Count (Whole Blood)
- Neutrophil Count (Whole Blood)
- Platelet Count
- Osmolality (Serum)
- Phosphorus - Inorganic Phosphate (Serum)
- Mean Platelet Volume (MPV) (Whole Blood)
- Monocyte Count (Whole Blood)
- Prealbumin - Transthyretin (Serum)
- Parathyroid Hormone-Related Protein (Serum)
- Parathyroid Hormone (Serum)
- Potassium (Serum)
- Prothrombin Time (Plasma)
- Protein S - Free (Plasma)
- Protein S Functional Activity (Plasma)
- Protein C Functional Activity (Plasma)
- Red Blood Cell Count - RBC (Whole Blood)
- Prolactin (Serum)
- Protein - Total (Serum)
- Red Cell Distribution Width (RCD) (Whole Blood)
- Progesterone (Serum)
- Protein S - Total (Plasma)
- Testosterone - Total (Serum)
- Sex Hormone Binding Globulin (Serum)
- Sodium (Serum)
- Thyroxine-Binding Globulin (TBG) (Serum)
- Selenium (Plasma, Serum)
- Thyroid Stimulating Hormone (TSH)
- Thyroxine - T4 (Serum)
- Thyroxine Free - Thyroxine Direct - FT4 - Free T4 - Unbound T4 (Serum)
- Antigen Tissue Plasminogen Activator (tPA) (Plasma)
- Antigen Tissue Plasminogen Activator Inhibitor-1 (PAI) (Plasma)
- Triglycerides (Serum)
- Transferrin (Serum)
- Total Iron-Binding Capacity - TIBC (Serum)
- Urea Nitrogen - BUN (Serum)
- 24 Hour Sodium (24 Hour Urine Collection) (Excretion)
- Retinol - Vitamin A (Serum)
- 1, 25 Dihydroxy - Vitamin D (Serum)
- 25 - Hydroxy - Vitamin D (Plasma)
- 24 Hour Potassium (24 Hour Urine Collection)
- Ascorbic Acid - Vitamin C (Serum)
- 24 Hour Urine Collection - 24 Hour Creatinine Collection (Clearance)
- Alpha-Tocopherol - Vitamin E (Serum)
- Uric Acid (Serum)
- 17 - Hydroxyprogesterone (Serum)
- 24 Hour Protein Excretion (Urine)
- 3-Hour Glucose Tolerance Test
- 1-Hour Glucose Tolerance Test (Plasma, Serum)
- White Blood Cell Count (WBC)
- Zinc (Serum)
- Cobalamin - Vitamin B12 (Serum)
Reference:
Pregnancy and Laboratory Studies
A Reference Table for Clinicians
Abbassi-Ghanavati, Mina MD; Greer, Laura G.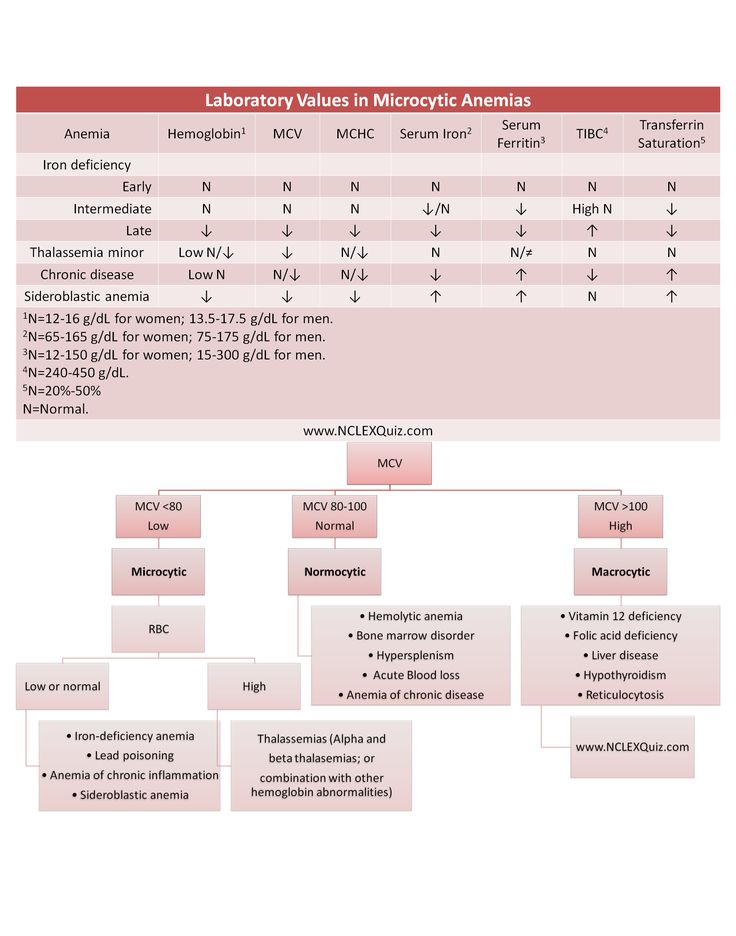 MD; Cunningham, F Gary MD
MD; Cunningham, F Gary MD
Author Information
Obstetrics & Gynecology: December 2009 - Volume 114 - Issue 6 - p 1326-1331
doi: 10.1097/AOG.0b013e3181c2bde8
Keyword Tags:
Pregnancy
Physiological changes in blood parameters during pregnancy
- INVITRO
- Library
- Laboratory ...
- Physiological ...
Pregnancy
ECO
14510 10 October
IMPORTANT!
The information in this section should not be used for self-diagnosis or self-treatment.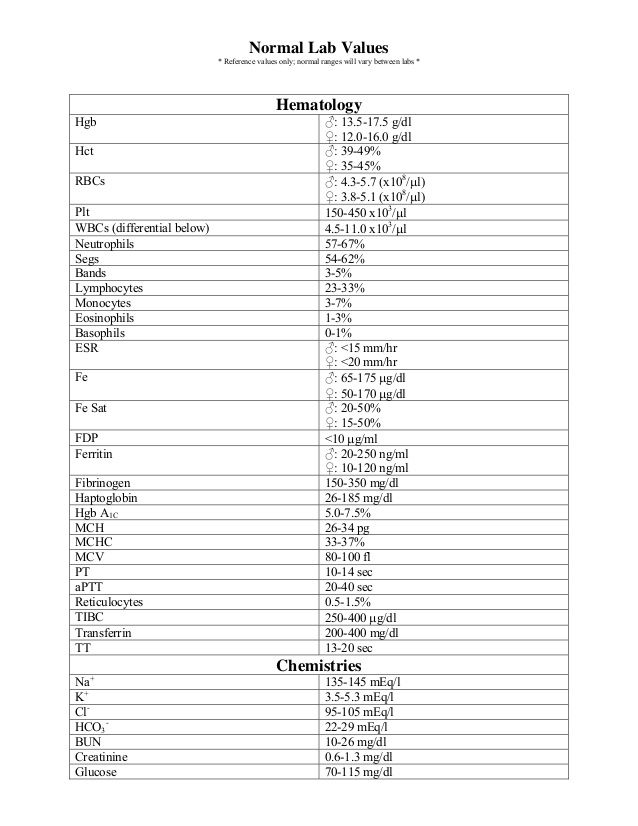 In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
For a correct assessment of the results of your analyzes in dynamics, it is preferable to do studies in the same laboratory, since different laboratories may use different research methods and units of measurement to perform the same analyzes.
Changes in coagulogram and clinical blood tests.
Changes in the coagulogram (No. 1, 2, 3, 4, 190, 164, 194) * of a pregnant woman is a physiological process associated with the appearance of the uteroplacental circulation. This process is associated with the evolutionary, adaptive reactions of the body of a pregnant woman. The body of a woman prepares for the costs during gestation and possible blood loss during childbirth. During the physiological course of pregnancy, the activity of the procoagulant link increases.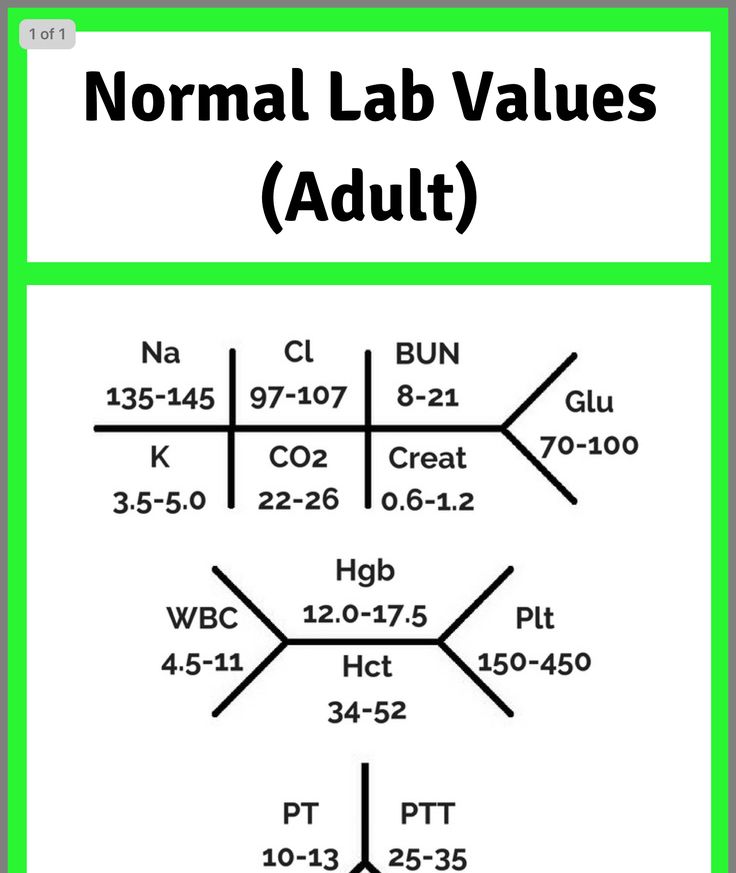 Already at the 3rd month of pregnancy, fibrinogen rises (this is the factor I (first) of the plasma coagulation system) and reaches maximum values on the eve of childbirth. Therefore, gynecologists reasonably recommend monitoring this indicator during pregnancy (1 time per trimester, if there are deviations of these indicators more often, 1 time per week). At the end of the third trimester of pregnancy, the concentration of fibrinogen in the serum increases, which may correspond to an increase in the processes of intravascular blood coagulation in the uteroplacental blood flow.
Already at the 3rd month of pregnancy, fibrinogen rises (this is the factor I (first) of the plasma coagulation system) and reaches maximum values on the eve of childbirth. Therefore, gynecologists reasonably recommend monitoring this indicator during pregnancy (1 time per trimester, if there are deviations of these indicators more often, 1 time per week). At the end of the third trimester of pregnancy, the concentration of fibrinogen in the serum increases, which may correspond to an increase in the processes of intravascular blood coagulation in the uteroplacental blood flow.
Simultaneously with the increase in fibrinogen and the activity of the external coagulation pathway, the activity of the internal mechanism of blood coagulation also increases, while shortening of the APTT is noted. Other links of the hemostasis system also change during pregnancy, such as a coagulation inhibitor - antithrombin III, which has a protein structure and has the ability to inhibit two or more fibrinolysis coagulation factors and the compliment system.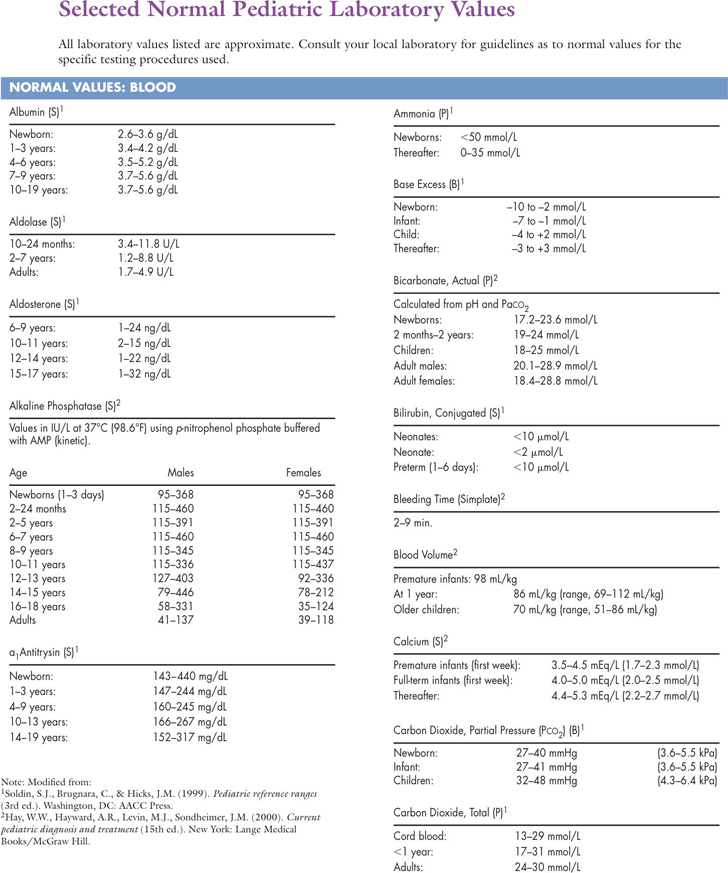 As pregnancy progresses, there is a gradual decrease in antithrombin III activity. In pregnant women, starting from early pregnancy, the level of D-dimer in the blood gradually increases. By the end of the gestation period, its values can be 3-4 times higher than the initial level. Lupus anticoagulant should not be produced normally in a pregnant woman. Pregnant women may experience slight changes in the complete blood count (No. 5). Indicators such as hemoglobin, hematocrit may decrease in the second half of pregnancy, and leukocytes may increase (#119)*.
As pregnancy progresses, there is a gradual decrease in antithrombin III activity. In pregnant women, starting from early pregnancy, the level of D-dimer in the blood gradually increases. By the end of the gestation period, its values can be 3-4 times higher than the initial level. Lupus anticoagulant should not be produced normally in a pregnant woman. Pregnant women may experience slight changes in the complete blood count (No. 5). Indicators such as hemoglobin, hematocrit may decrease in the second half of pregnancy, and leukocytes may increase (#119)*.
Changes in biochemical parameters
During pregnancy, a decrease in the total concentration of protein in the blood plasma is due to both partial dilution, as a result of fluid retention in the body, and a decrease in the concentration of albumin (No. 10) *. The decrease in albumin is due to its increased consumption for biosynthetic processes. However, it is impossible to exclude the factor of increasing vascular permeability and the redistribution of fluid and protein in the intercellular space, the violation of hemodynamics.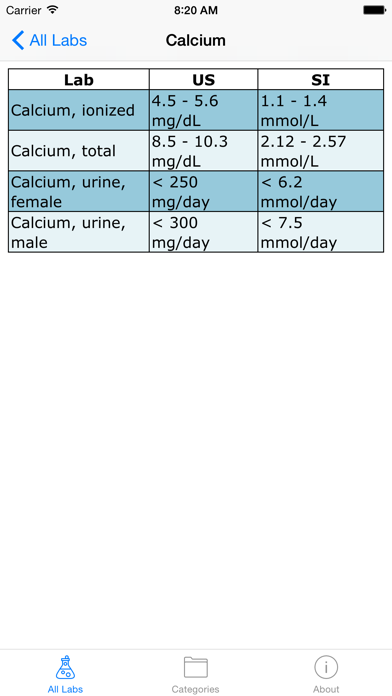 Changes in the concentration of blood proteins are also found on the proteinogram. In the first and second trimester of pregnancy, albumin decreases, which is associated with physiological hypervolemia. In the third trimester, an increase in the alpha-1-globulin fraction (No. 29)*, alpha-fetoprotein (No. 92)*. Alpha-2-globulin fraction (#29)* may increase due to proteins associated with pregnancy (begins to increase from 8-12 weeks of pregnancy and reaches a maximum in the third trimester). Beta globulins (#29)* increase due to an increase in the concentration of transferrin (#50)*. Also, in most cases, there is a slight increase in the level of gamma globulins (#29)*.
Changes in the concentration of blood proteins are also found on the proteinogram. In the first and second trimester of pregnancy, albumin decreases, which is associated with physiological hypervolemia. In the third trimester, an increase in the alpha-1-globulin fraction (No. 29)*, alpha-fetoprotein (No. 92)*. Alpha-2-globulin fraction (#29)* may increase due to proteins associated with pregnancy (begins to increase from 8-12 weeks of pregnancy and reaches a maximum in the third trimester). Beta globulins (#29)* increase due to an increase in the concentration of transferrin (#50)*. Also, in most cases, there is a slight increase in the level of gamma globulins (#29)*.
Minor changes in C-reactive protein (No. 43) *, observed more often in early pregnancy, may be the body's response to proliferation processes (increased cell division). Changes in the volume of circulating blood (CBV) and blood supply to the kidneys lead to changes in the nitrogen excretion function of the kidneys. There is a delay and accumulation of nitrogenous substances, while the amount of urea (No. 26) * decreases, especially in late pregnancy due to increased protein utilization (positive nitrogen balance).
There is a delay and accumulation of nitrogenous substances, while the amount of urea (No. 26) * decreases, especially in late pregnancy due to increased protein utilization (positive nitrogen balance).
Creatinine (No. 22)* decreases to the maximum in the I-II trimester (its concentration can decrease by almost 1.5 times), which is associated with an increase in the volume of the muscle mass of the uterus and fetus. The level of uric acid (#27)* is often reduced due to increased blood supply to the kidneys, but even minor violations of kidney function can lead to an increase in this level, and this is regarded as symptoms of toxemia.
Lipid metabolism changes significantly during pregnancy (profile No. 53)*. Since oxidative processes intensify, there is an increased utilization of cholesterol in the adrenal glands, the placenta. This leads to compensatory transient hypercholesterolemia, characterized by an increase in cholesterol, HDL. The level of HDL practically does not change.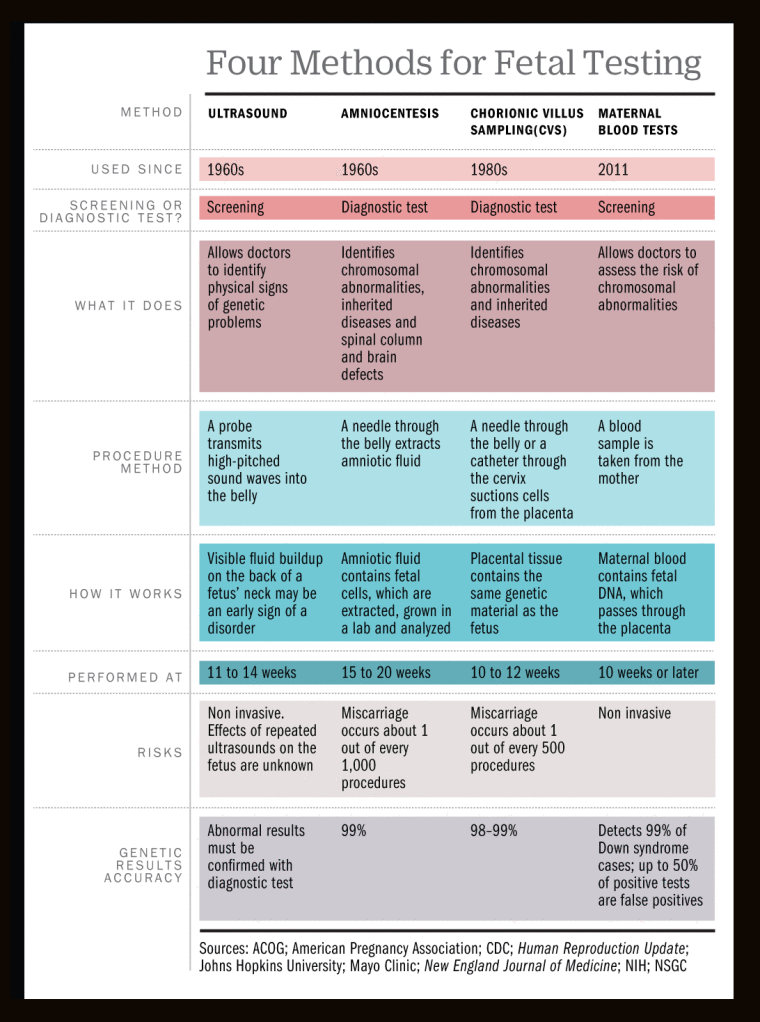 An increase in estrogen levels leads to hypertriglyceridemia, which is facilitated by hypoproteinemia, functional cholestasis. This increases the deposition of fat in the mammary glands, subcutaneous fat, this process is also associated with an increase in the transition of carbohydrates to fats due to an increase in insulin production.
An increase in estrogen levels leads to hypertriglyceridemia, which is facilitated by hypoproteinemia, functional cholestasis. This increases the deposition of fat in the mammary glands, subcutaneous fat, this process is also associated with an increase in the transition of carbohydrates to fats due to an increase in insulin production.
An indicator reflecting the level of endogenous insulin secretion is C-peptide (No. 148)*. Glucose readings (#16)* may vary slightly without reaching levels of hyperglycemia. Since during pregnancy the glomerular filtration rate increases and the permeability of the epithelium of the renal tubules increases, glucosuria (physiological) can be observed periodically. Most often, glucosuria appears at 27 to 36 weeks of gestation. The peculiarities of mineral metabolism in healthy pregnant women in comparison with non-pregnant women is the retention of sodium, potassium, chlorine salts in the body (No. 39)*, phosphorus (No. 41)*, it is the changes in phosphorus in the body of a pregnant woman that are associated with an increase in alkaline phosphatase (No.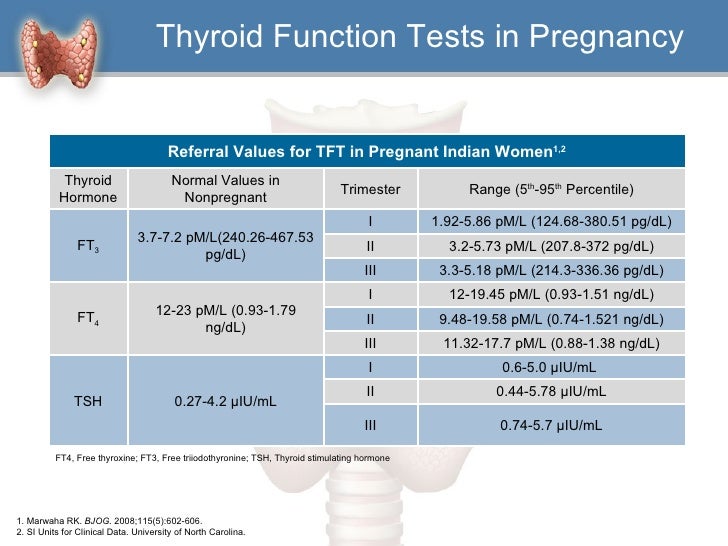 36) *. This is due to changes during pregnancy in the bone tissue and changes in the liver. As you know, during pregnancy, the need for calcium salts increases, which are necessary for the formation of the fetal skeleton, and the mother may experience a calcium deficiency (#37)*. Hypocalcemia in pregnant women can manifest itself in muscle cramps, spastic phenomena. Increasing iron intake during pregnancy can lead to anemia. This condition is characterized by a decrease in iron (No. 48) *, ferritin (No. 51) *, vitamins: B12 (No. 117) *, folic acid (No. 118) *. Changes in the endocrine system
36) *. This is due to changes during pregnancy in the bone tissue and changes in the liver. As you know, during pregnancy, the need for calcium salts increases, which are necessary for the formation of the fetal skeleton, and the mother may experience a calcium deficiency (#37)*. Hypocalcemia in pregnant women can manifest itself in muscle cramps, spastic phenomena. Increasing iron intake during pregnancy can lead to anemia. This condition is characterized by a decrease in iron (No. 48) *, ferritin (No. 51) *, vitamins: B12 (No. 117) *, folic acid (No. 118) *. Changes in the endocrine system
The pituitary gland, especially the anterior lobe, is enlarged. The pituitary hormones ACTH (No. 100)*, prolactin (No. 61)* play an important role in changing the metabolic processes of the pregnant woman's body. Therefore, these hormones can be elevated. The placenta also has hormonal activity. It produces progesterone (No. 63) *, free estriol (No. 134) *, b-hCG (No. 66) *, these hormones are similar in their action to growth hormone (No.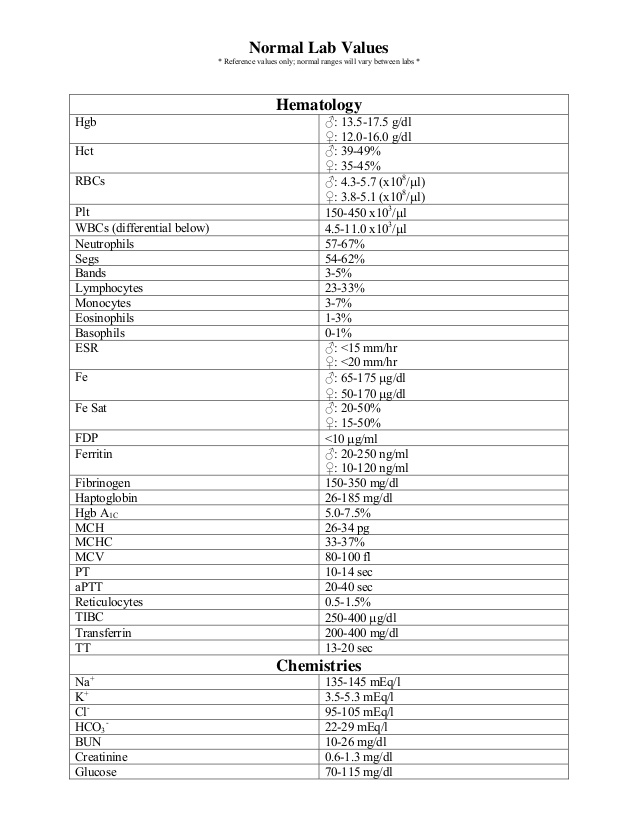 99) *. The thyroid gland also undergoes changes, it increases slightly, and in the first half of pregnancy its hyperfunction is noted. There is an increase in free T4 (No. 55) *, with normal T4 (No. 54) *. There is also an increase in the function of the parathyroid glands by a relative increase in parathyroid hormone (No. 102) *. FSH production (#59)* decreases during pregnancy.
99) *. The thyroid gland also undergoes changes, it increases slightly, and in the first half of pregnancy its hyperfunction is noted. There is an increase in free T4 (No. 55) *, with normal T4 (No. 54) *. There is also an increase in the function of the parathyroid glands by a relative increase in parathyroid hormone (No. 102) *. FSH production (#59)* decreases during pregnancy.
* - Research numbers in the Independent laboratory INVITRO.
In preparing the article, data from the Bulletin of Laboratory Services No. 9, 2001 were used.
Sources:
- Clinical guidelines "Normal pregnancy". Developed by: Russian Society of Obstetricians and Gynecologists. – 2020.
- Clinical guidelines "Multiple pregnancy". Developed by: Russian Society of Obstetricians and Gynecologists. – 2021.
IMPORTANT!
The information in this section should not be used for self-diagnosis or self-treatment.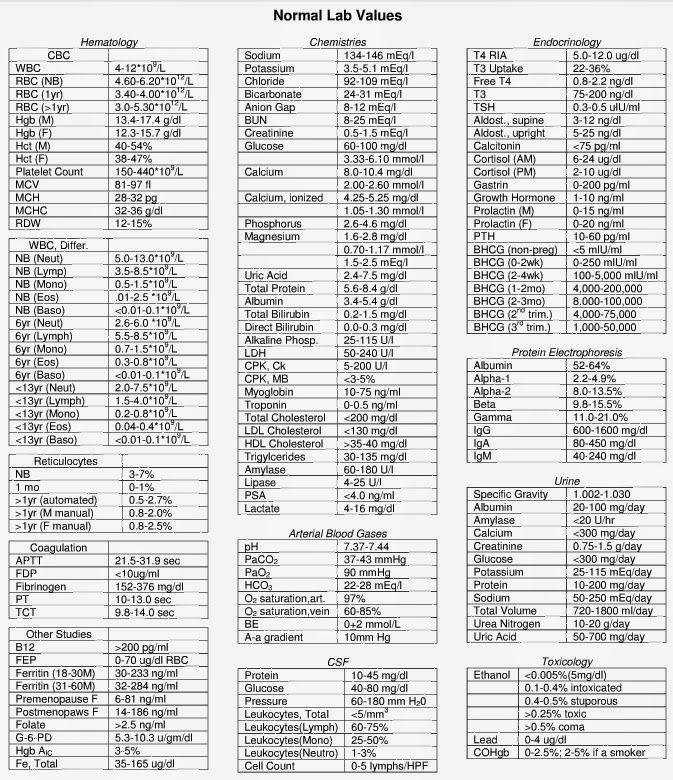 In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
For a correct assessment of the results of your analyzes in dynamics, it is preferable to do studies in the same laboratory, since different laboratories may use different research methods and units of measurement to perform the same analyzes.
Recommendations
-
PSA (prostate specific antigen) test
4917 may 13
-
Human papillomavirus
21128 04 May
-
Alkaline phosphatase
41016 16 April
Show more
ECO
Miscarriage
Pregnancy
hCG, Human Chorionic Gonadotropin
Human Chorionic Gonadotropin (hCG, β-hCG, beta-hCG, Human Chorionic Gonadotropin): indications for prescription, rules for preparing for the test, interpretation of the results and normal indicators.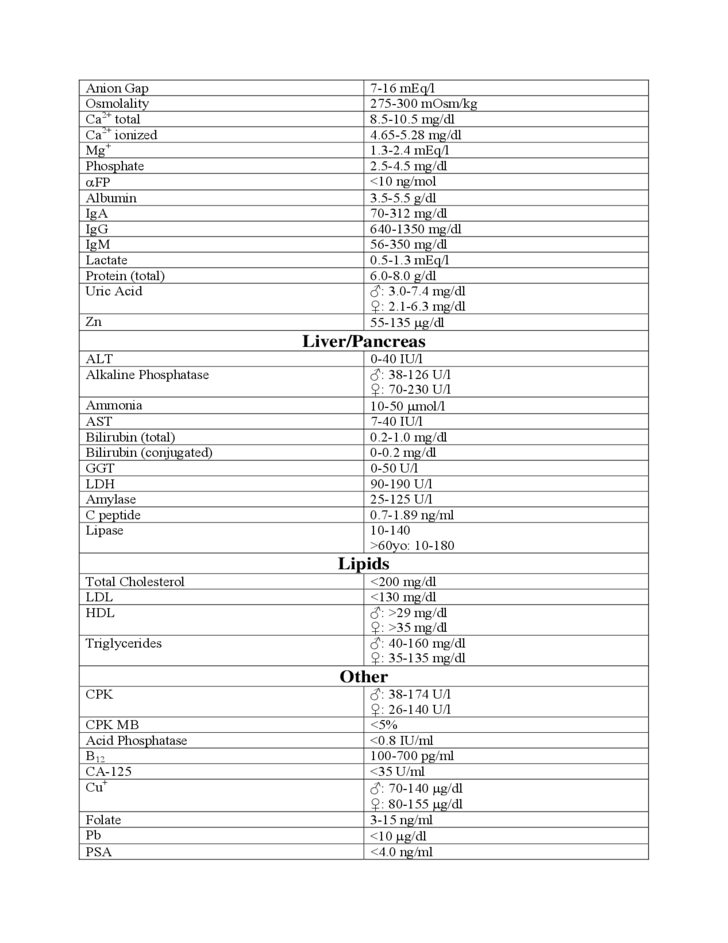
More
Infertility
Varicocele
ECO
Spermogram in INVITRO
Sperm analysis is an integral part of infertility diagnostics and monitoring of diseases of the male genital area. The analysis of the ejaculate includes the determination of the quantitative and qualitative morphological composition of spermatozoa using visual counting in the Goryaev chamber and special staining.
More
ECO
Hypogonadism
Menopause
Climax
Anti-Mullerian hormone (AMH, AMH, anti-Mullerian hormone)
Anti-Müllerian hormone: indications for prescription, rules for preparing for the test, interpretation of the results and norm indicators.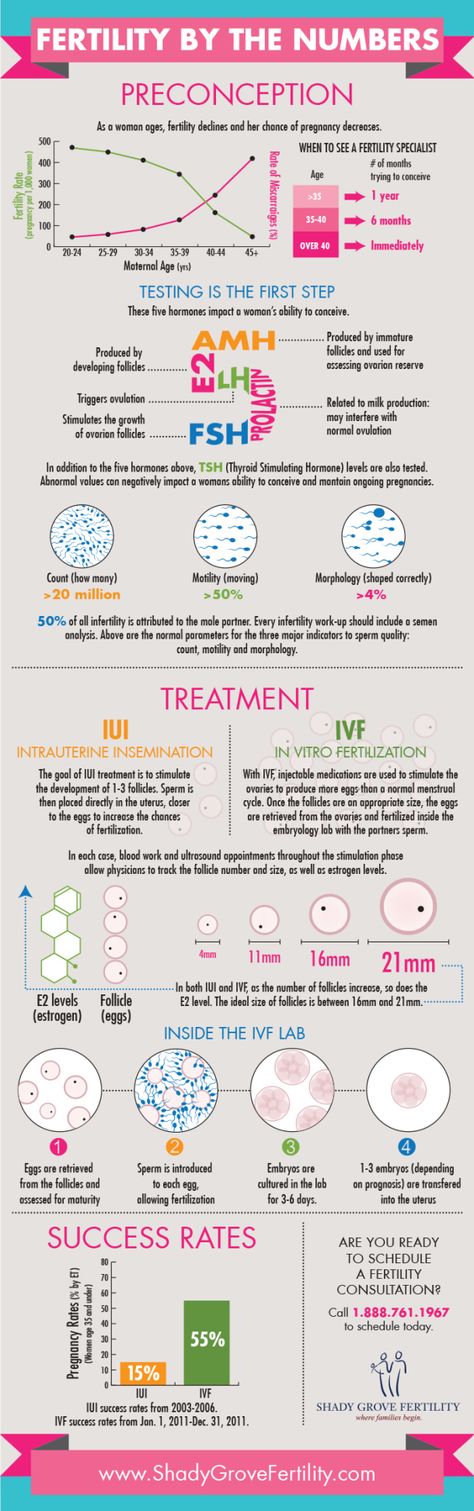
More
ECO
Blood transfusion
Pregnancy
Rh-affiliation (Rh-factor, Rh)
Rh-affiliation: indications for prescription, rules for preparing for the test, interpretation of the results and norm indicators.
More
Heredity
Pregnancy
ECO
Research to determine biological relationship in the family: paternity and motherhood
You can perform molecular genetic studies that reveal a predisposition to various diseases, and now also undergo research to establish biological relationship in the family: paternity and motherhood.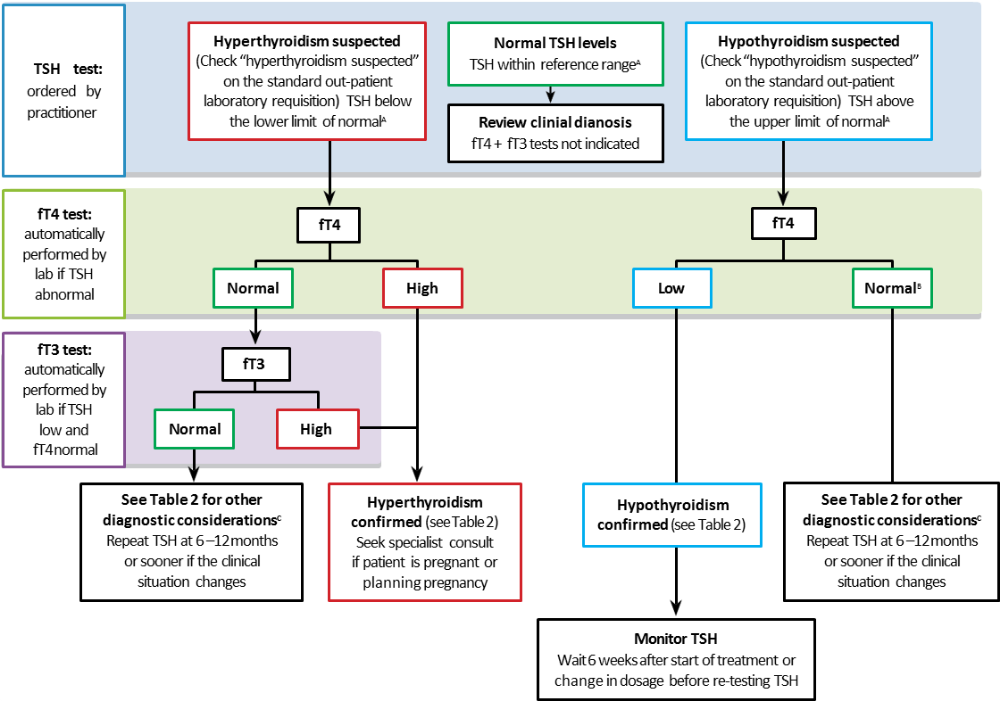
More
Pregnancy: what changes in a woman's body, laboratory features
views: 86685 Published: / Updated:
- Pregnancy
General
Pregnancy is the period of time during which a fetus develops inside a woman's uterus, culminating in the birth of a child.
During pregnancy, there are numerous physiological changes necessary to meet the needs of the growing fetus and the mother's body, which adapts to them. Most of these changes begin shortly after conception and continue into late pregnancy. Physiological adaptation is reflected in changes in the values of laboratory parameters. Some of the changes are well known, for example, a decrease in hematocrit and hemoglobin, creatinine; others, on the contrary, are known to a lesser extent and therefore their observation in the form of the result of the analysis can lead to misinterpretation.
The cardiovascular system
Changes in the work of the cardiovascular system occur among the very first. Their deep restructuring begins already in the early stages of gestation. The main events are physiological vasodilation and fluid retention in the body. Peripheral vasodilation leads to a decrease in vascular resistance and an increase in cardiac output, an increase in heart rate, and an increase in venous pressure.
Blood pressure decreases in the first and second trimesters, but rises to levels in non-pregnant women in the third trimester.
Water balance
Low blood pressure during pregnancy leads to activation of the renin-angiotensin-aldosterone system, resulting in increased secretion of antidiuretic hormone. There is a tendency to retain water and sodium, and the likelihood of edema formation increases.
Hematological changes
Pregnancy is accompanied by stimulation of hematopoietic processes.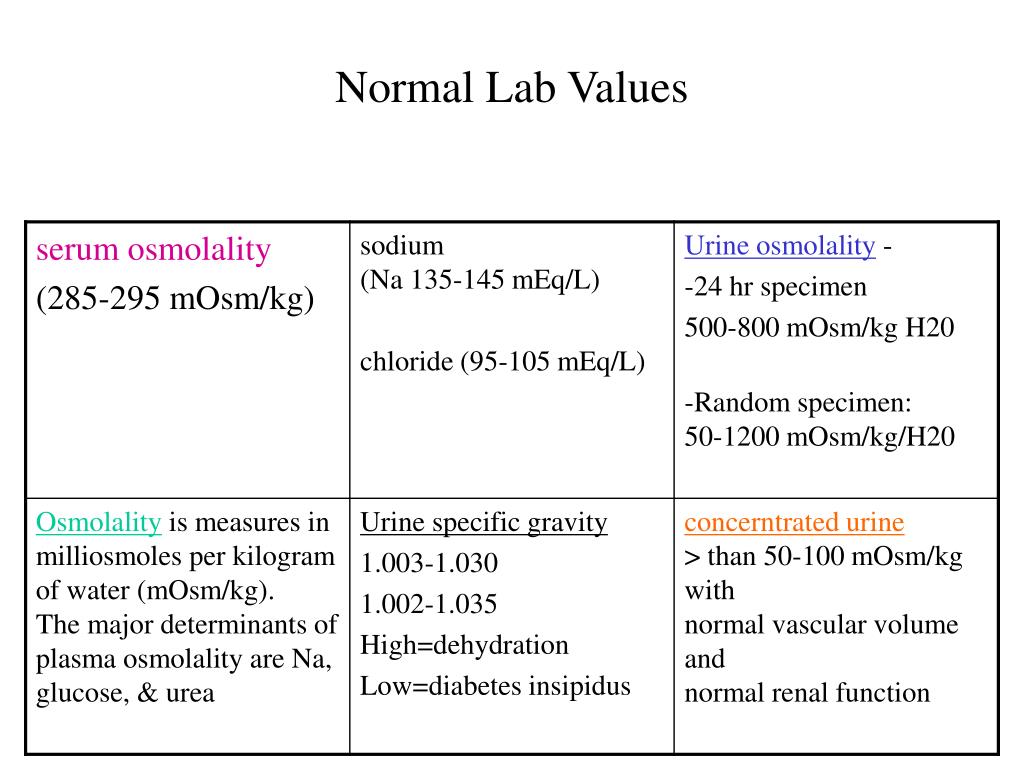 There is a general increase in plasma, the number of erythrocytes (RBC) and the total volume of circulating blood. Plasma volume increases during normal pregnancy. An increase of 15% occurs in the first trimester, in the second trimester this trend continues, reaching a maximum by 32 weeks. By this time, the plasma volume is increased exactly by half.
There is a general increase in plasma, the number of erythrocytes (RBC) and the total volume of circulating blood. Plasma volume increases during normal pregnancy. An increase of 15% occurs in the first trimester, in the second trimester this trend continues, reaching a maximum by 32 weeks. By this time, the plasma volume is increased exactly by half.
The number of red blood cells increases, but occurs more slowly compared to plasma, which makes the blood more dilute and leads to the "physiological anemia" of pregnancy. There is a decrease in hemoglobin and hematocrit and mean hemoglobin content in erythrocytes (MCH). The maximum decrease in hemoglobin values is observed at 32-34 weeks of pregnancy.
During pregnancy, the volume of red blood cells changes. The first 8 weeks of pregnancy, MCV decreases, by 16 weeks it returns to normal values, as in non-pregnant women, and then MCV increases.
The level of leukocytes (WBC) increases by an average of 20%.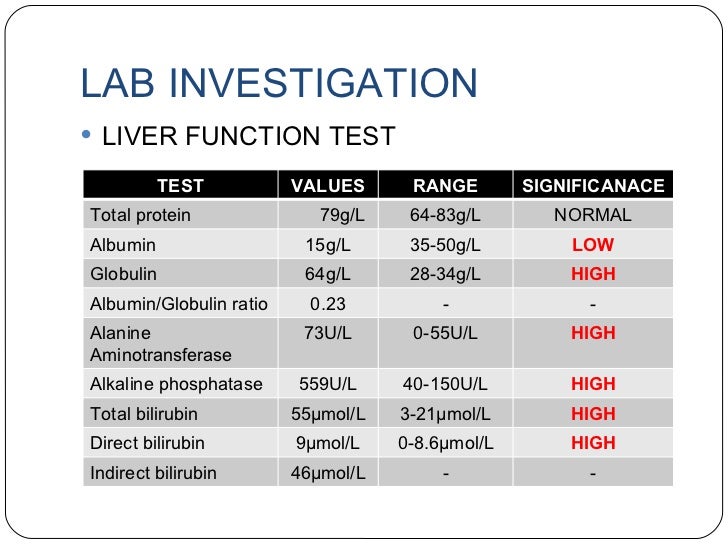 The following changes are noted in the leukocyte formula: the absolute number of neutrophils (stab and segmented) increases, the number of lymphocytes decreases.
The following changes are noted in the leukocyte formula: the absolute number of neutrophils (stab and segmented) increases, the number of lymphocytes decreases.
The number of platelets (PLT) varies ambiguously. Pregnancy is associated with increased platelet turnover.
An increase in blood volume is accompanied by an increase in ESR. In the first trimester, the ESR value is 15 mm/h, in the second - 25 mm/h, in the third - 40 mm/h.
Hemostasis indicators
Throughout the entire period of pregnancy, the body prepares for the upcoming blood loss, so certain changes occur in the hemostasis system.
Changes in the blood coagulation system during pregnancy lead to a physiological state of hypercoagulability, or an increased tendency to clot. In the third trimester, coagulation activity is twice as high as normal. The procoagulant activity of the hemostasis system increases, on the other hand, the activity of the fibrinolysis system decreases..jpg)
The concentration of factors VII, VIII, IX, X, XII and the von Willebrand factor increase.
Factor XI values decrease to 60-70% of those in non-pregnant women.
The level of fibrinogen increases significantly - up to 50%.
Levels of protein S, antithrombin III gradually decrease during pregnancy, the activity of protein C remains unchanged.
Plasma fibrinolytic activity decreases throughout pregnancy, but returns to normal within one hour after delivery.
Thrombin is generated as the gestational age increases. The value of D-dimer increases throughout pregnancy. Only 3–5 days after delivery, the D-dimer value returns to its original values.
Shortening of APTT is observed in the second and third trimester and is associated with an increase in the activity of procoagulants in the blood. In the third trimester, there is a shortening of prothrombin time.
carbohydrate metabolism
Pregnancy is a diabetogenic condition as it is associated with the development of insulin resistance. An increase in the level of estrogen and progesterone in the initial stages leads to hypertrophy of pancreatic cells that secrete insulin. As a result, insulin secretion and tissue sensitivity to it increase in the early stages.
An increase in the level of estrogen and progesterone in the initial stages leads to hypertrophy of pancreatic cells that secrete insulin. As a result, insulin secretion and tissue sensitivity to it increase in the early stages.
In the second trimester, insulin resistance begins to appear, reaching a peak in the third trimester. This is the result of the secretion of contrainsular hormones: human placental lactogen, growth hormone, progesterone, cortisol and prolactin. These hormones cause a decrease in the sensitivity of peripheral tissues to insulin, especially in adipose tissue and skeletal muscle, by interfering with insulin receptor signaling.
Insulin levels during pregnancy increase during fasting, after meals.
Fasting glucose often decreases due to:
- increased storage of tissue glycogen stores;
- increased use of peripheral glucose;
- reduce hepatic glucose production;
- Fetal glucose uptake.
Insulin resistance and relative hypoglycemia lead to an increase in the process of lipolysis - the formation of fats, which mainly allows the use of fat as fuel, saving glucose and amino acids for the fetus. The placenta allows the transfer of glucose, amino acids, and ketones to the fetus, but is impermeable to large lipids. If a woman's endocrine function of the pancreas is impaired and she cannot overcome the insulin resistance associated with pregnancy, then gestational diabetes develops.
During pregnancy, physiological transient glucosuria is often observed, which is associated with an increase in the glomerular filtration rate and an increase in the permeability of the renal tubular epithelium.
Protein metabolism
During the entire period of pregnancy, a woman needs more protein, since the processes of anabolism prevail over the processes of catabolism.
There is a physiological decrease in blood albumin, blood dilution also contributes to a decrease in the proportion of albumin.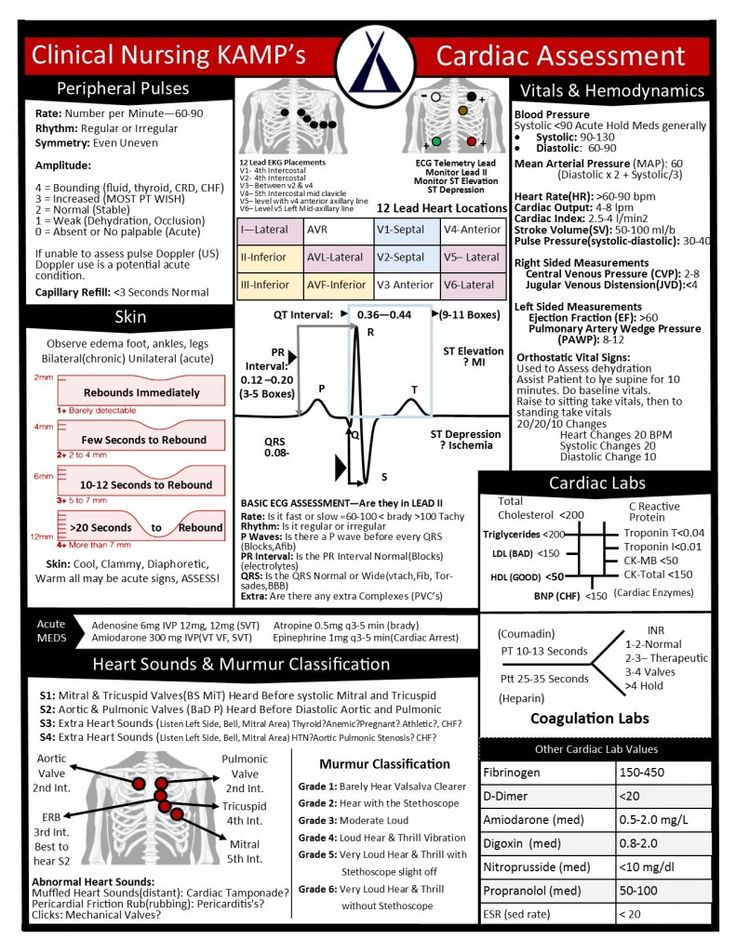
The proteinogram in the I and II trimester has the following features: a decrease in the level of albumin, a slight increase in a-2 and b-1 globulin fraction. In the III trimester, there is a sharp increase in the a-1 globulin fraction.
Due to increased protein metabolism, a positive nitrogen balance is observed. By increasing GFR by 75%, creatinine and urea levels are reduced. The decrease in creatinine occurs mainly in the I and II trimester, when there is an intensive growth of the uterus. The level of urea falls due to increased protein utilization, especially pronounced in the third trimester.
lipid metabolism
The general effects of altered lipid metabolism during pregnancy are the accumulation of fat reserves in the mother's body in the first half and increased fat mobilization in the second half of pregnancy.
Hypercholesterolemia is due to increased production of sex steroid hormones, changes in metabolism in the liver and adipose tissue. Elevated triglycerides provide the mother's need for energy. An increase in LDL cholesterol is associated with an increase in progesterone, in addition, LDL cholesterol is a source of placental progesterone. The increased concentration of estrogen during pregnancy causes an increase in total cholesterol, LDL cholesterol and triglycerides.
Elevated triglycerides provide the mother's need for energy. An increase in LDL cholesterol is associated with an increase in progesterone, in addition, LDL cholesterol is a source of placental progesterone. The increased concentration of estrogen during pregnancy causes an increase in total cholesterol, LDL cholesterol and triglycerides.
Regional deposition of fat in the mammary glands and subcutaneous fat is associated with an increase in the transition of carbohydrates into fats under the action of insulin.
Mineral exchange
Pregnancy causes an increase in the need for iron by 2-3 times for the synthesis of hemoglobin, for the production of certain enzymes. The need for folic acid increases 10-20 times, the need for vitamin B 12 - twice.
The third trimester marks the peak demand for calcium.
During pregnancy, the concentration of total calcium in the blood serum decreases due to a decrease in the proportion of blood albumin, but the level of ionized calcium remains unchanged.