Overproduce breast milk
Too much breast milk? How to reduce oversupply
Sometimes you may feel like you’re producing too much breast milk, especially in the first few weeks of breastfeeding. Read on to find out if you really have an oversupply of milk, and what you can do about it
Share this content
Breast milk is amazing, so having lots is a good thing, right? Well, not always... Some babies struggle with the fast flow that usually accompanies an overabundant milk supply. And mums with oversupply can often feel very uncomfortable, with frequently or constantly leaking breasts, and may be more likely to suffer from recurrent mastitis.
Fortunately, there are a number of strategies that can help. But before you try any of these, ask yourself two key questions:
Do I really have too much breast milk?
Some symptoms of oversupply (outlined below) may have a number of other possible causes. It’s unwise to try to decrease your milk supply until you’re sure that oversupply is the underlying problem. Otherwise you could end up with less breast milk than your baby needs, particularly in the crucial first month when you’re trying to establish your supply.
Is oversupply a problem for me or my baby?
If you’re sure you have an oversupply of breast milk, but you and your baby are happy, there’s no need to do anything. Most cases settle down after the first few months. And as your baby grows, he’ll get better at dealing with a fast flow, and may come to enjoy it!
Leaking doesn’t always mean too much breast milk
During the first four to six weeks after your baby is born, your levels of the milk-making hormone prolactin will be increasing each time milk is removed from your breasts. In these early weeks, your breasts are learning how much breast milk your baby needs and how much to make every hour. As a result, excessive leaking and breasts that fill quickly – and even spray milk during let down – are common and normal. 1
1
At the same time, your newborn is also learning to coordinate the way he sucks and swallows, so some coughing and spluttering at the breast is also to be expected.
After around four to six weeks, surges in your prolactin will gradually decrease, and your milk production should start to follow a more straightforward ‘supply and demand’ process based on your baby’s needs.2 But with so many hormonal changes happening in your body as a new mum, it’s not surprising that it can take time to adjust. Some mums find that their milk supply settles down quickly, while for others it may take a little longer.
Signs of breast milk oversupply in your baby
Overabundant milk supply seems to go hand-in-hand with a fast flow, especially during the first let down. Your baby may respond by coughing and spluttering near the start of a feed, clamping or biting down, or holding the breast very loosely in his mouth. He may come off the breast because the fast flow is a bit of a shock to him, and then cry because his feed has been interrupted. He’ll probably take in large volumes of milk, along with lots of air, and might spit up a lot and need frequent burping as a result. Be as gentle as possible if you’re burping him – jerky movements combined with a quickly filled belly can cause vomiting and upset some babies.
He’ll probably take in large volumes of milk, along with lots of air, and might spit up a lot and need frequent burping as a result. Be as gentle as possible if you’re burping him – jerky movements combined with a quickly filled belly can cause vomiting and upset some babies.
At the start of a breastfeed, the milk your baby is getting is relatively low in fat and consists mostly of lactose (sugar) and protein. As the feed progresses and your breast empties, the fat content of your milk steadily increases. In cases of oversupply, your baby may become full before he has completely drained your breast. This means that he is getting plenty of lactose-rich breast milk, but not as much of the high-fat milk that comes towards the end of a feed. Too much lactose, instead of a balanced meal, can be hard for babies to digest, resulting in explosive, frothy, green poos.
Paradoxically, in this situation your baby may want to feed constantly and be fussy in between feeds – although he’s taking in lots of calories, the low fat content of the milk means he never feels fully satisfied. This is because it’s the fat in food that makes us feel full. Think of the difference between eating dozens of rice crackers, and eating some cheese and biscuits – the cheese will make you feel more satisfied as it’s higher in fat.
This is because it’s the fat in food that makes us feel full. Think of the difference between eating dozens of rice crackers, and eating some cheese and biscuits – the cheese will make you feel more satisfied as it’s higher in fat.
However, all of the above symptoms can be caused by other things, such as reflux, allergies or even, conversely, a low milk supply. Only if they are combined with excessive weight gain is breast milk oversupply likely to be the cause. Babies are expected to gain around 900 g (2 lb) per month, but in cases of oversupply, they will put on much more – often around double that.1 If your baby appears to have symptoms of oversupply but is gaining an average amount of weight, see a lactation consultant or breastfeeding specialist for advice.
Oversupply symptoms you may experience
Mums with too much breast milk often experience uncomfortable feelings of engorgement and tension and constantly feel overfull.3 As we have seen, leaking breast milk is normal in the first six weeks or so, and not usually a sign of oversupply. But if you’re still getting soaked every time your baby feeds after this period, it may be an issue.
But if you’re still getting soaked every time your baby feeds after this period, it may be an issue.
Because a baby can’t always drain a very full breast, it’s also common to experience blocked ducts or repeated bouts of mastitis as a result of oversupply. However, these problems may also have other causes.
How to decrease milk supply
If you’ve established that you have too much breast milk and it’s a problem, here are a few simple measures that may help. For some mums these are sufficient:
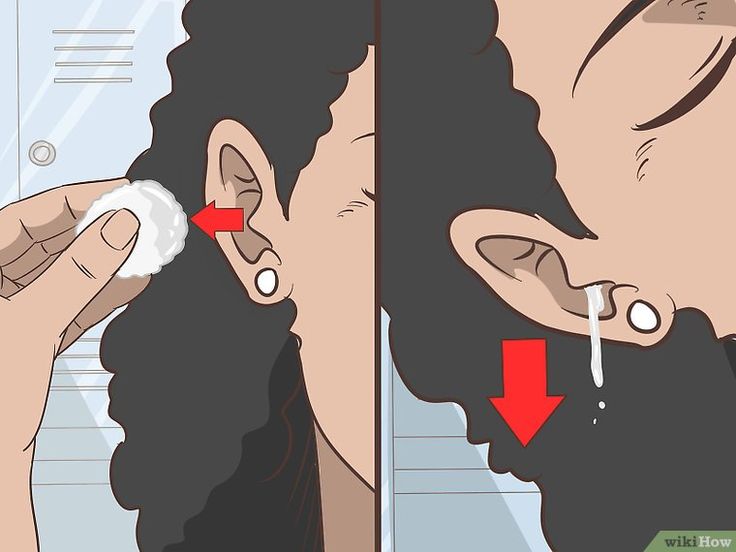
- Try laid-back breastfeeding. Feeding in a reclined position, or lying down, can be helpful because it gives your baby more control. He can set the pace and lift his head for a break if your flow is too fast for him. Remember to place a towel underneath you to catch any excess milk!
- Relieve pressure. If your breasts are very uncomfortable you can hand express or pump a little milk to relieve them – but try to express the smallest amount possible.
 Each time you remove milk, you’re sending your breasts a message to produce more. So, while expressing can bring temporary relief, in the long run it could make the problem worse. If you need to express and store milk for times when you’re apart from your baby, it’s best to wait until you’ve addressed your oversupply.
Each time you remove milk, you’re sending your breasts a message to produce more. So, while expressing can bring temporary relief, in the long run it could make the problem worse. If you need to express and store milk for times when you’re apart from your baby, it’s best to wait until you’ve addressed your oversupply. - Try nursing pads. If you're leaking milk, popping disposable nursing pads super or milk collection shells inside your bra could help you stay dry. If your leakage is only light to moderate or you have leaking breasts during pregnancy, Ultra thin disposable nursing pads will help you feel confident in a discreet way.
- Avoid lactation teas and supplements. If you’ve been drinking mother’s milk teas, eating lactation cookies or taking herbal supplements to encourage breast milk production in the early days, make sure you stop – these could now be part of the problem.
Block feeding to reduce milk supply
If you’ve tried the above and you or your baby are still having problems, a technique called block feeding could get your supply to a more manageable level. But get advice from a lactation consultant or breastfeeding specialist before trying this method.
But get advice from a lactation consultant or breastfeeding specialist before trying this method.
With block feeding, you breastfeed your baby whenever he wants for a period of four hours, but from one breast only. Your other breast will become very full of milk. As your breast milk contains something called ‘feedback inhibitor of lactation’ (FIL), the excessive fullness signals that breast to slow down milk production. It’s your body’s way of ensuring that your breasts don’t fill up endlessly.
Try this technique for 24 hours, alternating breasts every four hours. If there’s no improvement, you can increase the length of the blocks to six hours.
Full drainage and block feeding technique
If there’s still no improvement after another 24 hours, there’s another version of this technique that can be suitable for mums with more extreme oversupply, called ‘full drainage and block feeding’.3
With this method, you use an electric breast pump to fully drain your breasts at the start of the day, then feed your baby immediately afterwards. The flow will be slower, which means your baby should be able to cope better. He’ll also get more of the higher-fat milk that comes at the end of a feed, so will feel more satisfied.
The flow will be slower, which means your baby should be able to cope better. He’ll also get more of the higher-fat milk that comes at the end of a feed, so will feel more satisfied.
You can then begin block feeding for four hours at a time, as above. If this isn’t effective, switch to blocks of six, eight or 12 hours the next day, depending on how severe the oversupply problem is. Talk to a healthcare professional before attempting this technique.
You may not need to fully drain your breasts again after the first instance, but some mums need to do it once or twice more. Some mums notice an improvement within one or two days, or a little longer, but block feeding should not be continued for more than five days.
References
1 Morbacher N. Breastfeeding answers made simple. Amarillo TX, USA: Hale Publishing; 2010.
2 Cox DB et al. Blood and milk prolactin and the rate of milk synthesis in women. Exp Physiol. 1996;81(6):1007-1020.
3 van Veldhuizen-Staas CG. Overabundant milk supply: an alternative way to intervene by full drainage and block feeding. Int Breastfeed J. 2007;2(1):11.
Overabundant milk supply: an alternative way to intervene by full drainage and block feeding. Int Breastfeed J. 2007;2(1):11.
Oversupply of breastmilk | Pregnancy Birth and Baby
beginning of content4-minute read
Listen
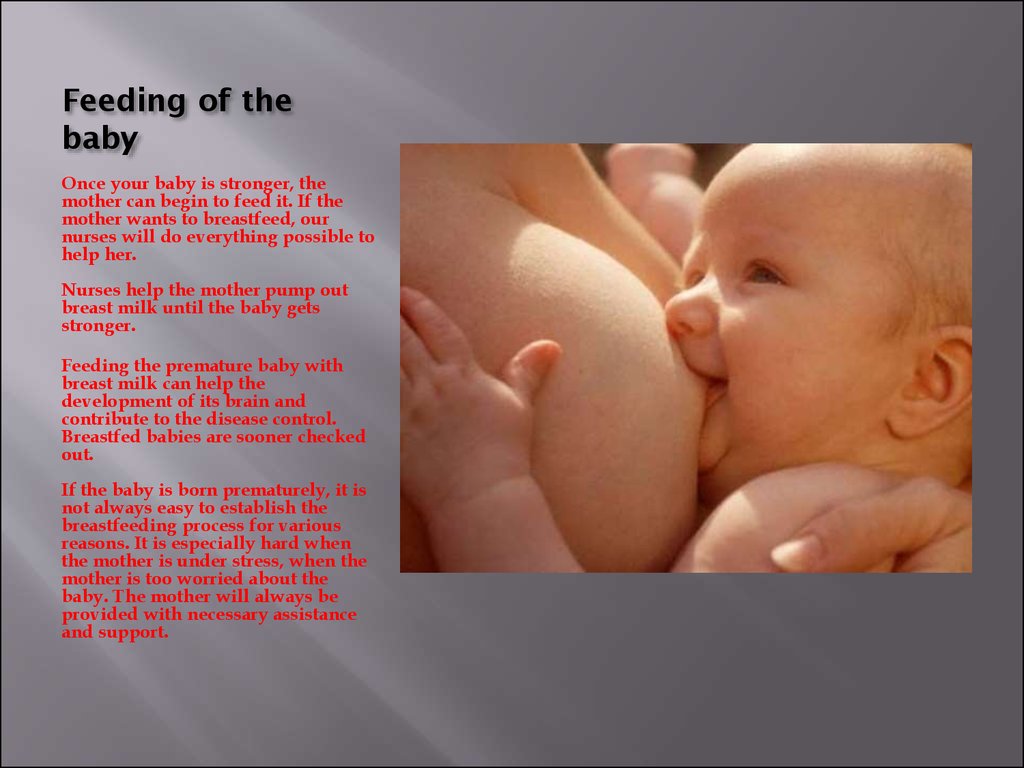
A mother’s milk supply usually adjusts to her baby’s needs after about 4 weeks of breastfeeding. Some mothers continue to make more milk than the baby requires, and this is known as ‘oversupply’.
Oversupply can make breastfeeding difficult for both mother and baby.
What are the causes of oversupply?
Breastmilk oversupply that continues after the first 4 weeks or so can have many causes. Feeding patterns may cause the oversupply, such as:
- feeding the baby on a set schedule rather than according to need
- pumping too much before a feed to make the breast soft and easier for the baby to latch onto
- the baby preferring to feed mainly from 1 breast
Other causes of oversupply include:
- an excess of the milk production-stimulating hormone prolactin in your blood (hyperprolactinemia)
- a congenital predisposition
How breastmilk oversupply affects your baby
Your baby may be unsettled or distressed during and after feeding, and it can be hard to know whether they are still hungry or are getting too much milk too fast.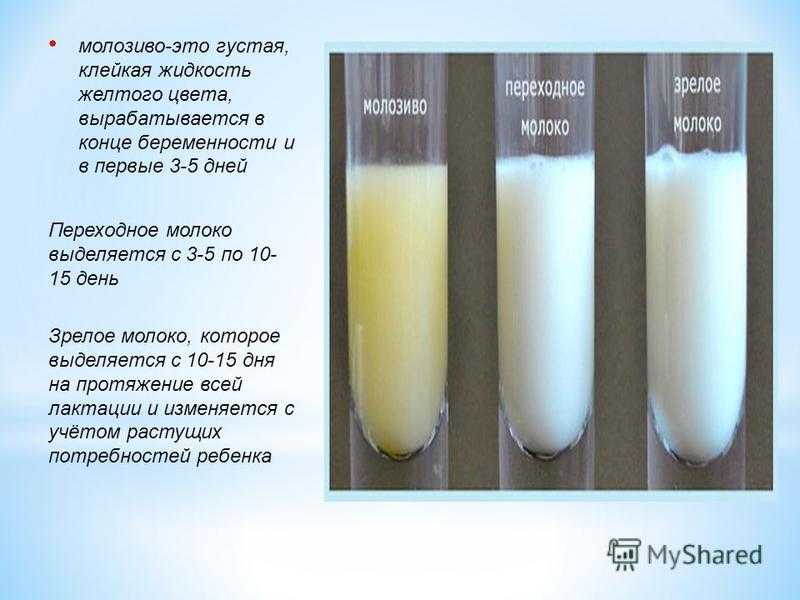 Your baby may:
Your baby may:
- choke and splutter at the breast due to the high rate of milk flow
- have trouble latching onto the breast
- feed for only short periods of time leading to ‘lactose overload’
- have a lot of urine (more than 10 wees a day) or diarrhoea with green, frothy poos and nappy rash
- have excessive wind, causing unsettled, colicky behaviour
- bring up a lot of milk after breastfeeding
- put on weight quickly
How breastmilk oversupply affects you
Oversupply can also cause problems for you.
You might feel your breasts refill very quickly after feeding your baby. They might feel lumpy and tight after breastfeeding. You might also leak more than usual or have an explosive milk-ejection reflex, which makes it difficult to feed in public, and can cause difficulties for your baby at the beginning of feeding.
You could develop blocked milk ducts or mastitis and breast abscesses.
Oversupply can make breastfeeding a less pleasurable experience for you or your baby. Some mothers think about early weaning if oversupply is not diagnosed and managed well.
Some mothers think about early weaning if oversupply is not diagnosed and managed well.
How is breastmilk oversupply diagnosed?
It is essential to have a health professional such as a lactation consultant, breastfeeding counsellor, doctor or child health nurse watch your baby breastfeed to diagnose true oversupply. It can easily be confused with breast engorgement or a fast ‘let-down’ reflex.
For help with the diagnosis and treatment of oversupply, contact a health professional, such as a lactation consultant, breastfeeding counsellor, or child health nurse, or call Pregnancy Birth and Baby on 1800 882 436.
How is breastmilk oversupply treated?
The aim of treatment is to reduce your milk production. This is best done while you are being supported by a lactation consultant, breastfeeding counsellor, or child health nurse.
‘Block feeding’ is a method that can help reduce milk supply in just a few days:
- Choose a time frame, usually from 3 to 4 hours, and feed your baby from only 1 breast during that time.

- Then change to the other breast for the same time period.
- Continue this pattern for a few days.
- You might need to hand express a small amount from the unused breast to relieve pressure or discomfort, but don’t empty it — the residual milk in the unused breast triggers the reduction in milk production.
Block feeding ensures that 1 breast always contains residual milk. This will trigger both breasts to reduce milk production, and should gradually resolve oversupply of milk. How long it takes depends on your situation.
Block feeding will also help to reduce the amount of thinner foremilk consumed by your baby. As your baby gets to drink more of the creamy hindmilk, you’ll see your baby’s stools get thicker. This tells you that you are on the way.
If your milk supply does not respond to block feeding, talk to your doctor.
The Australian Breastfeeding Association website has more tips about managing oversupply.
Sources:
Australian Breastfeeding Association (Too much milk), Australian Breastfeeding Association (Lactose overload in babies), Raising Children Network (Oversupply of breastmilk and engorgement), King Edward Memorial Hospital Obstetrics & Gynaecology (Clinical Practice Guideline: Breastfeeding challenges: oversupply/hyperlactation), Breastfeeding USA (Oversupply: Symptoms, causes, and what to do if you have too much milk))Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: January 2021
Back To Top
Related pages
- Breastfeeding your baby
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Transitional milk | Stages of breast milk production
During the first couple of weeks after birth, the composition of breast milk changes dramatically. Learn about the amazing properties of this transitional milk.
Share this information
A newborn changes literally every day, and the same can be said about breast milk. With the advent of milk, the breast can increase to an impressive size, and changes occur not only on the outside, but also inside. During the first week, the milk-producing cells and the connections between them are rebuilt and prepare the breast for the upcoming feeding. 1 From now until about the end of the second week, they will produce what is called transitional milk. 2
1 From now until about the end of the second week, they will produce what is called transitional milk. 2
“After the placenta is delivered, levels of progesterone, the pregnancy hormone, begin to decline rapidly,” explains Professor Peter Hartmann of the University of Western Australia, a leading authority on the composition of breast milk. “As progesterone levels decrease, milk synthesis increases and the composition is approaching the norm, although a couple more weeks are needed for the full maturation of the milk.
Stages of breast milk production: intermediate phase
If colostrum is the very first food of the baby, and mature milk is his main food for a long time, then transitional milk is a kind of bridge between them.
They should be considered as three different stages of milk production, not three types of milk. The main components remain unchanged throughout breastfeeding, only their quantity changes depending on the circumstances. During the transition period, the composition of milk undergoes the most significant changes, and this happens every day in accordance with the changing needs of the child.
During the transition period, the composition of milk undergoes the most significant changes, and this happens every day in accordance with the changing needs of the child.
Milk changes because it contains bioactive components, including cells, hormones and beneficial bacteria. The transition to mature milk does not happen all at once: the composition changes gradually and in strict accordance with the developmental needs of the baby. 3.4
“The amount of milk produced by the mother is the main influence on the composition of milk,” says Professor Hartman. “The composition of milk at low and higher levels of production is different.”
Transitional milk: increase
As the child grows, it needs more food and a different ratio of nutrients. The amount of milk produced during this period also increases significantly. You can produce 600-700 ml per day, 5 which is a very impressive amount compared to the small amount of colostrum that was produced in the early days.
"The composition of milk in all mammals varies according to the needs of the young"
Your breasts are now in "boost" mode: your body is learning to produce the amount of milk your baby needs. The breast becomes more mature, as does the milk. Compared to colostrum, transitional milk contains more fat and lactose, a natural sugar that gives your baby energy. 2
“The level of lactose rises sharply in the first two or three days after birth,” says Prof. Hartmann, “Fat composition also changes: the content of medium-chain fatty acids C10 and C12 increases. They are an easily digestible source of energy and have antiviral properties. In addition, sodium and chloride levels are greatly reduced during this period, so that the milk has a very low salt content.”
Proteins: correct ratio
The protein content of breast milk also does not remain unchanged. There are two types of proteins in human milk: casein and whey. Under the influence of acid in the child's stomach, casein turns into a solid mass (cottage cheese) and gives a feeling of satiety for a longer time. It also has antimicrobial properties. Whey, on the other hand, is rich in antibodies and remains liquid, so it is easily absorbed, which is especially important for newborns. As the child's gastrointestinal tract strengthens, the ratio of casein to whey in milk gradually changes. If in colostrum it is about 90:10, then after a month it reaches 60:40, and after a year of breastfeeding, the balance is set at 50:50. 6
Under the influence of acid in the child's stomach, casein turns into a solid mass (cottage cheese) and gives a feeling of satiety for a longer time. It also has antimicrobial properties. Whey, on the other hand, is rich in antibodies and remains liquid, so it is easily absorbed, which is especially important for newborns. As the child's gastrointestinal tract strengthens, the ratio of casein to whey in milk gradually changes. If in colostrum it is about 90:10, then after a month it reaches 60:40, and after a year of breastfeeding, the balance is set at 50:50. 6
This ratio of proteins is ideal for humans, as our body grows relatively slowly and the brain is constantly growing and becoming more complex. In addition, it promotes the supply of all the essential amino acids that a child needs for the healthy development of the brain, eyes and other organs.
The amount of whey protein in human milk is significantly higher than that of other mammals. In cow's milk, the ratio of whey and casein is the opposite: 20:80 (therefore, it is not suitable for feeding children under one year old).![]() 7
7
“Milk is designed to perform a specific task,” continues Professor Hartmann, “Some components are present in all milk, such as proteins and fats, but if you look at which proteins and which fats, it becomes clear which animal belongs to milk. The composition of milk in all mammals varies depending on the needs of the young.
Changing the protective properties of transitional milk
Although your baby is still very young, already in the first couple of weeks he begins to develop his own immune system, and now he needs your direct protection a little less.
The concentration of protective enzymes and antibodies in breast milk changes accordingly. The content of some substances, in particular lactoferrin (protective enzyme) and secretory immunoglobulin A (antibody), decreases, while other substances, such as the antibacterial enzyme lysozyme, on the contrary, increase. 8
“The protein content of milk decreases around the same time,” says Prof. Hartmann, “The synthesis of protective proteins occurs at the same rate, but they are more diluted due to increased milk production.”
Hartmann, “The synthesis of protective proteins occurs at the same rate, but they are more diluted due to increased milk production.”
The concentration of minerals such as zinc, copper and magnesium, which support the development of the child's immune system, also decreases as the immune system strengthens. 9
When breast milk is fully mature
During the transition period, the composition of breast milk changes significantly. By the end of the first month, it becomes fully mature. This means that the child will be able to eat them further as they grow. The composition of milk will no longer change much, no matter how long you continue breastfeeding - a few months, a year or more.
Would you like to know more? Read our free e-book Surprising Facts About Breast Milk or an article about mature milk.
Literature
1 Pang WW, Hartmann PE. Initiation of human lactation: secretory differentiation and secretory activation. 2 Ballard O, Morrow AL. Human milk composition: nutrients and bioactive factors. Pediatr Clin North Am . 2013;60(1):49-74. - Ballard O., Morrow A.L., "Composition of breast milk: nutrients and biologically active factors." Pediatrician Clean North Am. 2013;60(1):49-74. 3 Munblit D et al. Colostrum and mature human milk of women from London, Moscow, and Verona: determinants of immune composition. Nutrients. 2016; 8(11): 695. - Moonblit, D. et al., "Colostrum and mature breast milk from women in London, Moscow, and Verona: major factors in immune composition. 4 Pons SM et al. Triacylglycerol composition in colostrum, transitional and mature human milk. Eur J Clin Nutr . 2000;54(12):878-882. — Pons SM, "Triacylglycerol in colostrum, transitional and mature human milk". Yur J Klin Nutr. 2000;54(12):878-882. 5 Neville MC et al. Studies in human lactation: milk volumes in lactating women during the onset of lactation and full lactation. Am J Clin Nutr . 1988;48(6):1375-1386. - Neville M.S. et al., "Female Lactation Study: Milk Quantity in Lactating Women at the Beginning and Peak of Lactation." Am F Clean Nutr. 1988;48(6):1375-1386. 6 Kunz C, Lönnerdal B. Re-evaluation of the whey protein/casein ratio of human milk. 7 Martin CR et al. Review of infant feeding: key features of breast milk and infant formula. Nutrients. 2016;8(5). - Martin S.R. et al., Review of Infant Feeding Issues: Key Features of Breast Milk and Infant Formula. Nutrients. 2016;8(5). 8 Lönnerdal B et al. Longitudinal evolution of true protein, amino acids and bioactive proteins in breast milk: a developmental perspective. J Nutr Biochem. 2017;41:1-11. - Lönnerdahl B. et al., "Longitudinal evolution of true proteins, amino acids and biologically active proteins of human milk: a development perspective." G Nutr Biochem. 9Casey C. E. et al. Studies in human lactation: zinc, copper, manganese and chromium in human milk in the first month of lactation. Am J Clin Nutr 1985;41(6):1193-1200. - Casey S.I. et al., Female Lactation Study: Zinc, Copper, Magnesium, and Chromium in Breast Milk in the Early Months of Lactation. Am J Clean Nutr. 1985;41(6):1193-1200.  J Mammary Gland Biol Neoplasia. 2007;12(4):211-221. - Pang, W.W., Hartmann, P.I., "Lactation initiation in the lactating mother: secretory differentiation and secretory activation." F Mammary Gland Biol Neoplasia. 2007;12(4):211-221.
J Mammary Gland Biol Neoplasia. 2007;12(4):211-221. - Pang, W.W., Hartmann, P.I., "Lactation initiation in the lactating mother: secretory differentiation and secretory activation." F Mammary Gland Biol Neoplasia. 2007;12(4):211-221. 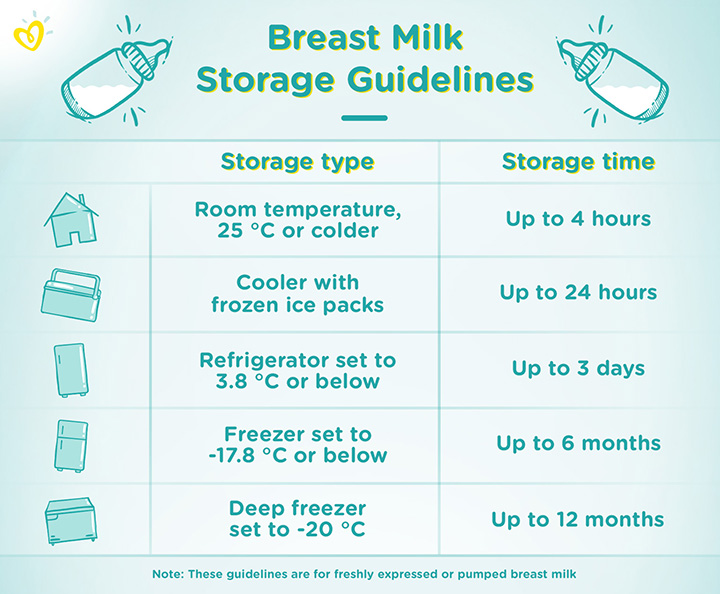 " Nutrients. 2016; 8(11): 695.
" Nutrients. 2016; 8(11): 695.  Acta Paediatr. 1992;81(2):107-112. Kuntz S, Lonnerdal W. Act Pediatr.1992;81(2):107-112. - Kuntz S., Lönnerdahl B., "New Evaluation of Whey Protein/Casein in Breast Milk". Akta Pediatr. 1992;81(2):107-112.
Acta Paediatr. 1992;81(2):107-112. Kuntz S, Lonnerdal W. Act Pediatr.1992;81(2):107-112. - Kuntz S., Lönnerdahl B., "New Evaluation of Whey Protein/Casein in Breast Milk". Akta Pediatr. 1992;81(2):107-112.  2017;41:1-11.
2017;41:1-11.
Dairy plant
“I don’t have enough milk,” says the young mother, and with a calm soul transfers the baby to artificial feeding. But to increase lactation, neither special natural data nor extraordinary efforts are required ...
Milk rivers
The only product that is ideal for a baby is breast milk. The most perfect milk formula cannot replace it 100%. Experts counted more than 500 components useful for the baby in the composition of milk. Synthesizing everything artificially, of course, will not succeed.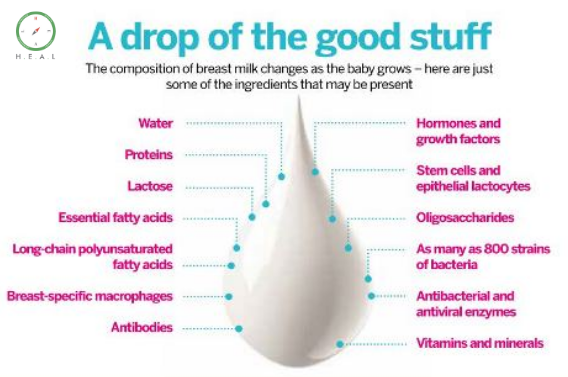 Fortunately, almost every mother can breastfeed. In only 3-5% of women, the body is physiologically unable to produce milk in the amount that the child needs. These are mothers who have serious problems with the hormonal system. Breastfeeding is not always safe for women with heart disease or cancer. In all other cases, the lack of milk is explained only by ignorance or non-compliance with the rules of lactation.
Fortunately, almost every mother can breastfeed. In only 3-5% of women, the body is physiologically unable to produce milk in the amount that the child needs. These are mothers who have serious problems with the hormonal system. Breastfeeding is not always safe for women with heart disease or cancer. In all other cases, the lack of milk is explained only by ignorance or non-compliance with the rules of lactation.
Milk is in the head
Milk production is a hormone-dependent process. When a baby takes a nipple into her mouth, a nerve-reflex impulse is sent to the hypothalamus of the mother's brain, which causes the production of the hormones prolactin and oxytocin. The main one - prolactin - stimulates the formation of milk in the alveoli. And oxytocin "compresses" the corresponding muscle cells of the alveoli, pushing milk into the excretory ducts.
In response to breastfeeding, prolactin is produced in the pituitary gland several times more. Thanks to this, a new supply of breast milk is prepared already during feeding, and 2 hours after it, about 70-75% of the sucked baby is restored for the next meal.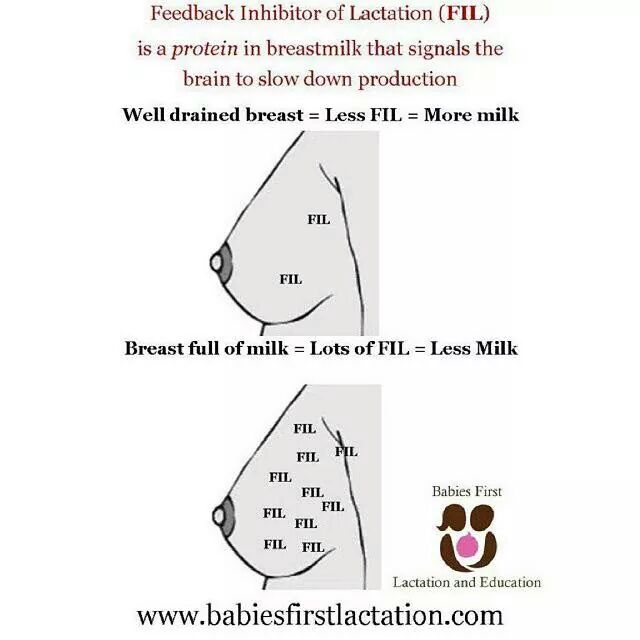 Therefore, the more often the baby snacks, the more milk is produced. However, nature will not allow the development of a “crisis of overproduction”. The volume of milk produced by each gland is strictly regulated by the intensity of its use. No need, no production.
Therefore, the more often the baby snacks, the more milk is produced. However, nature will not allow the development of a “crisis of overproduction”. The volume of milk produced by each gland is strictly regulated by the intensity of its use. No need, no production.
How to increase lactation
Do not give formula in the first days of life
Milk comes on the 3rd-5th day after birth. No need to be nervous and bottle feed your newborn. A woman who has given birth produces colostrum - a very concentrated liquid that contains all the nutrients the baby needs. The volume of colostrum is small, but it will be enough for the baby - the tiny stomach does not need more.
Breastfeed as needed
Do not wait between feedings. Demand creates supply.
If a hungry child begins to turn his head, open his mouth, you need to give him a breast. You should not “replace” the nipple with a dummy or a bottle of water: up to 6 months, the baby can do without “additional drinking” - breast milk completely fills the need for liquid. And sucking on a pacifier will calm the baby, but will not give the mother's body a signal to produce a new portion of milk.
And sucking on a pacifier will calm the baby, but will not give the mother's body a signal to produce a new portion of milk.
Do not shorten feeding time
There is an opinion that the child should be near the mother's breast for no more than 10-15 minutes.
But the baby does not owe anything to anyone. A newborn can be applied to the breast 12-15 times a day, each time for half an hour or even an hour. This is useful and mutually beneficial: after giving birth, mom needs to recover. And "feeding non-stop" gives her the opportunity to sit quietly or lie down with the baby. You should not be afraid to "fall out of life". The period of "constant feeding" lasts only the first 1.5-2 months. A grown-up baby will no longer want to suckle for hours - he has too many other things to do.
Pay attention to the child
Ideally, when the child is with his mother all the time. He is used to being cramped and warm in the womb, and after birth he expects to meet exactly the same conditions.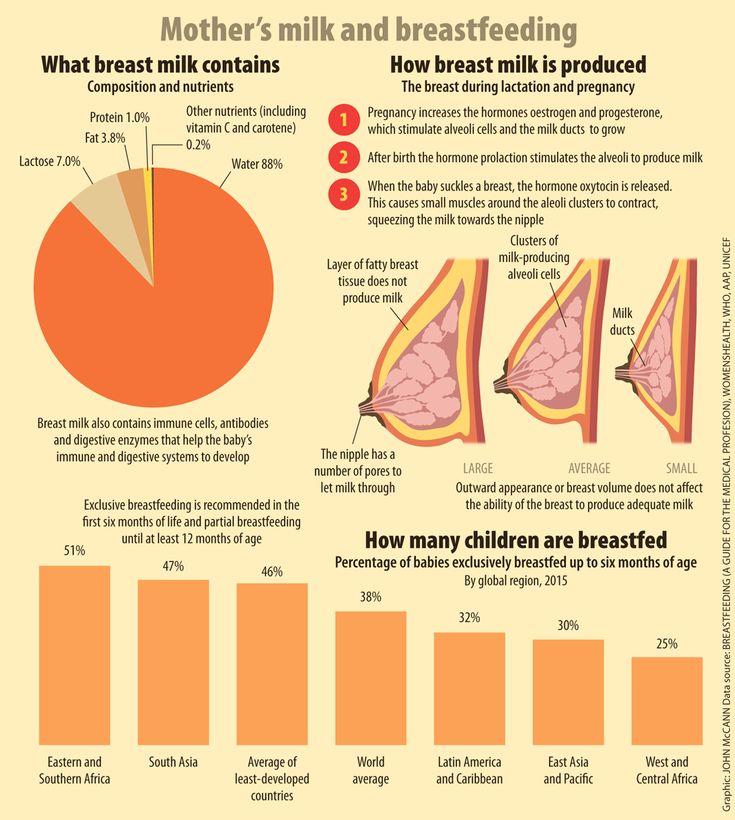 It is worth the first 1.5 months to be with the child around the clock, carry it in your arms or in a sling, sleep together, offer breasts to any squeak and grunt.
It is worth the first 1.5 months to be with the child around the clock, carry it in your arms or in a sling, sleep together, offer breasts to any squeak and grunt.
Do not formula feed
If it seems that there is not enough milk, you should not try to "diversify" the diet with milk formula. The first thing to do is to make sure your suspicion is correct. Unreasonable introduction of supplementary food can stop your own "milk production". While the baby is suckling, he sort of makes an order for the next time, for another feeding. That is, during feeding, the amount of milk necessary for the baby is consumed, and then as much as he needs will appear.
Do not skip meals
Sometimes mothers think - once I will give the baby a mixture, and the milk will “accumulate” for now. This is mistake. The body cannot work "in reserve". As soon as the alveoli are filled with milk, but it does not leave, production slows down. You can't save milk - you have to spend it all the time.