Birth trauma definition
What is Birth Trauma? - Birth Trauma Association
Birth trauma is a shorthand phrase for post-traumatic stress disorder (PTSD) after childbirth. We also use it for women who have some symptoms of PTSD, but not enough for a full diagnosis.
PTSD was first identified amongst soldiers returning from the Vietnam War, and most people still think of it as a condition experienced by soldiers. In fact, PTSD can follow any traumatic event – such as being in a car accident, being sexually abused or having a very difficult birth. It can also happen to people who have witnessed a traumatic event, so people who have seen someone else violently killed, for example, often experience PTSD. This is why some partners, and even midwives, experience PTSD after seeing a traumatic birth.
In most cases, what makes birth traumatic is the fear that you or your baby are going to die. We very often see birth trauma in women who have lost a lot of blood, for example, or who had to have an emergency caesarean because their baby’s heartrate suddenly dipped.
You can download our leaflet on coping with a difficult birth here.
Symptoms of birth trauma (postnatal PTSD)
There are four main symptoms:
- Re-experiencing the traumatic event through flashbacks, nightmares or intrusive memories. These make you feel distressed and panicky.
- Avoiding anything that reminds you of the trauma. This can mean refusing to walk past the hospital where you gave birth, or avoiding meeting other women with new babies.
- Feeling hypervigilant: this means that you are constantly alert, irritable and jumpy. You worry that something terrible is going to happen to your baby.
- Feeling low and unhappy (“negative cognition” in the medical jargon). You may feel guilty and blame yourself for your traumatic birth. You may have difficulty remembering parts of your birth experience.
Not everyone who has had a traumatic experience suffers from PTSD, but many do. It’s a completely normal response, and not a sign of weakness.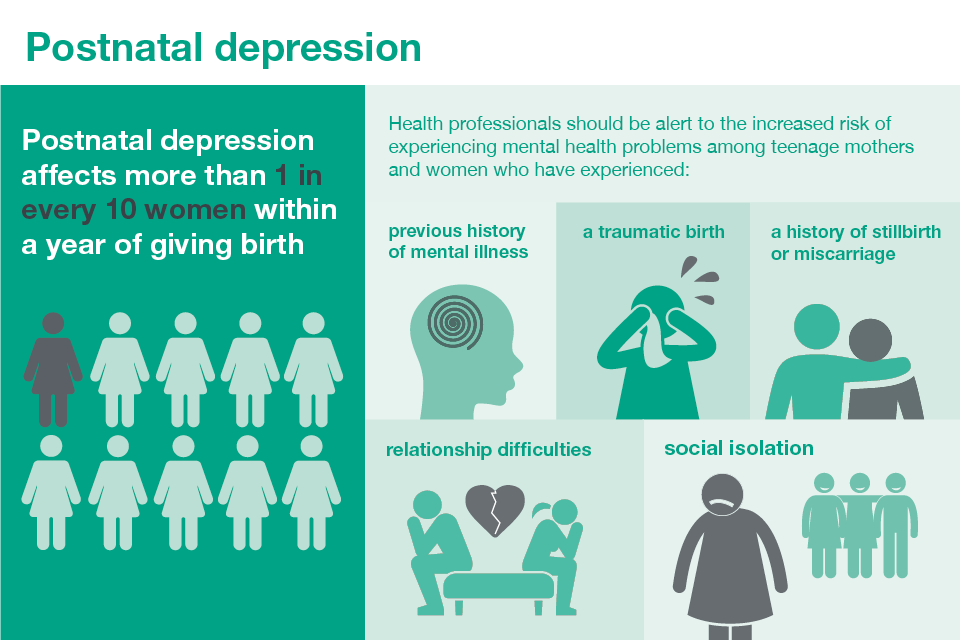 It’s also involuntary: brain scans show a difference between the brains of people with PTSD and those without. PTSD is not something that can be cured by “pulling yourself together” or “focusing on the positive,” despite what other people tell you.
It’s also involuntary: brain scans show a difference between the brains of people with PTSD and those without. PTSD is not something that can be cured by “pulling yourself together” or “focusing on the positive,” despite what other people tell you.
Who gets birth trauma?
Some women experience events during childbirth (as well as in pregnancy or immediately after birth) that would traumatise any normal person.
For other women, it is not always the sensational or dramatic events that trigger childbirth trauma but other factors such as loss of control, loss of dignity, the hostile attitudes of the people around them, feelings of not being heard or the absence of informed consent to medical procedures.
There is still a lot of research to be done, but some of the factors that make birth trauma more likely are:
- Lengthy labour or short and very painful labour
- Induction
- Poor pain relief
- Feelings of loss of control
- High levels of medical intervention
- Forceps births
- Emergency caesarean section
- Impersonal treatment or problems with staff attitudes
- Not being listened to
- Lack of information or explanation
- Lack of privacy and dignity
- Fear for baby's safety
- Stillbirth
- Birth of a baby with a disability resulting from a traumatic birth
- Baby’s stay in the special care baby unit or neonatal intensive care unit
- Poor postnatal care
- Previous trauma (for example, in childhood, with a previous birth or domestic violence)
Finally, people who witness their partner’s traumatic childbirth experience may also feel traumatised as a result. See our partners page for more information.
See our partners page for more information.
What is different about birth trauma?
Women affected by birth trauma often find that there is nowhere to turn for support because even other mothers who have not had traumatising births can find it hard to understand the impact of a traumatic birth. This can make sufferers lonely and depressed as they often feel they are somehow weaker than other women because they are unable to forget their birth experience. They may feel incredibly guilty as a result.
This is a terrible burden to shoulder. The nature of PTSD means it’s impossible to stop constantly thinking about the birth experience, but very few people are aware of this. Even health care professionals don't always understand.
Unfortunately, this lack of support can mean that relationships with friends and family may deteriorate. Many women end up feeling torn between their desire for more children and their determination to avoid another pregnancy. They may also lose interest in sex and these problems can place a great strain on relationships.
Some women also avoid any medical intervention that reminds them of their birth experience, such as smear tests.
For many women, their greatest concern is the day-to-day difficulties they encounter bonding with their baby who they see as a constant reminder of the trauma they have experienced.
The BTA aims to tackle this isolation by offering women much needed support and showing them that they are far from alone. By working together and providing women with a voice, we hope that we can help change those practices that contribute to birth trauma
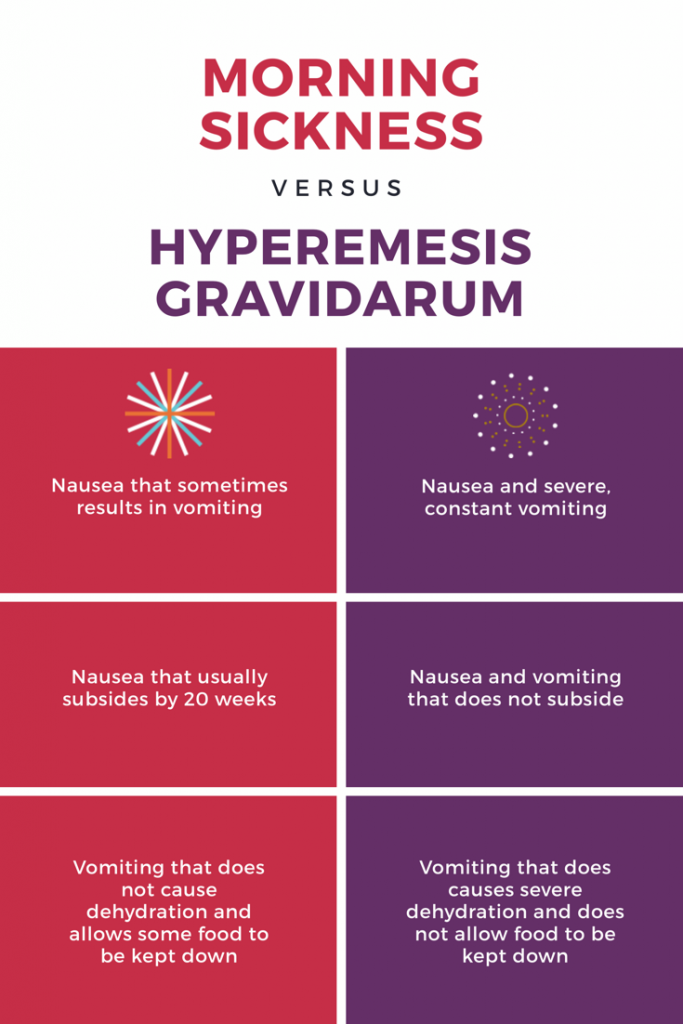
What’s the difference between birth trauma and postnatal depression?
Birth trauma can overlap with postnatal depression (PND) as some of the symptoms are the same, but the two illnesses are distinct and need to be treated individually.
Unfortunately, many women are wrongly diagnosed with PND and are prescribed medication that may do little, or nothing, to help their situation. Women tell us that they are frequently told by their health care professionals that they should try and move on with their lives or that they should just be grateful that they have a healthy baby. This can exacerbate the feelings of guilt and isolation that women already feel. Women may then end up with prescriptions for anti-depressants, simply because doctors do not understand the disorder.
This can exacerbate the feelings of guilt and isolation that women already feel. Women may then end up with prescriptions for anti-depressants, simply because doctors do not understand the disorder.
Sometimes PND can go hand in hand with birth trauma, however, and in those cases anti-depressants may be appropriate. If you are concerned that you have been misdiagnosed, do speak to your GP or health visitor. Please show them a copy of our leaflet if they appear to be unaware of birth trauma or the fact that it requires specialised treatment.
Birth trauma (emotional) | Pregnancy Birth and Baby
Birth trauma (emotional) | Pregnancy Birth and Baby beginning of content4-minute read
Listen
What is birth trauma?
'Birth trauma' is distress experienced by a mother during or after childbirth.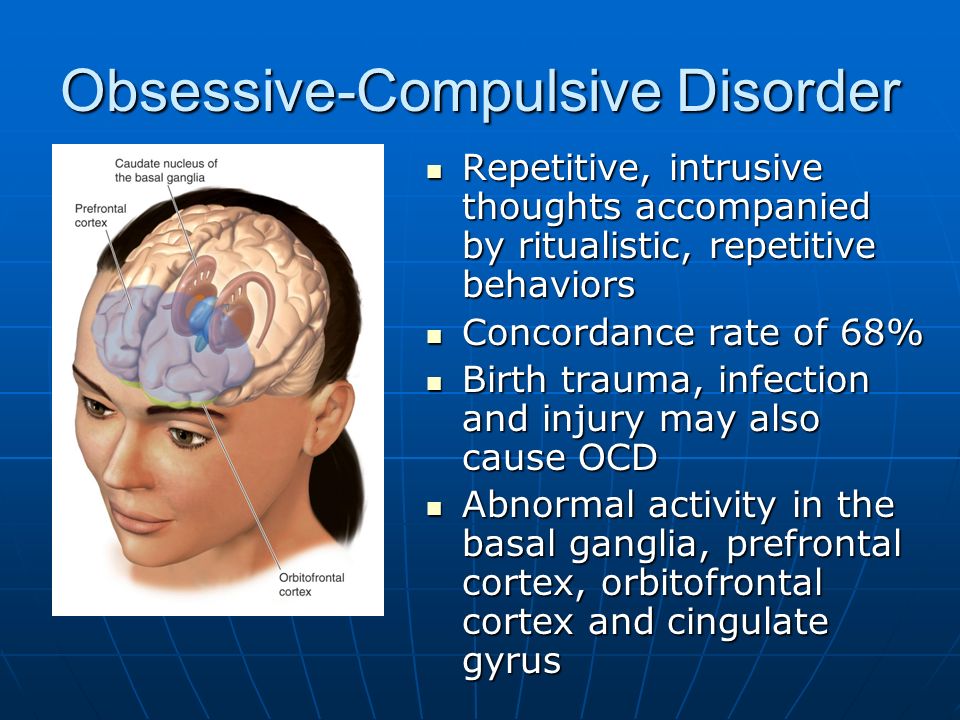 While trauma can be physical, it is often emotional and psychological.
While trauma can be physical, it is often emotional and psychological.
Birth trauma is not just about what happened during labour and the birth. It can also refer to how you, as the mother, are left feeling afterwards. Sometimes the effects of birth trauma can emerge and continue for some time after you've given birth.
At the time of birth, you may have felt fearful, helpless or unheard. After the birth, it's possible to feel shocked, guilty or numb and even experience panic attacks or anxiety.
If you notice any of these symptoms, you may be experiencing birth trauma. If so, you are certainly not alone. It's been estimated that up to 1 in 3 women who give birth may experience birth trauma.
Many women find the experience of childbirth emotionally traumatic. Birth trauma can't always be prevented, but there are things you can do to reduce your risk. If you are experiencing any signs of trauma, support and treatment are available.
What are the risk factors for birth trauma?
There are many factors that can contribute to birth trauma.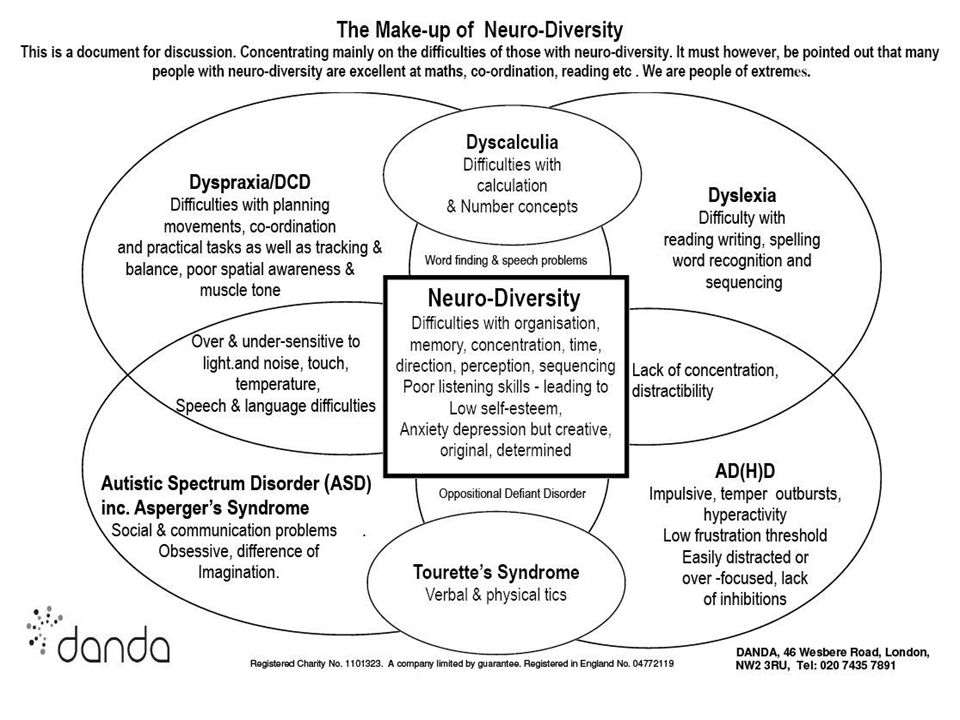 These include:
These include:
- your childbirth experience not going to plan, or not matching your expectations
- having a difficult labour or experiencing labour complications
- needing intervention during labour, such as an assisted delivery (using forceps or ventouse) or an emergency caesarean
- you or your baby suffering birth injury
- your baby needing medical attention after the birth
- stillbirth or neonatal death
- not receiving the care or support you needed at the time of birth, or afterwards
- previous birth trauma
- a tendency to experience anxiety
A woman may be especially at risk of trauma during pregnancy, birth and after the birth if she experienced trauma earlier in her life. This can include domestic violence, childhood sexual abuse, rape and migration-related trauma.
Can birth trauma be prevented?
Childbirth doesn't always go to plan. Many women who experience birth trauma are unable to avoid it because the risk factors (for example, a history of trauma) are beyond their control.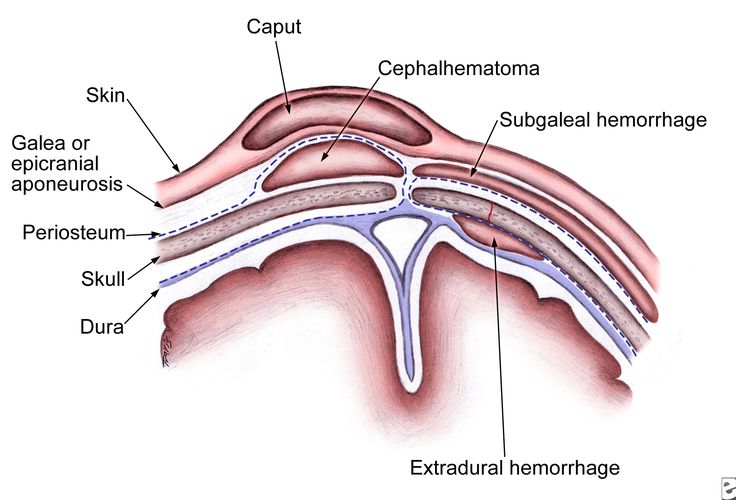
However, there are ways to help reduce the risk of birth trauma:
- Prepare for childbirth: Antenatal classes, for example, help you know what to expect and your options.
- Try to have realistic expectations: There is no 'right' way to give birth. Things don't always go to plan and some things are beyond your control.
- Try to keep an open mind: No one can predict what will or won't happen during pregnancy and birth.
- Establish a support network: Surround yourself with people who can support you.
- Seek mental health support: If you are prone to anxiety or depression, or if you had a difficult pregnancy or labour, counselling can help you come to terms with what happened.
How is birth trauma treated?
If you think you could be experiencing emotional trauma, it's very important to seek help as early as possible — which benefits both you and your family.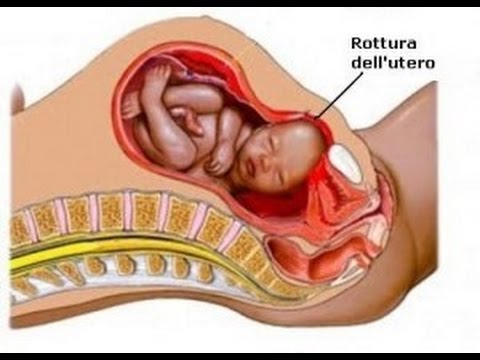
Some psychological symptoms, including the 'baby blues', are very common around the time of birth. But if you still feel distressed 2 or more weeks after the birth, you could have postnatal depression or anxiety.
In some cases, not getting treatment for birth trauma can lead to post-traumatic stress disorder (PTSD). One Australian study found that more than 1 in 20 mothers may show signs of PTSD at 12 weeks after giving birth.
It may help you to:
- talk to a midwife immediately after the birth about your experience
- talk to your doctor, midwife or maternal child health nurse at any stage about how you feel
- ask for practical and emotional support from friends and family
- use self-help measures, such as exercise and mindfulness
If needed, therapy or medicines can also be used as treatment. Your doctor is the best person to advise you on this.
Where can I go for more support and advice?
As well as asking your doctor or nurse for advice, you can get help and information from:
- Pregnancy, Birth and Baby — call 1800 882 436 to speak to a maternal child health nurse (7 days a week, 7am to midnight AEST).

- The Australian Birth Trauma Association offers advice, resources and a peer-to-peer support service.
- The Centre of Perinatal Excellence (COPE) provides information and a list of support services.
- Perinatal Anxiety & Depression Australia (PANDA) — call 1300 726 306 to speak with a counsellor (Mon to Fri, 9am to 7.30pm AEST).
Sources:
Australasian Birth Trauma Association (What is birth trauma), Australasian Birth Trauma Association (What is psychological birth trauma), Centre of Perinatal Excellence (When things don’t go to plan), Perinatal Anxiety & Depression Australia (Childbirth trauma), SA Health (South Australian Perinatal Practice Guideline - Managing women in distress after a traumatic birth experience), Centre of Perinatal Excellence (Preparing for birth), Centre of Perinatal Excellence (Recovering from a traumatic birth), Psychological Medicine (A prospective longitudinal study of the prevalence of post-traumatic stress disorder resulting from childbirth events), Perinatal Anxiety & Depression Australia (Complicated births), Perinatal Anxiety & Depression Australia (During pregnancy)Learn more here about the development and quality assurance of healthdirect content.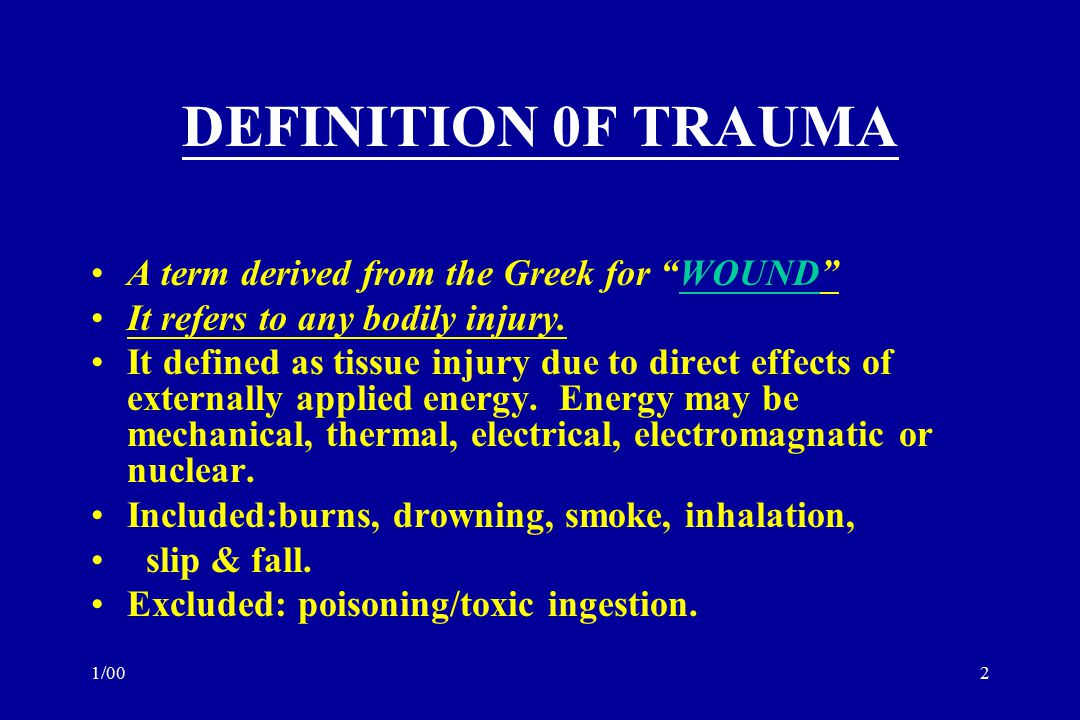
Last reviewed: May 2021
Back To Top
Related pages
- Mum's first few days after giving birth
- Your physical and emotional wellbeing
- Baby blues
- Birth injury (to the mother)
- Birth injury (to the baby)
Need more information?
Psychological Trauma - Birth Trauma
Read more on Australasian Birth Trauma Association website
Physical Trauma - Birth Trauma
For many women who have suffered from physical trauma as a result of childbirth, and who are struggling to cope, is it vital that healthcare providers
Read more on Australasian Birth Trauma Association website
What is Birth Trauma? - Birth Trauma
The delivery of a baby is a positive event for many women, but for some it can be a mixed experience or even very negative, resulting in physical and/or
Read more on Australasian Birth Trauma Association website
Considerations for birthing after birth trauma - Birth Trauma
In this post we consider some important points when making decisions about birthing after a birth trauma experience.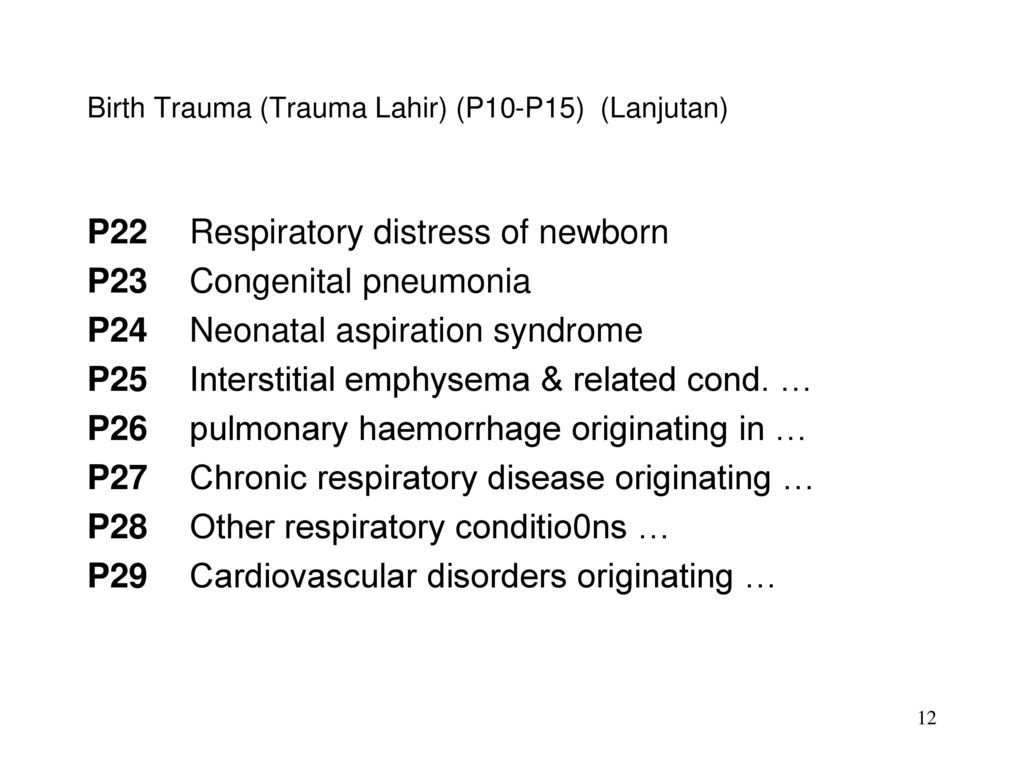
Read more on Australasian Birth Trauma Association website
Childbirth trauma and recovery | PANDA
While many pregnant women and their partners know birthing their baby will be hard work, very few expect labour and childbirth could be complicated.
Read more on Perinatal Anxiety and Depression Australia (PANDA) website
Family & Friends - Birth Trauma
If you are reading this then you may have someone close to you that has been impacted by a difficult birth experience, be it a partner, loved one or someone
Read more on Australasian Birth Trauma Association website
Early Postnatal - Birth Trauma
The early postnatal period is a time of emotional change for most women. Some women may experience distress or symptoms of depression at this time if they
Some women may experience distress or symptoms of depression at this time if they
Read more on Australasian Birth Trauma Association website
thinknatal - Birth Trauma
We have developed THINKNATALTM, a series of educational resources aimed at providing support and information on a variety of topics that are often excluded or
Read more on Australasian Birth Trauma Association website
Caesarean Section - Birth Trauma
Being abdominal surgery, pain in the early months is very common after a caesarean section (C-section) and needs to be managed with rest, pain relief, and
Read more on Australasian Birth Trauma Association website
Information for Parents (to be) - Birth Trauma
First we want you to know that we are with you and we are here for you. You are not alone.Times are challenging, staying at home, working from home, home
You are not alone.Times are challenging, staying at home, working from home, home
Read more on Australasian Birth Trauma Association website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.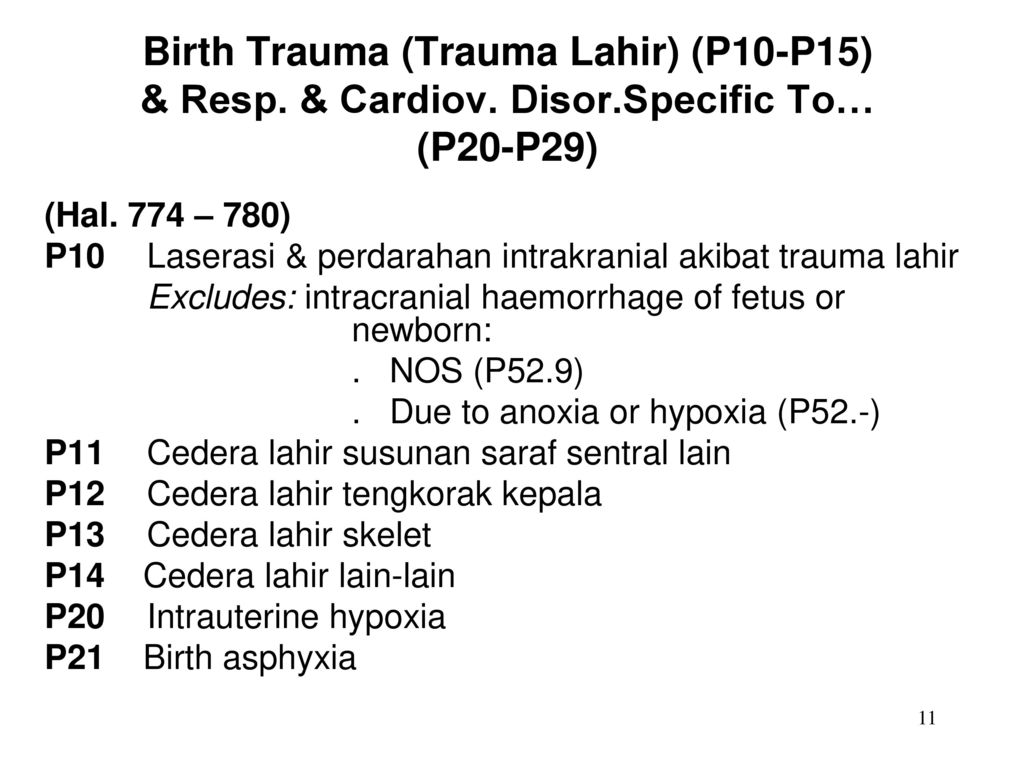
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.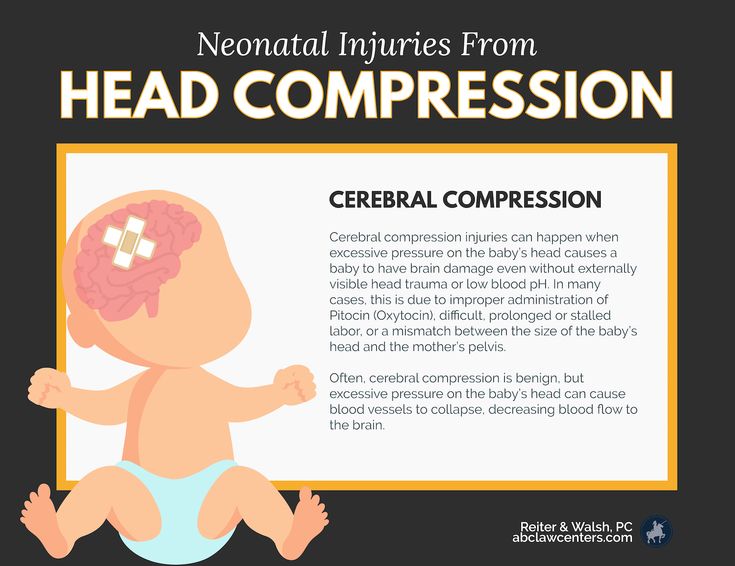
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Birth injuries: types, symptoms, complications
Birth injuries: types, symptoms, complications
Sometimes babies get injured during childbirth - according to statistics, about 10% of newborns need medical care. Birth injuries are not always easy to spot at a glance. They are easy to identify by characteristic signs that indicate the need for medical intervention.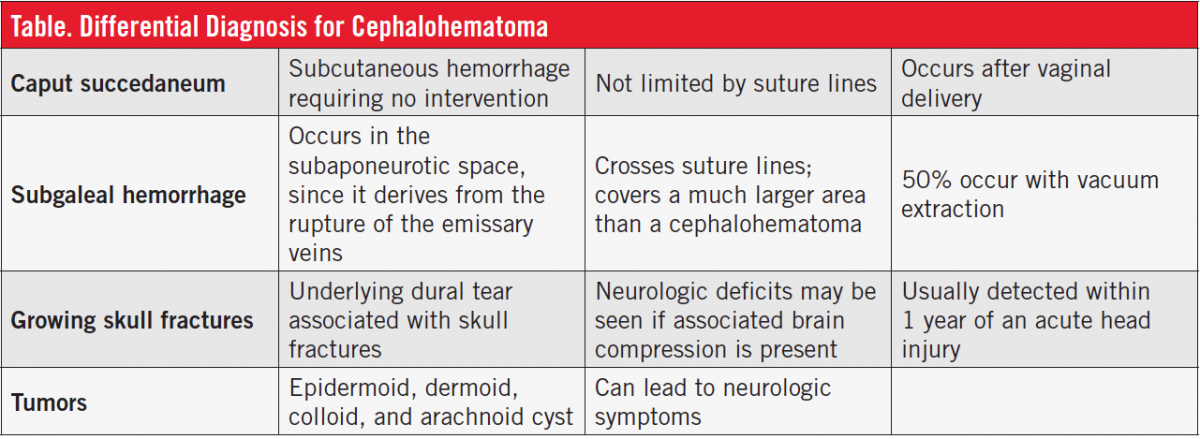 The sooner the child gets help, the less likely complications are.
The sooner the child gets help, the less likely complications are.
Sometimes during childbirth, children are injured - according to statistics, about 10% of newborns require medical care. Birth injuries are not always easy to spot at a glance. They are easy to identify by characteristic signs that indicate the need for medical intervention. The sooner the child gets help, the less likely complications are.
Most common birth injuries
Medicine knows many of their types. The following deviations occur most frequently:
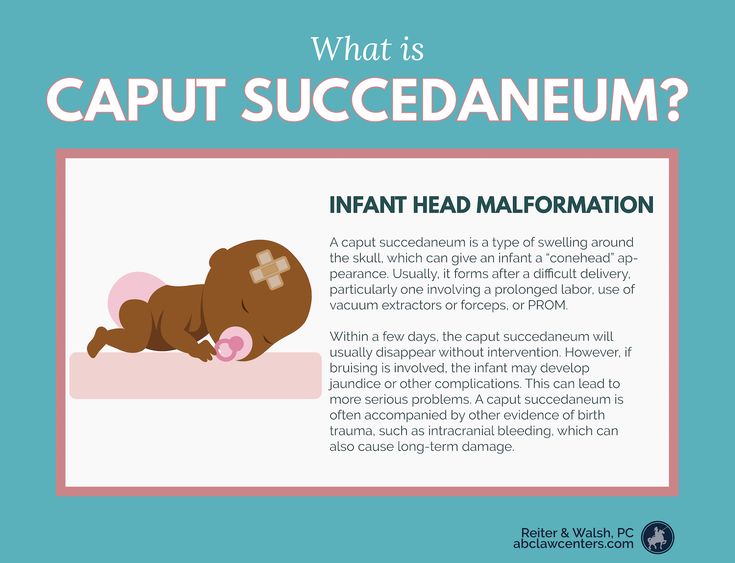
- injuries of cranial bones;
- damage to duplications of the dura mater;
- epidural hemorrhages;
- cephalohematomas;
- birth tumors.
They are also fraught with serious consequences that can greatly affect the child's quality of life. It is impossible to avoid complications without qualified medical care. Injuries received by the child during childbirth lead to the following complications:
- general developmental delay;
- delayed speech development;
- sleep disorders;
- epileptic syndrome;
- autism;
- clubfoot;
- cerebral palsy;
- hyperactivity;
- as well as a number of other diseases.
Damage affects the development of internal organs, the brain, the central nervous system, the spine, and the skeletal system. In the future, they can cause serious complications.
How to recognize a birth injury?
The consequences, as a rule, are not immediately noticeable - the problem worsens gradually, in some cases the process is delayed for 2-3 years. There are characteristic signs that indicate the need to show the baby to a specialist:
- Restless behavior of the child;
- frequent regurgitation;
- hand or foot movement disorders;
- skull asymmetry;
- reflex disorders;
- sleep disorders.
These signs are expressed to a greater or lesser extent - sometimes violations are visible immediately, but in most cases only a specialist can determine them
Risk group
Children at risk must be examined by a specialist. How do you know if your baby is in this group? It includes children who have had a hard time coming into the world.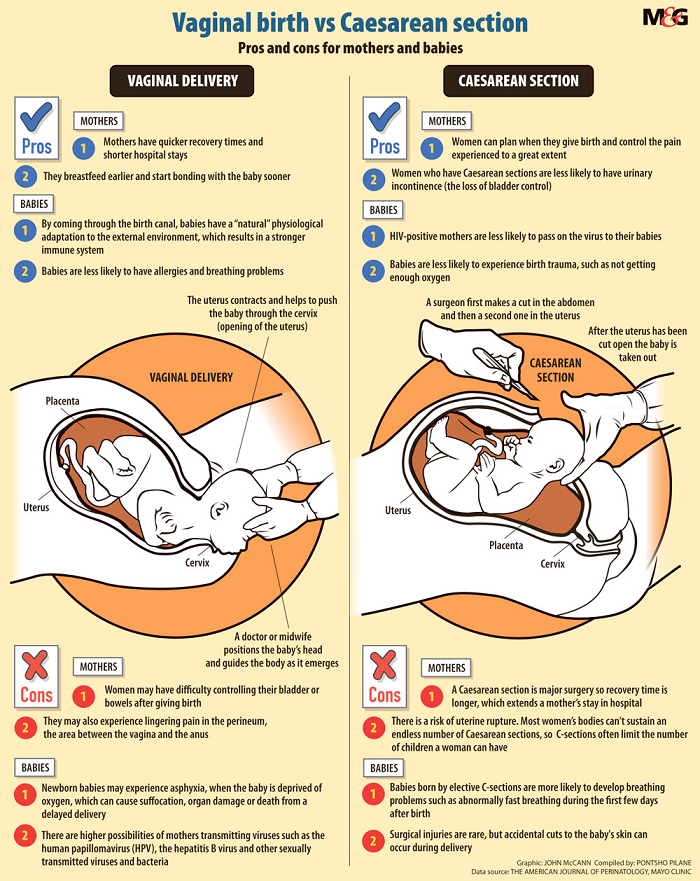 This can be judged by the following signs:
This can be judged by the following signs:
- cesarean section;
- large fruit weight - over 4 kg;
- state of hypoxia;
- cephalohematoma - swelling on the skull of a newborn;
- induction of labor and obstetric manipulations.
Children born as a result of difficult childbirth must be shown to a specialist. Qualified medical care will help to avoid the development of complications, even if the child was injured during childbirth. The Baby Plus Medical Center has all the necessary equipment for examination and laboratory tests. Our center is located in the village of VNIISSOK (Odintsovsky district, residential complex "Gusarskaya Ballada"). You can make an appointment right now! Our experts are ready to come to the residents of the Odintsovo district at home - they do not have to make an appointment for an examination.
Date of publication: 13.12.2018 17:05:16
Birth injury - causes of disease, methods, prevention Clinic "OSTEOMED" provides treatment of birth injuries, rehabilitation after birth injuries in newborns, infants (infants), babies.
 Birth trauma is treated with effective osteopathic methods. Traditional and modern methods of reflexology (reflexotherapy) are actively used in the treatment. We carry out the restoration of the child's nervous system (NS), recovery after birth injuries. In pediatric practice, an osteopathic approach is mainly used, which is absolutely gentle and safe for babies. The osteopath applies gentle hand pressure on the baby's head and body to ease the effects of birth stress, and correct tension in the skull bones and restore their proper movement. Children and babies feel great after treatment and sleep better.
Birth trauma is treated with effective osteopathic methods. Traditional and modern methods of reflexology (reflexotherapy) are actively used in the treatment. We carry out the restoration of the child's nervous system (NS), recovery after birth injuries. In pediatric practice, an osteopathic approach is mainly used, which is absolutely gentle and safe for babies. The osteopath applies gentle hand pressure on the baby's head and body to ease the effects of birth stress, and correct tension in the skull bones and restore their proper movement. Children and babies feel great after treatment and sleep better. Birth trauma is damage to tissues or organs of the fetus during childbirth (birth act) due to local action of mechanical forces on the fetus. Unfortunately, birth injuries in newborns are quite common.
90% of children have a birth injury, most often it is the cervical spine. If the diagnosis of "birth trauma" is not made, it is advisable for you to contact an osteopath if the following situations occurred during childbirth:
- long dry period
- Opening the fetal bladder by a doctor in the maternity hospital
- Stimulation of labor
- Obstetric manipulations: imposition of forceps, fruit squeezing
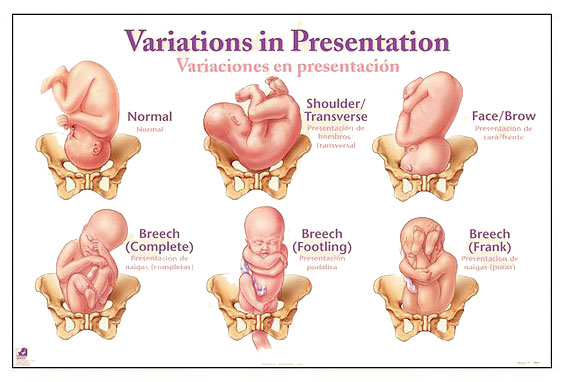
- The birth of a child in the pelvic presentation
- Caesarean section
- epidural (spinal) anesthesia in women in women in women and after 35 years
- the birth of a large fetus, more than 4 kg
- if your child was born in a state of hypoxia: blue, did not cry right away, there was an entanglement of the umbilical cord, low Apgar scores
- if your child had a cephalohematoma (swelling on the baby's head) - this indicates a serious injury to the bones of the skull
- your child has been diagnosed with PEP (perinatal encephalopathy), IUGR (intrauterine growth retardation)
Predisposing factors for birth trauma
The main predisposing factors leading to birth trauma are as follows:
1. Pathology of the prenatal period.
Pathology of the prenatal period.
2. Pathology of the antenatal period.
3. Wrong course of pregnancy.
4. Toxicosis, preeclampsia.
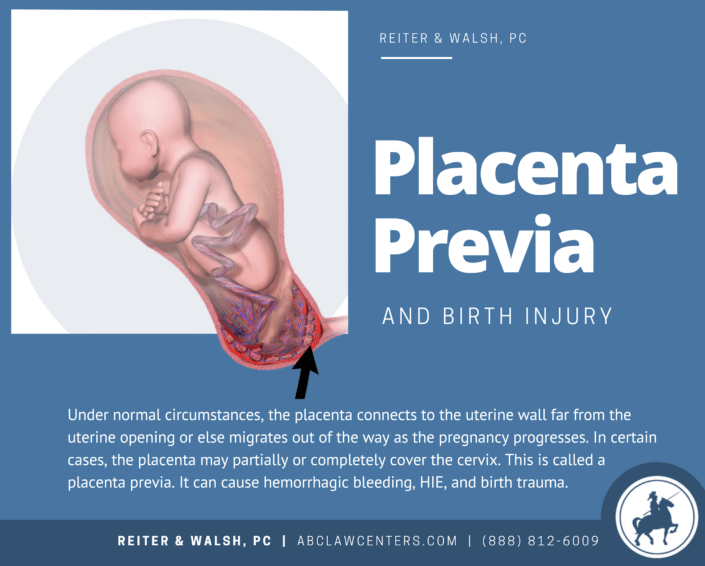
5. Placenta previa.
6. Infection of the birth canal (vagina, uterus, etc.).
7. Genital diseases of the mother (woman), diseases of the genital organs: salpingitis, inflammation of the appendages, salpingoophoritis, endometritis, vaginitis, vulvovaginitis, sexually transmitted diseases (venous diseases, venous diseases), infections, inflammatory diseases of the genital organs.
8. Extragenital diseases (diseases) of the mother. Diseases of the cardiovascular system, Rh incompatibility (Rh conflict) have a particularly strong influence.
9. Preterm pregnancy (fetal miscarriage).
10. Prolongation of pregnancy (post-term fetus).
11. Intrauterine fetal hypoxia (VGP, VUG, VUGP), chronic intrauterine hypoxia (lack of oxygen).
12. Cesarean section (birth trauma during caesarean section).
13. The use of a vacuum extractor in childbirth (vacuum extraction, vacuum extractors, a comprehensive vacuum system for obstetrics, a vacuum extractor). Vacuum fruit extraction.
14. Rapid delivery, stimulation in childbirth.
15. Stress, neurosis, neurasthenia.
16. Increased risk if previous pregnancies ended badly (miscarriage, stillbirth, stillbirth, congenital malformations - congenital malformations).
Mechanism of development, pathogenesis of birth trauma
What is the mechanism of development of birth trauma, its pathogenesis? All of the above factors cause fetal hypoxia and reduce the resistance of its organs and tissues, especially the brain. All this leads to traumatic effects during childbirth.
Classification of lesions of the nervous system in children
Neonatologist, neurologist, neuropathologist, microneuropathologist distinguish 2 main types of birth injuries (classification by localization):
1. Birth trauma of the central nervous system (CNS).
Birth trauma of the central nervous system (CNS).
2. Birth trauma of the peripheral nervous system (PNS).
There are also the following pathologies: obstetric paralysis (obstetric paralysis), intracranial birth injury (for example, traumatic brain birth injury of the head, brain, cerebellum), birth injury of the spinal cord (for example, birth injury of the cervical spine, neck), birth injuries of peripheral nerves , birth injury of soft tissues (for example, birth tumor), birth injury of bones, skeletal system (for example, fracture of the collarbone), birth injury of internal organs. Separately, obstetric trauma due to obstetric manipulations is singled out, especially in case of an abnormal course of childbirth.
Consequences of birth injuries
The consequences of birth trauma are varied. Hemorrhages in the brain, paralysis (paralysis), paresis (paresis), retarded growth and development of arms or legs, impaired muscle tone, convulsions, hypertension syndrome, intracranial hypertension, hydrocephalus, convulsive and non-convulsive seizures, damage to cranial nerves, liquorodynamic disorders, decerebrate rigidity, cerebral palsy (ICP), perinatal encephalopathy (PEP), psychomotor retardation, speech retardation, minimal brain dysfunction, pneumonia, urosepsis and the worst consequences.
Birth trauma prevention
How to avoid birth trauma in newborns? To avoid birth injuries, you must follow a number of recommendations:
- Plan conception and pregnancy in advance.
- Treat chronic conditions before pregnancy.
- Eliminate alcohol (alcoholic beverages), smoking (quit smoking) 3 months before conception and during pregnancy.
- Carry out activities aimed at the prevention and treatment of intrauterine fetal hypoxia.
- Give birth in a good health facility.
- Prior to delivery (1 month in advance) to communicate with such specialists as an obstetrician, gynecologist, midwife, neonatologist, neurologist, microneurologist, neuropathologist, resuscitator who will take part in childbirth.
- Eat well and take vitamins during pregnancy.
- During pregnancy, attend childbirth preparation courses.
- During pregnancy, rest more and work less, walk in the fresh air.
- During pregnancy, regularly visit a medical institution such as a antenatal clinic, conduct the necessary tests, examinations, and studies.
- During pregnancy, avoid contact with infectious patients (especially those with diseases such as influenza, adenovirus infection, parainfluenza, MS infection (respiratory syncytial infection), rotavirus infection (rotavirus infection), SARS, herpes (herpetic infection), rubella, measles, mumps (mumps, mumps), chicken pox (chickenpox), chlamydia, Ebola, plague, HIV infection, tuberculosis, diphtheria, tetanus, echinococcosis, toxoplasmosis, teratogenic infections).
- Carry out activities aimed at preventing Rh conflict (take into account the Rh blood of the father and mother Rh, use a condom during oral sex).
- During pregnancy, try to avoid exposure to such a pathological factor as ionizing radiation, radio waves (microwave ovens, microwave ovens, microwave ovens, x-rays, radiography, MRI - magnetic resonance imaging, NMRI (nuclear magnetic resonance imaging), CT (computed tomography), cellular phone, smartphone, tablet, computer).
- Exclude the intake of the following: medicines, medicines, medicines, medicines, dietary supplements, dietary supplements not prescribed by a doctor.
 Do not engage in self-medication, uncontrolled intake of drugs.
Do not engage in self-medication, uncontrolled intake of drugs.
Signs of birth trauma
Many parents, fathers and mothers ask us: “What are the first signs that a child has a birth injury?”, “How to determine a birth injury in a child, a newborn?” “Does the baby have a birth injury?” "What are the signs of birth trauma, the consequences of birth trauma?". You should consult a doctor if you notice any of the following symptoms:
Online entry
Online record
Date of visit
2.12.2022
Doctors
Our specialists
Smirnov Andrey Valerievich
Clinic Osteomeda, neurologist-Osteopat, candidate of medical sciences, member of ENRO, ENRO, ENER doctor of osteopathy in Europe (registration number 248041051021), lecturer at the "School of Osteopathy on the Neva" at the Department of Neurology, St. Petersburg Institute of Higher Education
Kristina Aleksandrovna Zoller
Neurologist-osteopath, candidate of medical sciences, member of ENRO and ROSA, doctor of osteopathy in Europe (registration number 204115070812), director of the "School of Osteopathy on the Neva", head of the course of osteopathy at the Department of Neurology, SPbIUVE
Kaprielov Karen Aleksandrovich
Osteopath, member of ENRO, doctor of osteopathy of Europe (registration number 244046031012), chiropractor
Cherny Roman Anatolyevich
Osteopath, member of ENRO, doctor of osteopathy of Europe (registration number 22212) School of Osteopathy on the Neva" at the Department of Neurology, St.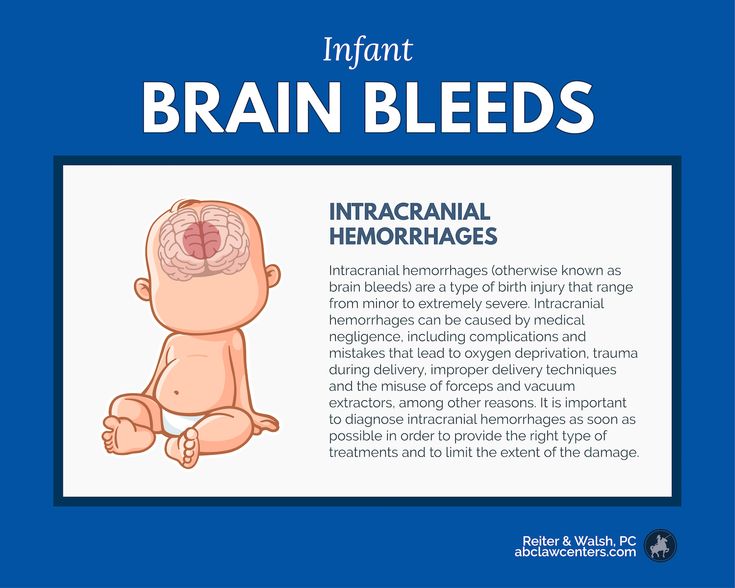 Petersburg Institute of Higher Education
Petersburg Institute of Higher Education
Poznyak Alina Alekseevna
Neurologist-osteopath, member of ENRO, Doctor of Osteopathy of Europe
Bekuzarova Svetlana Anatolyevna
Otopat doctor, manual therapist, kinesiotepection specialist
Komyakhov Andrey Valerievich
Neurologist-Osteopath, candidate of medical sciences, doctor of osteopathy of Europe, member of the ENRO (registration number 635042181721)
Azommedova Sakhila Khaladdinovna Narodinovna Narodinovna Narodinovna. , member of ENRO, M.D., Medicine Doctor (registration number 637042181712)
Tsivinsky Anton Dmitrievich
Neurologist-osteopath, candidate of medical sciences, member of ENRO, doctor of osteopathy of Europe (registration number 654051291721), chiropractor, specialist in the manufacture of individual orthopedic insoles
Tsoy Marina Removna
Neurologist-osteopath, Doctor of Osteopathy of Europe, M.D., Medicine Doctor
Vydra Anatoly Alexandrovich
Neurologist-osteopath, specialist in articulation, kinesiotherapy (registration number 589102271521), M.