Postpartum depression hallucinations
SAMHSA’s National Helpline | SAMHSA
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Main page content
-
SAMHSA’s National Helpline is a free, confidential, 24/7, 365-day-a-year treatment referral and information service (in English and Spanish) for individuals and families facing mental and/or substance use disorders.
Also visit the online treatment locator.
SAMHSA’s National Helpline, 1-800-662-HELP (4357) (also known as the Treatment Referral Routing Service), or TTY: 1-800-487-4889 is a confidential, free, 24-hour-a-day, 365-day-a-year, information service, in English and Spanish, for individuals and family members facing mental and/or substance use disorders. This service provides referrals to local treatment facilities, support groups, and community-based organizations.
Also visit the online treatment locator, or send your zip code via text message: 435748 (HELP4U) to find help near you. Read more about the HELP4U text messaging service.
The service is open 24/7, 365 days a year.
English and Spanish are available if you select the option to speak with a national representative. Currently, the 435748 (HELP4U) text messaging service is only available in English.
In 2020, the Helpline received 833,598 calls. This is a 27 percent increase from 2019, when the Helpline received a total of 656,953 calls for the year.
The referral service is free of charge. If you have no insurance or are underinsured, we will refer you to your state office, which is responsible for state-funded treatment programs. In addition, we can often refer you to facilities that charge on a sliding fee scale or accept Medicare or Medicaid.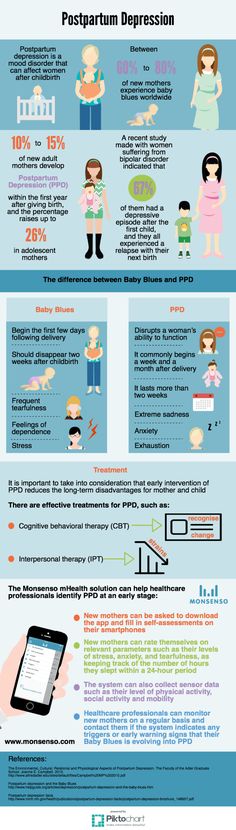 If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
The service is confidential. We will not ask you for any personal information. We may ask for your zip code or other pertinent geographic information in order to track calls being routed to other offices or to accurately identify the local resources appropriate to your needs.
No, we do not provide counseling. Trained information specialists answer calls, transfer callers to state services or other appropriate intake centers in their states, and connect them with local assistance and support.
-
Suggested Resources
What Is Substance Abuse Treatment? A Booklet for Families
Created for family members of people with alcohol abuse or drug abuse problems. Answers questions about substance abuse, its symptoms, different types of treatment, and recovery.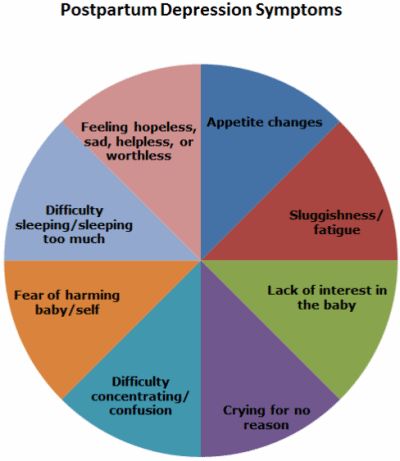 Addresses concerns of children of parents with substance use/abuse problems.
Addresses concerns of children of parents with substance use/abuse problems.It's Not Your Fault (NACoA) (PDF | 12 KB)
Assures teens with parents who abuse alcohol or drugs that, "It's not your fault!" and that they are not alone. Encourages teens to seek emotional support from other adults, school counselors, and youth support groups such as Alateen, and provides a resource list.After an Attempt: A Guide for Taking Care of Your Family Member After Treatment in the Emergency Department
Aids family members in coping with the aftermath of a relative's suicide attempt. Describes the emergency department treatment process, lists questions to ask about follow-up treatment, and describes how to reduce risk and ensure safety at home.Family Therapy Can Help: For People in Recovery From Mental Illness or Addiction
Explores the role of family therapy in recovery from mental illness or substance abuse. Explains how family therapy sessions are run and who conducts them, describes a typical session, and provides information on its effectiveness in recovery.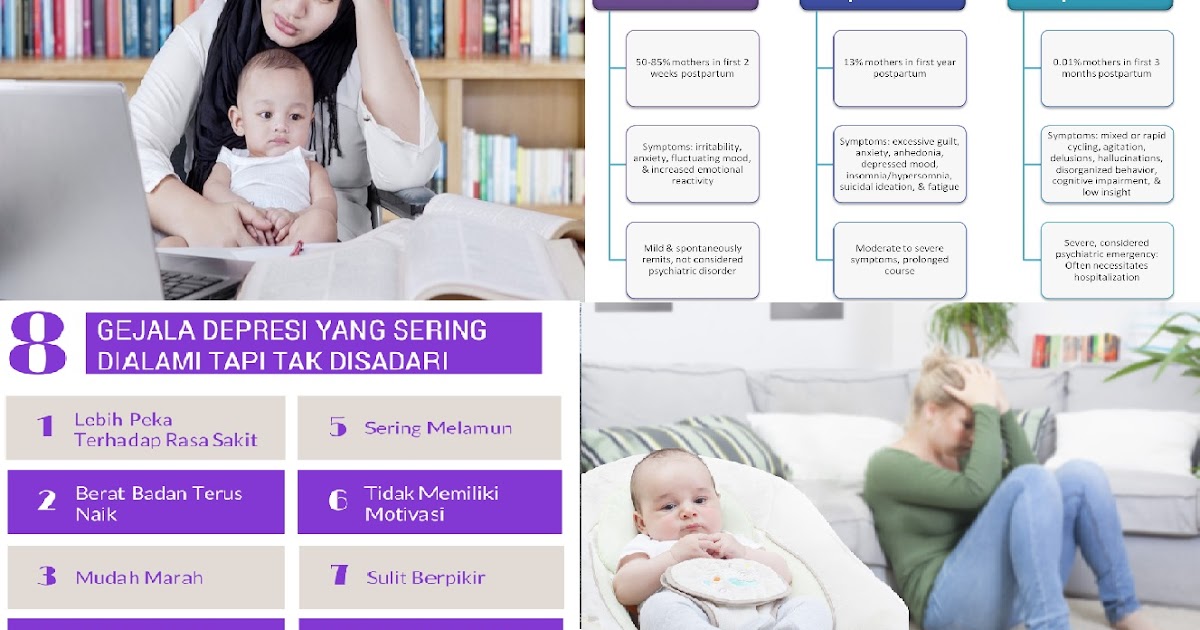
For additional resources, please visit the SAMHSA Store.
Last Updated: 08/30/2022
SAMHSA Behavioral Health Treatment Services Locator
HomeWelcome to the Behavioral Health Treatment Services Locator, a confidential and anonymous source of information for persons seeking treatment facilities in the United States or U.S. Territories for substance use/addiction and/or mental health problems.
PLEASE NOTE: Your personal information and the search criteria you enter into the Locator is secure and anonymous. SAMHSA does not collect or maintain any information you provide.
Please enter a valid location.
please type your address
-
FindTreatment.
 gov
gov Millions of Americans have a substance use disorder. Find a treatment facility near you.
-
988 Suicide & Crisis Lifeline
Call or text 988
Free and confidential support for people in distress, 24/7.
-
National Helpline
1-800-662-HELP (4357)
Treatment referral and information, 24/7.

-
Disaster Distress Helpline
1-800-985-5990
Immediate crisis counseling related to disasters, 24/7.
- Overview
- Locator OverviewLocator Overview
- Locator OverviewLocator Overview
- Finding Treatment
- Find Facilities for VeteransFind Facilities for Veterans
- Find Facilities for VeteransFind Facilities for Veterans
- Facility Directors
- Register a New FacilityRegister a New Facility
- Register a New FacilityRegister a New Facility
- Other Locator Functionalities
- Download Search ResultsDownload Search Results
- Use Google MapsUse Google Maps
- Print Search ResultsPrint Search Results
- Use Google MapsUse Google Maps
- Icon from Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers).
 Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers).
Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers). - Icon from Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers). Find programs providing methadone for the treatment of opioid addiction (heroin or pain relievers).
The Locator is authorized by the 21st Century Cures Act (Public Law 114-255, Section 9006; 42 U.S.C. 290bb-36d). SAMHSA endeavors to keep the Locator current. All information in the Locator is updated annually from facility responses to SAMHSA’s National Substance Use and Mental Health Services Survey (N-SUMHSS). New facilities that have completed an abbreviated survey and met all the qualifications are added monthly. Updates to facility names, addresses, telephone numbers, and services are made weekly for facilities informing SAMHSA of changes. Facilities may request additions or changes to their information by sending an e-mail to [email protected], by calling the BHSIS Project Office at 1-833-888-1553 (Mon-Fri 8-6 ET), or by electronic form submission using the Locator online application form (intended for additions of new facilities).
Updates to facility names, addresses, telephone numbers, and services are made weekly for facilities informing SAMHSA of changes. Facilities may request additions or changes to their information by sending an e-mail to [email protected], by calling the BHSIS Project Office at 1-833-888-1553 (Mon-Fri 8-6 ET), or by electronic form submission using the Locator online application form (intended for additions of new facilities).
Postpartum depression
Page 2 of 7
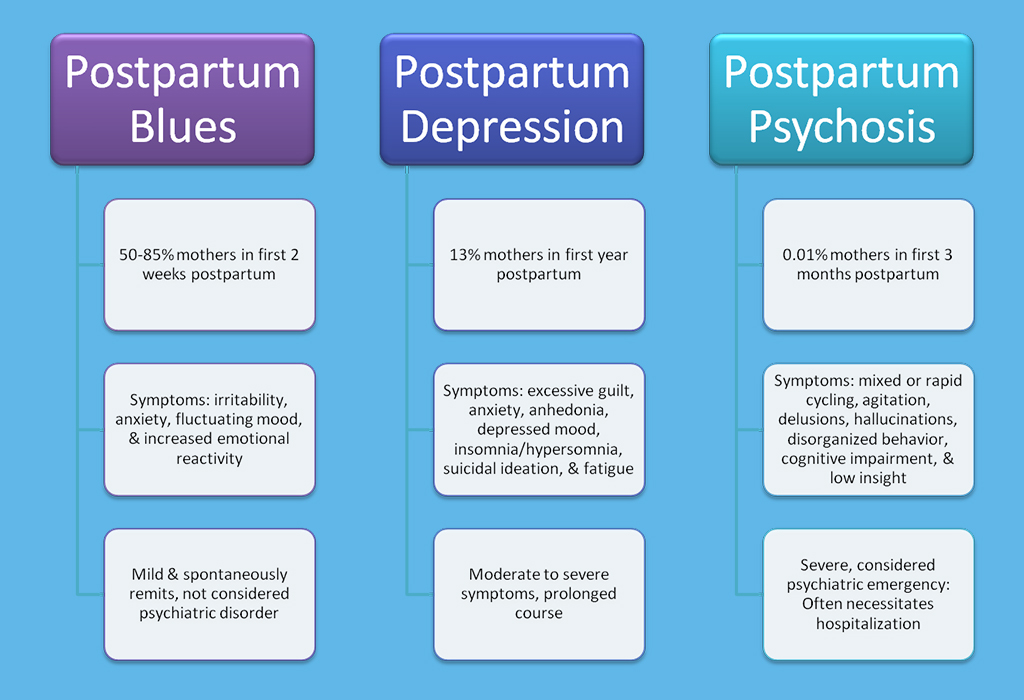
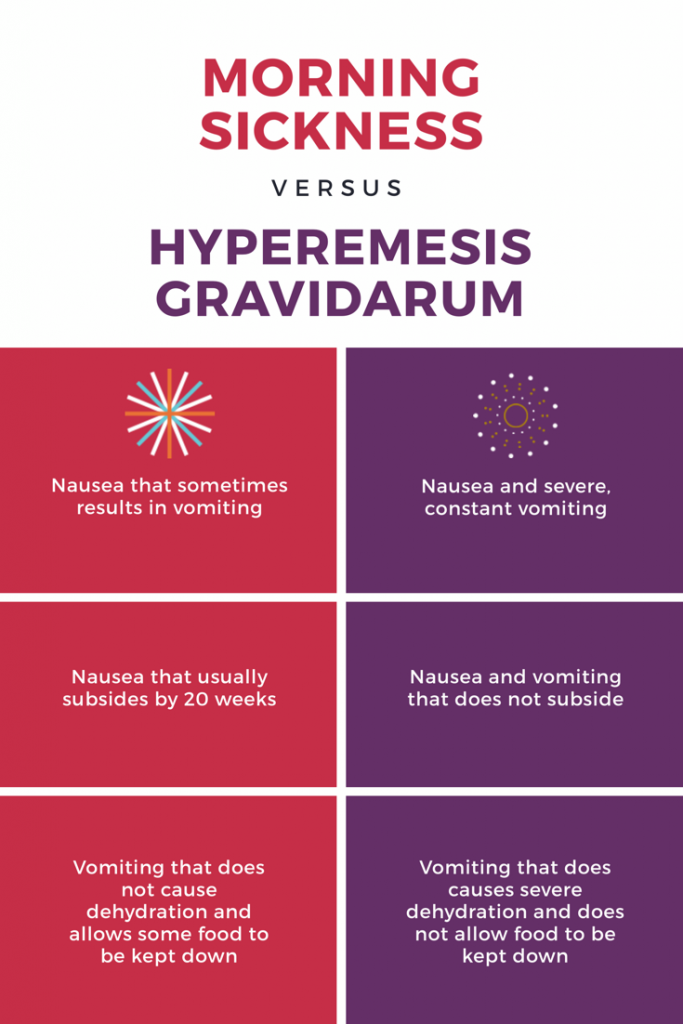
At least one in 10 mothers suffers from postpartum depression. It is one of the most frequent postpartum complications and occurs in 10-13% of women in labor. As a rule, in such cases it is not always possible to make a correct diagnosis, because mothers are reluctant to seek medical help. Psychotic states in the postpartum period occur in no more than 0.1-0.3% of cases. That is, out of every thousand women who give birth, from 1 to 3 suffer from an even more severe form of depression - postpartum psychosis, in which a woman develops delusions or hallucinations, often accompanied by an obsession with harming herself or the child. The psychotic state significantly impairs the woman's ability to function naturally in family and social life, and also poses a significant risk of committing a suicide attempt. In most cases, the postpartum psychotic state requires urgent hospitalization of the patient. Early postpartum depression develops in the first days or weeks after childbirth, and usually lasts from a week to a month. Late postpartum depression usually develops several months after pregnancy. Its duration can be different, but more often it lasts more than a month.
The psychotic state significantly impairs the woman's ability to function naturally in family and social life, and also poses a significant risk of committing a suicide attempt. In most cases, the postpartum psychotic state requires urgent hospitalization of the patient. Early postpartum depression develops in the first days or weeks after childbirth, and usually lasts from a week to a month. Late postpartum depression usually develops several months after pregnancy. Its duration can be different, but more often it lasts more than a month.
Most often, depression appears 30-35 days after birth and in some cases can last up to 1.5-2 years. However, in most cases, a depressive episode ends spontaneously safely 3-6 months after birth. Symptoms of postpartum depression meet the diagnostic criteria for depressive disorder. The patient has a deterioration in mood, a decrease in energy, activity, the ability to rejoice, have fun, a decrease in interests and difficulty in long-term concentration of attention.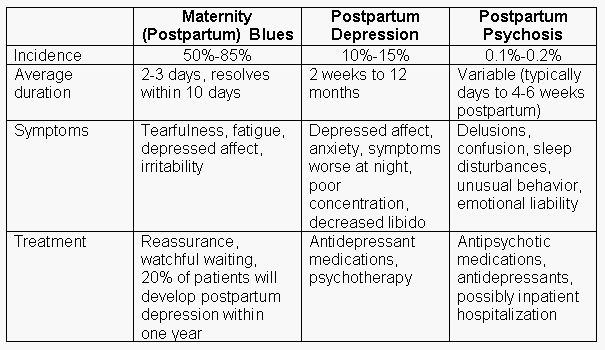 Severe fatigue is common, even after minimal effort. As a rule, sleep is disturbed and appetite worsens. Self-esteem and self-confidence are almost always reduced, even in mild forms of the disease. Often there are thoughts of one's own guilt and worthlessness. Low mood, which varies little from day to day, does not depend on circumstances and may be accompanied by symptoms such as loss of interest in the environment and the loss of sensations that give pleasure. Typical is awakening in the morning several hours earlier than usual, increased depression in the morning, severe psychomotor retardation, anxiety, loss of appetite, weight loss and decreased libido.
Severe fatigue is common, even after minimal effort. As a rule, sleep is disturbed and appetite worsens. Self-esteem and self-confidence are almost always reduced, even in mild forms of the disease. Often there are thoughts of one's own guilt and worthlessness. Low mood, which varies little from day to day, does not depend on circumstances and may be accompanied by symptoms such as loss of interest in the environment and the loss of sensations that give pleasure. Typical is awakening in the morning several hours earlier than usual, increased depression in the morning, severe psychomotor retardation, anxiety, loss of appetite, weight loss and decreased libido.
In most cases, postpartum depression remains unrecognized in the initial period. The most typical example is the prevailing idea of the "natural whims" or character flaws of a woman in labor who turns to her relatives for help instead of actively caring for the child. Loss of initiative and energy or fear of being judged and discussed by others often prevents a woman from seeking medical help.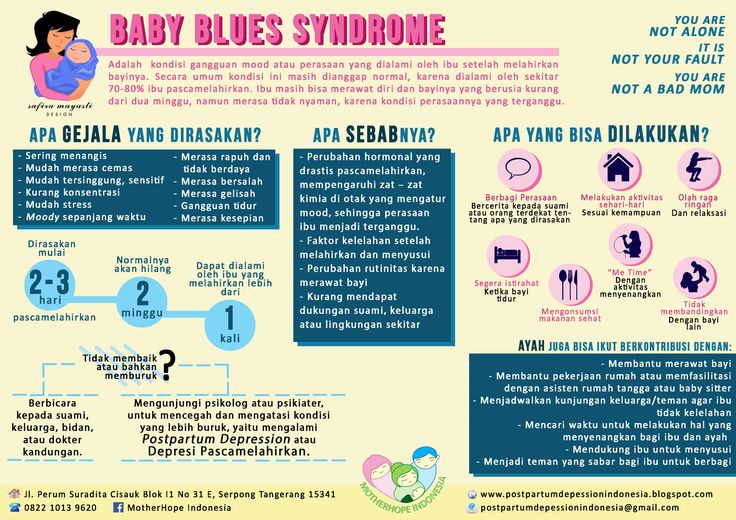 However, even when contacting a doctor, the disease often remains unrecognized, since some doctors tend to consider this condition as a temporary and natural reaction to the stress that childbirth is, especially for primiparas. At the same time, depression can increase over several months, and the treatment of this condition is delayed until there is an indication for emergency hospitalization.
However, even when contacting a doctor, the disease often remains unrecognized, since some doctors tend to consider this condition as a temporary and natural reaction to the stress that childbirth is, especially for primiparas. At the same time, depression can increase over several months, and the treatment of this condition is delayed until there is an indication for emergency hospitalization.
<< First < Previous 1 2 3 4 5 6 7 Next > Last >>
Treatment of postpartum depression in St. Petersburg
- Psychiatry
- Treatment of severe depression
- Postpartum depression
Due to natural causes, about 15% of new mothers are prone to postpartum depression. As a rule, the pathological condition becomes apparent to others already 4–5 days after birth. However, in some cases, the disease makes itself felt much later - the first symptoms may appear at a distance of up to 1 year.
As a rule, the pathological condition becomes apparent to others already 4–5 days after birth. However, in some cases, the disease makes itself felt much later - the first symptoms may appear at a distance of up to 1 year.
Treatment of postpartum depression in St. Petersburg is carried out on an outpatient basis or in a hospital clinic. Self-administration of sedatives during this important period for mother and child is categorically contraindicated.
If a new mother has a long-term bad mood, tearfulness, strange statements (for example, suicidal nature), or there are suspicions of hallucinations, a psychiatrist should be sought. It is important to understand that only a doctor can choose drugs that are safe for the health of a young mother and child, taking into account the characteristics of the current state of health and the severity of the mental disorder.
Typically, treatment for postpartum depression in a hospital does not take longer than 2-4 weeks. After discharge from the hospital, one should follow the recommendations of the attending physician and attend follow-up consultations necessary to correct treatment and withdraw from pharmacotherapy.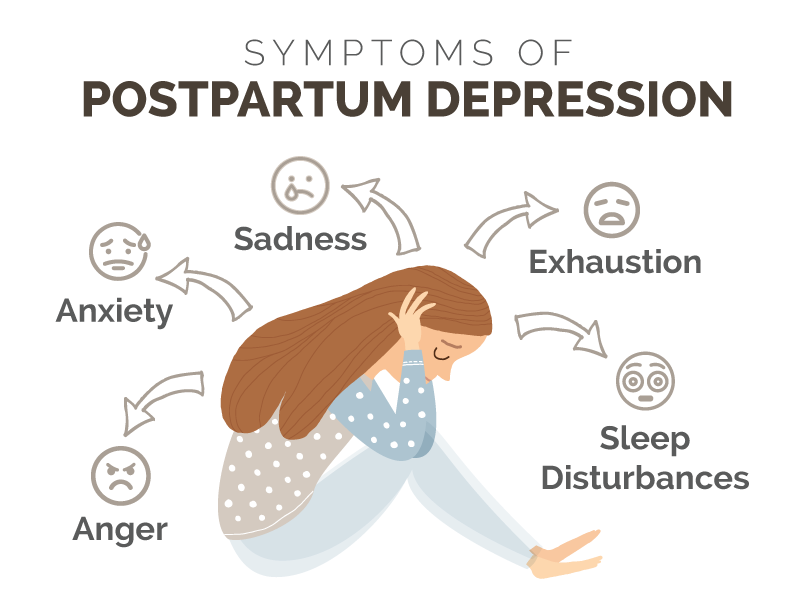
Quiz: Beck Depression Scale
In each group, identify the one statement that best fits how you felt this week and today. Before making your choice, make sure you read all of the statements in each group.
Doctor's consultation on the treatment of postpartum depression:
+7 (812) 407-18-00
Thank you for your trust!
- Anonymous treatment
- Accommodation in a room with a relative
- Post-discharge management
| Service | Price | |
|---|---|---|
| Psychotherapist appointment | 5 000 ₽ | |
| Family Therapy | 10 000 ₽ | |
| Psychiatric consultation | 5 000 ₽ | |
| Treatment of an exacerbation in a hospital | 8 900 ₽ | |
Reception of the chief physician Bocharov A. V. (Ph.D., Associate Professor) V. (Ph.D., Associate Professor) | 6 000 ₽ |
Predisposition to the disease
Causes of postpartum depression
Symptoms and signs of postpartum depression
When is postpartum depression diagnosed? Exercise therapy, phototherapy, various types of massage, acupuncture, and omega-3 fatty acids may also help.
In order to accurately diagnose postpartum depression, your doctor will need to run a series of tests.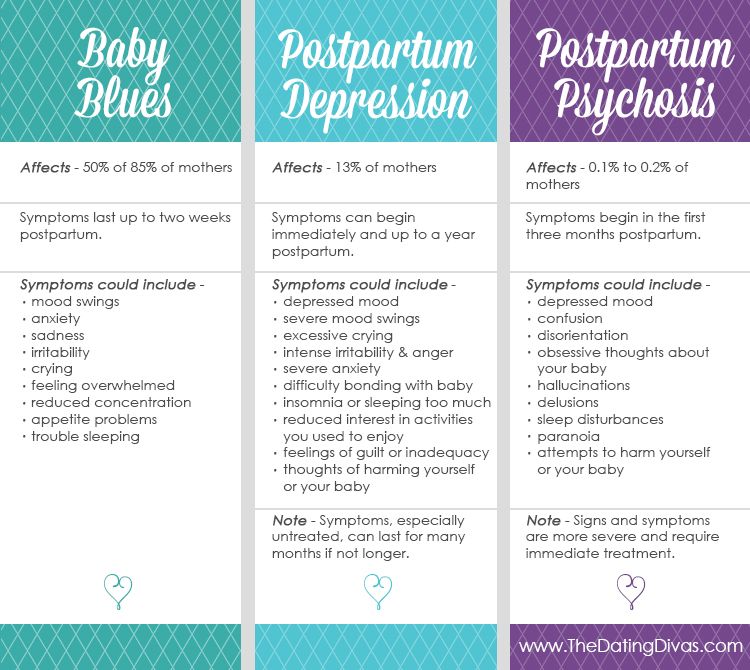 Many women experience fatigue, decreased mood and loss of energy after the birth of a child, but these signs do not always indicate depression.
Many women experience fatigue, decreased mood and loss of energy after the birth of a child, but these signs do not always indicate depression.
PPD is a well-known mental disorder, so it is usually recognized and treated with certainty. It may differ from case to case.
Standard care:
- support group;
- sessions with a psychologist or psychotherapist - conducted personally;
- taking drugs prescribed by a doctor.
If a woman has postpartum depression, then the likelihood of its recurrence in the next pregnancy increases. As a rule, PRD occurs at the second birth; however, if depression is detected at an early stage, the effectiveness of the treatment of postpartum depression is greatly increased.
Depending on how severe the depression is, doctors differentiate between psychotherapy and medication. In mild cases, the patient is allowed to choose the therapy, otherwise they are inclined to the second method. Antidepressants are usually prescribed, of which SSRIs are especially effective (no drowsiness, ankliolytic effect, good tolerance of the drug components).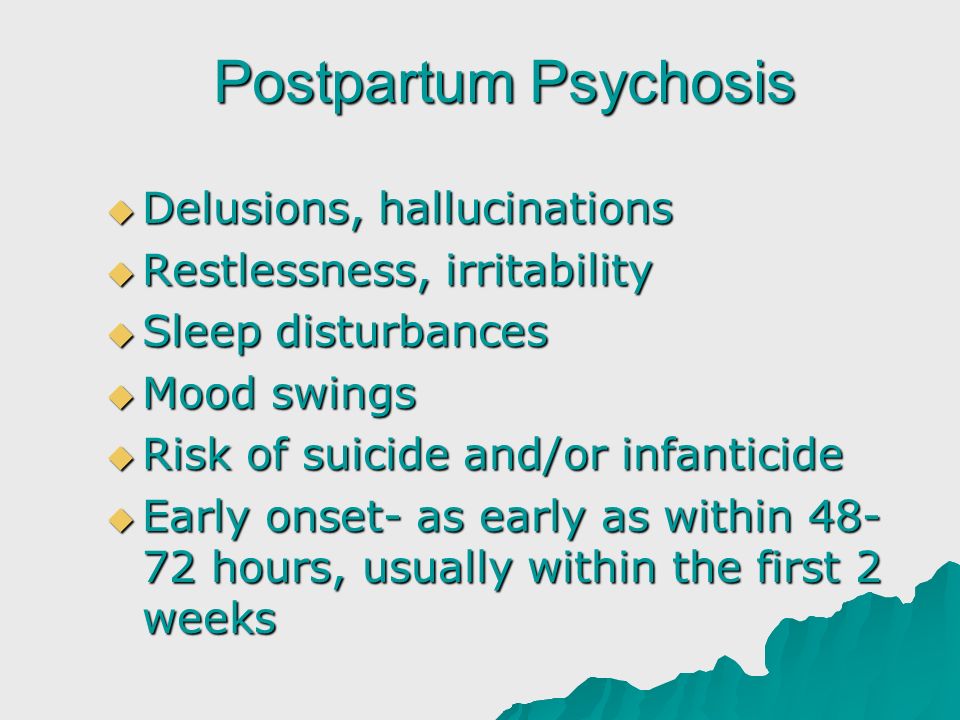 The choice of drugs is determined by the individual indicators of the woman (contraindications, tolerability). Shows good results and group therapy: members of such a service talk about postpartum depression and teach how to deal with it. The doctor should definitely find out if the woman has support in the family - interpersonal psychological therapy is used as a substitute for medications or an additional treatment for postpartum depression.
The choice of drugs is determined by the individual indicators of the woman (contraindications, tolerability). Shows good results and group therapy: members of such a service talk about postpartum depression and teach how to deal with it. The doctor should definitely find out if the woman has support in the family - interpersonal psychological therapy is used as a substitute for medications or an additional treatment for postpartum depression.
The difference from other types of depression lies in the fact that even with active treatment of postpartum depression anxiety and anxiety for the child does not disappear - women are still responsible for it. Stress arising from parental obligations and relationships with the baby, therapy is not stopped. However, the effect of treatment on the infant has not been studied.
Antidepressants for postpartum depression
Sources
Diagnostics and modern trends in therapy of postpartum depression - https://pubmed.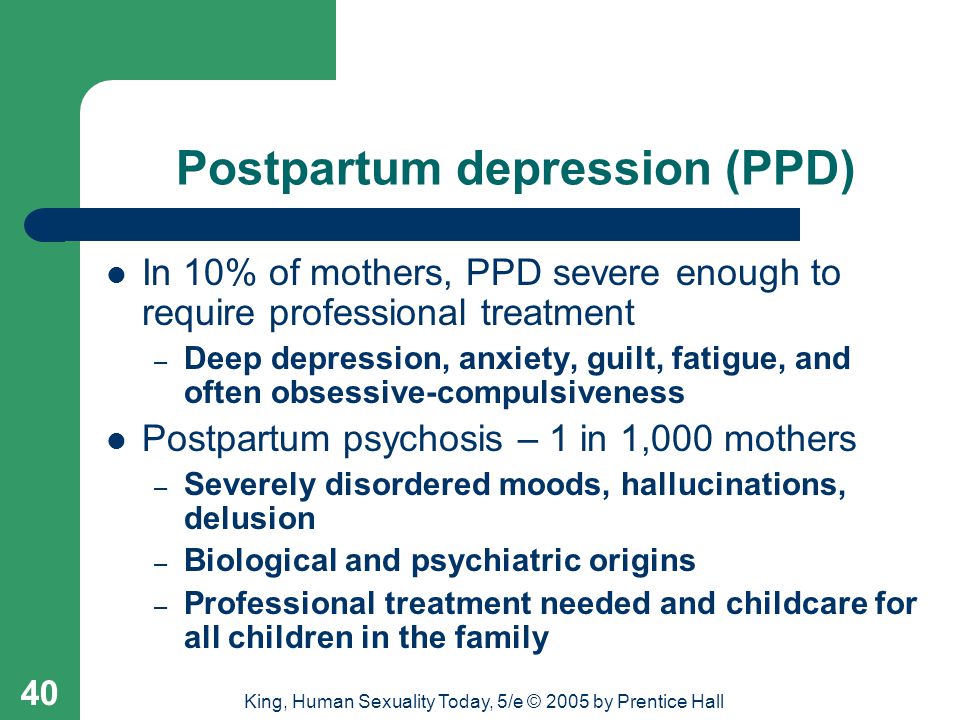 ncbi.nlm.nih.gov
ncbi.nlm.nih.gov
Selection of scales for assessing postpartum depression - https://psychiatr.ru
Peripartum depression ( formerly postpartum) - https://psychiatry.org
Postpartum depression: what you should know - https://www.webmd.com
Update date: 05/16/2022
- Depersonalization and derealization
- Suicidal behavior
- Anxiety disorder
Make an appointment
Date and time: (not set)
Make an appointment with a psychiatrist
Make an appointment with a psychiatrist
Select the date and time of your appointment
Today
02 December
Tomorrow
December 03
Sunday
December 04
Monday
December 05
Tuesday
December 06
Wednesday
December 07
Thursday
December 08
Friday
December 09
Saturday
December 10
Sunday
December 11
Monday
December 12
Tuesday
December 13
Wednesday
December 14
Thursday
December 15
Friday
December 16
Saturday
December 17
Sunday
December 18
Monday
December 19
Tuesday
December 20
Wednesday
December 21
Thursday
December 22
Friday
December 23
Saturday
December 24
Sunday
December 25
Monday
December 26
Tuesday
December 27
Wednesday
December 28
Thursday
December 29
Friday
December 30
Saturday
December 31
Postpartum depression is being treated
Bocharov Alexey
Viktorovich
Psychiatrist, psychotherapist
Head physician of clinic
Experience 41 years
Psychiatrist, psychotherapist, sexologist, child psychiatrist
Work experience 41 years
Sinenchenko Andrey
Georgievich
Psychiatrist, psychotherapist
PhD
Work experience 22 years
Psychiatrist, psychotherapist, narcologist
Work experience 22 years
Zun Sergey
Andreevich
Psychiatrist, narcologist
PhD
Experience 33 years
Psychiatrist, narcologist, psychotherapist
Work experience 33 years
Lisitsyna Elena
Alekseevna
Psychiatrist
Top category
Experience 33 years
Psychiatrist
Work experience 33 years
Buchelnikova Victoria
Viktorovna
Psychiatrist
Head of amb.