What are the odds of getting listeria while pregnant
Listeria from Food Safety for Moms to Be
While You're Pregnant Main Page
What Is Foodborne Illness? | Listeria | Toxoplasma
Spanish (Español)
Listeria: Frequently Asked Questions
"What is Listeria monocytogenes?"
It's a harmful bacterium that can be found in refrigerated, ready-to-eat foods (meat, poultry, seafood, and dairy - unpasteurized milk and milk products or foods made with unpasteurized milk), and produce harvested from soil contaminated with L. monocytogenes. Many animals can carry this bacterium without appearing ill, and thus, it can be found in foods made from animals. L. monocytogenes is unusual because it can grow at refrigerator temperatures where most other foodborne bacteria do not. When eaten, it may cause listeriosis, an illness to which pregnant women and their unborn children are very susceptible.
"How could I get listeriosis?"
By eating ready-to-eat meats, poultry, seafood, and dairy products that are contaminated with L. monocytogenes. You can also get listeriosis by eating contaminated foods processed or packaged in unsanitary conditions or by eating fruits and vegetables that are contaminated from the soil or from manure used as fertilizer.
"How could listeriosis affect me?"
The symptoms can take a few days or even weeks to appear and may include fever, chills, muscle aches, diarrhea or upset stomach, headache, stiff neck, confusion, and loss of balance. In more serious cases, listeriosis could also lead to the mother's death.
Most of the time, pregnant women who are infected with listeriosis don't feel sick. However, they can pass the infection to their unborn babies without even knowing it. That's why prevention of listeriosis is very important. In any case, if you experience any of the above symptoms, see your doctor or healthcare provider immediately.
Facts (Centers for Disease Control and Prevention) /cdn.vox-cdn.com/uploads/chorus_asset/file/1070358/missed_pills.0.png)
"How could listeriosis affect my baby?"
During the first trimester of pregnancy, listeriosis may cause miscarriage. As the pregnancy progresses to third trimester, the mother is more at risk. Listeriosis can also lead to premature labor, the delivery of a low-birth-weight infant, or infant death. Fetuses who have a late infection may develop a wide range of health problems, including intellectual disability, paralysis, seizures, blindness, or impairments of the brain, heart, or kidney. In newborns, L. monocytogenes can cause blood infections and meningitis.
Listeriosis & Pregnant Hispanic Women
Studies show that pregnant Hispanic women may have a higher incidence of listeriosis than pregnant non-Hispanic women. This is most likely because they might make and eat homemade soft cheese and other traditional foods made from unpasteurized milk. "Queso fresco"- a traditional homemade cheese, prepared from unpasteurized milk and widely consumed by Hispanics - has led to miscarriages, death of newborns, and premature delivery caused by L. monocytogenes.
"Queso fresco"- a traditional homemade cheese, prepared from unpasteurized milk and widely consumed by Hispanics - has led to miscarriages, death of newborns, and premature delivery caused by L. monocytogenes.
To prevent the risk of listeriosis, Hispanic pregnant women should not eat homemade soft cheeses and other traditional foods made from unpasteurized milk. Like all other pregnant women, they should follow the food safety precautions outlined below.
"How can I prevent listeriosis?"
The good news is that listeriosis can be prevented! Here's how...
Time to Chill
- Your refrigerator should register at 40° F (4° C) or below and the freezer at 0° F (-18° C). Place a refrigerator thermometer in the refrigerator, and check the temperature periodically. During the automatic defrost cycle, the temperature may temporarily register slightly higher than 40° F. This is okay.
- Refrigerate or freeze perishables, prepared food, and leftovers within two hours of eating or preparation.
 Follow the 2-Hour Rule: Discard food that's left out at room temperature for longer than 2 hours. When temperatures are above 90° F (32° C), discard food after 1 hour.
Follow the 2-Hour Rule: Discard food that's left out at room temperature for longer than 2 hours. When temperatures are above 90° F (32° C), discard food after 1 hour. - Use ready-to-eat, perishable foods, such as dairy, meat, poultry, seafood, and produce, as soon as possible.
Fridge TIPS
- Clean your refrigerator regularly.
- Wipe up spills immediately.
- Clean the inside walls and shelves with hot water and a mild liquid dishwashing detergent; then rinse.
- Once a week, check expiration and "use by" dates, and throw out foods if the date has passed. Follow the recommended storage times for foods.
Refrigerator & Freezer Storage Chart (PDF).
To Eat or Not to Eat?
Don't eat:
- Hot dogs, deli meats, and luncheon meats - unless they're reheated until steaming hot.
- Soft cheeses like Feta, Brie, and Camembert, "blue-veined cheeses," or "queso blanco," "queso fresco," or Panela - unless they're made with pasteurized milk.
 Make sure the label says, "made with pasteurized milk."
Make sure the label says, "made with pasteurized milk." - Refrigerated pâtés or meat spreads.
- Refrigerated smoked seafood - unless it's in a cooked dish, such as a casserole. (Refrigerated smoked seafood, such as salmon, trout, whitefish, cod, tuna, or mackerel is most often labeled as "nova-style," "lox," "kippered," "smoked," or "jerky." These types of fish are found in the refrigerator section or sold at deli counters of grocery stores and delicatessens.)
- Raw (unpasteurized) milk or foods that contain unpasteurized milk.
It's okay to eat:
- Canned or shelf-stable (able to be stored unrefrigerated on the shelf) pâtés and meat spreads.
- Canned or shelf-stable smoked seafood.
- Pasteurized milk or foods that contain pasteurized milk.
Note: See your doctor or healthcare provider if you have questions about listeriosis.
>
Listeriosis During Pregnancy
Pregnant women are told time and again: Don’t eat raw meat, avoid unpasteurized cheese, steer clear of deli counter salads. Why? You can largely blame listeriosis, a foodborne illness that doesn’t pose much risk for mom but can be harmful for baby. Find out what causes listeriosis, what your odds are of contracting it and the steps you can take to prevent it.
Why? You can largely blame listeriosis, a foodborne illness that doesn’t pose much risk for mom but can be harmful for baby. Find out what causes listeriosis, what your odds are of contracting it and the steps you can take to prevent it.
What Is Listeriosis?
Technically speaking, listeriosis is an infection caused by Listeria monocytogenes bacteria. Practically speaking, listeriosis is a type of food poisoning that can cause pregnancy complications.
Listeria bacteria are found in soil, water and sewage, but they can also contaminate food—so if you eat something that’s been contaminated with listeria, you can develop listeriosis. The listeria bacteria is killed with heating and pasteurization, so listeriosis is usually linked to eating uncooked meats or vegetables, raw or unpasteurized milk products, or processed foods (such as hot dogs and deli meat) that become contaminated after being cooked at the food processing facility.
Listeriosis can make people feel sick, but rarely causes severe health problems. What’s scary for moms-to-be, however, is that having it during pregnancy increases the risk of miscarriage, stillbirth and preterm birth. Babies of moms who had listeriosis during pregnancy are also at risk for listeria infection.
What’s scary for moms-to-be, however, is that having it during pregnancy increases the risk of miscarriage, stillbirth and preterm birth. Babies of moms who had listeriosis during pregnancy are also at risk for listeria infection.
How Common Is Listeriosis During Pregnancy?
Wondering what are the odds of getting listeriosis while pregnant? Good news—they’re very low. It’s true that pregnant women have an increased risk of contracting listeriosis, but the real risk is still tiny. According to the Centers for Disease Control and Prevention (CDC), there are approximately 1,600 cases of listeriosis in the United States each year. But only about one in seven cases—or about 200 cases per year—occur in pregnant women, out of nearly 4 million pregnancies every year.
“You’re much more likely to step outside and slip on ice on your front steps in the winter than you are to contract listeria,” says Kelly Kasper, MD, ob-gyn and associate clinical professor at the Indiana University School of Medicine.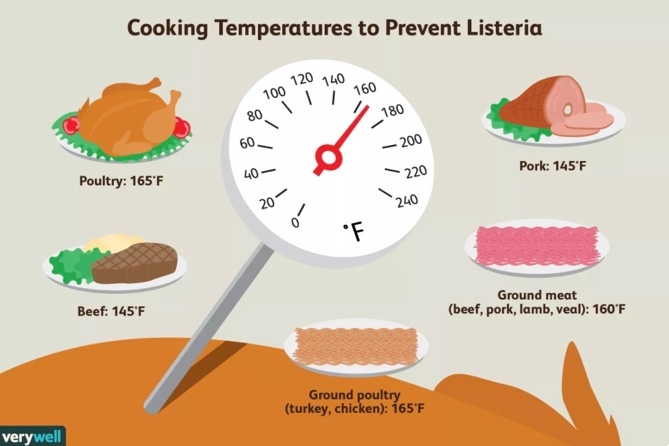 And if you do get listeria, baby might not— transmission of listeriosis from mom to baby is not a sure thing. Plus, listeria infections are easily treatable with antibiotics.
And if you do get listeria, baby might not— transmission of listeriosis from mom to baby is not a sure thing. Plus, listeria infections are easily treatable with antibiotics.
How Do You Know If You Have Listeriosis?
“The symptoms of a listeria infection look a lot like a cold or mild flu,” Kasper says. “The most common symptom is a fever. You might also have muscle aches or a sore throat.” Some people also have diarrhea.
Because the symptoms are so nonspecific, it’s impossible to tell if you have listeriosis solely based on symptoms. That’s why doctors tell pregnant women to contact their health care provider if they’re running a fever—not because they’re always worried about listeriosis, but because fever is a symptom of all kinds of ailments, many of which should be diagnosed and treated right away. The only way to figure out if your symptoms pose a threat to you or baby is to have them checked out by a qualified health care provider.
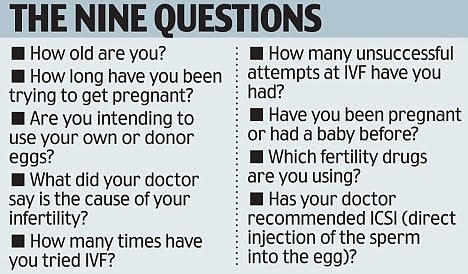
So how do you test for listeria in pregnancy? If your doctor suspects listeriosis—if you have symptoms of listeriosis and have recently eaten some suspect food, for instance—she can order a simple blood test to determine if you have listeriosis or not.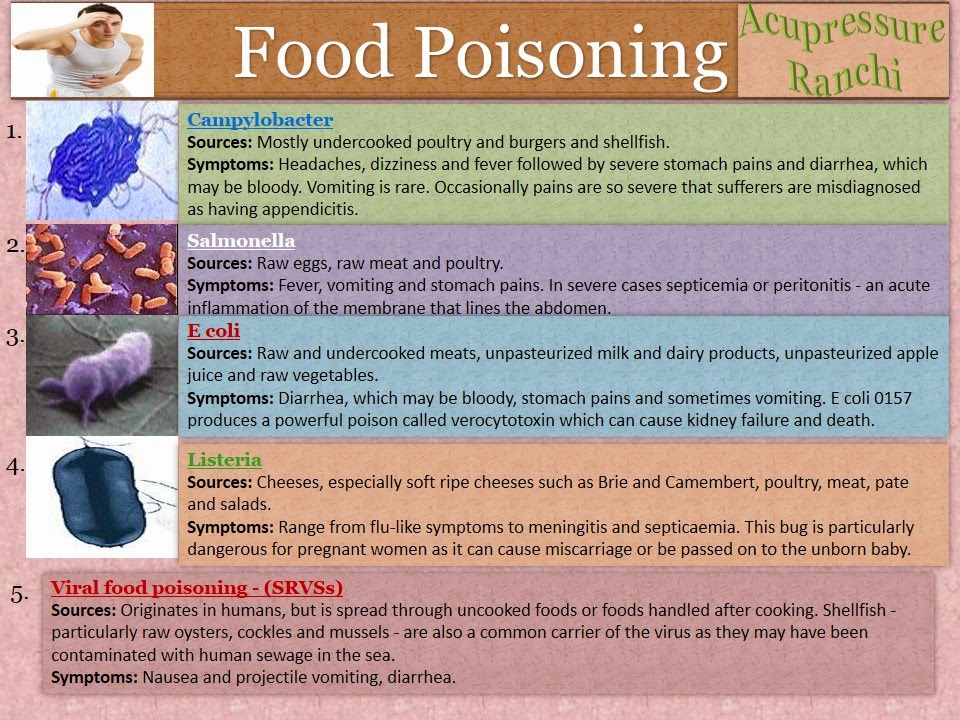
How Does Listeriosis Affect Baby?
Listeriosis increases the risk of miscarriage, stillbirth, preterm delivery and listeriosis infection once baby is born, but the odds of anything bad happening to baby are slim. Here’s why:
• Listeria infection can spread from mom to baby through the placenta, but it’s not a sure thing. So even if you get listeriosis, baby might not. The antibiotics used to treat listeriosis during pregnancy can prevent infection of the fetus.
• Antibiotics can also be used to treat (and prevent complications of) listeriosis in newborns. While listeriosis in babies can cause severe blood infections, meningitis, pneumonia and even death, treatment with antibiotics can resolve the infection and usually prevent complications.
How To Prevent Listeriosis During Pregnancy
If you want to decrease your risk of getting listeriosis to almost zero, you can follow the official listeriosis prevention guidelines and avoid eating the following during pregnancy:
- Unpasteurized soft cheeses
- Refrigerated smoked seafood
- Raw or unpasteurized milk products
- Cold (or room temp) deli meats or hot dogs (they’re fine if they’re heated to steaming hot)
- Prepared deli counter salads, such as egg salad, tuna salad and seafood salad
Or you can take a slightly more relaxed approach. Given the extreme improbability of contracting listeriosis from properly handled foods, Kasper suggests eating food you’ve prepared yourself and following common sense guidelines when you prep and store it:
Given the extreme improbability of contracting listeriosis from properly handled foods, Kasper suggests eating food you’ve prepared yourself and following common sense guidelines when you prep and store it:
• Store foods safely. Make sure your refrigerator is set to 40 degrees Fahrenheit or below, and return items to the fridge as soon as possible after using. Don’t let foods sit out for long periods at room temperature.
• Wash fruits and vegetables. Rinse any raw produce thoroughly under running tap water before eating.
• Pay attention to expiration dates. If your lunch meat is past its expiration date (or if it smells or looks funny), throw it away.
“You want to be smart about listeria and keep yourself healthy. But at the same time, you don’t want to quit living,” Kasper says. “There are some things that we know are very important, common and threatening to a pregnancy, like influenza—that’s why we recommend the flu shot.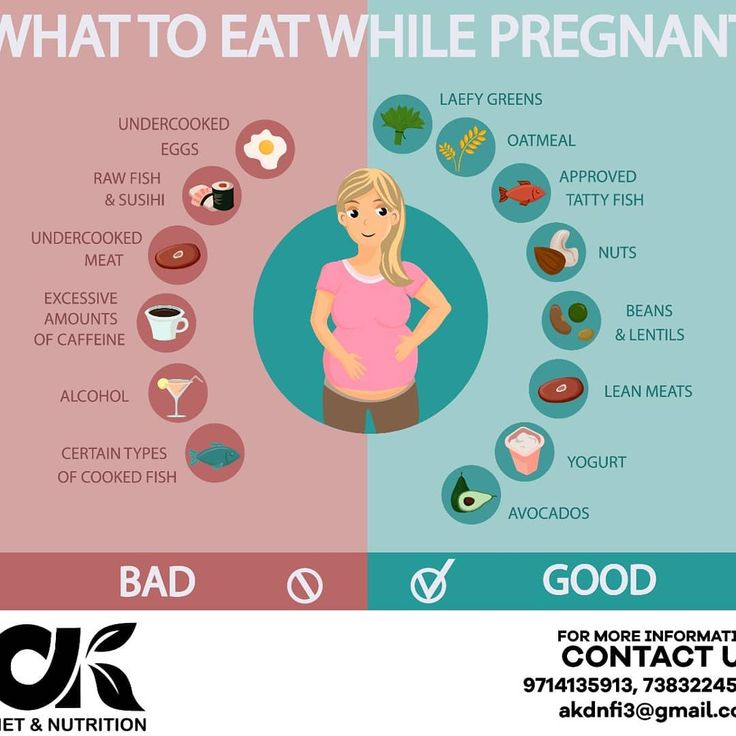 Listeriosis is very uncommon. You don’t have to put yourself in a plastic bubble because you’re afraid of what might happen.”
Listeriosis is very uncommon. You don’t have to put yourself in a plastic bubble because you’re afraid of what might happen.”
What do you do if you have listeriosis? Oral antibiotics can effectively treat listeriosis during pregnancy. Taking the antibiotics can help baby as well. Research shows that treating moms-to-be with high doses of antibiotics during pregnancy decreases the incidence of listeriosis-related preterm births and stillbirths.
Stories From Moms-To-Be Who Have Had Listeriosis
“I know it’s rare but my doula ate a sub and she got so sick from listeriosis she went into labor. Thankfully she was full term. My OB is very strict about [sticking to safe foods]. That says something about the potential dangers. Something to keep in mind—to me [eating certain foods is] not worth the risk.”
“A friend of mine had listeriosis during her first pregnancy—the baby was okay!—and from what she told me, it was constant, uncontrollable vomiting. She said she was puking every five minutes, for a good hour or so. Poor thing!”
Poor thing!”
“A woman who goes to my OB practice did get listeriosis while I was pregnant with my first child and it did not have a good outcome. Even the doctors in the practice were shocked because it is so rare.”
Expert source: Kelly Kasper, MD, ob-gyn and associate clinical professor at the Indiana University School of Medicine.
Please note: The Bump and the materials and information it contains are not intended to, and do not constitute, medical or other health advice or diagnosis and should not be used as such. You should always consult with a qualified physician or health professional about your specific circumstances.
Listeriosis in Pregnancy: Symptoms, Causes and Risks
od Oscar
contents
Listeria monocytogenes (Listeria) is a type of bacteria that causes an infection called listeriosis. The bacterium is found in:
- TLO
- prashina
- water
- processed food
- raw meat
- animal faeces
Most cases of listeriosis are caused by eating food contaminated with bacteria.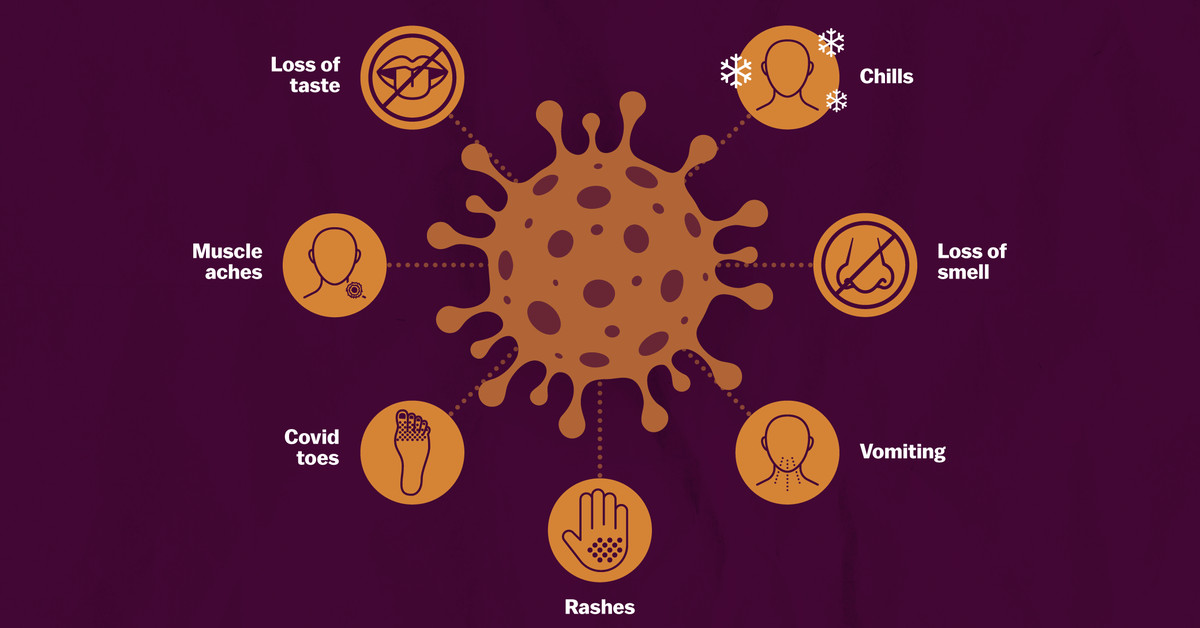 For most people, listeriosis causes only mild illness. However, it can lead to much more serious illness in unborn children or newborns if the mother is infected during pregnancy. Fetal infection can lead to miscarriage or stillbirth. Infection of a newborn can lead to pneumonia and death. For this reason, prevention of listeriosis during pregnancy is extremely important.
For most people, listeriosis causes only mild illness. However, it can lead to much more serious illness in unborn children or newborns if the mother is infected during pregnancy. Fetal infection can lead to miscarriage or stillbirth. Infection of a newborn can lead to pneumonia and death. For this reason, prevention of listeriosis during pregnancy is extremely important.
Pregnant women should avoid certain foods such as hot dogs, meats and soft cheeses to reduce their risk. Understanding food preparation methods and following food safety practices can also help prevent this infection.
In healthy adults who are not pregnant, eating foods contaminated with Listeria usually does not cause problems. Listeriosis is rare in healthy adults who are not pregnant, but the infection is 20 times more common in pregnant women. preliminary in obstetrics and gynecology. Most pregnant women do not have any symptoms or problems with the infection. However, the fetus is very sensitive to this type of bacteria. The infection can spread to and through the placenta. A listeriosis infection, known as listeriosis, is severe and often fatal for a child.
The infection can spread to and through the placenta. A listeriosis infection, known as listeriosis, is severe and often fatal for a child.
Symptoms may appear two days or two months after contact with bacteria. Healthy adults who are not pregnant usually show no symptoms at all.
Symptoms in pregnancy may be similar to flu or cold symptoms. These may include:
- fever
- headaches
- muscle pain
- chills
- nausea
- vomiting
- neck stiffness confusion
Be sure to see your doctor if you are pregnant and experience any of these symptoms. Sometimes a pregnant woman infected with listeriosis does not feel very ill. However, she can still pass the infection on to her unborn child without being aware of it.
Listeriosis is an infection caused by eating food contaminated with Listeria monocytogenes. Bacteria are commonly found in water, soil and animals. Vegetables can be contaminated from the soil. It can also be found in lean meats and unpasteurized dairy products, as animals often carry the bacteria, although they don't get it. Listeria is killed by cooking and pasteurization (the process of heating a liquid to a high temperature to kill germs).
It can also be found in lean meats and unpasteurized dairy products, as animals often carry the bacteria, although they don't get it. Listeria is killed by cooking and pasteurization (the process of heating a liquid to a high temperature to kill germs).
This bacterium is unusual because it grows well at the same temperature as your refrigerator. People usually become infected with listeriosis by eating the following contaminated foods:
- cooked meat, fish and poultry
- unpasteurized dairy products
- soft cheese products
- fruits and vegetables contaminated with soil or manure used as fertilizer
- food packaged in unsanitary conditions
Women with certain conditions have a slightly higher risk of infection. These include the following conditions:
Crops can take up to two days to grow. Since this is very serious for a child, your doctor may start treatment for listeriosis before it shows results.
If you are pregnant and sick with leaferiosis, you are subjected to increased risk:
- Pereti
- Nationalities
- Premature birth
- Give children with a low body weight at birth
- Death for the fetus
in some cases can be infected in some cases complications in pregnancy, including:
Listeria infection is often serious in infants.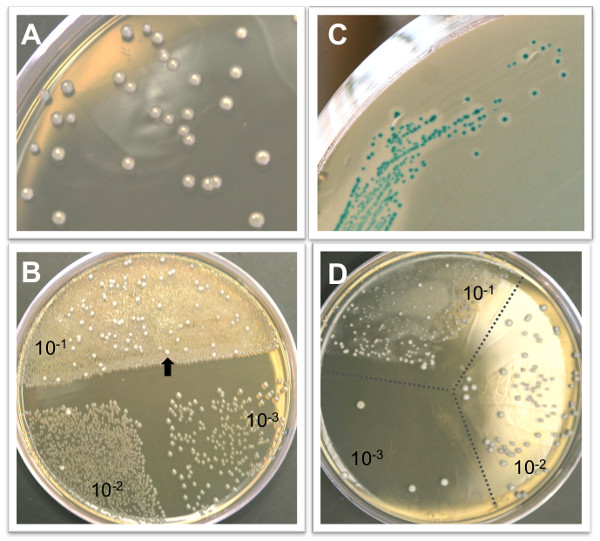 Its mortality rate is 20 to 30 percent. preliminary in obstetrics and gynecology. Early antibiotic treatment helps prevent fetal infection and other serious complications. Not all children whose mothers are infected will have problems.
Its mortality rate is 20 to 30 percent. preliminary in obstetrics and gynecology. Early antibiotic treatment helps prevent fetal infection and other serious complications. Not all children whose mothers are infected will have problems.
The key to preventing listeriosis infection during pregnancy is to follow the guidelines he recommends. Centers for Disease Control and Prevention (CDC). The organization recommends not eating foods with a high risk of listeria infection during pregnancy.
Avoid the following:
- hot dogs, luncheon meats, or cold cuts served cold or warmed to less than 165°F. Not recommended in restaurants that serve meat sandwiches.
- chilled meat spreads
- cooked meat "rare"
- raw product that has not been thoroughly washed
- raw (unpasteurized) milk
- cold-smoked seafood
- unpasteurized soft cheeses and brifetas. Hard cheeses such as cheddar and semi-hard cheeses such as mozzarella can be eaten, as well as pasteurized spreads such as cream cheese.

It is also important to follow food safety and handling regulations. This includes:
- Wash fruits and vegetables thoroughly in clean water, even if the skins are peeled.
- Cleaning company produces clean brush like melons and cucumbers.
- Read ingredient labels.
- Check expiration dates.
- Wash your hands frequently.
- Keep kitchen work surfaces clean.
- Keep your refrigerator at 40°F or below.
- Clean your refrigerator frequently.
- Cook food at the correct temperature. You should buy food thermometers to make sure food is cooked or heated to at least 160°F.
- Refrigerate or freeze perishable or prepared foods and leftovers within two hours of cooking; otherwise throw them away.
The United States Department of Agriculture (USDA) and the Food and Drug Administration (FDA) also conduct routine inspections and surveillance of potential sources of food contamination. They will remember all prepared chicken, pork and seafood products in the US if there are any differences due to contamination.
They will remember all prepared chicken, pork and seafood products in the US if there are any differences due to contamination.
After all, Listeria is so common that it can't always be prevented. Pregnant women should call their doctor if they have any of the common symptoms.
Pregnancy and childbirth with HIV
Pregnancy and childbirth are often associated with many questions and concerns. When pregnancy occurs against the background of HIV infection, there are even more questions.
First and foremost, if a woman with HIV finds out about her pregnancy, or a girl finds out about her positive HIV status and pregnancy at the same time, then you should contact the AntiAIDS Center as soon as possible!
Taking ARVs can conceive, bear and give birth to a healthy baby! The risk of transmitting HIV to him will be minimal. This is true for discordant couples (when only one of the partners is living with HIV) and when both partners are HIV positive. It is important to take ART correctly and achieve an undetectable viral load in the mother, as well as apply other preventive measures.
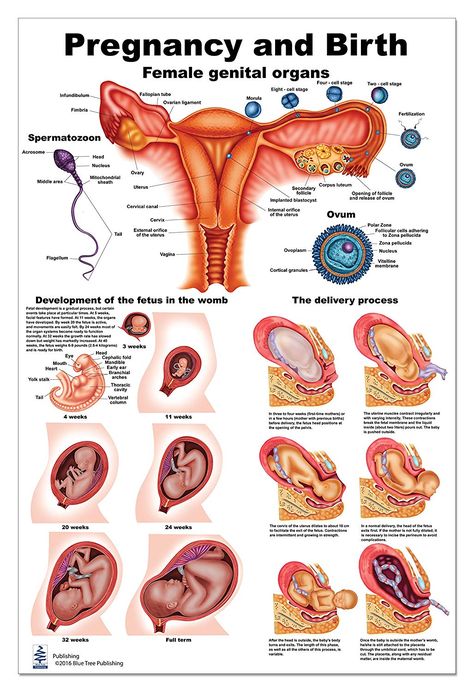
How can HIV be transmitted from mother to child? It can be transmitted through blood, vaginal secretions and breast milk. The risk of intrauterine transmission increases in late pregnancy and during childbirth. During childbirth, the child comes into contact with the mother's blood and vaginal discharge, from which the virus can enter the child's body through microtraumas on the child's skin.
HIV does not cross the placenta well and is rarely transmitted during early pregnancy. If at the time of conception a woman did not take ARVT, this does not mean that the child will be infected. But it is important to start taking ART as early as possible in order to achieve an undetectable viral load by late pregnancy and childbirth. And breastfeeding will need to be abandoned completely, even when taking ART.
Is pregnancy safe for a mother with HIV? With the right ARV therapy, pregnancy will be almost indistinguishable from pregnancy with HIV-negative status.
For discordant couples, where only one parent is HIV positive, there are special recommendations.
If the mother is HIV-negative and the father is HIV-positive, conception will carry the risk of infection for the mother. Sustained suppression of the viral load in the father is a prerequisite for conceiving a child. To eliminate the risk of infection of the mother, it is necessary to resort to the following methods:
- Semen purification. Viral particles are found only in the seminal fluid, but not in the spermatozoa themselves. Therefore, it is possible to separate the spermatozoa from the seminal fluid, test them for the absence of viral particles, and then insert them into the vagina.
- IVF (in vitro fertilization). In this case, the mother's egg is fertilized with purified father's sperm "in vitro" and then the resulting embryo is implanted in the uterus.
In almost 100% of cases, when using these methods, the risk of infection, both mother and child, is eliminated.
If the mother is HIV-positive and the father is HIV-negative, then the safest way is to inject semen into the vagina using an ordinary plastic syringe without a needle. It can be collected using a condom (no spermicidal lubricant) or a clean plastic biomaterial container. The collected sperm is injected with a syringe deep into the vagina on the days of ovulation. The risk of infection for the father is completely absent.
How safe is ARV therapy during pregnancy? ARV therapy is very important for the birth of a healthy baby. But expectant mothers may have questions about how safe it is during pregnancy.
Modern antiretroviral therapy has a very good safety profile for both mother and child. After numerous clinical studies, many ARV drugs have been proven safe - they do not affect the growth and development of the child and do not threaten the normal course of pregnancy.
The doctor always selects a specific regimen, taking into account other features of the mother's health and the course of pregnancy. Nevertheless, it is important for the expectant mother to carefully monitor her condition, regularly take prescribed tests and visit a doctor!
Nevertheless, it is important for the expectant mother to carefully monitor her condition, regularly take prescribed tests and visit a doctor!
When should I start ART? If a woman was not taking ART before pregnancy, it is usually started at 13–14 weeks of gestation. By this time, the formation of the main organs of the fetus is completed, and the risks of influencing the development of the child become minimal. But, if the mother has a very low CD4 count or a very high viral load, therapy is started immediately.
It is dangerous to delay the start of therapy beyond the 14th week. To protect the baby from HIV infection, a sustained low maternal viral load must be achieved by the time of birth. If it was not possible to start therapy in a timely manner, it should be done in any case, as soon as such an opportunity arises.
If you are already taking antiretroviral drugs and are planning a pregnancy, be sure to discuss this with your doctor! The doctor may suggest changing the regimen. It may turn out that your regimen already consists of drugs that are allowed during pregnancy, then nothing will have to be changed.
It may turn out that your regimen already consists of drugs that are allowed during pregnancy, then nothing will have to be changed.
If a regimen does need to be changed, it is safest to first ensure that the new regimen is well tolerated and produces sustained viral load suppression and then plan pregnancy. This usually becomes clear within 1-3 months of starting a new regimen.
Is there a need for special prevention of HIV transmission to the child after childbirth?
Prevention by taking ART. Babies born to mothers with HIV, regardless of the mother's viral load at the time of birth, are usually given prophylactic ARVs for several weeks. Therapy begins immediately after childbirth, the scheme and dosage is selected by the doctor individually.
Breastfeeding should be completely avoided. HIV is found in breast milk, and can also be transmitted to a child through microtrauma and cracked nipples. You can’t apply a baby to an empty breast either - even when there is no milk, the risk of transmitting the virus through microcracks in the nipple remains. You can't feed with expressed milk either.
You can't feed with expressed milk either.
If a mother is diagnosed with HIV already during breastfeeding, it should be discontinued. The child is prescribed a prophylactic course of antiretroviral drugs and is tested for HIV infection.
When can you know for sure that HIV infection has not been passed on to a child? Children are tested by PCR - it allows you to detect virus RNA in the blood. PCR is usually performed in the first two days after birth, then a month later, and then another three months later. Maternal antibodies completely disappear from the child's blood by 18 months - at this age, ELISA is done.
A negative PCR result on the second day after delivery indicates that the baby was NOT infected during pregnancy. A negative PCR after one month indicates that the baby most likely did NOT become infected during delivery. A negative PCR after 4 months of age indicates that the child is almost certainly NOT infected with HIV. The final confirmation of this is a negative ELISA result at 1.