Nausea burping pregnancy
Heartburn & Upset Stomach During Pregnancy
%PDF-1.4 % 1 0 obj /Producer(Adobe PDF Library 16.0.7)/Subject(Heartburn & Upset Stomach During Pregnancy)/Title(Heartburn & Upset Stomach During Pregnancy)/Trapped/False>> endobj 2 0 obj /MarkInfo>/Metadata 7 0 R/Names 8 0 R/Outlines 10 0 R/PageLayout/SinglePage/Pages 11 0 R/StructTreeRoot 109 0 R/Type/Catalog/ViewerPreferences>>> endobj 3 0 obj >/Font>>>/Fields[]>> endobj 4 0 obj > endobj 5 0 obj > endobj 6 0 obj > endobj 7 0 obj >stream application/pdf
Indigestion and heartburn in pregnancy
Indigestion and heartburn in pregnancy | Pregnancy Birth and Baby beginning of content3-minute read
Listen
Many women experience indigestion and heartburn while they are pregnant, which can be painful or uncomfortable. There are ways to help avoid or treat indigestion and heartburn, especially if it is mild. Sometimes the feeling of heartburn can be confused with a more serious condition called pre-eclampsia.
There are ways to help avoid or treat indigestion and heartburn, especially if it is mild. Sometimes the feeling of heartburn can be confused with a more serious condition called pre-eclampsia.
Indigestion, also called 'dyspepsia', is a feeling of pain or discomfort in the stomach (upper abdomen, or, tummy). This mostly occurs after eating or drinking but can happen some time after.
If you have indigestion in the early stage of your pregnancy, this may be caused by changes in your hormone levels. In the second or third trimester, indigestion becomes more common and may be caused by your baby pushing up against your stomach. As many as 8 in 10 women may have indigestion during their pregnancy.
Symptoms of indigestion may include:
- heartburn
- reflux or regurgitation (food coming back up from your stomach)
- burping
- feeling heavy, bloated or full
- feeling sick
- vomiting
Heartburn is a burning pain in the throat or chest, behind the breastbone, caused by stomach acid coming up the oesophagus (the tube that connects your mouth to your stomach) and irritating the lining.
In pregnant women, indigestion and heartburn can be caused by:
- eating a big meal
- eating high-fat foods
- eating chocolate or peppermint
- drinking fruit juice or caffeinated beverages (coffee, tea, cola drinks)
- doing physical activity soon after eating
- bending over
- feeling anxious
It's a good idea to take note of the particular foods, drinks or activities that give you indigestion while you are pregnant.
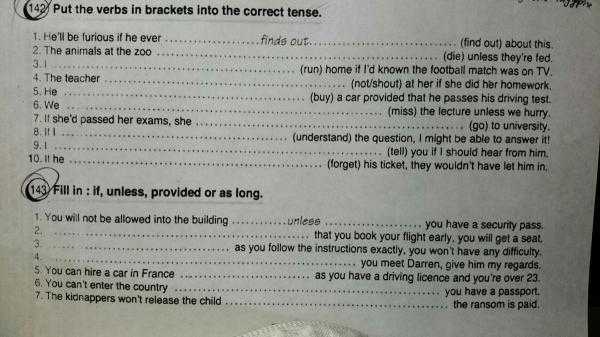
Avoiding indigestion and heartburn
If your symptoms are mild, it's possible that changes to your diet or lifestyle may help prevent indigestion and heartburn. You could try:
- eating smaller meals, more often
- avoiding eating just before bed
- avoiding foods and drinks that you suspect give you heartburn
- not drinking a lot of coffee at the end of the day
- avoiding eating and drinking at the same time, which can make your stomach more full
- sitting up straight while eating, and not lying down after a meal
- chewing gum, which may cause you to produce more saliva to help neutralise the acid
- stop smoking
- raise the head of your bed by 10 to 15cm
- sleep on your left side
If your indigestion is not helped by diet and lifestyle changes, or your symptoms are more severe, your doctor or midwife may suggest that you take a medicine for indigestion that is safe to use during pregnancy. Medicines can neutralise the acid in your stomach, reduce the amount of acid produced by your stomach and stop the acid rising into your oesophagus.
Medicines can neutralise the acid in your stomach, reduce the amount of acid produced by your stomach and stop the acid rising into your oesophagus.
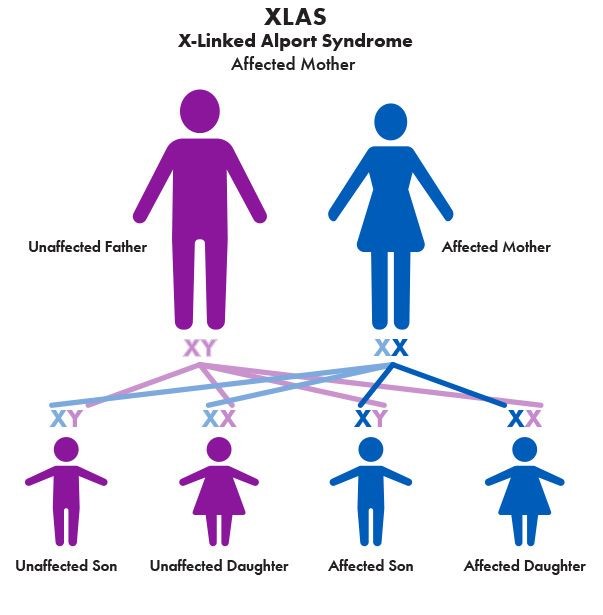
Heartburn symptoms and pre-eclampsia
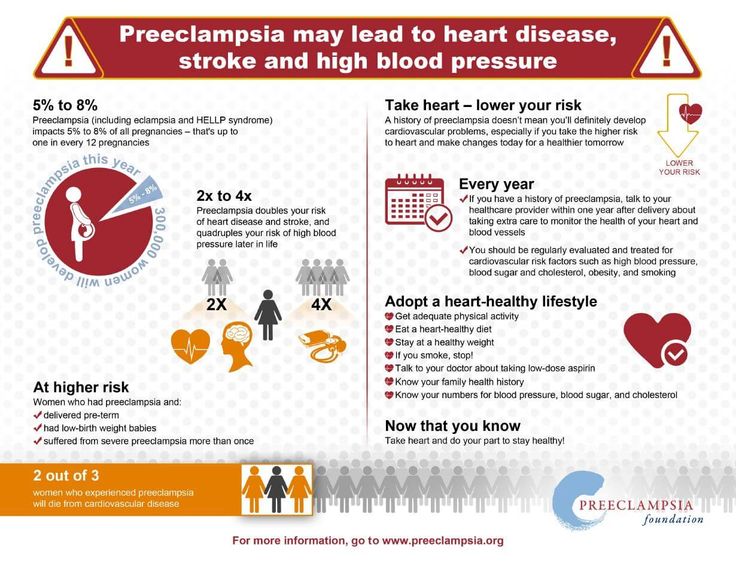
If your heartburn symptoms don't go away with medicine, it's important to see your doctor as it may be a sign of something more serious, such as pre-eclampsia. A pregnant woman with pre-eclampsia usually has high blood pressure and problems with her kidneys. Pre-eclampsia could also seriously affect a woman's liver, blood and brain. Any pregnant woman can experience pre-eclampsia – almost 1 in 20 Australian women will develop it.
Because pre-eclampsia is dangerous for both you and your baby, you should let your doctor know if your heartburn medicine is not working. This is especially important if you're also feeling very unwell or you have:
- sudden swelling of your hands, feet or face
- a headache that doesn't go away with simple painkillers
- problems with your eyesight such as blurring or seeing flashing lights or dots
- a strong pain below your ribs
Find out more about how pre-eclampsia is treated here.
Call Pregnancy, Birth and Baby on 1800 882 436 to speak to a maternal child health nurse.
Sources:
Royal Australian and New Zealand College of Obstetricians and Gynaecologists (Pre-eclampsia and high blood pressure during pregnancy), Gastroenterological Society of Australia (Heartburn - Oesophageal Reflux), Gastroenterological Society of Australia (Heartburn - Reflux), King Edward Memorial Hospital (Minor symptoms or disorders in pregnancy), Raising Children Network (Health problems in pregnancy), Royal Australian and New Zealand College of Obstetricians and Gynaecologists (Antenatal care during pregnancy), Department of Health (Clinical Practice Guidelines: Pregnancy Care), Mater Mothers Hospital (Pregnancy information for women and families)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: May 2020
Back To Top
Related pages
- Pre-eclampsia
- Common discomforts during pregnancy
Need further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Belching during pregnancy - causes, diagnosis and treatment
Belching during pregnancy is the release of gastric gases in a pregnant woman with a characteristic sound, which occurs due to contraction of the smooth muscles of the stomach with an open cardiac sphincter. The symptom is more often caused by physiological causes: hormonal changes, errors in diet, physical inactivity, but may also indicate the presence of a disease. To identify the root cause of erection during gestation, safe studies are prescribed - ultrasound, tests, pH-metry. To reduce belching, non-drug methods, prokinetics, and sedatives are used.
Causes of belching during pregnancy
During normal pregnancy
The release of a small amount of air through the oral cavity is a physiological process that is observed in absolutely healthy people. During the bearing of a child in a woman's body, changes occur in various organs and systems that can affect the frequency of belching. Physiological erection is characterized by belching of air with a specific sound, while the pregnant woman does not feel an unpleasant odor or taste in her mouth. The following factors contribute to the frequent release of gastric gases during pregnancy:
- Hormonal changes . From the first trimester, a woman has an increased synthesis of progesterone, which is necessary for normal gestation and a decrease in uterine tone. The hormone also affects the smooth muscles of the stomach and esophagus, causing them to relax excessively. Due to the stretching of the organs, an accumulation of gases occurs, provoking a reflex opening of the cardiac sphincter, a spasm of the pylorus and the release of air.

- Uterine growth . A significant increase in the volume of the uterus is detected in the second and third trimesters of pregnancy, which is accompanied by a displacement of neighboring organs. The stomach is pushed back to the diaphragm, compressed, as a result of which its contractile activity and coordination of the work of muscle sphincters are disturbed. This leads to frequent burping. Also, women note shortness of breath associated with insufficient expansion of the lungs.
- Reduced physical activity . At late gestational periods, it becomes difficult for a pregnant woman to do her usual work, so women often lead a hypodynamic lifestyle. The reduction in physical activity provokes hypotension of the muscles of the stomach and intestines, slow progress of the chyme through the alimentary canal. Belching occurs as a reflex act due to overstretching of the walls of the digestive tract, sometimes combined with heaviness in the stomach after eating.

- Aerophagy . Swallowing air while eating is a common cause of erections during pregnancy. This condition develops when talking while eating, insufficient chewing of food, snacking in a hurry. Due to the excess amount of air that has entered the stomach, the walls of the organ are overstretched, followed by a sharp contraction. This is manifested by prolonged erection with characteristic sounds, a feeling of fullness in the epigastrium.
- Use of certain foods . Failure to follow the recommendations of a gynecologist on nutrition during pregnancy can lead to belching. The symptom is often provoked by the use of fresh fruits and berries, black bread, legumes. The mechanism of development is associated with increased gas formation, which, against the background of a slowdown in gastric motility, causes flatulence and erection of gastric gases. Belching is also provoked by the use of chewing gum.
- Autonomic innervation changes .
 During pregnancy, a restructuring of all body systems, including the autonomic nervous system, occurs. The regulation of gastrointestinal motility is mainly realized through the parasympathetic fibers of the vagus nerve, with a change in neuro-reflex interactions, mild dyspeptic disorders are possible. Belching of gastric gases occurs at different times of the day, regardless of food intake.
During pregnancy, a restructuring of all body systems, including the autonomic nervous system, occurs. The regulation of gastrointestinal motility is mainly realized through the parasympathetic fibers of the vagus nerve, with a change in neuro-reflex interactions, mild dyspeptic disorders are possible. Belching of gastric gases occurs at different times of the day, regardless of food intake.
Specific pathologies of pregnancy
Dyspeptic disorders are one of the manifestations of specific diseases of the gestational period. These conditions have different etiologies and mechanisms of development; they can be caused by an immunological conflict, pathological visceral impulses from the uterus, and serious dysfunctions of the peripheral nerve plexuses. A sharp deterioration in the condition of a woman and the appearance of atypical symptoms are indications for seeking qualified help. Belching is observed in such pathological conditions as:
- Pregnancy cholestasis .
 Idiopathic bile stasis, according to various sources, affects 0.1-2% of pregnant women. It is believed that cholestasis is caused by increased synthesis of cholesterol and a violation of the colloidal balance of bile under the influence of estrogens. The disorder is manifested by intense itching of the skin, which is combined with jaundice, dark urine, dyspeptic disorders (eructation, nausea, flatulence).
Idiopathic bile stasis, according to various sources, affects 0.1-2% of pregnant women. It is believed that cholestasis is caused by increased synthesis of cholesterol and a violation of the colloidal balance of bile under the influence of estrogens. The disorder is manifested by intense itching of the skin, which is combined with jaundice, dark urine, dyspeptic disorders (eructation, nausea, flatulence). - Toxicosis . Belching during pregnancy is one of the symptoms of early toxicosis, which is detected in 50-60% of patients, starting from the 5th week of gestation. With a mild degree, the general condition of the pregnant woman is not disturbed, she is worried about nausea, salivation, and erection. Moderate and severe forms of the disease are characterized by repeated vomiting up to 20 times a day, up to the impossibility of enteral nutrition, dehydration.
- Intestinal atony . Difficulties with bowel movements are common, affecting about 60% of women during pregnancy.
 Constipation of pregnant women has neurogenic and hormonal prerequisites, the situation is aggravated by the pressure of the enlarged uterus on the intestines. Belching occurs reflexively in response to stagnation of feces, stretching of the intestinal walls, and a decrease in peristaltic activity. With intestinal atony, gastric gases have a fetid odor.
Constipation of pregnant women has neurogenic and hormonal prerequisites, the situation is aggravated by the pressure of the enlarged uterus on the intestines. Belching occurs reflexively in response to stagnation of feces, stretching of the intestinal walls, and a decrease in peristaltic activity. With intestinal atony, gastric gases have a fetid odor.
Other diseases of the digestive system
Belching during pregnancy may occur against the background of concomitant pathology of the digestive system, which is aggravated during gestation. The manifestation of chronic diseases during the period of bearing a child is caused by the influence of sex hormones, an increased load on the digestive system, and a violation of homeostasis reactions. With organic pathologies of the gastrointestinal tract, erection is usually accompanied by other symptoms (pain, stool instability), which requires a visit to a specialist. Lead to the development of belching:
- GERD.
 The appearance of reflux of aggressive gastric contents is associated with a decrease in the sensitivity of receptors to histamine, a slowdown in gallstone motility and an increase in intra-abdominal pressure. Symptoms are aggravated in the second or third trimester of pregnancy: women complain of acid erection, heartburn, periodic chest pains that appear after diet errors, being in a horizontal position.
The appearance of reflux of aggressive gastric contents is associated with a decrease in the sensitivity of receptors to histamine, a slowdown in gallstone motility and an increase in intra-abdominal pressure. Symptoms are aggravated in the second or third trimester of pregnancy: women complain of acid erection, heartburn, periodic chest pains that appear after diet errors, being in a horizontal position. - Chronic gastritis . If a woman had chronic inflammation of the stomach before pregnancy, then the probability of exacerbation is more than 75%. The severity of symptoms depends on the variant of gastritis. In a hyperacid state, there are pains in the epigastric region, sour eructation, stool disorders with a predominance of diarrhea. With reduced acidity, pregnant women complain of erection with a rotten smell, a feeling of heaviness and fullness of the stomach after eating.
- Chronic pancreatitis . Pregnant women are characterized by a decrease in the synthesis of digestive enzymes and a violation of their activation in the lumen of the duodenum, partial obstruction of the pancreatic ducts, so chronic pancreatitis is exacerbated in 1/3 of patients.
 For the disease, dyspeptic disorders are typical - nausea and periodic vomiting, belching, an increase in the volume of feces and the appearance of particles of undigested food in them.
For the disease, dyspeptic disorders are typical - nausea and periodic vomiting, belching, an increase in the volume of feces and the appearance of particles of undigested food in them. - Irritable bowel syndrome . In pregnant women, the symptoms of functional pathologies of the digestive tract may be aggravated. This is due to changes in autonomic innervation and a special psycho-emotional state of a woman, predisposing to dysregulation of intestinal motility. The disorder is manifested by polymorphic symptoms, which quickly arise and disappear. The condition often worsens with stress.
- Crohn's disease . This inflammatory bowel disease is classified as rare. According to statistics, in women, the disease often manifests itself during pregnancy. Crohn's disease is caused by immunological disorders, which are often triggered by an increase in estrogen levels. Belching is combined with pain in the abdomen (especially in the right iliac region), instability of the stool, nausea, and other dyspeptic symptoms.

Examination
The appearance of belching during pregnancy often indicates a specific gestational pathology or an exacerbation of a chronic gastrointestinal disease against the background of hormonal changes. The examination is prescribed by a gastroenterologist with the obligatory participation of an obstetrician-gynecologist in the diagnosis and selection of therapy. All patients are shown a comprehensive examination using laboratory and instrumental methods that do not pose a danger to either the mother or the fetus. For diagnostic purposes, the following are used:
- Ultrasound . Ultrasound of the abdominal cavity is the main instrumental diagnostic method, since this study is absolutely harmless to the child. Sonography reveals signs of inflammatory processes and morphological changes in the gastrointestinal tract. The study is not informative enough in late pregnancy due to a significant increase in the uterus.
- Intragastric pH .
 The occurrence of acid eructation during gestation usually occurs against the background of impaired secretion of hydrochloric acid, therefore a 24-hour measurement of acidity in the stomach is recommended. Additionally, pH-metry of the esophagus is performed - a decrease in the level of less than 4 indicates gastroesophageal reflux.
The occurrence of acid eructation during gestation usually occurs against the background of impaired secretion of hydrochloric acid, therefore a 24-hour measurement of acidity in the stomach is recommended. Additionally, pH-metry of the esophagus is performed - a decrease in the level of less than 4 indicates gastroesophageal reflux. - Breath test . To exclude gastrointestinal pathology against the background of H. Pylori infection, a non-invasive respiratory study is prescribed, based on the ability of the bacterium to break down urea in the stomach. The method sometimes gives false-negative results, therefore, to clarify the diagnosis, a specific fecal antigen in the blood is additionally determined.
- Laboratory blood tests . All patients are shown a standard biochemical blood test, which allows you to detect signs of protein-energy deficiency, detect problems in the functioning of the hepatobiliary system. According to the indications, it is recommended to study the blood plasma for the level of gastrin and pepsinogen, the determination of the main hormones.

- Endoscopy . EGDS is used for gestation according to strict indications, in cases where belching is accompanied by other dyspeptic disorders. The study allows you to examine the mucous membrane of the esophagus and stomach, visualize inflammatory foci. The endoscopic method is highly informative in assessing the contractile function of muscle sphincters.
The list of mandatory examination methods also includes a coprogram that detects specific changes in feces during inflammation, fermentopathy, maldigestion and malabsorption, analysis for helminth eggs, Gregersen's test for occult blood. If inflammatory bowel disease is suspected, pregnant women should be especially careful with sigmoidoscopy and colonoscopy.
Diet needs to be reviewed during pregnancy
Symptomatic treatment
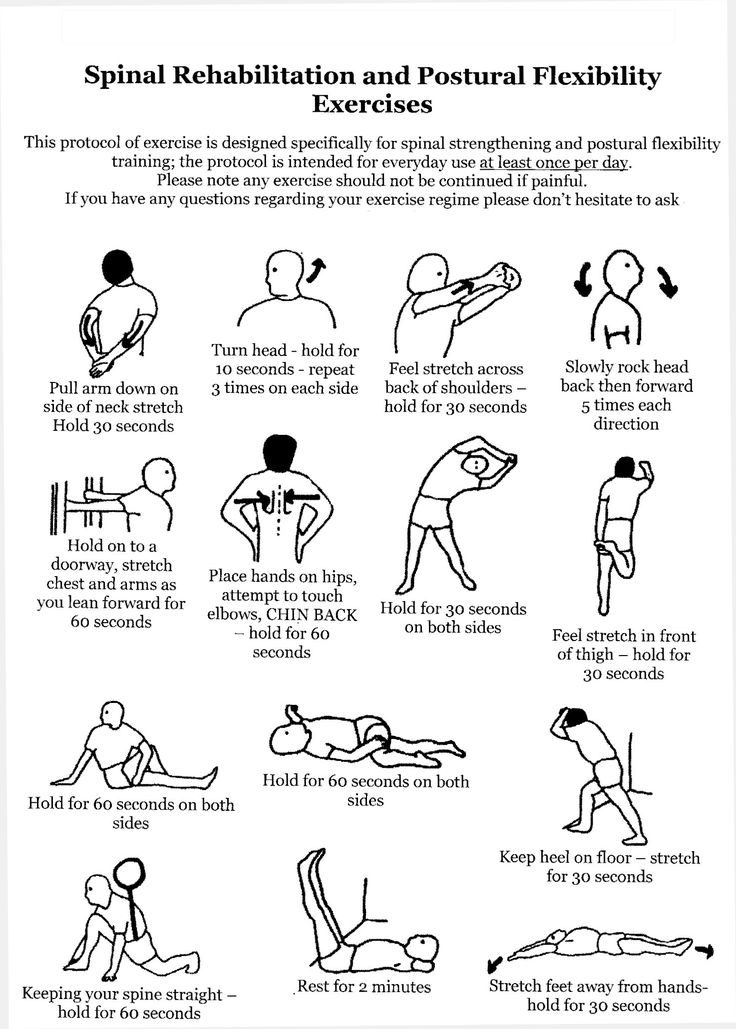
In most cases, belching during pregnancy is physiologically understandable and does not require special treatment. To reduce the frequency of erection, women are advised to adjust their eating habits: eat fractionally, in small portions, do not talk while eating, exclude foods that increase gas formation from the diet. Pregnant women should avoid sharp torso bending, it is undesirable to take a horizontal position immediately after eating.
To reduce the frequency of erection, women are advised to adjust their eating habits: eat fractionally, in small portions, do not talk while eating, exclude foods that increase gas formation from the diet. Pregnant women should avoid sharp torso bending, it is undesirable to take a horizontal position immediately after eating.
If belching bothers a woman very often or is accompanied by pain in the abdomen, stool disorders, other signs of dyspepsia, this may indicate the development of a disease of the digestive organs. In this situation, it is necessary to visit a gastroenterologist as soon as possible. Until an accurate diagnosis is established, it is allowed to take medications that are allowed during pregnancy - prokinetics, mild sedatives that help reduce unpleasant symptoms, but do not harm the baby's body.
Toxemia, Intestinal Problems & Heartburn
Find out how pregnancy affects your digestive tract, which trimesters are more likely to cause indigestion and nausea, and what to do to manage them.

During pregnancy, the burden on the mother's body increases. The body needs more nutrients, the body produces additional hormones. And the growing fetus puts pressure on neighboring organs, including the stomach and intestines. We tell you what symptoms are observed in each trimester, how to cope with toxicosis and get rid of heartburn.
Contents:
- 2. Toxicosis and pregnancy
- 3. Causes, risks and treatment of diarrhea during pregnancy
- 4. Heartburn and stomach pain during pregnancy
- 5. Bloating, constipation and microbiota during pregnancy
- 6. Note
Changes in the functioning of the gastrointestinal tract by trimesters of pregnancy
The average duration of pregnancy is 40 weeks, which are usually divided into trimesters in accordance with the stages of intrauterine development of the child.
Each trimester is accompanied by a number of changes in the body, including in the gastrointestinal tract:
| The first trimester of pregnancy 1–13 weeks 26 weeks | Third trimester of pregnancy 27–40 weeks |
| Morning sickness Morning sickness |
Atlas Genetic Test will help you find out how your genes affect the level of female sex hormones necessary for fertility and pregnancy.

Causes of gastrointestinal problems during pregnancy
Every pregnancy is accompanied by inevitable changes in the functioning of the digestive system. They are more often caused by hormonal changes and increased stress on the organs, but they can also be associated with lifestyle and health conditions, for example:
- Sedentary lifestyle and unbalanced diet;
- Certain drugs, including calcium or aluminum antacids;
- Viral and bacterial infections;
- Intolerance to certain nutrients and allergic reactions;
- Stress;
- Diseases of the thyroid gland.
If you have chronic diseases of the gastrointestinal tract and you are planning a pregnancy, try to consult your doctor in advance. Symptoms of conditions such as irritable bowel syndrome (IBS) or acid reflux are more likely to get worse during pregnancy. Your doctor will help prepare your body and create a prevention plan to help relieve symptoms during this time.
Irritable bowel syndrome, or IBS, is a functional bowel disease that causes frequent abdominal pain, impaired peristalsis, bloating, constipation, or diarrhea.
Morning sickness, vomiting and general malaise during pregnancy
Morning sickness and morning sickness during early pregnancy are common, because the body undergoes important changes necessary for the development of the child.
up to 90%
women experience nausea during pregnancy
Doctors find it difficult to say with certainty why pregnant women feel sick in the morning. The main theory is hormonal changes. But there are some patterns associated with an increased risk of morning sickness:
- Multiple pregnancy;
- Toxicosis during previous pregnancy;
- History of morning sickness during pregnancy in close relatives;
- Tendency to motion sickness in transport;
- Use of oral contraceptives containing estrogen before pregnancy;
- Frequent migraines;
- BMI 30 and above;
- Elevated levels of stress hormones
Risks of severe morning sickness and how to reduce nausea
Nausea and vomiting are usually not associated with a risk for mother and child and disappear by 16-20 weeks of pregnancy, but it is not necessary to wait so long - there are ways that can help reduce nausea and enjoy the process of waiting for a new person:
- Get plenty of rest - fatigue increases toxicosis;
- Avoid smells and foods that cause nausea;
- Eat something right after waking up.
 A toast or a slice of bread will help reduce nausea;
A toast or a slice of bread will help reduce nausea; - Avoid hunger - empty stomach increases nausea. Eat small meals often, prefer low-fat, high-carbohydrate foods;
- Try ginger - studies show it helps with nausea;
- Sip as often as possible and prefer still water.
Rarely, pregnant women may develop hyperemesis gestationis or excessive vomiting. This is a serious condition that can lead to dehydration, kidney damage, seizures, abnormal heart rhythms, and even death.
Signs of dehydration include dry mouth, dizziness, dark urine, infrequent urination and/or dizziness.
Symptoms of excessive pregnancy vomiting:
- frequent nausea for a long time and regular vomiting after meals;
- dry skin and lips;
- sudden weight loss;
- low blood pressure (below 90/60).
If symptoms of excessive pregnancy vomiting occur, do not wait until the condition resolves on its own. It is necessary to seek medical help as soon as possible - the doctor will prescribe treatment, help adjust the diet and lifestyle of the expectant mother.
It is necessary to seek medical help as soon as possible - the doctor will prescribe treatment, help adjust the diet and lifestyle of the expectant mother.
0.5–2%
pregnant women experience excessive vomiting
Diarrhea in pregnancy
The word "diarrhea" comes from the Greek language and literally means "to flow through". This is a condition during which bowel movements or bowel movements occur three times a day or more often. This phenomenon is especially typical for the third trimester of pregnancy, but it can also occur earlier.
Symptoms of diarrhea:
- Three or more bowel movements per day
- Urgent urge to have a bowel movement
- Abdominal pain and cramps
- Bloating
Causes of diarrhea during pregnancy poisoning, dysbacteriosis, bacterial and viral infections:
| Gastroenteritis | Use of lactose and gluten in case of intolerance to these nutrients |
| Bacterial infections: listeriosis or salmonella | Chronic gastrointestinal diseases: Crohn's disease, IBS, ulcerative colitis |
| Some antibiotics and antacids to reduce acidity | Laxatives |
| Sugar substitutes such as sorbitol | Overconsumption of certain foods |
Tip: If you have recently returned from a holiday in an exotic country with nausea and diarrhea and find out you are pregnant, see your doctor as soon as possible.
Gastroenteritis
One common cause of diarrhea during pregnancy is gastroenteritis or stomach flu. It is caused by bacterial or viral infections: norovirus, rotavirus, E. coli, salmonella, which enter the body through contact with contaminated surfaces, dishes, food and water.
Gastroenteritis usually lasts about three days. However, severe illness is a health hazard, especially during pregnancy, as it can cause dehydration, electrolyte imbalance, and lead to preterm labor.
The main symptoms of gastroenteritis are diarrhea without blood, nausea and vomiting, stomach cramps and pain, slight fever, headache and muscle pain.
Take extra precautions to reduce your risk of getting sick: frequent handwashing and surface disinfection. If the expectant mother has small children, they are not recommended to use the same cutlery.
Risks of diarrhea during pregnancy
Usually diarrhea during pregnancy is not a cause for concern. However, you should consult a doctor if the following symptoms occur during this period:
However, you should consult a doctor if the following symptoms occur during this period:
- Diarrhea for more than two days;
- Stools with blood or mucus;
- Sudden weight loss;
- Abdominal pain;
- Dehydration.
How to treat diarrhea during pregnancy
If you have diarrhea during pregnancy, drink plenty of fluids, avoid foods high in fat and sugar, avoid dairy products, and caffeinated drinks.
Dehydration is a serious risk, especially during pregnancy, so electrolyte balance should be restored first with fluids and simple foods:
| Moderate fruit juices | Drinks without alcohol and caffeine |
| Bananas | Potato |
| Rice | Toast |
| Rusks | Light soups and broths |
| Pasta | Applesauce |
Use the Atlas Microbiota Test to find out your body's ability to break down lactose and gluten.
Stomach pain and heartburn during pregnancy
Many women experience stomach pain during pregnancy, especially the upper part of the stomach, as well as heartburn - a burning sensation in the chest and esophagus.
This is more common in the third trimester, after about 27 weeks. This is an unpleasant but natural phenomenon during pregnancy: the baby grows inside the uterus and presses on other organs, including the stomach. And hormones cause the muscles to relax, which causes acid from the stomach to enter the esophagus and irritate it. In addition, pain can be caused by problems with certain organs such as the gallbladder, or inflammation of the pancreas.
Symptoms of heartburn during pregnancy:
- Burning in chest and esophagus;
- Feeling of overeating, heaviness or bloating;
- Belching, including with acid and/or food particles;
- Nausea.
It is unlikely that you will be able to avoid cramps and heartburn during pregnancy. However, some tips can help reduce their frequency:
However, some tips can help reduce their frequency:
Nutrition : try to avoid overeating - eat easily digestible food in small portions; do not eat three hours before bedtime; watch your posture while eating - so the pressure on your stomach will be less.
Smoking and alcohol: In addition to known harms to mothers and babies, tobacco smoke also relaxes the muscles in the lower esophagus, allowing acid to enter the esophagus. And alcohol provokes heartburn and acid reflux.
Although stomach pain and heartburn often accompany pregnancy, abdominal pain, especially in the third trimester, should be taken seriously. It can be a sign of preterm labor or placental abruption, and puts mother and baby at risk.
If you experience severe abdominal pain during pregnancy that is accompanied by the following symptoms, seek medical attention as soon as possible:
| Abdominal pain and fever | Bleeding |
| Regular seizures | Unusual vaginal discharge/ spotting |
| Vomiting | Low back pain |
| Pain or burning when urinating | Severe pain that lasts 30-60 minutes |
Bloating, constipation and microbiota during pregnancy
Excessive gas and constipation during pregnancy can be caused by hormonal changes, such as increased production of progesterone. This hormone, essential for nourishing the uterus and fetus, relaxes the muscles of the body, including the muscles in the intestines, which slows down digestion and increases flatulence. A similar reaction of the body can be observed before each menstruation, when the production of progesterone increases.
This hormone, essential for nourishing the uterus and fetus, relaxes the muscles of the body, including the muscles in the intestines, which slows down digestion and increases flatulence. A similar reaction of the body can be observed before each menstruation, when the production of progesterone increases.
Flatulence - bloating of the abdomen due to the accumulation of gases.
Here are a few simple rules that will help improve intestinal motility and avoid constipation and bloating:
- If you don't usually eat a lot of fiber and indigestible foods like legumes, try to gradually introduce them into your diet;
- Avoid carbonated drinks and fatty foods;
- Move more;
- Drink plenty of fluids.
If bloating and constipation are accompanied by severe pain that lasts more than 30 minutes, or if you have been constipated for two or more weeks, call your doctor.
Gut microbiota and bacteria during pregnancy
A woman's body goes through many changes during pregnancy, and this can affect the microbiota, the bacterial ecosystem that lives in the gut. Trillions of microorganisms do important work for the whole body: they synthesize vitamins and essential acids, keep your intestines working and protect it from disease and inflammation.
Trillions of microorganisms do important work for the whole body: they synthesize vitamins and essential acids, keep your intestines working and protect it from disease and inflammation.
The additional influx of female hormones that accompanies pregnancy alters gut function and affects the microbiota. This is good, because the bacterial community is constantly adjusting to external and internal conditions in order to keep up with the needs of the body.
To keep your gut bacteria running smoothly, they need your help. Provide them with healthy foods and plant fibers. Fruits, vegetables, whole grains, nuts, and seeds contain prebiotics, special substances that beneficial bacteria feed on. When properly balanced, the bacteria even increase your body's defenses against harmful microorganisms that can cause gastroenteritis during pregnancy.
The Atlas Microbiota Test helps you understand how to prepare your gut for a future pregnancy and reduce the risk of digestive problems.
☝️ Take note
Now you have all the necessary knowledge and tools to help you deal with digestive problems during pregnancy. They are quite varied and quite natural, but in some cases it is necessary to immediately seek medical help:
- Vomiting blood;
- Blood in stool;
- Diarrhea for more than two days;
- Constipation for more than two weeks;
- Sudden weight loss;
- Severe pain interfering with daily activities;
- Difficulty breathing;
- Pain when swallowing or difficulty swallowing;
- Excessive fatigue.
More articles on the causes of digestive problems on the blog:
- 7 foods that cause gas and bloating
- Lindsey J Wegrzyniak, Treatment of Hyperemesis Gravidarum, 2012
- Edwards A. et al., The Maternal Gut Microbiome During Pregnancy, 2018
- National Health and Safety (NHS), Vomiting and morning sickness in pregnancy
- Kudzai Kanhutu, Travel and pregnancy: an infectious diseases perspective, 2011
- CDC, Pregnant travelers
- U.