Miscarriage pains stomach
Miscarriage: the signs and what really happens | Pregnancy articles & support
It’s probably the biggest pregnancy anxiety but sometimes miscarriage is shrouded in myth and secrecy. Here are the facts you need to know.
Some women have no obvious signs of a miscarriage and only have it diagnosed during a scan. Other women have symptoms that can be intense, including bleeding or spotting, with or without stomach pain or cramps (NHS Choices, 2018a; Miscarriage Association, 2018a). Some pass clots or ‘stringy bits’.
"When symptoms do occur, they don’t always result in a miscarriage and might be part of a normal pregnancy. So if you get them, try not to panic."
Miscarriage symptoms and signs: bleeding
Bleeding can vary from light spotting or brownish discharge to heavy bleeding and bright red blood (Miscarriage Association, 2018a). It might come and go over several days.
Try to remember that light vaginal bleeding is relatively common during the first trimester (the first 12 weeks) and definitely isn’t a sure sign that you're having a miscarriage. One study found that in the first 20 weeks of pregnancy, 21% of the women experienced vaginal bleeding and 12% had a miscarriage after that (Everett, 1997). This means about half of the women who had vaginal bleeding continued having a healthy pregnancy.
Bleeding could be caused by any of the following:
If you start bleeding during pregnancy, contact your GP, midwife or the early pregnancy unit at your local hospital as soon as possible. If your symptoms are not severe and your baby is not due for a while, you'll be monitored. Some women may have to stay in hospital for observation(NHS Choices, 2018b).
How will I know what’s causing my bleeding?
You may need to have a vaginal or pelvic examination, an ultrasound scan or blood tests to check your hormone levels. Your doctor will also ask you about other symptoms but sometimes it might not be possible to find out what’s caused the bleeding.
Miscarriage symptoms and signs: stomach pain
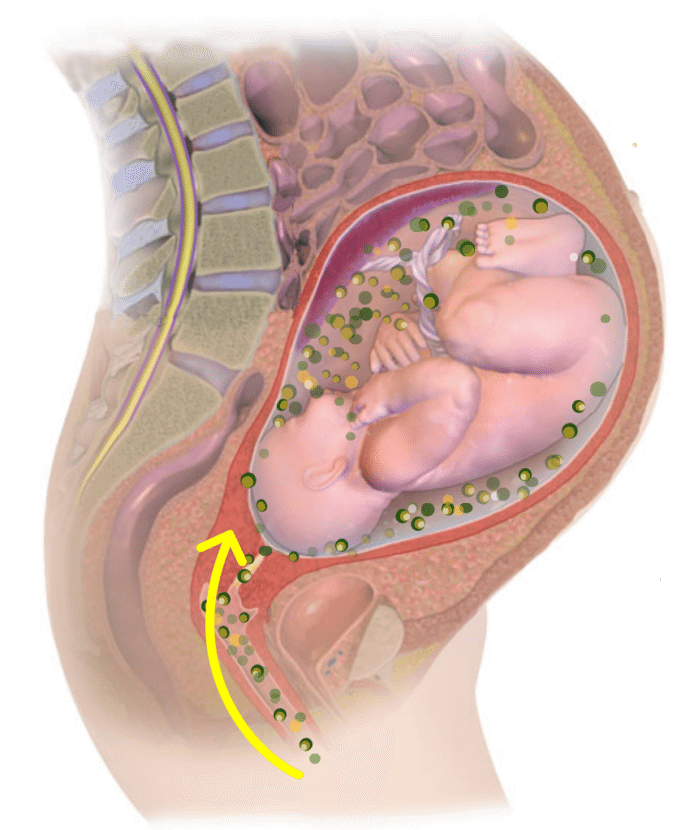
Stomach pain might be due to an upset tummy or constipation. Some women experience lower stomach cramps because of the recent implantation of the fertilised egg in the wall of the uterus. You can also get cramps in the early weeks because your womb is stretching and growing(Marcin, 2017).
Some women experience lower stomach cramps because of the recent implantation of the fertilised egg in the wall of the uterus. You can also get cramps in the early weeks because your womb is stretching and growing(Marcin, 2017).
If you have bleeding or spotting as well as pain, that may be a sign of miscarriage(Miscarriage Association, 2018a). Contact your GP or early pregnancy unit.
If you have sharp abdominal or one-sided pain or pain in your shoulders, and/or pain when you poo, go to A&E. They’ll give you an emergency scan. It’s especially important to get help if you have had an ectopic pregnancy before(NHS Choices, 2018a; Miscarriage Association, 2018a).
If pregnancy symptoms go away, is that a sign of miscarriage?
The sudden disappearance of pregnancy symptoms like nausea or cravings can also sometimes be a sign of miscarriage. But this doesn’t necessarily mean there is a problem. Some women don’t get many pregnancy symptoms anyway.
If you’ve been having strong pregnancy symptoms that suddenly reduce or stop well before your 12 weeks pregnant, your hormone levels might be dropping. You may want to do another pregnancy test and/or talk to your GP about a scan(Miscarriage Association, 2018a).
You may want to do another pregnancy test and/or talk to your GP about a scan(Miscarriage Association, 2018a).
Miscarriage: How do you know for certain?
Miscarriage is usually diagnosed or confirmed with an ultrasound scan. It may take more than one scan to confirm it for definite.
In later (second trimester) pregnancy, bleeding, pain and passing a recognisable pregnancy sac or delivering a baby often confirms what has happened without a scan.
Miscarriage: What happens afterwards?
If there's no pregnancy tissue left in the womb, no treatment is required. If there is, your options to remove the tissue are as follows:
Discuss your options with the doctor in charge of your care and read more about available treatments on the NHS Choices website.
If your blood group is rhesus negative (RhD negative), you should be offered injections of a medication called anti-D immunoglobin afterwards. This prevents rhesus disease, which is a condition where antibodies in a pregnant woman's blood destroy her baby's blood cells (NHS Choices, 2018d).
Contact your hospital immediately if your bleeding becomes particularly heavy, you develop a high temperature, or you experience severe pain.
You should be advised to take a home pregnancy test after three weeks. If you're still pregnant, you may need further tests to make sure you don't have a molar pregnancy (an abnormal fertilised egg implanted) or an ectopic pregnancy (NHS Choices, 2016; Miscarriage Association, 2018b).
This page was last reviewed in April 2018
Further information
Our support line offers practical and emotional support in many areas of pregnancy, birth and early parenthood: 0300 330 0700.
We also offer antenatal courses which are a great way to find out more about birth, labour and life with a new baby.
Make friends with other parents-to-be and new parents in your local area for support and friendship by seeing what NCT activities are happening nearby.
For more help and advice on all pregnancy loss, contact The Miscarriage Association.
You can read more about miscarriage in our range of articles.
Miscarriage Pain: Causes, Symptoms, and Treatment
According to the American College of Obstetricians and Gynecologists (ACOG), miscarriage happens in at least 10 percent of clinically identified pregnancies. (Meaning, you actually knew you were pregnant; some miscarriages happen before you even miss your period.)
When miscarriage happens after you’ve already gotten a positive pregnancy test, it can be a physically and emotionally painful process.
We can’t make miscarriage any easier, but we can help you understand what’s happening. For instance, although abdominal pain is one of the most frequent symptoms of a miscarriage, it’s not the only type of pain or discomfort you might feel.
Here’s a breakdown of seven types of pain you might have during a miscarriage and what you can do to relieve your symptoms.
Cramping with a miscarriage is usually caused by your uterus contracting. Just like during your period, your uterus contracts to push contents out. Since your uterus is mostly a muscle, these contractions feel like muscle cramps (in other words, they hurt).
Since your uterus is mostly a muscle, these contractions feel like muscle cramps (in other words, they hurt).
You’ll usually feel these cramps on both sides of your lower abdomen or pelvic region. The cramps may come and go in waves or your pain may feel more constant. Unless your doctor has told you not to, you can treat your pain with over-the-counter (OTC) pain relievers like Motrin or Tylenol. You can also use a heating pad to ease cramping.
During a normal menstrual cycle, your uterus builds up lining to prepare for a pregnancy. When the pregnancy can’t continue, the lining needs to be shed.
Because your body has been preparing for pregnancy, there will be more lining and tissue, so your bleeding will be heavier than a period. The further along you are in the pregnancy, the heavier it will be.
To absorb the bleeding, you’ll need to wear a pad. ACOG doesn’t recommend using tampons during a miscarriage. And because the bleeding may last longer and be heavier than a typical period, you may notice some discomfort from moisture accumulation.
Blood loss with a miscarriage
You can lose a significant amount of blood with a miscarriage. Stay in touch with your doctor during the process and call if you experience dizziness or excessive blood loss (e.g., soaking more than two maxi pads per hour for more than 2 hours in a row).
To combat any discomfort, change your pad frequently and clean the area gently with water, avoiding soap.
The change in the vaginal environment from bleeding may also cause a yeast or bacteria overgrowth that could lead to vaginal odor. If you notice any signs of a yeast infection such as itching, or if the discharge becomes very foul smelling, call a doctor.
Gastrointestinal symptoms such as nausea, vomiting, and diarrhea can be caused by hormone changes, as well as side effects from any medication you take to manage the miscarriage. Diarrhea can also be caused by the relaxing of the smooth muscle, just like you experience with a period.
To combat nausea symptoms, drink plenty of water and try to eat small meals consisting of bland, gentle-on-the-stomach foods. These can include:
These can include:
- rice
- bananas
- oatmeal
- scrambled eggs
- plain grilled chicken
If your symptoms are making it hard for you to keep food down or stay hydrated, ask your doctor about taking an antinausea or antidiarrheal medication.
Similar to how your period cramps can lead to back pain, the uterine contractions during a miscarriage can cause back pain. This is usually felt in the lower back and the pain can be mild, moderate, or severe.
You can treat it just like you would your cramps — with pain relievers and heating pads — but if it’s really uncomfortable, don’t hesitate to ask your doctor what else you can do.
Shoulder pain is a symptom of ectopic pregnancy and it’s a serious medical emergency. If you have severe, one-sided pain, dizziness or fever, or pain affecting your rectum, pelvis, shoulder, or neck, call your doctor or get urgent medical care right away.
Ectopic pregnancy may not cause bleeding, so it can be a harder type of pregnancy to identify.
It’s normal to feel tired and weak with a miscarriage. You may also have a headache. If you experience excessive dizziness or feel like you may faint, tell your doctor or call your local urgent care center.
It’s also important to rest and drink plenty of water to manage these symptoms. Try to sleep, stay hydrated, and eat nutrient-dense foods.
No matter how far along in your pregnancy you are when you miscarry, you’re allowed to feel grief. Miscarriage emotions can be complicated and messy. You may feel both sad and relieved that it’s over, or you may feel intense and sometimes overwhelming grief.
No matter your situation, you might feel disappointed, hopeless, or scared to conceive again. You might experience anxiety, mood swings and irritability, and even depression.
Talking about your loss can help. Try turning to trusted friends and family members, social media groups, or a mental health professional. Miscarriage can also lead to clinical depression, similar to postpartum depression — so be sure to seek medical attention if you experience any symptoms.
The severity of your miscarriage symptoms will depend on how far along you are in your pregnancy and what type of miscarriage you have. Still, a miscarriage at any stage can be difficult because all bodies respond differently.
You may choose expectant management to let your body pass the tissue on its own, you might use medication that can speed up the process, or you may choose a surgical procedure called a dilation and curettage (D&C) to remove the contents of the uterus.
The bleeding that occurs with miscarriage can be different for everyone, too. In general, you can expect menstrual-like bleeding for about a week. After that, spotting can continue for several weeks — sometimes even until your next period. And when is that? Again, it varies: Your menstrual cycle can restart anywhere between 4 to 8 weeks after the miscarriage.
When to seek medical help
If you suspect you’re having a miscarriage, you should always consult with your doctor. Your provider will also stay in touch with you throughout the recovery process.
Depending on the timing of your miscarriage and how it’s managed, it may be 2 or 3 weeks before you’re feeling like yourself again physically. In some cases, your doctor may order an ultrasound to confirm that your uterus is clear of retained tissue.
For some people, the emotional pain of a miscarriage can last much longer. It’s important to remember that the stage of your pregnancy when you miscarried doesn’t matter: You experienced a loss, and loss naturally comes with feelings of grief.
Sometimes that grief can get too big for you to handle on your own. As with postpartum depression after a birth, symptoms of depression can develop after a miscarriage. In fact, according to a 2015 journal article, nearly 20 percent of women report symptoms of depression and/or anxiety after miscarriage.
If you think you might be depressed or are simply struggling to manage your emotional recovery after miscarriage, don’t be afraid or ashamed to reach out for support. A licensed mental health professional can help you process your loss and begin to heal.
You can also look for a miscarriage support group to connect with other people who have shared your experience. You can search or contact any of the following resources for local and online miscarriage support groups:
- Hope After Loss
- Share Pregnancy and Infant Loss Support
- Empty Cradle
- First Candle
- Empty Arms Bereavement Support
- The Compassionate Friends
- The Miscarriage Association (UK)
Miscarriage can be a difficult experience on your body, mind, and heart. You can help ease physical symptoms with rest, fluids, OTC pain relievers — and stay in touch with your doctor if you have any complications.
It’s also important to address the emotional pain of a miscarriage. Talking to a mental health professional or finding support from a local or online pregnancy loss group can help you take steps toward healing.
Miscarriage, how to avoid - Planning and management of pregnancy in the gynecology of the Literary Fund polyclinic after a miscarriage
- Gallery
- News
- Blog
- Reviews
- Jobs
- Licenses
- Insurance partners
- Controlling organizations
- Schedule of reception of citizens on personal appeals
- What you need to know about coronavirus infection?
- Rules for patients
- Online doctor's consultation
- to corporative clients
- The documents
A miscarriage is always associated with severe consequences for the whole body of a woman and for her reproductive organs in particular, it also affects the family situation, disrupts the woman's work schedule. An unfavorable outcome of pregnancy requires great mental and physical costs on the part of parents. Therefore, contacting doctors to find out the causes of the problem is the very first and correct step towards the birth of a child.
An unfavorable outcome of pregnancy requires great mental and physical costs on the part of parents. Therefore, contacting doctors to find out the causes of the problem is the very first and correct step towards the birth of a child.
Any competent gynecologist will tell you that the problem of miscarriage can be solved. With proper preparation for pregnancy and its management, the next time you will have a successful pregnancy. Most girls after a miscarriage go to extremes: they try to get pregnant again as soon as possible. And if this succeeds, then the miscarriage is very often repeated. And you need to give the body a rest for 2-3 months, then identify and eliminate the cause. And only then try.
Causes of miscarriage
Many are convinced that miscarriages are due to a fall, bruise, or some other physical shock. Any woman who has had a miscarriage can remember that not long before she either fell or lifted something heavy. And I am sure that she lost her unborn child precisely because of this. However, those women whose pregnancy was normal also fall and lift heavy things. Most sudden miscarriages do not occur for this reason. The reason is in violations of the pregnancy itself. Approximately half of miscarriages are due to abnormal genetic development of the fetus, which can be hereditary or accidental. Merciful nature, following the principles of natural selection in everything, destroys the defective and unviable fetus. But you should not be afraid of this. The fact that there is a defect in one embryo does not mean at all that all the others will be the same.
However, those women whose pregnancy was normal also fall and lift heavy things. Most sudden miscarriages do not occur for this reason. The reason is in violations of the pregnancy itself. Approximately half of miscarriages are due to abnormal genetic development of the fetus, which can be hereditary or accidental. Merciful nature, following the principles of natural selection in everything, destroys the defective and unviable fetus. But you should not be afraid of this. The fact that there is a defect in one embryo does not mean at all that all the others will be the same.
The woman's body is almost always to blame for the other half of miscarriages. They are caused by various known and unknown factors, such as: acute infectious diseases suffered in the first trimester of pregnancy, poor environment or difficult working conditions, excessive psychological or physical stress, abnormal development of the uterus, radiation, alcohol, smoking and certain types of drugs.
The causes of early and late miscarriage may differ, although they may overlap. The most important thing is to find out and eliminate or compensate for your own cause of miscarriage. Having discovered the cause, the gynecologist will tell you how to avoid another loss.
The most important thing is to find out and eliminate or compensate for your own cause of miscarriage. Having discovered the cause, the gynecologist will tell you how to avoid another loss.
Miscarriage
Miscarriage statistics also include “missed pregnancy”. Sometimes it happens that the embryo dies and lingers in the uterine cavity. Most often, this fact is detected by ultrasound. The dead fetus may begin to decompose, and this, thereby, will lead to poisoning of the mother's body.
Doctors resort to surgical curettage, which is associated with a risk of inflammation and complications. With such a miscarriage, the next pregnancy is planned after the body is fully restored - not earlier than a year. During this year, you will have to find out the cause of the missed pregnancy and treat it.
Miscarriage up to 6 weeks
The main causes of miscarriage on this line are malformations of the embryo itself. Statistics say that from 70-90% of embryos had chromosomal abnormalities: they are random and will not occur in other pregnancies. You may have been ill, taken medication, or were under the influence of other harmful factors. Fate saved you from a child with malformations.
You may have been ill, taken medication, or were under the influence of other harmful factors. Fate saved you from a child with malformations.
The human body is perfect and finds a way to correct the situation by miscarriage. Today is a tragedy for you. The real tragedy would be the preservation and birth of a sick, non-viable child. So don’t cry and understand: everything is for the best, you won’t help grief with tears ... And after three months, try again - it will almost certainly turn out to be successful.
It should also be noted that the fact of a miscarriage does not mean that you have lost something. So for a period of 7-8 weeks, the absence of an embryo in the fetal egg is found - "anembryony". It is believed that in 80-90% of cases, miscarriages are undiagnosed non-developing pregnancies.
Miscarriage between 6 and 12 weeks
Miscarriage in this period is also considered early. Its most common causes are:
Endocrine disorders
Endocrine disorders, when the ovaries do not synthesize enough hormones to keep the fetus in the womb, or the amount of male sex hormones is increased, is one of the most common causes of miscarriage and miscarriage.
Imbalance of hormones in a woman's body is very likely to lead to an early termination of pregnancy. With a lack of the main hormone progesterone produced by the ovaries, this happens most often. Another hormonal problem is an increase in the tone of the uterus, which provokes the expulsion of the fetus.
Progesterone prepares the uterine mucosa for implantation and is the hormone for maintaining pregnancy in the first months. If conception occurs, the fetus cannot properly establish itself in the uterus. As a result, the fertilized egg is rejected. But pregnancy can be saved with the help of progesterone preparations if this problem is detected in time.
An excess of male sex hormones that suppress the production of estrogen and progesterone can also be the cause of an early miscarriage. Often, the cause of recurrent miscarriages are androgens that affect the formation and development of pregnancy; as well as thyroid and adrenal hormones. Therefore, a change in the function of these glands can lead to miscarriage.
Undertreated sexual infections
This problem must be solved before conception. Often the cause of miscarriage is sexually transmitted infections: syphilis, trichomoniasis, toxoplasmosis, chlamydia, cytomegalovirus and herpetic infections. Their effect on the fetus and the course of pregnancy is different for each woman and depends on the timing of infection, the activity of the microorganism, the degree of immune protection and the presence of other adverse factors. Depending on the situation, they can lead to the formation of fetal malformations, intrauterine infection, feto-placental insufficiency, early miscarriage or premature birth. Infection of the fetus and damage to the membrane of the fetus leads to miscarriage. To avoid this, infections should be treated before pregnancy. The use of therapy is possible during pregnancy as prescribed by a doctor.
Viral infections and other diseases
Any disease accompanied by intoxication and fever above 38 about C can lead to a miscarriage. Rubella, influenza and viral hepatitis occupy a leading position in this list. At a period of 4-10 weeks for pregnancy, ordinary tonsillitis can also become tragic, pneumonia carries a more serious risk. Pyelonephritis and appendicitis can cause early labor. When planning a pregnancy, it is imperative to undergo a medical examination in order to identify and treat foci of infections.
Rubella, influenza and viral hepatitis occupy a leading position in this list. At a period of 4-10 weeks for pregnancy, ordinary tonsillitis can also become tragic, pneumonia carries a more serious risk. Pyelonephritis and appendicitis can cause early labor. When planning a pregnancy, it is imperative to undergo a medical examination in order to identify and treat foci of infections.
Extremely dangerous during pregnancy rubella - it leads to severe fetal malformations, so infection during pregnancy is an indication for medical abortion.
Any disease during pregnancy can lead to non-viability of the fetus. And the body, through a miscarriage, insures you against unwanted offspring. With such a miscarriage, the next pregnancy has every chance of going well.
Immune causes of miscarriage
Sometimes antibodies that are hostile to the fetus are formed in the blood of a pregnant woman. This cause can be predicted and eliminated in advance. Most often, the conflict occurs when the embryo inherits the positive Rh factor of the father, and the negative Rh factor, the mother's body rejects the embryonic tissues that are alien to it. Constant monitoring of antibody titer and the introduction of anti-Rhesus immunoglobulins allows you to maintain and maintain pregnancy. In case of an immune conflict, progesterone preparations are also used to prevent miscarriage, which in this case has an immunomodulatory effect.
Most often, the conflict occurs when the embryo inherits the positive Rh factor of the father, and the negative Rh factor, the mother's body rejects the embryonic tissues that are alien to it. Constant monitoring of antibody titer and the introduction of anti-Rhesus immunoglobulins allows you to maintain and maintain pregnancy. In case of an immune conflict, progesterone preparations are also used to prevent miscarriage, which in this case has an immunomodulatory effect.
Reduced immunity
Reduced immunity during pregnancy also refers to immune causes. The body is simply not able to grow a new life in itself. You need to take care of yourself and recover before the next conception.
Anatomical causes of miscarriage
Anatomical causes of miscarriage are the most intractable. Malformations of the uterus are a serious reason for miscarriage. Sometimes you just have to deal with it.
Miscarriage between 12 and 22 weeks
Such a miscarriage is considered late. Its causes coincide with the causes of miscarriages in the early stages (anatomical, immune, infectious, endocrine).
Its causes coincide with the causes of miscarriages in the early stages (anatomical, immune, infectious, endocrine).
At this time, miscarriage also occurs due to isthmic-cervical insufficiency - a weak cervix cannot hold the fetus and opens. For this reason, a miscarriage can occur in the 2nd or 3rd trimester. Isthmic-cervical insufficiency is observed in 15.0-42.7% of women suffering from miscarriage. Careful monitoring of the pregnant woman allows you to identify the problem in time and make surgical correction of the cervix before the onset of childbirth.
In isthmic-cervical insufficiency, there is only one method of treatment - mechanical narrowing of the cervical canal. To do this, the neck is either sewn up or a special ring is put on it. However, the latter method is less efficient, because the ring can easily slide off the neck, then it will no longer hold back the process of opening it.
After suturing, if necessary, it is possible to use antibiotics and drugs that normalize the microflora of the vagina. The treatment of the vagina and the control of the state of the seams are carried out daily for 5 days. Stitches are removed at 37-38 weeks and with premature onset of labor.
The treatment of the vagina and the control of the state of the seams are carried out daily for 5 days. Stitches are removed at 37-38 weeks and with premature onset of labor.
Isthmic-cervical insufficiency may be primary (for no apparent reason), may be the result of abortion or hormonal disorders (increased levels of androgens - male sex hormones or their precursors).
Miscarriage after 22 weeks
Such a loss is hard to forget. Obstetricians talk about premature birth after the 28th week of pregnancy. Traditionally, a child born after this period is considered viable. But medicine knows many cases when it was possible to save the life of earlier children.
We recommend that you be carefully examined for miscarriage, check the above factors. In addition to them, the cause of a miscarriage can be antiphospholipid syndrome, while the woman's body perceives the child as something alien and rejects it. This disease, like the others listed, can be corrected; you have a very real chance of bearing a child.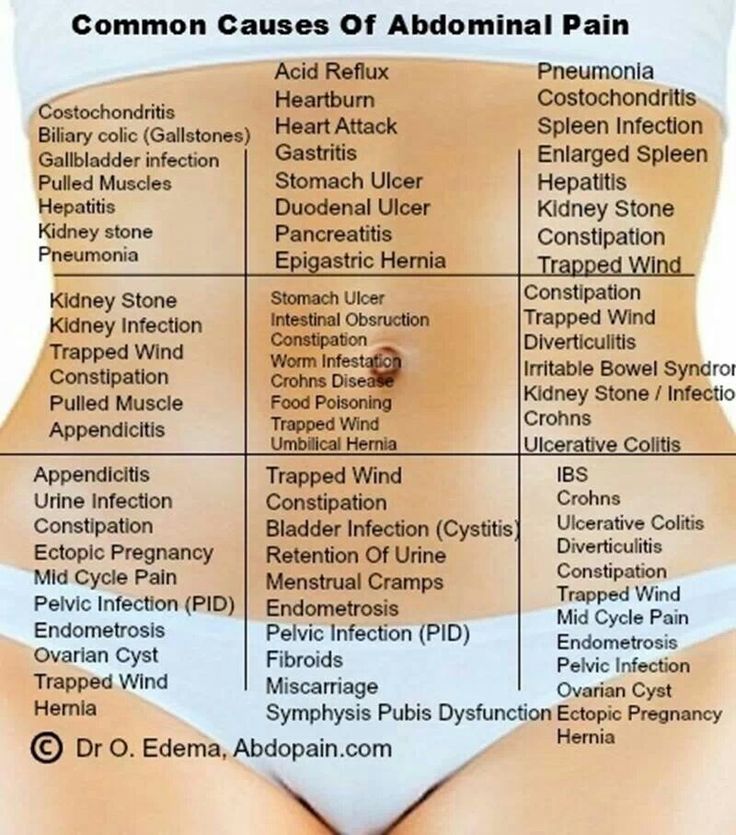
Miscarriages due to hemostasis disorders
All of the above causes account for only 30-40%. Up to 70% of miscarriages are caused by disorders in the blood coagulation system (hemostasis).
Blood coagulation disorders leading to pregnancy loss can be divided into thrombophilic (increased clotting) and hemorrhagic (bleeding tendencies). Both of these extremes are dangerous to the fetus. Various disorders leading to the formation of small blood clots lead to the fact that the fetus loses sufficient blood supply, development is disturbed and the fetus is rejected.
The main hemorrhagic changes can appear even in childhood in the form of increased bleeding during cuts, tooth extractions, the onset of menstruation. But sometimes they declare themselves only during pregnancy and are the cause of a miscarriage. Bleeding in the early stages and detachment of the chorion is difficult to stop.
You may not guess, but incomprehensible headaches, weakness, fatigue, temporary loss of smell or hearing may be symptoms of disorders in the blood coagulation system.
When planning a pregnancy, a genetic examination should be carried out and, if necessary, treatment should be initiated.
It is advisable to be examined for hidden hemostasis defects even for those who consider themselves healthy. This will allow you to predict the occurrence of complications and prevent loss. Early therapy can prevent miscarriage at 98% of cases. If defects in hemostasis are already detected during pregnancy, it can be difficult to maintain it.
What to do after a miscarriage?
Find the cause! The ideal option is to be examined by future parents: it is much more reasonable to postpone conception and spend two or three months to identify the causes than to risk getting pregnant again, spend two months waiting, and then lose everything again and still go to the doctors.
Until you understand the reason, it will not evaporate. In most cases, the answers lie on the surface. Take care of your health and your future baby.
Sign up for a consultation with an obstetrician-gynecologist by phone +7 (495) 150-60-01
Tyan Oksana Alexandrovna
Head of the department, obstetrician-gynecologist Doctor of the highest category Work experience: 26 years
Volkova Polina Dmitrievna
Obstetrician-gynecologist, doctor of ultrasound diagnostics Doctor of the highest category Experience: 35 years
Postnikova Nadezhda Anatolyevna
Obstetrician-gynecologist, ultrasound specialist Work experience: 35 years
Moiseeva Alla Vitalievna
Obstetrician-gynecologist, doctor of ultrasound diagnostics Doctor of the first category Work experience: 37 years
Zabolotnova Olga Valentinovna
Obstetrician-gynecologist Doctor of the first category Experience: 25 years
Shchelokova Elena Nikolaevna
Obstetrician-gynecologist Doctor of the highest category Work experience: 38 years
Pass or medical card number:
Contact phone: *
Select the day of your appointment:
Additional information:
I am not a robot
By clicking the "Submit Application" button, you agree to the terms Privacy Policy and User Agreement
miscarriage, symptoms - Health Clinic 365 G.
 Yekaterinburg
Yekaterinburg Causes of miscarriage
Questions to the doctor about miscarriage
Diagnostics of miscarriage
Treatment and prevention of miscarriage
- this . According to statistics, 10 to 20% of all pregnancies end in miscarriage. However, the real numbers could be much higher, as a large number of miscarriages happen very early, and women are not even aware of their pregnancy. Most miscarriages happen due to abnormal development of the fetus.
Miscarriage is quite common, but this fact does not make things easier. It is always difficult to cope with the realization that there was a pregnancy, but no child. Try to deal with the situation psychologically and understand what could be causing the miscarriage, what increases the risk of it, and what type of treatment might be needed.
Miscarriage symptoms .
Most miscarriages occur before 12 weeks. Signs and symptoms of a miscarriage include:
- Vaginal bleeding or spotting (although quite common in early pregnancy)
- Pain or cramps in the abdomen or lower back
- Fluid vaginal discharge or tissue fragments
It is important to consider the fact that in early pregnancy, spotting or vaginal bleeding is quite common. In most cases, women who experience light bleeding during the first three months have an uneventful pregnancy thereafter. In some cases, even with heavy bleeding, the pregnancy does not end in a miscarriage.
In most cases, women who experience light bleeding during the first three months have an uneventful pregnancy thereafter. In some cases, even with heavy bleeding, the pregnancy does not end in a miscarriage.
Some women who have a miscarriage develop an infection in the uterus. This infection, also called septic miscarriage, can cause:
- Fever (feeling hot, chills)
- Body pains
- Thick, foul-smelling vaginal discharge
When to see a doctor.
Contact your doctor in the following cases:
- Bleeding, even if only light spotting occurs
- Profuse, liquid vaginal discharge without pain or bleeding
- Isolation of tissue fragments from the vagina
You can place a piece of tissue to be isolated in a clean container and take it to your doctor for examination. It is unlikely that the study will give any accurate results, but if it is determined that the fragments of the excreted tissue are from the placenta, the doctor will be able to conclude that the symptoms that appear are not associated with the presence of a tubal (ectopic) pregnancy.