Placenta low line during pregnancy
What complications can affect the placenta?
Complications that can affect the placenta during pregnancy or childbirth include:
- low-lying placenta and placenta praevia
- retained placenta – when part of the placenta remains in the womb after giving birth
- placental abruption – when the placenta starts to come away from the wall of the womb
These complications aren't common.
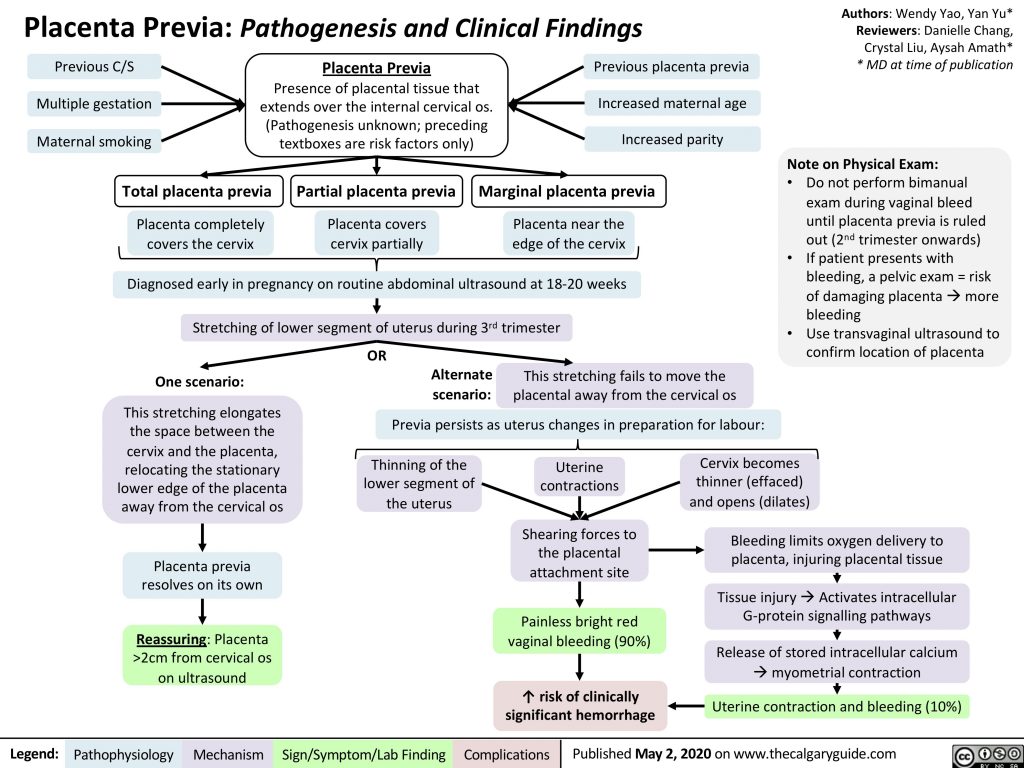
Low-lying placenta and placenta praevia
As your pregnancy progresses, your womb expands and this affects the placenta's position. The area where the placenta is attached usually stretches upwards, away from your cervix.
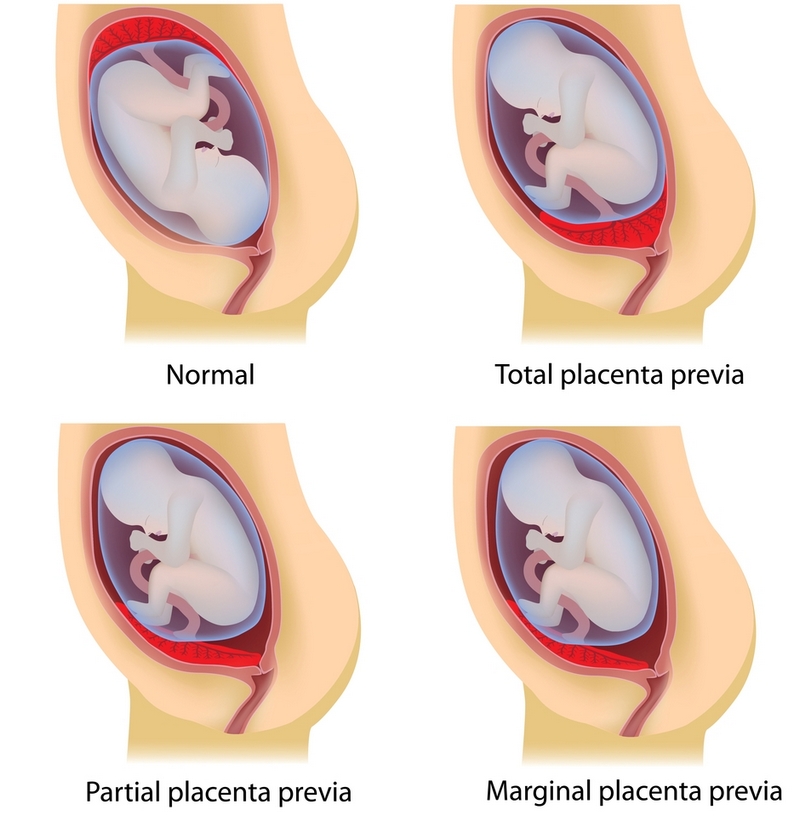
If the placenta stays low in your womb, near to or covering your cervix, it may block the baby's way out.
This is called low-lying placenta if the placenta is less than 2cm from the cervix, or placenta praevia if the placenta is completely covering the cervix.
Placenta praevia, where the cervix is completely covered at the end of pregnancy, affects about 1 in every 200 births.
The position of your placenta will be recorded at your 18- to 21-week ultrasound scan.
If your placenta is significantly low, you'll be offered an extra ultrasound scan later in your pregnancy (usually at about 32 weeks) to check its position again.
For 9 in every 10 women, the placenta will have moved into the upper part of the womb by this point.
If the placenta is still low in your womb, there's a higher chance that you could bleed during your pregnancy or during your baby's birth. This bleeding can be very heavy and put you and your baby at risk.
You may be advised to come into hospital at the end of your pregnancy so emergency treatment (such as a blood transfusion) can be given very quickly if you bleed.
If the placenta is near or covering the cervix, your baby can't be delivered through the vagina, so a caesarean section will be recommended.
A low-lying placenta can be associated with painless, bright red bleeding from the vagina during the last 3 months of pregnancy. If this happens to you, contact your midwife or GP immediately.
Retained placenta
After your baby's born, part of the placenta or membranes can remain in the womb. This is known as retained placenta. If untreated, a retained placenta can cause life-threatening bleeding.
Breastfeeding your baby as soon as possible after the birth can help your womb contract and push the placenta out.
Your midwife may also ask you to change your position (for example, by moving to a sitting or squatting position). In some cases, you may be given an injection of a medicine to help your womb contract.
If these methods don't work, a doctor may need to remove the placenta by hand. This can be painful, so you'll be given an anaesthetic.
Placental abruption
Placental abruption is a serious condition in which the placenta starts to come away from the inside of the womb wall.
It can cause stomach pain, bleeding from the vagina and frequent contractions.
It can also affect the baby, increasing the risk of premature birth, growth problems and stillbirth.
It's not clear what causes placental abruption, but factors that increase the risk include injury to the abdominal area, smoking, cocaine use and high blood pressure.
If you're near your due date, the baby will need to be born straight away and a caesarean section may be recommended.
But if the baby's very premature and the abruption is minor, you may be kept in hospital for close observation.
Always speak to your midwife or GP if you're concerned about any aspect of your health when you're pregnant. You can also call NHS 111.
Further information
- Vaginal bleeding in pregnancy
- Antenatal care
Page last reviewed: 22 August 2022
Next review due: 22 August 2025
Low-lying placenta (placenta praevia) | Tommy's
Is a low-lying placenta common?
The position of your placenta will be checked at your mid-trimester ultrasound scan, at around 18-21 weeks of pregnancy. If your placenta is low-lying, you have another scan later in your pregnancy (usually about 32 weeks).
Because the lower part of the womb stretches more as the baby grows, the placenta usually moves into the upper part of the womb by this point. 90% of women who have a low-lying placenta at 20 weeks will not go on to have a low-lying placenta later in the pregnancy.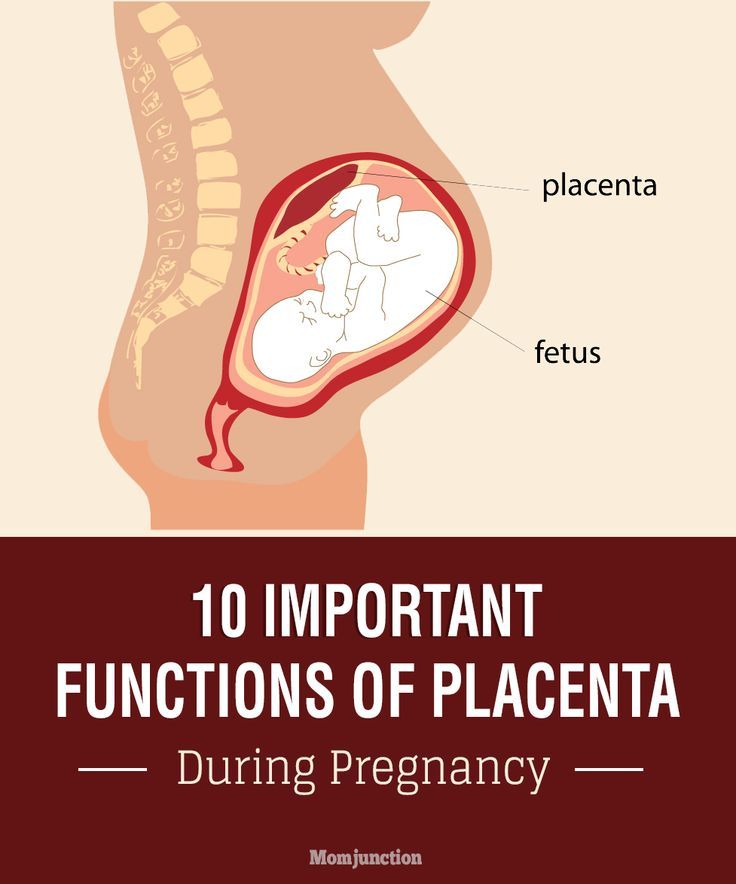
If you have had a baby by caesarean section before, the placenta is less likely to move upwards.
Only 1 in every 200 women have placenta praevia at the end of their pregnancy.
Am I likely to have placenta praevia?
Placenta praevia is more likely if you:
- smoke cigarettes
- have had fertility treatment to get pregnant, such as in vitro fertilisation (IVF)
- have had 1 or more caesarean sections
- are aged 40 or older
- are having more than 1 baby
- have had surgery on the womb
- are a cocaine user
- are expecting a boy
- have endometriosis.
Is there anything I can do to help the placenta move up?
Unfortunately not. The best thing you can do is concentrate on staying as healthy as you can. You may need extra scans, so make sure you go to all your antenatal appointments and follow your healthcare professional’s advice.
How can placenta praevia affect me and my baby?
There is a risk that you may have vaginal bleeding, particularly towards the end of your pregnancy.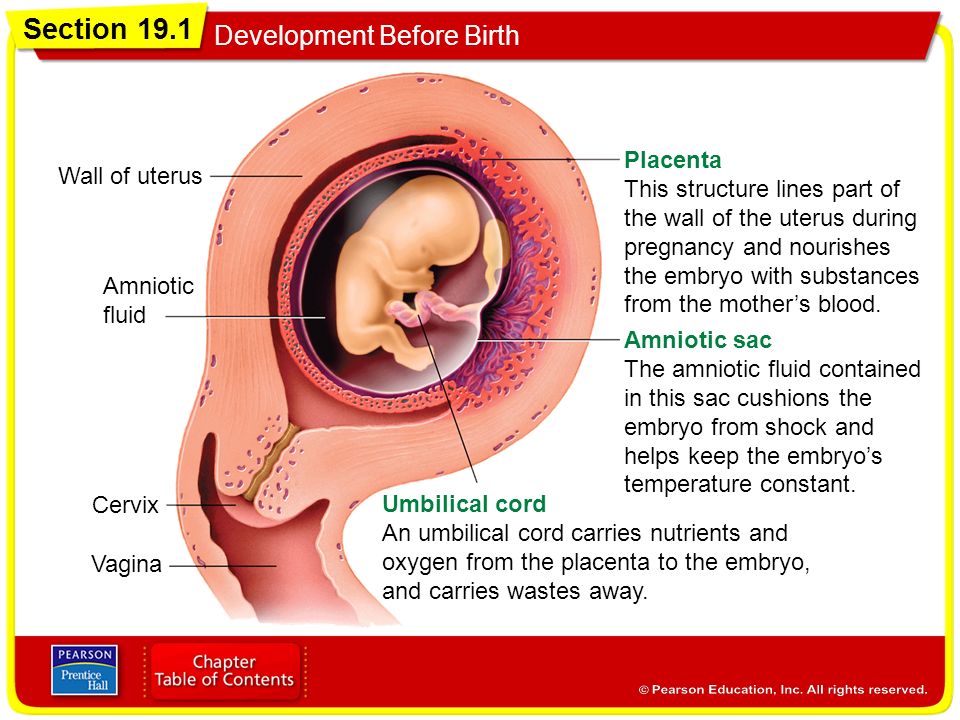 Bleeding from placenta praevia may be very heavy and can sometimes put mum and baby at risk.
Bleeding from placenta praevia may be very heavy and can sometimes put mum and baby at risk.
How is a low-lying placenta diagnosed?
Your midwife or doctor will look at your placenta’s position at your 18 to 21 week ultrasound scan.
If your placenta is low, you'll be offered an extra ultrasound scan later in your pregnancy (usually at about 32 weeks) to check its position again.
In 90% of cases, the placenta is no longer low-lying by this point.
Your midwife or doctor may think you have placenta praevia if:
- you have bleeding during the second or third trimester – this is usually painless and may happen after sex
- if the baby is lying in an unusual position, for example bottom first (breech) or lying across the womb (transverse)
If you have any bleeding during pregnancy, with or without pain, you should always get checked out straight away. If you’re in your first trimester, contact your doctor, midwife or Early Pregnancy Unit.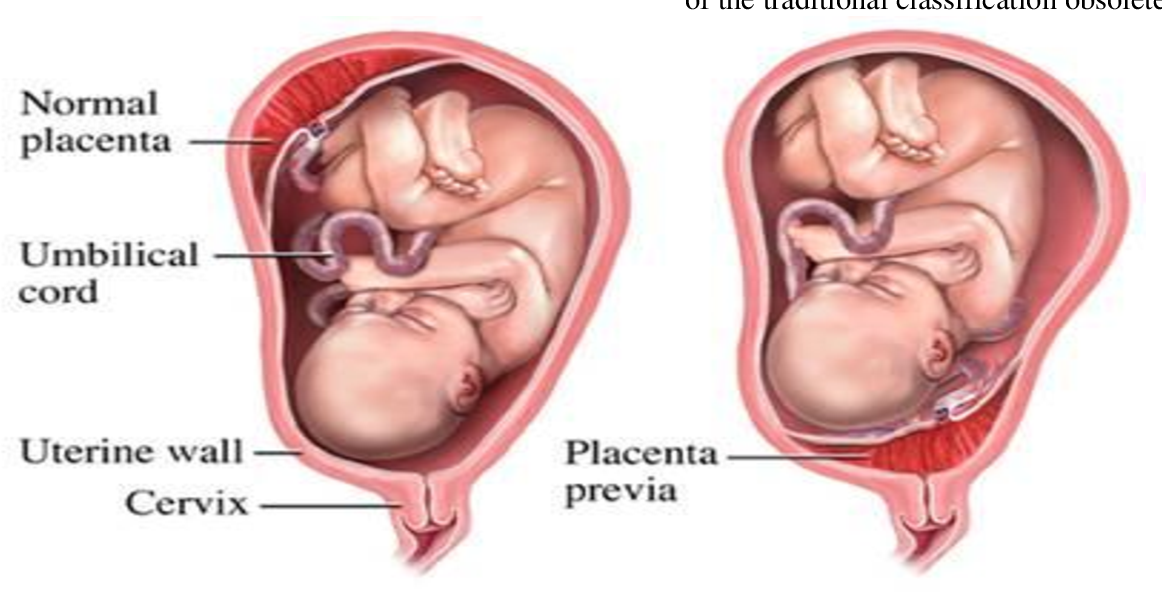 If you are more than 12 weeks pregnant, go to your local A&E or contact your hospital maternity unit immediately.
If you are more than 12 weeks pregnant, go to your local A&E or contact your hospital maternity unit immediately.
You may be advised to avoid having sex (including the use of penetrative sex toys) for the rest of your pregnancy.
What treatment will I have?
Extra scans
If your placenta is low-lying at your 20-week scan, you’ll be offered another ultrasound scan at around 32 weeks. This may include a transvaginal ultrasound scan, which is when a probe is gently placed inside the vagina to check exactly where your placenta is lying. Don’t worry, this is safe for you and your baby.
The length of your cervix may also be measured at your 32-week scan to predict whether you may go into labour early and whether you are at increased risk of bleeding.
If the placenta hasn’t moved up, you should be offered another ultrasound scan at 36 weeks. The results of this scan will help you and your doctor plan the safest way for you to give birth.
Medication
If you have placental praevia, there is a risk you may give birth prematurely. So you may be offered a course of steroid injections between 34 and 36 weeks of pregnancy to help your baby’s lungs to become more mature.
So you may be offered a course of steroid injections between 34 and 36 weeks of pregnancy to help your baby’s lungs to become more mature.
If you do go into labour early, you may be offered medication to try to stop your contractions. This will give you time to have a course of steroid injections. If you have severe bleeding or progressing labour your baby may need to be delivered.
If you have vaginal bleeding, you may need to be admitted to hospital. This is because there is a small risk that you could bleed suddenly and heavily. If this happens, you may need an emergency caesarean section.
What do I need to do if I have a low-lying placenta?
If you know you have a low-lying placenta, you should contact the hospital immediately if you have:
- vaginal bleeding, including spotting
- contractions
- pain, including any vague, period-like aches.
If you have any bleeding, your doctor may need to do an internal examination to check where it’s coming from.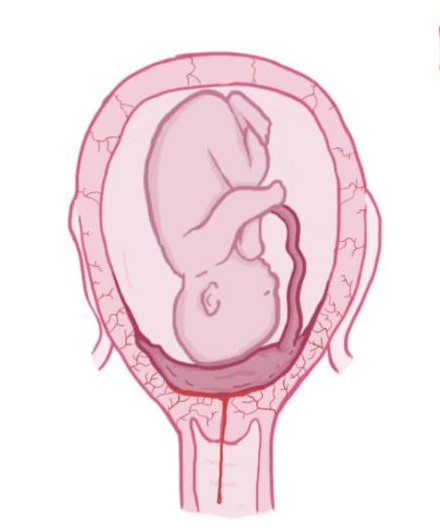 This is safe and they will ask for your permission before they start.
This is safe and they will ask for your permission before they start.
Anaemia
Anaemia is a blood condition that develops when you don’t have enough red blood cells. Red blood cells contain haemoglobin, a protein that carries oxygen around your body and to your baby.
If you have a low-lying placenta, it’s important to try to avoid developing anaemia, which can be common in pregnancy. Eating a healthy, balanced diet will help you either prevent or manage anaemia. Iron supplements may also help, if your healthcare team recommends them.
How will my baby be born?
Your healthcare team will talk to you about what your options are for giving birth.
You may be advised to give birth early if you have any heavy bleeding before your due date.
If the edge of your placenta is very close (less than 20mm) to your cervix (entrance to the womb), the Royal College of Obstetricians and Gynaecologists state that the safest way to give birth is by caesarean section.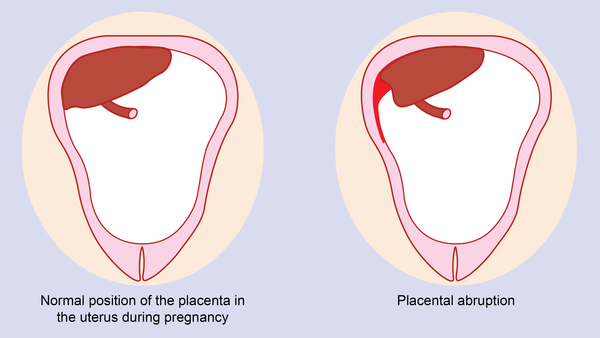 This will usually be between 36 and 37 weeks. Your doctor will discuss your options with you, but how you give birth is ultimately your decision. But if you have had vaginal bleeding during your pregnancy, you may be advised to have your caesarean earlier than this.
This will usually be between 36 and 37 weeks. Your doctor will discuss your options with you, but how you give birth is ultimately your decision. But if you have had vaginal bleeding during your pregnancy, you may be advised to have your caesarean earlier than this.
If the placenta is further than 20mm from your cervix, you may be able to have a vaginal birth if you want one.
If you are having a caesarean section, a senior obstetrician (a doctor who specialises in pregnancy) will be there. This is because you may have heavy bleeding during the surgery. If this happens, you may need a blood transfusion. This is more likely if you have placenta praevia.
Talk to your doctor before your surgery if, for any reason, you do not want a blood transfusion.
Unfortunately, complications are more common in caesarean sections if you have a low-lying placenta. Your doctor should talk to you about the risks of major bleeding and hysterectomy (removal of the womb) before your caesarean. For most women, the risk of hysterectomy is low and will only occur as a last resort if other measures to control bleeding are not effective.
For most women, the risk of hysterectomy is low and will only occur as a last resort if other measures to control bleeding are not effective.
If you have placenta praevia:
- you are at higher risk of having your baby early (less than 37 weeks).
- your baby will need to be born by caesarean section because the placenta is blocking the birth canal.
Your mental health
Being diagnosed with complications in pregnancy can be hard. And being asked to look out for certain symptoms, such as bleeding, and needing extra appointments and check-ups can cause anxiety and stress. It may also be a lonely experience when those around you don’t understand what it’s like.
Remember that you can tell your midwife or doctor how you feel. They will do their best to reassure you and answer any questions you may have.
You can also call our pregnancy line on 0800 014 7800 (Monday to Friday, 9am to 5pm), or email us at [email protected]
If you are struggling to cope, there is professional support available. Don’t suffer in silence. Tell your midwife or GP how you feel. They will help you access the support you need.
Don’t suffer in silence. Tell your midwife or GP how you feel. They will help you access the support you need.
Find out more about looking after our mental health in pregnancy.
Abdominal decompression
Abdominal decompression is performed in our antenatal clinic.
Abdominal decompression is a physiotherapy procedure performed by therapeutic application of reduced (negative) air pressure to the lower body.
Abdominal decompression procedures are used to treat threatened miscarriage, pregnancy-induced edema and hypertension; hypotrophy and hypoxia of the fetus, inflammatory diseases of the internal genital organs, dysmenorrhea, infantilism, infertility, with simultaneous prevention of varicose veins of the lower extremities.
Abdominal decompression allows you to:

Advantage over traditional methods of treatment:
An important factor in local decompression is the increased transport of oxygen and metabolites, which ensures the normalization of placental function and the removal of fetal hypoxia. At the same time, a change in volumetric blood flow in the abdominal organs relieves vascular spasm caused by hypertension. The therapeutic effect is also achieved as a result of improved blood supply to the kidneys.
Your attending obstetrician-gynecologist will examine you, determine the indications and contraindications for abdominal decompression.
Indications for abdominal decompression treatment:
Contraindications:
The procedure is as follows. The woman is placed horizontally in a special apparatus resembling a hermetic dome-shaped chamber in such a way that the chamber contains the lower part of the body up to the level of the chest. Upper body and head rest comfortably on the couch. Through the control of a specially designed computer program, a negative, pulsating pressure is created inside the chamber. The doctor individually selects a set of all necessary indicators to achieve the optimal effect of the procedure. The duration of the procedure is 20-30 minutes.
The referral for abdominal decompression is given by the local obstetrician-gynecologist of the antenatal clinic or the attending physician in the pregnancy pathology department. The date and time of the procedure will be determined by the doctor performing the abdominal decompression.
Abdominal decompression is carried out in the antenatal clinic, in room No. 16
(2nd floor) every day except Saturday and Sunday.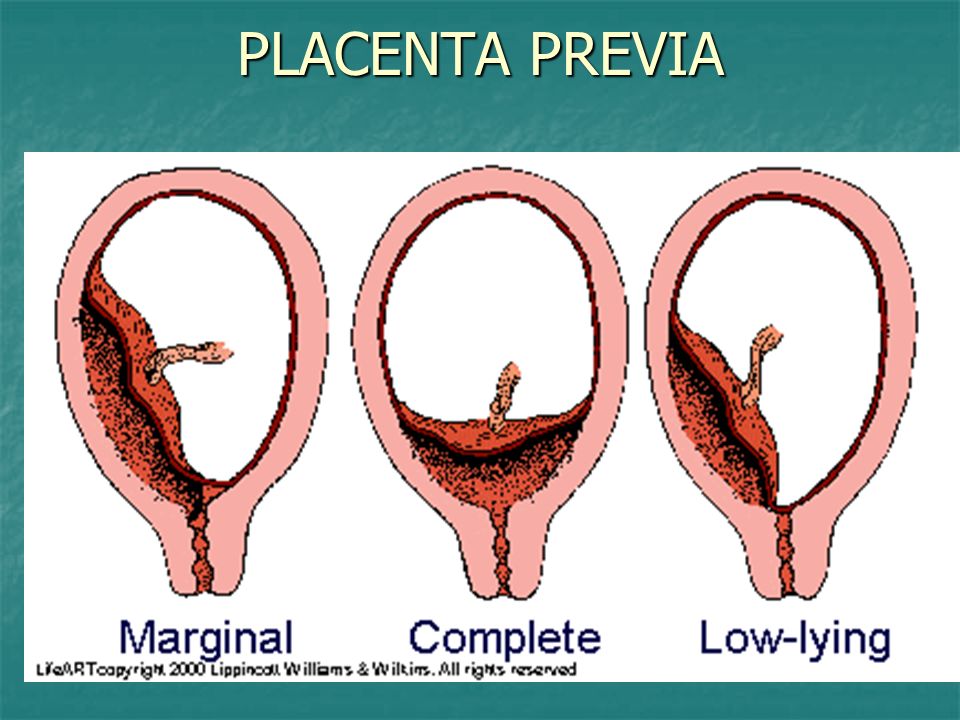
Time of the procedure: from 10 am to 2 pm.
You must have a referral from a doctor, a change of shoes, cotton socks and trousers with you.
Increased uterine tone during pregnancy
Nicotine constricts the blood vessels of the future mother, as well as the vessels of the placenta and umbilical cord, through which the fetus is nourished. Of course, smoking by itself is unlikely to lead to hypertonicity, but in combination with other factors, it may well
If the work is associated with constant stress, it has harmful effects or it is physically difficult, give it up as soon as possible. If this is not possible, use your rights, which are enshrined in the labor legislation of the Russian Federation
Hypertonicity must be distinguished from Braxton-Hicks contractions: it lasts much longer than these training contractions and usually does not go away on its own (or goes away only after some long time)
what is hypertonicity
, - muscle, and according to the laws of physiology, muscle tissue is reduced under the influence of any factor.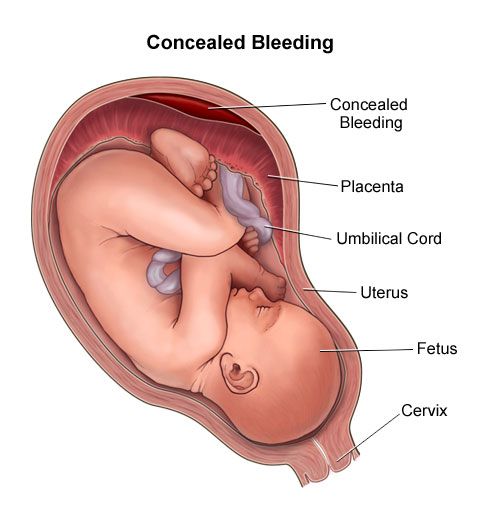 Slightly the uterus contracts in women every month during menstruation, much stronger during labor pains. The uterus can also contract during pregnancy, doctors call this condition hypertonicity. What it looks like: suddenly, at some point, a woman feels that her stomach is tense, becomes hard, as if “hardening”. This state lasts for a long time - half an hour, an hour, half a day or even all day. Additionally, discomfort (or pain) in the lower back or sacrum may also appear. It is clear that such tension in the abdomen worries the mother, because since the uterus is contracting, then perhaps there is a threat of termination of pregnancy. But here it all depends on how much and how often the stomach tenses.
Slightly the uterus contracts in women every month during menstruation, much stronger during labor pains. The uterus can also contract during pregnancy, doctors call this condition hypertonicity. What it looks like: suddenly, at some point, a woman feels that her stomach is tense, becomes hard, as if “hardening”. This state lasts for a long time - half an hour, an hour, half a day or even all day. Additionally, discomfort (or pain) in the lower back or sacrum may also appear. It is clear that such tension in the abdomen worries the mother, because since the uterus is contracting, then perhaps there is a threat of termination of pregnancy. But here it all depends on how much and how often the stomach tenses.
Braxton-Hicks contractions
It turns out that the stomach can tense up not only when there is a threat of miscarriage. Starting from the end of the second trimester, the expectant mother can feel the so-called training contractions (Brexton-Hicks contractions) - the stomach also tenses with them for a while, as if “hardening”, - in general, the sensations are the same as with hypertonicity. But the main difference between such contractions and hypertonicity is that they last for a very short time (a few seconds - a couple of minutes) and pass by themselves, as well as if you change the position of the body or take a shower. Braxton-Hicks contractions occur up to about ten times a day, and by the end of pregnancy they appear even more often. These contractions are completely normal during pregnancy, and they do not indicate any threat of interruption. It’s just that with their help, the uterus, as it were, prepares (trains) for childbirth.
But the main difference between such contractions and hypertonicity is that they last for a very short time (a few seconds - a couple of minutes) and pass by themselves, as well as if you change the position of the body or take a shower. Braxton-Hicks contractions occur up to about ten times a day, and by the end of pregnancy they appear even more often. These contractions are completely normal during pregnancy, and they do not indicate any threat of interruption. It’s just that with their help, the uterus, as it were, prepares (trains) for childbirth.
where does hypertonicity come from
Hypertonicity can appear in any trimester of pregnancy. In the early stages, it occurs more often due to the fact that there is not enough progesterone, a hormone that is needed for the normal course of pregnancy. Another cause of hypertonicity is some changes in the uterine wall, for example, fibroids (a knot of uterine muscle tissue), endometriosis (growth of the uterine mucosa into the thickness of the wall), and inflammatory diseases. In these situations, the wall of the uterus is not able to stretch as it should. At later dates, hypertonicity can develop, on the contrary, with overstretching of the uterus (with polyhydramnios, large fetuses, multiple pregnancies). Very often, hypertonicity is provoked by some kind of physical activity too strong for a woman, for example, if, in a fit of “nesting”, the mother suddenly began to move and rearrange something in the apartment herself, or she simply moved for a very long time without resting. Someone hypertonicity occurs after psychological overstrain.
In these situations, the wall of the uterus is not able to stretch as it should. At later dates, hypertonicity can develop, on the contrary, with overstretching of the uterus (with polyhydramnios, large fetuses, multiple pregnancies). Very often, hypertonicity is provoked by some kind of physical activity too strong for a woman, for example, if, in a fit of “nesting”, the mother suddenly began to move and rearrange something in the apartment herself, or she simply moved for a very long time without resting. Someone hypertonicity occurs after psychological overstrain.
how to recognize hypertonicity
Hypertonicity must be distinguished from Braxton-Hicks contractions - as mentioned earlier, it lasts much longer than these training contractions and usually does not go away by itself (or goes away only after some long time). But if the mother cannot understand whether she has hypertension or not, you should consult a doctor. If there is still an increased tone of the uterus, the doctor, simply by placing his hand on his stomach, will feel a seal, tension, up to the feeling of a stone at hand.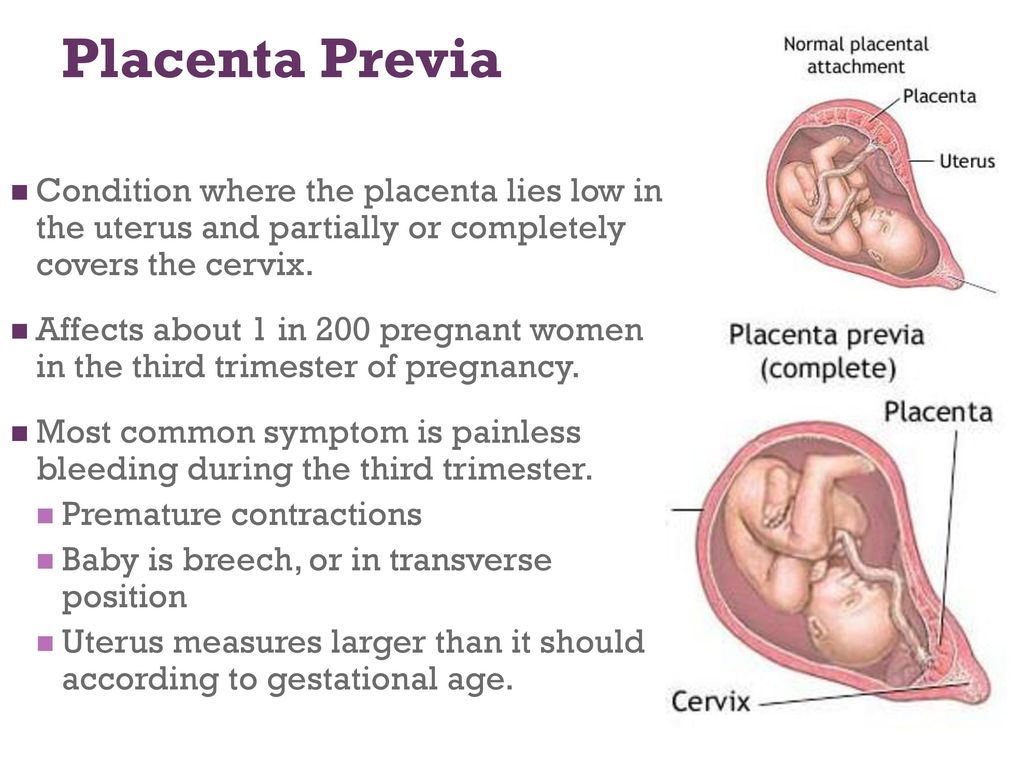 In addition, you can always do an ultrasound, on which, with hypertonicity, areas of local thickening of the muscular layer of the uterus are visible, and also look at the cervix, by the state of which you can also judge whether there is a threat of abortion or not.
In addition, you can always do an ultrasound, on which, with hypertonicity, areas of local thickening of the muscular layer of the uterus are visible, and also look at the cervix, by the state of which you can also judge whether there is a threat of abortion or not.
what to do in case of hypertonicity
If it appears, the first thing you need to do is:
1. Calm down and lie down if possible. Do not panic, extra stress will not bring any benefits, especially since without consulting a doctor it is still not clear whether there is hypertonicity and how pronounced it is. Or maybe it's a false alarm? In addition, you can use relaxation techniques (breathing, auto-training, etc.).
2. Call your doctor. Of course, the doctor will not make a diagnosis in absentia, but since he knows the history of the expectant mother, her real or possible problems, he will be able to give the right direction for further action.
3. If it is not possible to contact your doctor, you can contact any clinic or antenatal clinic where pregnant women are treated. If medical institutions are already closed (late evening, at night), you can call an ambulance - she will take you to the nearest hospital or maternity hospital (you can also get there by taxi).
If medical institutions are already closed (late evening, at night), you can call an ambulance - she will take you to the nearest hospital or maternity hospital (you can also get there by taxi).
4. Hypertonicity is well eliminated by special medicines that relax the uterus (tocolytics), and if the doctor has prescribed them, then you should not be afraid to take them: they help quickly enough and do not harm the child.
how to prevent hypertonicity
There are simple rules that can prevent or reduce the risk of hypertonicity:
1. Quit smoking, watch your weight, do not eat surrogate foods. No matter how trite it may sound, but it is a healthy lifestyle that is the basis of our well-being.
2. Distribute your forces correctly. Laundry, cooking can wait if the expectant mother suddenly feels that she needs a rest. If any activities require physical or psychological stress, cancel them for a while. Do not attend events or places where you may feel uncomfortable, reduce communication with people that are unpleasant for you.