Miscarriage jelly like blood clots during period
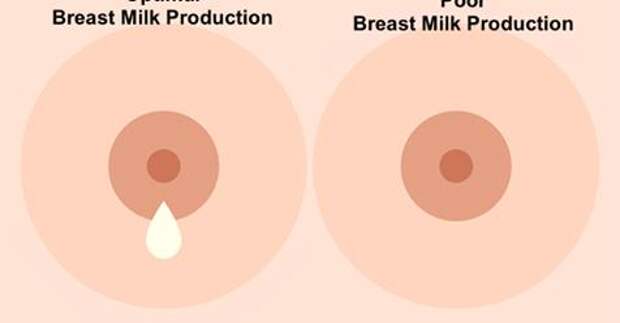
What does a miscarriage look like? Symptoms and seeking help
Miscarriage, or pregnancy loss, can look and feel different for each person. Common symptoms include bleeding and cramping.
It is important to note that bleeding is common during pregnancy — especially in early pregnancy. It does not necessarily mean that anything is wrong.
The only way to accurately identify a pregnancy loss is to test pregnancy hormone levels and have an ultrasound of the uterus.
Read on to learn more about what pregnancy loss can look and feel like.
According to a 2016 study, not all pregnancy losses involve bleeding. Overall, they do not follow a single pattern. This is why it is crucial to seek medical care for bleeding and any unusual symptoms during pregnancy.
Pregnancy loss during the first trimester may involve:
- heavy bleeding
- bleeding that starts light and gets heavier
- passing blood clots or tissue
- cramping, which may come in waves
- a gush of fluid from the vagina
If a person takes a pregnancy test after experiencing a pregnancy loss during the first trimester, the result may be negative, or the test may have a positive line that gets fainter.
Experiencing pregnancy loss later in the first trimester and beyond will involve passing more tissue.
Second-trimester pregnancy loss can also cause intense cramping and sometimes even contractions.
In addition to bleeding and cramping, some people may notice larger blood clots.
According to a 2019 meta-analysis, one-quarter of pregnant women experience bleeding during the first trimester. Another study from 2016 puts that percentage higher, at closer to 20–40%.
A large-scale 2010 study found that about 12% of pregnant women experienced pregnancy loss, and about two-thirds of that group reported bleeding during their pregnancy.
Some differences between bleeding due to a pregnancy loss and other types of bleeding during pregnancy include:
- Amount of blood: Heavy bleeding is more likely to signal a pregnancy loss.
- Bleeding pattern: Bleeding that gets progressively heavier may indicate a pregnancy loss.
- Pain: Cramping, especially when it occurs in a clear pattern, is more likely to signal a pregnancy loss.
- Passing tissue: Some — not all — people who experience a pregnancy loss pass large blood clots or tissue.
For people who do experience bleeding during a pregnancy loss, the duration tends to depend on how far the pregnancy has progressed.
Pregnancy losses that occur in the first weeks of pregnancy tend to cause bleeding that lasts a few days. Those that occur later may cause bleeding that lasts for as long as 4 weeks.
Sometimes, the bleeding stops and starts again. Over time, it should get lighter.
A very early pregnancy loss is sometimes called a chemical pregnancy. These pregnancies are lost shortly after the embryo implants, usually within a few days or weeks.
A chemical pregnancy may be detectable by a pregnancy test, but it would likely not be seen on an ultrasound.
In many cases, early pregnancy losses can happen before a person knows they are pregnant.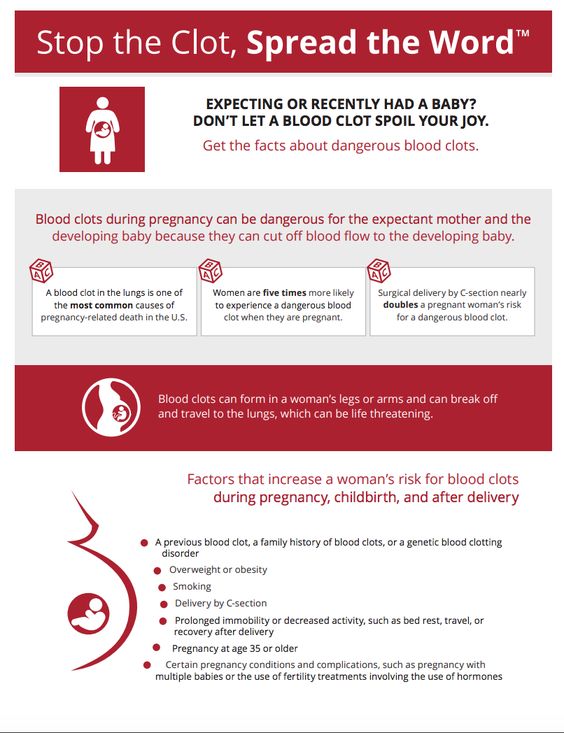
In fact, around 80% of early pregnancy losses occur in the first trimester, or in weeks 0–13. The end of these early pregnancies may be mistaken for a period because the symptoms are similar.
For example, both a period and an early pregnancy loss can involve bleeding and cramping. Pregnancy tissue that passes out of the vagina may look like typical blood clots that occur during a period.
It is possible that a person will not realize they have missed a period. Instead, they may mistake the symptoms of a pregnancy loss for those of a menstrual period.
Pregnancy losses and periods can both cause:
- vaginal bleeding
- passing blood clots or tissue
- abdominal pain
However, a pregnancy loss will often cause additional symptoms that set it apart from a period, especially if the pregnancy loss occurs several weeks into the pregnancy. These symptoms include:
- larger clots or pregnancy loss tissue
- more clots than typical periods
- lower abdominal cramping
- back pain
- passing a significant amount of clear or pinkish fluid
- sudden heavy bleeding, or heavier bleeding than a typical period
- longer bleeding
- sudden easing of some early pregnancy symptoms, such as nausea and breast tenderness
It is important to remember that bleeding during the first weeks of a pregnancy is not uncommon, and it is not always a sign of pregnancy loss or a problem with a pregnancy.
However, if a person experiences other symptoms of pregnancy loss, they should seek care from a doctor.
A “missed miscarriage” refers to a delay between the loss of the pregnancy and any bleeding or passing of tissue.
During a missed miscarriage, an embryo dies but does not leave the uterus for several weeks. In fact, a pregnant person may not realize the pregnancy has ended until an ultrasound finds no heartbeat.
When the embryo does leave the uterus, the blood, tissue, and clots may be dark brown. The tissue has had time to deteriorate, so bright red blood or heavy bleeding may not occur. The bleeding may last several days to several weeks.
A doctor may prescribe medication to help the person who has had the pregnancy loss bleed and pass the tissue. Surgery may also be necessary.
It is not possible for healthcare professionals to stop a pregnancy loss once it starts.
Call a doctor and schedule an appointment within 24 hours if any of the following occur:
- vaginal bleeding
- a fever
- intense pain or cramping
- bleeding that stops and starts again
- any other changes in the pattern of bleeding, even if a doctor has already addressed the cause
- bleeding that lasts for longer than 7 days, even if a doctor has already confirmed pregnancy loss
Pregnant people should receive emergency medical attention if they:
- experience heavy bleeding during the second trimester and cannot reach their doctor
- bleed heavily enough to soak through more than one pad per hour for more than 2 hours
- feel faint, lightheaded, or confused
- experience contractions, amniotic fluid leakage, the water breaking, or other signs of premature labor
Most pregnancy losses pass on their own.
In some cases, the fetus dies without causing any bleeding. When this happens, the person carrying the fetus may want to wait for the pregnancy to pass on its own or want it to be over as quickly as possible.
If a person wants to expedite a pregnancy loss, a doctor can supply medication that helps with passing the pregnancy at home. This approach is safest during early pregnancy.
A healthcare professional can also perform surgery to remove the remains of the embryo or fetus.
Sometimes a pregnancy loss is incomplete, leaving behind tissue that can lead to infection or other health problems. When this happens, a doctor may recommend medication or surgery.
Doctors used to advise couples to wait 1 month, or sometimes much longer, before trying to conceive again after a pregnancy loss.
However, research now shows that there is no medical justification for this recommendation. If a couple feels ready, it is safe to begin trying to conceive again right away.
A 2017 study indicates that fertility may even be slightly higher immediately following a pregnancy loss.
Sometimes, however, it takes a while for a menstruating person’s cycle to resume following a pregnancy loss.
This can make it difficult to time sexual intercourse for conception and to accurately date a pregnancy — especially if a person becomes pregnant before the first menstrual period after a pregnancy loss.
To improve accuracy, it can be helpful to:
- monitor basal body temperature
- use ovulation tests
- try other ways to predict fertility
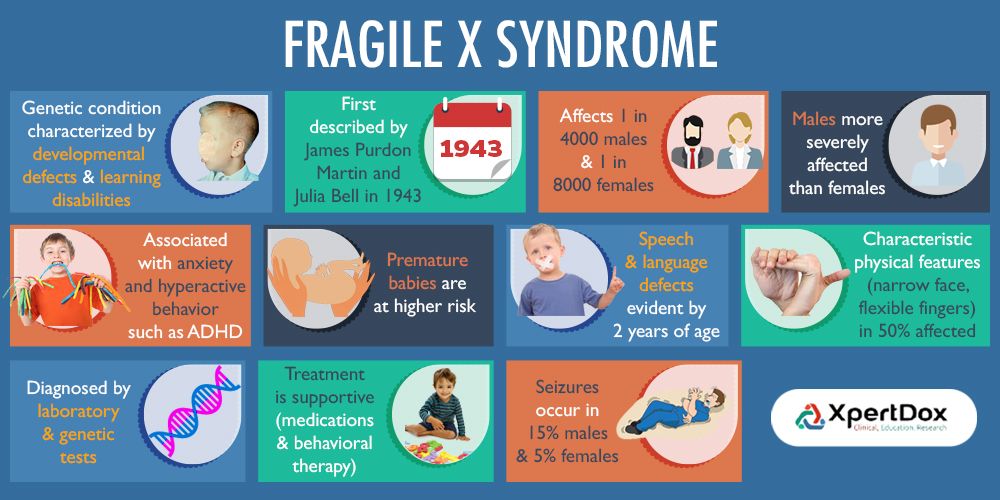
Early pregnancy losses can sometimes result from chromosomal irregularities. This means that the developing embryo or fetus has an irregular number of chromosomes.
These irregularities usually occur at random, meaning they are unlikely to reoccur. In other words, experiencing one pregnancy loss does not increase the likelihood of experiencing another.
A 2017 study finds that 15. 7% of women with a previous pregnancy loss had another during the 2-year study period.
7% of women with a previous pregnancy loss had another during the 2-year study period.
Meanwhile, a 2016 study finds that women were more likely to become pregnant in the 3 months following a pregnancy loss.
Many people become pregnant again shortly after a pregnancy loss, and a smaller number experience multiple losses in a row.
The risk of repeat pregnancy losses increases with age, according to a 2019 study. The risk is also higher among people with a history of:
- preterm labor
- gestational diabetes
- stillbirth
- cesarean delivery
A 2017 study found that 15.7% of participants whose most recent pregnancy ended in a pregnancy loss went on to have a second pregnancy loss.
A 2018 study focused on women who had three or more pregnancy losses. This study found that 64.5% of those women had a live birth within 5 years. Some of these participants may have received fertility treatments.
Pregnancy loss is one of the less common causes of bleeding during pregnancy, especially when the bleeding occurs early on.
But bleeding in early pregnancy is not always a sign of pregnancy loss.
Some other signs of pregnancy loss include cramping and passing blood clots or tissue.
Only a healthcare professional can accurately identify a pregnancy loss. For this reason, it is important to consult a doctor or nurse midwife about any bleeding during pregnancy.
What does an early miscarriage look like?
Bleeding is common in the early weeks of pregnancy. That is why bleeding alone should not be seen as an indication of an early pregnancy loss.
In addition to bleeding, an early pregnancy loss may cause a person to experience:
- a gush of clear or pale pink fluid from the vagina
- passing blood clots or tissue
- a sudden decrease in pregnancy symptoms (such as nausea and morning sickness)
- a negative result on a pregnancy test, or a positive sign that is very faint
How do I know if I’m miscarrying?
The signs and symptoms of a pregnancy loss will remain largely the same, no matter the week.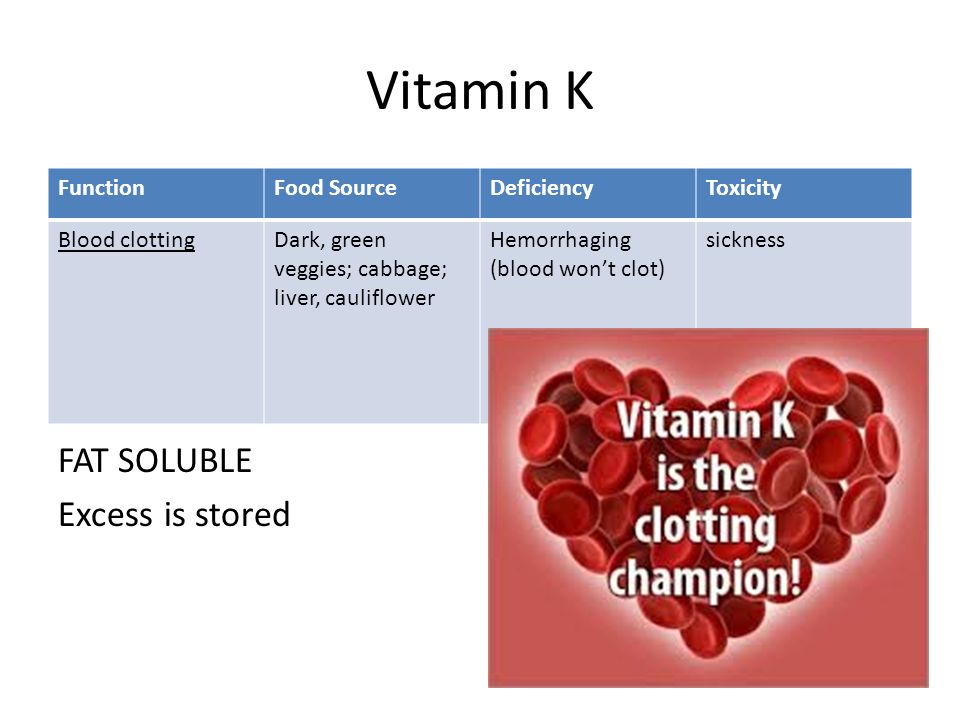 But the further along a person is, the greater the amount of tissue loss during the miscarriage.
But the further along a person is, the greater the amount of tissue loss during the miscarriage.
Symptoms of pregnancy loss include:
- sudden bleeding, sometimes heavy
- a gush of clear or pink fluid from the vagina
- mild to severe back pain and abdominal cramping
- contraction-like pain
What does miscarriage tissue look like?
The clots and tissue passed during a pregnancy loss may look like typical period clots, or they may be larger.
Pregnancy loss tissue includes:
- the fetus or embryo
- gestational sac
- placenta
When a pregnancy is more advanced (after 6 to 8 weeks), the gestational sac may be noticeable. Before that, it may be too small to see.
The tissue passed during a pregnancy loss may be:
- brown
- black
- dark red
- bright red or pink
- white or gray, in some cases
If the pregnancy began to deteriorate before the start of bleeding, the clots may be smaller and darker. This is common with a missed miscarriage.
This is common with a missed miscarriage.
What does miscarriage tissue vs. a blood clot look like?
It is not always easy to tell the difference between pregnancy loss tissue and a blood clot. Both may look like typical period clots, though it is not uncommon for them to be larger than normal.
Actual pregnancy tissue may not be discernible until after the eighth week. Then, the tissue may look like pink, white, or gray tissue. A person may also be able to see a fluid-filled sac in the passed tissue.
Bleeding, Clots, Timing, and Other Signs
Miscarriage is fairly common in the first trimester. It happens in about 10 percent of known pregnancies.
In some cases, miscarriage can occur before you know you’re pregnant. If this happens, you might not notice anything different from your usual period.
The further along you are in a pregnancy, the less likely it is that a miscarriage will feel like a period.
Continue reading to learn more about early miscarriage, including specific symptoms to watch for, when you should see a doctor, and more.
The most common symptoms of early miscarriage are cramping and bleeding.
However, spotting or light bleeding during early pregnancy aren’t always a sign of miscarriage. If this happens, watch for any other unusual symptoms.
Other symptoms of miscarriage
- cramping in your abdomen or lower back (This could start out like period cramps, but the pain typically worsens over time.)
- nausea
- diarrhea
- passing fluids, larger-than-normal blood clots, or tissue from your vagina
Timing
A miscarriage can happen any time after fertilization. If you didn’t know you were pregnant, it would be easy to mistake it for a period.
Both a period and a miscarriage can cause spotting to heavy bleeding.
After the first eight weeks or so, it’s less likely that you’ll mistake a miscarriage for a period.
Duration
You know how long and heavy your typical period is.
During a miscarriage, bleeding gets heavier and lasts longer than a period.
As your cervix starts to dilate, cramping may become more painful than typical period cramping.
Characteristics
Bleeding during miscarriage can appear brown and resemble coffee grounds. Or it can be pink to bright red.
It can alternate between light and heavy or even stop temporarily before starting up again.
If you miscarry before you’re eight weeks pregnant, it might look the same as a heavy period. Later, you’re more likely to notice fetal or placental tissue.
Menstruation products
Heavy bleeding, pieces of tissue, or large blood clots on your menstruation products could mean that you’re having more than a heavy period.
See a doctor if you’re soaking through a tampon or pad every hour for more than two consecutive hours.
You should call a doctor or other healthcare provider any time you experience unexpected pain or excessive bleeding.
These symptoms can result from an ectopic pregnancy. This occurs when a fertilized egg has implanted outside the uterus, possibly inside a fallopian tube. It’s a medical emergency.
It’s a medical emergency.
You should also call a doctor if you experience bleeding alongside:
- mucus
- tissue
- blood clots
- what feels like uterine contractions
If you believe you’re having a miscarriage, ask your doctor the following:
- Should I collect a sample of blood or tissue? (This isn’t always necessary.)
- Should I go to an emergency room or make an office appointment?
- Is it fine to drive myself, or do you recommend against it?
If it appears that you’ve had a miscarriage, your doctor will want to perform a physical exam.
Be sure to discuss all your symptoms, including the amount of:
- bleeding
- clotting
- pain
- any tissue that may have been expelled
Testing may include:
- an ultrasound to check the uterus for signs of an embryo or a heartbeat
- a blood test to check for human chorionic gonadotropin (hCG), a substance that indicates pregnancy
There’s no way to stop a miscarriage in progress.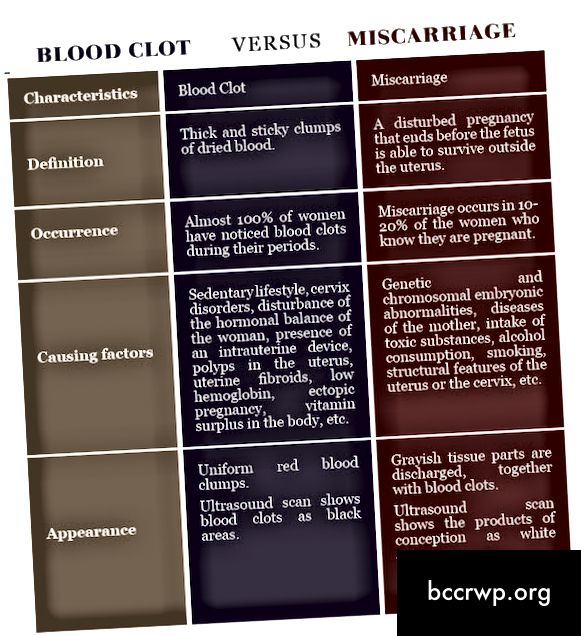 If your doctor determines that you’ve experienced a miscarriage, they’ll want to check for:
If your doctor determines that you’ve experienced a miscarriage, they’ll want to check for:
- signs of infection
- uncontrollable bleeding
- tissue that may be left in your uterus
It can take two weeks or more to completely expel the tissue naturally. Your doctor will review with you typical bleeding patterns to expect. If you have heavy bleeding lasting several days or any signs of infection, you may need medical treatment.
If your doctor isn’t sure that all of the pregnancy tissue has been cleared from your uterus, they may order an ultrasound to confirm.
Your doctor can prescribe medication, such as misoprostol (Cytotec), to increase uterine contractions to help you expel the tissue.
You’ll experience cramping and bleeding as you pass tissue and blood.
Most people pass the tissue within 24 hours after taking the drug. For others, it can take a few days to complete. Either way, it doesn’t require a hospital stay.
Your doctor may be able to prescribe pain medication to help ease your symptoms.
If your blood type is Rh negative, you’ll need an injection of Rh immunoglobulin. This may help prevent complications in a future pregnancy.
There are also a few surgical options to remove tissue from the uterus. This includes:
- Vacuum aspiration. Your doctor inserts a thin tube that contains a suction device into your uterus. This can be done with local anesthesia in your doctor’s office.
- Dilation and curettage (D&C). Your doctor dilates your cervix, and then uses an instrument called a curette to scrape your uterine lining. This can be done at a surgical center or operating room on an outpatient basis. Regional or general anesthesia can be used.
Both of these treatments have been well-studied and are considered safe. They each carry a very small risk of serious complications.
If you’ve experienced a miscarriage, it’s important to understand that it isn’t your fault.
In many cases, doctors are unable determine the cause. Here are some things that can contribute to miscarriage:
Here are some things that can contribute to miscarriage:
During the first trimester
As many as 80 percent of miscarriages occur in the first trimester.
When a miscarriage occurs in the first five weeks after fertilization, it’s called a “chemical pregnancy.” It’s so early that you might not have known you were pregnant.
Although your period may seem heavier than usual, there might not be any other noticeable sign of miscarriage.
Miscarriages in the first trimester often have to do with chromosome abnormalities that interfere with normal development. Missing or extra chromosomes are linked to 50 percent of all miscarriages.
Sometimes, a fertilized egg simply doesn’t develop into an embryo (blighted ovum).
It may help to know that having sex, exercising, morning sickness, and previous use of oral contraceptives don’t cause miscarriage. Even an accidental fall doesn’t necessarily cause it.
According to the American College of Obstetricians and Gynecologists (ACOG), smoking and alcohol consumption in the first trimester may result in a slightly higher risk of miscarriage. But the research on this is mixed.
But the research on this is mixed.
It’s also worth noting that drinking less than 200 milligrams of caffeine per day doesn’t appear to increase the risk of miscarriage.
Some things that may increase the risk of early miscarriage are:
- fibroids or other abnormalities of the uterus
- hyperthyroidism or hypothyroidism
- uncontrolled diabetes
- use of cocaine or similar drugs
During the second trimester
About 2 to 3 percent of miscarriages occur during the second trimester.
Some things that may increase the risk are:
- conditions that can cause blood clots
- early preeclampsia or eclampsia
- fetal abnormalities
- fibroids or other abnormalities of the uterus
- infection of the uterus
- lupus
- prior surgery of the cervix
- trauma
- uncontrolled diabetes
- hyperthyroidism or hypothyroidism
- high blood pressure
- use of cocaine or similar drugs
During the third trimester
Losing a pregnancy starting from the 20th week of pregnancy and into the third trimester is considered stillbirth, not miscarriage.
In general, the risk of stillbirth increases with maternal age.
If you’ve experienced a miscarriage, it doesn’t mean you’ll have another, and it doesn’t mean you can’t have children.
Most people who experience a miscarriage can go on to have a successful pregnancy.
Miscarriage shouldn’t affect your ability to get pregnant. You can ovulate and become pregnant within two weeks of an early miscarriage.
If you don’t want to become pregnant again, you should use birth control right away.
About 1 percent of people have multiple miscarriages. If you’ve experienced several miscarriages, your doctor might recommend special testing.
Even if you’ve had three miscarriages in a row, there’s a 70 percent chance your next pregnancy will be successful.
Your doctor will probably advise you to avoid sex, tampons, and douches for two weeks. This will help prevent infection.
They may also want you to take a pregnancy test after about two weeks. This can help them determine whether your hormone levels are back to normal.
This can help them determine whether your hormone levels are back to normal.
In the meantime, call your doctor if you:
- are bleeding heavier than expected or notice that the blood stays bright red
- are soaking through more than two maxi pads an hour for more than two hours
- notice a foul-smelling discharge
- experience abdominal tenderness or severe pain
- have persistent cramping
- develop a fever or chills
For the first few days, you may notice blood clots and tissue passing, but this should taper off after about a week. It will take about four to eight weeks for your regular period to return.
Mild exercise following an early miscarriage is usually fine, but check with your doctor. It may depend on how far along you were, as well as your overall health.
There are many emotions a person might have following a miscarriage. Some feel anger, sadness, or profound loss. Others might feel relieved.
These feelings may have to do with whether you knew you were pregnant or if you were trying to have a baby.
Pregnancy and miscarriage also cause hormone fluctuations, which can affect your emotions.
Everyone is different, so there’s no correct way to feel about experiencing a miscarriage. It may take some time for you to process everything.
You may find it helpful to talk to your partner, family, or friends about what you’re going through.
You may also consider looking into support groups for people who have experienced miscarriage. Sometimes it helps to talk to others who have been through the same thing.
Here are a few places to seek support:
- your doctor’s office or local hospital for referrals to support services
- clergy
- Compassionate Friends, which has a searchable database of local chapters
- March of Dimes Loss and Grief Forum
- Share Pregnancy & Infant Loss Support which offers online support and information on how to find local groups
If grief continues to worsen after a few weeks, talk to a doctor about your options for treatment. You may benefit from grief counseling or treatment for depression.
You may benefit from grief counseling or treatment for depression.
Miscarriage isn’t your fault.
Physical recovery generally takes a few weeks. Everyone has their own timetable for emotional recovery.
There’s no need to rush yourself or to pretend to “get over it” for anyone else’s sake.
And if you need it, reaching out for support is a reasonable thing to do. You aren’t alone in this.
Blood clots during menstruation, why large blood clots can come out during menstruation, what to do
Contents
- Physiological causes
- Predisposing factors
- When do blood clots during menstruation indicate gynecological pathology?
Normal menstruation is the basis of a woman's reproductive health. The concept of the norm includes regular (every 21–35 days) painless menstruation, during which 40–150 ml of blood is released within 3–7 days. Menstrual flow has a dark red or brownish (at the end of the cycle) color and a uniform consistency. 1
1
Any deviation from the specified parameters should alert the woman. One of the most common concerns is blood clots during menstruation
PHYSIOLOGICAL CAUSES
Menstruation occurs after an egg produced by the female body has not been fertilized. The inner layer of the uterus (endometrium), where the embryo was supposed to be fixed, is rejected. Menstrual flow is thicker than normal blood, precisely due to the content of endometrial tissue in them. Why can blood clots form during menstruation in absolutely healthy women? The fact is that when walking and other active movements, menstruation comes out gradually and freely. However, after a night's sleep or sitting for a long time, a woman may notice the release of one or more jelly-like clots. This happens because the blood lingers in the uterus and has time to clot. Also, the appearance of thickening contributes to a large amount of secretions. The alternation of heavy and scanty menstruation is characteristic of periods of hormonal changes (puberty, premenopause).
PREDISPOSING FACTORS
In order to understand why menstruation comes with blood clots, we list the possible causes of this process:
Hormone therapy, taking oral contraceptives. The appearance of such a side effect of drugs as increased menstrual bleeding is often observed with the independent use of drugs without consulting a gynecologist.
Hormone therapy, oral contraceptives. The appearance of such a side effect of drugs as increased menstrual bleeding is often observed with the independent use of drugs without consulting a gynecologist.
First menstruation after abortion or gynecological surgery.
Heavy periods may be the only symptom of early miscarriage. Elements of the fetal egg, which look like a small clot, can be detected by a woman, but more often go unnoticed.
WHEN DO THE BLOOD CLOTTS DURING THE TIME SAY ABOUT GYNECOLOGICAL PATHOLOGY?
The main pathological causes of this process are:
- Endometriosis is the growth of endometrial-like tissue outside the uterus.
 A variation of this disease is adenomyosis, in which the inner lining of the uterus grows into its muscle tissue. Both of these pathologies are accompanied by pain in the lower abdomen and heavy prolonged menstruation. If during menstruation a large blood clot came out, resembling a liver in appearance, then there is reason to suspect that the patient has one of these diseases.
A variation of this disease is adenomyosis, in which the inner lining of the uterus grows into its muscle tissue. Both of these pathologies are accompanied by pain in the lower abdomen and heavy prolonged menstruation. If during menstruation a large blood clot came out, resembling a liver in appearance, then there is reason to suspect that the patient has one of these diseases. - Uterine polyps - focal hyperplasia of the endometrium in the form of single or multiple formations on a wide base or on a stalk. One of the manifestations of the disease is an increase in the amount of menstrual flow. The appearance of large clots is especially often caused by a polyp, which is located on the cervix, as it prevents the timely release of secretions.
- Uterine fibroids. The growth of this benign tumor-like formation leads to the appearance of pain, as well as lengthening and intensification of menstrual bleeding.
In addition, blood during menstruation may be released more slowly and thicken in some congenital pathologies. These include such anomalies in the structure of the female genital organs, such as a saddle, bicornuate or septate uterus.
These include such anomalies in the structure of the female genital organs, such as a saddle, bicornuate or septate uterus.
WHAT TO DO IF THERE IS BLOOD CLOTS?
In case of any changes in the nature of menstruation (their frequency, duration, consistency, etc.), a woman should visit a gynecologist. In the event that large blood clots come out during menstruation, this must be done as quickly as possible. The doctor will interview the patient in detail, conduct a gynecological examination and prescribe the necessary laboratory and instrumental studies to the patient. After identifying the exact cause of the phenomenon, treatment of the underlying disease is prescribed, which led to the appearance of thickening of menstrual blood. It is impossible to figure out on your own why blood clots appear during menstruation. At the same time, a specialist can easily determine the cause of this symptom and effectively eliminate it. Self-medication for various menstrual irregularities can be very dangerous due to the development of serious complications and even infertility.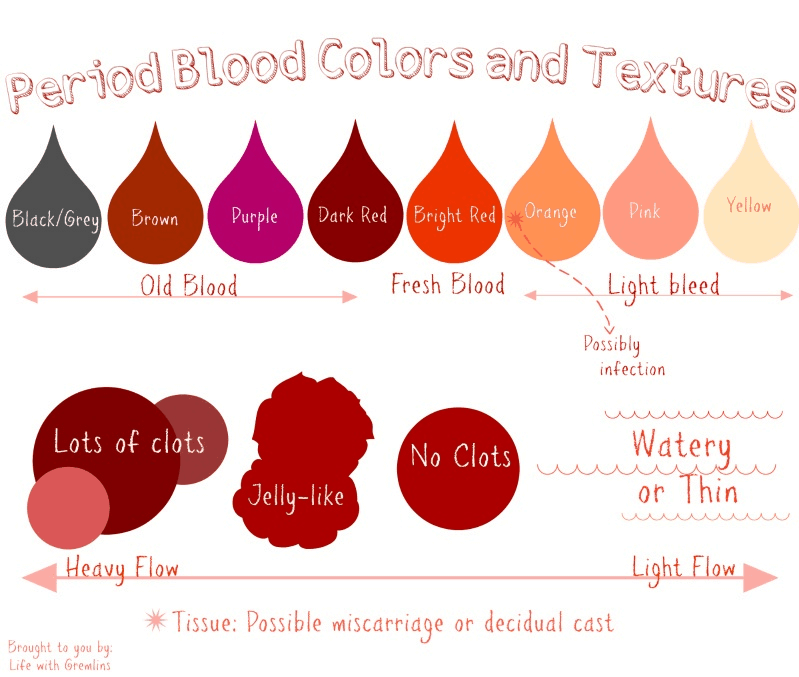
References:
- Smetnik V.P. All about menstruation.
Causes of heavy periods, what to do, very heavy bleeding during periods with blood clots
Contents
- Heavy periods: causes
- Heavy periods: what to do?
- Therapeutic tactics
Heavy periods (menorrhagia) is one of the types of abnormal uterine bleeding (AMB). AUB is understood as any violation of the menstrual cycle that does not meet the parameters of normal menstruation (too long, heavy or frequent uterine bleeding). The causes of heavy bleeding during menstruation can be gynecological and extragenital. The appearance of very heavy periods requires a full examination of the patient, identification of the cause and its subsequent elimination.
HEAVY PERIOD: CAUSES
In modern gynecology, all factors contributing to the appearance of menorrhagia are included in the PALM-COEIN classification. It combines a number of gynecological pathologies and diseases of other localizations. Abundant periods with clots according to PALM-COEIN may be due to the following reasons:
Abundant periods with clots according to PALM-COEIN may be due to the following reasons:
- P - uterine polyp.
- A - adenomyosis (endometriosis).
- L - uterine leiomyoma.
- M - malignancy and hyperplasia.
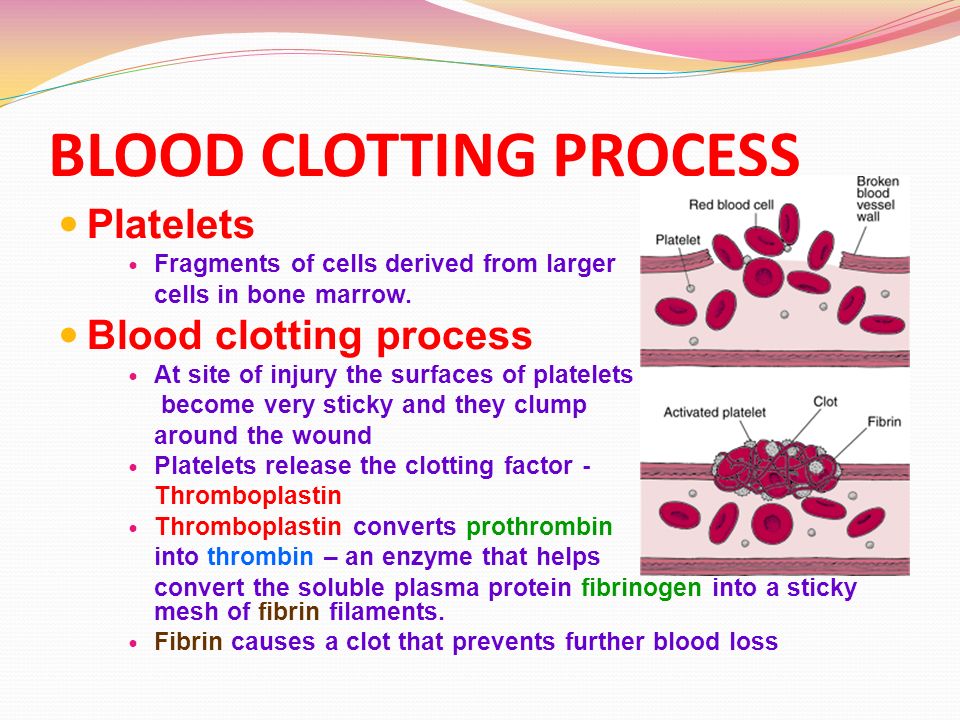
- C - coagulopathy.
- O - ovulatory disorders.
- E - endometrial changes.
- I - iatrogenic ovulatory dysfunction.
- N - still unknown cause due to incomplete diagnosis or impossibility to conduct a full-fledged study. 1
The first four diseases cause heavy periods with blood clots in women of older reproductive age and practically do not occur in adolescents and young girls. Coagulopathy, on the contrary, is most often observed in 20% of adolescents and 10% of women. Under coagulopathy understand disorders in the blood coagulation system, which are manifested by hemorrhagic syndrome (increased bleeding) of varying severity. Coagulation disorders are observed in hemophilia, von Willebrand disease and taking certain drugs (anticoagulants and antiplatelet agents).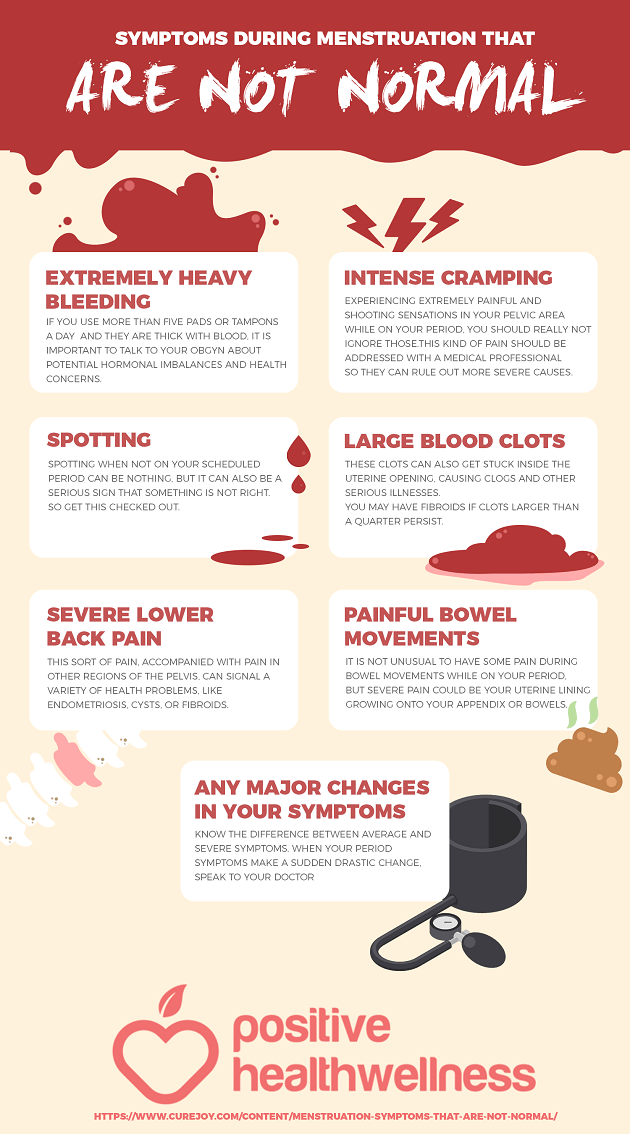 1 Causes of heavy periods with clots can also be associated with endocrinopathies and dysregulation of the menstrual cycle by the central nervous system. This group includes:
1 Causes of heavy periods with clots can also be associated with endocrinopathies and dysregulation of the menstrual cycle by the central nervous system. This group includes:
- Prolonged neuropsychic stress.
- Overweight or underweight, including rapid weight gain or weight loss.
- Uterine leiomyoma.
- Significant physical activity.
- Changes in thyroid function.
A common cause of heavy periods with large clots is endometriosis - an abnormal growth of endometrioid tissue (the inner layer of the uterine wall). This tissue is sensitive to the action of sex hormones and is rejected by the same mechanism as the endometrium of the uterus during menstruation. Clinically, endometriosis is manifested by profuse and prolonged bleeding, pelvic pain and inability to conceive a child.
HEAVY PERIOD: WHAT TO DO?
The only right decision is to seek qualified gynecological care. Only a doctor can determine the cause and type of abnormal uterine bleeding. The AUB diagnostic algorithm includes two stages. The first is the collection of complaints and anamnesis. According to statistics, about 50% of women with complaints of heavy menstrual bleeding do not actually have them, and 25% of patients without complaints suffer from AUB3. An indicator of menorrhagia is the release of blood in the form of clots, the use of ultra-absorbent pads, or the simultaneous use of several hygiene products (tampon , pad, menstrual cup). A clinical sign of heavy uterine bleeding is also the need to change the hygiene product more often than 1 time in 2 hours, the presence of traces of blood on the bed linen after sleep
The AUB diagnostic algorithm includes two stages. The first is the collection of complaints and anamnesis. According to statistics, about 50% of women with complaints of heavy menstrual bleeding do not actually have them, and 25% of patients without complaints suffer from AUB3. An indicator of menorrhagia is the release of blood in the form of clots, the use of ultra-absorbent pads, or the simultaneous use of several hygiene products (tampon , pad, menstrual cup). A clinical sign of heavy uterine bleeding is also the need to change the hygiene product more often than 1 time in 2 hours, the presence of traces of blood on the bed linen after sleep
At the second stage, differential diagnosis is carried out among all possible causes and the leading one is identified. For this, the following are used:
- General, bacteriological and oncocytological smears.
- Determination of hormonal status.
- Screening for sexually transmitted infections.
- Colposcopy and hysteroscopy.

- Complete blood count.
- Ultrasound examination of the pelvic organs.
- Consultation with a hematologist and examination ordered by a specialist.
The scope of the diagnostic program is determined individually. In some cases, a standard gynecological examination of the patient (smears, blood tests and ultrasound) is sufficient, while in others, advanced diagnostics are required. 3
THERAPEUTIC TACTICS
AUB therapy is carried out in several stages. The main task is to get rid of heavy menstrual bleeding and prevent their recurrence. For this purpose, the following are used:
Medical methods of hemostasis - antifibrinolytic agents, non-steroidal anti-inflammatory drugs and combined oral contraceptives. Conservative treatment is used in adolescents and women of young reproductive age without pathological changes in the endometrium.
Surgical hemostasis - separate diagnostic curettage of the mucous membrane of the cervical canal and uterine cavity, followed by histological examination.