Miscarriage at four months
Understanding Second Trimester Loss | Obstetrics and Gynecology
Pregnancy loss in the second trimester can be the result of a very preterm delivery (like a spontaneous miscarriage in the second trimester) or death of the fetus (called a fetal demise). About 2-3% of pregnancies will be lost in the second trimester, a rate that is much lower than in the first trimester. Once a pregnancy gets to about 20 weeks gestation, less than 0.5% will end in a fetal demise.
A loss at this time in pregnancy is most often a hard and sad experience. Many friends and family already know you are pregnant. What do you do? What do you say? For most women and their partners, the process of grieving is no different than losing a person who has been in your life for some time. You often have hopes and dreams about your child before that child is born, and losing the pregnancy in the second or third trimester is certainly a loss for a family.
Why see a UC Davis Health specialist?
Our specialists can evaluate you quickly in an office setting. Any laboratory testing or ultrasound examinations that need to be done can be performed easily and conveniently. We perform our own ultrasound examination in the office and can share the results with you immediately. Treatment of a second trimester loss is very different than early miscarriage, and our specialists can provide all options to you and your family. We understand that losses at this time require both emotional and medical support. We are happy to review all treatment options but also know that you may need some time. It is also important for you to know that a fetal demise in the second trimester is not a medical emergency so treatment is not immediately indicated.
If you are having very heavy vaginal bleeding or are feeling very sick, you should go to the Emergency Room to see our physicians.
Symptoms of a second trimester loss
- Bleeding: Most commonly, bleeding is a sign of a problem with the placenta and does not indicate a fetal demise. But, bleeding can be a sign that the cervix is opening without labor (called cervical insufficiency).
 With cervical insufficiency, the cervix begins to open early without contractions; as the cervix opens more, contractions then follow.
With cervical insufficiency, the cervix begins to open early without contractions; as the cervix opens more, contractions then follow. - Cramping: Pregnancy losses in the second trimester can be due to early labor.
- Loss of fetal movement: This can indicate a fetal demise. Most women can feel the baby moving by the 20th week. If the baby has been moving and you no longer feel that same movement, it is important to contact the doctor’s office immediately to make sure the baby is fine. Decreased fetal movement is more commonly a sign that there is a problem with the pregnancy and only rarely does it mean the fetus has died.
Most women less than 20 weeks of pregnancy do not notice any symptoms of a fetal demise.
The test used to check for a fetal demise in the second trimester is an ultrasound examination to see if the baby is moving and growing. Fetal demise is diagnosed when the ultrasound examination shows no fetal heart activity.
What causes a second trimester loss?
The causes of a pregnancy loss in the second trimester are very different than early pregnancy loss. There are medical conditions that increase the risk for cervical insufficiency or preterm labor before viability which include:
There are medical conditions that increase the risk for cervical insufficiency or preterm labor before viability which include:
- Prior surgery to the cervix
- Use of illicit drugs, especially cocaine
- Fetal abnormalities (genetic or structural problems)
- Uterine infection (this is more common in developing countries and less common in the United States)
- Physical problems with the uterus, including fibroids or abnormalities in the shape of the uterus
There are also some medical conditions that are associated with fetal death in the second trimester which include:
- Fetal abnormalities (genetic or structural problems)
- Poorly controlled maternal cnoditions like thyroid disease, diabetes or hypertension
- Lupus (systemic lupus erythematosus)
- Autoimmune or genetic conditions that increase a woman’s risk of forming blood clots in her legs or her lungs (like antiphospholipid syndrome)
- Very early pre-eclampsia or eclampsia of pregnancy
- Trauma
The specialists at UC Davis Health will review with you what testing is indicated to help learn more about why a second trimester loss occurred. Despite the testing that is available, about half of the time there is no identifiable reason for a second trimester loss. We can work with you to figure out what may be helpful with a next pregnancy or to learn more about medical issues that are important for your future.
Despite the testing that is available, about half of the time there is no identifiable reason for a second trimester loss. We can work with you to figure out what may be helpful with a next pregnancy or to learn more about medical issues that are important for your future.
Treatment of a second trimester loss
It is typically not safe for a woman to wait for the pregnancy to deliver on its own with a second trimester loss. There is a high chance of having significant bleeding when a pregnancy in the second trimester delivers on its own at home. In the case of fetal demise, a dead fetus that has been in the uterus for 4 weeks can cause changes in the body’s clotting system. These changes can put a woman at a much higher chance of significant bleeding if she waits for a long time after the fetal demise to deliver the pregnancy.
Our doctors are committed to providing all available treatment options. Testing to figure out the cause of the pregnancy loss can be performed regardless of the method a woman chooses for termination.
We understand that a second trimester loss is an emotional and stressful time and we want to ensure that the emotional needs of you and your family are met as well. We understand this is a time that you need support and we are sensitive to your wishes for remembrances and religious preferences. We will discuss these issues with you before any treatment.
When a diagnosis of fetal demise in the second or third trimester is made, options include:
- Surgical evacuation: This procedure, called a dilation and evacuation, can be performed in the second trimester, typically up to about 24 weeks. Surgical evacuation is the most common treatment women choose and involves removing the pregnancy through the cervix in the operating room while you are asleep. The cervix needs to be opened about 1-2 inches in diameter. The doctors can use different ways to open the cervix based on how far along the pregnancy is and your individual circumstance. The goal is to provide the safest care for each patient.
 After a surgical evacuation, normal activity can typically be resumed the following day. Opening or preparing the cervix for surgical evacuation of the pregnancy may involve:
After a surgical evacuation, normal activity can typically be resumed the following day. Opening or preparing the cervix for surgical evacuation of the pregnancy may involve: - Medicines (tablets) that are put in the vagina a few hours to one day before the procedure.
- Medicine (tablets) that you hold between your cheek and gums for 30 minutes before swallowing. You would use this medicine a few hours before the procedure.
- Placing thin sticks in your cervix, called osmotic dilators, to absorb water from the cervix which causes the dilator sticks to swell slowly over 4-24 hours. Having the osmotic dilators placed is similar to getting a Pap test.
Labor induction: This treatment uses medicines to cause the uterus to go into labor. For women with pregnancies beyond 24 weeks, this is commonly the only option. If you choose this option, you will be in the Labor and Delivery Unit at UC Davis Medical Center and will have all of the same pain treatments available to you as a woman who is naturally in labor (like IV pain medications or an epidural). The treatment typically starts with swallowing a pill to make the uterus more sensitive to the medications to induce labor. About 24 hours later, you are admitted to the Labor and Delivery Unit and will have medicine (tablets) put in the vagina every few hours to cause labor. Sometimes, women need medicine through an IV to also help get labor started. It may take 1-2 days for the uterus to go into labor and for the delivery to be complete. Up to 5% of women in the second trimester do not go into labor and need a surgical evacuation.
The treatment typically starts with swallowing a pill to make the uterus more sensitive to the medications to induce labor. About 24 hours later, you are admitted to the Labor and Delivery Unit and will have medicine (tablets) put in the vagina every few hours to cause labor. Sometimes, women need medicine through an IV to also help get labor started. It may take 1-2 days for the uterus to go into labor and for the delivery to be complete. Up to 5% of women in the second trimester do not go into labor and need a surgical evacuation.
Your doctor will be able to explain more details about the pros and cons of each treatment.
After treatment of a second trimester loss
Bleeding may continue for several weeks after a labor induction but tends to be much lighter with a surgical evacuation. Any bleeding may change in color from bright red to pink or brown. Lower abdominal cramping in the few days after treatment is also common. You should contact a doctor right away if the bleeding gets heavier instead of lighter over time, if a fever develops, or if vaginal discharge or a strange or unpleasant vaginal odor occurs. Avoid intercourse, douching, or using tampons for one week. Regular activities can be resumed right away, based on how you feel. Importantly, if you want to delay getting pregnant, it will be very important to start an effective method of contraception.
Avoid intercourse, douching, or using tampons for one week. Regular activities can be resumed right away, based on how you feel. Importantly, if you want to delay getting pregnant, it will be very important to start an effective method of contraception.
FAQs about second trimester loss
Q: What is cervical insufficiency?
A: This diagnosis is made when a woman has dilation of the cervix during the second trimester without having any contractions or signs of a uterine infection. Some studies suggest that some types of surgeries performed when women have advanced pre-cancerous changes in the cervix can increase the risk of cervical insufficiency. These surgeries include cervical conization (also known as a “cone biopsy”) or if a patient has had multiple LEEP procedures. With these surgeries, part of the cervix is removed to get rid of the pre-cancerous changes. Having these procedures increases the risk of having a second trimester loss by about 1%.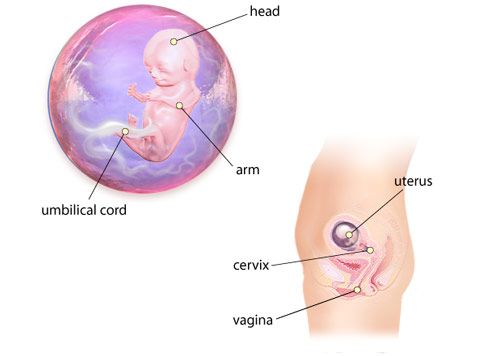 In women who have these types of procedures, the chance of having cervical insufficiency is about 1.5%.
In women who have these types of procedures, the chance of having cervical insufficiency is about 1.5%.
Q: What treatments are available if one of the tests shows I have a medical problem that increased the chance of a second trimester loss?
A: Our specialists will work with you to maximize your health status before you try to get pregnant again. For some women, this may mean treatment of a thyroid condition, improved control of diabetes, or changing medications being used for chronic illnesses. Some conditions may require blood thinners like aspirin or injectable medications that should be started early in the next pregnancy (after a normal pregnancy is seen with an early ultrasound exam).
Q: In my last pregnancy, I didn’t get any genetic testing and had a second trimester demise related to a genetic abnormality. What genetic testing is available for my next pregnancy to help figure out if the pregnancy is normal so I can learn earlier if the pregnancy is genetically normal?
A: It will be important to meet with a genetic counselor, if possible, before your next pregnancy, who can also review the details of the available tests. The counselor can also talk with you more about your history and your family history to make sure no genetic or familial medical problems are missed. There are a few different tests, all of which can be performed early in pregnancy, depending on what is right for you. Screening for some of the most common chromosomal abnormalities just from your blood (called NIPT or non-invasive prenatal testing). First trimester screening can be performed between 11 and 14 weeks which involves a blood test and an ultrasound examination. In some situations, chorionic villus sampling (a biopsy of the placenta) or expanded prenatal screening may be indicated. Our specialists and genetic counselors can work with you and your family to help you understand all of these tests and figure out what approach is right for you.
The counselor can also talk with you more about your history and your family history to make sure no genetic or familial medical problems are missed. There are a few different tests, all of which can be performed early in pregnancy, depending on what is right for you. Screening for some of the most common chromosomal abnormalities just from your blood (called NIPT or non-invasive prenatal testing). First trimester screening can be performed between 11 and 14 weeks which involves a blood test and an ultrasound examination. In some situations, chorionic villus sampling (a biopsy of the placenta) or expanded prenatal screening may be indicated. Our specialists and genetic counselors can work with you and your family to help you understand all of these tests and figure out what approach is right for you.
Q: After a second trimester loss, how long should I wait before I try to conceive again?
A: There is really no good information available to show the absolute right answer to that question. First, it may take a month or two to have any testing completed to help figure out why you had a second trimester loss. We know that it takes some time for your uterus and your body to get back to normal. The specialists at UC Davis usually recommend waiting at least 3 months after a second trimester loss before trying again to get pregnant.
First, it may take a month or two to have any testing completed to help figure out why you had a second trimester loss. We know that it takes some time for your uterus and your body to get back to normal. The specialists at UC Davis usually recommend waiting at least 3 months after a second trimester loss before trying again to get pregnant.
Managing a late miscarriage | Tommy's
A late miscarriage is one that happens during your second trimester, which is after the first 3 months of pregnancy, but before 24 weeks. If a baby dies at or after 24 weeks of pregnancy, this is called a stillbirth.
It can be very hard to understand why a very late loss is called a miscarriage rather than a stillbirth. This is because, from a legal point of view, a baby is thought to have a good chance of surviving if they are born alive at 24 weeks.
This distinction can be upsetting for some women who have a late miscarriage because they may also give birth to their baby and, understandably, feel that it should be called a stillbirth.
How will I know if I’m having a late miscarriage?
The most common signs of miscarriage are vaginal bleeding and strong, labour-like cramping pains. Sometimes, your waters may break and your baby may be born very quickly.
Some women have no signs at all that their baby has died and sadly only discover the loss when they attend a routine antenatal appointment for an ultrasound scan.
Other women may notice that their baby's movements have stopped, slowed down or changed. Contact your midwife or maternity unit immediately if you are worried about your baby’s movements.
Read more about the common symptoms of miscarriage.
Your treatment for a late miscarriage
If you have a late miscarriage, you will need to go through labour to give birth to your baby. This can be a very distressing time and you may be in shock. The staff caring for you at the hospital will understand this and will explain what your options are clearly so you can make a decision about your treatment. Ask as many questions as you need to so you feel as comfortable as possible.
Ask as many questions as you need to so you feel as comfortable as possible.
Your doctor may suggest that you can go home and wait to see if labour starts naturally. If you want to do that, try to have someone stay with you for support.
Your doctor may advise you to be induced, which means starting labour artificially. You may also choose to be induced as soon as possible if you don’t want to wait for labour to start naturally.
You will have to go into hospital to have an induction, where you should be given your own room or quiet area.
You may want to start having the labour induced as soon as possible. If so, you will be given medication to swallow, or pessaries to insert in your vagina, to induce labour. When this will happen may depend on when a private room is free.
You will be offered a medicine to help soften the cervix (the entrance to the womb), to allow the pregnancy to pass out of the womb. This medicine might be given as an oral tablet or a vaginal pessary.
You may also be given Oxytocin. This happens if your waters have broken and they need to encourage contractions if they haven’t started naturally. Oxytocin can also be used to make contractions regular and stronger.
It may take several hours for the medicine to be effective, and, depending on your stage of pregnancy, the labour can be very painful. You will be offered a range of pain relief to help with this. Sometimes the birth comes quickly. Sometimes it can take several more hours.
There will be a nurse or midwife with you, who can answer any questions about what is happening.
Seeing and holding your baby after a miscarriage
You can talk to the hospital staff about whether you want to see your baby and hold them after they are born.
The staff may also be able to do things like:
- help you create hand and footprints
- dress the baby in clothes you have chosen
- take a photograph and save it for in case you want to see it later.
There is no right or wrong thing to do. It depends on what the hospital staff may be able to do and how you and your partner feel. You should be able to take some time to think about it.
“When we were asked if I wanted to see our baby, Arthur, our feelings were all over the place. Did we want to see him? Would he look ok? We decided to see him and he was bought to us on the ward. The hospital took pictures of him, which are good, but I do wish I had taken my own. I think I felt a bit self-conscious about it. Was this a normal thing to do? Looking back, there is nothing more normal than taking a picture of your own child. We made the decision to make our own funeral arrangements as I wanted to keep Arthur’s ashes. We did have a little funeral for him. This was very small and private between me and my husband. My advice, and this is something I wish I had done, is even if you think you are handling everything OK, is go find a group or someone to talk to. Looking back, I really could have done with additional help to process my feelings.
Even though I thought I was fine, I was actually in a pretty bad place."
Jennifer
What will happen to my baby after a miscarriage?
Some hospitals offer burials or cremations for miscarried babies. Unfortunately, some hospitals are still not able to offer this service.
You may want to make your own arrangements for burial or cremation, whether you use a funeral director or specialist cremation service.
Find out more about what happens to your baby after a miscarriage.
There are lots of ways to commemorate your loss. Find out more about remembering your baby after miscarriage.
What will happen to my body during a miscarriage?
Your body will go through some changes as your pregnancy hormones begin to fall. Find out more about what happens to your body during a miscarriage.
Tests and treatments after a late miscarriage
Sometimes doctors can do tests to try to find out why you had a miscarriage and what this means for any future pregnancies.
You may also be offered a post-mortem examination of your baby to find out why they died. This will not happen without your permission (consent).
After this, your doctor will talk to you about your test results and what this might mean for your chances of having another miscarriage and successful pregnancy, if you want to get pregnant again.
Be aware that doctors may not be able to find out why you miscarried, which can be difficult and frustrating. But most couples are likely to have a successful pregnancy in the future, particularly if test results are normal.
Find out more about tests after miscarriage.
Your emotional health after a miscarriage
Losing a baby can be heart breaking and a late miscarriage may be particularly difficult for many parents. Your feelings and emotions are your own and no-one can tell you how you should or shouldn’t be feeling. There is no right or wrong way to feel about pregnancy loss.
It may take some time to recover, physically and emotionally. It’s important to take the time you need to grieve. In time, you may start thinking about the possibility of trying again, if that’s what you want to do.
It’s important to take the time you need to grieve. In time, you may start thinking about the possibility of trying again, if that’s what you want to do.
Having a miscarriage can impact your mental health. If you or someone you love feel that you need help, there is support available.
Telling other people about your miscarriage
If you’ve had a late miscarriage, you’ve probably already told friends and family about your pregnancy. Sharing the news that you’ve now lost the baby can be very upsetting and emotionally draining.
There's no one right way to tell people about your loss. You even may want to do it in different ways, depending on who you are speaking to. You may find the idea of telling everyone individually a bit daunting. If so, you could ask your partner, a family member or friend to tell people for you.
Make sure you take care of yourself as you go through this process. You don’t need to explain any details about what happened or tell people that everything is ok. You and your partner will be processing your own feelings and emotions about what has happened, so try not to worry too much about how other people take the news. Hopefully, you have friends and family who can support you and your partner during this difficult time and help you move through your grief.
You and your partner will be processing your own feelings and emotions about what has happened, so try not to worry too much about how other people take the news. Hopefully, you have friends and family who can support you and your partner during this difficult time and help you move through your grief.
Miscarriage, how to avoid - Planning and management of pregnancy in the gynecology of the Literary Fund polyclinic after a miscarriage
- Gallery
- News
- Blog
- Reviews
- Jobs
- Licenses
- Insurance partners
- Controlling organizations
- Schedule of reception of citizens on personal appeals
- What you need to know about coronavirus infection?
- Rules for patients
- Online doctor's consultation
- to corporative clients
- The documents
A miscarriage is always associated with severe consequences for the whole body of a woman and for her reproductive organs in particular, it also affects the family situation, disrupts the woman's work schedule. An unfavorable outcome of pregnancy requires great mental and physical costs on the part of parents. Therefore, contacting doctors to find out the causes of the problem is the very first and correct step towards the birth of a child.
An unfavorable outcome of pregnancy requires great mental and physical costs on the part of parents. Therefore, contacting doctors to find out the causes of the problem is the very first and correct step towards the birth of a child.
Any competent gynecologist will tell you that the problem of miscarriage can be solved. With proper preparation for pregnancy and its management, the next time you will have a successful pregnancy. Most girls after a miscarriage go to extremes: they try to get pregnant again as soon as possible. And if this succeeds, then the miscarriage is very often repeated. And you need to give the body a rest for 2-3 months, then identify and eliminate the cause. And only then try.
Causes of miscarriage
Many are convinced that miscarriages are due to a fall, bruise, or some other physical shock. Any woman who has had a miscarriage can remember that not long before she either fell or lifted something heavy. And I am sure that she lost her unborn child precisely because of this.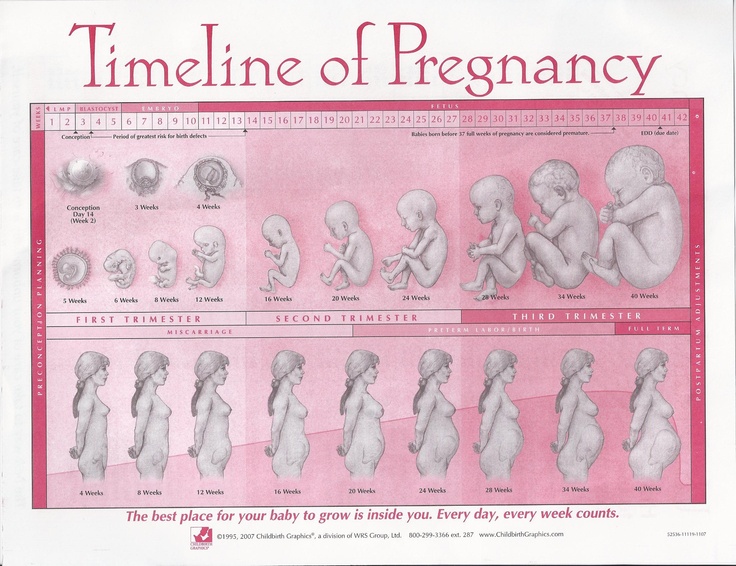 However, those women whose pregnancy was normal also fall and lift heavy things. Most sudden miscarriages do not occur for this reason. The reason is in violations of the pregnancy itself. Approximately half of miscarriages are due to abnormal genetic development of the fetus, which can be hereditary or accidental. Merciful nature, following the principles of natural selection in everything, destroys the defective and unviable fetus. But you should not be afraid of this. The fact that there is a defect in one embryo does not mean at all that all the others will be the same.
However, those women whose pregnancy was normal also fall and lift heavy things. Most sudden miscarriages do not occur for this reason. The reason is in violations of the pregnancy itself. Approximately half of miscarriages are due to abnormal genetic development of the fetus, which can be hereditary or accidental. Merciful nature, following the principles of natural selection in everything, destroys the defective and unviable fetus. But you should not be afraid of this. The fact that there is a defect in one embryo does not mean at all that all the others will be the same.
The woman's body is almost always to blame for the other half of miscarriages. They are caused by various known and unknown factors, such as: acute infectious diseases suffered in the first trimester of pregnancy, poor environment or difficult working conditions, excessive psychological or physical stress, abnormal development of the uterus, radiation, alcohol, smoking and certain types of drugs.
The causes of early and late miscarriage may differ, although they may overlap. The most important thing is to find out and eliminate or compensate for your own cause of miscarriage. Having discovered the cause, the gynecologist will tell you how to avoid another loss.
The most important thing is to find out and eliminate or compensate for your own cause of miscarriage. Having discovered the cause, the gynecologist will tell you how to avoid another loss.
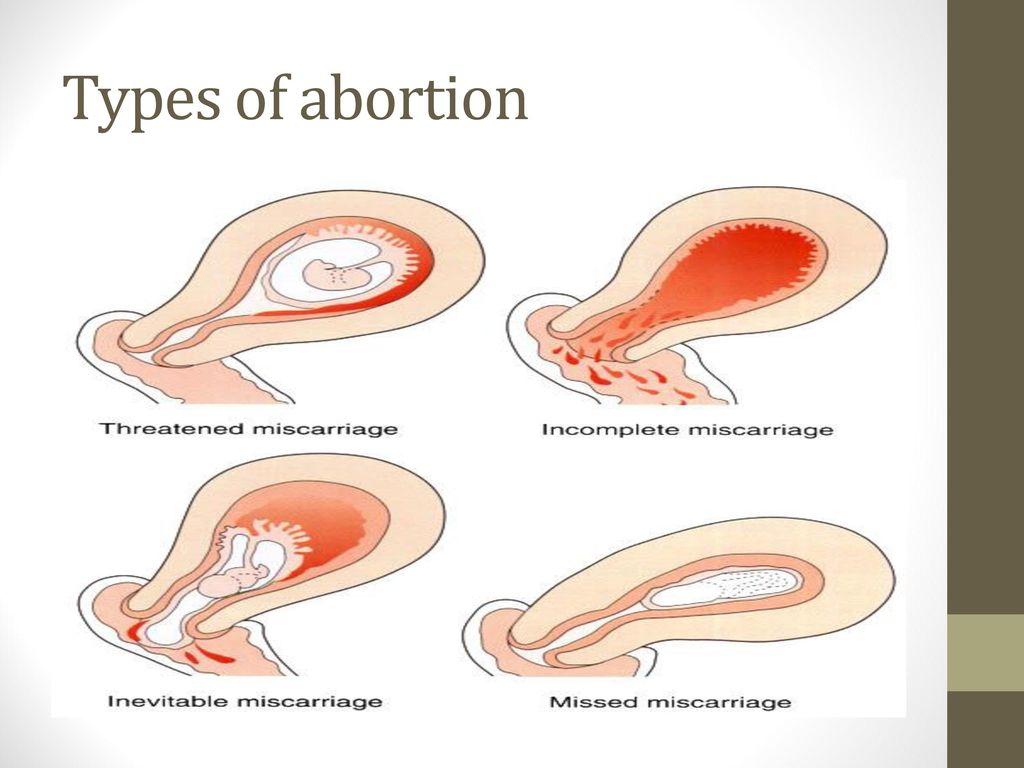
Miscarriage
Miscarriage statistics also include “missed pregnancy”. Sometimes it happens that the embryo dies and lingers in the uterine cavity. Most often, this fact is detected by ultrasound. The dead fetus may begin to decompose, and this, thereby, will lead to poisoning of the mother's body.
Doctors resort to surgical curettage, which is associated with a risk of inflammation and complications. With such a miscarriage, the next pregnancy is planned after the body is fully restored - not earlier than a year. During this year, you will have to find out the cause of the missed pregnancy and treat it.
Miscarriage up to 6 weeks
The main causes of miscarriage on this line are malformations of the embryo itself. Statistics say that from 70-90% of embryos had chromosomal abnormalities: they are random and will not occur in other pregnancies. You may have been ill, taken medication, or were under the influence of other harmful factors. Fate saved you from a child with malformations.
You may have been ill, taken medication, or were under the influence of other harmful factors. Fate saved you from a child with malformations.
The human body is perfect and finds a way to correct the situation by miscarriage. Today is a tragedy for you. The real tragedy would be the preservation and birth of a sick, non-viable child. So don’t cry and understand: everything is for the best, you won’t help grief with tears ... And after three months, try again - it will almost certainly turn out to be successful.
It should also be noted that the fact of a miscarriage does not mean that you have lost something. So for a period of 7-8 weeks, the absence of an embryo in the fetal egg is found - "anembryony". It is believed that in 80-90% of cases, miscarriages are undiagnosed non-developing pregnancies.
Miscarriage between 6 and 12 weeks
Miscarriage in this period is also considered early. Its most common causes are:
Endocrine disorders
Endocrine disorders, when the ovaries do not synthesize enough hormones to keep the fetus in the womb, or the amount of male sex hormones is increased, is one of the most common causes of miscarriage and miscarriage.
Imbalance of hormones in a woman's body is very likely to lead to an early termination of pregnancy. With a lack of the main hormone progesterone produced by the ovaries, this happens most often. Another hormonal problem is an increase in the tone of the uterus, which provokes the expulsion of the fetus.
Progesterone prepares the uterine mucosa for implantation and is the hormone for maintaining pregnancy in the first months. If conception occurs, the fetus cannot properly establish itself in the uterus. As a result, the fertilized egg is rejected. But pregnancy can be saved with the help of progesterone preparations if this problem is detected in time.
An excess of male sex hormones that suppress the production of estrogen and progesterone can also be the cause of an early miscarriage. Often, the cause of recurrent miscarriages are androgens that affect the formation and development of pregnancy; as well as thyroid and adrenal hormones. Therefore, a change in the function of these glands can lead to miscarriage.
Undertreated sexual infections
This problem must be solved before conception. Often the cause of miscarriage is sexually transmitted infections: syphilis, trichomoniasis, toxoplasmosis, chlamydia, cytomegalovirus and herpetic infections. Their effect on the fetus and the course of pregnancy is different for each woman and depends on the timing of infection, the activity of the microorganism, the degree of immune protection and the presence of other adverse factors. Depending on the situation, they can lead to the formation of fetal malformations, intrauterine infection, feto-placental insufficiency, early miscarriage or premature birth. Infection of the fetus and damage to the membrane of the fetus leads to miscarriage. To avoid this, infections should be treated before pregnancy. The use of therapy is possible during pregnancy as prescribed by a doctor.
Viral infections and other diseases
Any disease accompanied by intoxication and fever above 38 about C can lead to a miscarriage. Rubella, influenza and viral hepatitis occupy a leading position in this list. At a period of 4-10 weeks for pregnancy, ordinary tonsillitis can also become tragic, pneumonia carries a more serious risk. Pyelonephritis and appendicitis can cause early labor. When planning a pregnancy, it is imperative to undergo a medical examination in order to identify and treat foci of infections.
Rubella, influenza and viral hepatitis occupy a leading position in this list. At a period of 4-10 weeks for pregnancy, ordinary tonsillitis can also become tragic, pneumonia carries a more serious risk. Pyelonephritis and appendicitis can cause early labor. When planning a pregnancy, it is imperative to undergo a medical examination in order to identify and treat foci of infections.
Extremely dangerous during pregnancy rubella - it leads to severe fetal malformations, so infection during pregnancy is an indication for medical abortion.
Any disease during pregnancy can lead to non-viability of the fetus. And the body, through a miscarriage, insures you against unwanted offspring. With such a miscarriage, the next pregnancy has every chance of going well.
Immune causes of miscarriage
Sometimes antibodies that are hostile to the fetus are formed in the blood of a pregnant woman. This cause can be predicted and eliminated in advance. Most often, the conflict occurs when the embryo inherits the positive Rh factor of the father, and the negative Rh factor, the mother's body rejects the embryonic tissues that are alien to it. Constant monitoring of antibody titer and the introduction of anti-Rhesus immunoglobulins allows you to maintain and maintain pregnancy. In case of an immune conflict, progesterone preparations are also used to prevent miscarriage, which in this case has an immunomodulatory effect.
Most often, the conflict occurs when the embryo inherits the positive Rh factor of the father, and the negative Rh factor, the mother's body rejects the embryonic tissues that are alien to it. Constant monitoring of antibody titer and the introduction of anti-Rhesus immunoglobulins allows you to maintain and maintain pregnancy. In case of an immune conflict, progesterone preparations are also used to prevent miscarriage, which in this case has an immunomodulatory effect.
Reduced immunity
Reduced immunity during pregnancy also refers to immune causes. The body is simply not able to grow a new life in itself. You need to take care of yourself and recover before the next conception.
Anatomical causes of miscarriage
Anatomical causes of miscarriage are the most intractable. Malformations of the uterus are a serious reason for miscarriage. Sometimes you just have to deal with it.
Miscarriage between 12 and 22 weeks
Such a miscarriage is considered late.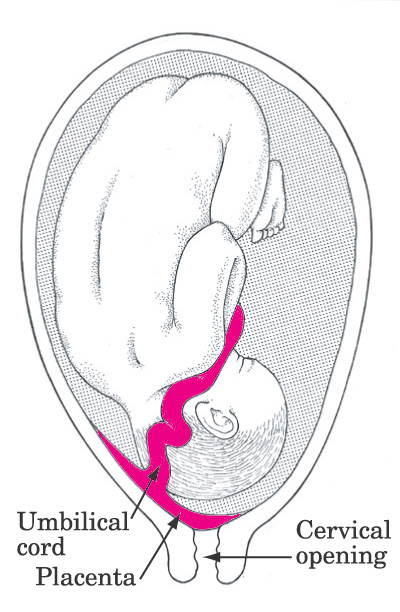 Its causes coincide with the causes of miscarriages in the early stages (anatomical, immune, infectious, endocrine).
Its causes coincide with the causes of miscarriages in the early stages (anatomical, immune, infectious, endocrine).
At this time, miscarriage also occurs due to isthmic-cervical insufficiency - a weak cervix cannot hold the fetus and opens. For this reason, a miscarriage can occur in the 2nd or 3rd trimester. Isthmic-cervical insufficiency is observed in 15.0-42.7% of women suffering from miscarriage. Careful monitoring of the pregnant woman allows you to identify the problem in time and make surgical correction of the cervix before the onset of childbirth.
In isthmic-cervical insufficiency, there is only one method of treatment - mechanical narrowing of the cervical canal. To do this, the neck is either sewn up or a special ring is put on it. However, the latter method is less efficient, because the ring can easily slide off the neck, then it will no longer hold back the process of opening it.
After suturing, if necessary, it is possible to use antibiotics and drugs that normalize the microflora of the vagina. The treatment of the vagina and the control of the state of the seams are carried out daily for 5 days. Stitches are removed at 37-38 weeks and with premature onset of labor.
The treatment of the vagina and the control of the state of the seams are carried out daily for 5 days. Stitches are removed at 37-38 weeks and with premature onset of labor.
Isthmic-cervical insufficiency may be primary (for no apparent reason), may be the result of abortion or hormonal disorders (increased levels of androgens - male sex hormones or their precursors).
Miscarriage after 22 weeks
Such a loss is hard to forget. Obstetricians talk about premature birth after the 28th week of pregnancy. Traditionally, a child born after this period is considered viable. But medicine knows many cases when it was possible to save the life of earlier children.
We recommend that you be carefully examined for miscarriage, check the above factors. In addition to them, the cause of a miscarriage can be antiphospholipid syndrome, while the woman's body perceives the child as something alien and rejects it. This disease, like the others listed, can be corrected; you have a very real chance of bearing a child.
Miscarriages due to hemostasis disorders
All of the above causes account for only 30-40%. Up to 70% of miscarriages are caused by disorders in the blood coagulation system (hemostasis).
Blood coagulation disorders leading to pregnancy loss can be divided into thrombophilic (increased clotting) and hemorrhagic (bleeding tendencies). Both of these extremes are dangerous to the fetus. Various disorders leading to the formation of small blood clots lead to the fact that the fetus loses sufficient blood supply, development is disturbed and the fetus is rejected.
The main hemorrhagic changes can appear even in childhood in the form of increased bleeding during cuts, tooth extractions, the onset of menstruation. But sometimes they declare themselves only during pregnancy and are the cause of a miscarriage. Bleeding in the early stages and detachment of the chorion is difficult to stop.
You may not guess, but incomprehensible headaches, weakness, fatigue, temporary loss of smell or hearing may be symptoms of disorders in the blood coagulation system.
When planning a pregnancy, a genetic examination should be carried out and, if necessary, treatment should be started.
It is advisable to be examined for hidden hemostasis defects even for those who consider themselves healthy. This will allow you to predict the occurrence of complications and prevent loss. Early therapy can prevent miscarriage at 98% of cases. If defects in hemostasis are already detected during pregnancy, it can be difficult to maintain it.
What to do after a miscarriage?
Find the cause! The ideal option is to be examined by future parents: it is much more reasonable to postpone conception and spend two or three months to identify the causes than to risk getting pregnant again, spend two months waiting, and then lose everything again and still go to the doctors.
Until you understand the reason, it will not evaporate. In most cases, the answers lie on the surface. Take care of your health and your future baby.
Sign up for a consultation with an obstetrician-gynecologist by phone +7 (495) 150-60-01
Tyan Oksana Alexandrovna
Head of the department, obstetrician-gynecologist Doctor of the highest category Work experience: 26 years
Volkova Polina Dmitrievna
Obstetrician-gynecologist, doctor of ultrasound diagnostics Doctor of the highest category Experience: 35 years
Postnikova Nadezhda Anatolyevna
Obstetrician-gynecologist, ultrasound specialist Work experience: 35 years
Moiseeva Alla Vitalievna
Obstetrician-gynecologist, doctor of ultrasound diagnostics Doctor of the first category Work experience: 37 years
Zabolotnova Olga Valentinovna
Obstetrician-gynecologist Doctor of the first category Experience: 25 years
Shchelokova Elena Nikolaevna
Obstetrician-gynecologist Doctor of the highest category Work experience: 38 years
Pass or medical card number:
Contact phone: *
Select the day of your appointment:
Additional information:
I am not a robot
By clicking the "Submit Application" button, you agree to the terms Privacy Policy and User Agreement
Spontaneous miscarriage and miscarriage
Over the past 10 years, the number of spontaneous miscarriages has been growing rapidly. The International Histological Classification Organization (FIGO) has declared an epidemic of the situation with an increase in the frequency of miscarriages.
The International Histological Classification Organization (FIGO) has declared an epidemic of the situation with an increase in the frequency of miscarriages.
Spontaneous miscarriage is the termination of pregnancy before the fetus reaches a viable term (up to 22 weeks of pregnancy and fetal weight 500g.).
Most miscarriages (about 80%) occur before 12 weeks of gestation. Moreover, in the early stages up to 8 weeks of pregnancy, the cause of miscarriage is chromosomal abnormalities in 50% of cases. It turns out that nature eliminates the defective product of conception. And these causes are difficult to prevent, especially in the presence of hereditary diseases. Fortunately, accidental breakdowns are much more common than genetically determined ones. Therefore, subsequent pregnancies usually end happily. But the remaining 50% of miscarriages have completely real and removable causes. They can be easily identified at the stage of preparation for pregnancy by a gynecologist.
What are the reasons?
- chronic diseases: inflammatory diseases of the uterus and appendages, polycystic ovary syndrome, uterine fibroids, endometriosis, malformations of the genital organs.
- infections: toxoplasmosis, listeriosis, genital tuberculosis, sexual infections - chlamydia, mycoplasma, ureaplasma, syphilis.
- antiphospholipid syndrome.
- endocrine diseases: diabetes, thyroid disease.
- metabolic disorders in the body: obesity, folic acid deficiency, iron deficiency, vitamin D deficiency.
- male factor.
Of course, these causes are identified and eliminated before the planned conception.
There are harmful factors that can affect the development of the fetus in the early stages of pregnancy and lead to miscarriage:
- alcohol consumption.
- use of caffeine (4-5 cups of coffee per day).
- smoking (more than 10 cigarettes per day).
- drug use.
- taking medications with a teratogenic effect (for example: aspirin, nise and others from this group of drugs; antifungals; antidepressants; some antibiotics and a number of other drugs).
- toxins and occupational hazards: ionizing radiation, pesticides, inhalation of anesthetic gases.
What are the signs of possible pregnancy loss?
These are complaints of pain in the lower abdomen and lower back, bloody discharge from the genital tract. It is necessary to consult a doctor to rule out an ectopic pregnancy and conduct an additional examination (hCG test, blood test for progesterone, ultrasound).
In early pregnancy, with dubious ultrasound data or suspected non-developing (missing) pregnancy, expectant management is chosen with a repetition of a gynecologist's examination, ultrasound, tests after 7-10 days. If a the diagnosis was made and the fact of uterine pregnancy was confirmed, with a threatened miscarriage, preservation therapy is carried out in an outpatient day hospital. A miscarriage that has begun requires hospitalization in the gynecological department. In the case of a non-developing pregnancy, an abortion is performed.
In accordance with the clinical treatment protocol approved by the Ministry of Health of the Russian Federation dated 07.06.2016. Preference is given to drug therapy aimed at terminating pregnancy with prostaglandin analogues (misoprostol) with or without prior use of an antiprogestin (mifepristone). In case of need for surgical treatment (with incomplete miscarriage with infected miscarriage), it is recommended to use aspiration curettage (with an electric vacuum source or a manual vacuum aspirator). What has a significant advantage over curettage of the uterine cavity because it is less traumatic and can be performed on an outpatient basis.
All women who have had a miscarriage need treatment to prevent complications and prevent recurrent miscarriages. Why is rehabilitation therapy necessary?
According to the decision of the XVIII World Congress of Obstetricians and Gynecologists , the diagnosis of chronic endometritis should be made to absolutely all women who have had an undeveloped pregnancy. Two out of three miscarriages according to Professor V.E. Radzinsky are caused by this disease. When examining the material from the uterine cavity, infectious pathogens were isolated: ureaplasmas, mycoplasmas, streptococci, staphylococci, Escherichia coli, viruses (herpes, HPV). Therefore, it is very important to carry out treatment immediately after the termination of pregnancy.
Two out of three miscarriages according to Professor V.E. Radzinsky are caused by this disease. When examining the material from the uterine cavity, infectious pathogens were isolated: ureaplasmas, mycoplasmas, streptococci, staphylococci, Escherichia coli, viruses (herpes, HPV). Therefore, it is very important to carry out treatment immediately after the termination of pregnancy.
If time is lost, it is necessary to carry out additional diagnostics: a pipel biopsy of the endometrium with a histological examination and a study for infections, including tuberculosis. Then, taking into account the results obtained, symptomatic anti-inflammatory therapy is carried out (immunomodulators, antibacterial drugs, physiotherapy, gynecological massage, mud therapy). In parallel, an examination is prescribed to identify other causes of miscarriage (male factor, chronic maternal diseases, genital infections, antiphospholipid syndrome).
In the medical center "Mifra-Med" at the level of modern requirements of medicine, all the possibilities of a complete adequate examination have been created: all types of tests, ultrasound, hysteroscopy, aspiration biopsy, consultations of narrow specialists (endocrinologist, therapist, neurologist, urologist).