Labor without dilation
What Is Prodromal Labor?
Written by Alexandra McCray
In this Article
- Prodromal Labor vs. True Labor
- How to Tell if You’re Really in Labor
When you’re pregnant and get contractions, it means the muscles of your uterus are tightening and releasing. The contractions help widen (dilate) your cervix to help your baby journey through the birth canal. All that usually signals that you’re about to go into labor.
But sometimes contractions don’t make your cervix change the way it would if your labor had started for real. Your doctor may describe this as uterine contractions without cervical change. Some people call this “prodromal labor” (prodromal means early signs). Others refer to it as “false labor.” But doctors avoid both terms because they consider them imprecise or misleading.
Prodromal Labor vs. True Labor
Unlike actual labor, contractions without cervical change don’t get you and your baby ready for delivery. Doctors don’t know what causes them. They can happen at different times in your pregnancy. Your contractions may be regular and might remind you of menstrual cramps. They shouldn’t get worse over time and will go away. Lying down or drinking water may help you stay comfortable until the contractions pass.
Braxton-Hicks contractions are another type that don’t change your cervix. They may come on less regularly than prodromal labor. You may have Braxton-Hicks contractions in the evening or after you’ve moved a lot. You might get one or two contractions an hour. They are more distinct and often may feel like tightening in one part of your womb. But you might not feel anything. Shifting your body or walking can help end the contractions.
Real labor, by contrast, usually happens in three stages. It starts with regular contractions. They can come every 5-15 minutes and last 60-90 seconds in the beginning. In the first stage of labor, your cervix opens and thins to let your baby move into the birth canal. A pink or bloody discharge may appear as this happens. This could be the mucus plug at the end of your cervix releasing. If you see heavy bleeding or your water breaks, call your doctor right away.
The first stage can last for 12-19 hours or less. You should give your doctor updates and they will tell you what to do next.
Over time, your contractions grow stronger, last longer, and happen more often as you move into the second stage of labor. You might feel cramps in your legs and lower back pressure.
How to Tell if You’re Really in Labor
Cervical change is the key sign that you’re in labor. But it can be hard for you to tell. Keeping track of your contractions and what they feel like can help you distinguish when your baby is ready to be born or if it’s a false alarm.
Signs of contractions without cervical change include if they:
- Don’t have a pattern
- Get better when you rest, change positions, or drink water
- Don’t get stronger
- Start strong and then weaken
- Don’t become more frequent
You may be in true labor and should call your doctor or go to the hospital if:
- Your contractions last longer, become more painful, come every 5 minutes or less, and happen for more than an hour
- Your belly, pelvis, and lower back hurt but changing positions doesn’t help
- Your water breaks.
This could be a small or large amount of liquid.
- Pink, red, or brown discharge appears
- You have a lot of vaginal bleeding
- You have consistent, painful contractions before your 37th week. This could be preterm labor
If you still aren’t sure if you’re in labor, call your doctor. They may be able to give you pain medication and help you relax if you are worried.
Slow progress in labour – signs and management
beginning of content8-minute read
Listen
What is slow progress in labour?
Slow progress in labour is when any of the stages of your labour take longer than expected. It may also be called failure to progress or prolonged labour.
Slow progress in labour can be difficult to define. This is due to variations in labour for different people and the evidence available to support this. It’s important to note that when labour progress is checked, many factors are taken into consideration. This includes the wellbeing of both you and your baby. Your birthing preferences are also important.
Your healthcare team will assess labour progress through observations and physical examinations, including:
- cervical dilatation (opening of the cervix)
- cervical effacement (thinning out of the cervix)
- lowering of your baby’s head in your pelvis
- increasing strength and duration of your contractions
Slow progress in labour can be risky to both you and your baby.
What are the causes of slow progress in labour?
Slow progress in labour may be more likely if your:
- the baby is large
- the baby has a large head
- the baby is in a difficult position
- contractions aren’t strong enough and your cervix doesn’t open (dilate)
- pelvis is too small to fit your baby through
You may also have a greater chance of slow progress in labour if:
- you are overweight
- you have gained a lot of weight during your pregnancy
- this is your first baby
When does slow progress in labour happen?
Slow progress in labour can happen at any stage of your labour.
First stage of labour
The first stage of labour happens in 3 phases:
- the latent phase
- the active phase
- the transition phase
This stage of labour often stops and starts. It may take up to:
- 12 hours if it’s your first baby
- 10 hours if you’ve had a baby before
Sometimes your contractions won’t be strong enough to dilate your cervix fully. This happens when:
- your cervix doesn’t dilate by about 1cm every hour
- your labour stops altogether
If this happens, your doctor might talk with you about options to intervene and get your labour moving. You have the right to make your own choices about the interventions you want.
Second stage of labour
The second stage of labour is the time between full cervical dilatation (10cm) and the birth of your baby.
This stage could last:
- up to 3 hours if it’s your first child
- up to 2 hours if you’ve had a baby before
If the second stage of labour is taking longer than expected, your doctor will talk with you about your options. They may recommend intervening. It is your choice to have any interventions to help speed up the delivery of your baby.
Third stage of labour
The third stage of labour is the time between the birth of your baby and the delivery of the placenta. This usually lasts about 30-60 minutes depending on how this stage is managed (active or physiological). This stage of labour is carefully supervised.
Active management of labour is recommended to reduce the risk of postpartum haemorrhage (bleeding after the birth). Your midwife or doctor will give you an injection of a medicine called oxytocin after your baby is born. They will clamp and cut the umbilical cord and apply gentle traction to the cord to deliver the placenta.
This is optional and some people choose to deliver the placenta naturally without intervention. This is called physiological management.
How is slow progress in labour managed?
If you have slow progress during labour, your midwife and doctor will monitor you closely.
They will measure:
- how much your cervix is dilating
- how long your contractions last
- how often you are having contractions
They will continuously check the health of both you and your baby. If there are any concerns these will be discussed with you.
If you are in the first stage of labour, your midwife and doctor may recommend:
- breaking your waters
- giving you a medicine called oxytocin
This will speed up your contractions and make them stronger.
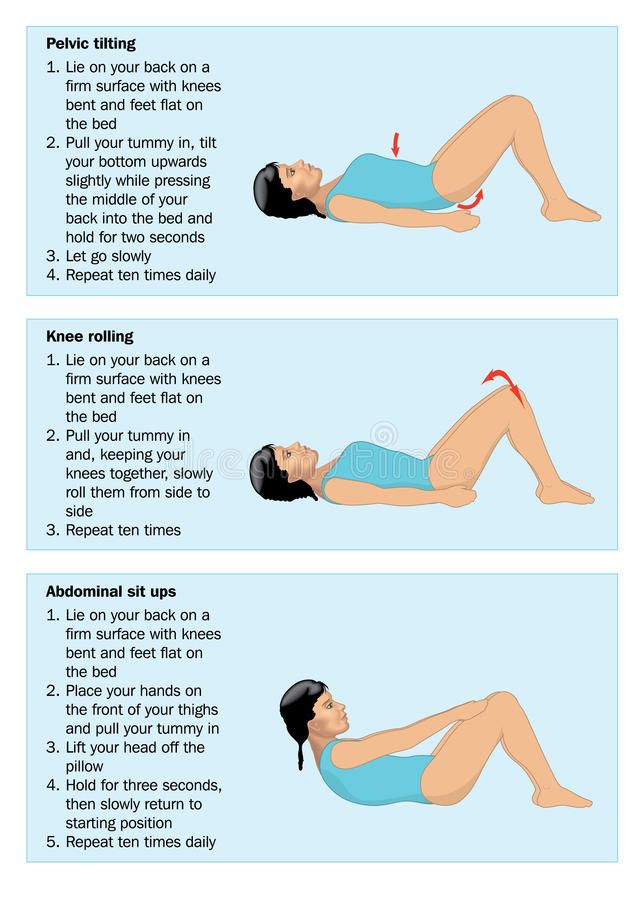
Other things you can try to help your labour progress include:
- changing position
- moving around and staying active
- relaxation techniques
- pain medicine
If your baby has already entered your birth canal, your doctor may suggest delivering your baby using: forceps or ventouse (vacuum cup).
In some cases, an emergency caesarean may be recommended if there is concern that you or your baby are unwell.
What are the risks of slow progress in labour?
Sometimes, slow progress in labour can result in health issues for you and your baby.
What are the risks to my baby?
The risk of slow progress in labour to your baby depends on many factors. Your healthcare team will explain any concerns they may have about your baby’s health.
They may have an increased risk of:
- low oxygen levels
- abnormal heart rhythm
- meconium (poo) in the amniotic fluid
- infection (when germs get in their body)
If meconium (poo) is in the amniotic fluid, this can be a sign that your baby is distressed. Meconium is your baby’s first poo and is very sticky and tar-like. Babies usually have their first poo after they are born. But some babies who are stressed during labour may pass meconium when they are still in the womb. If this happens your baby might breathe in amniotic fluid containing meconium. This can make it difficult for them to breathe after birth. When they are born they may require special care.
If either forceps or ventouse are used to help you have your baby, there is a risk your baby may have some swelling or marks on their head. These usually fade quite quickly.
What are the risks to me?
Slow labour can increase the risks of post-partum haemorrhage and uterine infection. Assisted delivery can injure the mother, but most injuries will be temporary and will heal over time. Sometimes the injury can be more long lasting and may need further treatment.
Your medical team may suggest an emergency caesarean if other interventions don’t work. As with any type of surgery, there are some risks. At this point a caesarean is usually the safest option for both you and your baby.
What happens after my baby’s birth?
If your labour didn’t go to plan, you might feel different emotions about your birth. You may feel stressed and experience anxiety about motherhood.
If you feel sad, disappointed or distressed by what happened, it’s important to talk to someone. You might want to consider contacting:
- Your doctor
- Perinatal Anxiety & Depression Australia (PANDA) on 1300 726 306
- Australasian Birth Trauma Association
- Beyond Blue on 1300 22 4636
Will I have slow progress in future births
Every pregnancy and birth are different. You won’t necessarily have slow progress in your next labour.
If you’re worried about any future pregnancies, you should talk to your doctor or midwife. They can explain what happened and discuss any further pregnancy risks.
Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call. Available 7am to midnight (AET), 7 days a week.
Sources:
Safe Care Victoria (Care during labour and birth), Queensland Government (Stages of labour), Royal Australian and New Zealand College of Obstetricians and Gynaecologists (RANZCOG) (Provision of routine intrapartum care in the absence of pregnancy complications), Queensland government (Guideline: Normal Birth)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: July 2022
Back To Top
Related pages
- Giving birth - stages of labour
- Induced labour
- Interventions during labour
- Labour complications
Need more information?
Labour complications
Even if you’re healthy and well prepared for childbirth, there’s always a chance of unexpected problems. Learn more about labour complications.
Read more on Pregnancy, Birth & Baby website
Interventions during labour
An ‘intervention’ is an action taken by a midwife or doctor that literally intervenes in the birthing process. Read about the different types of intervention.
Read more on Pregnancy, Birth & Baby website
Assisted delivery (forceps or ventouse)
An assisted delivery, sometimes called an 'instrumental delivery', is when your doctor will help in the birthing process.
Read more on Pregnancy, Birth & Baby website
Shoulder dystocia
Shoulder dystocia happens when a baby's shoulder gets stuck behind the mother’s pubic bone during birth. It is a medical emergency that requires immediate intervention. Find out why here.
Read more on Pregnancy, Birth & Baby website
Retained placenta
A retained placenta is when part or all of the placenta is not delivered after your baby is born. It can lead to serious infection or blood loss.
Read more on Pregnancy, Birth & Baby website
Complicated births | PANDA
Giving birth can lead to a range of complex feelings, especially when the experience is a difficult or traumatic one.
Read more on Perinatal Anxiety and Depression Australia (PANDA) website
Placenta accreta
Placenta accreta is a serious but rare pregnancy complication that causes heavy bleeding. If you have it, you will need special care at the birth.
Read more on Pregnancy, Birth & Baby website
Childbirth trauma and recovery | PANDA
While many pregnant women and their partners know birthing their baby will be hard work, very few expect labour and childbirth could be complicated.
Read more on Perinatal Anxiety and Depression Australia (PANDA) website
Pregnant with twins? About twin pregnancy | Raising Children Network
Pregnant with twins? Twin pregnancy can have more complications, so you’ll need more check-ups. Here’s what to expect in your pregnancy and antenatal care.
Read more on raisingchildren.net.au website
Causes - Miracle Babies
Every year in Australia around 48,000 newborn babies require the help of a NICU or SCN, there are many factors linked to premature birth and also many that remain unexplained
Read more on Miracle Babies Foundation website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OK Healthdirect Australia acknowledges the Traditional Owners of Country throughout Australia and their continuing connection to land, sea and community. We pay our respects to the Traditional Owners and to Elders both past and present.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Induction of labor or induction of labor
The purpose of this information material is to familiarize the patient with the induction of labor procedure and to provide information on how and why it is performed.
In most cases, labor begins between the 37th and 42nd weeks of pregnancy. Such births are called spontaneous. If medications or medical devices are used before the onset of spontaneous labor, then the terms "stimulated" or "induced" labor are used in this case.
Labor should be induced when further pregnancy is for some reason unsafe for the mother or baby and it is not possible to wait for spontaneous labor to begin.
The purpose of stimulation is to start labor by stimulating uterine contractions.
When inducing labor, the patient must be in the hospital so that both mother and baby can be closely monitored.
Labor induction methods
The choice of labor induction method depends on the maturity of the cervix of the patient, which is assessed using the Bishop scale (when viewed through the vagina, the position of the cervix, the degree of its dilatation, consistency, length, and the position of the presenting part of the fetus in the pelvic area are assessed). Also important is the medical history (medical history) of the patient, for example, a past caesarean section or operations on the uterus.
The following methods are used to induce (stimulate) labor:
- Oral misoprostol is a drug that is a synthetic analogue of prostaglandins found in the body. It prepares the body for childbirth, under its action the cervix becomes softer and begins to open.
- Balloon Catheter - A small tube is placed in the cervix and the balloon attached to the end is filled with fluid to apply mechanical pressure to the cervix. When using this method, the cervix becomes softer and begins to open. The balloon catheter is kept inside until it spontaneously exits or until the next gynecological examination.
- Amniotomy or opening of the fetal bladder - in this case, during a gynecological examination, when the cervix has already dilated sufficiently, the fetal bladder is artificially opened. When the amniotic fluid breaks, spontaneous uterine contractions will begin, or intravenous medication may be used to stimulate them.
- Intravenously injected synthetic oxytocin - acts similarly to the hormone of the same name produced in the body. The drug is given by intravenous infusion when the cervix has already dilated (to support uterine contractions). The dose of the drug can be increased as needed to achieve regular uterine contractions.
When is it necessary to induce labor?
Labor induction is recommended when the benefits outweigh the risks.
Induction of labor may be indicated in the following cases:
- The patient has a comorbid condition complicating pregnancy (eg, high blood pressure, diabetes mellitus, preeclampsia, or some other condition).
- The duration of pregnancy is already exceeding the norm - the probability of intrauterine death of the fetus increases after the 42nd week of pregnancy.
- Fetal problems, eg, problems with fetal development, abnormal amount of amniotic fluid, changes in fetal condition, various fetal disorders.
- If the amniotic fluid has broken and uterine contractions have not started within the next 24 hours, there is an increased risk of inflammation in both the mother and the fetus. This indication does not apply in case of preterm labor, when preparation of the baby's lungs with a special medicine is necessary before delivery.
- Intrauterine fetal death.
What are the risks associated with labor induction?
Labor induction is not usually associated with significant complications.
Occasionally, after receiving misoprostol, a patient may develop fever, chills, vomiting, diarrhea, and too frequent uterine contractions (tachysystole). In case of too frequent contractions to relax the uterus, the patient is injected intravenously relaxing muscles uterus medicine. It is not safe to use misoprostol if you have had a previous caesarean section as there is a risk of rupture of the uterine scar.
The use of a balloon catheter increases the risk of inflammation inside the uterus.
When using oxytocin, the patient may rarely experience a decrease in blood pressure, tachycardia (rapid heartbeat), hyponatremia (lack of sodium in the blood), which may result in headache, loss of appetite, nausea, vomiting, abdominal pain, depression strength and sleepiness.
Induction of labor, compared with spontaneous labor, increases the risk of prolonged labor, the need for instrumentation
(use of vacuum or forceps), postpartum hemorrhage, uterine rupture, the onset of too frequent uterine contractions and the associated deterioration of the fetus, prolapse umbilical cord, as well as premature detachment of the placenta.
If induction of labor is not successful
The time frame for induction of labor varies from patient to patient, on average labor begins within 24-72 hours. Sometimes more than one method is required.
The methods used do not always work equally quickly and in the same way on different patients. If the cervix does not dilate as a result of induction of labor, your doctor will tell you about your next options (which may include inducing labor later, using a different method, or delivering by caesarean section).
ITK833
This informational material was approved by the Women's Clinic on 01/01/2022.
Natural birth or caesarean section?
16/03/2018 - 13:35
Expectant mothers often face a dilemma: what will be better for her and the baby - natural childbirth or caesarean section. Both that and the other method of obstetrics have their pros and cons, their indications and contraindications.
Aleksey Sherstobitov, head of the obstetric department of the Chelyabinsk Regional Perinatal Center, obstetrician-gynecologist of the highest category, helped the Ural-press-inform agency to dispel the fears and unnecessary fears of women.
- Alexey Vasilyevich, in your opinion, as a professional, what choice should I make (natural birth or caesarean section), based on the benefits for mother and child?
- Until about the 1980s, the percentage of caesarean sections was about 2-4 percent of the total volume of deliveries. And we are all alive and well. And everything is fine with our grandmothers and mothers.
- What are the advantages of natural childbirth?
- In case of childbirth through natural birth canal, there is no pain syndrome in the postoperative period. The recovery process for the female body as a result of natural childbirth is much faster than after a cesarean section. There are fewer complications. Accordingly, the time of stay of a woman in labor in a hospital is reduced. The woman goes home on the third or fourth day. After caesarean section - only for 4-5 days. In addition, during natural childbirth, the baby is immediately brought to the mother's breast, which is good for the health of the newborn and for the mother's lactation.
- When is natural childbirth contraindicated?
- For certain medical conditions in a woman (eg, somatic, eye, cardiovascular disease), vaginal delivery is more of a risk than a benefit. For some women, a caesarean section is performed according to indications that occur during childbirth (acute fetal hypoxia and others). There are also relative indications - breech or foot presentation, large fetus.
- Is the woman's age an indication for caesarean section?
- Now women are increasingly giving birth at a late reproductive age. Previously, a woman aged 33 years and older was written late. And that was an indication for a caesarean section. Now there is no such term, and women at this age also give birth through the natural birth canal. We have several women who are 44-47 years old sometimes pass through us in a week.
- How old was your oldest woman in labor?
- 51 years old (her first daughter was already 31 years old). There was also a woman who had her first pregnancy at the age of 49.
- Can a woman in labor be an indication for a caesarean section?
- There are several countries in the world where the indication of a woman's desire to have a caesarean section is legislated. The Russian Federation is not included in this list of countries. Therefore, we do not perform cesarean at the request of a woman without medical indications. Indications for a caesarean section are clearly regulated by the order of the Ministry of Health of the Russian Federation. They are divided into a number of groups: planned and emergency indications during pregnancy, as well as emergency during childbirth. And there is no such indication as the desire of a woman.
- The number of births by caesarean section has increased dramatically. Why did this happen?
- Perinatal focus of medicine has expanded the range of indications for operative delivery. For example, earlier women with heart defects were strictly forbidden to give birth. At the moment, these defects are being corrected. For a woman, therapy is selected, and she becomes pregnant. Subject to certain rules, a favorable outcome is guaranteed. The method of delivery is chosen in each case individually, depending on the degree of compensation of the defect by the time of delivery.
- Have caesarean sections become more advanced today?
- Yes. The technique of performing caesarean section operations is being improved, more modern suture material is used, when sutured, the lower uterine segment is better restored, less scar tissue is formed.
- Previously, if a woman had a caesarean section during her first birth, then only a caesarean section during her second and subsequent births ...
- Absolutely right. But for the fourth year in our perinatal center, women with a scar on the uterus give birth through the natural birth canal.
- And now, after the first caesarean, a woman, having become pregnant for the second time, can choose - to give birth through the natural birth canal or she will have a caesarean section?
- Yes. If a woman with a scar on the uterus wants to give birth through the birth canal, she must sign up for a planned hospitalization with us. She will need to submit the protocol of the previous operation - a caesarean section. We will see how it was performed, we will find out from the woman if there were any complications in the postoperative period. Doctors working in the ultrasound department will assess the condition of the lower uterine segment, the obstetrician - the viability of the scar.
Then the woman in labor enters the department of pathology of pregnant women, where a consultation is held with the participation of the chief physician, the head of the department, and employees of the department of the Chelyabinsk State Medical Academy. And we determine whether a woman can give birth through the natural birth canal or not.
- Does a pregnant woman with a scar on the uterus need early hospitalization in a maternity hospital?
- Each time the issue is resolved individually. It depends on many factors: parity (what kind of child a woman should give birth to), how far she lives from the perinatal center.