Premature signs of pregnancy
16 early signs of pregnancy
You’ve got one question on your mind: Could I be pregnant?
A pregnancy test is the only way to know for sure. But if it’s too early to take a test, you may be on the lookout for early signs – or maybe you think you’re already experiencing some early pregnancy symptoms.
Is it too early to tell if you’re pregnant? What symptoms may be the earliest signs of pregnancy? Below, we answer those questions and more.
How early can you tell if you’re pregnant?
Again, you’ll need to take a pregnancy test at the right time to confirm your hopes or suspicions. But when it comes to the first symptoms of pregnancy, everyone is different. Some people start to notice changes within a week after conception. Others might not notice anything until they miss their period.
When should you take a pregnancy test?
It’s usually recommended that you take a pregnancy test after you’ve missed your period. This is because pregnancy tests measure the level of human chorionic gonadotrophin (hCG) in your body, which is a hormone that starts to build up when you conceive. It can take around three to four weeks from the first day of your last period for there to be enough hCG in your body to show up on a test.
What are the first symptoms of pregnancy?
The most common sign of early pregnancy? A missed period.
Your menstrual cycle is your body’s way of preparing for a possible pregnancy each month. Part of that is the thickening of your uterine lining, which is where a fertilized egg would implant to begin a pregnancy.
If you’re not pregnant, your period is how your uterus sheds that extra lining. If you are pregnant, that lining stays put and you don’t get your normal flow. This is why a missed period is often the earliest sign of pregnancy.
Of course, a delayed or missed period doesn’t always mean you’re pregnant. If your body is under a lot of stress or you have a hormonal imbalance, you could be experiencing an irregular menstrual cycle.
What other symptoms can be early signs of pregnancy?
Every person – and every pregnancy – is different. So, if you are pregnant, you’ll likely experience a unique combination of common, not-so-common and sometimes overlapping symptoms. And, they may show up earlier or later than expected. Here are more than a dozen possible symptoms of early pregnancy.
1. Spotting or light bleeding
Many women are surprised to learn that spotting or light bleeding can be an early sign of pregnancy, but about one-third of women experience it. This is often called implantation bleeding because doctors believe it occurs as the fertilized egg attaches (or implants) itself into the uterine lining. This is different from bleeding that could occur from something like a miscarriage – which is usually heavier.
When does implantation bleeding occur?
Implantation bleeding typically occurs 10 to 14 days after conception, which is just before or right around the time your period is due. So, you may think you’ve gotten your period.
But implantation bleeding is a light flow, which may start and stop over a couple days. And while it can take on a range of colors, it’s more likely to be pink, brown or light red.
Your period, on the other hand, may start off light in flow and in color but after a couple days becomes heavier, changes to a crimson red color and lasts up to a week or so.
2. Lower abdominal pain or cramping
While cramps and lower-abdominal pain can signal a coming period, they can also be a sign of egg implantation.
What do implantation cramps feel like?
Implantation cramps can occur with or without spotting or bleeding, and may feel different from period cramps. For example, you might feel mild to moderate prickling, pulling or tingling that comes and goes over a few days.
But menstrual cramps can often feel like a throbbing or dull ache, and typically start a day or two before your period.
3. Higher basal body temperature
If you’ve been tracking your basal body temperature (BBT) to increase your chances of getting pregnant, you probably know that your BBT goes up slightly right after ovulation. If you’re pregnant, your temperature may remain elevated rather than dipping back down.
Of course, you could be running hot for other reasons, but if it lasts more than a few weeks, pregnancy may be the explanation.
4. Changes in cervical mucus
If you’ve already been checking your cervical mucus to figure out when you’re most fertile, here’s a reason to continue: In the first few weeks of pregnancy, the amount of cervical discharge may increase and become stickier and whiter.
5. Breast tenderness, swelling or tingling
When you’re pregnant, your body experiences big changes in hormones – specifically, increases in estrogen and progesterone – to support your growing baby. This change in hormones can contribute to many symptoms, including breast tenderness.
Oftentimes, increased breast tenderness, swelling or tingling start to become noticeable a few days before a missed period.
If you usually experience breast tenderness leading up to your period or shortly after it begins, pregnancy-related breast tenderness and swelling will likely be more intense than you’re used to and stick around. You may also experience nipple soreness.
6. Fatigue
Fatigue in early pregnancy is common, and some women might notice it before they know they’re pregnant. In fact, fatigue may set in as soon as one week after conception. This is thanks to those sudden changes in hormone levels, particularly increasing progesterone.
7. Frequent urination
If you’re making more trips to the bathroom than usual around the time your next period is due, it may be a sign of pregnancy.
Certainly, your drinking habits play a big role in how many times you pee in a day. However, pregnancy increases the amount of blood in your body, which gives your kidneys more fluid to filter and more waste to get rid of.
So if you’re pregnant, you may notice you’re peeing a lot more – a symptom that can start early on and (unfortunately) last throughout your pregnancy.
8. Nausea or vomiting
Morning sickness might be the most well-known of all pregnancy symptoms, taking the form of food aversion or nausea, and even vomiting for some. This symptom can set in as early as two weeks after conception, which is around the fourth week of pregnancy and right around the time you’d miss your period if you were pregnant.
But some may not experience nausea or vomiting at all. And despite its name, morning sickness can actually happen at any time of the day or night.
9. Darkening areolas
When you’re pregnant, your areolas (the areas round your nipples) will likely grow and darken. Usually, these changes are gradual and continue throughout pregnancy. However, some women notice these changes really early on in combination with other symptoms.
10. Bloating or constipation
We all experience bloating or constipation from time to time, but both are quite common during pregnancy. Once again, those changing hormones are the culprit. They slow down digestion, which can cause a buildup of air in the gut and lead to constipation.
Early on, bloating or constipation may be mild and accompanied with other pregnancy symptoms. But – as a heads up – if you really are pregnant, these symptoms may stick around throughout your whole pregnancy.
11. Metallic taste in your mouth
Many women report a metallic taste in their mouth during pregnancy. Once again, hormones are to blame – specifically, estrogen.
Typically, this symptom (as well as changes in taste overall) is common in the first trimester but may occur at other times too – including before a missed period.
12. Sensitivity to smell
Many women report that sensitivity to smell was one of their first signs of pregnancy. In fact, as many as two-thirds of women become more sensitive or reactive to the smells around them during pregnancy.
And oftentimes, this heightened sense of smell can stick around through the first trimester or beyond, and contribute to other symptoms such as nausea, and food cravings or aversions.
13. Mood changes
From a stressful day at work to the natural wonders of your menstrual cycle, there are a lot of things that can affect your mood. But changes in mood are very common during pregnancy – and they may be especially noticeable early on as your body gets a sudden burst of estrogen and progesterone.
If you are pregnant, any mood changes you’re experiencing are likely coupled with other symptoms such as fatigue or nausea. You may feel more sensitive or weepy. Or perhaps your fuse is a little shorter and you’re more easily annoyed.
14. Headaches
Headaches are a part of life. They come with colds and allergies. They come with stress or fatigue, or when you cut down on caffeine to help prepare your body for pregnancy. But they can also come with pregnancy.
Headaches can happen thanks to the increasing blood volume and hormonal changes that occur in early pregnancy. You can also get headaches if you’re dehydrated as a result of nausea.
15. Dizziness
As blood flow increases during pregnancy, blood pressure can also decrease and lead to dizzy spells. Usually, dizziness is more of a second trimester symptom, but some women may notice it very early on, too.
16. Nasal congestion
A lot of people are shocked to learn that nasal congestion can be a pregnancy symptom. You may wonder if you’re coming down with something or your allergies are acting up. But if you’re noticing a stuffy or runny nose along with other pregnancy signs, you might be taking a pregnancy test in the near future.
The mucous membranes in the nose are also affected by hormones and increased blood flow throughout your body. This can cause blood vessels to swell, resulting in congestion and even sneezing.
Could you have early pregnancy symptoms and not be pregnant?
Yes. As we’ve mentioned, many early pregnancy symptoms can overlap with symptoms of other conditions, especially premenstrual symptoms. So, the best way to know if the symptoms you’re experiencing are pregnancy related is to try to relax and patiently wait until it’s time to take a pregnancy test.
When should you see a doctor about a new pregnancy?
If you’ve taken a pregnancy test and it’s positive, go ahead and make your first prenatal visit right away. This is also a great time to start looking into educational resources like the myHealthyPregnancy app.
At the first prenatal visit, you’ll get a physical exam and other tests to make sure everything is looking healthy, and you’ll learn about the rest of your prenatal appointment schedule. You’ll also get to talk through any expectations and questions you have, such as which foods to eat and avoid while pregnant.
Preparing for pregnancy checklist | HealthPartners Blog
Yay! Your trying-for-a-baby days are about to begin. You’re ready to get to work, but is your body ready for pregnancy?
Our bodies are capable of incredible things, but that doesn’t mean getting pregnant is easy for everyone. That’s why preparing your body for pregnancy is so important. Your physical, mental and emotional health are essential for increasing your chances of conception and a healthy pregnancy.
From figuring out when you’re most fertile during your cycle to what to eat while trying to get pregnant, we’ve put together a preparing-for-pregnancy checklist to help you get started on preconception planning.
Preparing for pregnancy Part 1: Take your first baby steps
Stop using birth control
One of the first things to do before getting pregnant is simple: you’ll need to stop any birth control methods you’re using. Just make sure you’re ready.
Barrier birth control methods, like condoms or a diaphragm, can be used until the day you start trying to conceive. If you’re using contraceptives like birth control pills or an intrauterine device (IUD), you may want to switch to a barrier method now if you’re planning to start trying in the next couple months. Why?
In order to get pregnant, you need to begin regular ovulation again. Ovulation occurs when an egg is released from your ovary – which is something birth control pills, rings, patches, implants and hormonal IUDs are meant to prevent. These types of hormonal birth control methods can also make your cervical mucus thicker, which helps prevent sperm from reaching an egg if it is released.
Getting pregnant immediately after stopping birth control is possible, but it could take several months.
Track your menstrual cycle
The first day of your period marks the beginning of a new menstrual cycle – the monthly process that makes pregnancy possible. And tracking your cycle helps you do two things: understand the patterns of body changes you experience throughout your cycle and narrow down your fertile window.
Your fertile window is when your chances of conceiving are highest. Your fertile window also includes your ovulation window, which is a roughly 24- to 72-hour time period when conception can occur.
When are most women usually fertile? The average cycle length is 28 days, but it can range from 21-35 days. Depending on your cycle, your fertile window can be six to 10 days in length and occurs mid-cycle.
So, the next time your period rolls around, start tracking. Record when your period starts and when it ends, what you notice about your flow, and any symptoms you have. These symptoms might include cramps, back aches or breast tenderness during your period and throughout the rest of your cycle.
If this seems a little daunting, don’t worry. You can use a fertility tracker app to help. There are dozens of mobile apps out there designed to make it easy to track your period and symptoms, visualize patterns and (eventually) time your baby-making sessions. Some apps include:
- Clue
- Flo
- Fertility Friend
- premom (which pairs with their ovulation testing kits)
Eventually, you may start tracking fertility data like basal temperature or ovulation test data too. Your basal temperature – your resting body temperature – can rise slightly when you’re ovulating. And at-home ovulation tests can help detect a surge in luteinizing hormone (LH) in your urine, which signals ovulation is near.
Both can help you figure out your most fertile days and time sex for the best chances of conception – and a fertility tracker can be extremely helpful in keeping track of all the data each month.
Schedule a preconception checkup
The best way to prepare your body for pregnancy is to make sure your body is healthy – and that’s where a preconception visit with an OB-GYN, certified nurse-midwife (CNW) or family medicine doctor comes in.
A preconception checkup is similar to an annual physical but includes additional care geared toward family planning and pregnancy. It may take a couple of weeks for you to get in for an appointment. That’s why we recommend that you make a preconception appointment early on.
Here are some of the things you can expect during your visit:
- A review of your medical and reproductive history, including:
- Whether you’re up to date on recommended immunizations like tetanus, hepatitis and whooping cough
- Current medications you’re taking (including vitamins and supplements)
- Health conditions you’re managing, like diabetes, anxiety, high blood pressure or other medical concerns
- Past pregnancies
- A discussion about your lifestyle and working environments
- Pre-pregnancy diet and prenatal vitamin recommendations
- A physical exam, which may include a Pap test and pelvic exam
- Lab tests (depending on a variety of factors like your age or current health conditions)
- A time to ask any preconception planning questions or concerns that are on your mind – now is the perfect time to ask your doctor, nurse practitioner or midwife
What’s the difference between a midwife and OB-GYN? Or how about a family doctor for pregnancy? All can provide you with incredible care now and if you get pregnant. Choosing the right person for you comes down to your health, pregnancy goals and preferences.
Ask your partner to schedule his own preconception exam, too
Your partner’s health is just as important as yours when you’re trying to have a baby. Health issues like obesity, depression or stress, and lifestyle factors such as smoking and drinking alcohol are just a sampling of the factors that can impact male fertility. So, get your own appointment on the books and ask him to do the same.
Planning for pregnancy Part 2: How to prepare your body for pregnancy
Start taking a prenatal multivitamin
Many women wonder when to start taking prenatal vitamins. Once you know you’re pregnant? Before? The first few weeks of pregnancy are important for fetal health and development. Certain vitamins – especially folic acid – help with development and help reduce birth defects.
When you do conceive, the earliest you may find out you’re pregnant is around Week 4. So if you’re planning for pregnancy starting prenatal vitamins before you’re pregnant (and continuing them throughout your pregnancy) is important.
There are plenty of prenatal multivitamin brands to choose from – just make sure you read the labels. Look for prenatal vitamins that have a minimum of 400 milligrams of folic acid and aim to take them for a full month before becoming pregnant.
Begin a pre-pregnancy diet
Maintaining a healthy, balanced diet is always important for your health and well-being. But when you’re trying to conceive, give your body the nutrients it needs to support a healthy pregnancy.
What does a pre-pregnancy diet look like? Eating a variety of foods is important. Your body needs adequate protein, carbohydrates and fats for energy, as well as folic acid, calcium and iron. These are the same nutrients you'll want to include in your diet once you are pregnant.
- Proteins – Protein helps support important body functions like tissue repair, hormone function and muscle building.
It also helps you regulate your blood sugar. Lean proteins like fish that are low in mercury, skinless turkey or chicken, low-fat dairy, and legumes (peas, beans and lentils) help support body function while also limiting your intake of saturated fats.
- Fats – Saturated fats raise blood lipids. Over time, this can increase your risk for heart disease. So, reduce your intake of saturated fats like butter, cheese, and fatty meats such as beef and some pork products. Instead, add more unsaturated fats like olive oil, avocados, peanuts and tree nuts to your diet.
- Carbohydrates – Carbohydrates give your body energy but complex carbohydrates are the best choice. Processed foods like cookies, chips and soda – and anything with refined sugar added – are simple carbohydrates that don’t provide much if any nutritional value. But complex carbohydrates like whole grains, fruits and vegetables are low in sugar or have natural sugars, and are excellent sources of essential vitamins and fiber:
- Asparagus
- Avocado
- Bananas
- Beets
- Broccoli
- Brussels sprouts
- Citrus fruits
- Eggs
- Fortified grains
- Legumes
In addition to eating a balanced diet of proteins, fats and carbs in pre-pregnancy, you should also:
- Increase your water intake – Aim for 8-10 cups of water per day.
- Reduce your caffeine intake – You should cap yourself at 200 mg of caffeine per day, which is roughly the equivalent of one large cup of coffee.
- Assess your weight – Being overweight (and underweight) can have an impact on your fertility, making it more difficult to conceive or sustain a healthy pregnancy. Being overweight while pregnant can also increase the risk of high blood pressure, gestational diabetes, oversized babies and more.
Make a quit plan
Over the years, numerous studies have shown that smoking while pregnant, as well as drinking and using other drugs, can be harmful to mothers and their babies. But you might not know that smoking, drinking and drug use while you’re trying to conceive may be detrimental too.
Smoking has been linked to a range of fertility issues, including increased risk of ectopic pregnancy, damage to eggs as they develop in your ovaries, changes to your uterine lining that may make correct embryo implantation less likely, and more.
When it comes to drinking while trying to conceive, one of the biggest concerns is the impact alcohol can have in the early weeks of pregnancy. Crucial organ development happens in the first few weeks – before you might know that you’re pregnant – and excessive drinking can lead to complications. Try to avoid or limit alcohol while trying to conceive, then avoid during pregnancy.
If you need help quitting, talk with your doctor, midwife or nurse practitioner during your preconception exam. They can connect you with helpful resources, and if you’re a HealthPartners insurance plan member, you have free access to a health coach. Just call 800-311-1052 to get started.
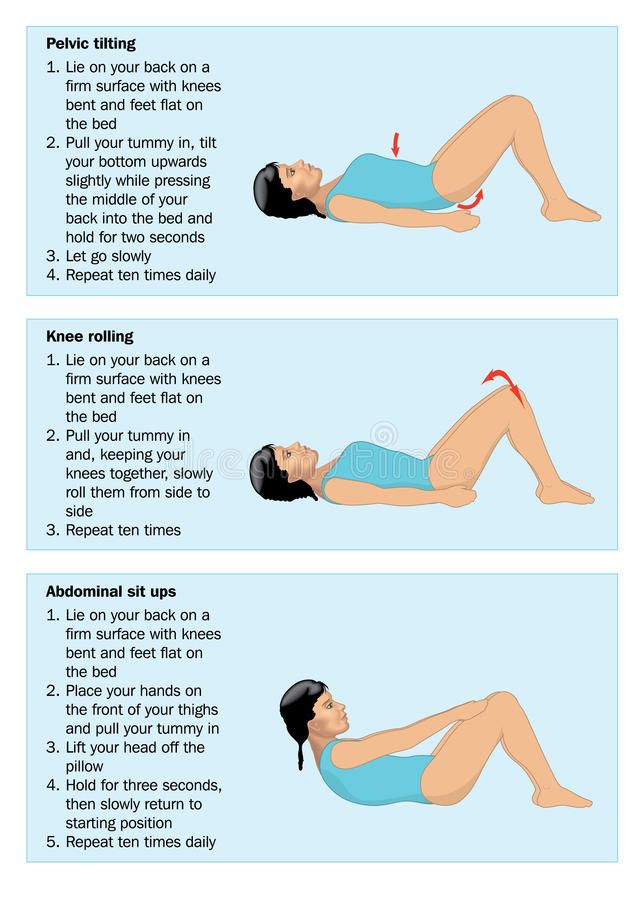
Start exercising before getting pregnant
Physical activity – along with a healthy diet – is important for maintaining a healthy weight and strengthening and conditioning your body. Pregnancy is a lot of work for your body. Staying active and exercising can improve your overall health, help prepare your body for pregnancy and set your baby up for a healthy start.
How often should you exercise when you’re trying to get pregnant?
Generally, 30 minutes of moderate exercise five times a week (or 150 minutes each week) is a good goal. If you’re not used to exercising regularly, start with 10- to 15-minute blocks and work your way up. If you’re already pretty active, try to increase your activity level to between 150 and 300 minutes each week.
What type of exercise should you do if you’re trying to get pregnant?
Walking is an easy, relatively low-impact way to get moving. Restorative exercises like stretching, yoga and foam rolling are great for relaxation and healing from more strenuous activities. Squats can also be a good strengthening exercise – especially since you may be getting low to pick up toys or your baby in the near future. What’s more, these are also safe exercises to do during pregnancy. So it’s worth getting familiar with at least a few of them.
Limit toxin exposure at home and at work
From cleaning products to cosmetics, you encounter toxins every day – many of which can be harmful to reproductive health. While you may not be able to eliminate exposure to certain toxins, there are steps you can take to minimize or avoid exposure. Some tips include:
- Avoid secondhand smoke whenever possible
- Ditch chemical-based household cleaners and make your own using vinegar and water
- Avoid heavy use of in-home air fresheners
- Don’t overuse aerosol sprays (e.g. hairspray, deodorant, etc.)
- Drink filtered water
- Don’t spray for bugs and rodents inside your home: Keep your home clean, use bait traps and (if necessary) hire only a licensed pest control expert
- Always rinse vegetables and fruits with warm water or scrub with a clean brush if needed. Produce labeled “pre-washed” or “ready to eat” does not need to be rinsed.
- Use BPA-free products (BPA is a chemical used in food containers and packing, and many hygiene products)
- Talk to your company about potential toxins you may be exposed to in the workplace
Look for ways to reduce stress and increase rest
Stress can impact your health in a lot of different ways. Stress can cause physical symptoms like increased heart rate, high blood pressure, headaches, fatigue, muscle soreness and upset stomach. Stress can affect your mood, making you feel anxious, overwhelmed, restless or irritable. Stress can also lead to behavior changes like overeating or undereating, social withdrawal or angry outbursts.
The bottom line? Stress can negatively impact your overall health and well-being – which can impact your fertility and your eventual pregnancy. So, look for ways to reduce stress and destress, as well as get more rest.
We know, we know. Easier said than done, right? But here are a few suggestions for how to reduce stress when trying to conceive:
- Busy schedule – If your schedule is hectic, look for ways to cut back on your commitments or delegate responsibilities. For example, if you host a monthly book club, ask another member to take over for a while. If you have a lot of errands to run, ask your partner to pitch in. If you need to hit the grocery store, consider using a delivery service.
- Work – If you’re stressed about work, talk to your supervisor about getting a little extra support or changing up your schedule.
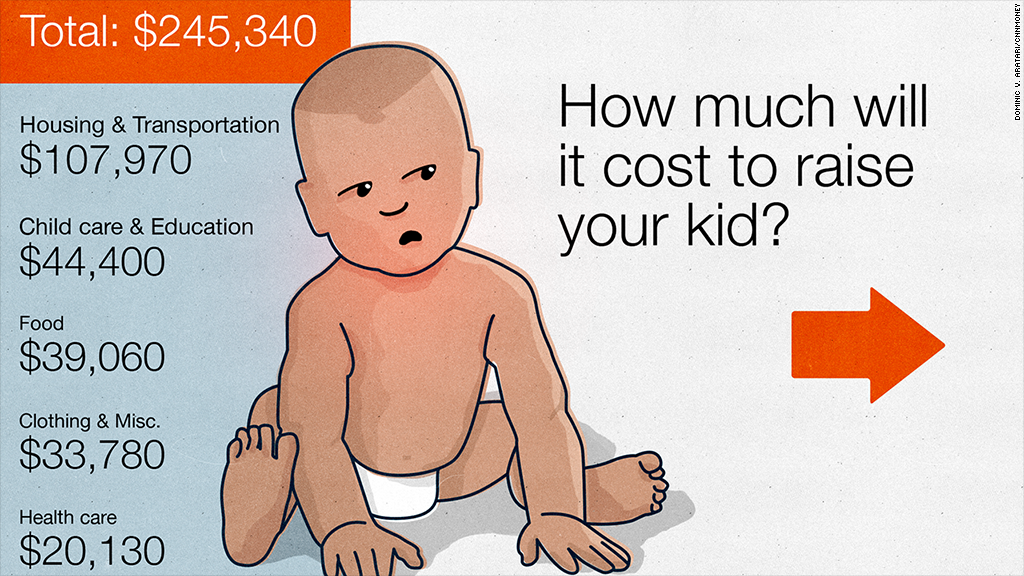
- Finances – If you’re stressed about finances, make a budget tracker with your partner. Also review your insurance coverage for prenatal care, postpartum care and pediatric care, and learn about your company’s maternity leave policy. This can help you prepare for what’s to come.
- Intimacy – If you’re stressed about the time you and your partner will spend trying to conceive, know that you’re not alone. When trying to conceive, many couples feel like sex can turn into a chore. So, try to carve out additional time for you and your partner to connect – inside and outside the bedroom.
If you think you need a little help to reduce stress, talk with your primary care doctor. They can work with you to manage your stress and connect you with a mental health specialist if needed.
Schedule your next trip to the dentist
Your oral health is an important part of your overall health. Plus, hormonal changes – not to mention more frequent snacking and morning sickness – during pregnancy can affect your teeth and gums. So, good daily brushing habits and keeping up on your regular trips to the dentist are important.
Pregnancy planning Part 3: Get busy
Use pregnancy-friendly lubricants
Lubricants help make sex more enjoyable and comfortable – especially when you’re trying to get pregnant. But the vast majority of lubricants aren’t designed for trying-to-conceive couples. These lubricants can be harmful to sperm, interfering with sperm motility, integrity and survival.
Fertility-friendly lubricants mimic the consistency of your cervical mucus and provide a protective environment for sperm as they make their way through your reproductive system. Ask your doctor, midwife or nurse practitioner for a safe recommendation.
Have sex
Sex is an important part of the baby making equation. So, if you’re ready to start trying for a baby, make regular lovemaking a priority.
Be spontaneous yet committed to regular sex. Don’t worry about timing at first, just focus on having unprotected sex frequently throughout your cycle, and use your fertility tracking journal or app to record the days you have sex.
Start preparing your mind and body for pregnancy today
This is such an exciting time in life for you and your partner – and a little planning can go a long way.
Get started by putting aside your birth control, tracking your cycle to get more familiar with your body and making a preconception appointment. Then focus on things like adding a daily prenatal vitamin, diet and exercise, kicking bad habits and so on. Finally, let the practice begin. Get a fertility-friendly lubricant and start your baby-making sessions. You’ll be scheduling your first prenatal appointment before you know it.
We also have a robust pregnancy resource guide that connects you with all kinds of tips and information to help you on your pregnancy journey.
Preterm birth | Shchelkovsky perinatal center
What is preterm birth?
Preterm labor is defined as regular uterine contractions resulting in changes in the cervix that begin before 37 weeks of gestation. Changes in the cervix include flattening (the cervix shortens) and dilatation (the cervix opens, allowing the fetus to enter the birth canal).
Why is preterm birth a concern?
Premature birth is a major health and social problem because babies who are born “too early” are not well developed for extrauterine life. They may be born with serious health problems. Some health problems, such as cerebral palsy, can last a lifetime. Other problems, such as learning disabilities, may appear later in childhood or even into adulthood.
Which premature babies are most at risk of health problems?
The risk of health problems is highest for babies born before 34 weeks of gestation. However, babies born between 34 and 37 weeks of gestation are also at risk.
What are the risk factors for preterm birth?
Factors that increase the risk of preterm birth include the following: having a preterm birth, a short cervix, a short interval between pregnancies, a history of certain types of uterine or cervical surgery, some pregnancy complications such as multiple pregnancies, and having history of bleeding, lifestyle factors such as low body weight before pregnancy, smoking during pregnancy, and substance abuse during pregnancy
Is there anything I can do to prevent preterm labor if I am at high risk?
If you have had a preterm birth and are planning another pregnancy, preconception examination (before conception). When you become pregnant, from the earliest dates it is necessary to be observed by an obstetrician-gynecologist. You may be referred to a healthcare professional who is experienced in managing high-risk pregnancies. In addition, you may be given certain medications or other treatments to help prevent preterm labor if you have risk factors.
What are the signs and symptoms of preterm labor and what should I do if I have any of them?
from the vagina (watery, mucous, or bloody), intermittent or cramping pain in the uterus, pain in the lower abdomen and lower back, mild abdominal cramps, with or without diarrhea
How is preterm birth diagnosed?
Premature birth can only be diagnosed if there are changes in the cervix. Your obstetrician should perform a manual examination to determine if there is or is not a change in the cervix. You may need to be examined several times within a few hours in order to assess changes in dynamics. A transvaginal ultrasound may be done to measure the length of the cervix.
If I have PR symptoms, does that mean I will definitely go into labor?
It is difficult for health care professionals to predict which women with symptoms of PB will definitely go into preterm labor. Only about 1 in 10 women with symptoms of PB will have them within the next 7 days. In about 3 out of 10 women, preterm labor stops on its own.
Premature birth - PCMC medical blog article
Preterm labor occurs when contractions begin before the 37th week of pregnancy. Along with contractions, changes occur in the cervix, which signal the onset of labor. The cervix begins to thin, a process called "fogging", and the cervix begins to dilate so that the baby can enter the birth canal. A normal pregnancy lasts about 40 weeks, so any labor that begins before this time is called an early or preterm labor.
Preterm birth factors
In most cases, the specific cause of preterm labor is unknown. Some risk factors have been identified that increase the likelihood of preterm birth. In addition to premature rupture of the amniotic sac, some of these major risk factors include the following:
Maternal factors in preterm birth
- Pre-eclampsia, or high blood pressure during pregnancy.
- Chronic medical problems including diabetes and kidney disease.
- Infections, especially streptococcal infection, urinary tract infections, vaginal infections, infections of fetal tissues or placenta.
- Abnormal structure of the uterus.
- Cervical incompetence, or a weak cervix that cannot remain closed as the child grows.
- Previous preterm birth.
Pregnancy-related risk factors for preterm birth
- Abnormal placenta or decreased placental function.
- Placenta previa, in which the placenta sits unusually low in the uterus, sometimes covering the opening of the cervix.
- Placental abruption, in which the cervix separates from the uterus too early during pregnancy.
- Premature rupture of the membranes of the amniotic sac.
- Hydramniosis, or too much amniotic fluid.
Fetus-related risk factors for preterm birth
- Signs of an unhealthy uterine environment, usually identified by fetal behavior.
- Pregnancy with twins, triplets or more.
- Erythroblastosis fetalis, or Rh/blood group incompatibility.
- Regular antenatal care with your obstetrician will help identify most of these problems. In fact, good prenatal care and proper nutrition are two of the best ways to reduce the risk of preterm birth.
Signs and symptoms of preterm labor
The warning signs of preterm labor are very similar to those of term labor. However, every woman experiences them differently. At first, they may be obvious or subtle. If you feel like you are having contractions, contact your doctor immediately. Don't worry about a possible false alarm. If it's a preterm birth, the sooner you and your doctor start treating it, the better the chances of a good outcome for you and your baby. Warning signs and symptoms of preterm labor include:
- Five or more contractions within an hour. They may feel like menstrual cramps or be relatively painless.
- Watery fluid from the vagina, or trickle of fluid (may indicate a discharge of water).
- Dull pain in the small of the back felt below the waist. It can be permanent, or it can come and go.
- Intestinal upset, nausea or diarrhoea.
- Pressure in the pelvis or lower abdomen, which may feel like a baby is pressing on you. You may also feel like you need to have a bowel movement.
- Vaginal discharge or bleeding.
- Increase or change in vaginal discharge which may be watery, bloody or mucous.
Because the symptoms of preterm labor can mimic other medical problems, it's best to have your doctor make the diagnosis. Remember that pregnant women usually have mild Braxton Hicks contractions late in pregnancy. However, frequent, regular contractions usually occur only during childbirth.
What are the risk factors for preterm birth?
Having a risk factor, or even multiple risk factors, does not mean you will go into preterm labor. Women without risk factors may also go into preterm labor without a known cause. However, if you have any of the risk factors listed below, discuss them with your doctor and learn what to do if you have a preterm birth.
- History of bladder or urinary tract infection.
- Sexually transmitted diseases or vaginal infections.
- Deficiency of red blood cells (anemia), especially in early pregnancy.
- During pregnancy, you had an infection with a temperature above 38 degrees.
- Vaginal bleeding any time after the 20th week of pregnancy.
- Multiple first trimester abortions or one or more second trimester abortions.
- Underweight or overweight before pregnancy.
- A bleeding disorder such as thrombophilia.
- You became pregnant through in vitro fertilization (IVF).
- You became pregnant within six months of giving birth to your previous child.
- You continue to smoke, drink alcohol or use illegal substances during pregnancy.
- You are in a situation of domestic violence, physical, sexual or emotional abuse.
- You are in a situation with insufficient social support.
- You are under a high level of stress.
- The work is associated with a long stay on the legs.
If you know you are at risk for preterm birth, consult with your obstetrician prior to pregnancy to start your pregnancy in the best possible health. Once you become pregnant, good prenatal care is essential. Your doctor will discuss managing your pregnancy to prevent preterm labor based on your situation and risk factors.
In addition to the above risk factors, some specific risks have been identified based on age and ethnicity. For example, African-American women are 50% more likely to have a preterm birth than Caucasian women. The chance of preterm birth is higher in women younger than 18 years of age, as well as in women over 35 years of age.
If I am at risk for preterm birth, is there anything I can do to prevent it?
Even if you're at an increased risk for preterm birth, there's a lot you can do to have a healthy and fulfilling pregnancy. Get good prenatal care from your obstetrician. Your doctor will monitor your health and that of your child. Be sure to discuss any symptoms that bother you, even if they seem minor to you.
Eat a quality, balanced diet, including extra calcium, iron, and folic acid. Take prenatal vitamins every day if possible, starting a few months before pregnancy.
Refrain from tobacco, alcohol throughout pregnancy. Talk to your doctor about all medications you take, including over-the-counter drugs and herbal supplements.
Research shows a link between preterm birth and in vitro fertilization (IVF), as IVF often results in multiple pregnancies, a risk factor for preterm birth. This is another topic to discuss with your obstetrician. Your doctor may recommend medicines to reduce your risk of preterm labor, including weekly progesterone injections or vaginal suppositories during the second trimester of pregnancy.
Your doctor may advise you to limit heavy lifting, strenuous physical activity, or spending too much time on your feet if you are at risk for preterm labor or have signs of preterm labor.
Since chronic diseases such as diabetes and high blood pressure increase the risk of preterm birth, it is important that you visit your health care provider during pregnancy.
Thanks to advances in preterm care, more babies born before 40 weeks of age are surviving and doing well. However, preventing preterm birth is the best way to ensure a healthy baby is born.
How can you tell a real contraction from a Braxton Hicks contraction?
You may have experienced painless Braxton Hicks contractions throughout your third trimester of pregnancy. They are usually irregular and do not dilate the cervix. As the due date approaches, these “training contractions” can become more frequent, and women usually feel as if they are about to go into labor. It can be difficult for women during their first pregnancy to distinguish "real" contractions from Braxton Hicks contractions later in pregnancy.
If you think you are having contractions that are not Braxton Hicks, drink fluids, avoid strenuous activities, and rest.