How to know when your child has an ear infection
Ear Infections in Children, Babies & Toddlers
What is an ear infection?
An ear infection is an inflammation of the middle ear, usually caused by bacteria, that occurs when fluid builds up behind the eardrum. Anyone can get an ear infection, but children get them more often than adults. Five out of six children will have at least one ear infection by their third birthday. In fact, ear infections are the most common reason parents bring their child to a doctor. The scientific name for an ear infection is otitis media (OM).
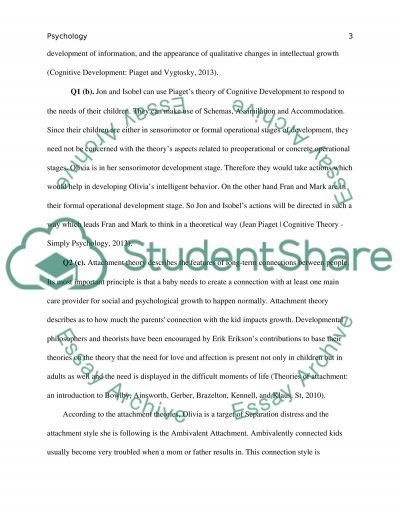
What are the symptoms of an ear infection?
There are three main types of ear infections. Each has a different combination of symptoms.
- Acute otitis media (AOM) is the most common ear infection. Parts of the middle ear are infected and swollen and fluid is trapped behind the eardrum. This causes pain in the ear—commonly called an earache. Your child might also have a fever.
- Otitis media with effusion (OME) sometimes happens after an ear infection has run its course and fluid stays trapped behind the eardrum.
A child with OME may have no symptoms, but a doctor will be able to see the fluid behind the eardrum with a special instrument.
- Chronic otitis media with effusion (COME) happens when fluid remains in the middle ear for a long time or returns over and over again, even though there is no infection. COME makes it harder for children to fight new infections and also can affect their hearing.
How can I tell if my child has an ear infection?
Most ear infections happen to children before they’ve learned how to talk. If your child isn’t old enough to say “My ear hurts,” here are a few things to look for:
- Tugging or pulling at the ear(s)
- Fussiness and crying
- Trouble sleeping
- Fever (especially in infants and younger children)
- Fluid draining from the ear
- Clumsiness or problems with balance
- Trouble hearing or responding to quiet sounds
What causes an ear infection?
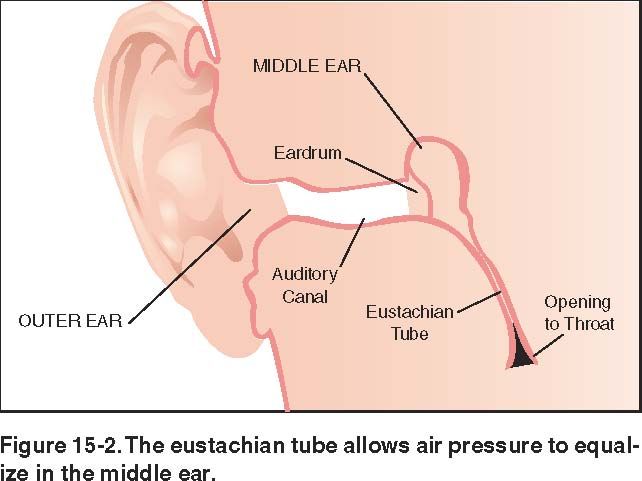
An ear infection usually is caused by bacteria and often begins after a child has a sore throat, cold, or other upper respiratory infection. If the upper respiratory infection is bacterial, these same bacteria may spread to the middle ear; if the upper respiratory infection is caused by a virus, such as a cold, bacteria may be drawn to the microbe-friendly environment and move into the middle ear as a secondary infection. Because of the infection, fluid builds up behind the eardrum.
If the upper respiratory infection is bacterial, these same bacteria may spread to the middle ear; if the upper respiratory infection is caused by a virus, such as a cold, bacteria may be drawn to the microbe-friendly environment and move into the middle ear as a secondary infection. Because of the infection, fluid builds up behind the eardrum.
Image
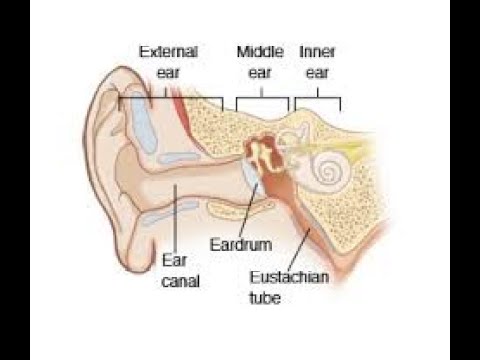
Source: NIH/NIDCDThe ear has three major parts: the outer ear, the middle ear, and the inner ear. The outer ear, also called the pinna, includes everything we see on the outside—the curved flap of the ear leading down to the earlobe—but it also includes the ear canal, which begins at the opening to the ear and extends to the eardrum. The eardrum is a membrane that separates the outer ear from the middle ear.
The middle ear—which is where ear infections occur—is located between the eardrum and the inner ear. Within the middle ear are three tiny bones called the malleus, incus, and stapes that transmit sound vibrations from the eardrum to the inner ear. The bones of the middle ear are surrounded by air.
The bones of the middle ear are surrounded by air.
The inner ear contains the labyrinth, which help us keep our balance. The cochlea, a part of the labyrinth, is a snail-shaped organ that converts sound vibrations from the middle ear into electrical signals. The auditory nerve carries these signals from the cochlea to the brain.
Other nearby parts of the ear also can be involved in ear infections. The eustachian tube is a small passageway that connects the upper part of the throat to the middle ear. Its job is to supply fresh air to the middle ear, drain fluid, and keep air pressure at a steady level between the nose and the ear.
Adenoids are small pads of tissue located behind the back of the nose, above the throat, and near the eustachian tubes. Adenoids are mostly made up of immune system cells. They fight off infection by trapping bacteria that enter through the mouth.
Why are children more likely than adults to get ear infections?
There are several reasons why children are more likely than adults to get ear infections.
Eustachian tubes are smaller and more level in children than they are in adults. This makes it difficult for fluid to drain out of the ear, even under normal conditions. If the eustachian tubes are swollen or blocked with mucus due to a cold or other respiratory illness, fluid may not be able to drain.
A child’s immune system isn’t as effective as an adult’s because it’s still developing. This makes it harder for children to fight infections.
As part of the immune system, the adenoids respond to bacteria passing through the nose and mouth. Sometimes bacteria get trapped in the adenoids, causing a chronic infection that can then pass on to the eustachian tubes and the middle ear.
How does a doctor diagnose a middle ear infection?
The first thing a doctor will do is ask you about your child’s health. Has your child had a head cold or sore throat recently? Is he having trouble sleeping? Is she pulling at her ears? If an ear infection seems likely, the simplest way for a doctor to tell is to use a lighted instrument, called an otoscope, to look at the eardrum. A red, bulging eardrum indicates an infection.
A red, bulging eardrum indicates an infection.
A doctor also may use a pneumatic otoscope, which blows a puff of air into the ear canal, to check for fluid behind the eardrum. A normal eardrum will move back and forth more easily than an eardrum with fluid behind it.
Tympanometry, which uses sound tones and air pressure, is a diagnostic test a doctor might use if the diagnosis still isn’t clear. A tympanometer is a small, soft plug that contains a tiny microphone and speaker as well as a device that varies air pressure in the ear. It measures how flexible the eardrum is at different pressures.
How is an acute middle ear infection treated?
Many doctors will prescribe an antibiotic, such as amoxicillin, to be taken over seven to 10 days. Your doctor also may recommend over-the-counter pain relievers such as acetaminophen or ibuprofen, or eardrops, to help with fever and pain. (Because aspirin is considered a major preventable risk factor for Reye’s syndrome, a child who has a fever or other flu-like symptoms should not be given aspirin unless instructed to by your doctor. )
)
If your doctor isn’t able to make a definite diagnosis of OM and your child doesn’t have severe ear pain or a fever, your doctor might ask you to wait a day or two to see if the earache goes away. The American Academy of Pediatrics issued guidelines in 2013 that encourage doctors to observe and closely follow these children with ear infections that can’t be definitively diagnosed, especially those between the ages of 6 months to 2 years. If there’s no improvement within 48 to 72 hours from when symptoms began, the guidelines recommend doctors start antibiotic therapy. Sometimes ear pain isn’t caused by infection, and some ear infections may get better without antibiotics. Using antibiotics cautiously and with good reason helps prevent the development of bacteria that become resistant to antibiotics.
If your doctor prescribes an antibiotic, it’s important to make sure your child takes it exactly as prescribed and for the full amount of time. Even though your child may seem better in a few days, the infection still hasn’t completely cleared from the ear. Stopping the medicine too soon could allow the infection to come back. It’s also important to return for your child’s follow-up visit, so that the doctor can check if the infection is gone.
Stopping the medicine too soon could allow the infection to come back. It’s also important to return for your child’s follow-up visit, so that the doctor can check if the infection is gone.
How long will it take my child to get better?
Your child should start feeling better within a few days after visiting the doctor. If it’s been several days and your child still seems sick, call your doctor. Your child might need a different antibiotic. Once the infection clears, fluid may still remain in the middle ear but usually disappears within three to six weeks.
What happens if my child keeps getting ear infections?
To keep a middle ear infection from coming back, it helps to limit some of the factors that might put your child at risk, such as not being around people who smoke and not going to bed with a bottle. In spite of these precautions, some children may continue to have middle ear infections, sometimes as many as five or six a year. Your doctor may want to wait for several months to see if things get better on their own but, if the infections keep coming back and antibiotics aren’t helping, many doctors will recommend a surgical procedure that places a small ventilation tube in the eardrum to improve air flow and prevent fluid backup in the middle ear. The most commonly used tubes stay in place for six to nine months and require follow-up visits until they fall out.
The most commonly used tubes stay in place for six to nine months and require follow-up visits until they fall out.
If placement of the tubes still doesn’t prevent infections, a doctor may consider removing the adenoids to prevent infection from spreading to the eustachian tubes.
Can ear infections be prevented?
Currently, the best way to prevent ear infections is to reduce the risk factors associated with them. Here are some things you might want to do to lower your child’s risk for ear infections.
- Vaccinate your child against the flu. Make sure your child gets the influenza, or flu, vaccine every year.
- It is recommended that you vaccinate your child with the 13-valent pneumococcal conjugate vaccine (PCV13). The PCV13 protects against more types of infection-causing bacteria than the previous vaccine, the PCV7. If your child already has begun PCV7 vaccination, consult your physician about how to transition to PCV13. The Centers for Disease Control and Prevention (CDC) recommends that children under age 2 be vaccinated, starting at 2 months of age.
 Studies have shown that vaccinated children get far fewer ear infections than children who aren’t vaccinated. The vaccine is strongly recommended for children in daycare.
Studies have shown that vaccinated children get far fewer ear infections than children who aren’t vaccinated. The vaccine is strongly recommended for children in daycare. - Wash hands frequently. Washing hands prevents the spread of germs and can help keep your child from catching a cold or the flu.
- Avoid exposing your baby to cigarette smoke. Studies have shown that babies who are around smokers have more ear infections.
- Never put your baby down for a nap, or for the night, with a bottle.
- Don’t allow sick children to spend time together. As much as possible, limit your child’s exposure to other children when your child or your child’s playmates are sick.
What research is being done on middle ear infections?
Researchers sponsored by the National Institute on Deafness and Other Communication Disorders (NIDCD) are exploring many areas to improve the prevention, diagnosis, and treatment of middle ear infections. For example, finding better ways to predict which children are at higher risk of developing an ear infection could lead to successful prevention tactics.
Another area that needs exploration is why some children have more ear infections than others. For example, Native American and Hispanic children have more infections than do children in other ethnic groups. What kinds of preventive measures could be taken to lower the risks?
Doctors also are beginning to learn more about what happens in the ears of children who have recurring ear infections. They have identified colonies of antibiotic-resistant bacteria, called biofilms, that are present in the middle ears of most children with chronic ear infections. Understanding how to attack and kill these biofilms would be one way to successfully treat chronic ear infections and avoid surgery.
Understanding the impact that ear infections have on a child’s speech and language development is another important area of study. Creating more accurate methods to diagnose middle ear infections would help doctors prescribe more targeted treatments. Researchers also are evaluating drugs currently being used to treat ear infections, and developing new, more effective and easier ways to administer medicines.
NIDCD-supported investigators continue to explore vaccines against some of the most common bacteria and viruses that cause middle ear infections, such as nontypeable Haemophilus influenzae (NTHi) and Moraxella catarrhalis. One team is conducting studies on a method for delivering a possible vaccine without a needle.
Where can I find additional information about ear infections?
The NIDCD maintains a directory of organizations that provide information on the normal and disordered processes of hearing, balance, smell, taste, voice, speech, and language.
Use the following keywords to help you search for organizations that can answer questions and provide printed or electronic information on ear infections:
- Otitis media (ear infection)
- Speech-language development
- Early identification of hearing loss in children
NIDCD Information Clearinghouse
1 Communication Avenue
Bethesda, MD 20892-3456
Toll-free voice: (800) 241-1044
Toll-free TTY: (800) 241-1055
Email: nidcdinfo@nidcd.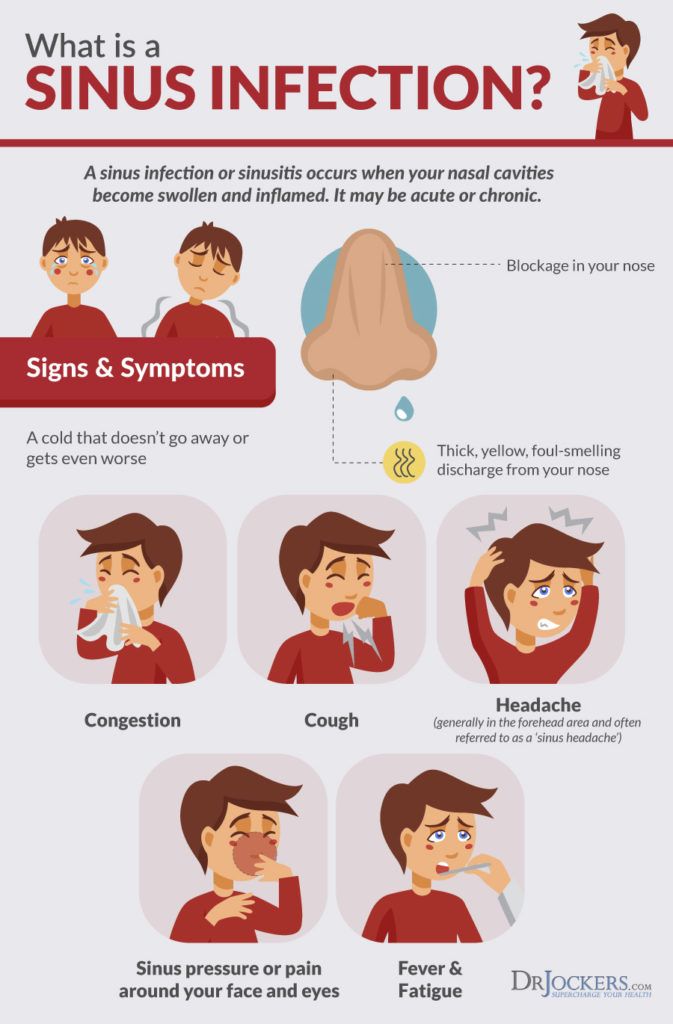 nih.gov
nih.gov
Ear Infections in Babies and Toddlers
Featured Expert:
Ear infections in babies and toddlers are extremely common. In fact, according to the National Institutes of Health, five out of six children will experience an ear infection before their third birthday.
"Many parents are concerned that an ear infection will affect their child's hearing irreversibly—or that an ear infection will go undetected and untreated," says David Tunkel, M.D., Johns Hopkins Medicine pediatric otolaryngologist (ENT). "The good news is that most ear infections go away on their own, and those that don't are typically easy to treat."
Childhood Ear Infections Explained
Ear infections happen when there is inflammation— usually from trapped bacteria—in the middle ear, the part of the ear connects to the back of the nose and throat.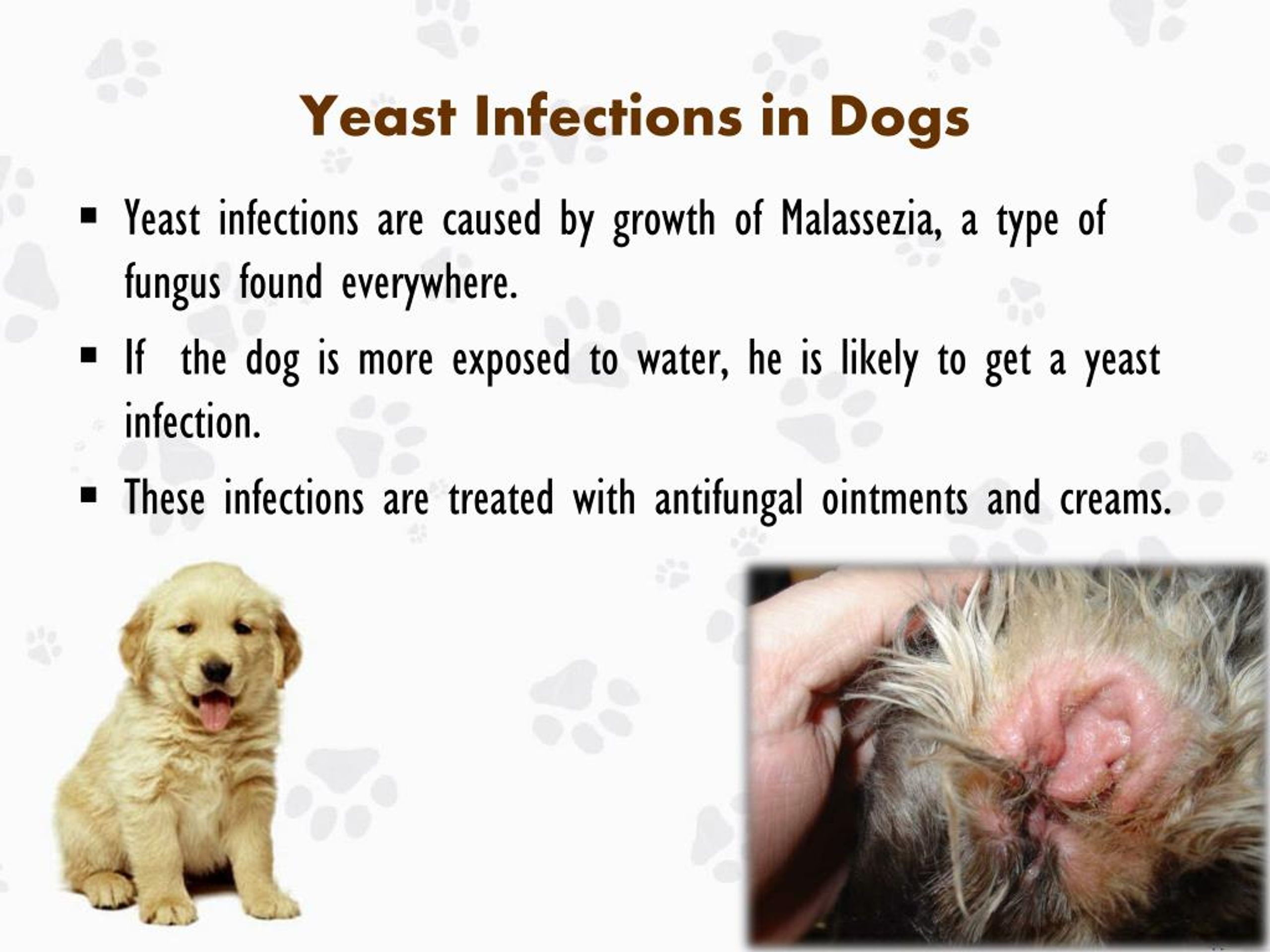 The most common type of ear infection is otitis media, which results when fluid builds up behind the eardrum and parts of the middle ear become infected and swollen.
The most common type of ear infection is otitis media, which results when fluid builds up behind the eardrum and parts of the middle ear become infected and swollen.
If your child has a sore throat, cold, or an upper respiratory infection, bacteria can spread to the middle ear through the eustachian tubes (the channels that connect the middle ear to the throat). In response to the infection, fluid builds up behind the eardrum.
Children are more likely to suffer from ear infections than adults for two reasons:
- Their immune systems are underdeveloped and less equipped to fight off infections.
- Their eustachian tubes are smaller and more horizontal, which makes it more difficult for fluid to drain out of the ear.
"In some cases, fluid remains trapped in the middle ear for a long time, or returns repeatedly, even when there's no infection," Tunkel explains.
Ear Infection Signs and Symptoms
The telltale sign of an ear infection is pain in and around the ear. Young children can develop ear infections before they are old enough to talk. That means parents are often left guessing why their child appears to be suffering. When your child can't say "my ear hurts," the following signs suggest an ear infection could be the culprit:
Young children can develop ear infections before they are old enough to talk. That means parents are often left guessing why their child appears to be suffering. When your child can't say "my ear hurts," the following signs suggest an ear infection could be the culprit:
- Tugging or pulling the ear
- Crying and irritability
- Difficulty sleeping
- Fever, especially in younger children
- Fluid draining from the ear
- Loss of balance
- Difficulty hearing or responding to auditory cues
Signs that require immediate attention include high fever, severe pain, or bloody or pus-like discharge from the ears.
Pediatric Otolaryngology
Our pediatric otolaryngologists provide compassionate and comprehensive care for children with common and rare ear, nose, and throat conditions. As part of the Johns Hopkins Children's Center, you have access to all the specialized resources of a children's hospital.
Learn more about Pediatric Otolaryngology
Ear Infection Treatments
Most ear infections go away without treatment. "If your child isn't in severe pain, your doctor may suggest a 'wait-and-see' approach coupled with over-the-counter pain relievers to see if the infection clears on its own," Tunkel says.
The reason: Treating an infection with antibiotics may cause the bacteria causing the infections to become resistant to those antibiotics—and that makes treating future infections more difficult. Equally important, in most cases antibiotics aren't necessary. Otitis media tends to get better without them. While you may be tempted to treat your child's ear infection with homeopathic or natural medicine, Tunkel warns they aren’t well studied.
Your best bet is to work with your child's health care provider to determine the appropriate course of action. In nearly every case, treatment decisions depend on the child’s age, degree of pain and presenting symptoms.
Under 6 months
Babies under six months almost always receive antibiotics. At this age, children are not fully vaccinated. Equally important, there's no research about the safety of skipping antibiotics for babies under 6 months of age — and complications from ear infections can be more severe when they occur in young babies. Bacteria trapped behind the eardrum can spread to other parts of the body and cause serious infections.
6 months to 2 years
For children between the ages of 6 months and 2 years, the American Academy of Pediatrics (AAP) recommends shared decision-making between parents and providers about whether to treat ear infections that are not severe. The best course is often to watch the child for two to three days before prescribing antibiotic treatment. If the child is in pain, or the ear infection is advanced, your child's doctor may suggest immediate antibiotic treatment.
Over 2 years
With children over the age of 2, ear infections that are not severe are likely to clear on their own, without treatment. "In the meantime, you can treat pain with over-the-counter medications, such as ibuprofen or acetaminophen," Tunkel says. If there's no improvement after two to three days, antibiotics may be warranted.
"In the meantime, you can treat pain with over-the-counter medications, such as ibuprofen or acetaminophen," Tunkel says. If there's no improvement after two to three days, antibiotics may be warranted.
Unfortunately, some children suffer from recurrent ear infections, sometimes up to five or six a year. Kids who get repeated infections may benefit from a surgical procedure where doctors insert small tubes in the eardrums to improve air flow and prevent fluid buildup. "Tubes don't prevent all ear infections, but they make managing them significantly easier," Tunkel explains.
Ear Infection Prevention
There are several steps you can take to reduce your child's risk of developing ear infections, including:
- Vaccinate your child: Children who are up-to-date on their vaccines get fewer ear infections than their unvaccinated counterparts. The 13-valent pneumococcal conjugate vaccine (PCV13) protects against 13 types of infection-causing bacteria.

- Consider breastfeeding: Breast milk contains antibodies that may help reduce the risk of ear infections and a host of other ailments. Whether you feed milk or formula, make sure your child sits up during feedings to prevent fluid from flowing into the middle ear.
- Wash your hands frequently: The best way to protect your child against cold and flu is to keep your hands clean. Wash your hands with soap and water and scrub them clean for a full 20 seconds each time you visit the sink.
- Steer clear of sick people: Don't allow your child to spend time with children or adults who are sick.
- Avoid secondhand smoke: Studies show that children who are exposed to secondhand smoke are up to three times more likely to develop ear infections than those who don't have those exposures.
Whether your child has ear infections or not, it's important to ensure they're able to hear well. "No child is too young to have a hearing test," Tunkel says. "We use a variety of techniques to test infant hearing and we can identify a hearing problem even in newborns."
"No child is too young to have a hearing test," Tunkel says. "We use a variety of techniques to test infant hearing and we can identify a hearing problem even in newborns."
What are the main causes of ear infections in children?
Children under 10 years of age are much more susceptible than older children and adults to infections in the middle ear, a small space that lies deep behind the eardrum.
Older children and adults usually get infections in the ear canal but not in the middle ear.
The eardrum acts as a barrier protecting the middle ear. Infections in this area occur when bacteria or viruses that are inhaled enter the back of the nose, travel up the Eustachian cavity and infect the middle ear. Young children naturally did not have time to develop immunity to the many bacteria or viruses in the air.
A number of major causes, infection is inevitable:
First, young age: children have ineffective Eustachian tubes and have not developed immunity to many infections.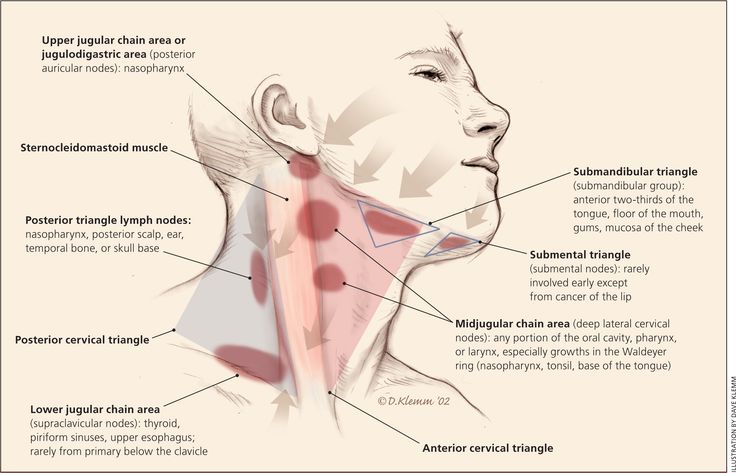
Secondly, being in large groups indoors, at school or kindergarten.
However, the main significant factor that can be controlled is exposure to smoke. Children in families of smokers are more prone to ear infections.
How can you tell if your child has an ear infection?
Diagnosing an ear infection in children can be difficult, especially in a child who is too young to tell you they have an earache.
The main symptoms are that the child is upset and has a temperature. Some children rub or pull on their ears. A doctor examining a child's ear will see a red eardrum.
Sometimes infected fluid deep in the eardrum causes the eardrum to rupture and blood with the infected fluid leaks out of the ear. This is commonly referred to as a tympanic membrane rupture. Once the eardrum bursts, often the child will feel much less pain. Most ruptured eardrums heal within a few weeks.
Should I take my child to an ENT doctor for an ear infection?
If you suspect your child has an ear infection, the first thing to do is to relieve the pain with pediatric paracetamol and ibuprofen.
It would be wise to see a pediatric otolaryngologist during the daytime for a routine appointment. At least half of all ear infections clear up within 3 days, so simply treat the pain until it goes away. In some children, the infection persists and may require a course of oral antibiotics.
Will ear infections go away without antibiotics?
At least half of childhood ear infections go away without antibiotics. Most of them can be simply treated with regular children's paracetamol and ibuprofen. Most infections resolve within 3 days.
What happens if the infection is not treated?
If the infection does not go away within a few days, and if no further treatment is given, first, the child will experience pain for a much longer period. During this period, the infected ear will hear worse. However, many cases may simply require additional time to heal.
If the infection progresses, the infection may spread to the bone behind the ear.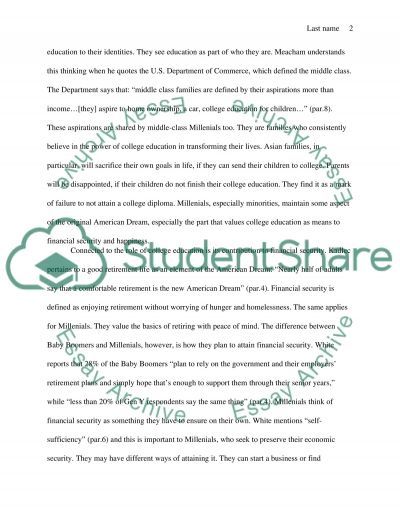 From here, it can progress outward, towards the skin, and begin to leak out. This can affect the muscles below the neck and cause an abscess in the muscle. Most seriously, it can spread inward and cause a potentially life-threatening infection of the brain.
From here, it can progress outward, towards the skin, and begin to leak out. This can affect the muscles below the neck and cause an abscess in the muscle. Most seriously, it can spread inward and cause a potentially life-threatening infection of the brain.
Ear infection in children and adults: symptoms and treatment
Contents
- Causes of ear diseases
- Symptoms and treatment of diseases
- Middle ear infections
- External ear infections
- Swimmer's ear
- Names of diseases of the ears
- Ear diseases
- Which doctor to contact for ear pain 906 Diagnosis and admission 906 906 at the doctor's office
- Preparations for treatment of ear diseases
- Recipes of folk remedies for the treatment of ears
- Complications caused by diseases of the ears
- Conclusion
Contents
Causes of ear diseases
Infections or other factors may be the preconditions for the occurrence of such diseases.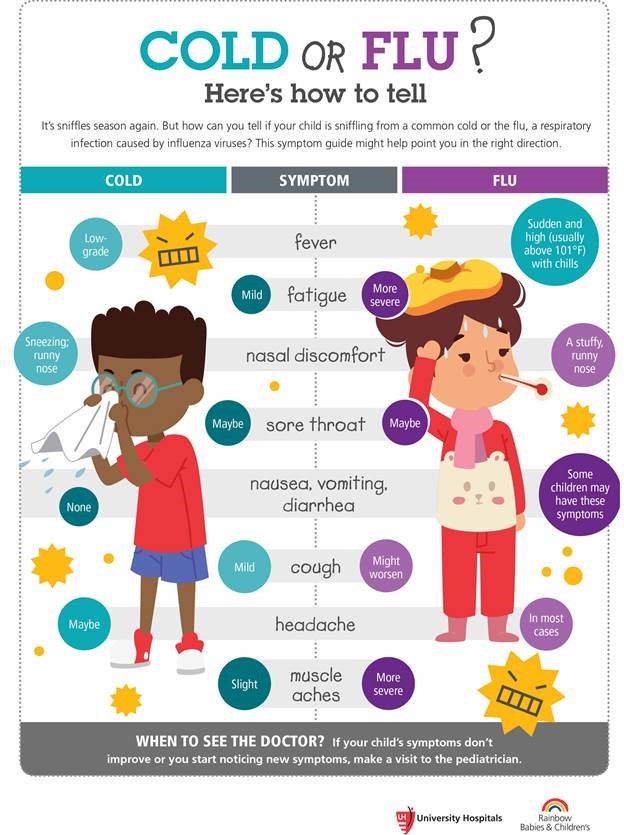 Sometimes ear pain can occur as a result of complications from other diseases or damage to the hearing aid itself.
Sometimes ear pain can occur as a result of complications from other diseases or damage to the hearing aid itself.
Common causes of ear problems are:
- Sinusitis or tonsillitis, especially if they are chronic. If left untreated for a long time, it can lead to the spread of the infection. It can even reach the middle ear.
- A decrease in body temperature leads to vasoconstriction, and such conditions are very favorable for the reproduction of bacteria that lead to an inflammatory process.
- Destruction of the tympanic membrane, violation of its integrity resulting from trauma.
- Pathologies of the jaw can affect the condition of the inner ear.
- Cervical osteochondrosis.
- Inflammation of the tonsils.
- Acute forms of viral and catarrhal diseases.
- Allergic reactions.
- Diabetes mellitus.
- Inaccurate or very frequent removal of sulfur by mechanical means.
- Failure in the circulation of the brain.
- Presence of a foreign body or obstruction of the ear.
- Too much physical effort.
- Disorders of the endocrine system.
- Decreased immunity due to an unbalanced diet, lack of vegetables and fruits in it.
- Dental diseases.
All of the above factors worsen the body's resistance to various infections. The link lists the reasons why the ears itch inside.
What causes ear infections?
Ear infections occur when one of your Eustachian (auditory) tubes becomes inflamed due to swelling, causing fluid to accumulate in your middle ear. The Eustachian tubes are small tubes that connect between the ear and the back of the throat. Eustachian tube blockages are caused by:
- allergies
- inflammation of the paranasal sinuses
- excess mucus
- smoking
- infected or enlarged adenoids
Symptoms and treatment of diseases
Pain occurs suddenly, a person may not immediately guess what the problem is and waits for the pain to go away by itself, but delaying treatment is fraught with consequences. Knowing the symptoms will help determine which disease is worrying at the moment.
Knowing the symptoms will help determine which disease is worrying at the moment.
Middle ear infections
The middle ear is located just behind the eardrum. Middle ear infections usually occur when bacteria or viruses from the mouth, eyes, and nasal passages enter the middle ear area. The result is pain and a feeling of clogged ears. Some people may experience hearing problems as the inflamed eardrum becomes insensitive to sound. A buildup of fluid or pus behind the eardrum also affects hearing. It may seem that the sore ear is under water. Fever and general weakness may accompany a middle ear infection.
How to treat otitis media
Acute otitis media is most common in children, although adults can also suffer from it, in whom the disease can be chronic with periods of exacerbations. Its occurrence is associated with the development of SARS, influenza or exacerbation of infectious and inflammatory processes in the nasopharynx. The disease has the character of a complication, a secondary process against the background of a weakening of the general immune defense or a decrease in local resistance of the mucous membranes.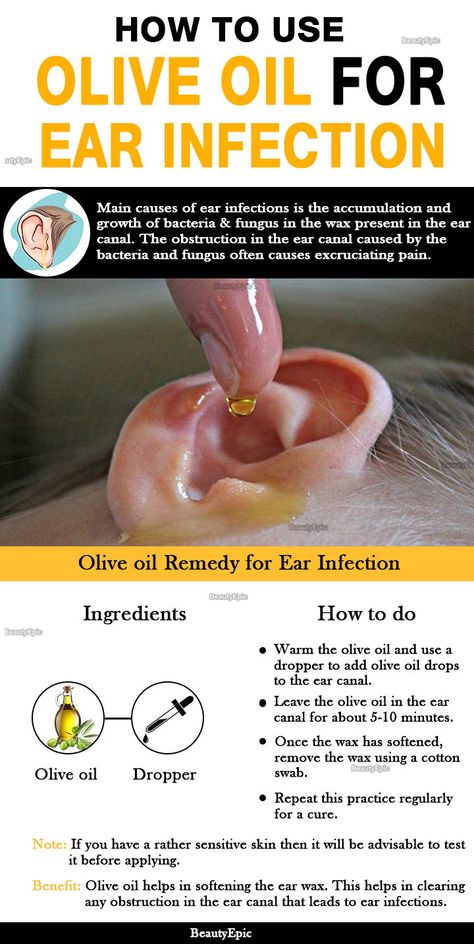 Hypothermia, improper ear care, chronic runny nose, abuse of sprays and drops with vasoconstrictive substances contribute to the formation of symptoms of otitis media.
Hypothermia, improper ear care, chronic runny nose, abuse of sprays and drops with vasoconstrictive substances contribute to the formation of symptoms of otitis media.
A common cause of otitis media is penetration into the ear cavity of the infection in an ascending way - from the nasopharynx with acute respiratory viral infections or adenoiditis, sinusitis. Rarely, the introduction of microbes occurs with the flow of blood or lymph from distant foci. In such a situation, otitis media can be treated both conservatively, through the use of local and systemic drugs, and operatively, with the risk of pus breaking into the cranial cavity and unbearable pain.
Often acute otitis media is manifested by fever and general malaise against the background of sharp and severe pain in the ear area, on one side or on both sides at once. In the process of accumulation of fluid and edema in the ear cavity, hearing decreases, especially at the peak of the process, with perforation of the membrane and outflow of pus, with adequate treatment, this symptom gradually disappears. In the absence of any medicinal measures when using traditional methods, complications and permanent hearing loss may develop. Only a doctor can prescribe treatment for otitis media (inflammation of the middle ear).
In the absence of any medicinal measures when using traditional methods, complications and permanent hearing loss may develop. Only a doctor can prescribe treatment for otitis media (inflammation of the middle ear).
Broad-spectrum antibiotics are given first. In addition to them, ear drops with anti-inflammatory, analgesic and antiseptic effects are used.
If there is a threat of the spread of the process, a breakthrough of pus into the cranial cavity, or if there are special indications, the ENT doctor may resort to surgical treatment - puncture of the membrane (paracentesis) to drain pus from the tympanic cavity, while continuing all the necessary therapeutic measures.
Separately, it is worth dwelling on dubious and dangerous recipes labeled “how to quickly cure otitis media” from the Internet or at the prompts of the older generation. Doctors strongly do not recommend practicing them, especially if there is a threat of perforation of the membrane or there is a hole in it.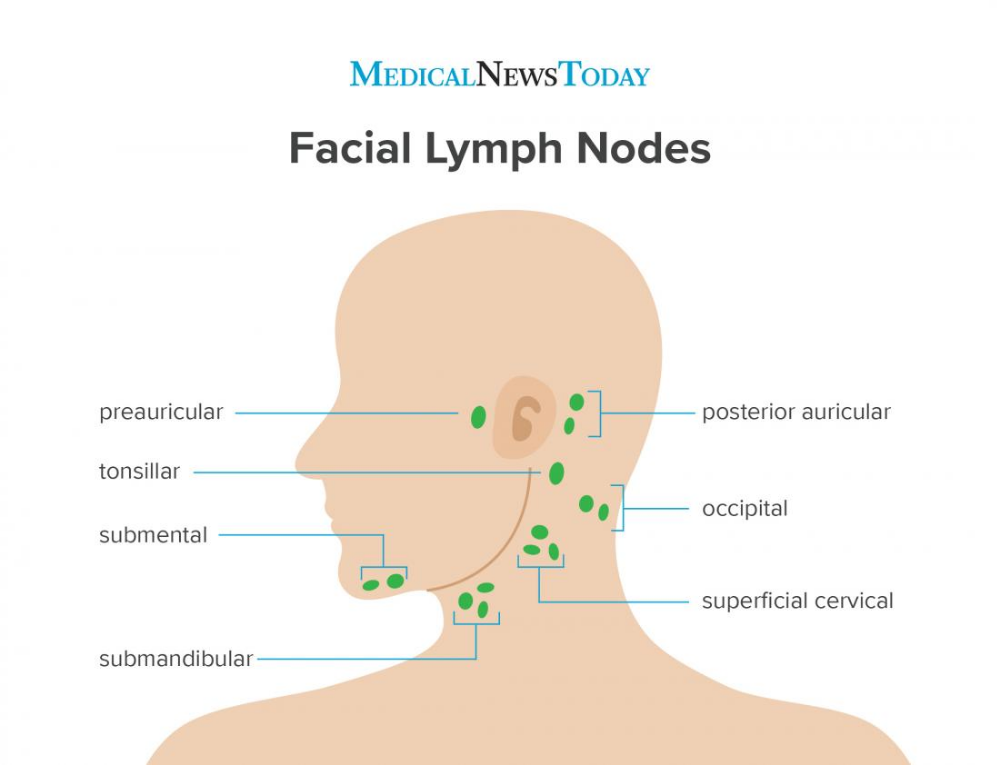 Instillation into the ear of various decoctions and tinctures, especially alcohol, outdated drugs threatens not only with persistent hearing loss, but also with the possibility of developing meningitis.
Instillation into the ear of various decoctions and tinctures, especially alcohol, outdated drugs threatens not only with persistent hearing loss, but also with the possibility of developing meningitis.
Infection of the outer ear
The outer ear includes the auricle and external auditory canal. External ear infections may begin as an itchy rash on the outside of the ear. The ear canal is an ideal breeding ground for germs, and as a result, an outer ear infection can develop. External ear infections can be caused by irritation or damage to the ear canal by foreign objects. Common symptoms include ear canal pain and swelling. The ear may become red and hot to the touch.
How to treat otitis externa
A common variant of the pathology is otitis externa, an inflammatory process affecting the skin or cartilage of the auricle, as well as the area of the ear canal and the outer part of the membrane facing the canal. Therapy depends on the causes that caused it, since inflammation can be infectious (microbial, less often viral) or allergic, can be caused by water ingress and swelling of sulfur, which causes irritation ("swimmer's ear"). Inflammation with this type of otitis can be acute, lasting up to two weeks on average, and chronic, when the process of tissue damage lasts for months. The cause is usually microbes belonging to the group of opportunistic pathogens (most often staphylococcus and Pseudomonas aeruginosa), less often fungi.
Inflammation with this type of otitis can be acute, lasting up to two weeks on average, and chronic, when the process of tissue damage lasts for months. The cause is usually microbes belonging to the group of opportunistic pathogens (most often staphylococcus and Pseudomonas aeruginosa), less often fungi.
See also: Inflammation of the middle ear
How is otitis media treated in such cases? Traditionally, local therapy in the form of drops, turundas with drugs or physiotherapy procedures (stimulating, warming, regenerating techniques) are used. Only with the ineffectiveness of the above measures, they resort to systemic therapy - the appointment of drugs orally or in the form of injections. The question of how to cure otitis of this form is decided by the ENT doctor, he prescribes drops or ointments for skin pathology in the auricle (with antibiotics, anti-inflammatory and hormonal components). If manifestations of otitis externa are accompanied by an increase in temperature, reception is indicated antipyretics in age dosages, oral antibiotics are used in bacterial process .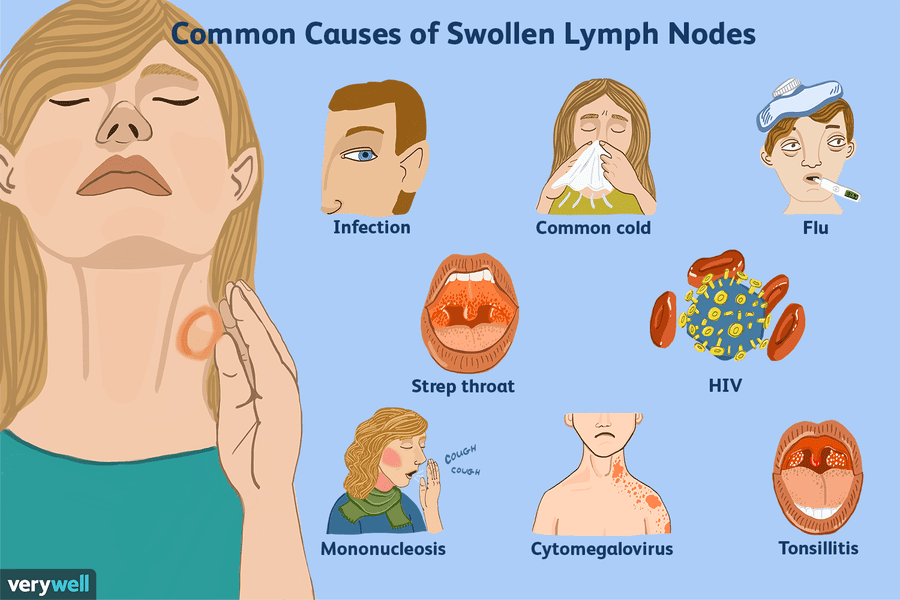
If the nature of the infection is fungal (determined by culture data and the clinical picture), the doctor determines how otitis media is treated - with the help of external or internal drugs with antifungal components .
Do not practice various folk and home remedies to eliminate inflammation, especially if the cause is an abscess or boil. It is forbidden to squeeze them out or process them with tinctures, make lotions. Self-medication threatens with dangerous complications with the spread of pus to the inner ear and even into the cranial cavity. Any recipes of traditional medicine should be discussed with a doctor, in some cases they may be contraindicated, especially in the presence of an allergic nature of inflammation.
Swimmer's ear
People who spend a lot of time in the water are at risk of developing outer ear infections. The water that enters the ear canal after swimming creates an ideal breeding ground for germs.
Ear infections can go away on their own in many cases, so minor ear pain is nothing to worry about. If the symptoms do not go away within 3 days and new symptoms appear, such as fever, a doctor should be consulted.
If the symptoms do not go away within 3 days and new symptoms appear, such as fever, a doctor should be consulted.
Diagnosis of ear infections in adults
To make a correct diagnosis, the doctor must ask about the symptoms, as well as the drugs the patient is taking. The doctor usually uses an instrument called an otoscope to look at the eardrum and ear canal for signs of infection.
Names of diseases of the ears
Most ear diseases have a similar clinical picture, manifested in the form of pain, itching, burning, redness of the skin, discharge, hearing loss. With a strong inflammatory process, there is a deterioration in the functioning of the vestibular apparatus - impaired coordination, dizziness, nausea, vomiting.
Ear diseases
Eustachitis
Infectious pathology in which the auditory canal is damaged, the ventilation process in the tympanic cavity is disturbed, catarrhal otitis media develops. The cause of the disease is the penetration of pathogenic microorganisms from the nasopharynx and upper respiratory tract.
Symptoms:
- pain, sensation of water inside the ear, discomfort worse with movement;
- hearing loss;
- an increase in temperature indicates the development of a purulent process.
The most dangerous ear pathology is deafness. The congenital form occurs even in the womb due to viral infections in the mother, the acquired form develops in children under three years old, as a complication of other diseases, when exposed to certain drugs.
Mastoiditis
Infectious pathology, characterized by inflammation of the mastoid process of the temporal bone, the presence of a purulent process, occurs when the infection spreads from the middle ear. The main pathogens are influenza bacillus, pneumococci, staphylococci, streptococci.
Signs of illness:
- fever;
- signs of severe intoxication;
- impairment of auditory perception;
- throbbing pain;
- auricle swollen, slightly protruding;
- there is purulent discharge from the ear.
A sudden attack of vertigo often indicates the beginning of an inflammatory process in the inner ear.
Meniere's disease
Against the background of the disease, narrowing and damage of blood vessels occur, blood supply is disturbed, fluid accumulates near the ear cavity. The exact causes of the development of pathology have not yet been identified, some experts believe that the disease is of viral origin, other doctors adhere to the hereditary theory. Trigger factors - disturbances in the work of blood vessels, low levels of estrogen, changes in the water-salt balance.
Clinical picture:
- tinnitus, congestion;
- dizziness, nausea;
- balance worsens;
- Loud noises cause irritation.
Minier's disease is considered incurable, therapy is aimed at prolonging the remission stage. Patients should adhere to a salt-free diet, give up addictions, and avoid exposure to ultraviolet radiation.
Acoustic neuritis (cochlear neuritis)
The disease refers to pathologies of a neurological nature, the causes of the disease are inflammatory processes in the nasopharynx, injuries, cervical osteochondrosis, cardiovascular and endocrine diseases, atherosclerosis, brain injuries.
Symptoms:
- hearing impairment;
- flickering of black spots before eyes;
- dull headaches;
- tinnitus;
- attacks of vertigo.
If the disease is started, necrosis of the tissues of the auditory nerve will begin, which will lead to complete irreversible hearing loss.
Otomycosis
Fungal infection that affects the membranes and ear canal, the causative agents of the disease are yeast-like and mold fungi.
Symptoms:
- itching, stuffy ear;
- plugs, ulcers and crusts form;
- the ear swells, discharge from the ear canal appears, the skin dries up.

Otomycosis is most often diagnosed in diabetics, HIV-positive people, and cancer patients.
Otitis and tympanitis
Inflammatory process in various parts of the hearing organs, the most common ear disease, develops as a complication of flu, colds, tonsillitis, sinusitis, ear injuries. Most often diagnosed in children and the elderly.
Types and symptoms of otitis media:
- Otitis externa. With an organic form, boils appear on the outer part of the auditory canal, which develop in the sebaceous glands, hair follicles, the disease is accompanied by sharp pain, an increase in the parotid lymph nodes, and ulcers form at the site of bursting abscesses. Diffuse otitis media develops when the ear is damaged by viruses, bacteria, fungi, purulent discharge appears, the ear turns red, itches, clicks, the touch is accompanied by pain, unpleasant sensations increase when the mouth is opened.
- Otitis media - develops when pathogenic microorganisms penetrate into the ear cavity, which irritate the Eustachian tube.
 At the initial stage of the disease, there is a strong shooting pain that radiates to the head, the temperature rises, and auditory perception worsens. The second stage is accompanied by purulent discharge, while the pain disappears, the temperature decreases. The disappearance of suppuration against the background of severe hearing loss indicates the beginning of the third stage of the disease.
At the initial stage of the disease, there is a strong shooting pain that radiates to the head, the temperature rises, and auditory perception worsens. The second stage is accompanied by purulent discharge, while the pain disappears, the temperature decreases. The disappearance of suppuration against the background of severe hearing loss indicates the beginning of the third stage of the disease. - Labyrinth - inflammation of the inner ear, accompanied by bouts of dizziness, poor balance, nausea, vomiting, tinnitus. As the pathology develops, the color of the skin changes, and discomfort occurs in the region of the heart.
- Mesotympanitis is a type of purulent otitis, the symptoms are similar to inflammation of the middle ear, pus is released periodically.
- Epitympanitis - a severe form of otitis media, in which the bone rots, the walls of the middle ear are destroyed, purulent discharge has a sharp unpleasant odor, severe and prolonged pain.
Heating of the ear with otitis media can only be carried out in the absence of temperature and purulent discharge.
Sinusitis
Sinusitis is an inflammation of the mucous membrane of the paranasal sinuses. It occurs as a secondary disease against the background of colds, rhinitis or flu, as well as with a mechanical injury to the nose. A sharp pain in the sinuses is almost immediately transmitted to the ear.
See also: Adhesive otitis: symptoms and treatment of the disease
Otogenic sepsis
Severe complication that occurs as a result of the spread of purulent inflammation from the middle ear. Infection through the lymphatic tract or through the vessels of the meninges enters the general circulation. The diagnosis is typical for young and middle age. Symptoms come on suddenly and include:
- temperature fluctuations;
- chills;
- increased sweating;
- tachycardia;
- refusal to eat;
- deterioration of health;
- shortness of breath.
Surgery is mandatory, so this condition requires immediate hospitalization.
Otosclerosis
This is a hereditary pathology in which the bony labyrinth of the inner ear is affected. It occurs more often in women after 45 years of age. But the first manifestations can appear at a young age. Without appropriate treatment, it often leads to the development of bilateral hearing loss. The disease can be suspected by the following symptoms:
- gradual hearing loss without cause;
- incomprehensible sound or noise in one or both ears;
- dizziness;
- improve hearing in noisy environments;
- balance disorders.
With such manifestations, you need to contact an otolaryngologist.
Earplug
A buildup of earwax that partially or completely blocks the ear canal. Frequent condition, which is accompanied by the following manifestations:
- sensation of a foreign object;
- ear congestion and hearing loss;
- coughing may occur;
- yawns;
- slight dizziness, as from motion sickness in transport.
Often, symptoms appear after water procedures. A clot of sulfur swells due to water ingress, and completely blocks the passage in the ear.
Tonsillitis
Tonsillitis is an inflammation of the lymphoid tissue in the palatine tonsils, provoked by pathogenic flora. Given the close location, dull, aching pain goes to the ear.
The disease has two forms - chronic and acute. For diagnosis, a number of studies are prescribed, including blood and urine tests.
Ear Injuries
Sudden changes in pressure (at great depths in water or air) cause injury to the eardrum. Also, damage is possible when exposed to loud sound vibrations. This condition is characterized by pain and bleeding. With mechanical damage to various objects, with bruises or blows, dizziness, severe ringing in the ears are noted. Temporary deafness is characteristic.
It is also possible to form various neoplasms in the ear. Usually, the tumor forms inside the auricle or near it.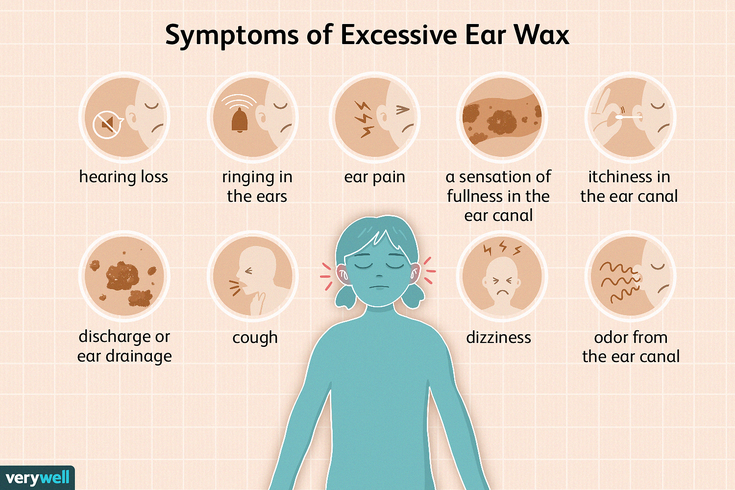 It rarely affects the middle section. They are characterized by slow growth and the absence of painful symptoms.
It rarely affects the middle section. They are characterized by slow growth and the absence of painful symptoms.
Which doctor to contact in case of ear pain
An otolaryngologist deals with diseases of the ENT organs. This is the first specialist you go to if characteristic symptoms appear.
ENT examines the anamnesis, prescribes tests and examinations:
- complete blood count;
- examination of secretions;
- fibroendoscopic examination of the mucosa;
- roentgen.
In some cases - a serious pathology, abscess, rapid development - the ENT sends an appointment to other specialists: a surgeon, an infectious disease specialist, an audiologist, a traumatologist.
Taking into account this or that diagnosis, it is possible to preliminarily name what tests the doctor will prescribe for ear pain:
- Tympanometry - a study of the mobility of the tympanic membrane.
- Audiometry – hearing test for suspected hearing loss.
- CT or MRI can detect purulent, intraosseous or intracranial complications - mastoiditis, purulent abscess, meningitis.
- Tympanocentesis - puncture of the eardrum with a needle for additional research. The same procedure is carried out to extract pus or accumulation of fluid in the cavity.
- In case of repeated suppuration, the procedure of myringotomy is performed - dissection of the tympanic membrane. This allows you to permanently relieve pain and save the patient from a purulent abscess.
Important! MRI provides more information than CT specifically on the localization of pus and fluid.
If the doctor sees a strong need, in some, especially advanced cases, an X-ray is prescribed.
Diagnosis and appointment with a doctor
If you have pain in your ear, or if your hearing begins to decrease for no apparent reason, you should definitely contact an otolaryngologist. Depending on the symptoms, you may need to consult an audiologist - a doctor who deals with hearing disorders.
Diagnostic methods
Complaints of the patient, as well as the study of family history, play an important role in making a diagnosis. The doctor performs an external examination of the auricle. If this is not enough to determine the disease, then resort to hardware methods.
- Otoscopy is a painless method of examining the outer ear using an otoscope. This is an instrument that looks like a tube with a light. Helps to identify hidden infections, injuries, and to detect a foreign body
- Tympanometry - an acoustic method for studying the functionality of the auditory tube and the mobility of the ossicles in the middle ear
- Audiometry - a test for the study of hearing acuity. Carried out by an audiologist on computer
- X-ray of the ear and temporal bone - recommended for inflammatory pathologies. Helps to identify pathological changes in the parts of the inner ear
- ultrasound
- Computed tomography
Bacterial culture is performed for discharge and suspected bacterial infection.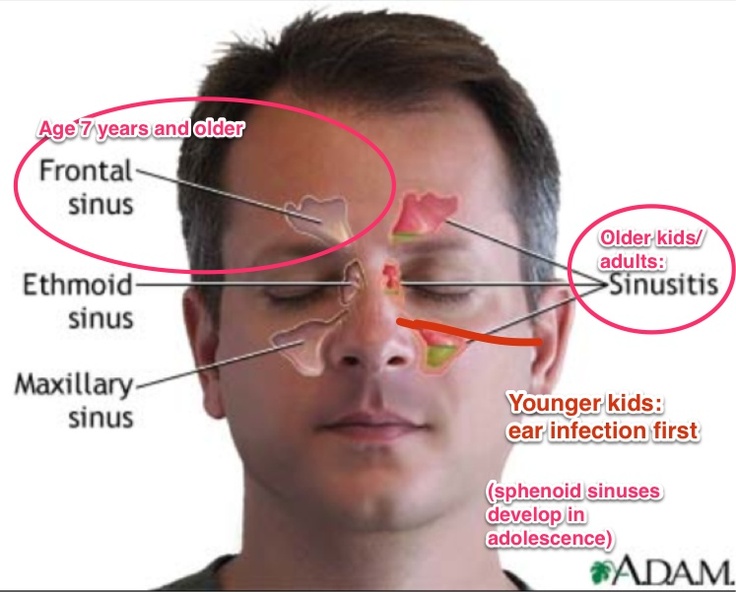 It detects the sensitivity of bacteria to antibiotics, which allows you to choose the best therapy. In chronic ear infections, a complete blood count is prescribed.
It detects the sensitivity of bacteria to antibiotics, which allows you to choose the best therapy. In chronic ear infections, a complete blood count is prescribed.
Preparations for the treatment of ear diseases
Therapy is carried out in a complex manner, provoking factors, the degree of development of pathological processes and the patient's condition are taken into account. It is important not only to drink medicine, but also to avoid stressful situations, follow the rules of hygiene, eat right, drink vitamins to maintain immunity.
Antibacterials
Ear problems in adults (symptoms and treatment to be considered individually by a doctor) help to eliminate antibiotics. They kill and prevent the reproduction of pathogenic microflora. Broad-spectrum drugs are selected.
| Name | Application | Contraindications |
| Amoxiclav. | Tablets are taken before meals.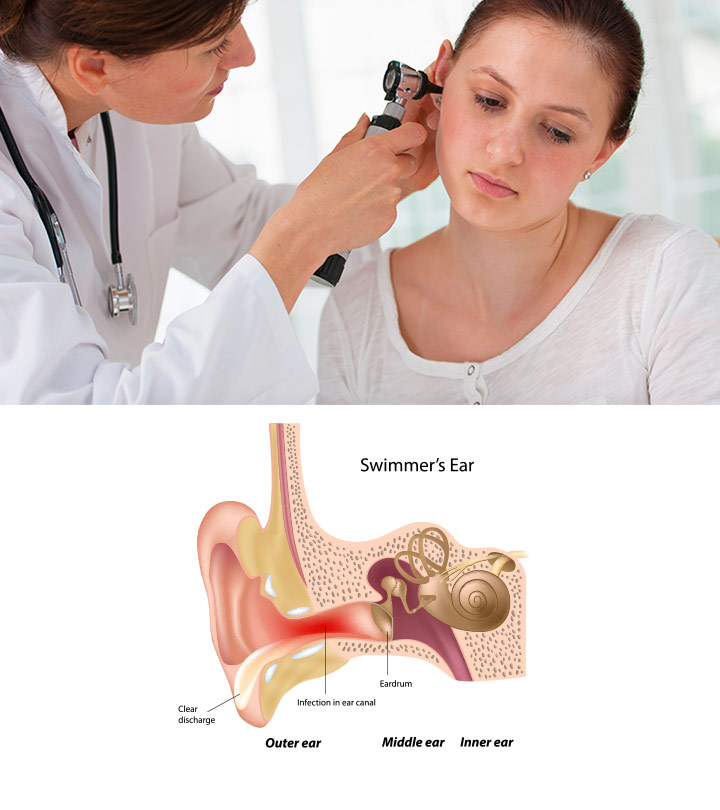 The course of treatment lasts 5-14 days. Patients are prescribed 250-500 mg every 8 hours. The course of treatment lasts 5-14 days. Patients are prescribed 250-500 mg every 8 hours. |
|
| Cephalexin. | The drug is prescribed at 250-500 mg every 6-12 hours. The duration of treatment is 1-2 weeks. |
|
Antibacterial agents in the form of ointments, drops are used to treat mild diseases or boils. Some drugs contain hormonal components that suppress the development of the inflammatory process.
Ear drops
Taking into account the pathology, stage, general condition of the patient and the main diagnosis, the doctor prescribes antibacterial, analgesic and / or anti-inflammatory drops.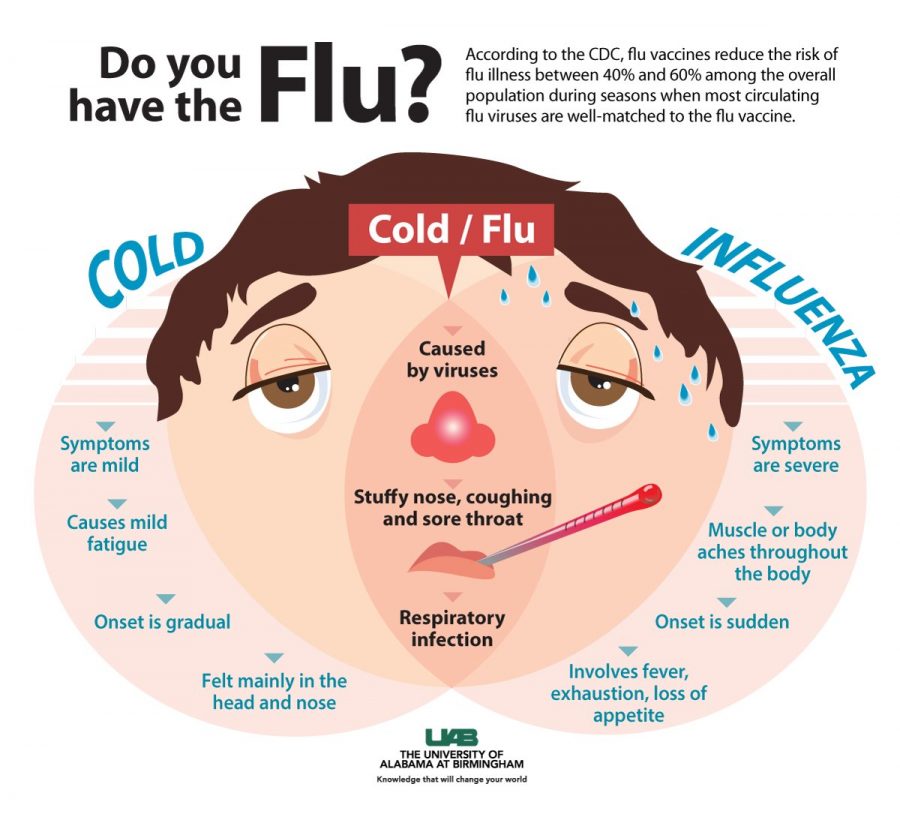
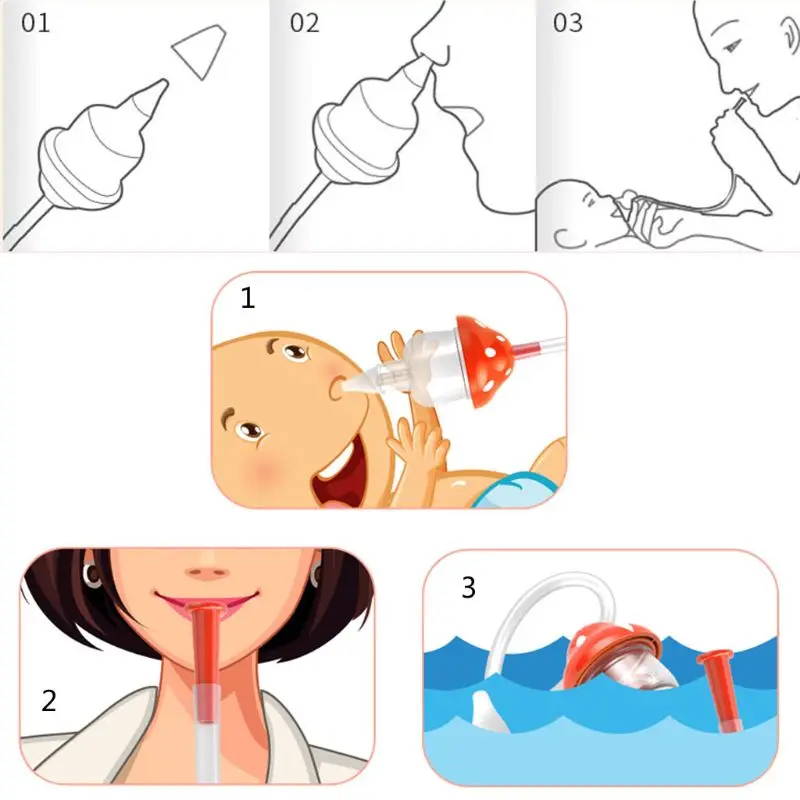
Before instillation, be sure to clean the ear canal with hydrogen peroxide, wipe it dry, and only then inject the drug.
The following types of drops by groups are popular:
- antibacterial - Anauran, Tsipromed, Candibiotic;
- hormonal - Sofradex, Polydex with phenylephrine;
- bactericidal - Otofa, Normaks;
- painkillers - Ototon, Phenazone, they are also used for local anesthesia to relieve ear pain in an adult.
Before treating a sore ear with drops, they must be warmed in the palm of your hand. During the procedure, the lobe is pulled down and back, and after the drops have got inside, they lightly press on the tragus. Be sure to lie down on each side for 5-10 minutes so that the medicine gets inside.
Important! Children under one year old are usually not prescribed ear drops. If the child's ears hurt, Nazivin is usually recommended nasally.
Antihistamines
Drugs reduce the development of allergic processes. They are more used as symptomatic therapy, since the underlying cause of the disease is not affected.
They are more used as symptomatic therapy, since the underlying cause of the disease is not affected.
See also: Sensorineural hearing loss: Symptoms, causes, treatment and ICD-10 code
| Title | Application | Contraindications |
| "Suprastin". | The usual dosage is 75-100 mg 3-4 r. per day. |
|
| Tavegil. | The daily dosage is a maximum of 6 tab. Standard reception provides 1 tab. 2 p. in a day. |
|
Medicines restore the patency of the auditory tube, also relieve swelling of the mucous membrane and itching that accompanies many pathologies.
Painkillers and antiseptic ointments
Antiseptics help avoid infection and reduce inflammation. The following remedies are able to relieve pain:
- Sofradex - a drug with antibacterial and anti-inflammatory action for local use;
- Levomekol - accelerates tissue regeneration, activates the synthesis of interferon, disinfects the internal cavity;
- Tetracycline is a broad-spectrum antibiotic prescribed for otitis media and otitis externa.
The ointment is applied with cotton swabs and compresses. The drugs are contraindicated in case of rupture of the eardrum, inflammation of the middle ear and allergies.
Non-steroidal anti-inflammatory drugs
Medicines reduce pain and inflammation, eliminate high fever.
| Name | Application | Contraindications |
| Ibuprofen. | 20-30 mg/kg every 6 hours |
|
| Paracetamol. | The standard dosage is 500-1000 mg, the time interval between doses is 4-6 hours. |
|
Ear diseases in adults, the symptoms and treatment of which are determined by an otolaryngologist, cause discomfort to a person and disrupt his usual way of life. Non-steroidal anti-inflammatory drugs relieve the condition. Ear drops with anesthetic ("Otipax") have a positive effect. They have an anesthetic effect.
Glucocorticosteroid anti-inflammatory drugs
The preparations eliminate the cause of the inflammatory process and also have an anti-allergic effect.
| Name | Application | Contraindications |
| Dexamethasone. | 3 caps. in each ear 3 p. per day. Treatment is carried out 2-14 days. in each ear 3 p. per day. Treatment is carried out 2-14 days. |
|
| Prednisone. | 4-5 caps. 3-4 p. in a day. |
|
During therapy, the otolaryngologist recommends adherence to strict hygiene without fail in order to speed up the healing process. To wash the ear canal, special antiseptics are used.
Recipes for folk remedies for the treatment of ears
Non-traditional methods are used only for mild forms of ear disease and after consultation with a doctor. The components used can provoke side effects or aggravate a person's condition.
| Name | Recipe | Application and effectiveness |
Ammonium chloride and camphor. | Dissolve salt (1tbsp) in warm water (1L). Mix camphor oil (10 g) and ammonia 100% (100 g). Combine all ingredients, stirring until white flakes disappear. | Soak a cotton swab in the resulting solution, wring it out well and apply it to the ear for a short time. The medicine reduces inflammation and pain. |
| Garlic oil. | Grind garlic, 150 mg pour vegetable oil (60 mg). Leave in refrigerator for 10 days. | The resulting solution is placed in the ear canal on a small piece of cotton wool. Treatment is carried out 14-16 days for 3 r. per day. |
| Lemon juice. | Extract juice, strain and use as directed. | Drip 2-3 r. per day for 3-4 drops. for 5 days |
Propolis tincture has a regenerating and antimicrobial effect. A moistened cotton swab is placed in the external auditory meatus. It should be changed 2-3 r. per day.
Traditional medicine
Traditional medicine methods are recommended to be used in combination . The recipes listed below help to increase blood circulation in the affected area of the body, which allows effective treatment.
The recipes listed below help to increase blood circulation in the affected area of the body, which allows effective treatment.
In addition, non-traditional medicine significantly reduces pain and improves the tone of the whole organism.
Before performing the procedures presented, you should consult with your doctor.
Dry heat is considered one of the most effective methods of treatment.
You will need salt to make it at home.
Heat it in a frying pan to a temperature of sixty degrees Celsius.
As a result, the salt should acquire a yellowish tint . Then pour the resulting mixture into a cotton bag.
If the compress is scalding, leave the pouch on the windowsill for a few minutes. Make sure the salt doesn't get cold. Warmth, when touching the affected area, should be pleasant, but not hot.
Keep lotion near ear for thirty minutes. Then wrap your head in a tight bandage.
You will notice the result after the first application.
Complications caused by diseases of the ears
Lack of correct and timely therapy leads to serious consequences. It is important to see a doctor, undergo an examination and start treatment in order to prevent complications:
| Name | Description |
| Labyrinth (otitis media). | The cause is an infection after otitis media that has spread to the inner ear. It also provokes a gradual deterioration in hearing to complete deafness. |
| Meningitis. | Complication after mastoiditis. The purulent contents enter the membrane of the brain. |
| Encephalitis. | Inflammation affecting the meninges caused by pathogens. |
| Abscess. | Microbes penetrate into the region of the temporal bone under the membrane of the brain or into its cells.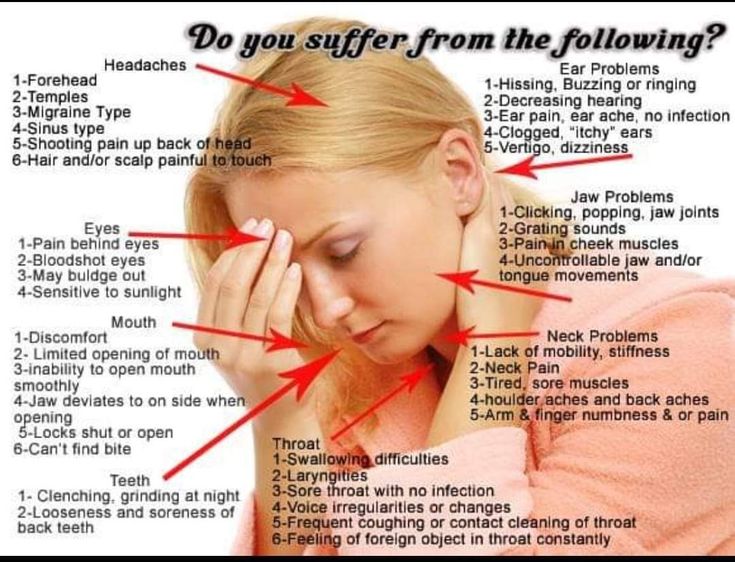 The body temperature rises, the patient's condition worsens. There is lethargy, severe headache and vomiting. The body temperature rises, the patient's condition worsens. There is lethargy, severe headache and vomiting. |
Ear diseases in adults are not dangerous if you go to the hospital in time. Considering the symptoms, the doctor determines the source of the development of pathological processes. He will select the treatment after the diagnosis and will monitor the condition until complete recovery.
Conclusion
Ear diseases are particularly painful. Therefore, it is important to consult an ENT doctor at the first symptoms. Children are particularly susceptible to ear infections.
Therefore, in order to prevent diseases, it is necessary to follow simple rules. First of all, take care of the hygiene of the organ of hearing. Remember to wash your ears daily and clean them once a week. Try not to use cotton swabs, as there is a high risk of sulfur plugs.
In addition, strengthen the body's immune system. Watch your diet and use more vitamins.