How to help your child with depression and anxiety
SAMHSA’s National Helpline | SAMHSA
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Main page content
-
SAMHSA’s National Helpline is a free, confidential, 24/7, 365-day-a-year treatment referral and information service (in English and Spanish) for individuals and families facing mental and/or substance use disorders.
Also visit the online treatment locator.
SAMHSA’s National Helpline, 1-800-662-HELP (4357) (also known as the Treatment Referral Routing Service), or TTY: 1-800-487-4889 is a confidential, free, 24-hour-a-day, 365-day-a-year, information service, in English and Spanish, for individuals and family members facing mental and/or substance use disorders. This service provides referrals to local treatment facilities, support groups, and community-based organizations.
Also visit the online treatment locator, or send your zip code via text message: 435748 (HELP4U) to find help near you. Read more about the HELP4U text messaging service.
The service is open 24/7, 365 days a year.
English and Spanish are available if you select the option to speak with a national representative. Currently, the 435748 (HELP4U) text messaging service is only available in English.
In 2020, the Helpline received 833,598 calls. This is a 27 percent increase from 2019, when the Helpline received a total of 656,953 calls for the year.
The referral service is free of charge. If you have no insurance or are underinsured, we will refer you to your state office, which is responsible for state-funded treatment programs. In addition, we can often refer you to facilities that charge on a sliding fee scale or accept Medicare or Medicaid. If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
The service is confidential. We will not ask you for any personal information. We may ask for your zip code or other pertinent geographic information in order to track calls being routed to other offices or to accurately identify the local resources appropriate to your needs.
No, we do not provide counseling. Trained information specialists answer calls, transfer callers to state services or other appropriate intake centers in their states, and connect them with local assistance and support.
-
Suggested Resources
What Is Substance Abuse Treatment? A Booklet for Families
Created for family members of people with alcohol abuse or drug abuse problems. Answers questions about substance abuse, its symptoms, different types of treatment, and recovery. Addresses concerns of children of parents with substance use/abuse problems.
Addresses concerns of children of parents with substance use/abuse problems.It's Not Your Fault (NACoA) (PDF | 12 KB)
Assures teens with parents who abuse alcohol or drugs that, "It's not your fault!" and that they are not alone. Encourages teens to seek emotional support from other adults, school counselors, and youth support groups such as Alateen, and provides a resource list.After an Attempt: A Guide for Taking Care of Your Family Member After Treatment in the Emergency Department
Aids family members in coping with the aftermath of a relative's suicide attempt. Describes the emergency department treatment process, lists questions to ask about follow-up treatment, and describes how to reduce risk and ensure safety at home.Family Therapy Can Help: For People in Recovery From Mental Illness or Addiction
Explores the role of family therapy in recovery from mental illness or substance abuse. Explains how family therapy sessions are run and who conducts them, describes a typical session, and provides information on its effectiveness in recovery.
For additional resources, please visit the SAMHSA Store.
Last Updated: 08/30/2022
Alcohol, Tobacco, and Other Drugs
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Misusing alcohol, tobacco, and other drugs can have both immediate and long-term health effects.The misuse and abuse of alcohol, tobacco, illicit drugs, and prescription medications affect the health and well-being of millions of Americans. SAMHSA’s 2020 National Survey on Drug Use and Health reports that approximately 19.3 million people aged 18 or older had a substance use disorder in the past year.
Alcohol
Data:
- In 2020, 50.0% of people aged 12 or older (or 138.5 million people) used alcohol in the past month (i.e., current alcohol users) (2020 NSDUH)
- Among the 138.5 million people who were current alcohol users, 61.
 6 million people (or 44.4%) were classified as binge drinkers and 17.7 million people (28.8% of current binge drinkers and 12.8% of current alcohol users) were classified as heavy drinkers (2020 NSDUH)
6 million people (or 44.4%) were classified as binge drinkers and 17.7 million people (28.8% of current binge drinkers and 12.8% of current alcohol users) were classified as heavy drinkers (2020 NSDUH) - The percentage of people who were past month binge alcohol users was highest among young adults aged 18 to 25 (31.4%) compared with 22.9% of adults aged 26 or older and 4.1% of adolescents aged 12 to 17 (2020 NSDUH)
- The 2019 National Survey on Drug Use and Health reports that 139.7 million Americans age 12 or older were past month alcohol users, 65.8 million people were binge drinkers in the past month, and 16 million were heavy drinkers in the past month
- About 2.3 million adolescents aged 12 to 17 in 2019 drank alcohol in the past month, and 1.2 million of these adolescents binge drank in that period (2019 NSDUH)
- Approximately 14.5 million people age 12 or older had an alcohol use disorder (2019 NSDUH)
- Excessive alcohol use can increase a person’s risk of stroke, liver cirrhosis, alcoholic hepatitis, cancer, and other serious health conditions
- Excessive alcohol use can also lead to risk-taking behavior, including driving while impaired.
 The Centers for Disease Control and Prevention reports that 29 people in the United States die in motor vehicle crashes that involve an alcohol-impaired driver daily
The Centers for Disease Control and Prevention reports that 29 people in the United States die in motor vehicle crashes that involve an alcohol-impaired driver daily
Programs/Initiatives:
- STOP Underage Drinking interagency portal - Interagency Coordinating Committee on the Prevention of Underage Drinking
- Interagency Coordinating Committee on the Prevention of Underage Drinking
- Talk. They Hear You.
- Underage Drinking: Myths vs. Facts
- Talking with your College-Bound Young Adult About Alcohol
Relevant links:
- National Association of State Alcohol and Drug Abuse Directors
- Department of Transportation Office of Drug & Alcohol Policy & Compliance
- Alcohol Policy Information Systems Database (APIS)
- National Institute on Alcohol Abuse and Alcoholism
Tobacco
Data:
- In 2020, 20.7% of people aged 12 or older (or 57.
 3 million people) used nicotine products (i.e., used tobacco products or vaped nicotine) in the past month (2020 NSDUH)
3 million people) used nicotine products (i.e., used tobacco products or vaped nicotine) in the past month (2020 NSDUH) - Among past month users of nicotine products, nearly two thirds of adolescents aged 12 to 17 (63.1%) vaped nicotine but did not use tobacco products. In contrast, 88.9% of past month nicotine product users aged 26 or older used only tobacco products (2020 NSDUH)
- Data from the 2019 NSDUH reports that 58.1 million people were current (i.e., past month) tobacco users. Specifically, 45.9 million people aged 12 or older in 2019 were past month cigarette smokers (2019 NSDUH)
- Tobacco use is the leading cause of preventable death, often leading to lung cancer, respiratory disorders, heart disease, stroke, and other serious illnesses. The CDC reports that cigarette smoking causes more than 480,000 deaths each year in the United States
- The CDC’s Office on Smoking and Health reports that more than 16 million Americans are living with a disease caused by smoking cigarettes
Electronic cigarette (e-cigarette) use data:
- Data from the Centers for Disease Control and Prevention’s 2020 National Youth Tobacco Survey.
 Among both middle and high school students, current use of e-cigarettes declined from 2019 to 2020, reversing previous trends and returning current e-cigarette use to levels similar to those observed in 2018
Among both middle and high school students, current use of e-cigarettes declined from 2019 to 2020, reversing previous trends and returning current e-cigarette use to levels similar to those observed in 2018 - E-cigarettes are not safe for youth, young adults, or pregnant women, especially because they contain nicotine and other chemicals
Resources:
- Tips for Teens: Tobacco
- Tips for Teens: E-cigarettes
- Implementing Tobacco Cessation Programs in Substance Use Disorder Treatment Settings
- Synar Amendment Program
Links:
- Truth Initiative
- FDA Center for Tobacco Products
- CDC Office on Smoking and Health
- National Institute on Drug Abuse: Tobacco, Nicotine, and E-Cigarettes
- National Institute on Drug Abuse: E-Cigarettes
Opioids
Data:
- Among people aged 12 or older in 2020, 3.4% (or 9.5 million people) misused opioids in the past year.
 Among the 9.5 million people who misused opioids in the past year, 9.3 million people misused prescription pain relievers and 902,000 people used heroin (2020 NSDUH)
Among the 9.5 million people who misused opioids in the past year, 9.3 million people misused prescription pain relievers and 902,000 people used heroin (2020 NSDUH) - An estimated 745,000 people had used heroin in the past year, based on 2019 NSDUH data
- In 2019, there were 10.1 million people age 12 or older who misused opioids in the past year. The vast majority of people misused prescription pain relievers (2019 NSDUH)
- An estimated 1.6 million people aged 12 or older had an opioid use disorder based on 2019 NSDUH data
- Opioid use, specifically injection drug use, is a risk factor for contracting HIV, Hepatitis B, and Hepatitis C. The CDC reports that people who inject drugs accounted for 9 percent of HIV diagnoses in the United States in 2016
- According to the Centers for Disease Control and Prevention’s Understanding the Epidemic, an average of 128 Americans die every day from an opioid overdose
Resources:
- Medication-Assisted Treatment
- Opioid Overdose Prevention Toolkit
- TIP 63: Medications for Opioid Use Disorder
- Use of Medication-Assisted Treatment for Opioid Use Disorder in Criminal Justice Settings
- Opioid Use Disorder and Pregnancy
- Clinical Guidance for Treating Pregnant and Parenting Women With Opioid Use Disorder and Their Infants
- The Facts about Buprenorphine for Treatment of Opioid Addiction
- Pregnancy Planning for Women Being Treated for Opioid Use Disorder
- Tips for Teens: Opioids
- Rural Opioid Technical Assistance Grants
- Tribal Opioid Response Grants
- Provider’s Clinical Support System - Medication Assisted Treatment Grant Program
Links:
- National Institute on Drug Abuse: Opioids
- National Institute on Drug Abuse: Heroin
- HHS Prevent Opioid Abuse
- Community Anti-Drug Coalitions of America
- Addiction Technology Transfer Center (ATTC) Network
- Prevention Technology Transfer Center (PTTC) Network
Marijuana
Data:
- The percentage of people who used marijuana in the past year was highest among young adults aged 18 to 25 (34.
 5%) compared with 16.3% of adults aged 26 or older and 10.1% of adolescents aged 12 to 17 (2020 NSDUH)
5%) compared with 16.3% of adults aged 26 or older and 10.1% of adolescents aged 12 to 17 (2020 NSDUH) - 2019 NSDUH data indicates that 48.2 million Americans aged 12 or older, 17.5 percent of the population, used marijuana in the past year
- Approximately 4.8 million people aged 12 or older in 2019 had a marijuana use disorder in the past year (2019 NSDUH)
- Marijuana can impair judgment and distort perception in the short term and can lead to memory impairment in the long term
- Marijuana can have significant health effects on youth and pregnant women.
Resources:
- Know the Risks of Marijuana
- Marijuana and Pregnancy
- Tips for Teens: Marijuana
Relevant links:
- National Institute on Drug Abuse: Marijuana
- Addiction Technology Transfer Centers on Marijuana
- CDC Marijuana and Public Health
Emerging Trends in Substance Misuse:
- Methamphetamine—In 2019, NSDUH data show that approximately 2 million people used methamphetamine in the past year.
 Approximately 1 million people had a methamphetamine use disorder, which was higher than the percentage in 2016, but similar to the percentages in 2015 and 2018. The National Institute on Drug Abuse Data shows that overdose death rates involving methamphetamine have quadrupled from 2011 to 2017. Frequent meth use is associated with mood disturbances, hallucinations, and paranoia.
Approximately 1 million people had a methamphetamine use disorder, which was higher than the percentage in 2016, but similar to the percentages in 2015 and 2018. The National Institute on Drug Abuse Data shows that overdose death rates involving methamphetamine have quadrupled from 2011 to 2017. Frequent meth use is associated with mood disturbances, hallucinations, and paranoia. - Cocaine—In 2019, NSDUH data show an estimated 5.5 million people aged 12 or older were past users of cocaine, including about 778,000 users of crack. The CDC reports that overdose deaths involving have increased by one-third from 2016 to 2017. In the short term, cocaine use can result in increased blood pressure, restlessness, and irritability. In the long term, severe medical complications of cocaine use include heart attacks, seizures, and abdominal pain.
- Kratom—In 2019, NSDUH data show that about 825,000 people had used Kratom in the past month. Kratom is a tropical plant that grows naturally in Southeast Asia with leaves that can have psychotropic effects by affecting opioid brain receptors.
 It is currently unregulated and has risk of abuse and dependence. The National Institute on Drug Abuse reports that health effects of Kratom can include nausea, itching, seizures, and hallucinations.
It is currently unregulated and has risk of abuse and dependence. The National Institute on Drug Abuse reports that health effects of Kratom can include nausea, itching, seizures, and hallucinations.
Resources:
- Tips for Teens: Methamphetamine
- Tips for Teens: Cocaine
- National Institute on Drug Abuse
More SAMHSA publications on substance use prevention and treatment.
Last Updated: 04/27/2022
A teenager in depression: psychologist's advice on how to avoid trouble
Parents of teenagers often pay attention to the fact that their children suddenly change: until recently, a cheerful child loses interest in studies, friends, and life in general. He is not happy with everything. The son or daughter looks tired, refuses to eat. Lose weight or, conversely, gain weight. Many tend to attribute this to a transitional age, but it is important not to miss the onset of depression. How to recognize it and sound the alarm in time, says Elena Sizikova, a psychologist at the Kutuzovsky family center.
How to recognize it and sound the alarm in time, says Elena Sizikova, a psychologist at the Kutuzovsky family center.
— What symptoms should alert parents?
- Sleep disturbance - insomnia or drowsiness. The child may complain of difficulty concentrating. Experience feelings of worthlessness and guilt (often unfounded). Sometimes depression in children manifests itself in behavior - hyperactivity, enuresis, school failure. The teenager is restless, obnoxious, denies everything. It comes to antisocial or aggressive behavior. May become sullen, avoid family contact. Or vice versa - to seem too emotional, sensitive, especially with peers. He does not care about his appearance, his performance at school.
— Why is this condition dangerous?
- It is often accompanied by obsessive thoughts about death, suicidal intentions or attempts. A teenager in this state can start using alcohol and drugs. Depression in a teenager should not be underestimated: it can lead to serious, dangerous, even irreparable consequences.
- How to prevent this? What to do if symptoms of depression appear?
- If you know or suspect that your child is thinking about death or is a member of destructive groups in social networks, then you should urgently seek help from a psychologist. For example, to one of the family centers in Moscow. It's hard to do it on your own.
If we are talking about the prevention of teenage depression, then it is important to understand that adolescence is a very difficult, conflicting age. It is impossible to avoid conflict situations. Yes, and you don't need to. The most important thing is to try to create such a psychological climate in the family so that the teenager feels supported, knows that he is heard and considered.
- It's easy to say, but how can parents create such an atmosphere?
- There are several methods: active emotional support for a child in a state of depression and encouragement of his positive aspirations. This will help ease the situation.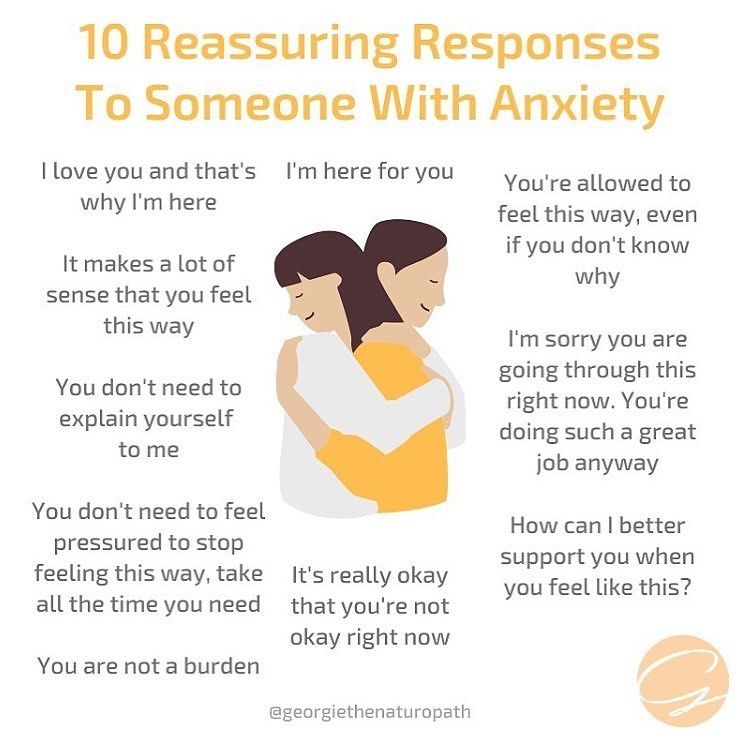 It is possible and necessary to teach a teenager to socialize and overcome stress - psychologists will also help here. Another method is to expand the time perspective and self-understanding.
It is possible and necessary to teach a teenager to socialize and overcome stress - psychologists will also help here. Another method is to expand the time perspective and self-understanding.
- You said that conflicts should not be avoided, and a positive atmosphere cannot be created in a short time. How to behave when conflict is inevitable?
- Clearly express your fears and concerns to the teenager so that he can understand them. Bring a teenager to a frank conversation to find out what is happening to him. He must know that he will be listened to without criticism and condemnation. An adult needs to show his willingness to listen and understand, which does not mean forgiveness at all. It simply creates a solid foundation on which to build further relationships. A teenager needs his parents to listen to him, but not give advice until he himself asks them about it. It is difficult to come to terms with this, but parents need to accept and understand: a teenager does not have to follow the advice of elders at all. He makes his choice.
He makes his choice.
Only with this approach is it possible to have a meaningful dialogue between two equal people - an adult and a teenager. Only on such a basis can constructive communication and behavior be built.
HOW TO TALK TO YOUR TEEN
| If you hear | Be sure to say | Never say |
| "I hate studying, class..." | "What's going on with us that makes you feel this way?" | "When I was your age... you're just lazy!" |
| "Everything seems so hopeless..." | “Sometimes we all feel overwhelmed. Let's think about what problems we have and which one needs to be solved first" | "Better think of those who are worse off than you" |
| "Everyone would be better off without me!" | “You mean a lot to us, and your mood worries me. | "Don't talk nonsense. Let's talk about something else" |
| "You don't understand me!" | “Tell me how you feel. I really want to know this" | "Who can understand the youth of our day?" |
| "I have done a terrible thing..." | "Let's sit down and talk about it" | "What you sow, so shall you reap!" |
| "What if I don't succeed?" | "If it doesn't work, I'll know you did your best" | "If you don't succeed, it means you didn't try hard enough!" |
Source
How to identify anxiety and depression in a child
Scientists have developed a task that helps identify children with anxiety and depression, writes sciencenews.org with link to PLOS One.
The task of scientists was to introduce children into a situation of uncertainty. Adults took turns taking children aged 3 to 7 to a dimly lit room with a mysterious covered heap. To create a sense of expectation, adults said: “I have something here that I can show you" or "Let's be be silent so that it does not wake up. Then the adult opened hidden pile, which turned out to be a terrarium, and pulled out realistic looking plastic snake.
Each child wore a small motion sensor attached to belt. These sensors recorded the movements of the child, for example, when they started to move quickly or turned, at a speed 100 times per second. The researchers wanted to find out if the movements during a fearful situation in children diagnosed with depression or anxiety and children without such a diagnosis. It turned out that they differ. Diagnosed children are more likely to turn away from perceived threat - a hidden terrarium than those without illness.
In fact, sensors can identify depression and anxiety disorder in very young children in about 80% of cases. Such a tool can be useful because, despite widespread recognition that children as young as, for example, 3 years may suffer from mental disorders, the diagnosis of these disease remains challenging. Such children often do not show there are no outward signs, because they keep their emotions inside.
However, it is becoming increasingly clear that these children are at increased risk of developing mental health problems and physical health later in life, says Lisabeth DiLalla is a developmental psychologist at the University School of Medicine Southern Illinois at Carbondale. Scientists have wondered if whether to change it.
According to Joan Luby, a psychiatrist at the Medical School Washington University in St. Louis, it's possible. Luby's study found that treating preschoolers with depression helps children feel joy again, at least in short term. "When you identify small children as in need of help, says Louby, you can cure them more efficiently.
"When you identify small children as in need of help, says Louby, you can cure them more efficiently.
Depression from childhood
Until 1980, few experts believed that young children able to experience depression or anxiety while researchers did not find that children aged 7 years can actually get depressed. K 19the 90s became it is clear that depression and anxiety can start in children as young as 3 years. But for many children, the symptoms of depression manifest themselves as they may seem not very obvious: they can become aggressive, hyperactive, or have difficulty with maneuvers food. As a result, these so-called "internalizing disorders" are more likely to remain undiagnosed at a young age.
Although estimates vary widely, it is believed that between 10 and 20 percent of preschool and childhood children suffer anxiety disorder and about 2 percent depression, and some even express suicidal feelings. real levels, probably higher. Because children under the age of 8 cannot articulate their own feelings, physicians must rely how the teacher evaluates the behavior of the child. But children with anxiety or depression are often so quiet and unobtrusive that educators and teachers do not notice their difficulties.
real levels, probably higher. Because children under the age of 8 cannot articulate their own feelings, physicians must rely how the teacher evaluates the behavior of the child. But children with anxiety or depression are often so quiet and unobtrusive that educators and teachers do not notice their difficulties.
These kids are "not squeaky wheels," Ellen McGinnis describes - clinical psychologist at the University of Vermont Medical Center in Burlington.
She and other scientists focused their research on finding objective ways to identify children with disorders. it research can be laborious and lengthy. Being graduate student, McGinnis videotaped the behavior of children during time of experiments with a snake or other similar tasks on detection of anxiety. Several researchers then looked these videos to gauge children's reactions. McGinnis took two years to evaluate 10 children.
She then teamed up with her husband, a biomedical engineer UVM by Ryan McGinnis to find a more efficient way identify children with depression or anxiety. Result: connection classic anxiety test with a commercially available motion sensor.
Result: connection classic anxiety test with a commercially available motion sensor.
According to Ellen McGinnis, of the 63 children recruited for the test, 21 were diagnosed with anxiety or depression after 90 minute conversation between a qualified doctor and a person providing care and education.
In the snake test, the researchers found that the most expressive moments detected by the sensors were obtained after about 20 seconds of waiting prior to opening. Faced with a closed terrarium, children with anxiety or depression turned their body 180 degrees from the terrible object. “Children who have been diagnosed with anxiety are more likely to turned away from this potentially threatening situation than children who were not then diagnosed,” says Ryan McGinnis.
He was surprised that at the moment the plastic snake appeared, the sensors found no difference between diagnosed and undiagnosed children him. “I was surprised how many children were very excited to see snake,” says Ryan McGinnis.
The researchers were able to use the sensor data to correctly analyze 14 out of 21 children. The false positive rate was low: sensors classified only five children with no clinical diagnosis as having depression or anxiety.
Researchers say it's not the gold standard, but still better than the widely used questionnaire in which parents report their child's problems. On the checklist only eight out of 21 children's behaviors are correctly identified child with a diagnosis.
Since the task was simple and the sensor technology readily available (unit price is less than $4 and the components needed to measure body motion are already present in most mobile phones), Ryan McGinnis believes that combining technology with behavioral tasks has great potential. "You can really use something similar for universal screening,” he says.
Depression test
Sarah Bufferd is a clinical psychologist at the State University California in San Marcos - expressed a desire to check if they work whether the sensors are on the children in a similar way during the task, which increases feelings of sadness, helplessness, or frustration.
Many researchers working on the early detection of children with mental health problems, also monitor these children in for many years. So they can see if they carry over such early mental health problems at later life. In 2014, Bufferd and her team showed that children with signs of depression at age 3 more prone to depression in three years. Related studies of older children age showed a similar continuity.
A new study now shows that very young children with mental health problems may also be prone to more physical problems health in adolescence. Children with higher levels internalization at age 5 about 30 percent more likely suffer from health problems such as poor sleep, headaches pain and abdominal pain in the next 12 years (with differences for sex and temperament). Those who had higher rates of internalization, also 30 percent more likely to mindlessly ate during adolescence. Mental health in age 5 years affects physical health later in life.
Early treatment
With evidence emerging that mental health problems health in preschool institutions develop into adulthood, researchers began to explore the possibility of treating the smallest. The work in the Luby laboratory is indicative, which is almost deals exclusively with preschool depression.
In 2016, Luby showed that there are fewer children with depression responded to the reward than their non-depressed peers. Her team connected 78 children aged 4 to 7 to electroencephalogram (EEG) - a non-invasive machine that measures electrical activity in the brain. fifty three children were diagnosed with depression using a test.
The test consisted of the children playing a guessing game on the computer. Children who gave more correct answers scored more points and, ultimately, received the best prizes. The EEG showed that even after the correct answer, children with depression showed less brain activity than their healthy peers - a sign that their reactions to the reward were muted. Similar suppressed responses to rewards have been linked to depression in adolescents and adults.
Similar suppressed responses to rewards have been linked to depression in adolescents and adults.
Meanwhile, Luby also studied children receiving modified a form of conventional psychotherapy known as therapy parent-child interactions, or PCIT. Psychotherapist trains caregivers to help them cope with destructive behavior and tantrums. The therapist is watching parent and child through a one-way mirror and communicate with adults through an in-ear microphone. Similarly, in Luby's study preschoolers and their caregivers followed the PCIT setting, but with emphasis to reduce the feelings of guilt and shame that usually accompany depression.
Luby found that children who received treatment had more lower depression scores and less severe depression than children placed in the waiting group. In addition, children who received a modified form of PCIT began to demonstrate the same response to reward as non-depressed children. “The treatment changed the response to the reward,” Luby says.
 Tell me what's going on"
Tell me what's going on"