When can you get the epidural
9 myths about epidurals – debunked | Your Pregnancy Matters
MedBlog
Your Pregnancy Matters
March 23, 2021
Your Pregnancy Matters
Megan Maxwell, M.D. Anesthesiology and Pain Management
Epidurals are among the safest, most effective options for labor pain management.Epidurals are one of the safest, most effective, and most widely used forms of pain management for women in labor around the world. More than 60 percent of laboring patients choose to get an epidural, according to the American Society of Anesthesiologists.
Research has shown that getting an epidural is safe and effective for nearly all laboring moms and their babies. But nevertheless, myths persist.
Choosing a labor pain relief method is a personal decision. You deserve the facts to make an educated choice. So, we've put together a list of the nine most common myths about labor pain epidurals, based on questions that patients have asked my colleagues and me. Let's get to debunking!
Myth: There's a limited window to get an epidural in laborReality: There's no specific cervical dilation range to wait for to get an epidural.We can place your epidural at the beginning, middle, or even toward the end of labor – we have safely placed epidurals in women who were dilated to 10cm. UT Southwestern has anesthesiologists on staff 24/7 to provide an epidural as soon as you want it.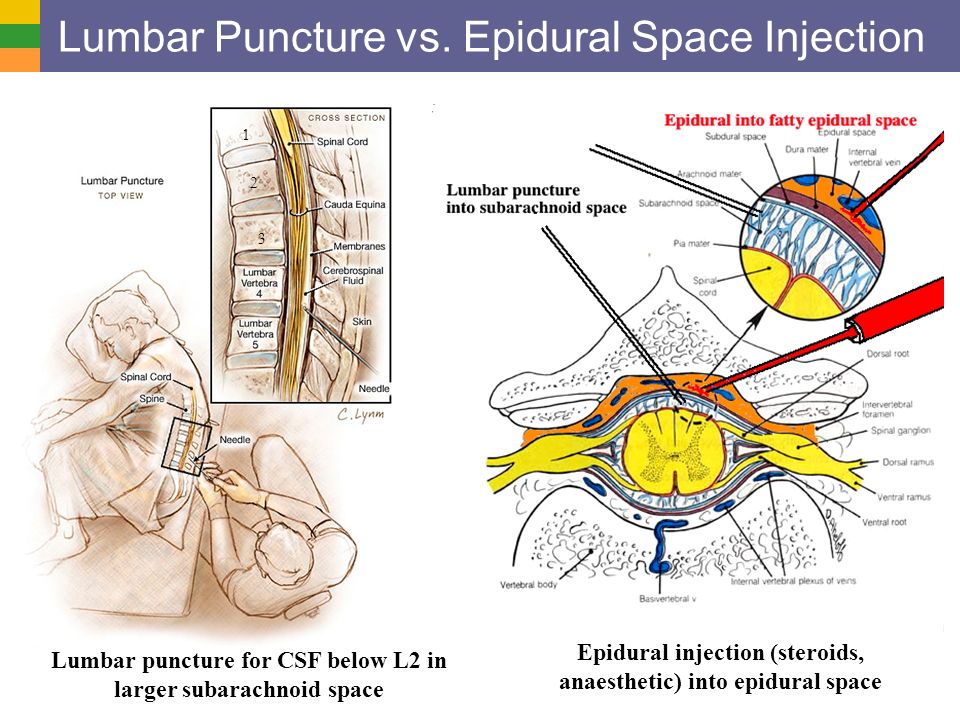 The only timing criteria are that you:
The only timing criteria are that you:
- Are in active or induced labor, which your Ob/Gyn or midwife will confirm.
- Can remain still and calm for five to 10 minutes for the procedure, which might be tough if you're close to delivering.
Once in a while, patients are within minutes of delivering when they get to the hospital. In those cases, there simply may not be time to give the epidural. This is uncommon but tends to happen more frequently in women who've given birth before.
Related reading: What to do when the baby’s coming – right now
Myth: Any laboring mom is eligible for an epidural.Reality: Nearly every patient is eligible, but there are a few exceptions.Epidural might not be recommended for patients with certain health conditions, such as:
- Bleeding disorders
- Conditions that require blood thinners
- History of severe brain or spine problems
If you are concerned about your risks, talk with your doctor.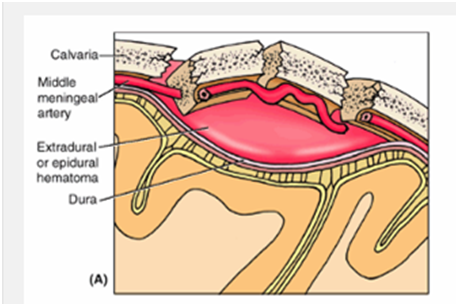 They can set up a consultation with an anesthesiologist to discuss your options.
They can set up a consultation with an anesthesiologist to discuss your options.
Many drugs, from Tylenol to the medication in an epidural, can potentially cross the placenta and affect the baby, but research has shown that the amount of medication that enters your bloodstream and the baby's when you have an epidural is quite low.
Studies have shown that getting an epidural does not negatively affect the baby's Apgar scores (newborn functional testing), nor does it increase the risk of needing neonatal intensive care.
Related reading: Should I stop taking medication when I’m pregnant?
Myth: Moms who get epidurals need C-sections more often. Reality: Epidural doesn't increase the likelihood of a C-section, studies show.
Reality: Epidural doesn't increase the likelihood of a C-section, studies show.Several landmark studies have shown that getting an epidural does not increase the chance you'll need a cesarean section delivery. Previously, we thought epidurals may increase your risk of vacuum- or forceps-assisted delivery, but more recent evidence has suggested this is no longer true.
While the epidural should block most of the pain of labor, it should not complicate labor or prevent you from pushing. Epidural medication will not cause fetal distress or cause the baby to "get stuck." When this happens, it's likely that the situation would have occurred regardless of whether the patient had received an epidural.
Myth: Labor will take longer and I'll be stuck in one spot if I get an epidural.Reality: There is no credible research to suggest this is true.Labor is typically divided into two stages – progressive cervical dilation to 10cm and pushing.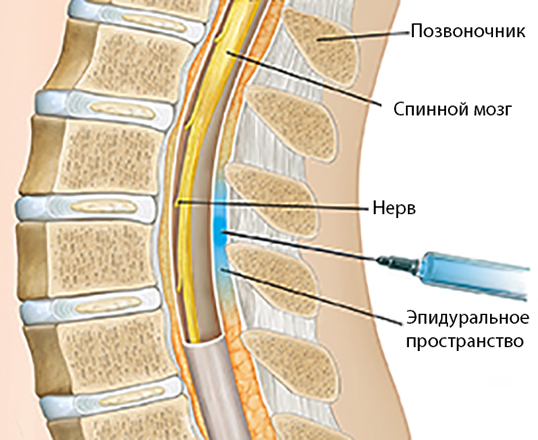 Getting an epidural has no effect on how long stage one takes. Some research suggests the pushing stage might be a bit longer if you are more relaxed and pushing is less urgent, but we're likely talking minutes, not hours.
Getting an epidural has no effect on how long stage one takes. Some research suggests the pushing stage might be a bit longer if you are more relaxed and pushing is less urgent, but we're likely talking minutes, not hours.
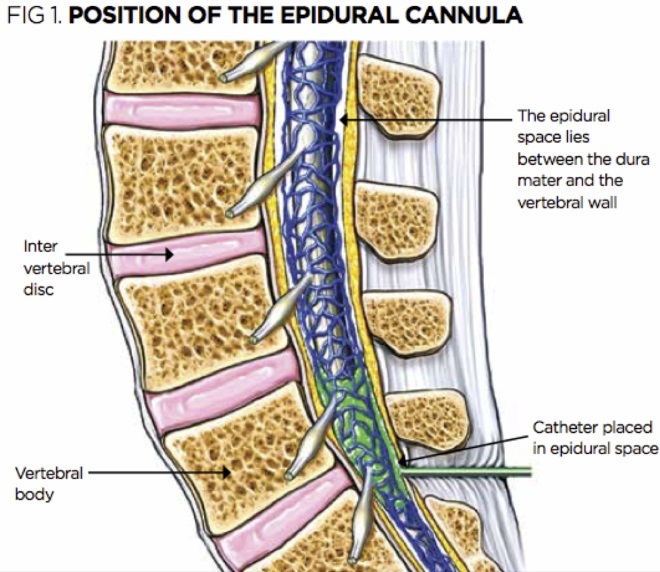
Advancements in epidural medication administration over the last 20 years have allowed us to control pain without making you feel as weak. You'll still be able to feel pressure from contractions (with less or no pain), and you'll still be able to push. The anesthesia team will securely tape the catheter in place after it is inserted so that you can move comfortably in the bed and switch positions as you like.
Myth: Epidurals cause prolonged back pain after delivery.Reality: Getting an epidural will not cause chronic back pain.The more likely culprit is that your body is sore from the pregnancy and delivery experience, and the constant bending and lifting required for newborn care.
After any injection, from a flu shot to an epidural, you'll likely feel some pain and swelling at the injection site, which should resolve within a week. Me personally, I felt like the tenderness was a fair trade for three less painful labors and deliveries.
Me personally, I felt like the tenderness was a fair trade for three less painful labors and deliveries.
While not impossible, permanent nerve damage or paralysis is extremely unlikely – estimated at less than 1 in 240,000 patients. Pushing and positioning during labor can cause temporary injuries, such as nerve compression (a "pinched" nerve). Pushing is a very physical, stressful body event that can cause swelling and nerve irritation. Even in these cases, temporary damage is extremely rare.
Myth: I have a lower-back tattoo, so I can't get an epidural.Reality: Patients with low-back tattoos can safely get epidurals.Theoretically, there is some risk that the tattoo ink could be introduced into the spinal canal. But reports of tattoo-related epidural complications are very rare and controversial.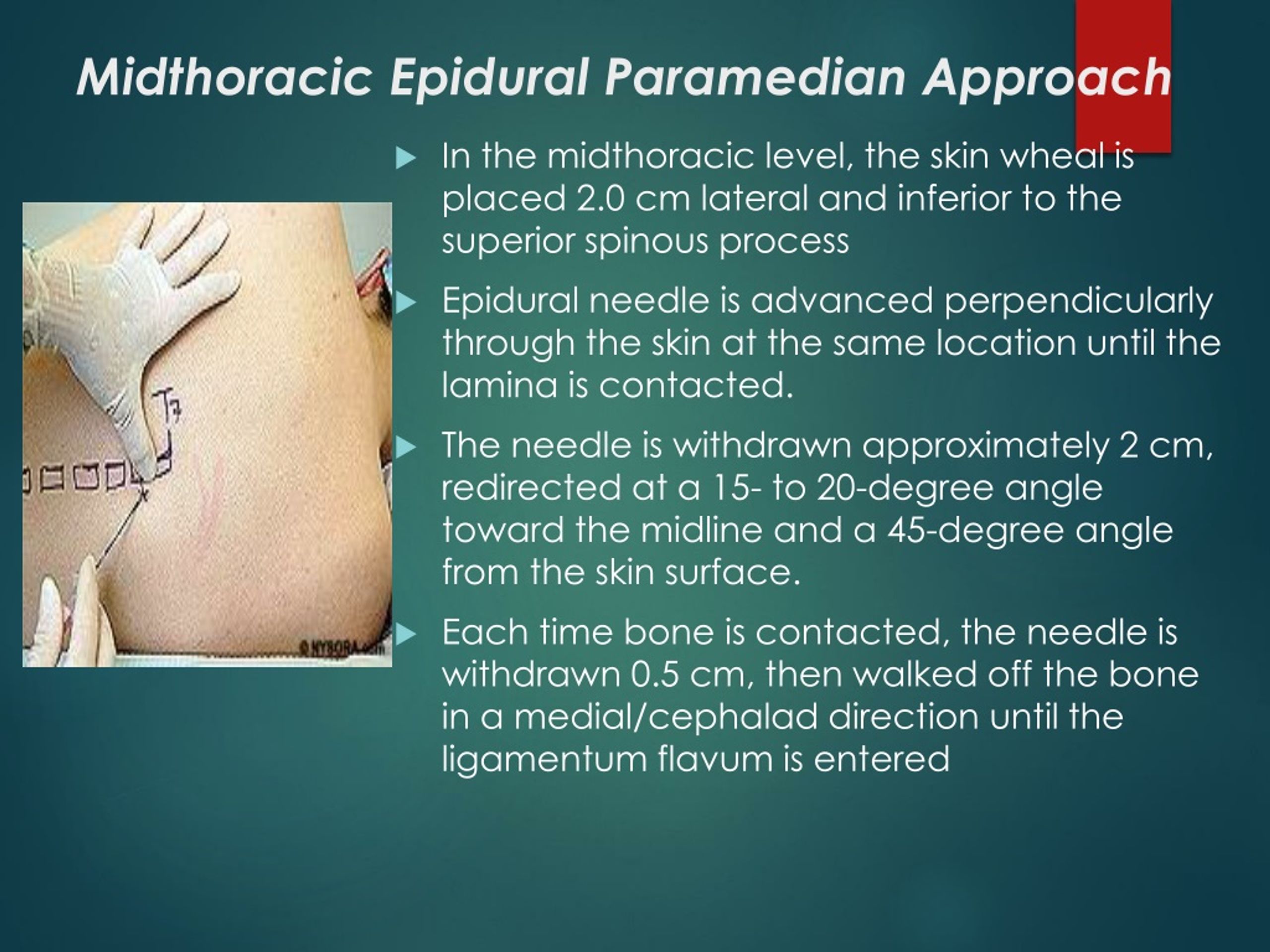 To avoid that tiny risk, we will find a suitable spot on the spine where there is little to no ink.
To avoid that tiny risk, we will find a suitable spot on the spine where there is little to no ink.
Labor pain is very intense – I know firsthand from having my own babies. Choosing an epidural is not a failure. It's a choice to help you stay calm and focused, which is so important for a successful delivery. There are plenty of things to worry about as a mom – so you shouldn't feel defeated if your birth plan changes and you decide to get an epidural.
If you, your partner, or your labor support person can't tolerate the sight of needles, tell your doctor right away. Epidural needles are thin but long – depending on your weight, the needle will be 9 to 11cm long.
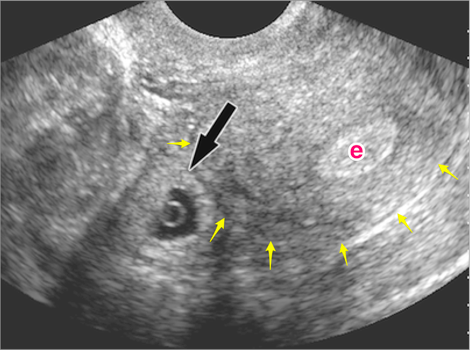
The anesthesiologist positions the epidural injection for maximum pain relief without disturbing the spinal nerves.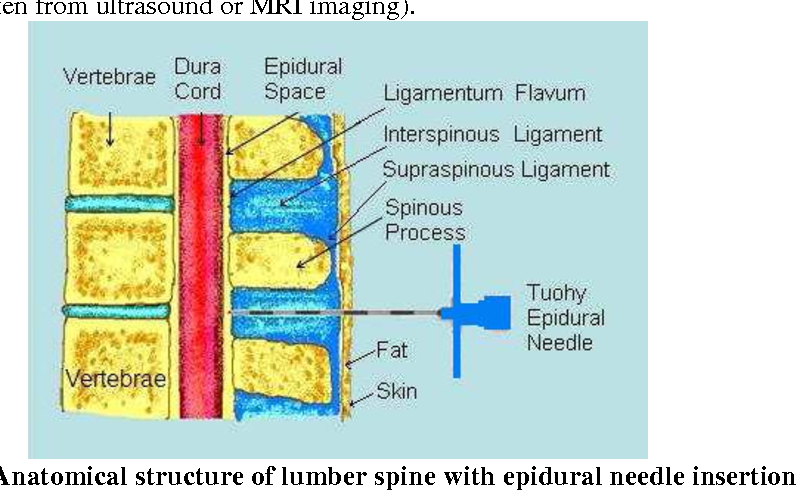
Your anesthesiologist will ask you to hold as still as possible for five to 10 minutes. We ask patients to curl forward, with their back arched like a shrimp. They will numb a spot on your spine, then insert the needle and a tiny tube into your spine. It will feel like a pinch, and you will feel some pressure as the needle is positioned – we're looking for just the right spot for maximum pain relief without disturbing the spinal nerves.
Within 10 to 20 minutes, you should feel little to no pain from the waist down. You won't be able to walk while the medication is flowing and your legs will feel weak – that is normal. Feeling and mobility will return within an hour or so after the needle is removed.
Your injection site might be sore for a few days after delivery. Fewer than 1 percent of patients develop a severe headache due to leakage of spinal fluid. Some women report feeling itchy or nauseous as the medication wears off.
Choosing your preferred pain relief method for labor and delivery is a personal decision.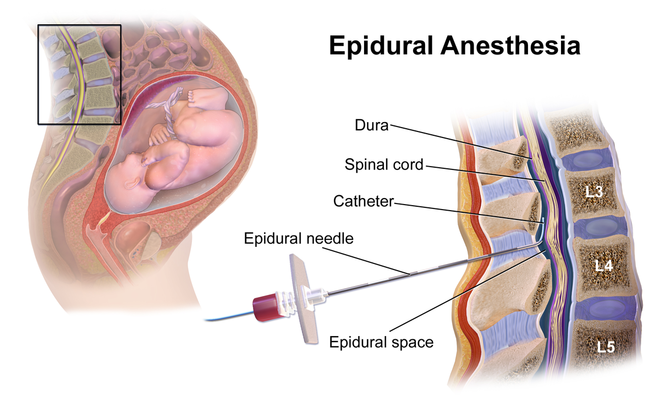 Whether you plan to have an epidural or decide to update your birth plan during labor, we will be ready to help you manage your pain. At the end of the day, your health and safety – and that of your baby – is the most important part of the birth experience.
Whether you plan to have an epidural or decide to update your birth plan during labor, we will be ready to help you manage your pain. At the end of the day, your health and safety – and that of your baby – is the most important part of the birth experience.
To talk with an Ob/Gyn about labor pain relief options, call 214-645-8300 or request an appointment online.
More in: Your Pregnancy Matters
Mental Health; Your Pregnancy Matters
- Robyn Horsager-Boehrer, M.
 D.
D.
October 11, 2022
Prevention; Your Pregnancy Matters
- Robyn Horsager-Boehrer, M.D.
October 4, 2022
Mental Health; Your Pregnancy Matters
- Meitra Doty, M.
 D.
D.
September 27, 2022
Your Pregnancy Matters
- Robyn Horsager-Boehrer, M.D.
September 20, 2022
Men's Health; Women's Health; Your Pregnancy Matters
- Yair Lotan, M.
 D.
D.
September 6, 2022
Your Pregnancy Matters
August 29, 2022
Your Pregnancy Matters
- Patricia Santiago-Munoz, M.D.
August 23, 2022
Mental Health; Your Pregnancy Matters
August 11, 2022
Your Pregnancy Matters
- Emily Adhikari, M.
 D.
D.
August 2, 2022
More Articles
Epidurals for Labor: Risks, Benefits and Other FAQs
It’s no secret that giving birth is painful! But every woman finds a way to manage the pain of childbirth — whether that’s through breathing exercises, position changes, or an epidural.
During your third trimester, your OBGYN will ask you about your preference for pain management during labor. Whatever your decision, you can change your mind even during labor (up until a certain point). Our goal is to support you so that you can have a positive birthing experience, whatever that looks like for you.
About 70% of women in our practice choose to receive an epidural during labor. And all of them have had very similar questions, fears and concerns about the process.
What is an epidural?
An epidural is a common type of anesthetic used in labor for pain relief.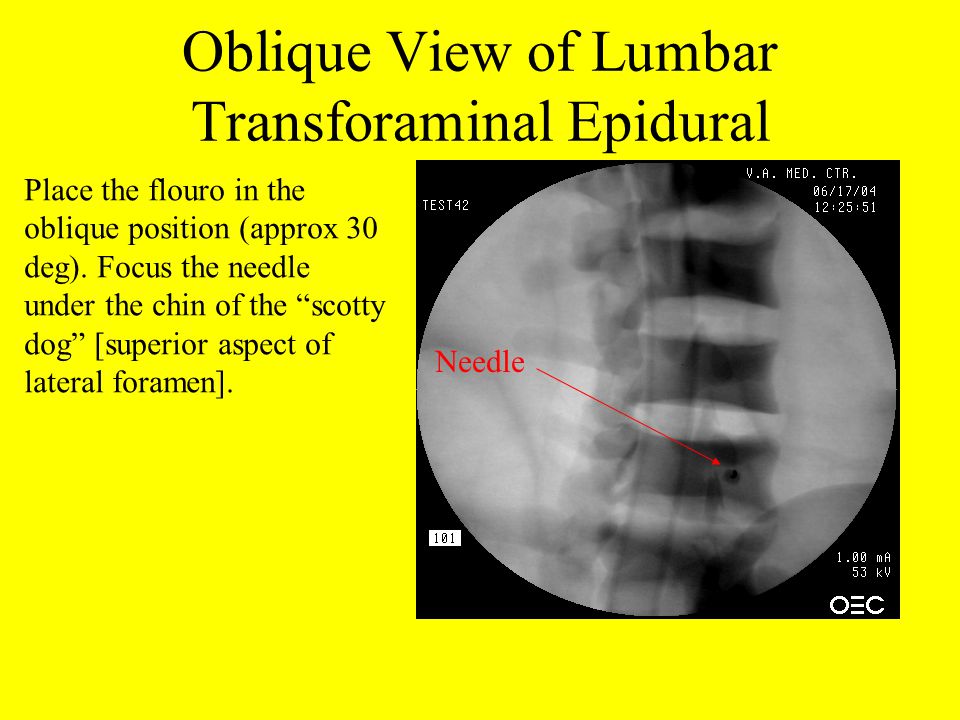 Epidurals are the best option available for relieving labor pain. An epidural can be given at any time during the labor process.
Epidurals are the best option available for relieving labor pain. An epidural can be given at any time during the labor process.
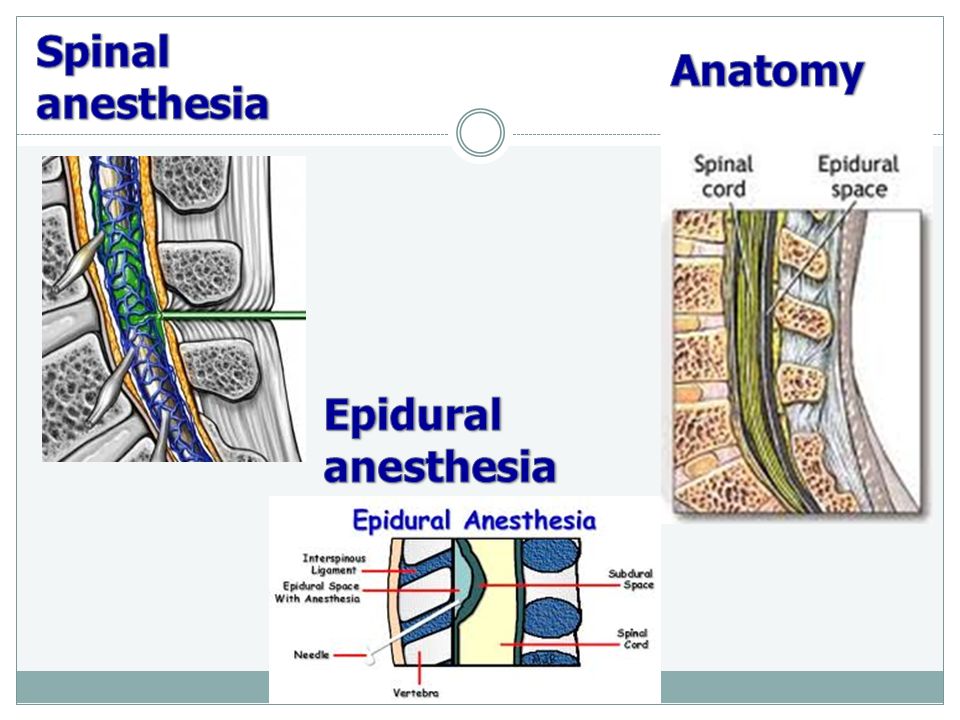
While you are sitting up an anesthesiologist will first numb your skin and then insert a needle and a tiny tube (called a catheter) into the lower part of your back. The needle is removed and the catheter is left in place so that medication can be delivered through the tube. The medication typically runs continuously until delivery, with more medication given through the tube as needed.
The process takes about 15 minutes to complete. As long as you’re able to get into the right position and stay still for the time it takes to place the catheter, you can receive the epidural at any point during labor. That means that you can still receive an epidural even if you initially thought you didn’t want one!
Is the epidural needle painful?
Before the epidural is placed, you’ll be given a numbing injection. The first injection will feel like a short bee sting. This lasts only for a moment. Once that area is numb from the injection, the anesthesiologist will place the catheter to deliver the pain relieving medication. It takes about 20 minutes for contraction pain to subside.
This lasts only for a moment. Once that area is numb from the injection, the anesthesiologist will place the catheter to deliver the pain relieving medication. It takes about 20 minutes for contraction pain to subside.
An epidural creates a feeling of numbness from your belly to your toes. You may still feel pressure during labor, but the pain will be drastically reduced. If you are still uncomfortable even after having the epidural placed, the anesthesiologist may give you additional medication through the catheter or place the catheter in a slightly different position.
Because you will feel numb, it will be hard to move your legs. You won’t be able to walk around with an epidural in place. You may not feel as great of an urge to push, but you will still be able to push. Your team will help you know when and how to push through your contractions.
You also won’t feel the need to urinate, so we will place a foley catheter in your bladder.
Will an epidural harm my baby?
Medication from an epidural does NOT harm your baby.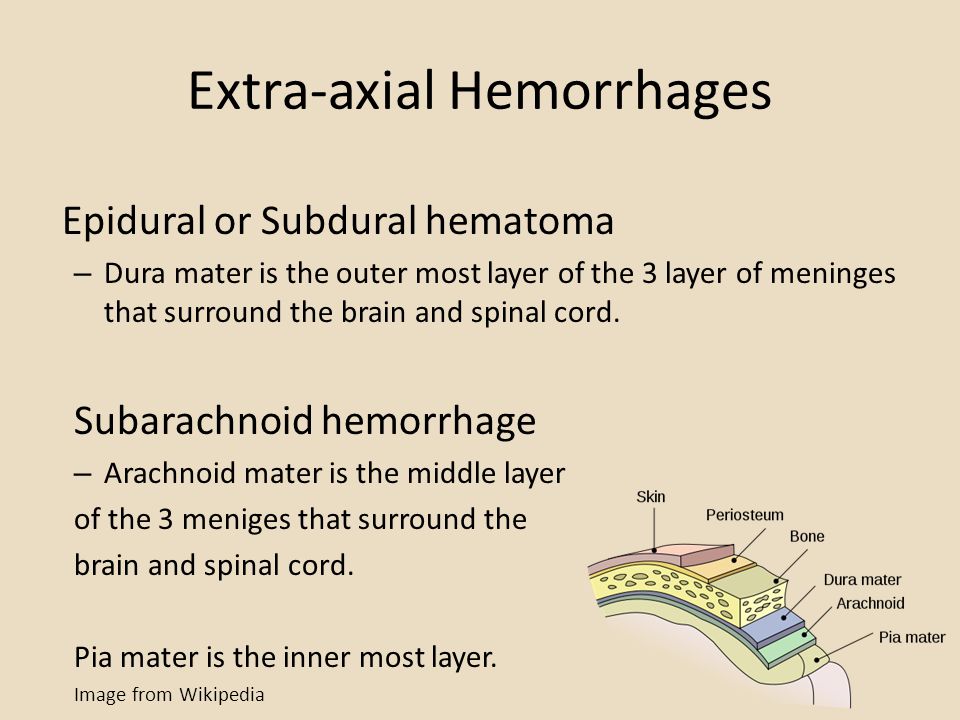 Because the anesthesia from the epidural doesn’t enter your bloodstream, it will not transfer to your baby through the placenta.
Because the anesthesia from the epidural doesn’t enter your bloodstream, it will not transfer to your baby through the placenta.
How long does the epidural last?
The epidural is intended to last for the duration of your labor and will be removed after you deliver your baby. It will take a couple of hours for the numbness to completely go away. You will be able to walk around after the epidural wears off.
To manage pain after delivery, you’ll be given ibuprofen. Ice packs can also be applied to help with discomfort after labor.
What are the side effects from an epidural?
Epidurals are very safe. Serious complications are rare. The most common side effect we see is a decrease in blood pressure. To prevent this, you will be given extra IV fluid before having an epidural placed. If needed, the anesthesiologist may also give you medication to bring your blood pressure up.
Who shouldn’t get an epidural?
Occasionally there are circumstances where women can’t get an epidural.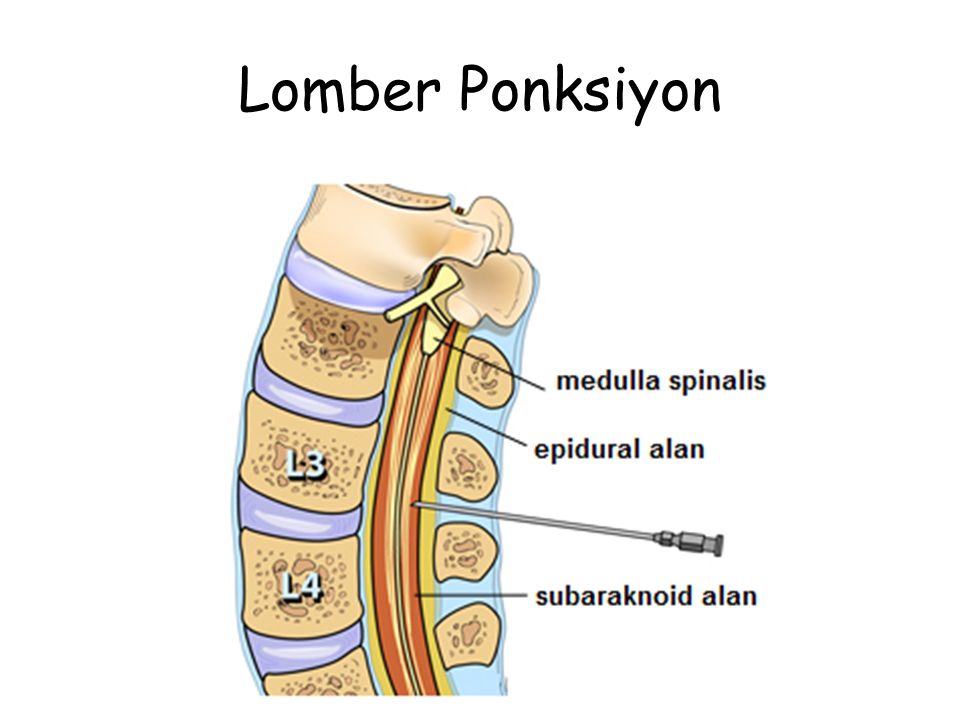 Occasionally we see this in women who have a low platelet count. Additionally, women who are taking blood thinners (such as heparin) to prevent a blood clot during pregnancy should not receive an epidural within 12 hours of taking that medication.
Occasionally we see this in women who have a low platelet count. Additionally, women who are taking blood thinners (such as heparin) to prevent a blood clot during pregnancy should not receive an epidural within 12 hours of taking that medication.
Will an epidural slow down delivery or cause me to need a C-section?
Some women are actually able to deliver more quickly after receiving an epidural because they feel more relaxed. They can push through the stronger contractions because they are in less pain. Other women may be in labor a little longer because they do not feel the urge to push to the same extent.
Your labor and delivery team will monitor you and your baby to be sure that you are progressing through labor at a safe rate.
There is no evidence that receiving an epidural makes you more likely to require a C-section. In fact, if you do need a C-section, having an epidural in place can help you be prepared for the C-section more quickly.
Other Ways to Manage Pain During Childbirth
An epidural is not the only way to manage pain during childbirth.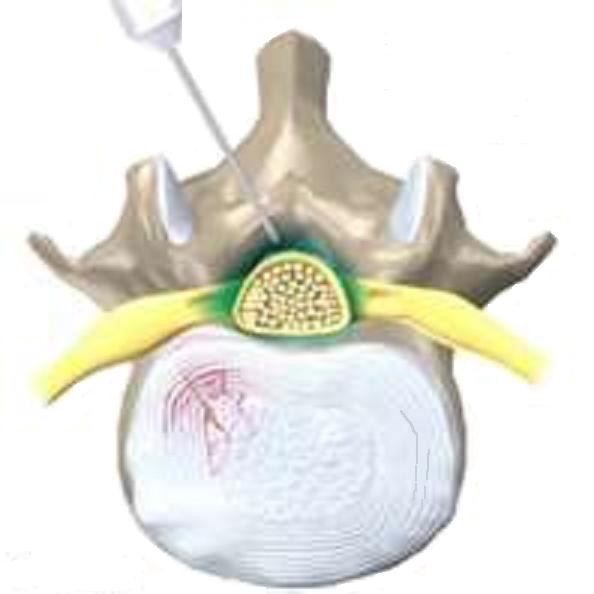 You have several options available to you. You are also able to make changes to your birth plan while you are in labor.
You have several options available to you. You are also able to make changes to your birth plan while you are in labor.
Non-medicated pain control options
There are several non-medicated (or non-pharmacologic) pain control options. Read about other methods of pain relief during childbirth.
Intravenous (IV) and Intramuscular pain relief:
Pain relieving medication (opioids) can be given to help take the edge off of labor pain to make it more tolerable. This medication is either given to you through an IV or as an injection.
Opioids given through an IV catheter do enter your bloodstream, therefore they do transfer to your baby. Side effects include grogginess or sleepiness for both you and your baby.
Conclusion
We don’t judge your reasons for or against receiving an epidural. Some of our patients choose not to receive any pain medications during labor while others request an epidural as soon as possible. (You may be surprised by how many women change their minds during labor!) There isn’t a right or wrong way of giving birth, and you aren’t more or less of a mom or a woman based on your pain management decision.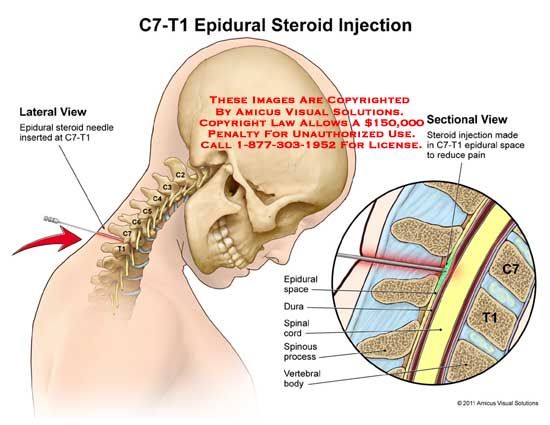
Whether you want a less painful labor or a medication-free labor, we are here to support you. Our goal is that you and your baby are safe and healthy!
Not Found (#404)
Paracelsus Medical Center
Page not found.
The above error occurred while the Web server was processing your request.
Please contact us if you think this is a server error. thank you.
Please wait, download may take time
Loading...
Do you know which doctor you want to see
You know the service you want to sign up for
Service selection
A second consultation is considered to be a consultation of one specialist within 30 days from the date of the previous appointment.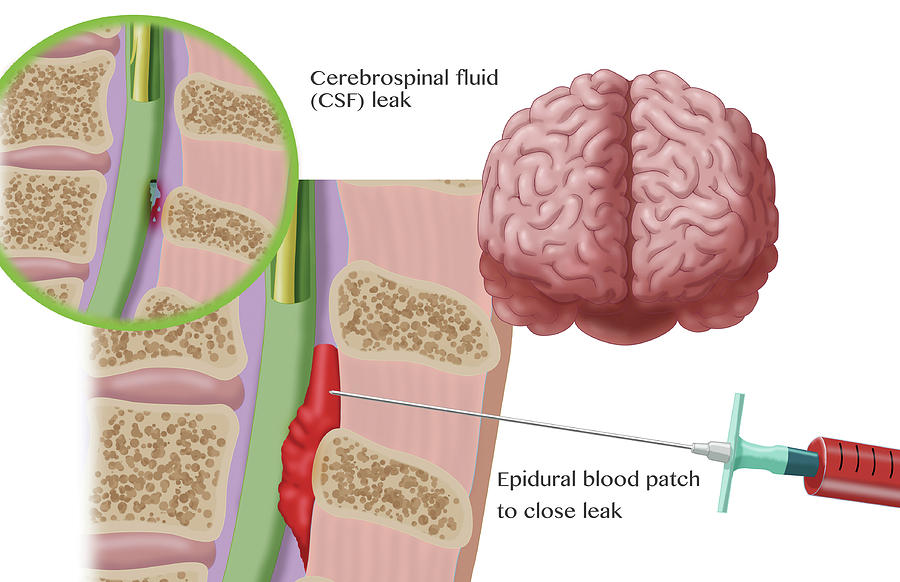 On the 31st day from the previous visit to a specialist of this profile, the consultation will be primary.
On the 31st day from the previous visit to a specialist of this profile, the consultation will be primary.
The choice of a specialist
Service selected:
Choosing a specialist service
A second consultation is considered to be a consultation of one specialist within 30 days from the date of the previous appointment. On the 31st day from the previous visit to a specialist of this profile, the consultation will be primary.
Address selection:
st.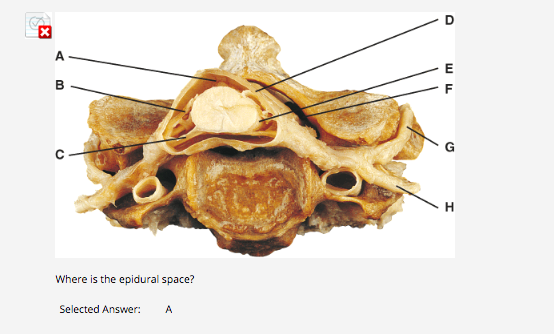 Vikulova, 33, building 2 st. Bolshakova, d. 68
Vikulova, 33, building 2 st. Bolshakova, d. 68
Date selection:
Time of receipt:
Password
Password
Register Can't login? account activation
To gain access to your personal account, enter the e-mail that was specified during registration, we will send instructions for password recovery
To gain access to your personal account, enter the e-mail that was specified during registration, we will send instructions for reactivating your account
Your application has been accepted, our specialists will answer your question as soon as possible!
Telephone
Comment
Dear patients!
Multidisciplinary Clinic and Maternity Hospital "Paracelsus" informs you, according to the Letter of the Ministry of Finance of the Russian Federation to the Federal Tax Service dated March 25, 2022. N BS-4-11 / 3605, that subparagraph 3 of paragraph 1 of Article 219The Tax Code of the Russian Federation provides for the right of a taxpayer to receive a social tax deduction in the amount paid by him in the tax period for medical services provided by medical organizations engaged in medical activities to him, his spouse, parents, children (including adopted children) in under the age of 18, wards under the age of 18 (in accordance with the list of medical services approved by the Government of the Russian Federation).
N BS-4-11 / 3605, that subparagraph 3 of paragraph 1 of Article 219The Tax Code of the Russian Federation provides for the right of a taxpayer to receive a social tax deduction in the amount paid by him in the tax period for medical services provided by medical organizations engaged in medical activities to him, his spouse, parents, children (including adopted children) in under the age of 18, wards under the age of 18 (in accordance with the list of medical services approved by the Government of the Russian Federation).
Joint order of the Ministry of Taxation of Russia and the Ministry of Health of Russia of July 25, 2001 N 289 / BG-3-04 / 256 (hereinafter - the order of July 25, 2001) approved the form of the Certificate of payment for medical services for submission to the tax authorities of the Russian Federation (hereinafter - the Certificate payment for medical services).
This certificate certifies the fact of receiving a medical service and its payment through the cash desk of a healthcare institution at the expense of the taxpayer.
Thus, if the taxpayer submits to the tax authority a Certificate of payment for medical services, the taxpayer's failure to submit the relevant contract for the provision of medical services and (or) documents confirming payment cannot be grounds for refusing to provide such a deduction.
The amounts are based on payment data. Therefore, checks, an agreement and a clinic license are not needed to make a deduction.
Sample certificate attached.
Help Sample
Your application has been accepted, our specialists will contact you shortly!
Telephone
Comment
All about epidural anesthesia - Private maternity hospital Ekaterininskaya 9 Clinics0001
What to do if long-term epidural anesthesia (analgesia) is contraindicated for you or you do not want to have it during childbirth for some reason?
There is, in fact, only one real alternative - childbirth can be anesthetized with narcotic analgesics (usually fentanyl or promedol).
In certain situations (regular strong contractions, good dilatation of the cervix, satisfactory condition of the child according to ultrasound and CTG), it is safe and effective.
But, firstly, the duration of the effective action of narcotic analgesics in childbirth is much shorter (from 30 minutes to 1 hour) than the duration of the effect of DEA. Secondly, the possibility of prolonging such pain relief is significantly limited, since high doses of narcotic analgesics increase the risk of respiratory depression in mother and child. This method is usually used when there are contraindications to DEA.
There are no medical procedures that do not carry potential risks and do not have contraindications for the patient. Long-term epidural anesthesia (DEA) is no exception, and it would be irresponsible not to talk about them.
What are the contraindications for DEA?
- Injuries of the spine and metal structures in the lumbar region, some congenital diseases of the spine and severe forms of curvature (scoliosis).
- Pronounced blood coagulation disorders in the direction of reducing the density of the blood clot (hypocoagulation).
- Allergy to the local anesthetic ropivacaine (very rare).
- Severe heart disease with fixed cardiac output.
- Tattoo in the lumbar region (the paint may contain salts of heavy metals, the entry of which into the epidural space is highly undesirable).
- The categorical written refusal of the patient from DEA (with justification of the reasons for the refusal).
What is the risk of complications and side effects with DEA?
- Insufficiently effective pain relief (mosaic block).
- Unintentional puncture of the dura mater with the development of post-puncture headache syndrome.
- Sudden drop in blood pressure.
- Nausea, vomiting, chills.
- Post-puncture back pain.
- Respiratory and cardiac arrest.
- Urinary retention and dysfunction of the pelvic organs.
- Development of persistent neurological complications in the form of paresis and paralysis.
A very impressive and intimidating list, especially the second half of it.
But according to world statistics for the 1990-2000s, the risk of fatal complications of regional anesthesia (DEA is a regional method) is 25-38 cases per 10 million obstetric patients, and does not differ significantly from the risk of general anesthesia.
The risk of developing any complications of EA (not only fatal, but generally all) is higher, but it is also quite low, and, according to various estimates, is 1 case per 50,000-80,000 births. This risk is about 8-10 times less than the risk of dying in an accident (driver, passenger or pedestrian).
Despite the impressive list of contraindications and risks, there are many undeniable advantages of using long-term epidural anesthesia (DEA).
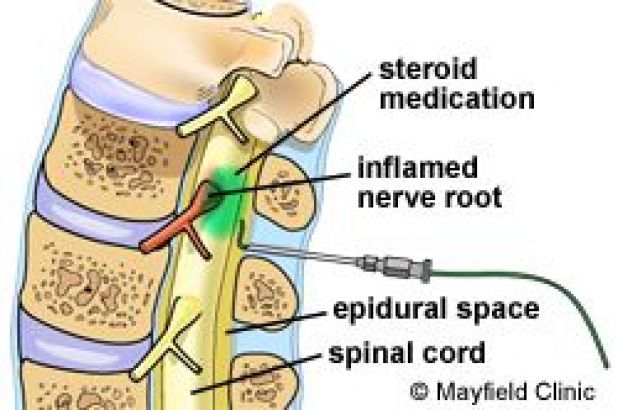
There is practically no effect on the child - the area of action of the anesthetic is limited to the nerve roots of the spinal cord of the woman in labor; neither the blood flow in the umbilical cord nor the fetal heart rate is affected by DEA performed in compliance with all safety rules.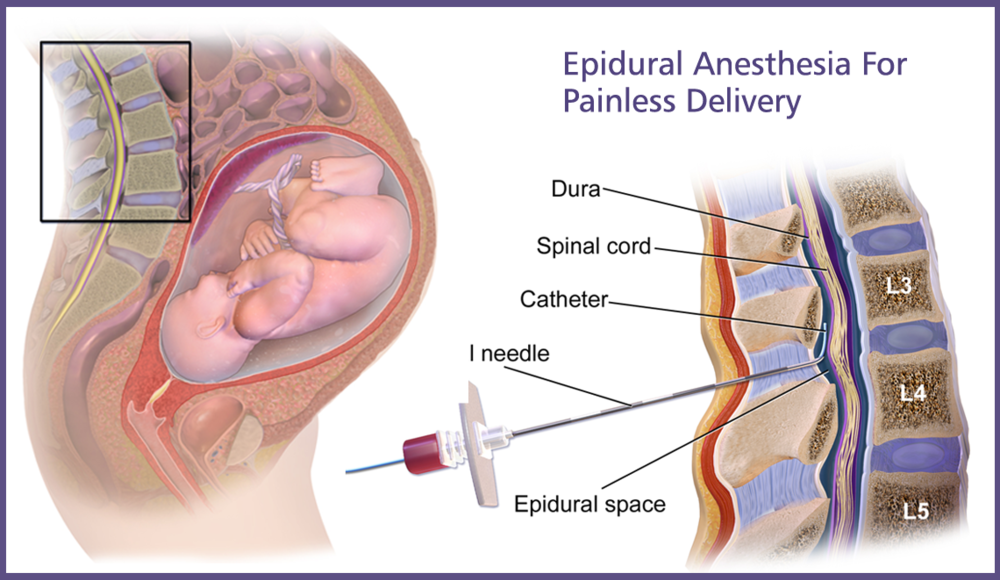
If the situation in labor is such that there is an indication for an emergency caesarean section, an epidural catheter inserted in labor allows you to quickly inject a large dose of anesthetic (about 4 times more than for pain relief in labor), adequate for a caesarean section - and more one significant plus DEA. This is called "conversion of analgesia to anesthesia".
In such a situation, drugs for general anesthesia are either not used at all or are used in small doses (depending on the situation), which significantly reduces the burden on the body of the mother and child, and allows the patient to “recover” faster after the operation. DEA lowers blood pressure by 15-20 percent of baseline, and in patients with high blood pressure, it is a real lifesaver.
What can be said to conclude this large, complex and rather acute topic?
⠀
Absolutely safe medical procedures with zero risk do not exist in principle. But compliance with all the rules, safety precautions, indications and contraindications allows you to reduce the risk to an insignificant minimum.