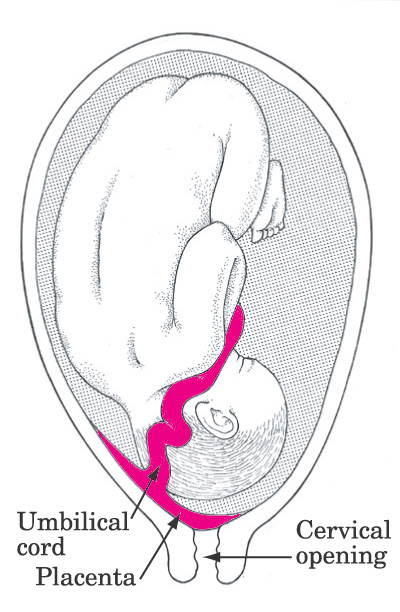
Miscarriage with closed cervix
Threatened Miscarriage: Why It Happens & How To Stop It
A threatened miscarriage is defined as any vaginal bleeding that happens during the first 20 weeks of pregnancy, while the cervix remains closed. Despite the anxiety that it causes, this occurrence is very common, especially in the first trimester and less so in the second. As many as 20% of all expecting women will have some type of vaginal bleeding and about half of these will still carry to term successfully.
A threatened miscarriage can raise the risk of miscarriage by 2.6 times. Moreover, 17% of women who suffered a threatened abortion but did not miscarry may go on to have further complications within the same pregnancy. This is why it’s critical to carefully investigate, monitor and treat any expecting woman who presents with vaginal bleeding.
Threatened miscarriage doesn't necessarily mean pregnancy loss
SymptomsA threatened miscarriage presents with vaginal bleeding. The bleeding can range from mild spotting to heavy bleeding, sometimes with clots. The color of the blood can also range from soft brown to bright red (the latter indicating a fresh bleeding). The vaginal bleeding is sometimes accompanied by lower abdominal or back pain, which may resemble period pain or feel different. The cervix remains closed at all times. If the cervix opens, the threatened miscarriage becomes an imminent miscarriage and it can no longer be prevented from happening.
If bleeding and pain occur, but the pregnancy cannot be located on a transvaginal ultrasound, ectopic pregnancy or a chemical miscarriage (a miscarriage that happens before the pregnancy reaches a clinically visible size) are the most common explanations.
What Causes a Threatened MiscarriageThere is a wide variety of possible causes and favoring factors for a (threatened) miscarriage.
Often, a problem with the pregnancy itself is what causes a miscarriage and all its accompanying symptoms. A chromosomal abnormality in the embryo, an embryo that has stopped developing, a blighted ovum (a pregnancy that is missing an embryo altogether) or very rarely even a molar pregnancy (a very abnormal development of the placenta) will all trigger the woman’s body to eliminate the pregnancy that is no longer viable.
A chromosomal abnormality in the embryo, an embryo that has stopped developing, a blighted ovum (a pregnancy that is missing an embryo altogether) or very rarely even a molar pregnancy (a very abnormal development of the placenta) will all trigger the woman’s body to eliminate the pregnancy that is no longer viable.
Another very common reason for a threatened abortion is a progesterone deficiency, which may result from a more general Luteal Phase Defect syndrome or from an isolated inability to produce sufficient amounts of progesterone for that particular pregnancy. Whatever the underlying cause, it can be easily treated with progesterone supplements or HCG (Human Chorionic Gonadotropin) injections, which both increase progesterone levels.
A bacterial infection in the proximity of the uterus (such as a vaginal infection that has reached the cervix and uterus), or one that has spread to the blood (bacteremia) from another part of the body, can often induce a miscarriage.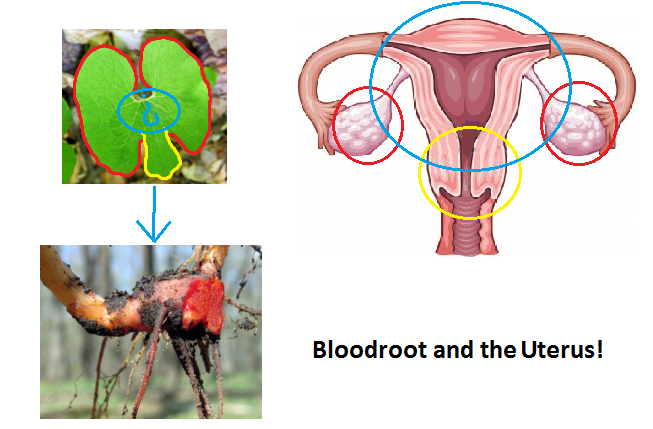 It’s unfortunately very difficult to salvage a pregnancy that has been exposed to bacterial infection, even with prompt use of antibiotics.
It’s unfortunately very difficult to salvage a pregnancy that has been exposed to bacterial infection, even with prompt use of antibiotics.
Certain types of viral and parasitic infections can also trigger a miscarriage. Toxoplasmosis, Rubella, Cytomegalovirus, HIV, Syphilis, even Influenza, have been all been associated with failed pregnancies in various studies.
Occasionally, an anatomic abnormality of the uterus could hinder the pregnancy from developing normally. For example, certain uterine malformations (arcuate uterus, septate uterus, unicornuate uterus, etc.) or uterine growths like fibroids, polyps and adhesions may create an unfavorable environment for the pregnancy and set off various complications, including a threatened miscarriage.
A threatened abortion can have multiple causes, many of which can be treated
Untreated chronic diseases such as thyroid conditions (particularly hypothyroidism and hyperthyroidism), diabetes or chronic high blood pressure have long been linked to miscarriage and pregnancy complications.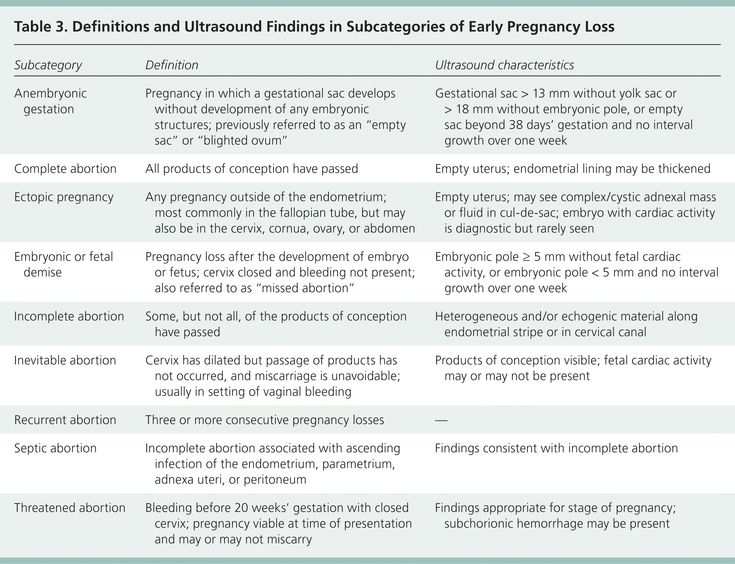 Similarly, systemic autoimmune disorders (lupus, antiphospholipid syndrome) and clotting abnormalities (thrombophilia) can lead to an unfavorable pregnancy outcome if they are not properly managed.
Similarly, systemic autoimmune disorders (lupus, antiphospholipid syndrome) and clotting abnormalities (thrombophilia) can lead to an unfavorable pregnancy outcome if they are not properly managed.
Sometimes, an Rh incompatibility between the mother and fetus is what activates the rejection response from the mother’s body, in cases when the mother is Rh negative. Rh is a type of blood antigen and is easily tested for with a quick blood test. Normally this rejection almost never happens with a first pregnancy, but an immune response could develop with subsequent pregnancies.
Exposure to certain medications and chemical substances during early pregnancy has also been shown to increase the likelihood of a miscarriage. Alcohol, drug use, smoking and even high caffeine intake (over 200mg per day) are associated with various negative pregnancy outcomes.
A traumatism of any kind to the abdomen may also conceivably trigger a pregnancy loss.
When no obvious cause can be identified for a threatened miscarriage, it is called unexplained (or idiopathic). More subtle underlying mechanisms may be at work, some that we cannot yet clinically study or test for, or that we have just begun investigating. Possibilities include: an irritable uterus (a uterus that doesn’t relax as it should during the pregnancy and keeps cramping and contracting), advanced maternal age (age over 35), emotional stress, excessive physical exercise, sexual intercourse.
Tests and diagnosisIf you are dealing with a threatened miscarriage, your doctor will probably order a few medical tests to better understand the source of the problem and make the best decision for you and your pregnancy.
A transvaginal ultrasound is typically the first investigation performed, since it can offer a quick and clear picture of the pregnancy, its location and whether or not the cervix is still closed. It will help indicate if the pregnancy has stopped developing, is ectopic or is still developing normally. As a general rule, if a normally developed embryo with a good heartbeat is discovered in the uterus and the cervix is still closed, then there is a very good chance that the pregnancy will continue successfully, in spite of the vaginal bleeding (in some studies, over 90% odds).
It will help indicate if the pregnancy has stopped developing, is ectopic or is still developing normally. As a general rule, if a normally developed embryo with a good heartbeat is discovered in the uterus and the cervix is still closed, then there is a very good chance that the pregnancy will continue successfully, in spite of the vaginal bleeding (in some studies, over 90% odds).
First trimester ultrasound, showing a healthy pregnancy and embryo
The doctor may also perform a pelvic exam to look at the cervix and vagina and determine if the source of the bleeding may be the cervix instead. A high vaginal or cervical swab and a Pap test will usually be taken with this occasion to look for any possible infections.
A series of blood tests is also recommended.
HCG (Human Chorionic Gonadotropin) blood levels will normally correlate with the gestational age, so a large discrepancy may point to a pregnancy that is not developing normally.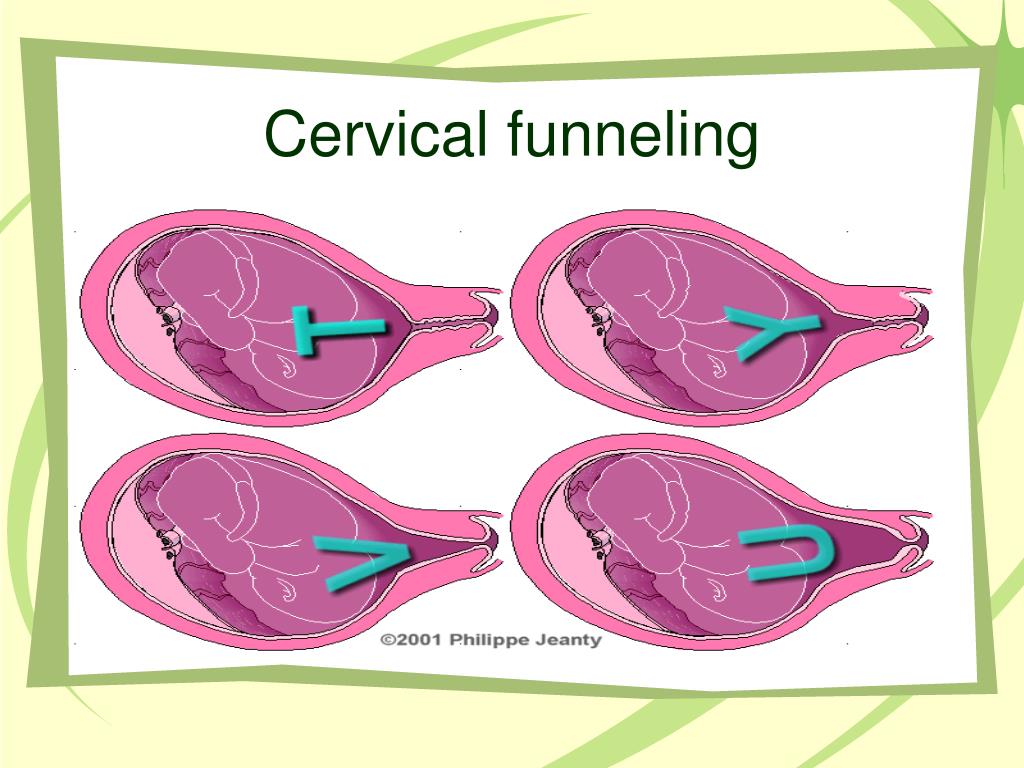 A series of HCG tests taken every 48h will often show whether the pregnancy is advancing or failing, since HCG titers are expected to double every 48-72h.
A series of HCG tests taken every 48h will often show whether the pregnancy is advancing or failing, since HCG titers are expected to double every 48-72h.
A progesterone blood test is very relevant in determining whether the pregnancy may benefit from progesterone supplements.
Other blood tests may include: a Complete Blood Count, TSH (Thyroid Stimulating Hormone) levels to check for thyroid dysfunction, Blood group and Rh.
In cases where there is a history of recurrent miscarriage - especially if consecutive, screening panels for Thrombophilia and APS (Antiphospholipid Syndrome), as well as ANA (Antinuclear Antibodies) titers will probably be additionally recommended.
A urine test (urinalysis) is indicated as well, to screen for a UTI (urinary tract infection).
If the pregnancy is non-viable for whatever reason (abnormal embryo, embryo that has stopped developing, no heartbeat, blighted ovum, etc. ) usually the course of action is either a watchful wait (for a natural miscarriage to take place) or a pregnancy termination procedure (an abortion). Various factors may influence this decision, depending on the risks involved and the woman’s personal choice. An ectopic pregnancy will always need to be treated promptly, either with medication or surgically.
) usually the course of action is either a watchful wait (for a natural miscarriage to take place) or a pregnancy termination procedure (an abortion). Various factors may influence this decision, depending on the risks involved and the woman’s personal choice. An ectopic pregnancy will always need to be treated promptly, either with medication or surgically.
If however, the pregnancy is progressing normally despite the bleeding and there is a good fetal heartbeat present, pregnancy support and tocolytic therapy (medications that relax the uterus) may be initiated, especially when there is pain involved and/or a history of multiple miscarriages.
Needless to say, treatment of any underlying conditions affecting fertility, like infections, autoimmune diseases, thyroid dysfunction, diabetes, thrombophilia etc. needs to be initiated as soon as possible and is essential for the favorable progression of the pregnancy.
Certain medications may be helpful when dealing with threatened miscarriage or repeated pregnancy loss
I have compiled a comprehensive list of pregnancy supporting medications that have been studied, used and proven to be largely safe and effective for both mother and baby in cases of threatened miscarriage. Some of them are widely known and available and some are only used in certain parts of the world.
Some of them are widely known and available and some are only used in certain parts of the world.
As an important note, the medications listed here may or may not be recommended during pregnancy in all countries and/or by all doctors. Depending on each country’s medical system regulations and each doctor's professional views, some of these drugs may be discouraged to use during pregnancy or unavailable.
First trimester treatment options for threatened abortion (weeks 2 to 12)
The first trimester is the most sensitive part of embryo development, a time when any minor mistake or interference could possibly result in a birth defect. This is why most medications are restricted or discouraged during this time, unless the benefits of taking them outweigh the risks involved. Still, there are a few relatively safe treatment options if you are dealing with a threatened miscarriage at this stage:
Acetaminophen (Paracetamol) is likely the safest painkiller to take during pregnancy. It is classified as a mild analgesic, so it may be of help if the vaginal bleeding is accompanied by mild to moderate pain. Don’t take it for more than 3 days in a row without speaking to a doctor, though. Trade names also include Tylenol, Panadol.
It is classified as a mild analgesic, so it may be of help if the vaginal bleeding is accompanied by mild to moderate pain. Don’t take it for more than 3 days in a row without speaking to a doctor, though. Trade names also include Tylenol, Panadol.
Drotaverine is an antispasmodic drug that helps calm smooth muscle contractions (including those of the uterus). It is considered completely safe during pregnancy and is available in Asian and Eastern European countries. According to medical studies however, it is only effective to relieve uterine cramps in a little less than 50% of patients. Trade names include No-Spa, Droverin.
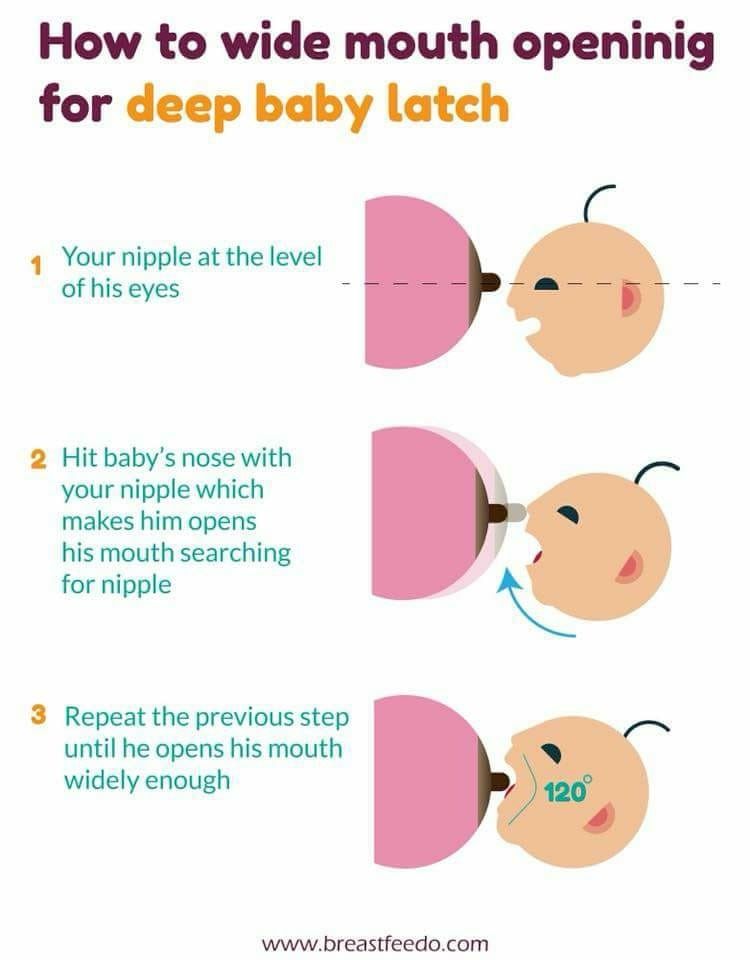
Micronized progesterone supplements are often recommended when dealing with a threatened abortion and even preventively during the first trimester, when there is a history of recurrent pregnancy loss. Progesterone is an essential hormone during pregnancy, which relaxes the uterus and makes the uterine lining more receptive.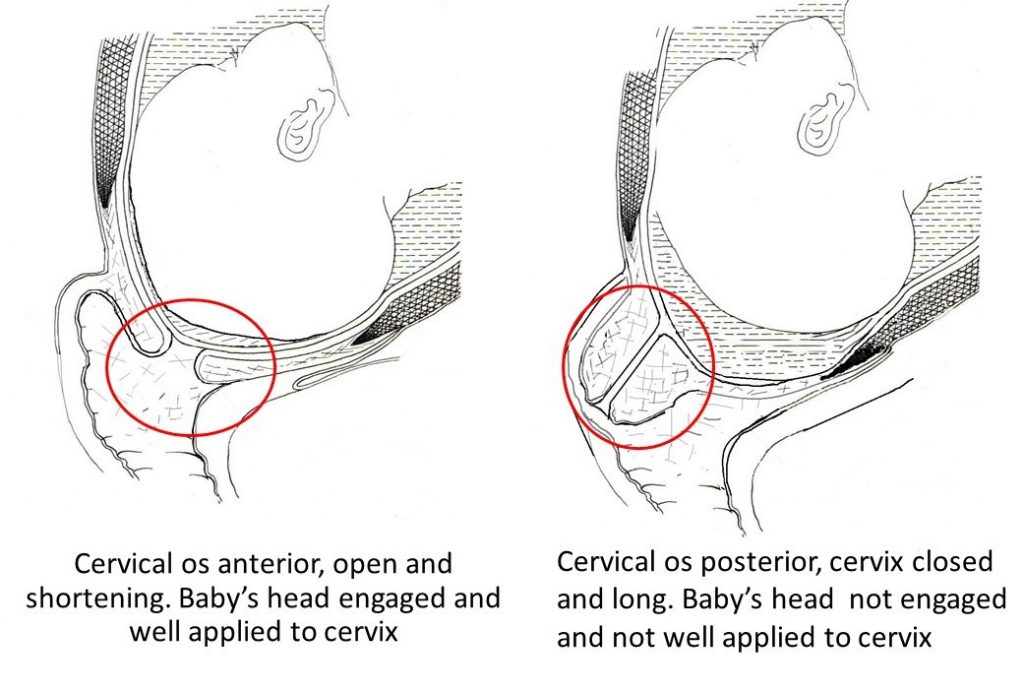 Micronized progesterone supplements are safe to take and come in a variety of forms: oral pills, vaginal suppositories and vaginal gel, of which the vaginal route of administration seems to be the most effective on the uterus. Another very efficient supplement form is progesterone in oil, however it needs to be administered by intramuscular injection.
Micronized progesterone supplements are safe to take and come in a variety of forms: oral pills, vaginal suppositories and vaginal gel, of which the vaginal route of administration seems to be the most effective on the uterus. Another very efficient supplement form is progesterone in oil, however it needs to be administered by intramuscular injection.
HCG (Human Chorionic Gonadotropin) injectable supplements are an extracted form of the natural hormone that is released by the placenta after implantation. HCG keeps the corpus luteum from disintegrating and stimulates progesterone production, both essential for the continuation of the pregnancy. HCG intramuscular injections during the first trimester have been proven to reduce the odds of miscarriage and boost progesterone levels. However, certain brands of HCG should be avoided when the patient suffers from thrombophilia or certain other medical conditions. Trade names include Pregnyl, Novarel, Pubergen, Choragon and Ovidrel.
Sildenafil citrate (more widely known as Viagra) is a medicine that has shown promising results in certain studies where it was administered vaginally during pregnancy. It increased pregnancy retention and lowered miscarriage rates during the first trimester and it improved outcomes in cases of Fetal Growth Restriction and pre-eclampsia in later trimesters. Acting as a vasodilator, it improves blood circulation to and within the uterus when administered locally.
Low dose aspirin (or ‘baby aspirin’, meaning an aspirin dose of less than 100mg) is sometimes prescribed during pregnancy to improve blood flow when a minor blood clotting dysfunction is suspected. It is also useful in preventing miscarriage in cases with a history of recurrent pregnancy loss. It is however debatable whether taking it will improve or rather worsen an active bleeding within the uterus (since aspirin is a blood-thinner that delays coagulation).
Prednisolone is occasionally recommended by some doctors during the first trimester, to encourage pregnancy retention, usually when there is a history of recurrent pregnancy loss. Prednisolone is a corticosteroid that downregulates the immune system. A low dose of it may make it less likely for the mother’s body to interpret the pregnancy as a foreign body and reject it. Its use is, however, still controversial and depends on each doctor’s professional views.
Second trimester treatment options for threatened abortion (weeks 13 to 27)
A (threatened) miscarriage, by definition, can only happen within the first 20 weeks of pregnancy. After this period, it will be called preterm labor. However, most medications that work for preventing a threatened miscarriage during the first part of the second trimester will also work for preventing preterm labor later on.
The second trimester is a somewhat safer time to receive medical treatment, since organogenesis, the most sensitive part of development in the embryo, is now complete.
Metamizole (dipyrone) is used in certain countries (sometimes in combination with other medications) to reduce uterine contractions and lessen the pain sometimes associated with the bleeding.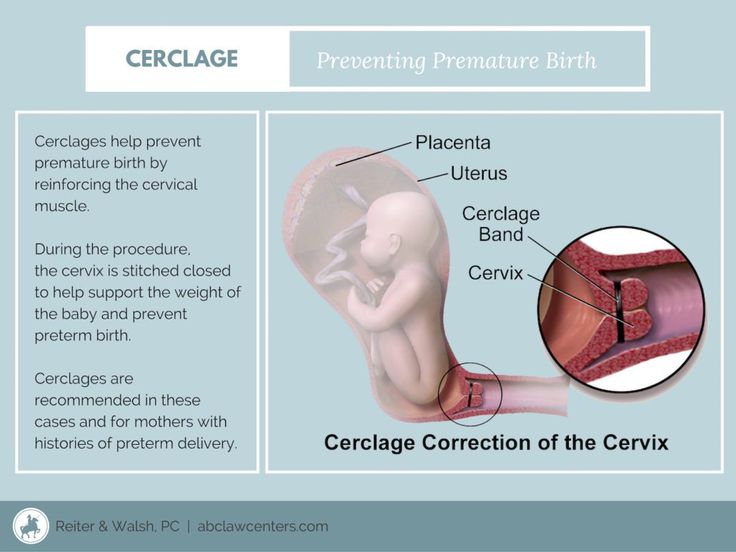 Metamizole is a painkiller, antispasmodic and fever reliever, with anti-inflammatory properties. It is not recommended during the third trimester, but it is considered generally safe when taken before 25 weeks of pregnancy. Mode of administration is usually oral or injectable (intramuscular).
Metamizole is a painkiller, antispasmodic and fever reliever, with anti-inflammatory properties. It is not recommended during the third trimester, but it is considered generally safe when taken before 25 weeks of pregnancy. Mode of administration is usually oral or injectable (intramuscular).
Diazepam is a less popular choice now than it was a couple of decades ago, but in some countries it is still viewed as an efficient aid in stopping a threatened miscarriage during the second trimester. Diazepam is a benzodiazepine with tocolytic features, inhibiting uterine contractions by acting as an alpha1 adrenergic antagonist. Usually delivered at low doses by intravenous drip or by intramuscular injection, it can also be taken orally and has proven a potent uterine muscle relaxant. Because of its sedative properties however, Diazepam is often frowned upon as a solution during pregnancy and it is only used during the second trimester, in certain parts of the world (such as Europe and Asia). This medication should not be taken during the first or third trimester, unless your doctor recommends it. Trade names include Valium, Vazepam.
This medication should not be taken during the first or third trimester, unless your doctor recommends it. Trade names include Valium, Vazepam.
Beta2 adrenergic agonists are typically a popular choice worldwide for treatment of both threatened miscarriage and preterm labor. They are vasodilators and uterine muscle relaxants that suppress uterine contractions very efficiently, however they are not as effective before at least 17-18 weeks of pregnancy, so they are a better choice for the second half of the second trimester (and until term). Medications in this category include: terbutaline, hexoprenaline, ritodrine, salbutamol/albuterol, etc. and are usually administered by intravenous drip in a hospital setting and sometimes as oral tablets. Side effects include headaches and an increased heart rate.
Nifedipine is a calcium channel blocker typically used to treat high blood pressure. It is also very efficient at suppressing uterine contractions, which is why some doctors use it to prevent a premature birth. Nifedipine is both available as oral tablets and injection. Its most frequent side-effect is an increased heart rate.
Nifedipine is both available as oral tablets and injection. Its most frequent side-effect is an increased heart rate.
Atosiban is an oxytocin receptor agonist which acts as a successful tocolytic (inhibits uterine contractions). It is typically given intravenously to prevent a threatened miscarriage and stop premature labor, in a hospital setting.
Nitroglycerine is a vasodilator commonly used for treating heart conditions. It can also be used as a local transdermal patch, to relax the uterus and improve blood flow to the pregnancy.
Magnesium sulphate used to be a more popular choice for treating a threatened miscarriage, as well as premature labor, however its use is now reduced to just a few countries. Due to its risks to both the mother and the baby and the lack of sufficient evidence supporting its efficiency, it is usually replaced by other therapeutic options nowadays.
Possible ComplicationsA threatened miscarriage can sometimes bring on additional complications.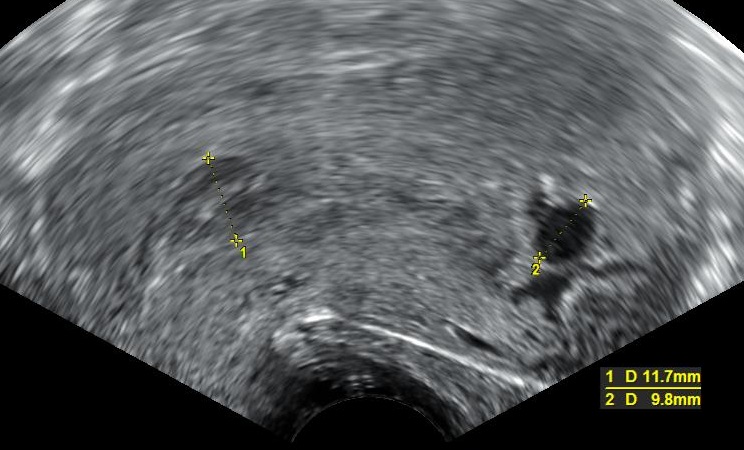
The most common complication are subchorionic hematomas, which are blood clots or blood collections that form between the uterine wall and the gestational membranes of the pregnancy. They are a rather common finding on first and second trimester ultrasound, but it does suggest a bleeding from behind the placenta so they need to be monitored carefully. When a retroplacental hematoma forms right behind the placenta, it could cause a placental abruption (which is when a part of the placenta detaches from the uterus). This is a serious complication that needs medical attention.
Ultrasound shows a large subchorionic hematoma (SCH) next to the gestational sac
In around half of the cases of threatened miscarriage, the bleeding and cramping unfortunately progress to a complete or partial miscarriage. This is more often the case in the first trimester, if the pregnancy has stopped developing and the embryo presents with no heartbeat on the ultrasound.
Occasionally during the second or third trimester, prolonged bleeding, uterine contractions or a local infection causing the threatened miscarriage might lead to PPROM (preterm premature rupture of membranes). This is when the ‘water’ breaks much too early in the pregnancy. The rupture of membranes may or may not be followed by a miscarriage or premature delivery. If the pregnancy remains in the uterus and no infection complicates it, there might still be hope for its continuation, even when the PPROM happens before the pregnancy is viable (before 24 weeks).
Other conditions sometimes associated with a threatened miscarriage are premature birth, intrauterine growth restriction of the fetus and low birth weight.
Natural remedies for Threatened MiscarriageAlthough it’s not recommended by all fertility specialists, bed rest can be helpful in some cases. There are women (including myself) who have spend the majority of their pregnancies in full bed rest, at home or in the hospital. So if you are dealing with vaginal bleeding and cramping during pregnancy and bed rest seems to help, listen to what your body is telling you and lie down for as long as you need. Physical activity can stimulate the muscles in the whole body and therefore increase uterine cramping and contractions as well. Also, standing or sitting can further increase the pressure on the cervix.
So if you are dealing with vaginal bleeding and cramping during pregnancy and bed rest seems to help, listen to what your body is telling you and lie down for as long as you need. Physical activity can stimulate the muscles in the whole body and therefore increase uterine cramping and contractions as well. Also, standing or sitting can further increase the pressure on the cervix.
- Increase your daily water intake. More water in the blood will help dilute the hormones that sustain uterine contractions, such as oxytocin. Reversely, dehydration can increase oxytocin concentrations in the blood and trigger more contractions.
- You may benefit from over-the-counter Magnesium supplements, since Magnesium is a natural muscle relaxant. In one study, expecting women who took Magnesium supplements had overall fewer pregnancy complications. Many forms of supplements are available, which include Magnesium citrate, Magnesium malate and Magnesium gluconate.
 Magnesium oxide, despite being the most popular form, is very poorly absorbed.
Magnesium oxide, despite being the most popular form, is very poorly absorbed. - Prenatal multivitamin supplements were found to reduce the number of early and late miscarriages in certain medical studies. In these studies, multivitamins were statistically more efficient at lowering miscarriage rate than any isolated vitamin supplement.
- More recent medical research has pointed to a link between low blood Vitamin D levels and first trimester miscarriage risk. A Vitamin D supplement could help prevent or at least lower the risk of pregnancy loss.
Miscarriage | Pregnancy Birth and Baby
The loss of a baby through miscarriage can be very distressing. A miscarriage generally occurs for reasons outside your control and nothing can be done to prevent or stop it from happening. Most women who have had a miscarriage will go on to have a healthy pregnancy in the future.
What is a miscarriage?
A miscarriage is the loss of your baby before 20 weeks of pregnancy. The loss of a baby after 20 weeks is called a stillbirth.
The loss of a baby after 20 weeks is called a stillbirth.
Up to 1 in 5 confirmed pregnancies end in miscarriage before 20 weeks, but many other women miscarry without having realised they are pregnant.
Common signs of miscarriage include:
- cramping tummy pain, similar to period pain
- vaginal bleeding
If you think you are having a miscarriage, see your doctor or go to your local emergency department.
Many women experience vaginal spotting in the first trimester that does not result in pregnancy loss.
What are the types of miscarriage?
There are several types of miscarriage — threatened, inevitable, complete, incomplete or missed.
Other types of pregnancy loss include an ectopic pregnancy, molar pregnancy and a blighted ovum.
Threatened miscarriage
When your body is showing signs that you might miscarry, that is called a 'threatened miscarriage'. You may have light vaginal bleeding or lower abdominal pain. It can last days or weeks and the cervix is still closed.
It can last days or weeks and the cervix is still closed.
The pain and bleeding may resolve and you can go on to have a healthy pregnancy and baby. Or things may get worse and you go on to have a miscarriage.
There is rarely anything a doctor, midwife or you can do to prevent a miscarriage. In the past bed rest was recommended, but there is no scientific proof that this helps at this stage.
Inevitable miscarriage
Inevitable miscarriages can come after a threatened miscarriage or without warning. There is usually a lot more vaginal bleeding and strong lower stomach cramps. During the miscarriage your cervix opens and the developing fetus will come away in the bleeding.
Complete miscarriage
A complete miscarriage has taken place when all the pregnancy tissue has left your uterus. Vaginal bleeding may continue for several days. Cramping pain much like labour or strong period pain is common — this is the uterus contracting to empty.
If you have miscarried at home or somewhere else with no health workers present, you should have a check-up with a doctor or midwife to make sure the miscarriage is complete.
Incomplete miscarriage
Sometimes, some pregnancy tissue will remain in the uterus. Vaginal bleeding and lower abdominal cramping may continue as the uterus continues trying to empty itself. This is known as an 'incomplete miscarriage'.
Your doctor or midwife will need to assess whether or not a short procedure called a ‘dilatation of the cervix and curettage of the uterus’ (often known as a ‘D&C’) is necessary to remove any remaining pregnancy tissue. This is an important medical procedure done in an operating theatre.
Missed miscarriage
Sometimes, the fetus has died but stayed in the uterus. This is known as a 'missed miscarriage'.
If you have a missed miscarriage, you may have a brownish discharge. Some of the symptoms of pregnancy, such as nausea and tiredness, may have faded. You might have noticed nothing unusual. You may be shocked to have a scan and find the fetus has died.
If this happens, you should discuss treatment and support options with your doctor.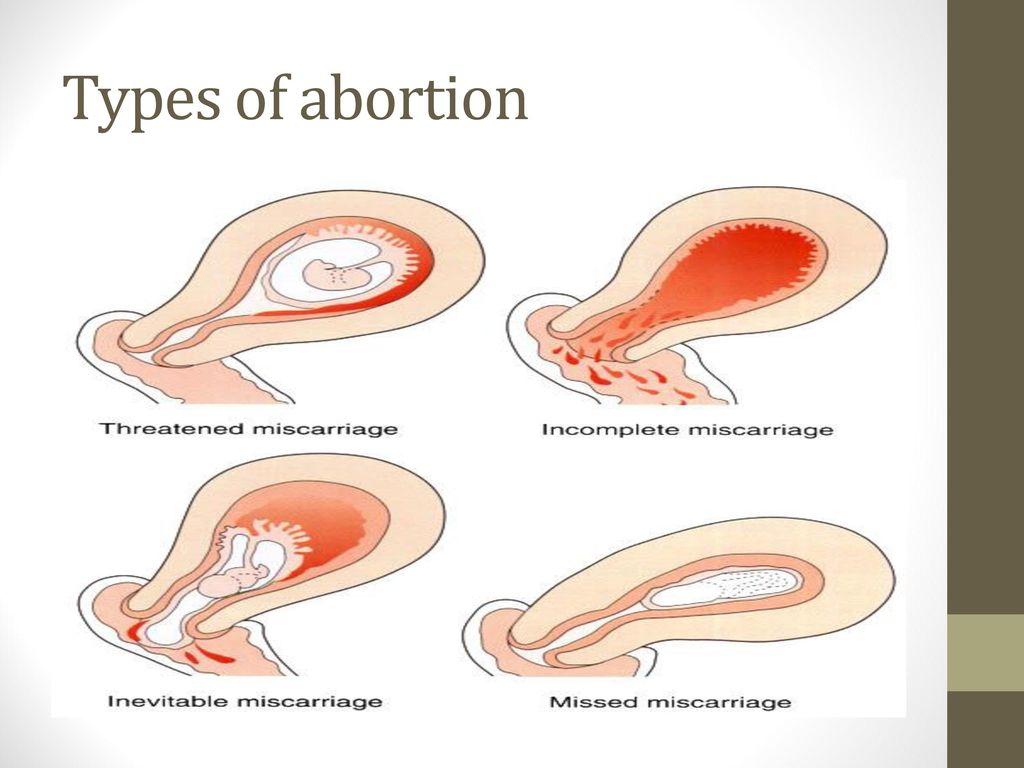
Recurrent miscarriage
A small number of women have repeated miscarriages. If this is your third or more miscarriage in a row, it’s best to discuss this with your doctor who may be able to investigate the causes, and refer you to a specialist.
A miscarriage can occur suddenly or over a number of weeks. The symptoms are usually vaginal bleeding and lower tummy pain. It is important to see your doctor or go to the emergency department if you have signs of a miscarriage.
The most common sign of a miscarriage is vaginal bleeding, which can vary from light red or brown spotting to heavy bleeding. If it is very early in the pregnancy, you may think that you have your period.
Other signs may include:
- cramping pain in your lower tummy, which can vary from period-like pain to strong labour-like contractions
- passing fluid from your vagina
- passing of blood clots or pregnancy tissue from your vagina
What really happens during a miscarriage?
WARNING — This article contains some graphic descriptions of what you might see during a miscarriage.
What should I do if I think I’m having a miscarriage?
If you are concerned that you are having a miscarriage, call your doctor or midwife for advice and support.
Keep in mind that many women experience vaginal spotting in the first trimester of pregnancy that does not result in a miscarriage.
If you are alone, consider calling your partner or a friend for help and support.
If you have very heavy bleeding, strong pain or feel unwell, call triple zero (000) or have someone take you to your nearest emergency department.
How is a miscarriage managed?
Unfortunately, nothing can prevent a miscarriage from happening once it has begun. What happens now depends on your own health and what is happening to you.
Each approach has benefits and risks. You should discuss these with your doctor.
Expectant or natural management
Also called ‘watch and wait’, expectant management may be recommended in early pregnancy. This involves going home and waiting until the pregnancy tissue has passed from your womb by itself. This can happen quickly, or it may take a few weeks.
This can happen quickly, or it may take a few weeks.
Medical management
You may be offered medication that speeds up the passing of the pregnancy tissue. You may be asked to stay in hospital until the tissue has passed, or you may be advised to go home.
Surgical management
You may be advised to have a form of minor surgery called a 'dilatation and curettage' (also called a D&C or a curette). This procedure is often recommended if you have heavy bleeding, significant pain or signs of infection. It may also be recommended if expectant or medical management has failed. You may also decide that you prefer this option.
This procedure is done under general anaesthesia in an operating theatre. It takes 5-10 minutes once you are asleep. The doctor opens the cervix and removes the remaining pregnancy tissue.
How is a miscarriage treated?
Once it is confirmed that you are having a miscarriage, your doctor may offer or recommend treatment. There are many options.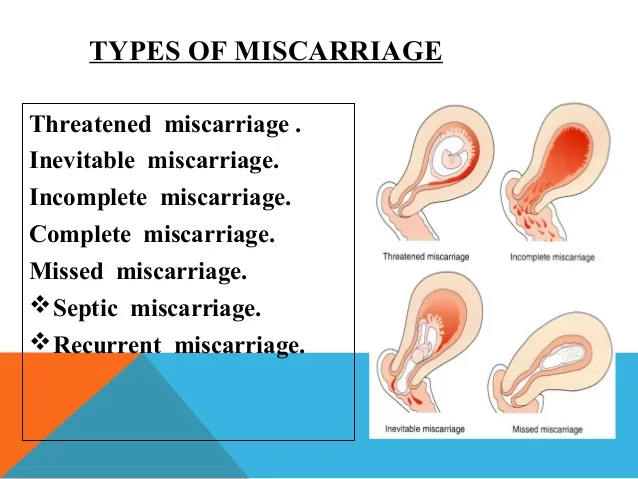 All have benefits and risks — discuss these with your doctor.
All have benefits and risks — discuss these with your doctor.
If the miscarriage is complete
If it seems the miscarriage is complete, you should still see your doctor for a check-up. You may be advised to have an ultrasound to make sure your uterus is empty.
If you go to hospital
If you go to your hospital’s emergency department, you will be seen first by a triage nurse, who will assess how urgently you need to be seen by a doctor. Depending on your symptoms, you will either be taken in to see a doctor immediately, or you will be asked to wait.
If you are waiting to be seen and your symptoms become worse or you feel like you need to go to the toilet, let the staff know immediately.
What happens if I miscarry at home?
Some women miscarry at home before they have a chance to see their doctor or get to the hospital.
If this happens, then:
- use pads to manage the bleeding
- if you can, save any pregnancy tissue that you pass, as your doctor may recommend it is tested to see why your miscarriage happened
- take medications such as paracetamol if you have pain
- rest
- call your doctor or midwife
There is a chance you may see your baby in the tissue that you pass, but often the baby is too small to recognise, or may not be found at all. It is normal to want to look at the remains, but you may decide you do not want to. There is no right or wrong thing to do.
It is normal to want to look at the remains, but you may decide you do not want to. There is no right or wrong thing to do.
Some women miscarry while on the toilet. This can also happen if you are out and about, or in hospital. There is no right or wrong way to handle this.
Why do miscarriages happen?
Many women wonder if their miscarriage was their fault. In most cases, a miscarriage has nothing to do with anything you have or have not done. There is no evidence that exercising, stress, working or having sex causes a miscarriage.
Most parents do not ever find out the exact cause. However, it is known that miscarriages often happen because the baby fails to develop properly, usually due to a chromosomal abnormality that was spontaneous, not inherited.
Occasionally, miscarriage is caused by:
- hormonal abnormalities
- immune system and blood clotting problems
- medical conditions such as thyroid problems or diabetes
- severe infections causing high fevers (not common colds)
- physical problems with your womb or cervix
What are the risk factors for miscarriage?
Women are more likely to have miscarriages if they:
- are older
- smoke
- drink alcohol in the first trimester
- drink too much caffeine in coffee, tea or energy drinks
- have had several previous miscarriages
Can you prevent a miscarriage?
Living healthily — no cigarettes, no alcohol and little to no caffeine — can decrease your risk of miscarriage.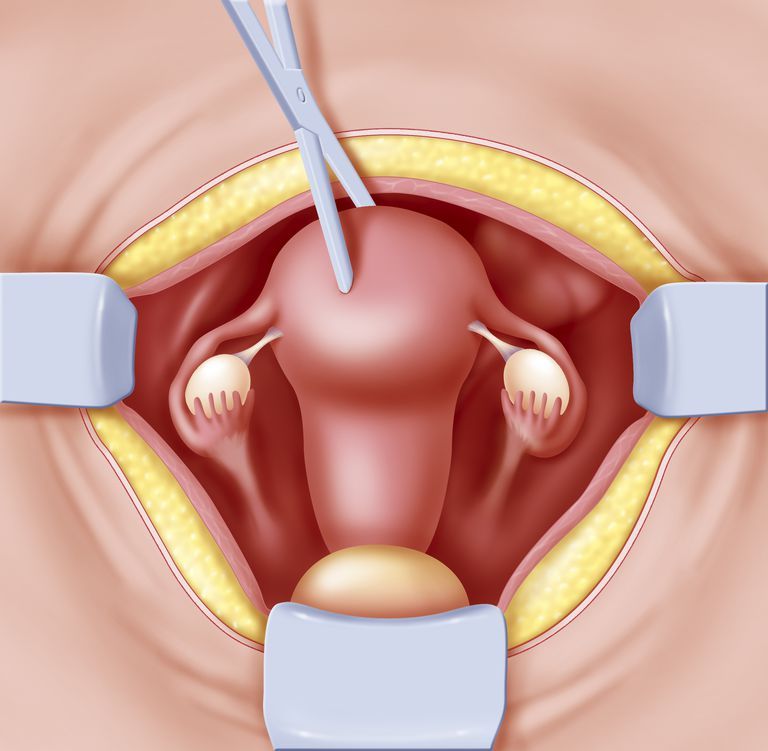 It’s a good idea to avoid contact with people who have a serious infectious illness when you’re pregnant.
It’s a good idea to avoid contact with people who have a serious infectious illness when you’re pregnant.
Who can I talk to for advice and support?
Talk to your doctor or midwife for information and advice on what do and how to look after yourself if you experience a miscarriage.
Your hospital should be able to provide details of available support services, such as bereavement support.
SANDS is an independent organisation that provides support for miscarriage, stillbirth and newborn death. You can call them on 1300 072 637 or visit www.sands.org.au.
You can also call Pregnancy, Birth and Baby on 1800 882 436, 7am to midnight (AET) to speak to a maternal child health nurse for advice and emotional support.
Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call. Available 7am to midnight (AET), 7 days a week.
Learn more here about the development and quality assurance of healthdirect content.
Spontaneous abortion (miscarriage)
If the pregnancy is terminated naturally before the fetus reaches gestational age, this is called a spontaneous abortion or miscarriage. More than half of miscarriages occur no later than 12 weeks of gestation due to fetal abnormalities. The rest falls on the period up to 20 weeks and is associated with pathologies of pregnancy. If the pregnancy is terminated in the second half, it is called preterm labor.
Spontaneous abortion, otherwise known as miscarriage, is one of the most common complications during pregnancy, accounting for 10-20% of diagnosed pregnancies, and is the rejection of a fetus weighing no more than 500 grams. and less than 22 weeks. Unfortunately, with such indicators, the fetus is not viable. Usually 80% of the total number of spontaneous abortions occurs before the 12th week of pregnancy.
Types of spontaneous abortion
1. Threat of miscarriage - characterized by mild uterine cramps, pulling pain in the lower abdomen and sometimes mild bloody discharge from the vagina.
2. A miscarriage that has begun - is characterized by more severe pain and profuse bleeding. At the same time, the tone of the uterus is slightly increased, and the internal os is closed.
3. Inevitable miscarriage - accompanied by dilatation of the cervix - a fetal egg can be distinguished - with profuse bleeding and severe cramps in the lower abdomen.
4. Incomplete miscarriage - part of the fetus comes out. The bleeding is so profuse that it can lead to the death of a woman.
5. Completed miscarriage - the fetal egg and the fetus itself are completely out. After that, the bleeding and spasms stop.
The etiology of miscarriage is due to many factors. Among them:
- genetic disorders;
- previous induced abortions;
- too little time has passed since the previous pregnancy;
- inflammatory infections in the mother, endocrine disorders;
- blood conflict between mother and fetus;
- taking hormonal contraceptives and certain medications;
- smoking during pregnancy and drinking alcohol;
- unknown causes.
To prevent miscarriage, it is necessary to give up bad habits, not to have abortions and to be regularly examined by a doctor.
Spontaneous abortion begins with the appearance of cramping, drawing pains, similar to pain during menstruation. Then bleeding from the uterus begins. At first, the discharge is slight or moderate, and then, after detachment of the fetal egg, abundant discharge with bloody clots begins. The appearance of these symptoms requires urgent hospitalization.
After examining a woman in a hospital, having determined the degree of detachment of the embryo, one of the following diagnoses will be made:
- the threat of pregnancy - detachment is only outlined or is completely insignificant. In this case, the pregnancy can be saved;
- a miscarriage that has begun - detachment is already quite decent with a pronounced pain syndrome. And in this case, the fetus can be saved;
- abortion in progress - detachment with displacement progresses, labor-like contractions begin.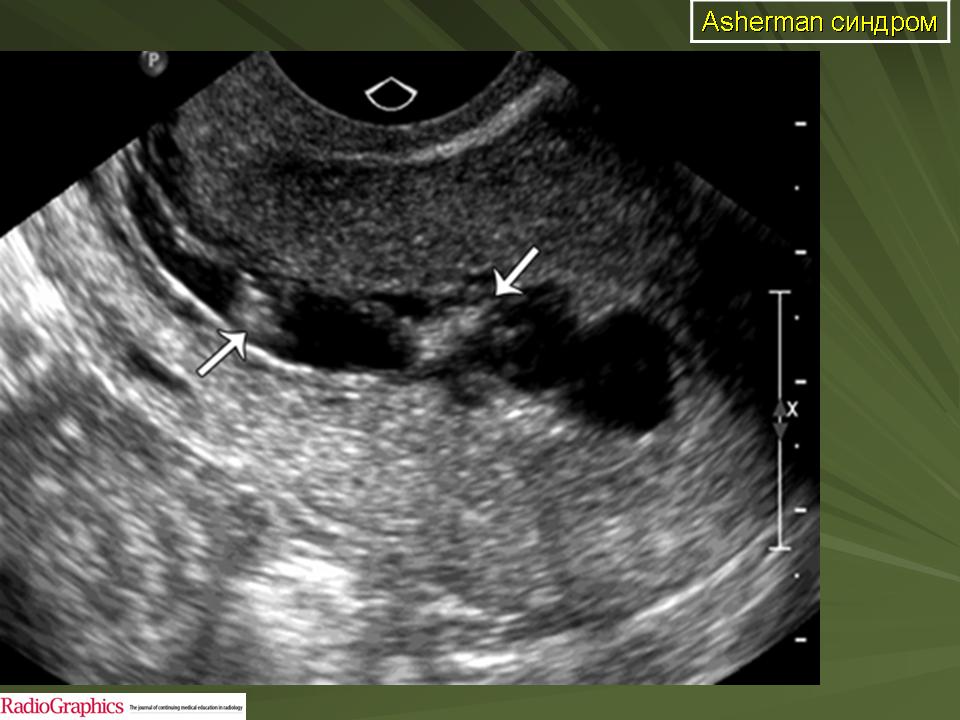 Pregnancy cannot be saved, cleaning is required;
Pregnancy cannot be saved, cleaning is required;
- incomplete miscarriage - independent exit of a part of the fetus and membranes, curettage is necessary for the final curettage of the uterus;
- late abortion - premature delivery of an unviable baby.
After a spontaneous abortion, it is recommended to take a short break in planning and take preventive measures to avoid recurrence.
In case of repeated miscarriage, a thorough comprehensive examination is necessary to determine the causes of miscarriage and eliminate them.
A miscarriage is a severe psychological trauma, especially during the first pregnancy. But do not give up, with a competent approach to planning and bearing, the next pregnancy will certainly end with the appearance of a long-awaited baby.
Causes of spontaneous abortion
1. Doctors call various chromosomal pathologies one of the main reasons: monosomy, autosomal trisomies, polyploidy. They account for 82-88% of spontaneous miscarriages.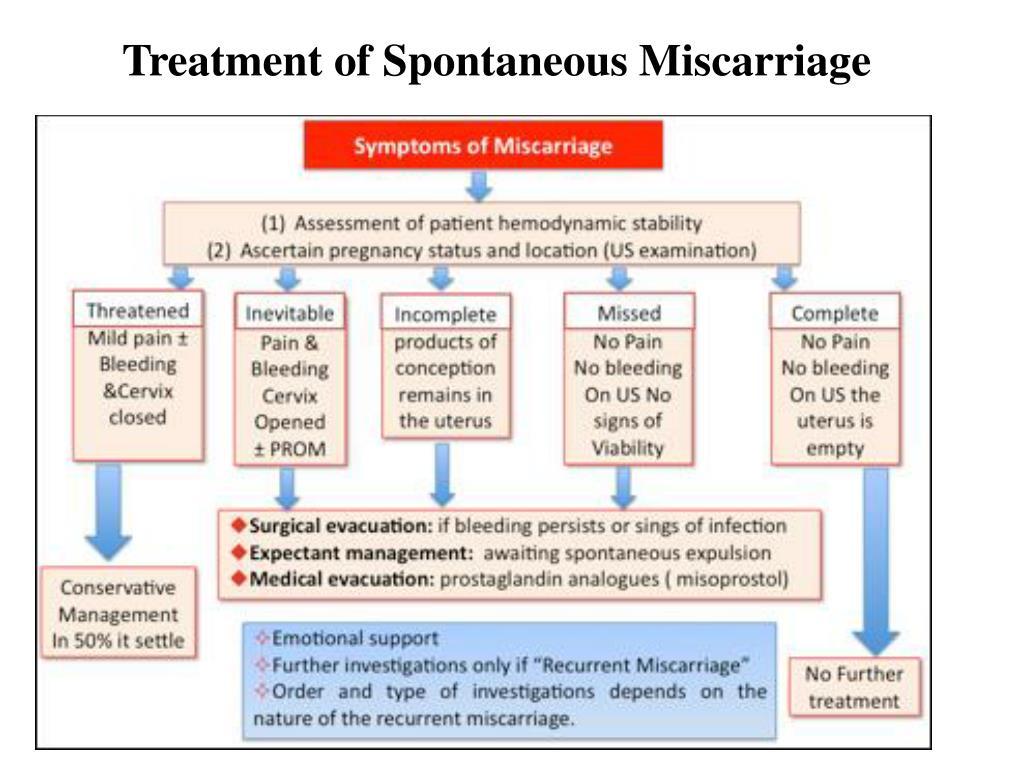
2. The second most common cause is disorders in the female genital area: endometritis - inflammation of the uterine mucosa - preventing the implantation of the fetal egg and its development and polycystic ovaries.
3. Hormonal disorders, namely progesterone deficiency.
4. Chronic diseases - uncontrolled diabetes mellitus, high blood pressure.
5. Viral infections rubella, chlamydia and others.
Treatment
In case of severe blood loss, ultrasound is performed to determine the viability of the fetus and rule out an ectopic pregnancy. A woman is prescribed bed rest and is treated with antispasmodic drugs to relax the uterine myometrium and stop bleeding.
If doctors still diagnose a spontaneous abortion that has begun, then the actions are reduced either to expectant tactics (within 2-6 weeks the fetal egg should come out by itself), or to prescribing drugs that accelerate the delivery of the fetus, or to vacuum aspiration (medical abortion ).
What is a spontaneous miscarriage and how does it happen? It's unpleasant and painful. But why is this happening and how to avoid such situations in the future? Find out more about this later.
What is it?
Early miscarriage is the death of an embryo or fetus in the womb before the 22nd week of pregnancy. It is usually caused by genetic breakdowns, pathologies, injuries or stress. Such a nuisance is quite common and approximately 15-20% of all successful conceptions can end in miscarriage.
What are the signs of a miscarriage?
To understand what's going on, you need to understand what a miscarriage looks like. The most common symptom is profuse bleeding with clots. Sometimes they can be mild at first, and then quite large. You should monitor your condition and if at least a slight bleeding has begun, you should immediately consult a doctor.
Sometimes a miscarriage can start suddenly. But it happens that before this there may be small pulling pains in the lower abdomen, lower back, smearing brown discharge.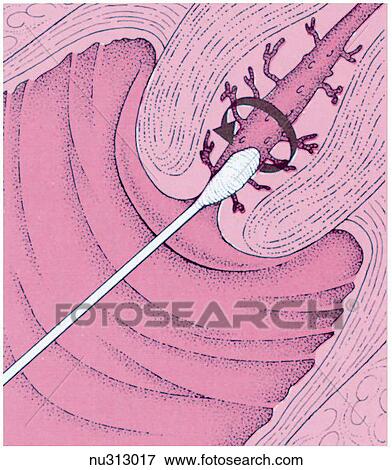
Women may not immediately realize that they have a miscarriage. Especially if the delay is only a few days, and the test was not done, then you might think that your period just started.
But usually a woman who already knows about her pregnancy remembers how a spontaneous miscarriage occurs forever. In most cases, this is profuse bleeding with blood clots, mucus and severe pain in the abdomen. If you do not immediately take action, you may experience chills, fever, the skin will become pale. The patient may even lose consciousness. If a woman does not immediately see a doctor or call an ambulance, she may even die from blood loss, as sometimes such bleeding is incredibly serious.
Spontaneous miscarriage can also have symptoms such as nausea, vomiting, frequent urination, dizziness, weakness,
What can cause an early miscarriage?
Why does it happen that a miscarriage occurs? Here you can name many reasons, but in each case, studies are carried out, the patient takes tests.
The causes of spontaneous abortion may be as follows in the first trimester:
- Increased contractile activity of the uterus, which literally "pushes" the fetus.
- Genetic abnormalities in the fetus. Sometimes this happens once in one woman, as a result of genetic "breakdowns". And it happens that the whole thing is in the genes of the future father and mother, and therefore it is necessary to look for problems together with a geneticist.
- Deficiency of the hormone progesterone. This is the so-called "pregnancy hormone". If it is not enough, then it is appointed additionally.
- Immunological disorders that prevent normal development of the embryo.
- Intoxication.
- In the second trimester, the causes of miscarriage may be slightly different:
- Uterine fibroids.
- Adhesions in the pelvic organs.
- Polyps in the uterus that prevent the embryo from developing normally.
- Endometriosis, which causes connective tissue to grow outside the uterus.
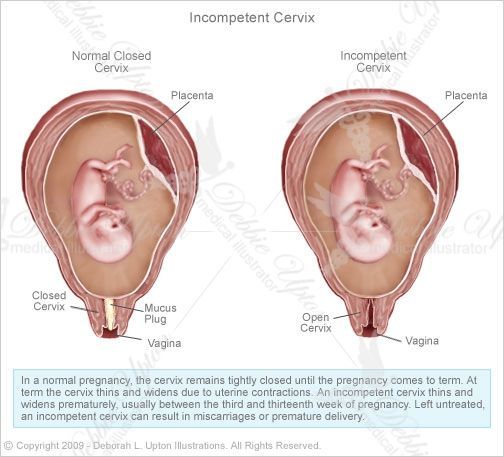
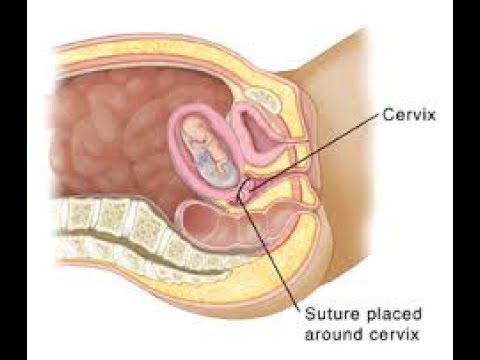
- Pathology of the cervix, namely an open cervix, which does not allow carrying a child and giving birth at term.
- Infections that can cross the placenta and cause fetal death.
- Some chronic diseases of the mother.
But besides this, there may be many other specific reasons that are individual for each woman. For example, hard physical work, activities in hazardous enterprises, severe stress and anxiety can also cause spontaneous abortion. The threat of spontaneous miscarriage occurs in many women, but not everyone can have an abortion. Much depends on the state of health, immunity, even emotional state.
What types of miscarriage can there be?
There are several types of spontaneous abortions:
- Early (up to 12 weeks)
- Late (13-22 weeks).
Some other types can also be distinguished:
- Threatened miscarriage. It is manifested by slight pains in the abdomen, spotting spotting, the muscles of the uterus are quite active.
 But at the same time, the cervix is closed.
But at the same time, the cervix is closed. - Incipient miscarriage. There is detachment of the fetal egg, bloody discharge. The cervix is closed, but the internal os is open.
- Abortion in progress. The fertilized egg comes out of the uterus, it is in the cervical canal. Severe pain and bleeding begin.
- Incomplete abortion. Part of the egg may come out of the uterus, and part may still be in it. In this case, there is severe bleeding, abdominal pain, shock may develop
- Complete abortion. With it, the fetal egg completely leaves the uterus. This is a "mini childbirth", while there is a slight bleeding, abdominal pain.
- Missed abortion. With it, the fetal egg remains in the uterus. In this case, the fetus is already dead. Such an egg can remain inside a woman for some time, her condition worsens, signs of pregnancy disappear.
Also, such miscarriages can be divided into several types:
- Interrupted biochemical pregnancy.
 It happens for 1-3 weeks. But a woman usually perceives it as the beginning of menstruation.
It happens for 1-3 weeks. But a woman usually perceives it as the beginning of menstruation. - Spontaneous miscarriage (up to 22 weeks).
- Preterm birth (after 22 weeks).
What cannot cause a miscarriage
Spontaneous abortion can happen to every woman. But there are certain risk factors that by themselves cannot cause a miscarriage, but can be provocateurs:
- Smoking.
- Alcohol abuse.
- Some disease (diabetes mellitus, high blood pressure).
- Age over 35.
Diagnosing a miscarriage
In order to accurately understand that a spontaneous abortion has occurred, it is necessary to correctly diagnose it. To do this, you should:
- Analyze the patient's complaints. Usually this is bleeding, pain and cramps in the abdomen, poor general health, pallor of the skin, fever.
- Perform a gynecological examination. Carry out palpation of the uterus, examination of the cervix, external pharynx.
- Perform colpocytological examination.
- They test for specific hormones.
- Ultrasound of the pelvic organs is performed.
If such miscarriages occur frequently, the cause must be investigated. To do this, conduct a variety of studies, consultations with geneticists, endocrinologists and other specialists.
How to treat?
How to treat spontaneous miscarriage depends on the type of miscarriage. If it is threatening and has begun, then the following should be done:
- The woman should be in the hospital.
- A diet that contains all essential minerals and trace elements.
- The patient must remain in bed.
- Sedative drugs and drugs that relax the muscles of the uterus should be given.
- If an abortion is "in progress", then all measures must be taken to stop the bleeding.
- If the abortion is complete and incomplete, then everything “unnecessary” that is in the uterus should be removed.
 For this, scraping can be used.
For this, scraping can be used. - If there is a missed abortion, then sometimes expectant tactics are used, when they are waiting for everything to “come out of the uterus by itself”. And sometimes they do scraping.
- Also, sometimes with a missed pregnancy, expectant management can be used, especially for nulliparous women. Then after about 4-6 weeks a spontaneous miscarriage can occur. Sometimes drug treatment is used, in which special pills are used to help complete the pregnancy. And sometimes they do surgical curettage.
In any case, abortion should not be left to chance, it is necessary to consult a doctor who will choose the treatment tactics.
What are the consequences?
Spontaneous miscarriage in early pregnancy usually carries certain risks. The consequences of spontaneous miscarriage can be different:
- Severe bleeding, pain.
- Infertility.
- But the most difficult and life-threatening miscarriages are those that a woman causes herself, at home.
 If they are not treated and the consequences are not eliminated, then they can end in the death of a woman.
If they are not treated and the consequences are not eliminated, then they can end in the death of a woman.
Usually, if the patient has been provided with quality medical care, there are practically no complications. After about 10 days, the bleeding stops, and after 4 weeks, the woman begins her regular menstruation.
Is there any prevention?
Pregnancy after spontaneous miscarriage can occur and be quite successful. But first you need to establish the cause of the abortion. If these are genetic problems, endocrine pathologies, troubles with the blood or uterus, then special treatment is necessary. But there are general recommendations that will help reduce the risk of miscarriages:
- After a termination of pregnancy, a woman needs to have a good rest, gain strength, drink a course of vitamins, possibly oral contraceptives, prescribed by a doctor. The next pregnancy is best planned in about 6 months.
- Maintain a healthy lifestyle.