How to help child with tonsillitis
Tonsillitis - Diagnosis and treatment
Diagnosis
Your child's doctor will start with a physical exam that will include:
- Using a lighted instrument to look at your child's throat and likely his or her ears and nose, which also may be sites of infection
- Checking for a rash known as scarlatina, which is associated with some cases of strep throat
- Gently feeling (palpating) your child's neck to check for swollen glands (lymph nodes)
- Listening to his or her breathing with a stethoscope
- Checking for enlargement of the spleen (for consideration of mononucleosis, which also inflames the tonsils)
Throat swab
With this simple test, the doctor rubs a sterile swab over the back of your child's throat to get a sample of secretions. The sample will be checked in the clinic or in a lab for streptococcal bacteria.
Many clinics are equipped with a lab that can get a test result within a few minutes. However, a second more reliable test is usually sent out to a lab that can often return results within several hours or a couple of days.
If the rapid in-clinic test comes back positive, then your child almost certainly has a bacterial infection. If the test comes back negative, then your child likely has a viral infection. Your doctor will wait, however, for the more reliable out-of-clinic lab test to determine the cause of the infection.
Complete blood cell count (CBC)
Your doctor may order a CBC with a small sample of your child's blood. The result of this test, which can often be completed in a clinic, produces a count of the different types of blood cells. The profile of what's elevated, what's normal or what's below normal can indicate whether an infection is more likely caused by a bacterial or viral agent. A CBC is not often needed to diagnose strep throat. However, if the strep throat lab test is negative, the CBC may be needed to help determine the cause of tonsillitis.
More Information
- Complete blood count (CBC)
Treatment
At-home care
Whether tonsillitis is caused by a viral or bacterial infection, at-home care strategies can make your child more comfortable and promote better recovery.
If a virus is the expected cause of tonsillitis, these strategies are the only treatment. Your doctor won't prescribe antibiotics. Your child will likely be better within seven to 10 days.
At-home care strategies to use during the recovery time include the following:
- Encourage rest. Encourage your child to get plenty of sleep.
- Provide adequate fluids. Give your child plenty of water to keep his or her throat moist and prevent dehydration.
- Provide comforting foods and beverage. Warm liquids — broth, caffeine-free tea or warm water with honey — and cold treats like ice pops can soothe a sore throat.
- Prepare a saltwater gargle.
 If your child can gargle, a saltwater gargle of 1/2 teaspoon (2.5 milliliters) of table salt to 8 ounces (237 milliliters) of warm water can help soothe a sore throat. Have your child gargle the solution and then spit it out.
If your child can gargle, a saltwater gargle of 1/2 teaspoon (2.5 milliliters) of table salt to 8 ounces (237 milliliters) of warm water can help soothe a sore throat. Have your child gargle the solution and then spit it out. - Humidify the air. Use a cool-air humidifier to eliminate dry air that may further irritate a sore throat, or sit with your child for several minutes in a steamy bathroom.
- Offer lozenges. Children older than age 4 can suck on lozenges to relieve a sore throat.
- Avoid irritants. Keep your home free from cigarette smoke and cleaning products that can irritate the throat.
-
Treat pain and fever. Talk to your doctor about using ibuprofen (Advil, Children's Motrin, others) or acetaminophen (Tylenol, others) to minimize throat pain and control a fever. Low fevers without pain do not require treatment.
Unless aspirin is prescribed by a doctor to treat a particular disease, children and teenagers should not take aspirin.
 Aspirin use by children to treat symptoms of cold or flu-like illnesses has been linked to Reye's syndrome, a rare but potentially life-threatening condition.
Aspirin use by children to treat symptoms of cold or flu-like illnesses has been linked to Reye's syndrome, a rare but potentially life-threatening condition.
Antibiotics
If tonsillitis is caused by a bacterial infection, your doctor will prescribe a course of antibiotics. Penicillin taken by mouth for 10 days is the most common antibiotic treatment prescribed for tonsillitis caused by group A streptococcus. If your child is allergic to penicillin, your doctor will prescribe an alternative antibiotic.
Your child must take the full course of antibiotics as prescribed even if the symptoms go away completely. Failure to take all of the medication as directed may result in the infection worsening or spreading to other parts of the body. Not completing the full course of antibiotics can, in particular, increase your child's risk of rheumatic fever and serious kidney inflammation.
Talk to your doctor or pharmacist about what to do if you forget to give your child a dose.
Surgery
Surgery to remove tonsils (tonsillectomy) may be used to treat frequently recurring tonsillitis, chronic tonsillitis or bacterial tonsillitis that doesn't respond to antibiotic treatment. Frequent tonsillitis is generally defined as:
- At least seven episodes in the preceding year
- At least five episodes a year in the past two years
- At least three episodes a year in the past three years
A tonsillectomy may also be performed if tonsillitis results in difficult-to-manage complications, such as:
- Obstructive sleep apnea
- Breathing difficulty
- Swallowing difficulty, especially meats and other chunky foods
- An abscess that doesn't improve with antibiotic treatment
A tonsillectomy is usually done as an outpatient procedure, unless your child is very young, has a complex medical condition or if complications arise during surgery. That means your child should be able to go home the day of the surgery. A complete recovery usually takes seven to 14 days.
A complete recovery usually takes seven to 14 days.
More Information
- Tonsillectomy
Preparing for your appointment
If your child is experiencing a sore throat, difficulty swallowing or other symptoms that may indicate tonsillitis, you'll likely start with a visit to your family doctor or your child's pediatrician. You may be referred to a specialist in ear, nose and throat disorders.
Your doctor is likely to ask you a number of questions about your child's condition. Be prepared to answer the following questions:
- When did the symptoms begin?
- If your child has had a fever, what was his or her temperature?
- Does he or she have difficulty swallowing foods, or does it hurt to swallow?
- Does anything improve symptoms, such as an over-the-counter pain reliever or warm liquids?
- Has your child been diagnosed with tonsillitis or strep throat before? If so, when?
- Do symptoms seem to affect his or her sleep?
- Has your child been exposed to anyone known to have strep throat?
Questions you may want to ask your doctor include the following:
- How long will it take to get test results?
- What is the best course of treatment?
- Should I be concerned with how frequently my child is getting tonsillitis?
- When can my child go back to school or resume other activities?
By Mayo Clinic Staff
Related
Associated Procedures
Products & Services
Tonsillitis (for Parents) - Nemours KidsHealth
What Is Tonsillitis?
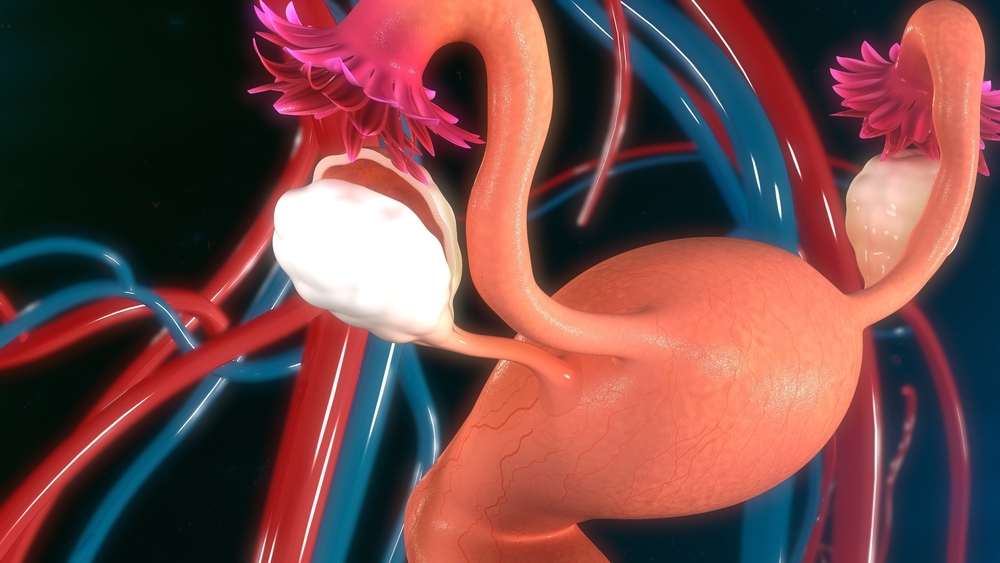
Tonsillitis (tahn-suh-LYE-tus) is an infection of the tonsils. Tonsils are lumps of tissue on both sides of the back of the throat that help the immune system protect the body from infections. Inflamed tonsils get red and swollen and can cause a sore throat.
Tonsils are lumps of tissue on both sides of the back of the throat that help the immune system protect the body from infections. Inflamed tonsils get red and swollen and can cause a sore throat.
What Are the Signs & Symptoms of Tonsillitis?
Inflamed tonsils look red and swollen, and may be covered with a yellow or whitish coating or spots. A child with tonsillitis may have:
- a sore throat
- fever
- bad breath
- swollen glands (lymph nodes) in the neck
- trouble swallowing
- stomachache
- headache
What Causes Tonsillitis?
Tonsillitis is usually caused by a
virussuch as:
- adenovirus
- the flu
- Epstein-Barr virus (mono)
Bacteria also can cause it, most commonly group A streptococcus (strep throat). Rarely, tonsillitis can be caused by something other than an infection.
Who Gets Tonsillitis?
Anyone at any age can get tonsillitis. Strep throat is most common in kids and teens ages 5 to 15.
Strep throat is most common in kids and teens ages 5 to 15.
How Is Tonsillitis Diagnosed?
Health care providers will ask about symptoms and do an exam. They'll check the inside of the mouth, the back of the throat, and the neck.
A health care provider may use a soft cotton swab to gently collect a sample from the tonsils and back of the throat. This can be:
- tested quickly with a rapid strep test that gives an answer within minutes
- sent to a lab for a throat culture, which takes a few days
If the rapid strep test doesn't show signs of strep, the health care provider will depend on the culture for a final diagnosis.
It's important to call your health care provider if your child has tonsillitis symptoms.
How Is Tonsillitis Treated?
Treatment depends on whether the tonsillitis is caused by:
- a virus, in which case the body will fight the infection on its own
- bacteria, in which case the doctor will prescribe an antibiotic.
 Help your child take the antibiotic exactly as directed. This helps symptoms clear up quickly and prevents spreading the infection to others.
Help your child take the antibiotic exactly as directed. This helps symptoms clear up quickly and prevents spreading the infection to others.It's important to finish the entire prescription — even if your child feels better in a few days — or the infection could come back. This also helps prevent a more serious health problem that streptococcus can cause, called rheumatic fever, which can damage the heart.
Rarely, a health care provider might recommend a tonsillectomy (surgery to remove the tonsils) if a child's tonsils get infected a lot or are so big they make it hard to breathe at night. Tonsillectomy used to be very commonly done. Now, experts use guidelines to decide if tonsil removal is the best treatment. In general, tonsillectomy may be considered if a child has seven sore throat episodes in 1 year, five episodes 2 years in a row, or three episodes 3 years in a row.
How Can I Help My Child Feel Better?
Make sure that your child drinks lots of fluids and gets plenty of rest. If swallowing hurts, serve liquids and soft foods. Some kids prefer warm drinks, like soup or sweetened tea. Other kids like the feel of cold or frozen foods on their throat, such as milkshakes, smoothies, ice pops, or ice cream. Older kids can suck on hard candies or throat lozenges.
If swallowing hurts, serve liquids and soft foods. Some kids prefer warm drinks, like soup or sweetened tea. Other kids like the feel of cold or frozen foods on their throat, such as milkshakes, smoothies, ice pops, or ice cream. Older kids can suck on hard candies or throat lozenges.
You can give a pain reliever, such as acetaminophen or ibuprofen, for throat pain. Don't give aspirin or other products that contain aspirin, though, because these can put kids at risk for Reye syndrome.
Is Tonsillitis Contagious?
Tonsillitis is contagious. Sneezing and coughing can pass the germ causing the illness from one person to the next.
Can Tonsillitis Be Prevented?
Try to keep kids away from anyone who already has tonsillitis or a sore throat, and make sure everyone in your family washes their hands well and often.
If someone in the family has tonsillitis, keep their drinking glasses and eating utensils separate, and wash them in hot, soapy water. They should not share food, drinks, napkins, or towels with other family members. Give them a new toothbrush after they're treated and no longer contagious.
Give them a new toothbrush after they're treated and no longer contagious.
What Else Should I Know?
If the sore throat gets worse, especially on one side, call your doctor. This could be a sign of a peritonsillar abscess. This happens when bacteria spread from the tonsil to the space around it and fill it with pus. Other signss of an abscess include fever, headache, earache, drooling, or a muffled voice. Treating an abscess might be done in a hospital, possibly with surgery to drain the infection. Tonsillectomy may be considered for kids who get multiple peritonsillar abscesses.
Chronic tonsillitis in children - Treatment and diagnosis at the EMC clinic in Moscow
Chronic tonsillitis is a long-term inflammation of the palatine tonsils. The reasons for the development of chronic tonsillitis in children may be hereditary predisposition, the presence of a viral or bacterial infection, allergies, decreased immunity (general and local), suffered in the past and possibly not completely cured tonsillitis (acute tonsillitis), as well as the presence of a source of infection in the cavity mouth, such as dental caries.
Getting on the tonsil, the infection lingers in the lacunae - internal crypts of the lymphoid tissue. In a healthy tonsil, the lacunae are always clean, healthy lymphoid tissue captures the incoming infectious agent and disinfects it, passing on air or food. A chronically diseased tonsil cannot do this. The tonsil captures the infection, but is not able to neutralize it, so it accumulates in the gaps. In the lacunae, which in chronic tonsillitis are modified (expanded and deformed), food debris, bacteria, fungi enter, leukocytes aspire to the same place, calcium salts fall out, which form the so-called purulent-caseous plugs and become an even greater source of infection. Therefore, chronic tonsillitis is usually accompanied by a concomitant violation of any body functions.
Symptoms of acute and chronic tonsillitis
-
Angina: sore throat, significant fever, deterioration of health, malaise, enlargement of regional lymph nodes. With fungal or bacterial tonsillitis, plaque may appear on the tonsils, viral tonsillitis is manifested by blistering rashes and swelling of the tonsils.

-
Chronic tonsillitis is often asymptomatic and is manifested only by exacerbations in the form of tonsillitis. Symptoms can be periodic discomfort or sore throat, bad breath, general weakness, malaise, excessive sweating, prolonged fever up to 37.1 - 37.3 degrees C, enlargement of regional lymph nodes.
In chronic tonsillitis, the functions of "target organs" (heart, kidneys, joints) may be impaired. Often this is manifested by pain in the joints, arthritis, arthrosis, endocarditis, pericarditis, myocarditis and other diseases. Therefore, chronic tonsillitis can be attributed to systemic diseases. If chronic tonsillitis occurs with complications (the so-called decompensated form of tonsillitis), surgery is recommended (removal of the tonsil).
With angina, a dangerous local complication is a peritonsillar abscess, when pus from the tonsils enters the surrounding tissues and an abscess forms. This is an acute and very painful condition in which it is contraindicated to self-medicate, you must immediately consult a doctor.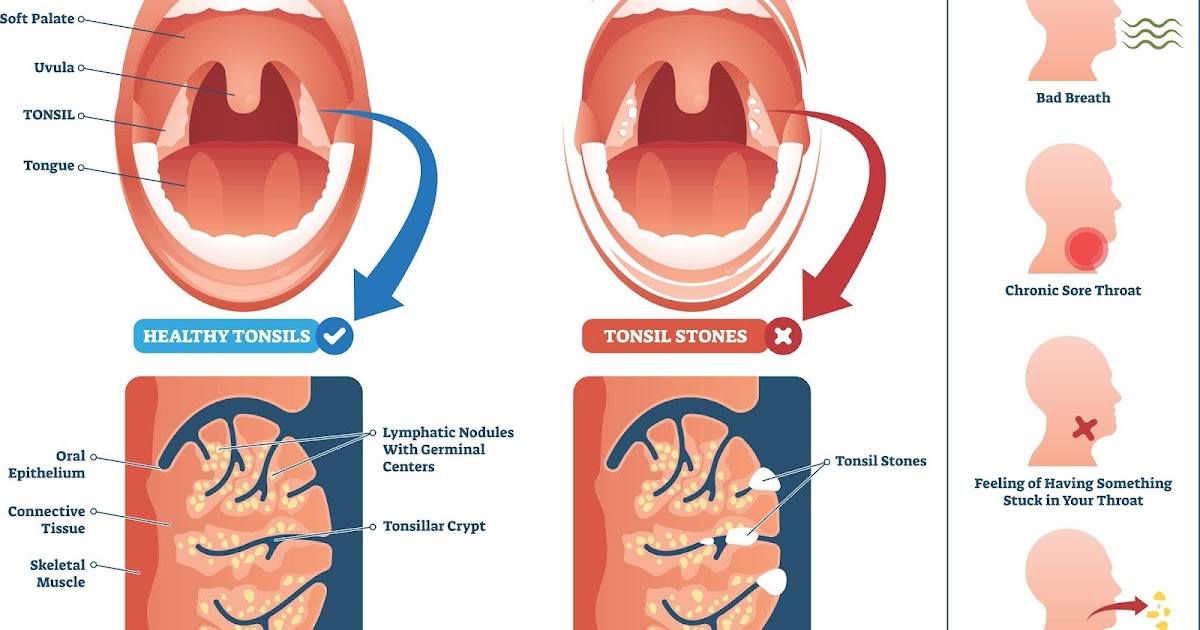 Peritonsillar abscess is an indication for the removal of the tonsils to exclude recurrence.
Peritonsillar abscess is an indication for the removal of the tonsils to exclude recurrence.
Diagnosis of chronic tonsillitis
Visual inspection. Signs of chronic tonsillitis are adhesions of the tonsils with arches, the presence of discharge (purulent, caseous) in the lacunae, a change in the shape and size of the anterior and posterior tonsil arches (Preobrazhensky's symptom), reddening of the arches (Gizet's symptom), their swelling (Zak's Symptom), an increase in regional lymph nodes.
Laboratory blood tests: ESR, leukocyte formula, markers of streptococcal infection (C-reactive protein, antistreptolysin O).
Diagnosis of angina
Visual inspection. Redness and swelling of the tonsils, the presence of plaque, enlargement and soreness of regional lymph nodes.
Laboratory tests: culture from the surface of tonsil plaques for flora and sensitivity to antibiotics, a smear for diphtheria (to exclude or confirm its presence), a clinical blood test.
Chronic tonsillitis in a child: treatment
In acute tonsillitis, antibiotic therapy is mandatory. Thus, not only the treatment of the tonsils is carried out, but the complications that often occur with angina are excluded. Local anti-inflammatory antibacterial or antiseptic therapy, analgesic treatment, antihistamines are recommended.
In chronic tonsillitis, conservative treatment consists in removing the contents from the lacunae of the tonsils (eg, gargling with antiseptic solutions, saline solutions; using local antiseptics in the form of lozenges and sprays). Conservative treatment is applied, as a rule, in courses. In addition, rinses with anti-inflammatory drugs, herbal infusions are prescribed. Physiotherapy is also used - ultraviolet irradiation and ultrasound on the submandibular region with anti-inflammatory drugs.
If conservative treatment fails, sore throats recur or signs of tonsillitis remain unchanged, surgical treatment is prescribed. If chronic tonsillitis is diagnosed, the tonsils are removed completely.
If chronic tonsillitis is diagnosed, the tonsils are removed completely.
At the European Medical Center, the child's tonsils are removed in a state of safe medication sleep, which relieves psychological discomfort and negative impressions from visiting the clinic. Simultaneously with the removal, the niche is coagulated, thereby 90% eliminates the risk of bleeding. Approximately one day after the operation, a small patient can leave the walls of the clinic.
Surgical treatment of childhood tonsillitis in the EMC Children's Clinic is carried out according to modern methods and protocols that have proven their effectiveness. To remove the tonsils, a radio wave knife, laser or high-frequency coagulation, bipolar tweezers are used. They can significantly reduce the length of stay in the hospital, significantly reduce the risk of postoperative bleeding and significantly reduce the period of complete recovery of the child after the intervention.
For medical reasons, EMC uses less radical methods: tonsillotomy, lacunotomy, ablation or fulguration of the tonsils, laser exposure.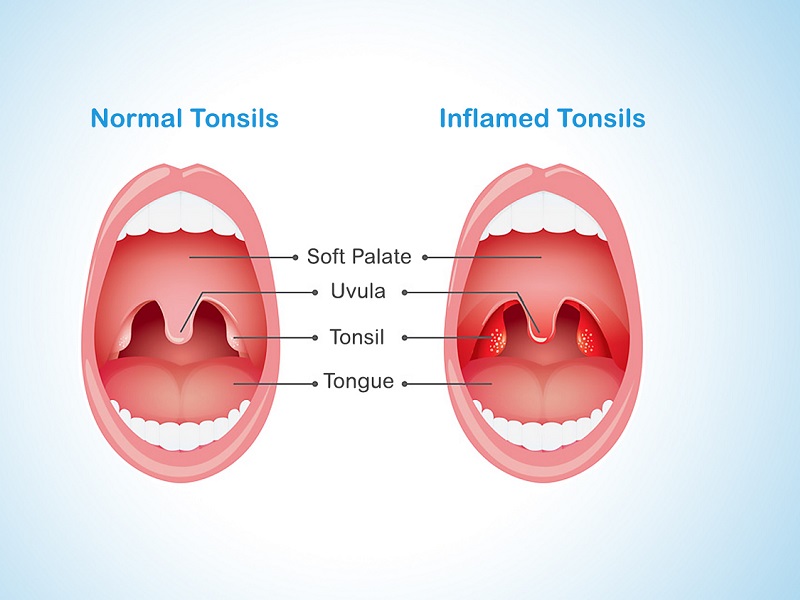 The decision on the most optimal method is made by the attending physician individually in each case, depending on the stage of the disease and the prevalence of the pathological process. If several options are suitable, the advantages of each of them are discussed with the parents of a small patient, the most optimal method is jointly selected.
The decision on the most optimal method is made by the attending physician individually in each case, depending on the stage of the disease and the prevalence of the pathological process. If several options are suitable, the advantages of each of them are discussed with the parents of a small patient, the most optimal method is jointly selected.
Tonsillitis signs and treatment in a child. Preparations.
Bacteria, viruses or fungus can cause tonsillitis in a child. It's contagious a disease in which the tonsils become inflamed. The most common causative agent acute tonsillitis is β-hemolytic streptococcus group A (GABHS, Streptococcus pyogenes), less often acute tonsillitis is caused by viruses (Adeno-Coxsackie, Epstein-Barr virus), group C and G streptococci, Neisseria gonorrhoeae, Corynebacterium diphtheriae, anaerobes and spirochetes, extremely rare chlamydia and mycoplasma. Viral forms of acute tonsillitis predominate in children in under 3 years of age (70–90%), after 5 years the number of bacterial forms increases (up to 30–50%). Streptococcal tonsillitis usually occurs in children aged 5–15 years, the greatest incidence is observed in the winter-spring period and early spring 1 .
Tonsillitis symptoms in children
It is important to notice the problem in time to avoid complications of the disease. Symptoms
appear approximately in the first two days 1 :
● Lethargy and weakness of the child;
● High temperature persists for several days (up to 39°C), the child is shivering and feverish;
● Headache;
● Child complains of severe sore throat when swallowing and yawning;
● There is an increase in lymph nodes, below the ear;
● The child begins to eat poorly and lose appetite, complains of nausea. May
be vomiting;
● Bad breath;
● Tonsils tend to enlarge and become red. May
purulent plaque will appear.
If a child has chronic tonsillitis, then you need to be especially careful.
Outside of exacerbation, chronic tonsillitis is accompanied by increased
fatigue, discomfort in the throat, dryness and sore throat. Several
Several
once a year, an exacerbation of the disease can be observed. Its symptoms are often similar to
acute form of tonsillitis.
Treatment of tonsillitis in children
Treatment of tonsillitis in children should be under constant supervision doctor. It is better not to self-medicate, as this can lead to complications.
During illness, the child needs to stay in bed and drink plenty of fluids. It is mandatory to prescribe a sparing diet, as well as compliance with the rules of oral hygiene. To relieve pain, rinsing with herbal infusions is often done. Often, sprays with an anti-inflammatory and analgesic component or rinses are included in the treatment. Topical therapy also includes lozenges such as Faringosept which have antimicrobial properties. If we talk about the treatment of chronic tonsillitis in a child, it is important to remember that treatment should be carried out both in the “calm” period and during exacerbations. If acute tonsillitis occurs, children are usually treated so:
If acute tonsillitis occurs, children are usually treated so:
● Rinsing with herbal infusions helps relieve pain. But eliminate the problem is impossible in this way, since only the symptoms are relieved;
● Anti-inflammatory drugs are used to improve the condition of the tonsils. sprays or lozenges;
●Sometimes the doctor advises to clean the tonsils - washing them from purulent plugs. This procedure is prescribed to a patient with frequent exacerbations of chronic tonsillitis, experiencing constant pain in the throat and lymph nodes in the neck. Often, washing the lacunae of the tonsils is the only way to save the tonsils and avoid a tonsillectomy (surgery to remove the tonsils). The procedure should be carried out outside the period of acute inflammation (tonsillitis).
To prevent frequent exacerbation of tonsillitis in a child, it is necessary to regularly strengthen the immune system. In the autumn and spring seasons, for prevention take vitamin C and gargle with infusions of calendula, chamomile or sage.