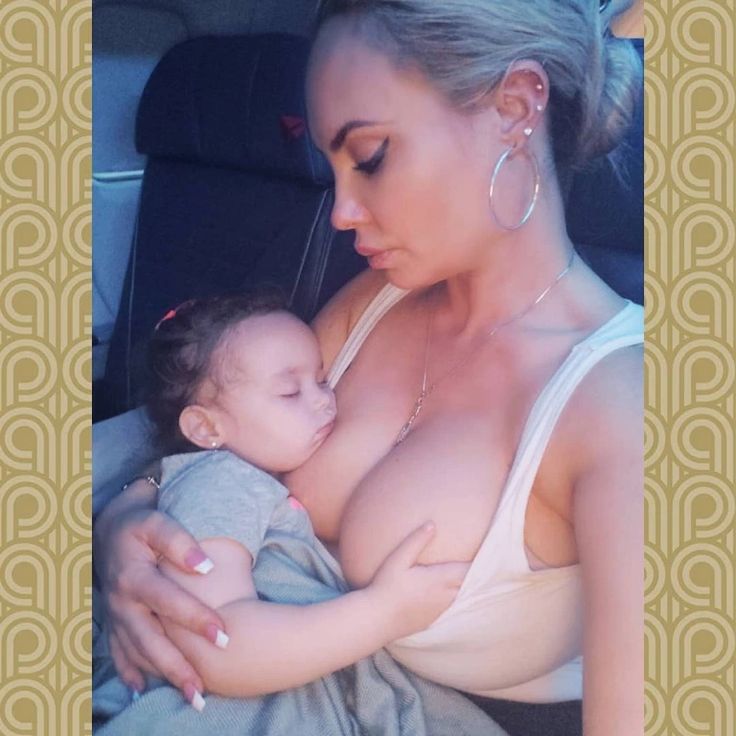
Mother baby breastfeeding
The Benefits of Breastfeeding for Both Mother and Baby
Written by Rebecca Buffum Taylor
Reviewed by Dan Brennan, MD on July 05, 2022
In this Article
- What is Breastfeeding?
- Signs Your Baby is Hungry
- Benefits of Breastfeeding for the Baby
- Breastfeeding Benefits for the Mother
- Will You Make Enough Milk to Breastfeed?
- What's the Best Position for Breastfeeding?
- How to Get Your Baby to 'Latch on' During Breastfeeding
- Tips for New Breastfeeding Moms
- Are There Medical Considerations With Breastfeeding?
- What Are Some Common Challenges With Breastfeeding?
- Where Can I Get Help With Breastfeeding?
What is Breastfeeding?
Breastfeeding is when you feed your baby breast milk, usually directly from your breast. It’s also called nursing. Making the decision to breastfeed is a personal matter. It's also one that's likely to draw opinions from friends and family.
Many medical experts, including the American Academy of Pediatrics (AAP) and the American College of Obstetricians and Gynecologists, strongly recommend breastfeeding exclusively (no formula, juice, or water) for 6 months. After the introduction of other foods, it recommends continuing to breastfeed through the baby’s first year of life.
How often you should breastfeed your baby depends on whether your baby prefers small, frequent meals or longer feedings. This will change as your baby grows. Newborns often want to feed every 2-3 hours. By 2 months, feeding every 3-4 hours is common, and by six months, most babies feed every 4-5 hours.
You and your baby are unique, and the decision to breastfeed is up to you.
Signs Your Baby is Hungry
One of the most common ways your baby will let you know they're hungry is to cry. Other signs your baby is ready to be fed include:
- Licking their lips or sticking out their tongue
- Rooting, which is moving their jaw, mouth, or head to look for your breast
- Putting their hand in their mouth
- Opening their mouth
- Fussiness
- Sucking on things
Benefits of Breastfeeding for the Baby
Breast milk provides the ideal nutrition for infants. It has a nearly perfect mix of vitamins, protein, and fat -- everything your baby needs to grow. And it's all provided in a form more easily digested than infant formula. Breast milk contains antibodies that help your baby fight off viruses and bacteria. Breastfeeding lowers your baby's risk of having asthma or allergies. Plus, babies who are breastfed exclusively for the first 6 months, without any formula, have fewer ear infections, respiratory illnesses, and bouts of diarrhea. They also have fewer hospitalizations and trips to the doctor.
It has a nearly perfect mix of vitamins, protein, and fat -- everything your baby needs to grow. And it's all provided in a form more easily digested than infant formula. Breast milk contains antibodies that help your baby fight off viruses and bacteria. Breastfeeding lowers your baby's risk of having asthma or allergies. Plus, babies who are breastfed exclusively for the first 6 months, without any formula, have fewer ear infections, respiratory illnesses, and bouts of diarrhea. They also have fewer hospitalizations and trips to the doctor.
Breastfeeding has been linked to higher IQ scores in later childhood in some studies. What's more, the physical closeness, skin-to-skin touching, and eye contact all help your baby bond with you and feel secure. Breastfed infants are more likely to gain the right amount of weight as they grow rather than become overweight children. The AAP says breastfeeding also plays a role in the prevention of SIDS (sudden infant death syndrome). It's been thought to lower the risk of diabetes, obesity, and certain cancers as well, but more research is needed.
The AAP says breastfeeding also plays a role in the prevention of SIDS (sudden infant death syndrome). It's been thought to lower the risk of diabetes, obesity, and certain cancers as well, but more research is needed.
Breastfeeding Benefits for the Mother
Breastfeeding burns extra calories, so it can help you lose pregnancy weight faster. It releases the hormone oxytocin, which helps your uterus return to its pre-pregnancy size and may reduce uterine bleeding after birth. There are continued benefits from breastfeeding beyond 1 year, and up to 2 years especially in the mother.Breastfeeding also lowers your risk of breast and ovarian cancer. It may lower your risk of osteoporosis, too.
Since you don't have to buy and measure formula, sterilize nipples, or warm bottles, it saves you time and money. It also gives you regular time to relax quietly with your newborn as you bond.
Will You Make Enough Milk to Breastfeed?
The first few days after birth, your breasts make an ideal "first milk." It's called colostrum. Colostrum is thick, yellowish, and there’s not a lot of it, but there's plenty to meet your baby's nutritional needs. Colostrum helps a newborn's digestive tract develop and prepare itself to digest breast milk.
Colostrum is the first phase of breast milk, which changes over time to give your baby the nutrition they need as they grow. The second phase is called transitional milk. You make this as your colostrum is gradually replaced with the third phase of breast milk, called mature milk.
You’ll start to make transitional milk a few days after birth. By 10 to 15 days after birth, you’ll make mature milk, which gives your baby all the nutrition they need.
Most babies lose a small amount of weight in the first 3 to 5 days after birth. This is unrelated to breastfeeding.
As your baby needs more milk and nurses more, your breasts respond by making more milk. Experts recommend trying to breastfeed exclusively (no formula, juice, or water) for 6 months. If you supplement with formula, your breasts might make less milk.
Experts recommend trying to breastfeed exclusively (no formula, juice, or water) for 6 months. If you supplement with formula, your breasts might make less milk.
Even if you breastfeed less than the recommended 6 months, it's better to breastfeed for a short time than no time at all. You can add solid food at 6 months but also continue to breastfeed if you want to keep producing milk.
Is your baby getting enough milk?
Many breastfeeding moms wonder whether their babies get enough milk for good nutrition. If your baby is getting enough breastmilk they should:
- Not lose more than 7% of their birth weight in the first few days after delivery
- Seem content for about 1-3 hours between feedings
- Have at least 6 diapers a day wet with very pale or clear pee by the time they are 7-10 days old
What's the Best Position for Breastfeeding?
The best position for you is the one where you and your baby are both comfortable and relaxed, and you don't have to strain to hold the position or keep nursing. Here are some common positions for breastfeeding your baby:
Here are some common positions for breastfeeding your baby:
- Cradle position. Rest the side of your baby's head in the crook of your elbow with their whole body facing you. Position your baby's belly against your body so they feel fully supported. Your other, "free" arm can wrap around to support your baby's head and neck -- or reach through your baby's legs to support the lower back.
- Football position. Line your baby's back along your forearm to hold your baby like a football, supporting the head and neck in your palm. This works best with newborns and small babies. It's also a good position if you're recovering from a cesarean birth and need to protect your belly from the pressure or weight of your baby.
- Side-lying position. This position is great for night feedings in bed. Side-lying also works well if you're recovering from an episiotomy, an incision to widen the vaginal opening during delivery. Use pillows under your head to get comfortable.
 Then snuggle close to your baby and use your free hand to lift your breast and nipple into your baby's mouth. Once your baby is correctly "latched on," support the head and neck with your free hand so there's no twisting or straining to keep nursing.
Then snuggle close to your baby and use your free hand to lift your breast and nipple into your baby's mouth. Once your baby is correctly "latched on," support the head and neck with your free hand so there's no twisting or straining to keep nursing. - Cross-cradle hold. Sit straight in a comfortable chair that has armrests. Hold your baby in the crook of your arm that's opposite the breast you will use to feed them. Support their head with your hand. Bring your baby across your body so your tummies face each other. Use your other hand to cup your breast in a U-shaped hold. Bring your baby's mouth to your breast and cradle them close, and don't lean forward.
- Laid-back position. This position, also called biological nurturing, is a lot like it sounds. It's meant to tap into the natural breastfeeding instincts you and your baby have. Lean back, but not flat, on a couch or bed. Have good support for your head and shoulders. Hold your baby so your entire fronts touch.
 Let your baby take any position they're comfortable in as long as their cheek rests near your breast. Help your baby latch on if they need it.
Let your baby take any position they're comfortable in as long as their cheek rests near your breast. Help your baby latch on if they need it.
How to Get Your Baby to 'Latch on' During Breastfeeding
Position your baby facing you, so your baby is comfortable and doesn't have to twist their neck to feed. With one hand, cup your breast and gently stroke your baby's lower lip with your nipple. Your baby's instinctive reflex will be to open the mouth wide. With your hand supporting your baby's neck, bring the mouth closer around your nipple, trying to center your nipple in the mouth above the tongue.
You'll know your baby is "latched on" correctly when both lips are pursed outward around your nipple. Your infant should have all of your nipple and most of the areola, which is the darker skin around your nipple, in their mouth. While you may feel a slight tingling or tugging, breastfeeding should not be painful. If your baby isn't latched on correctly and nursing with a smooth, comfortable rhythm, gently nudge your pinky between your baby's gums to break the suction, remove your nipple, and try again. Good "latching on" helps prevent sore nipples.
Good "latching on" helps prevent sore nipples.
Tips for New Breastfeeding Moms
Some things help you prepare for breastfeeding:
- Get regular prenatal care to help you avoid preterm birth.
- Tell your doctor you plan to breastfeed and ask what support the facility you plan to deliver in offers to help you breastfeed after birth.
- Take a breastfeeding class.
- Ask your doctor to connect you with a lactation consultant, who can teach you breastfeeding basics and help you if have issues.
- Talk to your doctor about any health conditions you have or medications you take that could interfere with breastfeeding.
- Tell your doctor and hospital health care providers that you want to breastfeed as soon as possible after delivery.
- Talk to friends who breastfeed or join a support group for breastfeeding.
- Stock up on the supplies you need for breastfeeding, such as nursing bras and other items.
These tips, called the ABCs of breastfeeding, will help you and your baby get comfortable with the process:
- Awareness.
 Watch for your baby's signs of hunger, and breastfeed whenever your baby is hungry. This is called "on demand" feeding. The first few weeks, you may be nursing eight to 12 times every 24 hours. Hungry infants move their hands toward their mouths, make sucking noises or mouth movements, or move toward your breast. Don't wait for your baby to cry. That's a sign their too hungry.
Watch for your baby's signs of hunger, and breastfeed whenever your baby is hungry. This is called "on demand" feeding. The first few weeks, you may be nursing eight to 12 times every 24 hours. Hungry infants move their hands toward their mouths, make sucking noises or mouth movements, or move toward your breast. Don't wait for your baby to cry. That's a sign their too hungry. - Be patient. Breastfeed as long as your baby wants to nurse each time. Don't hurry your infant through feedings. Infants typically breastfeed for 10 to 20 minutes on each breast.
- Comfort. This is key. Relax while breastfeeding, and your milk is more likely to "let down" and flow. Get yourself comfortable with pillows as needed to support your arms, head, and neck, and a footrest to support your feet and legs before you begin to breastfeed.
Are There Medical Considerations With Breastfeeding?
In a few situations, breastfeeding could cause a baby harm. Here are some reasons you should not breastfeed:
Here are some reasons you should not breastfeed:
- You are HIV positive. You can pass the HIV virus to your infant through breast milk.
- You have active, untreated tuberculosis.
- You're receiving chemotherapy for cancer.
- You're using an illegal drug, such as cocaine or marijuana.
- Your baby has a rare condition called galactosemia and cannot tolerate the natural sugar, called galactose, in breast milk.
- You're taking certain prescription medications, such as some drugs for migraine headaches, Parkinson's disease, or arthritis.
Talk with your doctor before starting to breastfeed if you're taking prescription drugs of any kind. Your doctor can help you make an informed decision based on your particular medication.
Having a cold or flu should not prevent you from breastfeeding. Breast milk won't give your baby the illness and may even give antibodies to your baby to help fight off the illness.
Breast milk won't give your baby the illness and may even give antibodies to your baby to help fight off the illness.
Also, the AAP suggests that -- starting at 4 months of age -- exclusively breastfed infants, and infants who are partially breastfed and receive more than half of their daily feedings as human milk, should be supplemented with oral iron. This should continue until foods with iron, such as iron-fortified cereals, are introduced in the diet. The AAP recommends checking iron levels in all children at age 1.
Discuss supplementation of both iron and vitamin D with your pediatrician. Your doctor can guide you on recommendations about the proper amounts for both your baby and you, when to start, and how often the supplements should be taken.
What Are Some Common Challenges With Breastfeeding?
- Sore nipples. You can expect some soreness in the first weeks of breastfeeding. Make sure your baby latches on correctly, and use one finger to break the suction of your baby's mouth after each feeding.
 That will help prevent sore nipples. If you still get sore, be sure you nurse with each breast fully enough to empty the milk ducts. If you don't, your breasts can become engorged, swollen, and painful. Holding ice or a bag of frozen peas against sore nipples can temporarily ease discomfort. Keeping your nipples dry and letting them "air dry" between feedings helps, too. Your baby tends to suck more actively at the start. So begin feedings with the less-sore nipple.
That will help prevent sore nipples. If you still get sore, be sure you nurse with each breast fully enough to empty the milk ducts. If you don't, your breasts can become engorged, swollen, and painful. Holding ice or a bag of frozen peas against sore nipples can temporarily ease discomfort. Keeping your nipples dry and letting them "air dry" between feedings helps, too. Your baby tends to suck more actively at the start. So begin feedings with the less-sore nipple. - Dry, cracked nipples. Avoid soaps, perfumed creams, or lotions with alcohol in them, which can make nipples even more dry and cracked. You can gently apply pure lanolin to your nipples after a feeding, but be sure you gently wash the lanolin off before breastfeeding again. Changing your bra pads often will help your nipples stay dry. And you should use only cotton bra pads.
- Worries about producing enough milk. A general rule of thumb is that a baby who's wetting six to eight diapers a day is most likely getting enough milk.
 It's best not to supplement your breast milk with formula, and never give your infant plain water. Your body needs the frequent, regular demand of your baby's nursing to keep producing milk. Some women mistakenly think they can't breastfeed if they have small breasts. But small-breasted women can make milk just as well as large-breasted women. Good nutrition, plenty of rest, and staying well hydrated all help, too.
It's best not to supplement your breast milk with formula, and never give your infant plain water. Your body needs the frequent, regular demand of your baby's nursing to keep producing milk. Some women mistakenly think they can't breastfeed if they have small breasts. But small-breasted women can make milk just as well as large-breasted women. Good nutrition, plenty of rest, and staying well hydrated all help, too. - Pumping and storing milk. You can get breast milk by hand or pump it with a breast pump. It may take a few days or weeks for your baby to get used to breast milk in a bottle. So begin practicing early if you're going back to work. Breast milk can be safely used within 2 days if it's stored in a refrigerator. You can freeze breast milk for up to 6 months. Don't warm up or thaw frozen breast milk in a microwave. That will destroy some of its immune-boosting qualities, and it can cause fatty portions of the breast milk to become super hot.
 Thaw breast milk in the refrigerator or in a bowl of warm water instead.
Thaw breast milk in the refrigerator or in a bowl of warm water instead. - Inverted nipples. An inverted nipple doesn't poke forward when you pinch the areola, the dark skin around the nipple. A lactation consultant -- a specialist in breastfeeding education -- can give you tips that allow women with inverted nipples to breastfeed successfully.
- Breast engorgement. Breast fullness is natural and healthy. It happens as your breasts become full of milk, staying soft and pliable. But breast engorgement means the blood vessels in your breast have become congested. This traps fluid in your breasts and makes them feel hard, painful, and swollen. Alternate heat and cold, for instance using ice packs and hot showers, to relieve mild symptoms. It can also help to release your milk by hand or use a breast pump.
- Blocked ducts. A single sore spot on your breast, which may be red and hot, can signal a plugged milk duct.
 This can often be relieved by warm compresses and gentle massage over the area to release the blockage. More frequent nursing can also help.
This can often be relieved by warm compresses and gentle massage over the area to release the blockage. More frequent nursing can also help. - Breast infection (mastitis). This occasionally results when bacteria enter the breast, often through a cracked nipple after breastfeeding. If you have a sore area on your breast along with flu-like symptoms, fever, and fatigue, call your doctor. Antibiotics are usually needed to clear up a breast infection, but you can most likely continue to breastfeed while you have the infection and take antibiotics. To relieve breast tenderness, apply moist heat to the sore area four times a day for 15 to 20 minutes each time.
- Stress. Being overly anxious or stressed can interfere with your let-down reflex. That's your body's natural release of milk into the milk ducts. It's triggered by hormones released when your baby nurses.
 It can also be triggered just by hearing your baby cry or thinking about your baby. Stay as relaxed and calm as possible before and during nursing -- it can help your milk let down and flow more easily. That, in turn, can help calm and relax your infant.
It can also be triggered just by hearing your baby cry or thinking about your baby. Stay as relaxed and calm as possible before and during nursing -- it can help your milk let down and flow more easily. That, in turn, can help calm and relax your infant. - Premature babies may not be able to breastfeed right away. In some cases, mothers can release breast milk and feed it through a bottle or feeding tube.
- Warning signs. Breastfeeding is a natural, healthy process. But call your doctor if:
- Your breasts become unusually red, swollen, hard, or sore.
- You have an unusual discharge or bleeding from your nipples.
- You're concerned your baby isn't gaining weight or getting enough milk.
Where Can I Get Help With Breastfeeding?
Images of mothers breastfeeding their babies make it look simple -- but some women need some help and coaching. It can come from a nurse, doctor, family member, or friend, and it helps mothers get over possible bumps in the road.
Reach out to friends, family, and your doctor with any questions you may have. Most likely, the women in your life have had those same questions.
The Benefits of Breastfeeding for Both Mother and Baby
Written by Rebecca Buffum Taylor
Reviewed by Dan Brennan, MD on July 05, 2022
In this Article
- What is Breastfeeding?
- Signs Your Baby is Hungry
- Benefits of Breastfeeding for the Baby
- Breastfeeding Benefits for the Mother
- Will You Make Enough Milk to Breastfeed?
- What's the Best Position for Breastfeeding?
- How to Get Your Baby to 'Latch on' During Breastfeeding
- Tips for New Breastfeeding Moms
- Are There Medical Considerations With Breastfeeding?
- What Are Some Common Challenges With Breastfeeding?
- Where Can I Get Help With Breastfeeding?
What is Breastfeeding?
Breastfeeding is when you feed your baby breast milk, usually directly from your breast. It’s also called nursing. Making the decision to breastfeed is a personal matter. It's also one that's likely to draw opinions from friends and family.
It’s also called nursing. Making the decision to breastfeed is a personal matter. It's also one that's likely to draw opinions from friends and family.
Many medical experts, including the American Academy of Pediatrics (AAP) and the American College of Obstetricians and Gynecologists, strongly recommend breastfeeding exclusively (no formula, juice, or water) for 6 months. After the introduction of other foods, it recommends continuing to breastfeed through the baby’s first year of life.
How often you should breastfeed your baby depends on whether your baby prefers small, frequent meals or longer feedings. This will change as your baby grows. Newborns often want to feed every 2-3 hours. By 2 months, feeding every 3-4 hours is common, and by six months, most babies feed every 4-5 hours.
You and your baby are unique, and the decision to breastfeed is up to you.
Signs Your Baby is Hungry
One of the most common ways your baby will let you know they're hungry is to cry. Other signs your baby is ready to be fed include:
Other signs your baby is ready to be fed include:
- Licking their lips or sticking out their tongue
- Rooting, which is moving their jaw, mouth, or head to look for your breast
- Putting their hand in their mouth
- Opening their mouth
- Fussiness
- Sucking on things
Benefits of Breastfeeding for the Baby
Breast milk provides the ideal nutrition for infants. It has a nearly perfect mix of vitamins, protein, and fat -- everything your baby needs to grow. And it's all provided in a form more easily digested than infant formula. Breast milk contains antibodies that help your baby fight off viruses and bacteria. Breastfeeding lowers your baby's risk of having asthma or allergies. Plus, babies who are breastfed exclusively for the first 6 months, without any formula, have fewer ear infections, respiratory illnesses, and bouts of diarrhea. They also have fewer hospitalizations and trips to the doctor.
They also have fewer hospitalizations and trips to the doctor.
Breastfeeding has been linked to higher IQ scores in later childhood in some studies. What's more, the physical closeness, skin-to-skin touching, and eye contact all help your baby bond with you and feel secure. Breastfed infants are more likely to gain the right amount of weight as they grow rather than become overweight children. The AAP says breastfeeding also plays a role in the prevention of SIDS (sudden infant death syndrome). It's been thought to lower the risk of diabetes, obesity, and certain cancers as well, but more research is needed.
Breastfeeding Benefits for the Mother
Breastfeeding burns extra calories, so it can help you lose pregnancy weight faster. It releases the hormone oxytocin, which helps your uterus return to its pre-pregnancy size and may reduce uterine bleeding after birth. There are continued benefits from breastfeeding beyond 1 year, and up to 2 years especially in the mother.Breastfeeding also lowers your risk of breast and ovarian cancer. It may lower your risk of osteoporosis, too.
There are continued benefits from breastfeeding beyond 1 year, and up to 2 years especially in the mother.Breastfeeding also lowers your risk of breast and ovarian cancer. It may lower your risk of osteoporosis, too.
Since you don't have to buy and measure formula, sterilize nipples, or warm bottles, it saves you time and money. It also gives you regular time to relax quietly with your newborn as you bond.
Will You Make Enough Milk to Breastfeed?
The first few days after birth, your breasts make an ideal "first milk." It's called colostrum. Colostrum is thick, yellowish, and there’s not a lot of it, but there's plenty to meet your baby's nutritional needs. Colostrum helps a newborn's digestive tract develop and prepare itself to digest breast milk.
Colostrum is the first phase of breast milk, which changes over time to give your baby the nutrition they need as they grow. The second phase is called transitional milk. You make this as your colostrum is gradually replaced with the third phase of breast milk, called mature milk.
You make this as your colostrum is gradually replaced with the third phase of breast milk, called mature milk.
You’ll start to make transitional milk a few days after birth. By 10 to 15 days after birth, you’ll make mature milk, which gives your baby all the nutrition they need.
Most babies lose a small amount of weight in the first 3 to 5 days after birth. This is unrelated to breastfeeding.
As your baby needs more milk and nurses more, your breasts respond by making more milk. Experts recommend trying to breastfeed exclusively (no formula, juice, or water) for 6 months. If you supplement with formula, your breasts might make less milk.
Even if you breastfeed less than the recommended 6 months, it's better to breastfeed for a short time than no time at all. You can add solid food at 6 months but also continue to breastfeed if you want to keep producing milk.
Is your baby getting enough milk?
Many breastfeeding moms wonder whether their babies get enough milk for good nutrition. If your baby is getting enough breastmilk they should:
If your baby is getting enough breastmilk they should:
- Not lose more than 7% of their birth weight in the first few days after delivery
- Seem content for about 1-3 hours between feedings
- Have at least 6 diapers a day wet with very pale or clear pee by the time they are 7-10 days old
What's the Best Position for Breastfeeding?
The best position for you is the one where you and your baby are both comfortable and relaxed, and you don't have to strain to hold the position or keep nursing. Here are some common positions for breastfeeding your baby:
- Cradle position. Rest the side of your baby's head in the crook of your elbow with their whole body facing you. Position your baby's belly against your body so they feel fully supported. Your other, "free" arm can wrap around to support your baby's head and neck -- or reach through your baby's legs to support the lower back.
- Football position. Line your baby's back along your forearm to hold your baby like a football, supporting the head and neck in your palm.
 This works best with newborns and small babies. It's also a good position if you're recovering from a cesarean birth and need to protect your belly from the pressure or weight of your baby.
This works best with newborns and small babies. It's also a good position if you're recovering from a cesarean birth and need to protect your belly from the pressure or weight of your baby. - Side-lying position. This position is great for night feedings in bed. Side-lying also works well if you're recovering from an episiotomy, an incision to widen the vaginal opening during delivery. Use pillows under your head to get comfortable. Then snuggle close to your baby and use your free hand to lift your breast and nipple into your baby's mouth. Once your baby is correctly "latched on," support the head and neck with your free hand so there's no twisting or straining to keep nursing.
- Cross-cradle hold. Sit straight in a comfortable chair that has armrests. Hold your baby in the crook of your arm that's opposite the breast you will use to feed them. Support their head with your hand. Bring your baby across your body so your tummies face each other.
 Use your other hand to cup your breast in a U-shaped hold. Bring your baby's mouth to your breast and cradle them close, and don't lean forward.
Use your other hand to cup your breast in a U-shaped hold. Bring your baby's mouth to your breast and cradle them close, and don't lean forward. - Laid-back position. This position, also called biological nurturing, is a lot like it sounds. It's meant to tap into the natural breastfeeding instincts you and your baby have. Lean back, but not flat, on a couch or bed. Have good support for your head and shoulders. Hold your baby so your entire fronts touch. Let your baby take any position they're comfortable in as long as their cheek rests near your breast. Help your baby latch on if they need it.
How to Get Your Baby to 'Latch on' During Breastfeeding
Position your baby facing you, so your baby is comfortable and doesn't have to twist their neck to feed. With one hand, cup your breast and gently stroke your baby's lower lip with your nipple. Your baby's instinctive reflex will be to open the mouth wide. With your hand supporting your baby's neck, bring the mouth closer around your nipple, trying to center your nipple in the mouth above the tongue.
You'll know your baby is "latched on" correctly when both lips are pursed outward around your nipple. Your infant should have all of your nipple and most of the areola, which is the darker skin around your nipple, in their mouth. While you may feel a slight tingling or tugging, breastfeeding should not be painful. If your baby isn't latched on correctly and nursing with a smooth, comfortable rhythm, gently nudge your pinky between your baby's gums to break the suction, remove your nipple, and try again. Good "latching on" helps prevent sore nipples.
Tips for New Breastfeeding Moms
Some things help you prepare for breastfeeding:
- Get regular prenatal care to help you avoid preterm birth.
- Tell your doctor you plan to breastfeed and ask what support the facility you plan to deliver in offers to help you breastfeed after birth.
- Take a breastfeeding class.
- Ask your doctor to connect you with a lactation consultant, who can teach you breastfeeding basics and help you if have issues.

- Talk to your doctor about any health conditions you have or medications you take that could interfere with breastfeeding.
- Tell your doctor and hospital health care providers that you want to breastfeed as soon as possible after delivery.
- Talk to friends who breastfeed or join a support group for breastfeeding.
- Stock up on the supplies you need for breastfeeding, such as nursing bras and other items.
These tips, called the ABCs of breastfeeding, will help you and your baby get comfortable with the process:
- Awareness. Watch for your baby's signs of hunger, and breastfeed whenever your baby is hungry. This is called "on demand" feeding. The first few weeks, you may be nursing eight to 12 times every 24 hours. Hungry infants move their hands toward their mouths, make sucking noises or mouth movements, or move toward your breast. Don't wait for your baby to cry. That's a sign their too hungry.

- Be patient. Breastfeed as long as your baby wants to nurse each time. Don't hurry your infant through feedings. Infants typically breastfeed for 10 to 20 minutes on each breast.
- Comfort. This is key. Relax while breastfeeding, and your milk is more likely to "let down" and flow. Get yourself comfortable with pillows as needed to support your arms, head, and neck, and a footrest to support your feet and legs before you begin to breastfeed.
Are There Medical Considerations With Breastfeeding?
In a few situations, breastfeeding could cause a baby harm. Here are some reasons you should not breastfeed:
- You are HIV positive. You can pass the HIV virus to your infant through breast milk.
- You have active, untreated tuberculosis.
- You're receiving chemotherapy for cancer.
- You're using an illegal drug, such as cocaine or marijuana.

- Your baby has a rare condition called galactosemia and cannot tolerate the natural sugar, called galactose, in breast milk.
- You're taking certain prescription medications, such as some drugs for migraine headaches, Parkinson's disease, or arthritis.
Talk with your doctor before starting to breastfeed if you're taking prescription drugs of any kind. Your doctor can help you make an informed decision based on your particular medication.
Having a cold or flu should not prevent you from breastfeeding. Breast milk won't give your baby the illness and may even give antibodies to your baby to help fight off the illness.
Also, the AAP suggests that -- starting at 4 months of age -- exclusively breastfed infants, and infants who are partially breastfed and receive more than half of their daily feedings as human milk, should be supplemented with oral iron. This should continue until foods with iron, such as iron-fortified cereals, are introduced in the diet. The AAP recommends checking iron levels in all children at age 1.
The AAP recommends checking iron levels in all children at age 1.
Discuss supplementation of both iron and vitamin D with your pediatrician. Your doctor can guide you on recommendations about the proper amounts for both your baby and you, when to start, and how often the supplements should be taken.
What Are Some Common Challenges With Breastfeeding?
- Sore nipples. You can expect some soreness in the first weeks of breastfeeding. Make sure your baby latches on correctly, and use one finger to break the suction of your baby's mouth after each feeding. That will help prevent sore nipples. If you still get sore, be sure you nurse with each breast fully enough to empty the milk ducts. If you don't, your breasts can become engorged, swollen, and painful. Holding ice or a bag of frozen peas against sore nipples can temporarily ease discomfort. Keeping your nipples dry and letting them "air dry" between feedings helps, too.
 Your baby tends to suck more actively at the start. So begin feedings with the less-sore nipple.
Your baby tends to suck more actively at the start. So begin feedings with the less-sore nipple. - Dry, cracked nipples. Avoid soaps, perfumed creams, or lotions with alcohol in them, which can make nipples even more dry and cracked. You can gently apply pure lanolin to your nipples after a feeding, but be sure you gently wash the lanolin off before breastfeeding again. Changing your bra pads often will help your nipples stay dry. And you should use only cotton bra pads.
- Worries about producing enough milk. A general rule of thumb is that a baby who's wetting six to eight diapers a day is most likely getting enough milk. It's best not to supplement your breast milk with formula, and never give your infant plain water. Your body needs the frequent, regular demand of your baby's nursing to keep producing milk. Some women mistakenly think they can't breastfeed if they have small breasts. But small-breasted women can make milk just as well as large-breasted women.
 Good nutrition, plenty of rest, and staying well hydrated all help, too.
Good nutrition, plenty of rest, and staying well hydrated all help, too. - Pumping and storing milk. You can get breast milk by hand or pump it with a breast pump. It may take a few days or weeks for your baby to get used to breast milk in a bottle. So begin practicing early if you're going back to work. Breast milk can be safely used within 2 days if it's stored in a refrigerator. You can freeze breast milk for up to 6 months. Don't warm up or thaw frozen breast milk in a microwave. That will destroy some of its immune-boosting qualities, and it can cause fatty portions of the breast milk to become super hot. Thaw breast milk in the refrigerator or in a bowl of warm water instead.
- Inverted nipples. An inverted nipple doesn't poke forward when you pinch the areola, the dark skin around the nipple. A lactation consultant -- a specialist in breastfeeding education -- can give you tips that allow women with inverted nipples to breastfeed successfully.

- Breast engorgement. Breast fullness is natural and healthy. It happens as your breasts become full of milk, staying soft and pliable. But breast engorgement means the blood vessels in your breast have become congested. This traps fluid in your breasts and makes them feel hard, painful, and swollen. Alternate heat and cold, for instance using ice packs and hot showers, to relieve mild symptoms. It can also help to release your milk by hand or use a breast pump.
- Blocked ducts. A single sore spot on your breast, which may be red and hot, can signal a plugged milk duct. This can often be relieved by warm compresses and gentle massage over the area to release the blockage. More frequent nursing can also help.
- Breast infection (mastitis). This occasionally results when bacteria enter the breast, often through a cracked nipple after breastfeeding. If you have a sore area on your breast along with flu-like symptoms, fever, and fatigue, call your doctor.
 Antibiotics are usually needed to clear up a breast infection, but you can most likely continue to breastfeed while you have the infection and take antibiotics. To relieve breast tenderness, apply moist heat to the sore area four times a day for 15 to 20 minutes each time.
Antibiotics are usually needed to clear up a breast infection, but you can most likely continue to breastfeed while you have the infection and take antibiotics. To relieve breast tenderness, apply moist heat to the sore area four times a day for 15 to 20 minutes each time. - Stress. Being overly anxious or stressed can interfere with your let-down reflex. That's your body's natural release of milk into the milk ducts. It's triggered by hormones released when your baby nurses. It can also be triggered just by hearing your baby cry or thinking about your baby. Stay as relaxed and calm as possible before and during nursing -- it can help your milk let down and flow more easily. That, in turn, can help calm and relax your infant.
- Premature babies may not be able to breastfeed right away. In some cases, mothers can release breast milk and feed it through a bottle or feeding tube.
- Warning signs.
 Breastfeeding is a natural, healthy process. But call your doctor if:
Breastfeeding is a natural, healthy process. But call your doctor if:- Your breasts become unusually red, swollen, hard, or sore.
- You have an unusual discharge or bleeding from your nipples.
- You're concerned your baby isn't gaining weight or getting enough milk.
Where Can I Get Help With Breastfeeding?
Images of mothers breastfeeding their babies make it look simple -- but some women need some help and coaching. It can come from a nurse, doctor, family member, or friend, and it helps mothers get over possible bumps in the road.
Reach out to friends, family, and your doctor with any questions you may have. Most likely, the women in your life have had those same questions.
Breastfeeding and the mother-child bond | Newborn Care
You've been imagining meeting your baby for months, and finally it's happened. The first weeks of breastfeeding are a special time when you get to know each other and forge an emotional connection.
Share this information
After the birth of a baby, all-consuming love and the desire to protect him can literally overwhelm you. However, an emotional connection is an individual experience, so don't worry if it doesn't happen right away. It takes time to get to know a child well. The emotional bond between parents and baby develops and strengthens in the process of caring for him.
For both parents, the most important thing is to get used to caring for a child: to be near him, to talk, to take him in his arms, to cuddle him. This increases your confidence in your parenting abilities, creates the best emotional, physical and psychological conditions for your baby, and also contributes to successful breastfeeding.
Skin-to-skin contact with your baby
You've probably heard how important skin-to-skin contact is when you cuddle a diaper-only baby against your bare chest (if it's cool, you can put a sweater or light blanket over the top). Early skin-to-skin contact, preferably within the first hour after birth, releases hormones that encourage the baby to find the breast and start suckling. 1 One study found that newborns who spent more than 50 minutes in skin-to-skin contact were eight times more likely to suckle spontaneously. 2 However, skin-to-skin contact is not only important in the first hour of life. This is a great way to calm the baby in any situation. In addition, it stimulates milk production.
Early skin-to-skin contact, preferably within the first hour after birth, releases hormones that encourage the baby to find the breast and start suckling. 1 One study found that newborns who spent more than 50 minutes in skin-to-skin contact were eight times more likely to suckle spontaneously. 2 However, skin-to-skin contact is not only important in the first hour of life. This is a great way to calm the baby in any situation. In addition, it stimulates milk production.
Skin to skin contact is good for the baby in many other ways. It normalizes the heartbeat and breathing, helps maintain optimal body temperature and healthy blood sugar levels. 3 If, for any reason, you are unable to hold your baby immediately after birth, skin-to-skin contact can be provided by your partner so that the baby can experience all the benefits listed, feeling safe, loved and warm.
Oxytocin: a prerequisite for breastfeeding and forming an emotional bond
Adjusting to your new role as a mother can be difficult, but precious moments in direct contact with your baby have a beneficial effect not only on him, but also on you.
Skin-to-skin contact in the mother's body creates a powerful calming hormonal cocktail, one of the main ingredients of which is oxytocin, the hormone of love and hugs. Oxytocin is produced with every contact with a newborn, and even when you just think about the baby or smell him. This smart hormone helps you adapt to motherhood. It stimulates "maternal behavior" - the desire to caress the child, look into his eyes and talk to him gently. 4
In addition, oxytocin fights feelings of anxiety and depression, thereby protecting you from postpartum depression. 5 It is also believed that the release of oxytocin shortly after birth prepares the brain for breastfeeding and stimulates milk production. 6
In addition, the mother produces beta-endorphin, a hormone that encourages her to respond to the needs of the child. Don't be surprised by the all-consuming desire to comfort a crying baby - this is a natural maternal instinct. In addition, beta-endorphin creates a feeling of pleasure and calmness. 3
3
What a newborn looks like
You will probably think your baby is the most beautiful creature in the world, but in fact, newborns usually look bruised and wrinkled, and sometimes even bruised or have a pointed skull, especially if forceps were used during birth or vacuum to extract the fetus.
In addition, the body of a newborn may be covered with so-called "stork bites" or "angel kisses" - red spots that disappear after a few months. The hands and feet of a newborn may have a bluish tint. All this is absolutely normal.
After a few days, the skin will smooth out, the head will become more round, and the primordial lubrication (cheesy white substance that protected the baby's skin in the womb) will disappear. There is no need to rinse off the lubricant - it is a natural moisturizer.
For the first few days, only the baby's head, buttocks and genitals should be washed (unless, of course, he has been soiled from head to toe with the contents of the diaper!). Bathing the whole baby is not required.
Bathing the whole baby is not required.
Washing your baby can be a great way for your partner to bond emotionally with the baby and take part in the care of the baby if the baby is fully breastfed. The rest of the baby's umbilical cord usually falls off within a couple of weeks. It does not look very pretty, but the main thing is to keep it clean and dry - then everything will be in order.
Making eye contact with the baby
Newborns can only see black, white and gray
(the color spectrum expands by about three months), 7 and their eyes can focus on objects no further than 25 cm (9.8 inches). This is enough for the baby to see your face while feeding. He may even briefly make eye contact with you. In the early days, you will have to feed the baby very often, so you will have the opportunity to enjoy this visual intimacy several times a day.
Forming an emotional connection with the voice
Full-term babies have good hearing. The fetus reacts to sounds as early as the 19th week of pregnancy. 8 It has been proven that newborns prefer the voice of their mother 9 to all others and even recognize the melodies they heard while they were in the womb. 10
8 It has been proven that newborns prefer the voice of their mother 9 to all others and even recognize the melodies they heard while they were in the womb. 10
Talking quietly to your baby creates two-way communication, which is important for your child's social development in the future. 11 You can talk about guests, about the view from the window - about anything. Newborns are very grateful listeners.
“Walking with Iris in the early days, I told her what I saw — trees, flowers, children playing,” recalls Anna, a mother from the UK.
Singing is another great way to form an emotional connection, 12 it doesn't matter if you have a voice. “While my daughter Leni was very young, I sang songs to her when I changed diapers,” says Charlotte, a mother from the UK, “Now she is 18 months old, and I still sing the same songs to her, usually at night. She loves it very much - familiar melodies calm her down.
The power of touch
Touch is very important for a child. Hugs, petting, rocking, and other caresses are a great way to soothe your baby and make him feel safe, 13 and stimulate the release of oxytocin. By the way, did you know that the baby has already developed a grasping reflex? Try touching his palms or stroking his feet and see what happens.
“While Vivienne and Marcus were babies, they liked having their feet massaged. Now I continue to do this before bed. I tried to take them in my arms as often as possible - it was a great way to establish an emotional connection with them, ”says Rachel, a mother from Australia.
Dee, a mother from South Africa, loved wearing her baby in a scarf sling. In her opinion, this not only allows you to establish an emotional connection with the child: “It helped us a lot to establish breastfeeding. Now my daughter is 17 months old, but she still loves it when I wear her in a sling.”
Attractive mother's scent
Newborns have a well-developed sense of smell, which plays a key role in establishing an emotional bond between mother and child. The newborn is attracted by the smell of the mother's breast. Scientists explain this by saying that Montgomery's glands (small bumps on the areola - dark areas of the skin around the nipples) secrete a secret that smells like amniotic fluid. 14
The newborn is attracted by the smell of the mother's breast. Scientists explain this by saying that Montgomery's glands (small bumps on the areola - dark areas of the skin around the nipples) secrete a secret that smells like amniotic fluid. 14
In addition, the baby recognizes the smell of the mother and can even smell her breast milk from that of another woman. 15 And when mother and baby hug and smell each other, oxytocin is released, which, as already mentioned, helps to establish an emotional connection and establish breastfeeding.
It is important to understand that all mothers and babies are different and it may take time for you to get used to each other. If you have any questions or concerns, please contact your healthcare provider for advice and assistance.
Literature
1 Klaus M. Mother and infant: early emotional ties. Pediatrics. 1998;102( E 1):1244-1246. - Klaus M. , "Mother and child: the origin of emotional bonds". Pediatrix (Pediatrics). 1998;102(E1):1244-1246.
, "Mother and child: the origin of emotional bonds". Pediatrix (Pediatrics). 1998;102(E1):1244-1246.
2 Gomez AP et al. Kangaroo method in delivery room for full-term babies. An Esp Pediatr. 1998;48(6):631-633. - Gomez A.P. et al., "Application of the Kangaroo Technique to Term Babies in the Delivery Room". An Esp Pediatr. 1998;48(6):631-633.
3 Crenshaw JT. Healthy birth practice #6: Keep mother and baby together—It’s best for mother, baby, and breastfeeding. J Perinat Educ . 2014;23(4):211-217. — Crenshaw, JT, "Physiological Birthing Practices #6: Mother and Baby Should Be Together - Better for Mother, Baby, and Breastfeeding." J Perinat Eduk (Perinatal education). 2014;23(4):211-217.
4 Britton JR et al. Breastfeeding, sensitivity, and attachment. Pediatrics. 2006;118(5): e 1436-1443. - Britton J.R. et al., Breastfeeding, Sensitivity and Attachment. Pediatrix (Pediatrics). 2006;118(5):e1436-1443.
- Britton J.R. et al., Breastfeeding, Sensitivity and Attachment. Pediatrix (Pediatrics). 2006;118(5):e1436-1443.
5 Kim S et al. Oxytocin and postpartum depression: delivering on what's known and what's not. Brain Res . 2014;1580:219-232. - Kim S. et al., "Oxytocin and postpartum depression: what we know and what we don't know." Brain Res. 2014;1580:219-232.
6 Uvänas-Moberg K, Prime DK. Oxytocin effects in mothers and infants during breastfeeding. Infant . 2013;9(6):201-206.- Uvenas-Moberg K., Prime D.K., "The effects of oxytocin on mother and child during breastfeeding." Infant. 2013;9(6):201-206.
7 Franklin A , Davies New evidence for infant color categories. Br J Dev Psychol. 2004;22(3):349-377. http://citeseerx.ist.psu. edu/viewdoc/download?doi=10.1.1.456.5409&rep=rep1&type=pdf - Franklin, A., Davis, I.R., "New Evidence for Color Perception in Infants ". Br J Dev Saikol. 2004;22(3):349-377.
edu/viewdoc/download?doi=10.1.1.456.5409&rep=rep1&type=pdf - Franklin, A., Davis, I.R., "New Evidence for Color Perception in Infants ". Br J Dev Saikol. 2004;22(3):349-377.
8 Hepper PG The development of fetal hearing. Arch DisChild. 1994;6(3): F 81-87. - Hepper P.J., Shahidullah B.S., "The Development of Hearing in the Prenatal Period". Arch Dis Child. 1994;6(3):F81-87.
9 Lee GY, Kisilevsky BS. Fetuses respond to father's voice but prefer mother's voice after birth. DevPsychobiol. 2014;56(1):1-11. — Lee JI, Kisilewski BS, "Fetus responds to paternal voice but prefers mother's voice after birth." Dev Psychobiol. 2014;56(1):1-11.
10 Partanen E et al. Prenatal music exposure induces long-term neural effects. PLoS One . 2013;8(10): e 78946. - Partanen, I. et al., Prenatal music listening has long-term effects on the brain. PLOS One. 2013;8(10):e78946.
- Partanen, I. et al., Prenatal music listening has long-term effects on the brain. PLOS One. 2013;8(10):e78946.
11 Kirk E et al. A longitudinal investigation of the relationship between maternal mind - mindedness and theory of mind. Br J Dev Psychol. 2015;33(4):434-445. — Kirk, I. et al., "Longitudinal study of the relationship between mother's orientation towards intelligence development and child's mental state model." Br Zh Dev Psychol. 2015;33(4):434-445.
12 de l'Etoile SK. Infant behavioral responses to infant-directed singing and other maternal interactions. Infant Behav Dev . 2006;29(3):456-470. - de l'Etoile SK, "Infant behavioral response to singing and other interactions with the mother." Infante Behave Dev. 2006;29(3):456-470.
13 Moore ER et al. Early skin-to-skin contact for mothers and their healthy newborn infants. Cochrane Database Syst Rev . 2012;5(3). - Mur I.R. et al., "Early skin-to-skin contact and its impact on mothers and healthy newborns". Cochrane Database Syst Rev. Rev. 2012;5(3).
Cochrane Database Syst Rev . 2012;5(3). - Mur I.R. et al., "Early skin-to-skin contact and its impact on mothers and healthy newborns". Cochrane Database Syst Rev. Rev. 2012;5(3).
14 Doucet S et al. The secretion of areolar (Montgomery's) glands from lactating women elicits selective, unconditional responses in neonates.PLoS One . 2009;4(10): e 7579. - Doucet S. et al., "Papillary gland secretion (Montgomery's glands) in lactating women induces a selective unconditioned response in the newborn." PLOS One. 2009;4(10):e7579.
15 Vaglio S. Chemical communication and mother-infant recognition. 2009;2(3):279-281. - Vaglio S., "Chemical Communication and Recognition in the Mother-Child Pair". Commune Integral Biol. 009;2(3):279-281.
Breastfeeding: how wonderful everything is created by nature!
Mother's milk is the nutrition for your baby that meets all the needs of the baby in the first year of life.
 It gives the child what he needs, and at the right time and in the right proportion. Mother's milk contains all the nutrients necessary for the growth and development of the child. During the first feeding, instead of milk, a woman produces colostrum - a yellowish-orange thick liquid. Colostrum, and subsequently milk, contains all the elements that strengthen your baby's immunity to resist various diseases. Indeed, numerous studies show that breastfed babies are much less susceptible to, or more tolerant of, diarrhea, respiratory infections, otitis media, and other infections common in infants.
It gives the child what he needs, and at the right time and in the right proportion. Mother's milk contains all the nutrients necessary for the growth and development of the child. During the first feeding, instead of milk, a woman produces colostrum - a yellowish-orange thick liquid. Colostrum, and subsequently milk, contains all the elements that strengthen your baby's immunity to resist various diseases. Indeed, numerous studies show that breastfed babies are much less susceptible to, or more tolerant of, diarrhea, respiratory infections, otitis media, and other infections common in infants. In addition to protecting the child's still undeveloped immune system, breast milk also prepares the body for the subsequent introduction of new products into the body. In any case, the baby accepts and digests mother's milk much better than any other baby food; a child absorbs 96% of the substances from mother's milk, and only 86% from baby food. The time during which mother's milk is digested is on average one and a half hours, any other milk is twice as long.

Should I breastfeed my baby?
For many, the answer is obvious, but some mothers wonder about the choice of feeding method.
For many weeks and months you will receive a lot of advice and information from a doctor, a wise mother or friends, and over time you have made your choice.
Mother's milk is the best for your baby. However, if you are unable to breastfeed, bottle feeding with a nipple contains today all the necessary essential nutrients for your baby to grow normally.
For you, mother
In addition to the practical benefits of breastfeeding in avoiding the time-consuming and costly preparations for bottle-feeding, the benefit is that breastfeeding will allow you to recover more quickly from childbirth. Sucking at the breast causes a slight contraction of the uterus. You do not feel it, but such contractions contribute to faster recovery after childbirth.
For both of you
Until you yourself become a mother, the "image of mother and child" is only a pretty picture.
 But to live in constant contact with a child, to find the physical closeness that united you before he was born, to continue to give him life - this is not as easy as it seems. It takes a lot of patience and effort. The baby feels the smell and warmth of the mother, her caress and feels safe. At such moments, a special emotional connection is born.
But to live in constant contact with a child, to find the physical closeness that united you before he was born, to continue to give him life - this is not as easy as it seems. It takes a lot of patience and effort. The baby feels the smell and warmth of the mother, her caress and feels safe. At such moments, a special emotional connection is born.
Breastfeeding is good for the baby
Breastfeeding is an unparalleled way of providing ideal nutrition to infants, with a unique biological and emotional impact on the health of both mother and child.
Breastfeeding should begin within 30 minutes of the birth of the baby.
Increasing the frequency of feedings stimulates milk production, so the baby should feed on his own, not on the clock, and as often as he wants.
The duration of each feeding is also determined by the child himself - he is at the breast for as long as he wants.

Breastfeed correctly. Both you and the baby should enjoy feeding.
The baby does not require any other food or drink other than mother's milk until at least 4 months of age. Water replaces breast milk, reduces the baby's appetite and, ultimately, milk production and duration of breastfeeding.
Do not give your baby any kind of pacifier - this prevents the baby from suckling properly at the breast.
When a mother becomes ill, her body produces antibodies that come with milk to the child and protect him from infection from the mother. A sick mother must continue to feed her child.
Breast milk prevents allergies as it contains large amounts of immunoglobulin A.
Sucking only the mother's breast ensures the correct development of teeth, muscles, face.
Breast milk contains antibodies that protect the baby from harmful viruses and bacteria. Colostrum, which is formed after childbirth, contains the highest concentrations of antibodies.

Breast milk provides better development of the nervous system, gastrointestinal tract, respiratory and endocrine systems.
Breastfeeding is convenient and clean.
Breastfeeding at least one child reduces the risk of breast cancer by 50%, protects against ovarian cancer.
Breastfeeding strengthens the bond between mother and child, not only at an early age, but throughout life.
Enjoy being with your child. Skin to skin contact, eye to eye, your love for him will provide you with spiritual intimacy with your child for many years.
Quality benefits of human milk
1. Breastfeeding is the highest art of motherhood.
2. Proteins are easy to digest.
3. Ideal protein standard. Proteins have the best amino acid composition.
4. A lot of immunoglobulin - protection against diseases.
5. Possesses proteolytic activity (has enzymes that break down protein in the child's stomach).

6. High content of unsaturated fatty acids.
7. B-lactose - maintains normal intestinal flora, there are no putrefaction processes.
8. More vitamins D, E, A, C.
9. The iron contained in human milk is better absorbed (than in cow's milk).
10. Women's milk is sterile.
11. Breastfed babies have a higher IQ.
Negative aspects of artificial feeding
1. Possibility of allergy.
2. After heat treatment, the composition of milk changes.
3. Risk of infection of the newborn.
4. Cow's milk contains no vitamins, no antibodies.
5. The flora in the intestines of the child is changing (putrid), the stool is shaped and rare.
6. Cow's milk proteins are harmful to the kidneys.
7. Relationship between child and mother at a distance.
8. Children get sick more often and more severely, they do not get a sense of satisfaction from communicating with their mother.