Delivering a baby at 33 weeks
Baby Born at 33 Weeks: What to Know
7 weeks before your due date is a surprising time to welcome your new baby to the world.
You might not have their crib set up yet, and maybe you had to throw together your hospital bag in a bit of a rush. But don’t worry, you’ll get up to speed soon.
So, what should you know about caring for a baby born at 33 weeks?
No doubt, they’ll require some extra attention compared to a baby born at full term, but your medical team will know exactly what to do.
Here’s our guide to what to expect when you have a baby born at 33 weeks.
In this article 📝
- What does a baby born at 33 weeks look like?
- What happens if a baby is born at 33 weeks?
- Do babies born at 33 weeks need NICU?
- What is the chance of survival for a baby born at 33 weeks?
- Can babies born at 33 weeks breathe on their own?
- Can you give birth naturally at 33 weeks?
What does a baby born at 33 weeks look like?
If you’re searching for baby born at 33 weeks pictures, you’ll notice that they look basically like a full-term baby.
A baby born at 33 weeks is classed as “moderate preterm,” so they are not quite as small or fragile-looking as “very preterm” or “extremely preterm” babies.
They’ll weigh somewhere in the region of 4.5 to five pounds, so while they’ll be small, their muscle development means they’ll be slightly more sturdy than even those born a week before.
What happens if a baby is born at 33 weeks?
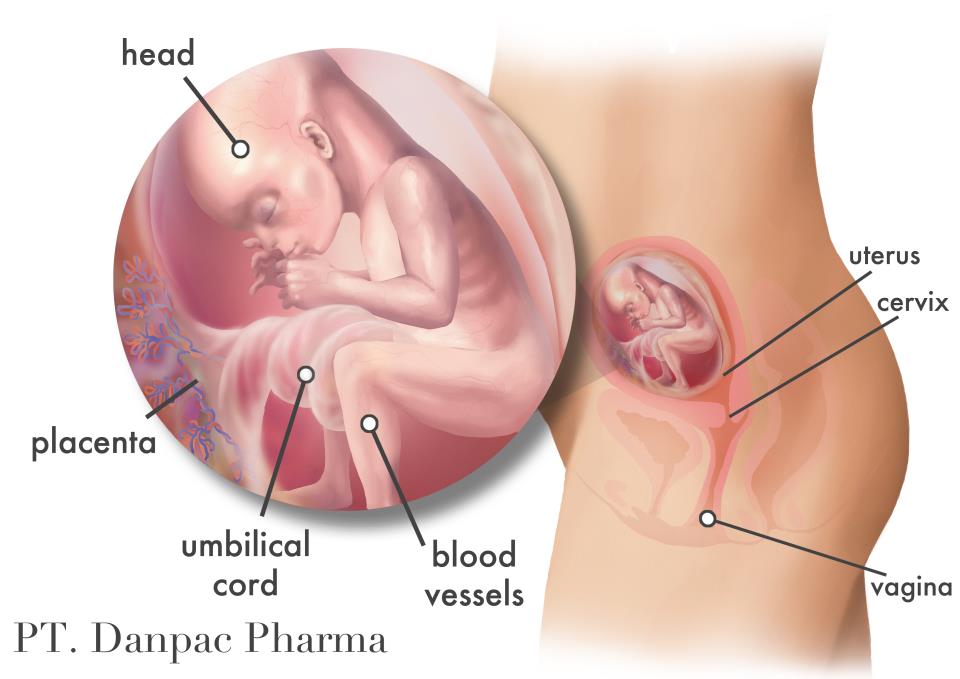
A baby born at 33 weeks is still almost two months from their due date, so they’ll need a little help starting out with things like breathing and feeding.
Popular Topics
- Lifestyle
- Pregnancy
- Motherhood
The length of your hospital stay will depend on your little one’s exact condition and can change from day-to-day.
At 33 weeks, your baby’s eyes will follow objects, and they may show an obvious response to you and your voice when you are near them.
Their limbs are stronger and their movements less jerky than babies born earlier than 33 weeks.
Even if you can’t hold them right away, spending time with them will be a great experience for you both.
Do babies born at 33 weeks need NICU?
Yes, it’s most likely that your baby born at 33 weeks will need a period of specialist care, and this is often in a NICU setting.
Their immune system is immature, so staying in a safe environment like an incubator (which will also help them keep warm) is a great start.
What is the chance of survival for a baby born at 33 weeks?
The baby born at 33 weeks survival rate is around 99.5%, according to one study. But of course, there are still risks to delivering so early.
There’s about a 70% chance a baby born at 33 weeks will have some kind of initial heart or breathing difficulties, which is why NICU is often the safest place for them to be.
Their long-term prognosis is great, and the vast majority of babies born at 33 weeks have no lasting issues relating to their premature arrival.
Can babies born at 33 weeks breathe on their own?
Sometimes, but the majority of babies born at this age will need some breathing assistance, to begin with.
This may be for a day or two or a week or two. Each baby is unique.
It’s also common for babies born at 33 weeks to experience some feeding difficulties, and they may be slow to gain weight.
Mastering the feeding reflex and getting strong enough to coordinate feeding and breathing can take some time.
You may be encouraged to try breastfeeding once or twice a day if you want to.
Can you give birth naturally at 33 weeks?
Giving birth at 33 weeks can happen for a range of reasons – and yes, you may spontaneously go into vaginal labor.
On the other hand, you might have an underlying condition or other medical reason for your labor may be induced early or to have a C-section.
The important thing, however it happens, is that your baby is here, safe and in the best place to receive the care they need.
Your baby’s here, mama! Congratulations!
You might also be interested in:
Baby Born at 34 Weeks: What to Know
Baby Born at 35 Weeks: What to Know
Baby Born at 36 Weeks: What to Know
Baby Born at 37 Weeks: What to Know
Premature Babies: All You Need to Know
What to Look for in a Preemie Pacifier
Survival Rate, Time in Hospital, More
The final months of pregnancy are full of prepping and planning. And, of course, planning is important. But be prepared: Many births don’t go according to plan.
And, of course, planning is important. But be prepared: Many births don’t go according to plan.
For example, you might end up having a cesarean delivery (C-section) or other interventions that you weren’t planning on. Or you may find yourself with much less time to prepare if your baby decides to show up to the party earlier than expected!
About 11 percent of babies worldwide are born early (premature). This means that they’re born more than 3 weeks before their estimated due date. About 85 percent of these are born between 32 and 36 weeks of pregnancy.
But if your baby is born even more prematurely — say, at 32 weeks — they still have very good odds at being healthy with some supportive medical care. Here’s what you need to know about a baby born at 32 weeks.
Yes, a baby can safely be born at 32 weeks, but they may need specialized care to help support their development as they navigate their early days in the world.
A baby who’s born before week 37 of pregnancy is considered to be premature. However, during pregnancy, every week — and even every day — makes a difference in a baby’s growth and development. This is why premature babies are grouped into four stages:
However, during pregnancy, every week — and even every day — makes a difference in a baby’s growth and development. This is why premature babies are grouped into four stages:
- late preterm, born between 34 and 36 weeks
- moderate preterm, born between 32 and 34 weeks
- very preterm, born between 25 and 32 weeks
- extremely preterm, born before 25 weeks
If your baby reaches 32 weeks of gestation (time in the womb) and is born at 32 weeks, they’re moderate preterm. Babies born at 32 weeks have a survival rate as high as 95 percent. They also have very good chances of growing into healthy babies and children without any complications.
Babies who are born very preterm and extremely preterm have a higher risk of complications and health problems than a baby born at 32 weeks.
How healthy and developed your baby is at 32 weeks also depends on what kind of pregnancy you have. If you’re carrying twins or other multiples they may be smaller than if you’re carrying a singleton baby.
At 32 weeks, babies still have a couple months to go before reaching their full birth weight, but they’re well developed. Your baby will look almost like a full-term baby, just smaller, thinner, and even more delicate.
They’ll have almost-there toenails and perhaps a few wisps of hair on their head. Most of the soft, downy hair (lanugo) that covered them earlier in the womb will have started falling off, but they’ll still be a little fuzzy.
They probably will not yet have fully formed fingernails. Their eyes, though developed, may be too sensitive to light to open just yet. By 32 weeks most babies are practicing breathing, and their lungs are in the final stages of development. Their skull and all their bones will still be very soft.
At 32 weeks, a baby may:
- weigh almost 4 pounds
- be between 16 and 17 inches long
- have a head size (circumference) between 11 and 12 inches
How long your baby needs to stay in the hospital after they’re born at 32 weeks depends on several things.
After birth, your premature baby will be taken to a special care nursery or the neonatal intensive care unit (NICU) in the hospital where you gave birth.
Most babies born at 32 weeks of pregnancy have only a few temporary health issues and need to stay in the NICU for only a few days to a few weeks. After birth, your baby may need extra help learning and developing the skills needed for feeding, staying warm, and breathing on their own.
Babies born at 32 weeks will generally not yet be strong enough to breastfeed because their sucking muscles are still weak and uncoordinated. They’ll likely need to be tube-fed for a few weeks.
That said, receiving breast milk is especially important for preterm babies. Compared to preterm babies who receive formula, those who receive human milk typically have higher survival rates, shorter NICU stays, and fewer serious health complications.
Even if you weren’t planning to breastfeed, you may consider expressing milk to help nourish your premature baby. You may also consider donor milk.
You may also consider donor milk.
Most babies born at 32 weeks don’t have breathing problems, but your doctors and nurses will make sure they’re breathing properly.
Before your baby can safely go home with you, your doctor will make sure they don’t have any other health problems and are growing and developing enough to do well without NICU care.
Before they’re discharged, your baby will be evaluated on their:
- weight gain
- ability to suck and swallow milk on their own
- temperature regulation
- eye development and sensitivity
Babies born at 32 weeks might have some temporary health problems such as:
- low birth weight
- jaundice
- hypothermia
- feeding difficulties
Some long-term issues in babies born at 32 weeks might show up months to years later. These are not common, but can include slower development. In most cases, babies with learning or developmental delays catch up later in childhood with a little bit of extra help.
A 2017 medical study in France that followed 5,170 babies who were born between 22 to 34 weeks of pregnancy found that babies born at 32 to 34 weeks had very low risks of long-term health problems.
The researchers found that about 1 percent of babies born at 32 to 34 weeks had the neuromotor disorder cerebral palsy.
The same study tested 2,506 2-year-olds who were born prematurely. In the group born at 32 to 34 weeks of pregnancy, 36.2 percent scored slightly lower than average on a questionnaire that was used to test brain development.
While this means that some babies born at 32 weeks may have delayed learning development and skills in early childhood, and early intervention can have a significant impact in improving skills.
If your baby is born at 32 weeks, they have very good chances of being born healthy and developing just fine.
They’ll be considered premature, specifically moderately preterm, and will need extra medical care to make sure they’re healthy and growing normally before they can go home. Your baby may be in the hospital or NICU for several days to weeks.
Your baby may be in the hospital or NICU for several days to weeks.
In rare cases, a baby born at 32 weeks may have neurodevelopmental (brain and learning) delays. In most cases, they’ll catch up with some extra help during early childhood.
Premature birth - Juno
Premature birth: content of the article
What is preterm birth
The birth of a baby weighing more than 0.5 kg from 22 to 37 weeks is considered early. According to statistics, 15 million babies are born prematurely around the world.
In our country, until 2012, babies were registered who were born at 28 weeks, and all those born earlier - a week later. The development of obstetrics made it possible to nurse critically premature babies and increased their survival statistics.
Who is at risk
Any pregnant woman can give birth prematurely. Some expectant mothers have a higher chance of preterm birth. The risk zone includes pregnant women:
- under 17 and over 35;
- have more than one fetus;
- have structural features of the uterus or its cervix;
- use harmful substances - drugs, alcohol, smoke;
- have heavy physical activity;
- have a history of preterm birth;
- work in hazardous production;
- are subjected to sexual, emotional abuse, stress, mental stress.

At risk are expectant mothers who are not registered during the gestation period or ignore ultrasound, screenings, laboratory tests.
The threat of early preterm birth is more common with diagnoses: diabetes mellitus, anemia, hypertension, genitourinary infections, hypothyroidism, problems with weight before conception (deficiency or obesity), thrombophilia, vaginal bleeding. There is also a risk when conceiving through IVF, with congenital malformations of the fetus.
If a woman has previously given birth to a child ahead of schedule, the chances of premature birth remain in subsequent pregnancies. The same applies to the weight of the crumbs: if the firstborn was born with a lack of body weight, then his brother or sister may be underweight.
Risk factors
Doctors point to a number of factors that take place long before the conception of a child. These include:
- Gynecological diseases suffered in childhood or adolescence;
- Early initiation of intimate life;
- Hereditary factor;
- Pathologies of previous pregnancy: preeclampsia, fetoplacental insufficiency, premature birth;
- Excessive uterine distension in multiple pregnancies, polyhydramnios;
- Threat of early miscarriage.

Another risk factor is surgery or trauma to the abdominal organs during the gestation period.
Risk of preterm birth at different terms
The birth of a child prematurely has many negative consequences for him. It depends on the trimester in which the pregnancy ended.
The most severe consequence is the death of the infant. With early preterm birth in the period of 22-24 weeks, the threat is the highest - up to 80% of babies die. This occurs against the background of intracranial hemorrhage of 3-4 degrees, cardiopulmonary insufficiency, intrauterine infection of the fetus.
Among those born in the period of 25 - 26 weeks, 40% of babies die, in 27 - 28 - about 20%, in 29 - 32 - no more than 10%, and in 33 - 34 - 2% of newborns are at risk.
Modern medicine is able to provide care for a premature baby and save his life. But no one can guarantee a full healthy life. Such a child can subsequently be given disappointing diagnoses: cerebral palsy, mental retardation, retinopathy of prematurity. He may suffer all his life from problems with the digestive and respiratory systems, impaired vision, hearing, delayed mental and physical development. Diagnosis implies disability.
He may suffer all his life from problems with the digestive and respiratory systems, impaired vision, hearing, delayed mental and physical development. Diagnosis implies disability.
For a woman in labor, preterm labor is usually not dangerous. Without concomitant pathologies, the mother's body does not care how long the child is born. There are only psychological problems: stress, fear and worries about the baby. It is better for a mother to tune in that her child, in case of severe prematurity, will be taken to the intensive care unit for nursing, so she will not see him immediately.
A newly minted mother needs rehabilitation. Therapy is prescribed, depending on the cause of the pathology: a complex of vitamins, antioxidants, hormones.
Why preterm birth is dangerous
Infants are immature: their body is covered with a large amount of cheese-like lubricant, there is a deficiency of subcutaneous fatty tissue, few hairs on the head and fluff on the body, cartilage on the ears and nose are soft, the nails do not go beyond the fingertips, the navel is located closer to the pubis.
Babies are underweight. Depending on the weight of the crumbs, 4 degrees of prematurity are distinguished: at the 1st degree, the baby weighs from 2500 to 2001 g, the 2nd - from 2000 to 1500 g, the 3rd - from 1500 to 1001 g, the 4th - 1000 g and below .
The development of the genital organs has not been completed: the testicles in boys are not lowered into the scrotum, and in girls the large labia do not cover the small and clitoris.
Children have immature lungs. They cannot breathe adequately - often they need help. The cry is weak. There are also problems with digestion. The body cannot absorb all the components from mother's milk.
Extrauterine life for children becomes a strong stress. It's hard to deal with him. They poorly resist infections, quickly lose heat, thermoregulation is impaired. They are subject to hemorrhages against the background of fragile vessels. Especially dangerous are hemorrhages in the cervical spinal cord and ventricles of the brain.
Among the complications of preterm birth are intracranial hemorrhages, asphyxia, intrauterine growth retardation.
Types of preterm birth
Several classifications have been adopted. Let's consider them.
- By term: critically early - up to 28 weeks, significantly early - from 28 to 32 weeks, moderately early or late - from 32 to 37 weeks;
- By the mechanism of attack: induced and spontaneous. Induced cause artificially for medical reasons. Occurs in 40% of cases. Spontaneous in 60% of cases begin with contractions, in 40% - with a rupture of the membranes;
- By the nature of the course: spontaneous, with regular labor activity, without it and artificially provoked. In 80% of cases, preterm labor begins spontaneously. At the same time, the fetal bladder can be intact - and then the contractions are regular, growing. Or amniotic fluid may pour out, labor activity is chaotic. For medical reasons, early delivery can be artificially induced.
 For example, in case of danger to the life of the mother, intrauterine death of the fetus, or defects that are incompatible with life;
For example, in case of danger to the life of the mother, intrauterine death of the fetus, or defects that are incompatible with life; - According to symptoms: threatening, incipient and incipient. With threatening early premature birth, the lower abdomen and lower back hurt, the tone rises. Her neck remains unchanged, the external os is closed. When the process begins, pains appear in the lower abdomen. Regular contractions may begin. The neck is flattened or shortened. The main symptom of the onset of preterm labor is regular labor activity. The cervix opens by 2 - 3 cm, it happens quickly.
In 40% of women in labor, water breaks, 35% gave birth quickly and quickly. The active phase lasts less than when the baby appears on time. The contractions are monotonous, long and painful, the pauses between them are small.
Causes of preterm birth
Doctors indicate the main causes of the pathology:
- Early activity of the fetal endocrine system;
- Infections and inflammatory processes - ureaplasmosis, mycoplasmosis, pyelonephritis, bacterial vaginosis.
 They stimulate the production of prostaglandins. Hormones affect the uterine muscles - cause contractions and premature birth;
They stimulate the production of prostaglandins. Hormones affect the uterine muscles - cause contractions and premature birth; - Placental bleeding. They occur with incorrect presentation or detachment. The situation is serious, there is a threat to the life of the mother. Therefore, with presentation, hospitalization is indicated;
- Neck weakness. In 20% of cases, it leads to preterm birth. This also includes such factors: the interval between the current and previous gestation is less than 2 years, the woman is expecting 4 children or more;
- Isthmic-cervical insufficiency. The cervix opens itself - a miscarriage or premature birth occurs. It is possible to open mechanically - when scraping after a miscarriage, IVF, abortion;
- Pathologies on the part of the baby - intrauterine infection, malformations of internal organs.
Chronic ailments, dental problems, angina, health status during gestation, genetic factors are all common reasons for early delivery.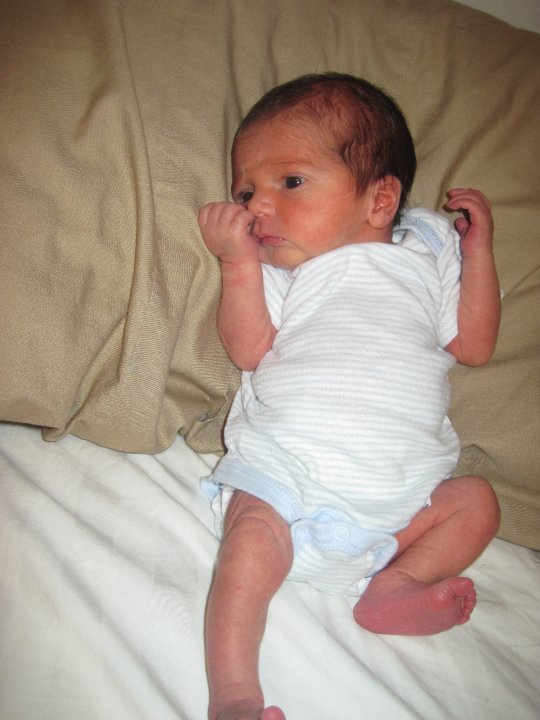 Sometimes it is impossible to determine. Although this is important for the development of effective means of preventing pathology.
Sometimes it is impossible to determine. Although this is important for the development of effective means of preventing pathology.
Symptoms of preterm labor
We list the signs by which you may suspect that the baby is in a hurry to be born ahead of time.
Spasms over the pubis. They are similar to pain during menstruation.
Pain, pressure and discomfort in the genitals, thighs, pelvis. There is a dull pain in the lumbar region.
Feeling of pressure, pressure in the back.
Diarrhea, spasms and pain in the intestines.
Vaginal discharge - they get worse. May be watery, pink, brown, bloody.
Contractions of varying intensity. Touch your stomach with your fingertips - you will feel the contraction and relaxation of the uterus. Counted more than 4 contractions in 60 minutes? Call an ambulance - you need an urgent examination by an obstetrician.
The following symptoms are also dangerous: sudden blurred vision, flashes and “flies” before the eyes, incessant migraine, swelling of the face or hands, temperature of 38º C and above, painful urination, abdominal trauma, decreased fetal activity in the 3rd trimester (less than 10 movements in 12 hours).
Any of the above symptoms indicate the risk of preterm birth. Seek medical attention.
Diagnosis of preterm birth
Includes several stages.
Transvaginal ultrasound. The length of the cervix is measured, fetal fibronectin is determined - a kind of "biological glue" that binds the fetal sac to the uterine mucosa.
Gynecological examination. Allows you to assess the degree of opening of the neck, its length.
Rapid test for the determination of phosphorylated protein-1. The test determines the possibility of preterm birth. In the future, this helps prevent iatrogenic complications.
When diagnosing, 2 parameters are evaluated:
- Regularity of contractions;
- Neck changes - shortening and smoothing. informative method. For example, with a neck length of 3 cm, the risk of preterm birth in the next week is 1%. The patient is not admitted to the hospital, there is no danger to her and the fetus.

Differential diagnosis
Its goal is to correctly diagnose. The early birth of a baby is accompanied by cramps in the lower abdomen, diarrhea, pain in the lumbar region. These same symptoms are characteristic of other conditions: appendicitis, colitis, cystitis, pyelonephritis.
When complaining of pain in the lower abdomen, the patient is examined for the consistency of the scar after the previous cesarean section, for example. When the temperature rises, flu, sore throat, viral infection are excluded.
Diagnosis
Preterm birth is stated based on the clinical picture. Doctors are guided by such markers.
The first is the length of the neck - less than 2 - 2.5 cm.
The second is the determination of phosphorylated protein-1.
The third is the regularity of contractions. There should be at least 4 in 20 minutes.
Fourth - neck changes in dynamics.
Fifth - assessment of the degree of maturity of the neck. Determined by the level of PSIFR-1 in the cervical canal.
Determined by the level of PSIFR-1 in the cervical canal.
Usually the process begins rapidly, suddenly and intensely.
Treatment for preterm birth
The goal is to reduce the tone of the myometrium, reduce uterine contractions. This is achieved by blocking oxytocin receptors - it is the hormone oxytocin that triggers the birth process.
Such antagonists of oxytocin receptors are tocolytics. One of the modern representatives of this group of drugs is atosiban.
The remedy is effective, but has contraindications. It is forbidden to treat pregnant women for less than 24 and more than 33 weeks, with uterine bleeding, growth retardation, distress or fetal death, severe preeclampsia, with rupture of the fetal membrane after 30 weeks, placenta previa or its detachment.
5 stages of preterm labor
The first stage is forecasting their onset. Depends on the situation: the process is starting, has begun, or it is a threat.
Stage two - prevention of respiratory distress syndrome in a child. Doctors stimulate the maturation of the lungs. Apply funds from the group of glucocorticoids.
Stage three - prolongation of pregnancy. Doctors try to delay preterm labor by giving the baby's lungs and placenta time to mature. For this, tocolytics are used - they inhibit the contractile activity of the uterus. Usually prophylaxis is carried out - tocolysis is carried out before contractions. When started, therapy is ineffective. The duration of treatment is a maximum of 48 hours.
Stage four - preparation for the birth of a premature baby. The woman in labor is transferred to a higher-level hospital. The physiology of preterm labor does not differ from the birth of a child at term. But close attention is required from doctors to minimize complications for mom and baby.
The fifth stage is the prevention of infections and their complications. At risk are women in labor whose waters have broken. If the patient gives birth before 34 weeks, she can be pierced with a course of dexamethasone. It accelerates the maturation of the placenta and internal organs of the baby, reduces the risk of complications.
If the patient gives birth before 34 weeks, she can be pierced with a course of dexamethasone. It accelerates the maturation of the placenta and internal organs of the baby, reduces the risk of complications.
OB sequence
When registering a patient with preterm birth, the doctor gets acquainted with the exchange card, studies the general, gynecological and infectious anamnesis, and the results of examinations. Clarifies complaints and evaluates the condition of the woman in labor. He examines her, measures the pulse and respiration rate, temperature, pressure, abdominal circumference and the height of the uterus.
Clarifies data on the fetus: movements, measures heart rate by auscultation - listening to the heart through the mother's stomach through the device. To assess the condition of the crumbs, the doctor performs cardiotocography. The device records the heart rate.
Ultrasound is performed to assess the condition of the child and mother's organs.
A gynecological examination is carried out: with intact membranes - external, with their rupture - internal. This is necessary to determine the position and position of the child, to assess the degree of disclosure.
Conduct a laboratory examination. They take a smear from the vagina: culture for β-hemolytic streptococcus, bacteriological culture, take blood and urine for a general analysis.
According to the results of the examination, the obstetrician confirms or refutes preterm birth, their stage.
The expectant mother is informed about her condition, forecasts for the child. At the slightest opportunity, they try to prolong the pregnancy. If the child is ready to be born in the near future, the doctor determines the tactics of assistance, coordinates the issue of anesthesia with the woman in labor.
In the absence of indications for a caesarean section, they give birth naturally. This is the best way - it is less traumatic for the baby. A gentle approach is what a weak newborn needs.
A gentle approach is what a weak newborn needs.
Preterm birth care policy
The woman in labor is provided with continuous psychological support. Describe the current obstetric situation.
With head presentation, they give birth naturally.
With pelvic - take into account clinical indications. Caesarean section is not the only effective method in this case. The operation does not improve the prognosis for a premature baby, but it puts an additional burden on the mother's body: it increases infection, morbidity, and complications.
With foot presentation, only a caesarean section is done.
Anesthesia is carefully selected. Avoid opiates - they depress the respiratory center, which is dangerous for premature babies.
At the birth of a baby before 34 weeks, vacuum aspiration is prohibited. It increases the risk of neonatal morbidity. Dosed episiotomy, exit forceps for the birth of the head and epidural anesthesia are performed.
The umbilical cord is clamped at least 1 minute after the baby is born. This tactic reduces the frequency of intraventricular hemorrhage in preterm pregnancies up to 37 weeks of gestation.
Control the state of the crumbs. CTG is done every hour for 40 minutes, auscultation - periodically.
General recommendations for prevention
You need to think about it from the first trimester. If you want to inform the baby, follow the advice of gynecologists.
- Take care of yourself. Rest, avoid nervous overload. Sleep at least 7 hours;
- Eat well. Eat foods rich in vitamins, exclude fast food, fatty, fried, spicy and salty foods from the diet. Give up coffee and strong tea;
- Observe the drinking regimen. Try not to feel thirsty - drink water every 2 hours. If you don't want to - don't force yourself;
- Avoid physical activity. Active training, hard work, general cleaning alone are taboo for a pregnant woman.
 Try not to go outside on ice - you may fall, you will strain your muscles - this can increase your tone and provoke premature birth;
Try not to go outside on ice - you may fall, you will strain your muscles - this can increase your tone and provoke premature birth; - Maintain personal hygiene. Wash your face after a bowel movement. Always wash and dry from front to back. This way you will not bring bacteria from the intestine into the vagina. Infections are provocateurs of premature birth;
- Lead a healthy lifestyle. Alcohol and cigarettes are taboo. Smoking pregnant women are predisposed to preterm labor. If you take medications on a regular basis, tell your gynecologist about it. Walk outdoors. Cancel active workouts in favor of leisurely walks in the park;
- Register at the antenatal clinic in the first trimester - at 6 ‒ 8 weeks. Visit a gynecologist, listen to him, take tests, undergo ultrasound, screenings;
- Be careful with sex. In the first trimester, it is better to limit or abstain from it as much as possible - the embryo must be fixed. With placenta previa and other pathologies, the gynecologist may forbid you to have intimate contacts - listen to him;
- Learn to understand your body.
 In the 2nd trimester, start listening to the baby: his movements, activity. Fix any changes, strange and unpleasant sensations - and talk about them to the doctor. In case of acute pain, contractions, spasms, blood, urgently call an ambulance - this may be a premature birth;
In the 2nd trimester, start listening to the baby: his movements, activity. Fix any changes, strange and unpleasant sensations - and talk about them to the doctor. In case of acute pain, contractions, spasms, blood, urgently call an ambulance - this may be a premature birth; - Maintain bed rest. A gynecologist can advise you to rest. For example, with increased uterine contractions, tone;
- Rest every hour. Sit in a chair, lift your legs up. This will relax the muscles, eliminate swelling;
- Be aware of the signs of preterm labor. In case of their threat, you will not miss a moment and consult a doctor. Perhaps the process can be stopped with the help of drugs. Treatment minimizes complications in the premature baby.
Preterm birth prevention
It is divided into 2 stages: before conception and after.
Preventive measures before conception
It is advisable to carry them out to mothers from the risk zone. The gynecologist limits intrauterine manipulations, such as curettage. During IVF, the number of embryos for transfer is regulated taking into account the age of the expectant mother and her health. Inform about the possibility of premature birth at conception through reproductive technologies.
The gynecologist limits intrauterine manipulations, such as curettage. During IVF, the number of embryos for transfer is regulated taking into account the age of the expectant mother and her health. Inform about the possibility of premature birth at conception through reproductive technologies.
Hydration is shown - enhanced drinking regimen. It improves fetoplacental blood flow and reduces the risk of preterm birth.
Eliminate infections. It is advisable to do this at the planning stage, since antibiotic treatment during gestation harms the fetus.
It is recommended to postpone the conception of a child soon after the birth of an older brother or sister. Mommy's body needs to recover from the previous pregnancy. It takes him at least 2 years to do this. During this time, the uterus will return to its previous state, strength, vitamin reserves and body reserves will be restored.
Vitamin complexes are prescribed for predisposition to preterm birth for planning and expectant mothers. Protein-rich dietary supplements are helpful. They strengthen the immune system, improve blood circulation, protect the pregnant woman from infections - and hence the child.
Protein-rich dietary supplements are helpful. They strengthen the immune system, improve blood circulation, protect the pregnant woman from infections - and hence the child.
Secondary prevention of early delivery
With the threat of premature birth, the condition of the pregnant woman is monitored at critical periods: from 2 to 12 and from 18 to 22 weeks. During these periods, it is better to stay in the hospital of the perinatal center. Doctors prescribe drugs to maintain and prolong pregnancy.
Therapy is selected on an individual basis.
With a short neck from 1 to 2.5 cm, progesterone suppositories are prescribed vaginally. The hormone is also shown in previous preterm births. This tactic reduces their risk by 35%. This is a natural hormone. It is efficient and safe. It is prescribed in the first trimester. Synthetic hormone is harmful: it can provoke gestational diabetes.
If there is a threat of early birth of the crumbs, sutures are placed on the neck. The expectant mother is out of the risk zone in this situation, stitches may not be applied.
The expectant mother is out of the risk zone in this situation, stitches may not be applied.
Another option is to install a pessary on the neck.
These methods reduce the statistics of premature births. But the mortality rate of newborns is not affected.
When carrying twins, circular or U-shaped sutures can be applied. In most cases, such tactics with a short neck in multiple pregnancies can provoke preterm labor. Vaginal progesterone is not prescribed.
For infections (for example, bacteriuria, gonococcus, syphilis, β-hemolytic streptococcus, bacterial vaginosis, chlamydia), antibiotic prophylaxis is prescribed. Depending on the diagnosis, penicillin, ampicillin, metronidazole, erythromycin, ceftriaxone, josamycin may be prescribed.
Terminals
Premature birth is one of the fears of many expectant mothers. Nobody is immune from this. But you can minimize the risks. Follow the recommendations of the gynecologist, take care of yourself, listen to your body, do not refuse to stay in the perinatal center.
Don't think bad. Modern medicine successfully nurses premature babies, reduces the risks of complications and consequences.
33 weeks pregnant what happens to the fetus
The third trimester is approaching its middle, and the 33rd week of pregnancy marks the beginning of the final leg of the journey. There is very little left before the birth, mom is filled with expectation. The fetus already looks like a full-fledged person, but development continues. Now his formed systems are working to strengthen and improve, and my mother's body is actively involved in this.
What's going on with the baby?
The size of the child continues to increase. At the 33rd week of pregnancy, he already weighs about 2 kg, and his height reaches almost 45 cm. Of course, if you are expecting twins, then the parameters of each child will be smaller. But while the fetus has not yet gained enough subcutaneous fat, it looks very small.
Important! At the 33rd week of pregnancy, the endocrine, digestive, nervous, immune, and urinary systems are formed and are actively functioning. The respiratory organs, thermoregulation of the body, and blood circulation continue to develop.
The respiratory organs, thermoregulation of the body, and blood circulation continue to develop.
During this period, the baby is already in the prenatal position, but it can still change. Nevertheless, the doctor gives recommendations on special exercises or sets the mother up for natural childbirth or a caesarean section. Now there will be no special changes in the development of the fetus, but the processes continue:
- Marigolds on tiny fingers have grown and taken their place.
- The baby's face has acquired individuality. Some mothers even think that they can determine who the son or daughter, or several children, will look like.
- The child distinguishes sounds, some he likes, others - no.
- Also, the baby is able to smell and taste, so everything that the mother eats is analyzed and evaluated by the child.
- The fetus reacts to the level of light - understands when it becomes darker or lighter.
- The breathing system is already ready for the first breath.

The baby's skin almost takes on a natural skin tone, and there are not so many wrinkles and folds now.
Interesting! The intensity of the movements of each fetus is different, because the babies already in the mother's stomach acquire character. Some are very active, while others are a little lazier. On average, a child must move or push up to 10 times in 2 hours. If the number of tremors is significantly less or there are none at all, you should immediately consult a doctor.
How does a woman feel?
The baby is growing so fast that the mother can literally feel it. He has little space in his stomach, so he kicks quite noticeably. His blows from the inside to the ribs can cause discomfort. A woman suffers from back pain, in this case the cat-dog exercise comes to the rescue, after which relief comes.
The vegetative-vascular system also makes itself felt to the expectant mother. Shortness of breath, heavy sweating, dizziness - all this is due to the fact that the woman's body works for the growth of the child, drawing strength, including from internal reserves.