Neural tube defects risk
Neural tube defects | Pregnancy Birth and Baby
Neural tube defects | Pregnancy Birth and Baby beginning of content4-minute read
Listen
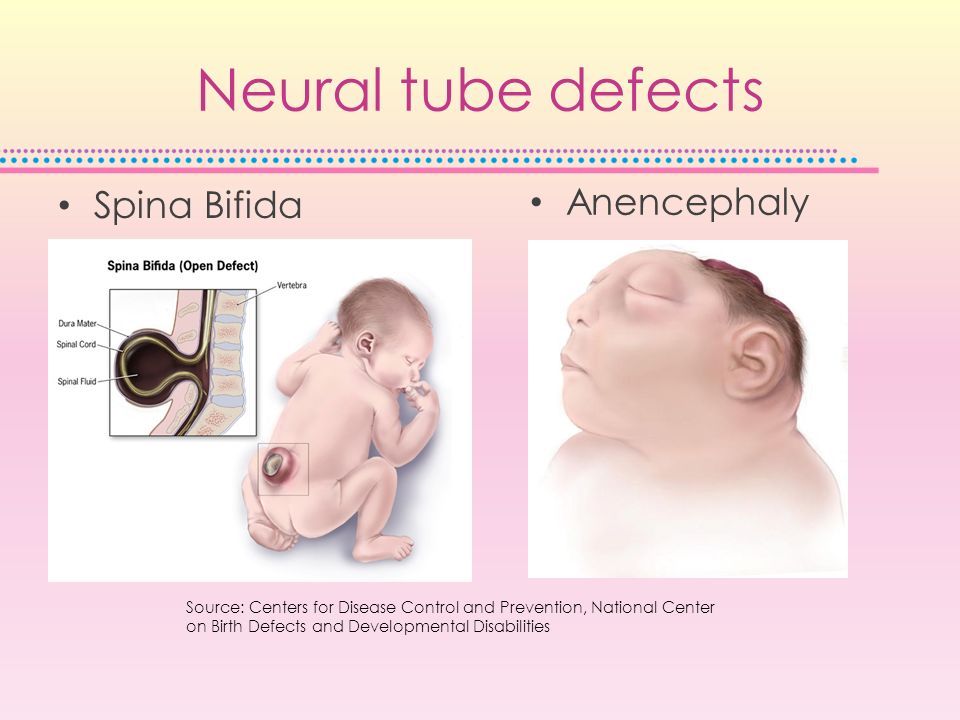
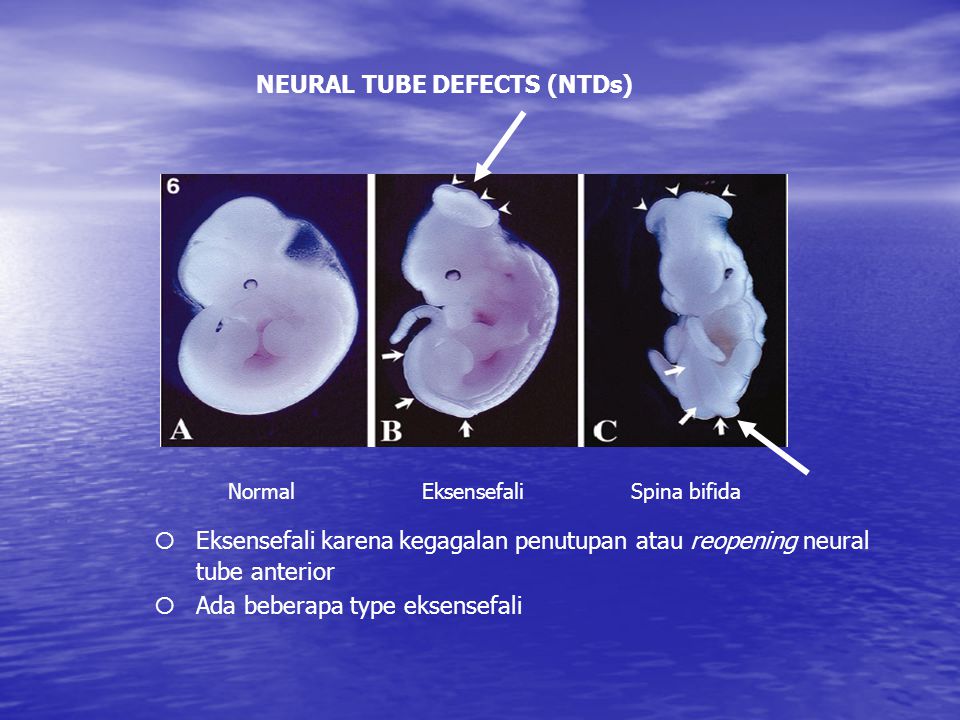
Neural tube defects are abnormalities that occur in the development of the spinal cord and brain of some babies. The most common defects are spina bifida (abnormal development of part of the spine and spinal cord) and anencephaly (severely abnormal development of the brain).
What are neural tube defects?
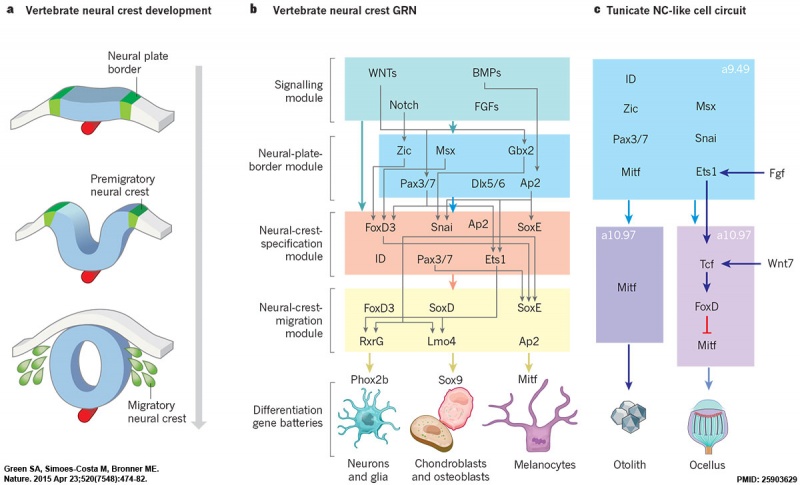
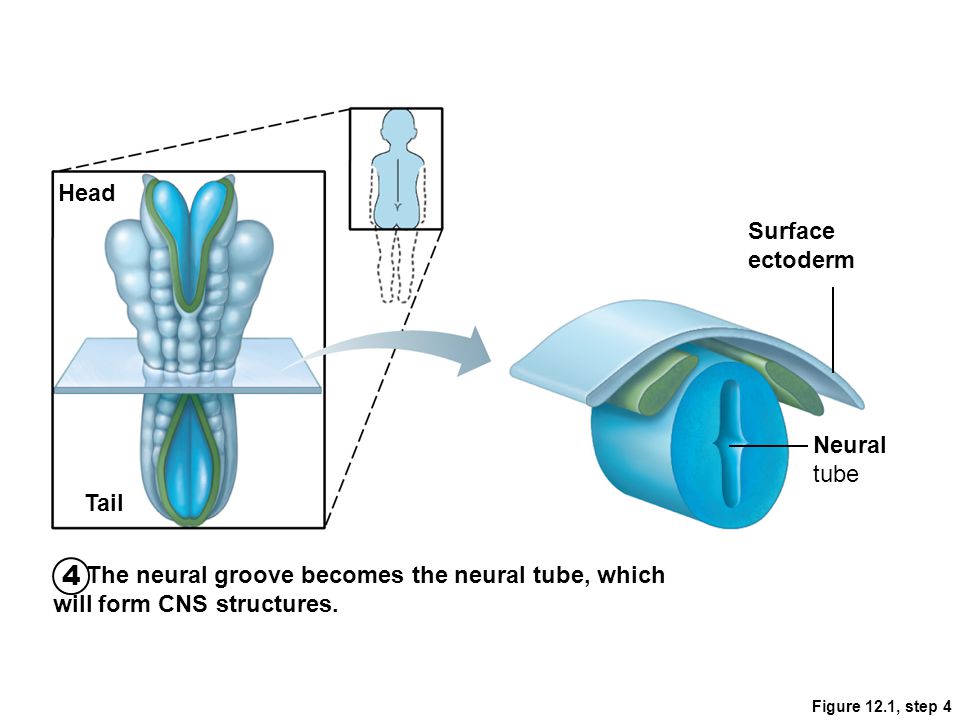
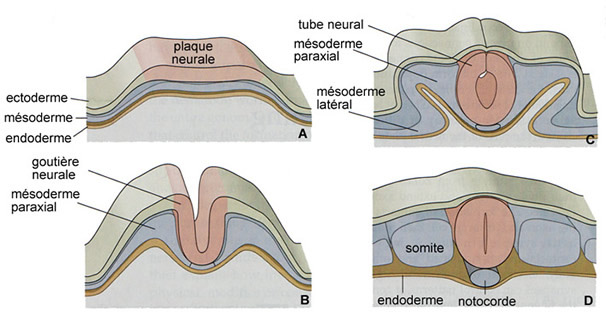
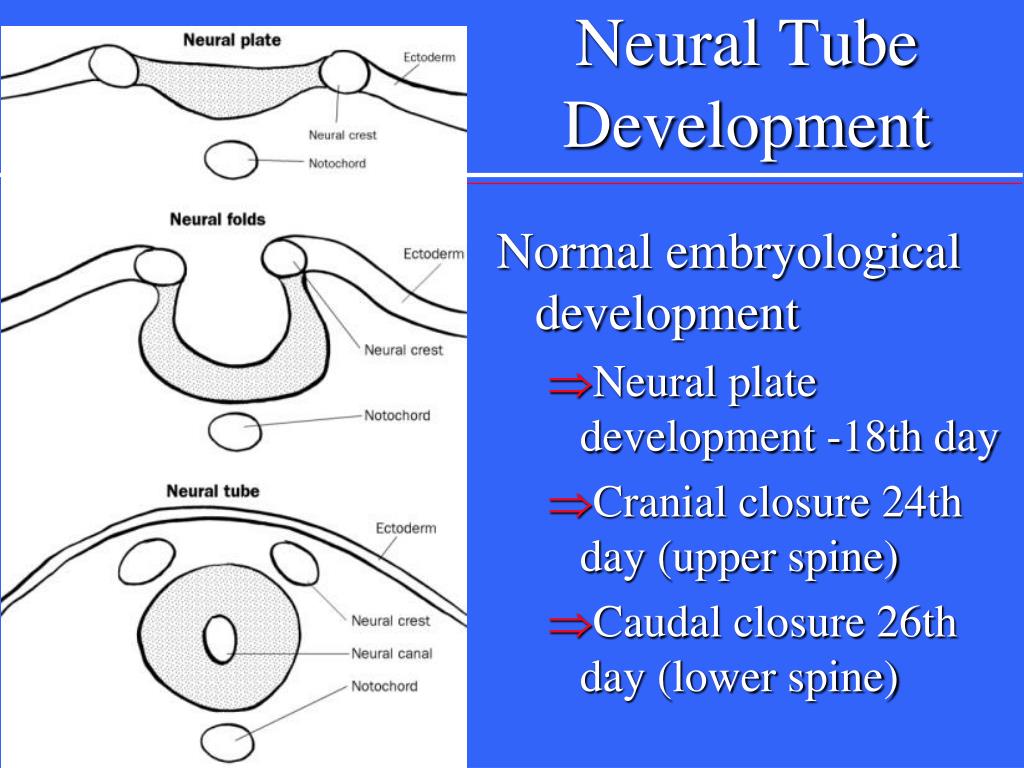
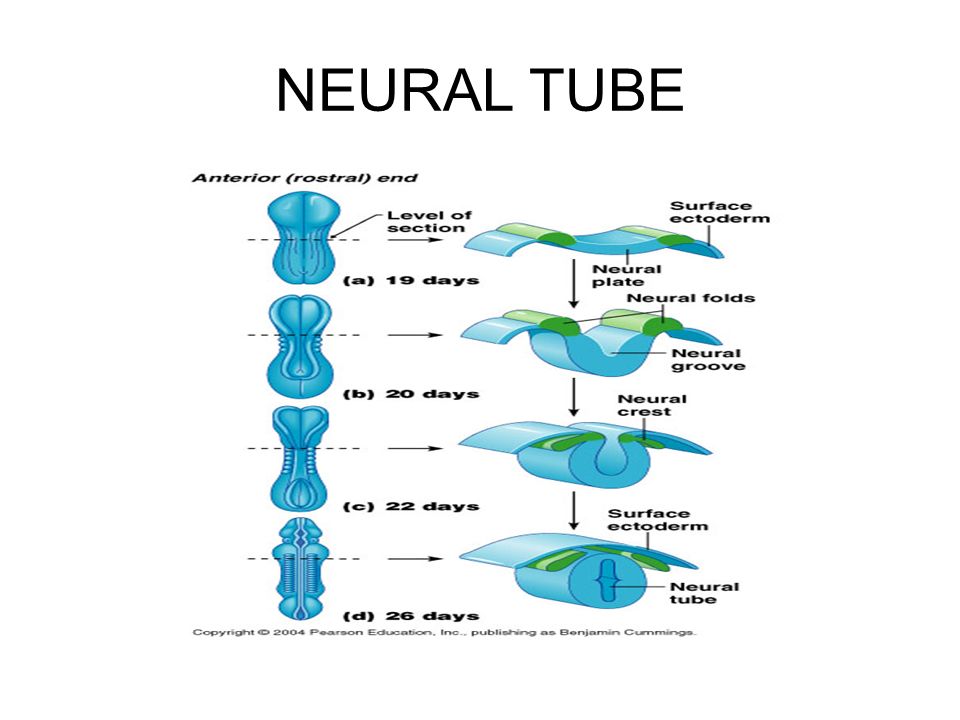
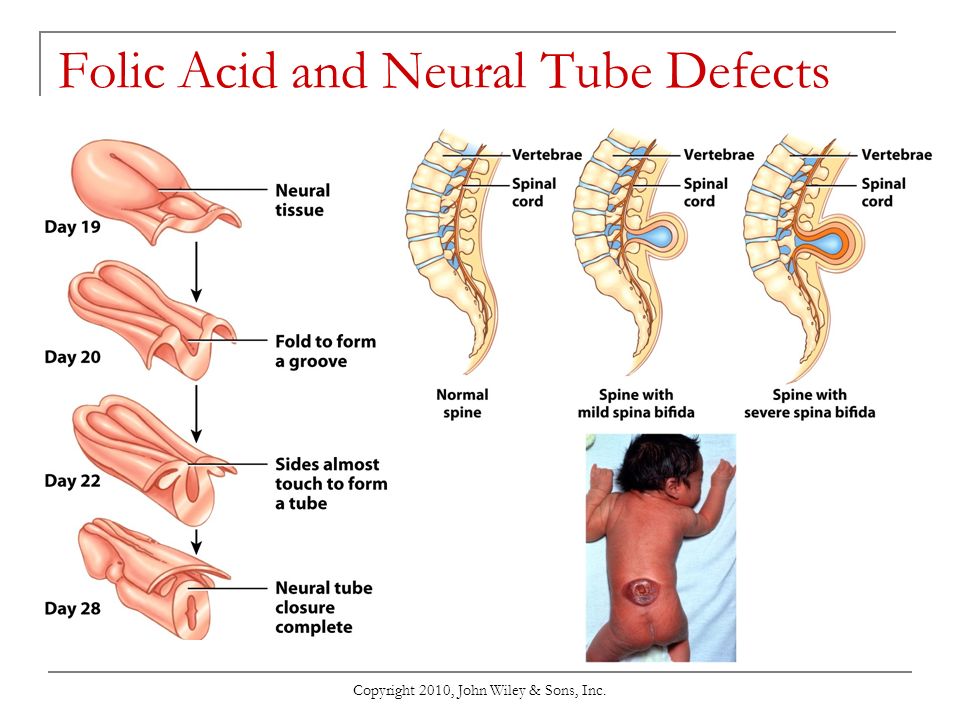
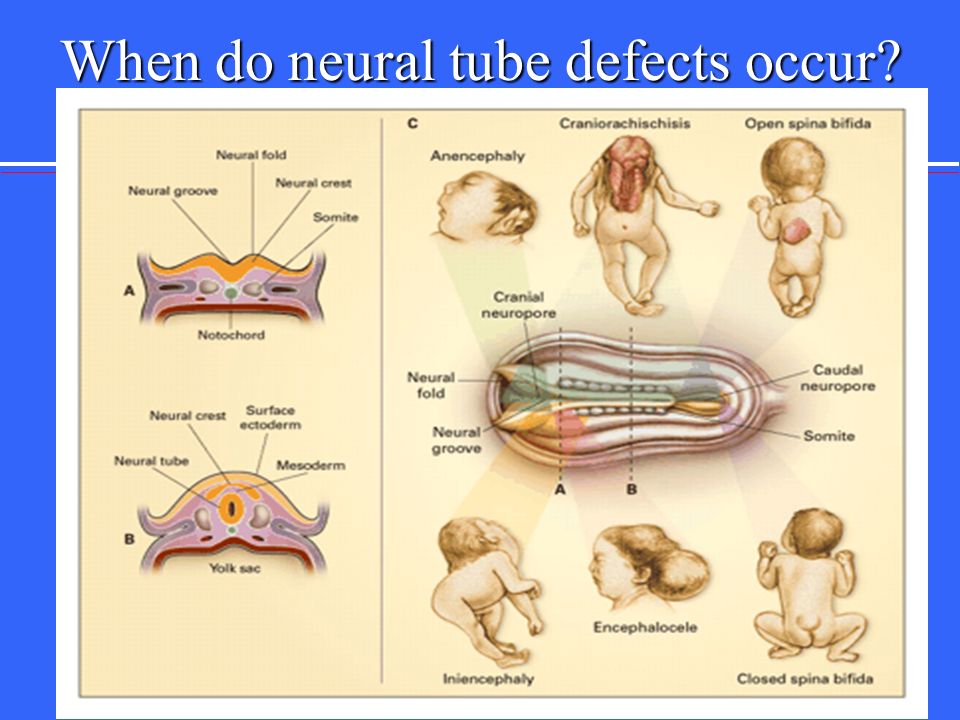
During the first month of life, an embryo (developing baby) grows a primitive tissue structure called the ‘neural tube’. As the embryo develops, the neural tube begins to change into a more complicated structure of bones, tissue and nerves that will eventually form the spine and nervous system.
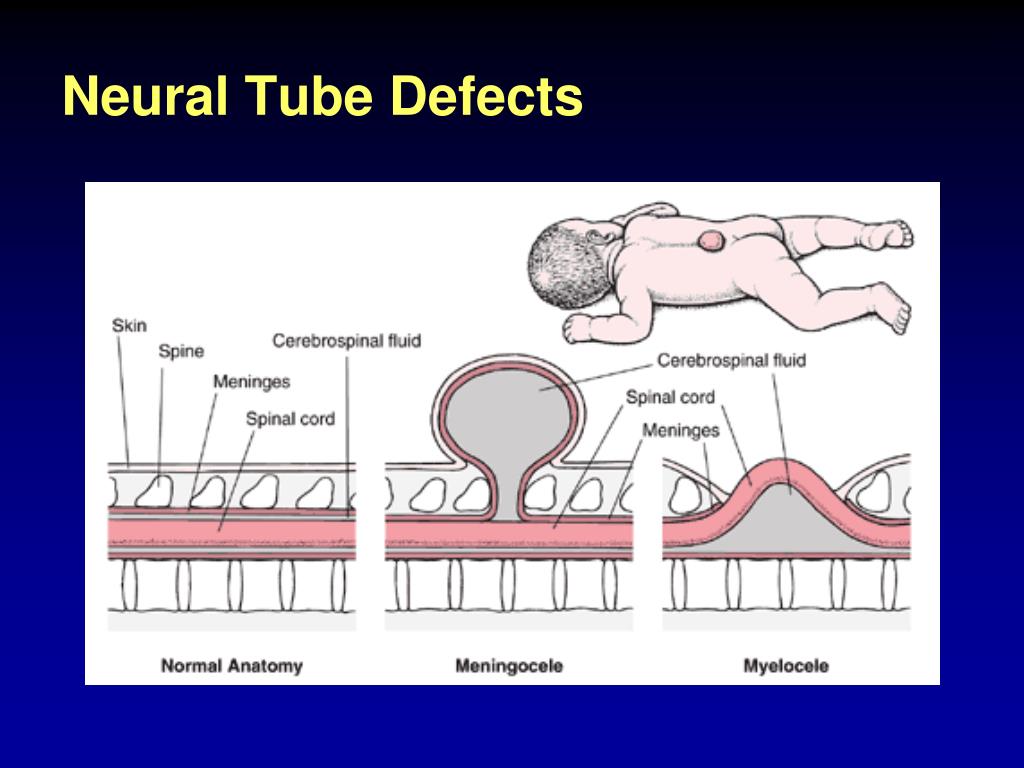
However, in cases of spina bifida, something goes wrong with the development of the neural tube and the spinal column (the ridge of bone that surrounds and protects the nerves) does not fully close. Spina bifida is a Latin term that means ‘split spine’.
The chance that a pregnancy will be affected by a neural tube defect is less than one in 1,000.
What causes neural tube defects?
The cause of neural tube defects is not certain, but it appears to be due to a combination of genetic and environmental factors.
Women are at increased risk of having a baby with a neural tube defect if:
- they have already had a baby with a neural tube defect
- they or their partner have a close relative born with a neural tube defect
- they have type 1 (insulin dependent) diabetes (not gestational diabetes)
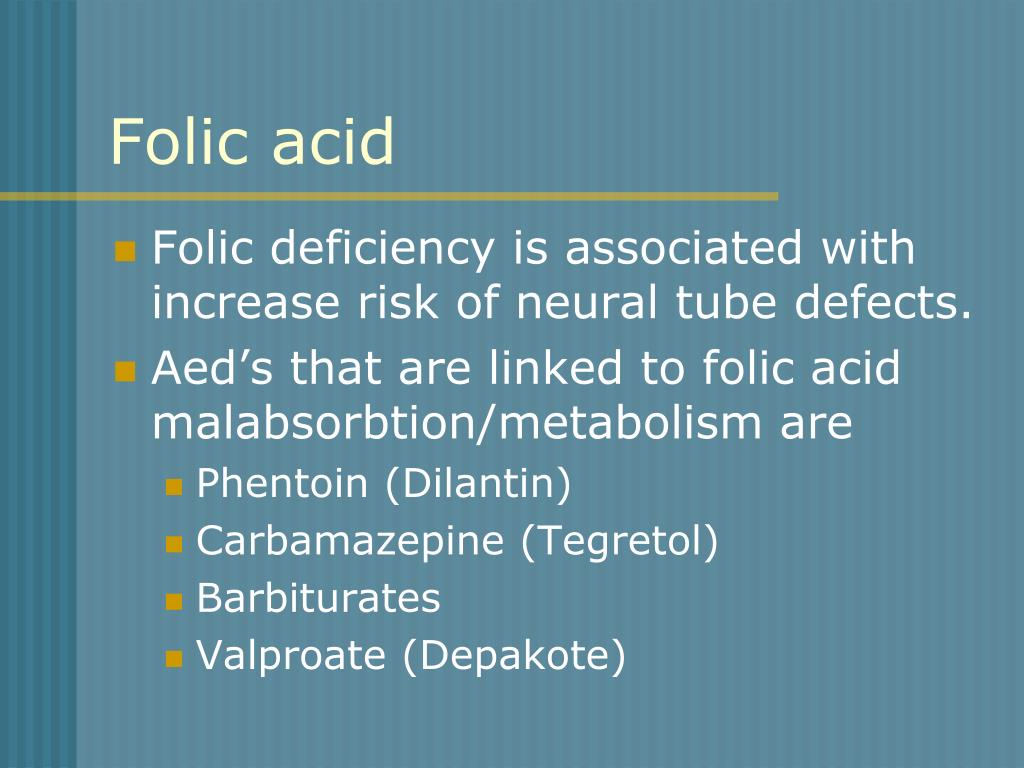
- they are obese, or take certain anti-epileptic medications, especially those containing sodium valproate or valproic acid
Prevention
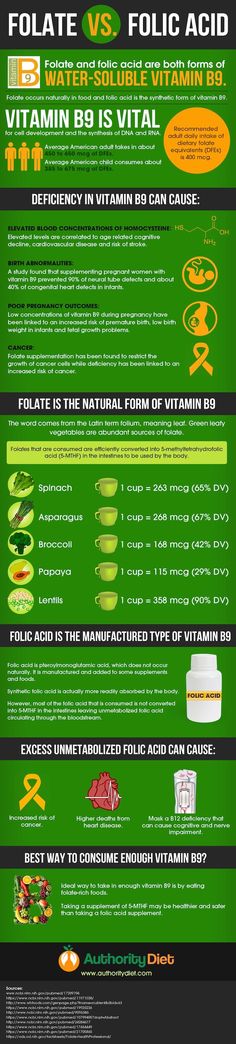
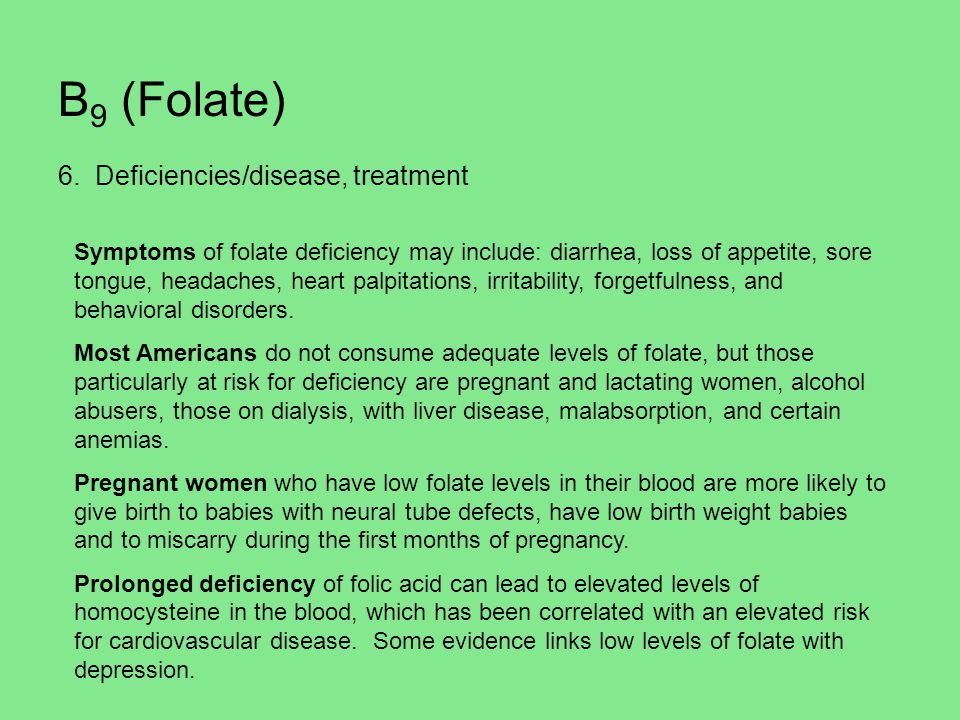
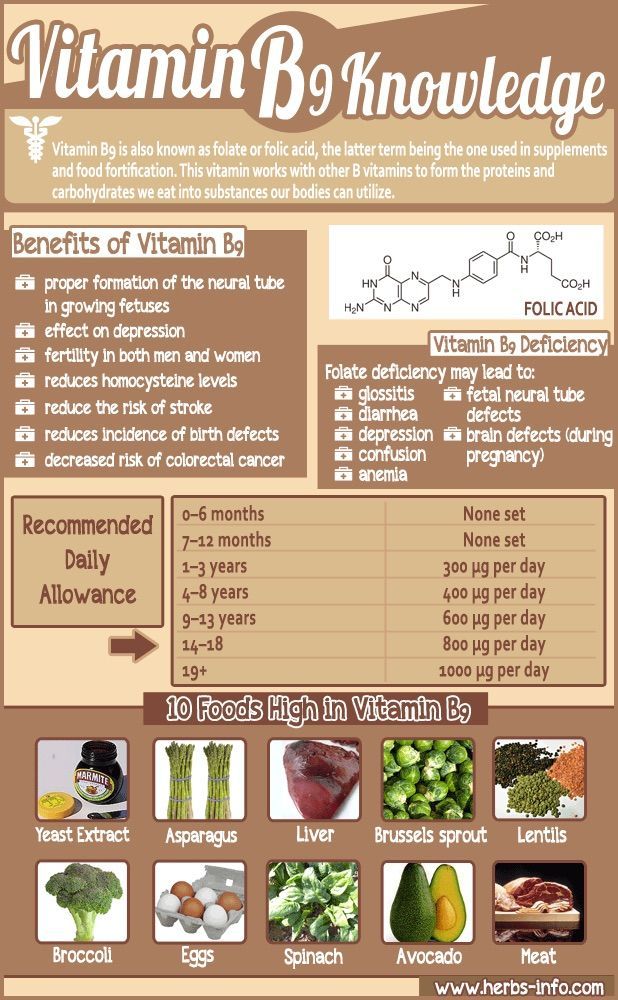
About 2 in 3 neural tube defects can be prevented through increasing folate (folic acid) intake at least a month before pregnancy and during the first 3 months of pregnancy.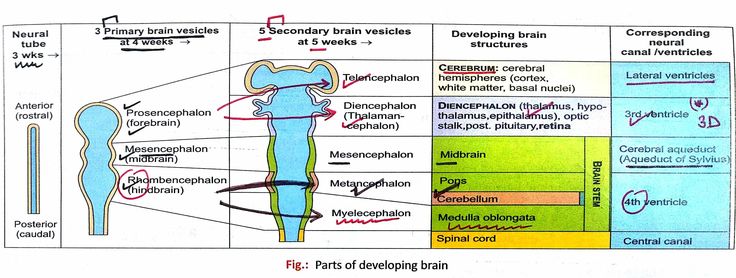 Adequate folate levels are critical during the early days of the developing embryo, particularly the 3rd and 4th week, the period in which neural tube defects occur and when many women won't know they are pregnant.
Adequate folate levels are critical during the early days of the developing embryo, particularly the 3rd and 4th week, the period in which neural tube defects occur and when many women won't know they are pregnant.
You can increase your folate intake by eating folate-rich foods, including folate-fortified foods in your daily diet, or by taking a folic acid supplement. Good sources of folate include green leafy vegetables, fruit (citrus, berries and bananas), legumes and some cereals (bread and many breakfast cereals now have added folate).
Women who take medicines to control epilepsy, seizures or psychiatric disorders should talk to their doctor before taking folate because it can interfere with how their medications work.
For more information see folate and pregnancy.
Diagnosis
Neural tube defects may be diagnosed during the ultrasound scan that is carried out around week 12 of the pregnancy or, more likely, during the anomaly scan that is carried out at around weeks 18 to 20.
Ultrasound scans
An ultrasound scan is a safe procedure that uses sound waves to create an image of the inside of your body. Most hospitals will offer women at least 2 ultrasound scans during their pregnancy. The first is usually at around 8 to 14 weeks and is sometimes called the ‘dating scan’ because it can help to determine when the baby is due. This first scan may be able to detect problems with your baby’s spine that could indicate spina bifida if the condition is severe. If a dating scan is done earlier than 12 weeks, another ultrasound called the nuchal translucency scan is done at 12 weeks to check amongst other things for signs of Down Syndrome, and if a dating scan is not done prior to this then this scan can be used as the dating scan.
Morphology scan
The morphology or anomaly scan is an ultrasound scan that is carried out around weeks 18 to 20 of your pregnancy. This scan aims to identify any physical problems with your baby. It is usually during this scan that spina bifida is diagnosed.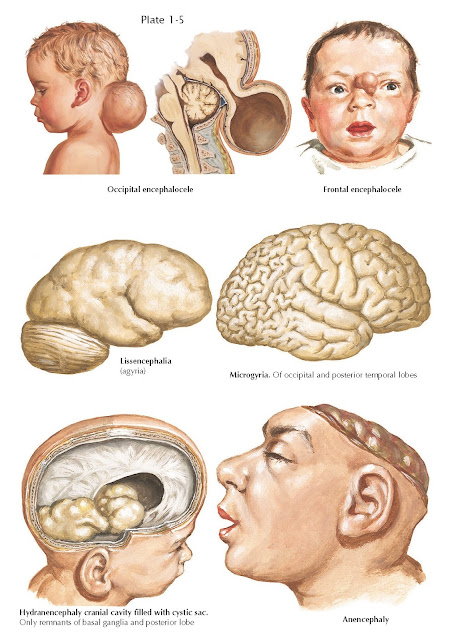
Coping with the results
If tests confirm that your baby has spina bifida, the implications will be fully discussed with you. You will need to consider your options carefully. Your options are to:
- continue with your pregnancy while getting information and advice so that you are prepared for caring for your baby
- end your pregnancy
If you are considering ending your pregnancy, you should talk to your doctor or midwife. They will be able to provide you with important information and advice.
Your options for ending your pregnancy will depend on how many weeks pregnant you are when you make the decision. If you decide to end your pregnancy, you may wish to talk to a counsellor afterwards. Your doctor or midwife will be able to arrange this for you.
Call Pregnancy, Birth and Baby on 1800 882 436 to discuss your options regarding your pregnancy with a maternal child health nurse.
Sources:
Australian Institute of Health and Welfare (Neural tube defects in Australia), The Centre for Genetics Education (Neural tube defects – spina bifida and anencephaly), RANZCOG (Planning for pregnancy), Women's and Children's Health Network (Screening tests for neural tube defects), Sydney Children's Hospital Network (Factsheet: What is spina bifida?)Learn more here about the development and quality assurance of healthdirect content.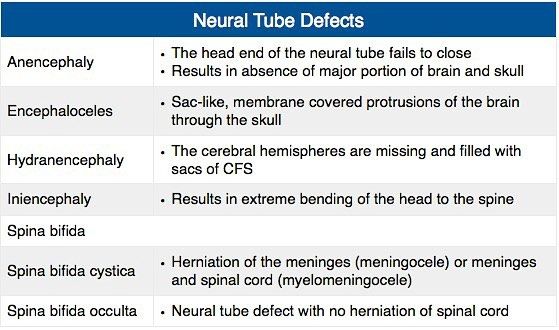
Last reviewed: March 2020
Back To Top
Need more information?
Pregnancy checkups, screenings and scans
Knowing what check-ups, screenings and scans to have and when to have them during your pregnancy is important information for every pregnant woman.
Read more on Pregnancy, Birth & Baby website
Neural tube defects: children & teens | Raising Children Network
Neural tube defects are brain and spinal cord abnormalities, including spina bifida, encephalocele and anencephaly. Read how they affect children.
Read more on raisingchildren.net.au website
Folate and pregnancy
Folate and folic acid are important for pregnancy since they can help prevent birth defects known as neural tube defects, such as spina bifida.
Read more on Pregnancy, Birth & Baby website
Spina bifida
Spina bifida is a condition that affects the normal development of a baby’s spine early in pregnancy.
Read more on Pregnancy, Birth & Baby website
Spina Bifida | Sydney Children's Hospitals Network
Spina Bifida comes from a latin term which means “split spine”
Read more on Sydney Children's Hospitals Network website
Maternal screening - Pathology Tests Explained
Why and when to get tested for maternal screening
Read more on Pathology Tests Explained website
Folic acid & iodine fortification, Summary - Australian Institute of Health and Welfare
Mandatory folic acid and iodine fortification of bread resulted in increased levels of folic acid and iodine in the food supply, increased folic acid and iodine intakes, a decreased rate of neural.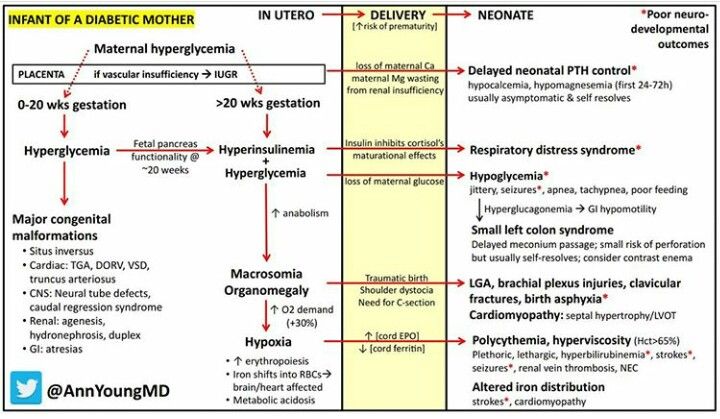 ..
..
Read more on AIHW – Australian Institute of Health and Welfare website
Folate | Jean Hailes
Folate is a B vitamin needed for healthy growing, in particular for the nervous system.
Read more on Jean Hailes for Women's Health website
Pregnancy at weeks 1 to 4
When you conceive, your body’s hormone levels change, but you may not notice any signs that you’re pregnant yet.
Read more on Pregnancy, Birth & Baby website
What supplements should I take during pregnancy? | Queensland Health
Find out what supplements and vitamins you need to take when trying to get pregnant, during pregnancy, after pregnancy and while breastfeeding.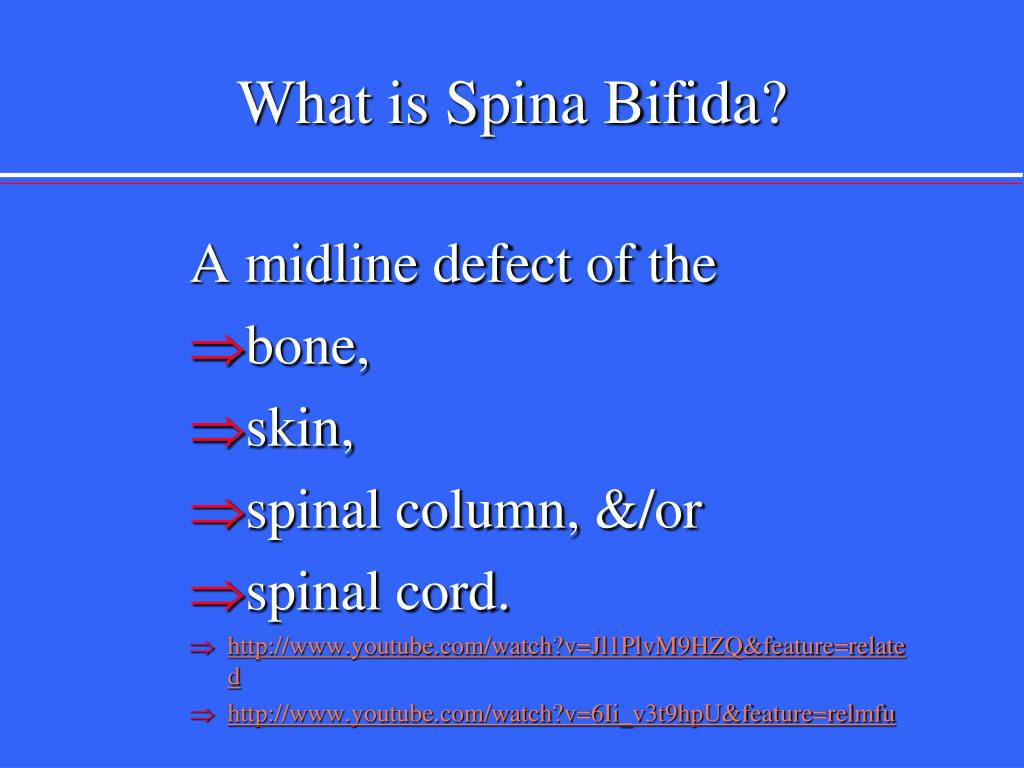
Read more on Queensland Health website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.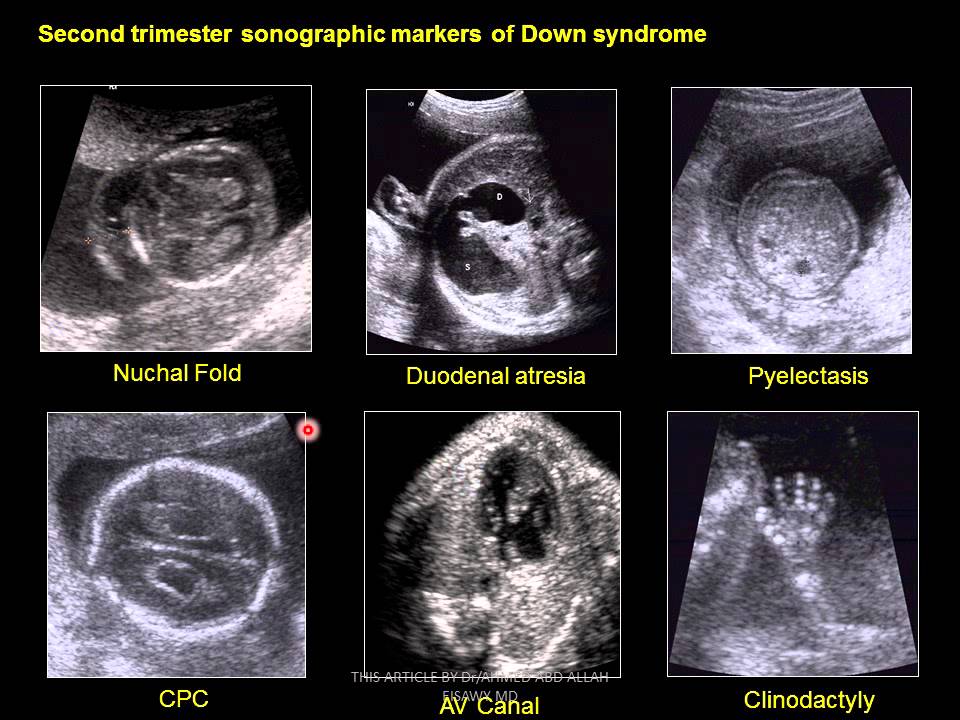
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Neural tube defects
Topics
In This Topic
KEY POINTS
Neural tube defects (NTDs) are birth defects of the brain and spinal cord. NTDs can cause serious problems for babies.
To help prevent NTDs, take a vitamin supplement that has 400 micrograms of folic acid in it every day, even if you’re not trying to get pregnant.
If you’re at high risk for NTDs, take 4,000 micrograms of folic acid every day. Talk to your provider about how to get this much safely.
Your risk for having a baby with an NTD is higher if you, your partner or your family members have an NTD, or if you’ve had a baby with an NTD.
Folic acid helps prevent NTDs only if you take it before and in the first weeks of pregnancy.
What are neural tube defects?
Neural tube defects (also called NTDs) are birth defects of the brain and spinal cord. Birth defects are health conditions that are present at birth. They change the shape or function of one or more parts of the body. Birth defects can cause problems in overall health, how the body develops or how the body works.
A baby’s neural tube normally starts out as a tiny, flat ribbon that turns into a tube by the end of the first month of pregnancy. If the tube doesn’t close completely, an NTD can happen. NTDs can cause serious problems for babies, including death.
NTDs can cause serious problems for babies, including death.
NTDs happen in about 3,000 pregnancies each year in the United States. Hispanic women are more likely than non-Hispanic women to have a baby with an NTD.
The two most common NTDs are spina bifida and anencephaly. Spina bifida affects about 1,500 babies a year in the United States. If your baby has spina bifida, the tiny bones of the spine don’t close completely, and part of the spinal cord pokes through the spine. Children with spina bifida may have paralyzed legs (not able to move) and problems controlling their bladder and bowel (going to the bathroom). Milder forms of spina bifida may cause fewer problems for children.
Anencephaly is one of the most severe NTDs. It affects about 1,000 babies each year in the United States. Anencephaly is caused when the upper part of the neural tube that forms the brain doesn’t close completely. Babies with this condition are missing major parts of the brain, skull and scalp. They do not survive long after birth, usually for just a few hours. Girls are 3 times more likely than boys to have anencephaly.
They do not survive long after birth, usually for just a few hours. Girls are 3 times more likely than boys to have anencephaly.
Taking folic acid before and during early pregnancy can help prevent NTDs in your baby. Folic acid is a B vitamin that every cell in your body needs for normal growth and development.
What causes NTDs?
We’re not exactly sure what causes NTDs. Experts think some may be caused by genetics. This means an NTD can be passed from parents to children through genes. Genes are part of your body’s cells that stores instructions for the way your body grows, looks and works.
NTDs also may be caused by things in your environment, which includes where you live, where you work, the kinds of foods you eat or have access to and how you like to spend your time. Some things in your environment can be harmful to a pregnancy, like certain drugs, cigarette smoke, air pollution and lead.
Are you at risk for having a baby with an NTD?
Any woman can have a baby with an NTD. But there are things that may make you more likely than other women to have a baby with an NTD. These are called risk factors.
But there are things that may make you more likely than other women to have a baby with an NTD. These are called risk factors.
Your risk for having a baby with an NTD is higher if:
- You’ve had a baby with an NTD. If you’ve had a baby with an NTD, there’s a 2- to 3-percent chance of having a baby with an NTD in another pregnancy. A genetic counselor can help you understand your risk for having a baby with an NTD. This is someone who is trained to help you understand medical conditions that run in families, and how they can affect your health and your baby’s health.
- You or your partner has an NTD, your partner has a child with an NTD or someone in either of your families has an NTD. This means you have a family history of NTDs. Use the March of Dimes Family Health History Form to keep track of health conditions, including NTDs, that may run in your family. Fill it out and share it with your health care provider or genetic counselor.
Other risk factors for NTDs include:
- Taking certain anti-seizure medicines. Talk to your health care provider before you get pregnant about how the medicine may affect your pregnancy.
- Obesity. Some studies show that being obese increases your risk for having a baby with an NTD. If you’re obese, you have an excess amount of body fat and your body mass index (BMI) is 30 or higher. To find out your BMI, go to cdc.gov/bmi. Talk to your provider about getting to a healthy weight before pregnancy.
- Diabetes. If your diabetes is uncontrolled, you may be at increased risk for having a baby with an NTD. Eating healthy foods and being active every day can help you keep your diabetes under control.
- Using opioids in the first 2 months of pregnancy. Opioids are highly addictive drugs. Your provider may prescribe an opioid to you as a painkiller if you’ve been injured or had surgery.
 Common prescription opioids include codeine, hydrocodone and oxycodone. These often are sold and used illegally. If you take any opioid during pregnancy, it can cause serious problems for your baby, like premature birth and drug withdrawal called neonatal abstinence syndrome (also called NAS). If you’re pregnant and taking any drug or medicine that may be an opioid, tell your health care provider right away.
Common prescription opioids include codeine, hydrocodone and oxycodone. These often are sold and used illegally. If you take any opioid during pregnancy, it can cause serious problems for your baby, like premature birth and drug withdrawal called neonatal abstinence syndrome (also called NAS). If you’re pregnant and taking any drug or medicine that may be an opioid, tell your health care provider right away. - A high body temperature early in pregnancy. This may be caused by a fever or by spending a lot of time in a hot tub or sauna. If you’re pregnant, stay out of hot tubs and saunas. If you do use them, limit the time to less than 10 minutes.
How can you help prevent NTDs in your baby?
Taking folic acid before and during early pregnancy can help prevent NTDs in your baby. NTDs happen in the first month of pregnancy, before you may know you’re pregnant. This is why it’s important to have enough folic acid in your body before you get pregnant.
Most women
To help prevent NTDs in your baby, take a vitamin supplement with 400 mcg of folic acid every day before getting pregnant. A supplement is a product you take to make up for certain nutrients that you don’t get enough of in the foods you eat. Start taking this amount of folic acid each day at least 1 month before pregnancy and through the first 12 weeks of pregnancy. Your folic acid supplement can be:
- A multivitamin. This is a pill that contains many vitamins and other nutrients that help your body stay healthy.
- A prenatal vitamin. This is a multivitamin that has nutrients you need during pregnancy. Your health care provider may give you a prescription for prenatal vitamins, or you can get them over the counter without a prescription.
- A supplement that contains just folic acid
Take a vitamin supplement with 400 mcg of folic acid each day, even if you’re not trying to get pregnant.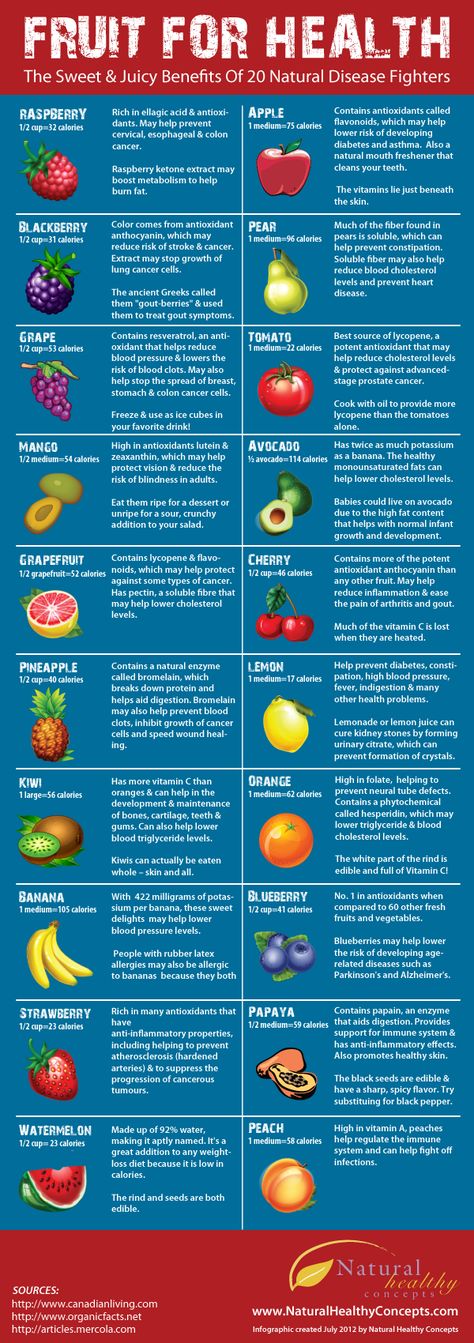
Women at high risk for NTDs
If you’re at high risk for having a baby with an NTD, it’s recommended you take 4,000 mcg of folic acid each day to help prevent an NTD. Start taking 4,000 mcg 3 months before you get pregnant through 12 weeks of pregnancy. You’re at high risk if:
- You’ve had a pregnancy with an NTD in the past.
- You or your partner has an NTD.
- Your partner has a child with an NTD.
Studies show that taking 4,000 mcg of folic acid before and during early pregnancy can help reduce your risk of having another baby with an NTD by about 70 percent. Ask your provider how to safely get this much folic acid. It’s not safe to take several multivitamins or prenatal vitamins because you can get too much of other nutrients, which may be harmful to your health. Your provider can help you figure out the best and safest way for you to get the right amount of folic acid.
Can you get folic acid from food?
Yes! You can get folic acid from foods that are fortified with folic acid.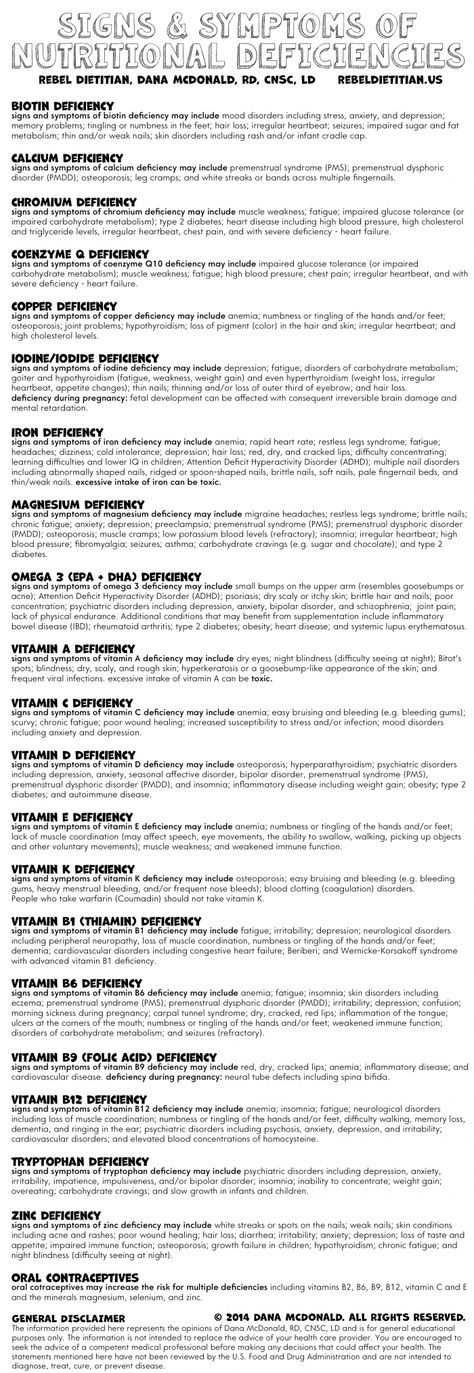 Fortified means a food has folic acid added to it. Check the product label to see how much folic acid you get in each serving. Look for the word “fortified” or “enriched” on labels on foods like:
Fortified means a food has folic acid added to it. Check the product label to see how much folic acid you get in each serving. Look for the word “fortified” or “enriched” on labels on foods like:
- Bread
- Breakfast cereal
- Cornmeal
- Flour
- Pasta
- Products made from a kind of flour called corn masa, like tortillas, tortilla chips, taco shells, tamales and pupusas
- White rice
Some fruits and vegetables are good sources of folic acid. When folic acid is naturally in a food, it’s called folate. Foods that are good sources of folate are:
- Beans, like lentils, pinto beans and black beans
- Leafy green vegetables, like spinach and Romaine lettuce
- Asparagus
- Broccoli
- Peanuts (But don’t eat them if you have a peanut allergy.)
- Citrus fruits, like oranges and grapefruit
- Orange juice (100 percent juice is best. This means one serving of juice is equal to one serving of fruit.
 )
)
It’s hard to get all the folic acid you need from food. Even if you eat foods that have folic acid in them, take your vitamin supplement each day, too.
Can you find out if your baby has an NTD before birth?
Yes. You can get prenatal tests (medical tests you get during pregnancy) called screening tests to find out if your baby is at increased risk of having an NTD. Screening tests for NTDs include:
- Maternal blood screening (also called a quad screen). It’s called a quad screen because it measures four substances in your blood. The test is done between 15 to 22 weeks of pregnancy.
- Ultrasound. This test uses sound waves and a computer screen to show a picture of your baby inside the womb. You usually get an ultrasound at 16 to 20 weeks of pregnancy.
If a screening test shows an increased risk of NTDs, your provider may recommend a diagnostic test to find out for sure if your baby has an NTD. Diagnostic tests for NTDs include:
- Amniocentesis.
 In this test, your provider takes some amniotic fluid from around your baby in the uterus (womb) to check for birth defects, like NTDs, in your baby. You can get this test at 15 to 20 weeks of pregnancy.
In this test, your provider takes some amniotic fluid from around your baby in the uterus (womb) to check for birth defects, like NTDs, in your baby. You can get this test at 15 to 20 weeks of pregnancy. - Detailed ultrasound of your baby’s skull and spine
If you find out that your baby has an NTD, talk to your health care provider to learn more about your baby’s condition and options for birth and treatment. For example:
- You can plan to have your baby in a hospital that specializes in caring for babies with NTDs. This way your baby can have any necessary surgery or treatment soon after birth.
- You can decide whether to have a vaginal or cesarean birth (also called c-section). During vaginal birth, the uterus contracts to help push the baby out through the vagina. A c-section is surgery in which your baby is born through a cut that your doctor makes in your belly and uterus. In some cases, a c-section may be safer for you and your baby than vaginal birth.
- If your baby has spina bifida, you can find out about surgery for your baby in the womb before birth. Surgery to repair spina bifida in the womb before birth is more effective than surgery after birth.
More information
- American Academy of Pediatrics
- Spina Bifida Association
- Centers for Disease Control and Prevention
Last reviewed: February, 2022
') document.write('
Preterm labor & premature birth
') document.write('') }
') document.write('') }
Principles for the prevention of fetal neural tube defects
03/27/2015
Despite significant advances in modern prenatal diagnosis, neural tube defects (NTD) of the fetus are still one of the most common congenital malformations.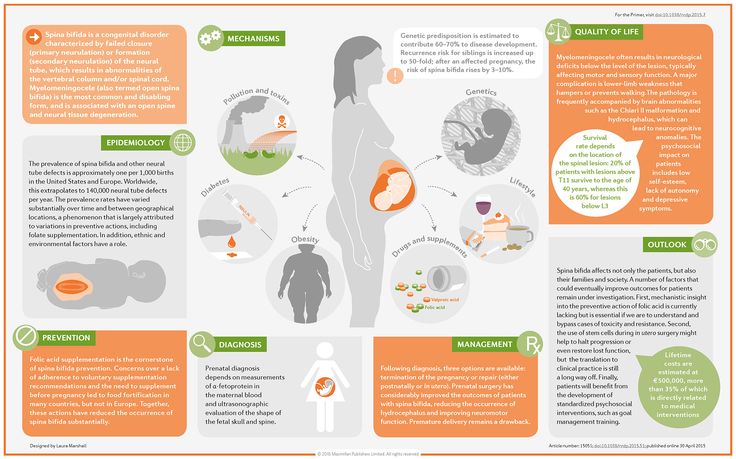 Annually in the USA, 1 case of NTD is registered per 1000 pregnancies, while 4000 pregnancies per year are terminated, including spontaneous miscarriage and induced abortion, due to fetal CNS developmental disorders. The annual incidence of fetal NTD in Russia is 0.45%; mortality due to NTD - 300 newborns (2% of total infant mortality).
Annually in the USA, 1 case of NTD is registered per 1000 pregnancies, while 4000 pregnancies per year are terminated, including spontaneous miscarriage and induced abortion, due to fetal CNS developmental disorders. The annual incidence of fetal NTD in Russia is 0.45%; mortality due to NTD - 300 newborns (2% of total infant mortality).
NTD, or spina bifida, is a significant factor in disability, although some forms of this pathology are currently amenable to surgical correction.
In most cases, NTDs result from failure of the ends of the neural tube to close or reopen. In humans, the neural tube is formed from the ectoderm, its closure occurs on the 21-28th day after conception. If the formation of the neural tube is disturbed, depending on the location of the defect, either anencephaly or spina bifida is formed, which is clinically manifested by paralysis of the lower extremities, bladder, rectum, etc.
The occurrence of NTD is due to both hereditary factors and the influence of the external environment. Among hereditary features, one can single out gender and ethnic differences, an increased degree of concordance in monozygotic twins, gene mutations and chromosomal abnormalities (a small number of NTDs). It is necessary to take into account the fact of the birth of children with NTD in history and hereditary history. Drugs that interfere with folate metabolism (trimethoprim, sulfasalazine, carbamazepine, phenytoin, valproic acid and other anticonvulsants, etc.), alcohol abuse, methanol can increase the risk of NTD. Acquired factors that can lead to the occurrence of NTD include diabetes mellitus, hyperthermia, smoking, etc. Factors such as place of residence, time of year at which conception occurred, mother's age, socio-economic conditions, as well as the nutritional factor.
Among hereditary features, one can single out gender and ethnic differences, an increased degree of concordance in monozygotic twins, gene mutations and chromosomal abnormalities (a small number of NTDs). It is necessary to take into account the fact of the birth of children with NTD in history and hereditary history. Drugs that interfere with folate metabolism (trimethoprim, sulfasalazine, carbamazepine, phenytoin, valproic acid and other anticonvulsants, etc.), alcohol abuse, methanol can increase the risk of NTD. Acquired factors that can lead to the occurrence of NTD include diabetes mellitus, hyperthermia, smoking, etc. Factors such as place of residence, time of year at which conception occurred, mother's age, socio-economic conditions, as well as the nutritional factor.
The incidence of NTD varies from 2 (Mexico and Ireland) to 0.2 (Finland and Japan) per 1000 births, and the recurrence rate in subsequent pregnancies is 2%. Despite its low prevalence, spina bifida is the most common birth defect and results in disability.
DNT were described by the ancient Egyptians, and in 1641 N. Tulp first depicted spina bifida. The alimentary factor was one of the first to be recognized as a risk factor for the development of spina bifida. Stein et al. noted a high incidence of NTDs in 18-year-old boys entering the military who were born during the famine at the end of World War II. Hibbard and Smithells further showed that women who gave birth to children with NTDs experienced vitamin deficiencies during pregnancy. According to their observations, as a result of taking multivitamin complexes, the frequency of recurrence of this pathology in subsequent pregnancies was sharply reduced.
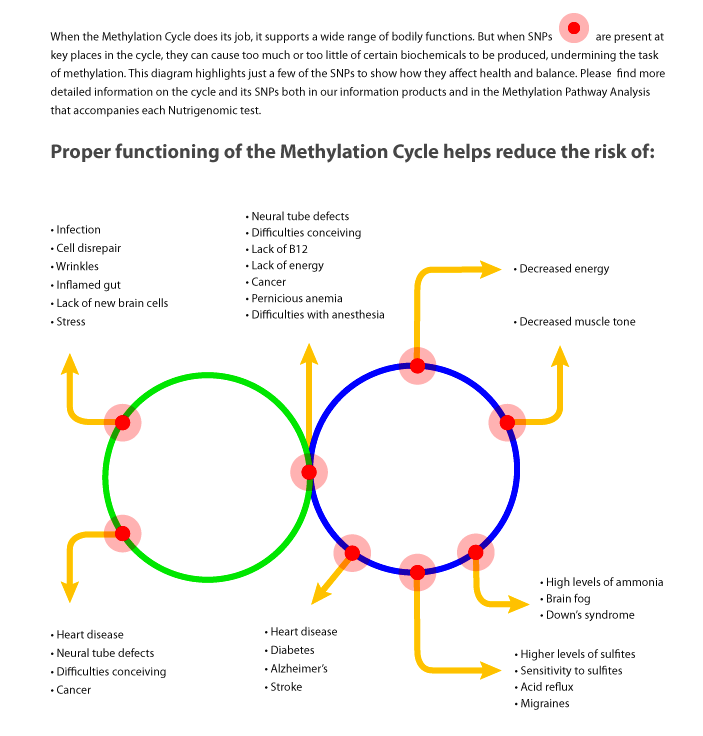
R.P. Steegers-Theunissen et al. for the first time suggested the existence of a link between the violation of folate-dependent processes of homocysteine (HC) metabolism and the development of NTD. Subsequently, they showed that the risk of spina bifida formation increases with an increase in the concentration of HC in the blood, and folic acid intake, in turn, reduces the content of HC in the blood plasma of pregnant women. The concentration of HC in the amniotic fluid in newborns born with NTD was higher than in the control group. When studying the metabolism of methionine in the extraembryonic and amniotic fluids, it was shown that the concentration of total HC in the embryonic fluid is significantly lower than in the mother's blood plasma, and the concentration of methionine is four times higher in the extraembryonic coelomic fluid and two times higher in the amniotic fluid compared to maternal plasma.
The concentration of HC in the amniotic fluid in newborns born with NTD was higher than in the control group. When studying the metabolism of methionine in the extraembryonic and amniotic fluids, it was shown that the concentration of total HC in the embryonic fluid is significantly lower than in the mother's blood plasma, and the concentration of methionine is four times higher in the extraembryonic coelomic fluid and two times higher in the amniotic fluid compared to maternal plasma.
In Denmark N.M. van der Put et al. revealed an increased frequency of C677T polymorphism of the gene encoding the enzyme methylenetetrahydrofolate reductase (MTHFR) in members of families in which children with NTD were born. The gene mutation was detected in 16% of mothers, 10% of fathers and 13% of newborns with spina bifida compared to 5% in the control group. Similar results have been obtained in other countries. This study shows that the risk of developing spina bifida increases seven-fold when a homozygous mutation in the mother and fetus is combined.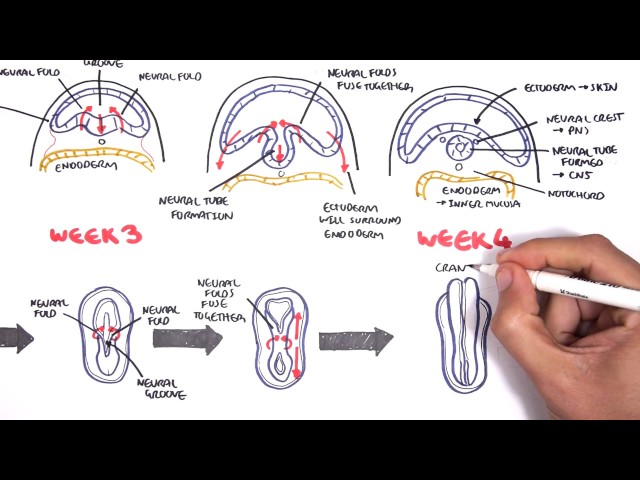 This proves the influence of HC metabolism disorders in the fetus on the development of NTD.
This proves the influence of HC metabolism disorders in the fetus on the development of NTD.
The severity of spina bifida can be different - from erased forms to gross defects with spina bifida in combination with myeloschisis.
The severity of spina bifida is distinguished:
Vertebral dermal sinus
Hidden cleft of the vertebral arch;
cystic cleft of the arch;
Spina bifida associated with myeloschisis.
Despite the fact that NTDs have been known to man since ancient times, all the mechanisms for the development of this defect are still unclear, although there is no doubt that genetic factors, unbalanced nutrition (deficiency of folates and B vitamins), hyperhomocysteinemia (HHC), factors environment (radioactive radiation, etc.).
Most studies in recent years demonstrate the impact of disturbances in the metabolism of folate in the methionine cycle on the pathogenesis of NTD. Since these processes are inextricably linked with each other, deficiency or defects of any cofactor (B vitamins, folates) and enzymes, which can be either acquired or genetically determined, lead either to HHC or to erased or pronounced forms of folate deficiency states.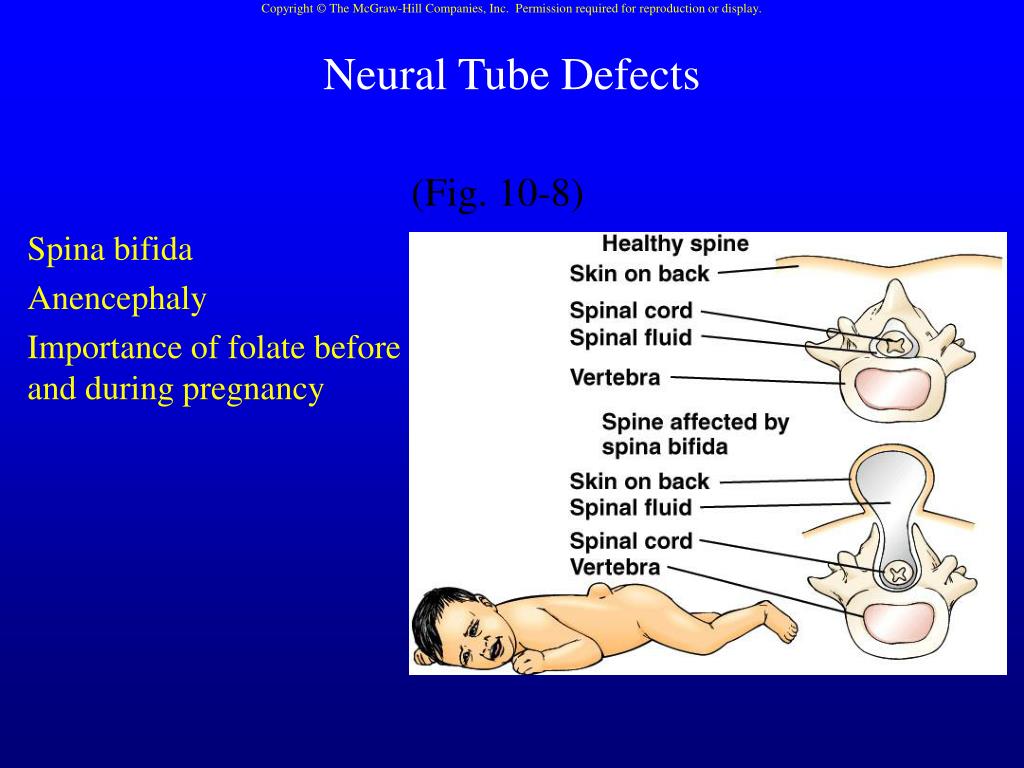
Many of the pathological effects of folate deficiency are associated with increased plasma levels of HC. The role of folates in the development of NTDs has been known for over 40 years, and the role of vitamins B 12 and B 6 were installed much later. Intracellular vitamin B 12 acts as a factor in the remethylation of HC to methionine with the participation of the enzyme methionine synthetase (MS). Vitamin B deficiency 12 can thus cause HHC, although blood folate levels may be normal or even elevated. This phenomenon is known as the "methylfolate trap".
It should be emphasized that the combination of HHC and folate deficiency, including with a lack of B vitamins, especially vitamin B 6 , is a powerful risk factor for the development of not only NTD, but also vascular complications: venous and arterial thrombosis, preeclampsia, premature detachment of a normally located placenta, fetoplacental insufficiency and fetal growth retardation syndrome, antenatal fetal death, early and late miscarriages.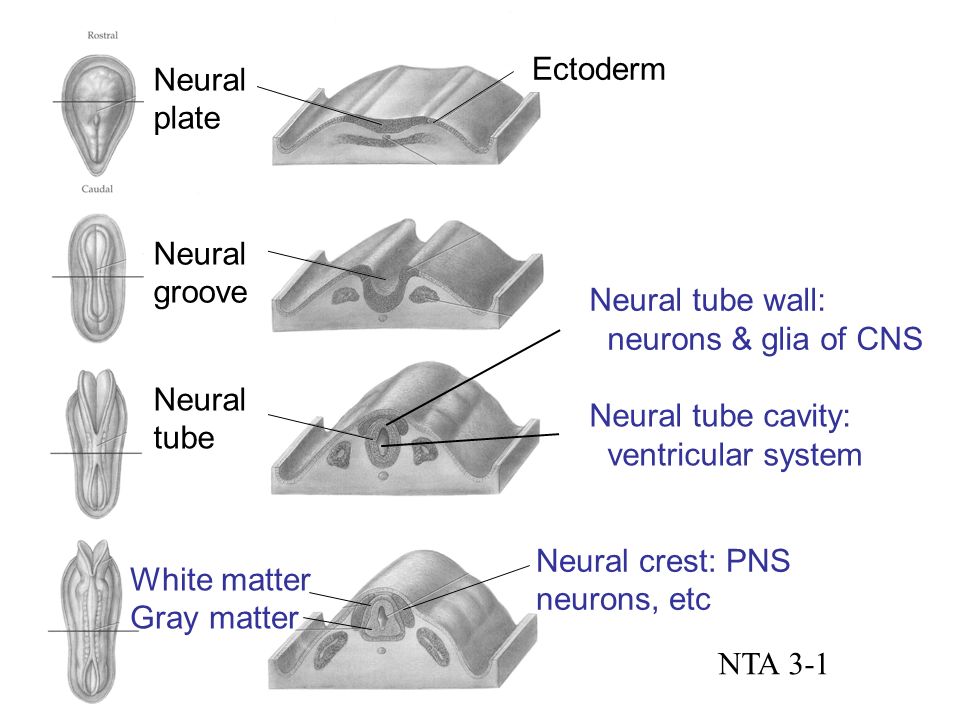 Vitamin B 6 in the form of pyridoxol-5-phosphate, it participates in the transsulfation of HC to cysteine with the help of the enzyme cystathionine-beta-synthetase (CBS).
Vitamin B 6 in the form of pyridoxol-5-phosphate, it participates in the transsulfation of HC to cysteine with the help of the enzyme cystathionine-beta-synthetase (CBS).
The metabolism of HC is inextricably linked to the methionine cycle. The synthesis of HC (in high concentrations - a cytotoxic amino acid) is the result of the formation of labile methyl groups due to the chemical processes of the methionine cycle. The formation of HC occurs in all cells, but the ways of its utilization differ. Most cells and tissues are able to remethylate HC (with the participation of folates, vitamin B 12 ), and only a few can carry out transsulfation processes. This, apparently, can explain the high efficiency of folic acid and B vitamins in reducing the level of HC in blood plasma.
The nervous tissue uses the following mechanisms to maintain the concentration of HC at the proper level:
remethylation with the participation of methionine synthetase with a normal content of vitamin B 12 and folates;
the transition of HC under the action of the enzyme cystathionine-beta-synthetase into cystathionine, which is a less toxic product for the brain and is subsequently used for the synthesis of cysteine;
export of HC to the blood.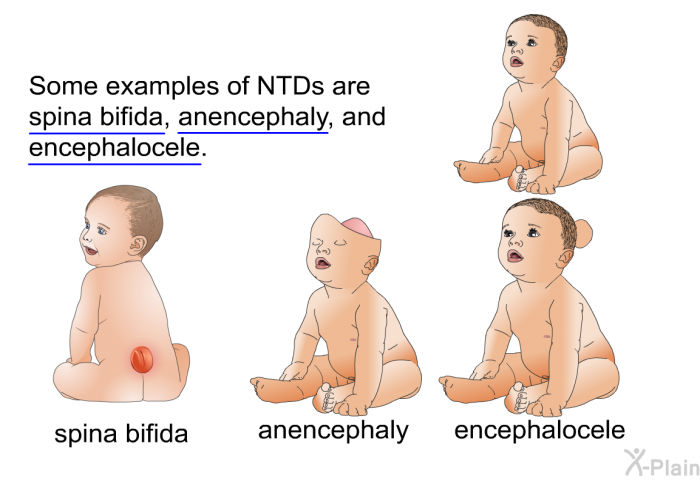
In the nervous system, as in other organs, HC metabolism disorders can occur as a result of genetic disorders, after taking various drugs and under the influence of other acquired factors.
The concentration of HC in the blood of pregnant women is 50-60% lower than outside pregnancy. Pregnancy is characterized by a change in the hormonal profile, an increase in circulating blood volume, cardiac output, peripheral vasodilation, changes in kidney function, and an increase in body weight. Possible reasons for the decrease in the concentration of HC are hemodilution, increased synthesis of steroids, as well as the consumption of methionine and HC by the growing fetus.
A number of studies have shown that oral contraceptives (OCs), containing even less than 50 micrograms of estrogen (in modern preparations - no more than 35 micrograms), disrupt the kinetics of folates, and in the blood of women using OCs, the content of vitamin A is increased and the concentration of vitamin B is reduced 12 and folic acid.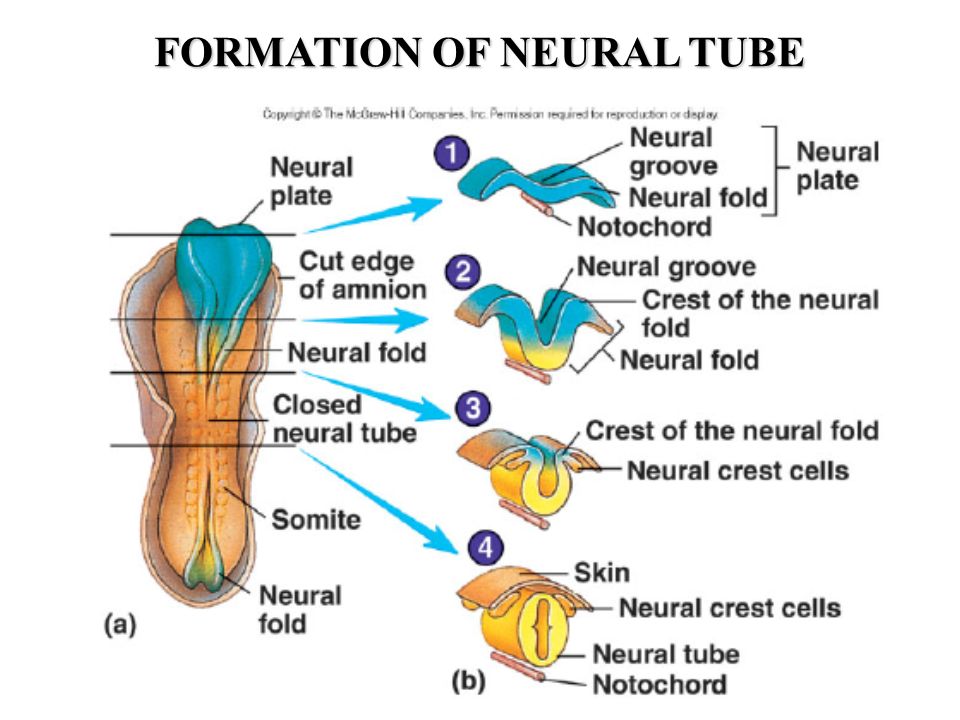 Thus, the risk of developing NTD is higher in patients who became pregnant immediately after long-term use of OCs, especially in the presence of genetic mutations in enzymes (MTHFR, MS, etc.), and who did not additionally take folic acid and B vitamins.
Thus, the risk of developing NTD is higher in patients who became pregnant immediately after long-term use of OCs, especially in the presence of genetic mutations in enzymes (MTHFR, MS, etc.), and who did not additionally take folic acid and B vitamins.
Studies on the role of vitamin B 12 in the process of HC remethylation and in the genesis of the development of NTDs, have been carried out in the last 5-10 years. It is proved that the participation of vitamin B 12 as a cofactor provides a more complete and rapid absorption of folic acid by cells. Study by M. Paskal et al. on vitamin B content 12 in the blood plasma of mothers who gave birth to children with spina bifida, showed that a decrease in the concentration of vitamin B 12 in maternal serum levels below 185 mmol / l correlates with a 3.5-fold increase in the risk of having a child with spina bifida. Average concentrations of vitamin B 12 in mothers of the spina bifida group were 21% less compared to the control group, while the differences between the concentrations of folate, vitamin B 6 and HC in blood serum and erythrocytes was not observed.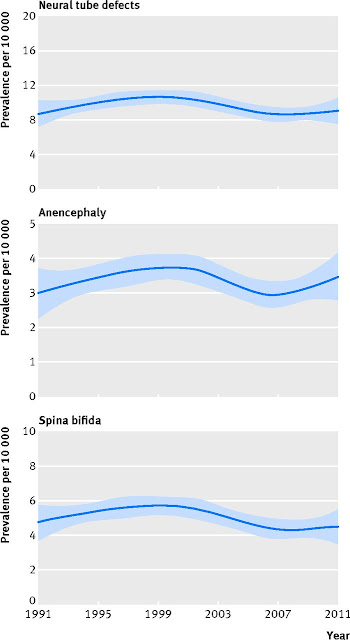 These data confirm the multifactorial nature of the origin of NTDs and the need to include vitamin B 12 along with folate in the prevention of fetal NTDs.
These data confirm the multifactorial nature of the origin of NTDs and the need to include vitamin B 12 along with folate in the prevention of fetal NTDs.
A special risk group for deficiency of folates and vitamins of group B are patients who have received hormonal contraception for a long time, as well as smokers, coffee abusers (more than 5 cups a day) and, of course, patients with genetic factors (mutation MTHFR, CBS, transcobalamin), malabsorption , unbalanced nutrition, diagnosed with HHC and fetal NTD in history. It should also be taken into account that up to 80% of women aged 18 to 40 have suboptimal blood folate concentrations.
Prophylactic administration of folates and B vitamins, as well as dietary adjustments, significantly reduce the incidence of neural tube defects in the fetus. Thus, in Dublin, cereals (grain fortification), which are an important part of the Irish diet, were enriched with vitamin B 12 (1981) and folic acid (1987), which led to a decrease in the frequency of birth of children with NTD from 4.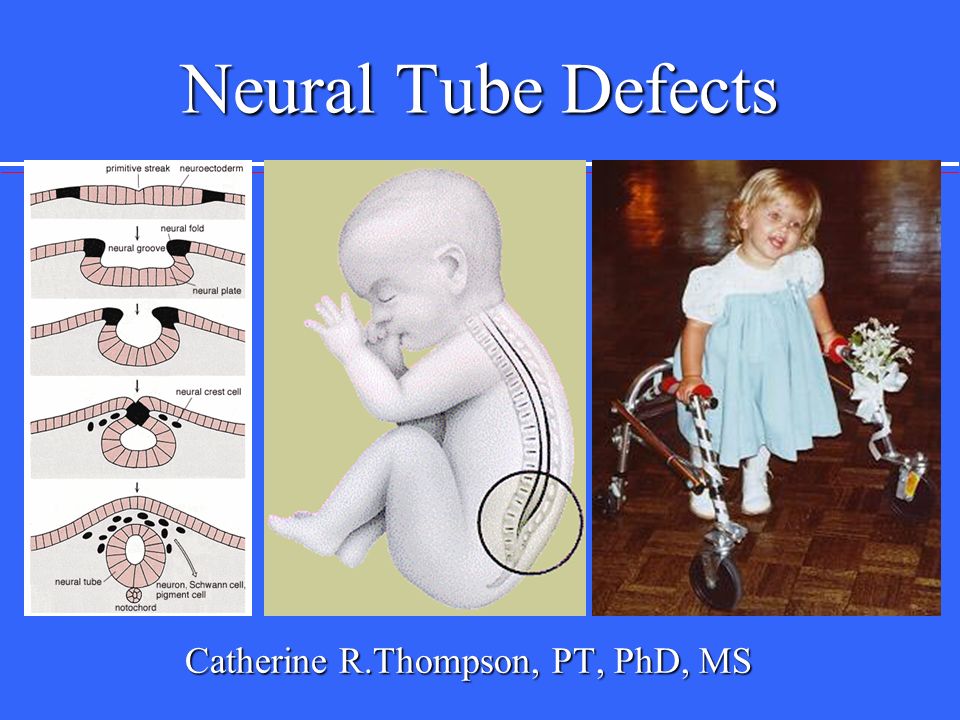 7 to 1.3 per 1000 newborns. NTD prevention has become a National Health Program in many developed countries. For example, the United States and Canada introduced a program to fortify grains with folates to reduce the risk of having children with NTDs, which resulted in a decrease in the number of newborns with NTDs by 19% (M.A. Honein et al., 2001). In a number of countries, there is a preference for programs aimed at the preventive use of folate-containing drugs by women of childbearing age. Thus, according to a multicenter study conducted in 33 clinical centers in England (1817 women examined), more than 75% of cases of NTD can be prevented by prescribing folic acid and vitamin B 12 .
7 to 1.3 per 1000 newborns. NTD prevention has become a National Health Program in many developed countries. For example, the United States and Canada introduced a program to fortify grains with folates to reduce the risk of having children with NTDs, which resulted in a decrease in the number of newborns with NTDs by 19% (M.A. Honein et al., 2001). In a number of countries, there is a preference for programs aimed at the preventive use of folate-containing drugs by women of childbearing age. Thus, according to a multicenter study conducted in 33 clinical centers in England (1817 women examined), more than 75% of cases of NTD can be prevented by prescribing folic acid and vitamin B 12 .
Current issues of optimal prevention of fetal NTDs are the duration of use and the dose of folic acid. According to the recommendations of various international organizations (including the Food and Drug Administration, USA; March of Dimes CDC-Alanta - Spina Bifida Assotiation Public Health Service; Reino Unido Junta de Sanidad y Consumo de Espana, 2001, etc.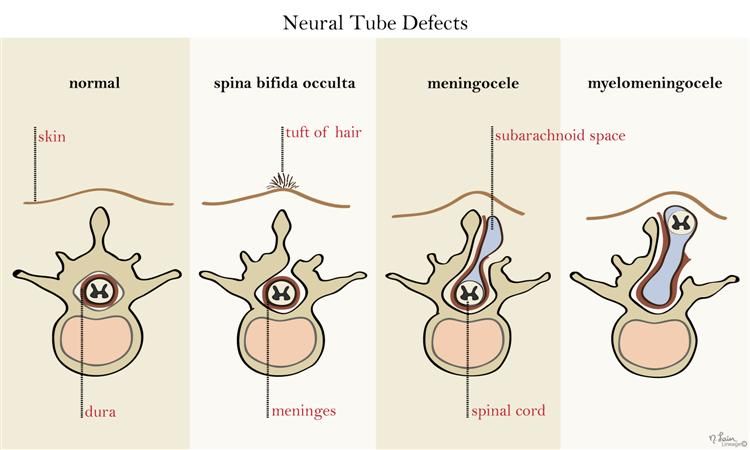 ), women with an uncomplicated history of NTD should receive 400 micrograms of folic acid per day in combination with vitamin B 12 at a dose of 2 mcg / day at least a month before conception and during the first trimester of pregnancy. In Italy, since 2005, the need for a daily intake of 400 micrograms of folic acid by women planning a pregnancy has been legally approved.
), women with an uncomplicated history of NTD should receive 400 micrograms of folic acid per day in combination with vitamin B 12 at a dose of 2 mcg / day at least a month before conception and during the first trimester of pregnancy. In Italy, since 2005, the need for a daily intake of 400 micrograms of folic acid by women planning a pregnancy has been legally approved.
In light of recent scientific evidence, it is important that, in addition to folic acid, drugs intended for the prevention of fetal NTD include vitamin B 12 .
Printed in abbreviated form.
Published in the magazine "Pharmateka" No. 1 (136), 2007
- Number:
- № 4/1 March - Pediatrics
10/17/2022 Pulmonology and otorhinolaryngologyVirucidal efficacy of ice groves due to a fixed combination of cetylpyridinium chloride and benzydamine hydrochloride against influenza virus A
In the midst of the SARS-CoV-2 corona virus infection, the search for effective methods to treat this infection has become relevant.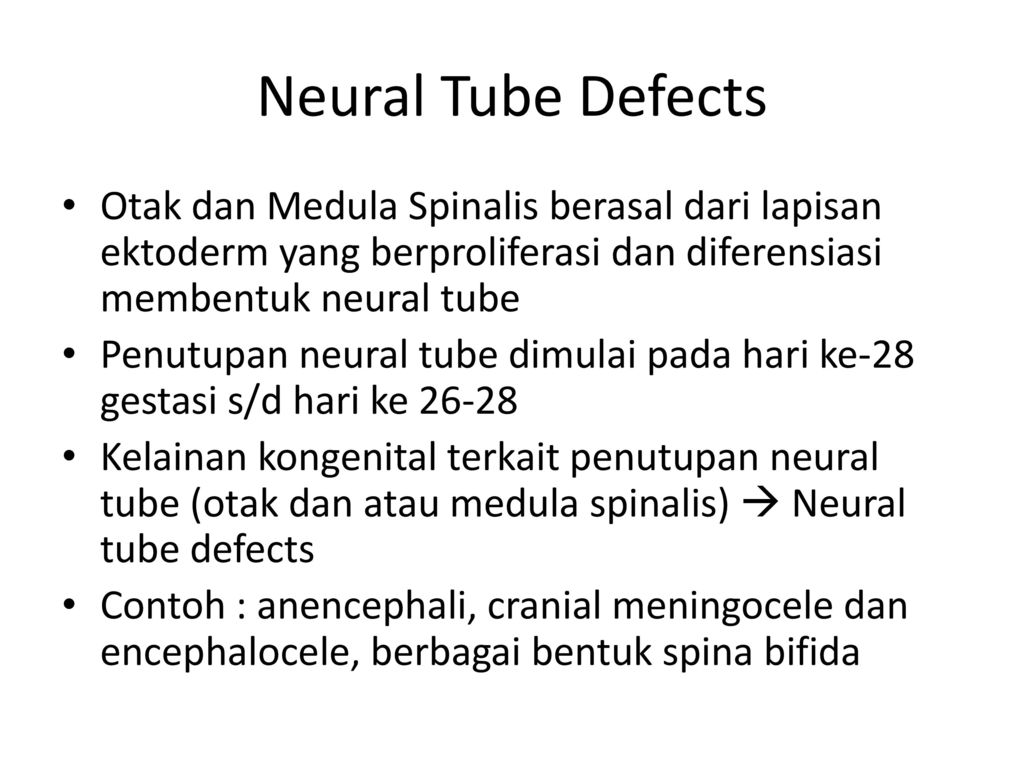 The drugs that, in addition to others, have turned their attention to themselves, have become oral antiseptics - the start of their health to a decrease in viral infection in the empty mouth and a decrease in the risk of transmission of infection. Before such antiseptics lie, zocrema, cetylpyridinium chloride (CPC), recent scientific data can demonstrate the most encouraging results looking at a wide range of antibacterial and antiviral drugs ...
The drugs that, in addition to others, have turned their attention to themselves, have become oral antiseptics - the start of their health to a decrease in viral infection in the empty mouth and a decrease in the risk of transmission of infection. Before such antiseptics lie, zocrema, cetylpyridinium chloride (CPC), recent scientific data can demonstrate the most encouraging results looking at a wide range of antibacterial and antiviral drugs ...
10/17/2022 PsychiatryPost-traumatic stress disorder in the minds of the military camp: space and possibility of phytotherapy Our viiSkovі struggle in the minds of trival, the sobbing of the sovereign Zhitta Sustyatyv, and our civilian is the country of the same novin, about the no -reasoning of the hen of the hen of the ties, we are wounding the worship of the waist.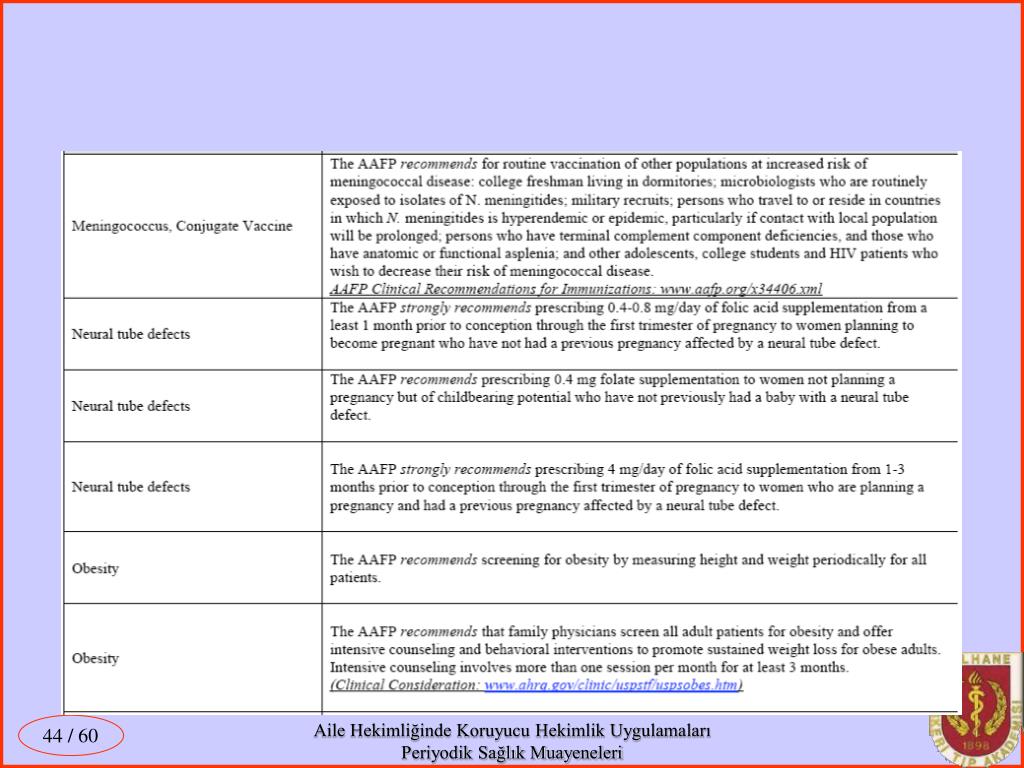 It negatively affects the psycho-emotional state of people, so now not only psychiatrists, but representatives of other medical specializations and non-medical doctors can get stuck with post-traumatic stress disorder (PTSD) ....
It negatively affects the psycho-emotional state of people, so now not only psychiatrists, but representatives of other medical specializations and non-medical doctors can get stuck with post-traumatic stress disorder (PTSD) ....
10/17/2022 PsychiatryGamalate-V6 in the wake of the anxious states
The anxious state is an emotional discord, mindful of anxiety for the restlessness in front of the future podia or in a situation of innocence. These physical changes are accompanied by organic symptoms (psychosomatic illnesses). On the other hand, organic illness can be troublesome, as if causing illness, pain, suffering of the patient, disrupted by the rhythm of that special social life, just work. Sedative drugs, especially benzodiazepines and sedatives, are most commonly seen in anxiety states.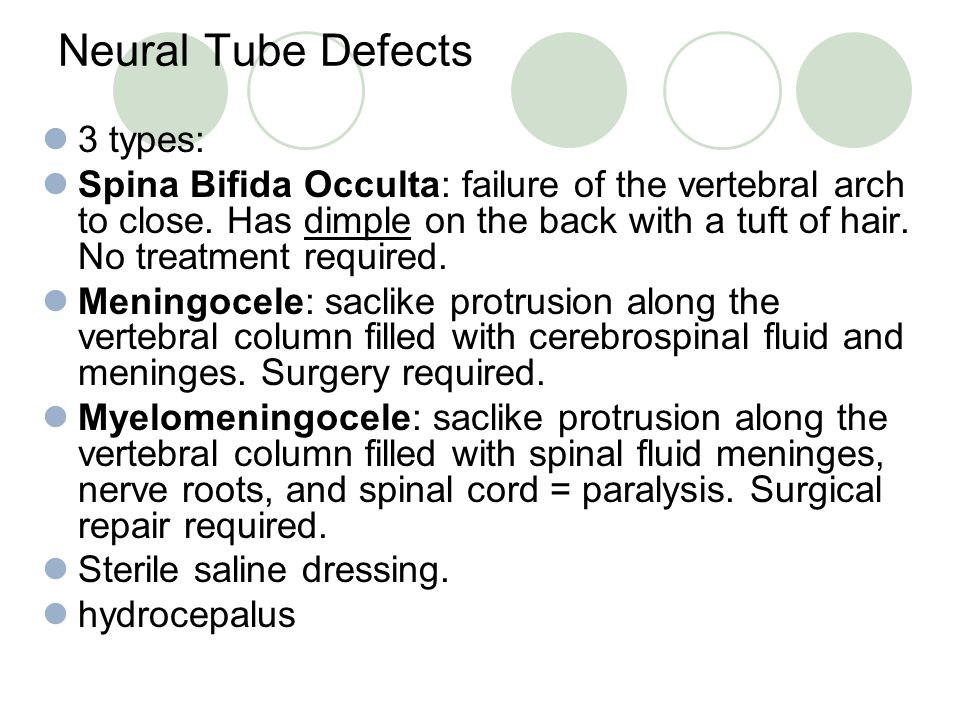 ...
...
10/17/2022 Diagnostics Algorithms for laboratory diagnostics of disorders in the hemostasis system
...
Malformations
Malformations- Popular Topics
- Air pollution
- Coronavirus disease (COVID-19)
- Hepatitis
- Data and statistics »
- News bulletin
- The facts are clear
- Publications
- Find the country »
- A
- B
- B
- G
- D
- E K 9008 I 9008 I 9008 I 9008 I0089
- Н
- О
- П
- Р
- С
- Т
- У
- Ф
- Х
- Ц
- Ч
- Ш
- Щ
- Ъ
- Ы
- Ь
- E
- Yu
- I
- WHO in countries »
- Reporting
- Regions »
- Africa
- America
- Southeast Asia
- Europe
- Eastern Mediterranean
- Western Pacific
- Media Center
- Press releases
- Statements
- Media messages
- Comments
- Reporting
- Online Q&A
- Developments
- Photo reports
- Questions and answers
- Latest information
- Emergencies "
- News "
- Disease Outbreak News
- WHO data »
- Dashboards »
- COVID-19 Monitoring Dashboard
- Basic moments "
- About WHO »
- CEO
- About WHO
- WHO activities
- Where does WHO work?
- Governing Bodies »
- World Health Assembly
- Executive committee
- Main page/
- Media Center /
- Newsletters/
- Read more/
- Malformations
\n
- \n
- development and strengthening of registration and surveillance systems; \n
- experience and capacity building; \n
- strengthening research and scientific work in the field of etiology, diagnosis and prevention; \n
- strengthening international cooperation.
 \n
\n
\n
Definition
\n
\nCongenital malformations are also referred to as congenital malformations, congenital disorders, or congenital deformities. Congenital malformations can be defined as structural or functional abnormalities (eg, metabolic disorders) that appear in utero and may be identified before birth, during birth, or later in life.
\n
Causes and risk factors
\n
\nApproximately 50% of all malformations cannot be attributed to any specific cause, but some causes or risk factors are known.
\n
Socio-economic factors
\n
\nAlthough low income may be an indirect determinant, malformations are more likely to occur in families and countries with insufficient resources. It is estimated that approximately 94% of severe malformations occur in middle- and low-income countries, where women often do not have access to sufficient and good enough food and may be exposed to some agent or factor, such as infection or alcohol, that provokes or enhances deviations from the norm in prenatal development. Moreover, motherhood in adulthood increases the risk of chromosomal abnormalities, including Down's syndrome, while motherhood at a young age increases the risk of certain congenital malformations.
Moreover, motherhood in adulthood increases the risk of chromosomal abnormalities, including Down's syndrome, while motherhood at a young age increases the risk of certain congenital malformations.
\n
Genetic factors
\n
\nIncest (consanguinity) increases the prevalence of rare genetic birth defects and almost doubles the risk of neonatal and infant mortality, mental retardation and severe birth defects in children born to first cousins . Some ethnic groups, such as Ashkenazi Jews and Finns, have a relatively high prevalence of rare genetic mutations that lead to an increased risk of malformations.\n
\n
Infections
\n
\nMaternal infections such as syphilis or measles are a common cause of birth defects in low- and middle-income countries.
\n
Maternal nutrition
\n
\nDeficiencies in iodine, folate, obesity, or conditions such as diabetes mellitus are associated with some malformations. For example, folic acid deficiency increases the risk of having a baby with a neural tube defect. In addition, increased intake of vitamin A may affect the normal development of the embryo or fetus.
For example, folic acid deficiency increases the risk of having a baby with a neural tube defect. In addition, increased intake of vitamin A may affect the normal development of the embryo or fetus.
\n
Environmental factors
\n
\nMaternal exposure to certain pesticides and other chemicals, as well as certain drugs, alcohol, tobacco, psychoactive substances, or radiation during pregnancy may increase the risk of developing the fetus or a newborn baby with birth defects. Working or living near or close to landfills, smelters, or mines can also be a risk factor, especially if the mother is exposed to other environmental risk factors or malnutrition.
\n
Prevention
\n
\nPregnancy and conception preventive health care, and prenatal care, reduce the incidence of some birth defects. Primary prevention of malformations includes the following measures:
\n
- \n
- Improving the nutrition of women during the reproductive period by ensuring adequate intake of vitamins and minerals, especially folic acid, as a result of daily oral supplementation or fortification of staple foods, such as wheat or corn flour.
 \n
\n - See to it that a pregnant woman does not consume or consume in a limited amount unhealthy foods, especially alcohol. \n
- Prevention of diabetes in pregnancy and during pregnancy through counseling, weight management, proper nutrition and, if necessary, insulin administration. \n
- Prevention of exposure to environmental hazardous substances (eg, heavy metals, pesticides, certain drugs) during pregnancy. \n
- Ensuring that any exposure of a pregnant woman to drugs or medical exposures (such as x-rays) is justified and based on a thorough analysis of the health risks and benefits. \n
- Increase vaccination coverage for women and children, especially against rubella virus. This disease can be prevented by vaccinating children. Rubella vaccine may also be given at least one month before pregnancy to women who did not receive the vaccine or who did not have rubella in childhood. \n
- Increase vaccination coverage for women and children, especially against rubella.
 This disease can be prevented by vaccinating children. Rubella vaccine may also be given to women who are not immune to the disease at least one month before pregnancy. \n
This disease can be prevented by vaccinating children. Rubella vaccine may also be given to women who are not immune to the disease at least one month before pregnancy. \n - Scaling up and strengthening training for health professionals and other staff involved in strengthening malformation prevention. \n
\n
Identification
\n
\nPre-conception (pre-conception) and near conception (per-conception) health care includes basic reproductive health care as well as medical genetic screening and counseling. Screening can be carried out during the three periods listed below.
\n
- \n
- Pre-pregnancy screening is designed to identify people who are at risk of developing certain health conditions or at risk of passing on any health conditions to their children. Screening includes family medical history and vector screening. Screening is especially important in countries where incestuous marriages are common.
 \n
\n - Preconception screening: maternal characteristics may increase risk, and screening results should be used to provide appropriate care based on risk. During this period, screening of young and mature mothers, as well as screening for the use of alcohol, tobacco and other psychoactive substances, can be carried out. Ultrasound can be used to detect Down's syndrome during the first trimester of pregnancy and severe fetal malformations during the second trimester. Additional tests and amniocentesis help detect neural tube defects and chromosomal abnormalities during the first and second trimesters of pregnancy. \n
- Newborn screening includes a clinical examination, as well as screening for hematological, metabolic, and hormonal disorders. Screening for deafness and heart disease, and early detection of birth defects, can facilitate life-saving treatment and prevent progression of the defect, which could lead to some form of physical, mental, or visual or hearing disability.
 In some countries, all newborns are screened for thyroid and adrenal abnormalities before being discharged from the maternity ward. \n
In some countries, all newborns are screened for thyroid and adrenal abnormalities before being discharged from the maternity ward. \n
\n
Treatment and care
\n
\nIn countries with adequate health services, structural congenital malformations can be corrected with pediatric surgery and provide timely treatment for children with functional problems such as thalassemia (inherited by recessive blood disease), sickle cell disorders, and congenital hypothyroidism.
\n
WHO activities
\n
\nIn 2010, the World Health Assembly published a report on birth defects. The report outlines the main components of establishing national programs for the prevention and care of birth defects before and after birth. The report also recommends priority actions for the international community to help establish and strengthen such national programs.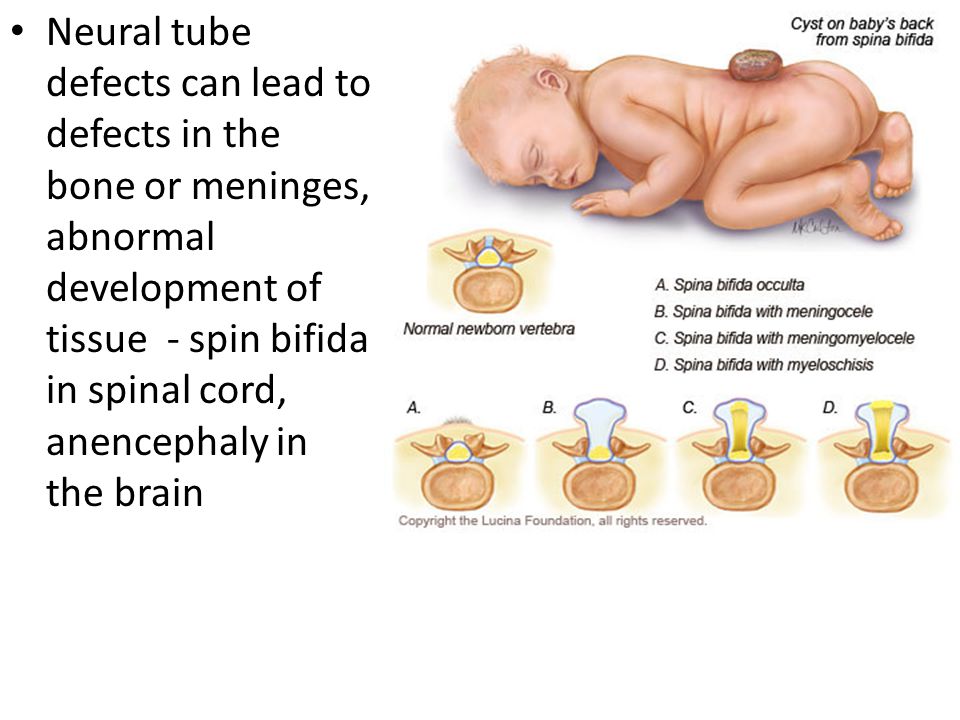
\n
\nThe Global Strategy for Women's and Children's Health, announced in September 2010 by the United Nations in collaboration with government leaders and other organizations such as WHO and UNICEF, plays a critical role in implementing efficient and cost-effective action to promote newborn and child health.\n
\n
\nWHO is also working with the National Center for Birth and Developmental Disorders, part of the US Centers for Disease Control and Prevention (CDC), and other partners to develop a global policy for salt fortification in foods folic acid at the country level. In addition, WHO is working with partners to provide the necessary technical expertise to conduct surveillance of neural tube defects, monitor efforts to fortify foods with folic acid salts, and strengthen laboratory capacity to assess risks for birth defects prevented by folic acid salts.
\n
\nThe International Clearing House for Surveillance and Research on Birth Defects is a voluntary, non-profit, international organization in official relations with WHO.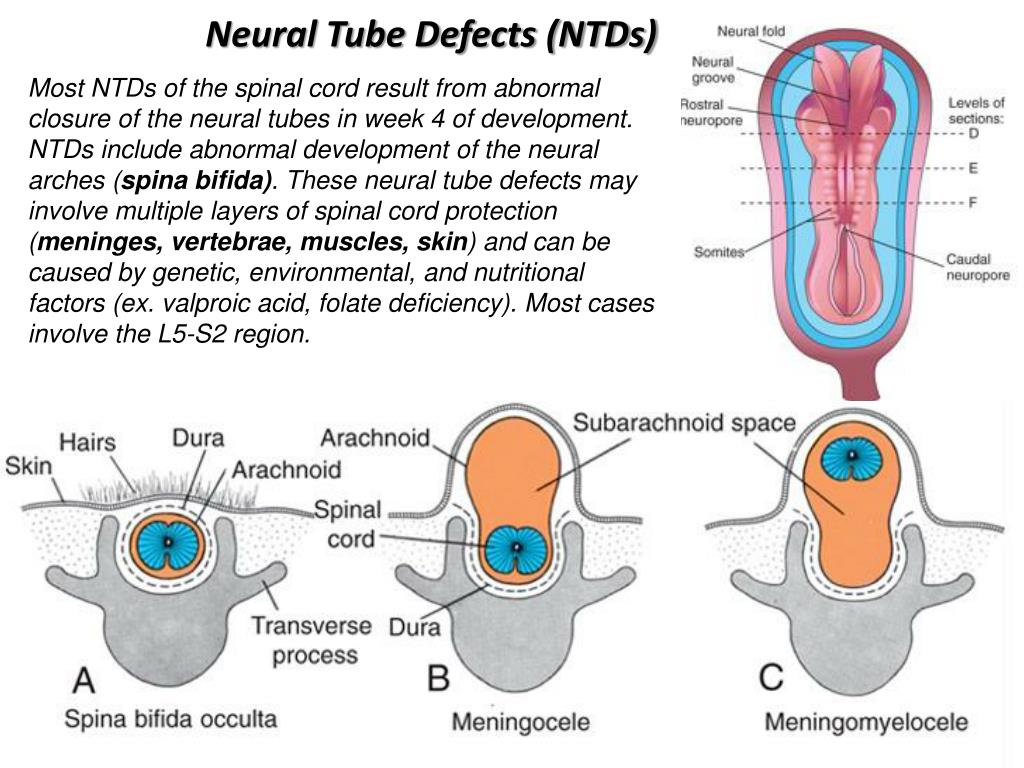 This organization collects surveillance data on birth defects and research programs around the world to study and prevent birth defects and mitigate their effects.
This organization collects surveillance data on birth defects and research programs around the world to study and prevent birth defects and mitigate their effects.
\n
\nThe WHO Departments of Reproductive Health and Research and Nutrition for Health and Development, in collaboration with the International Clearing House for Surveillance and Research on Birth Defects and the CDC National Center for Birth Defects and Development, organize annual seminars on surveillance and prevention of birth defects and preterm birth. The WHO Department of HIV/AIDS is collaborating with these partners to strengthen surveillance for malformations among women receiving antiretroviral drugs during pregnancy as an integral part of the monitoring and evaluation of national HIV programs.
\n
\nThe GAVI Alliance, partnered with WHO, is helping developing countries to increase the control and elimination of rubella and congenital rubella syndrome through immunization.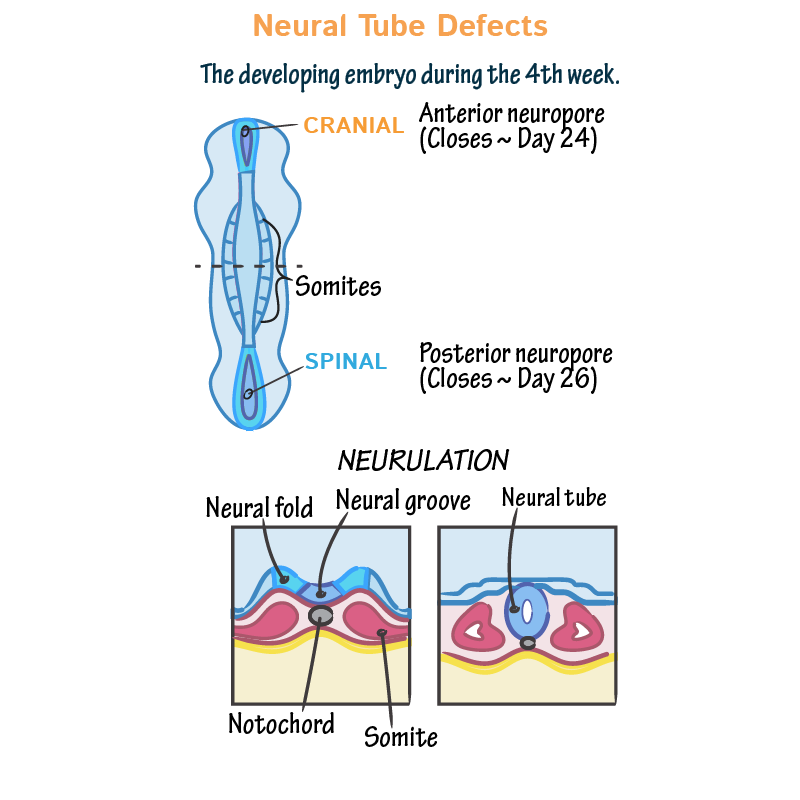
\n
\nWHO is developing normative tools, including guidelines and a global plan of action to strengthen health care and rehabilitation services in support of the implementation of the Convention on the Rights of Persons with Disabilities. Similarly, WHO is helping countries integrate health care and rehabilitation services into general primary health care, supporting the development of community-based rehabilitation programs and strengthening specialized rehabilitation centers and their links with community-based rehabilitation centers.
\n
United Nations Convention on the Rights of Persons with Disabilities
\n
\nThe WHO Department of Public Health and Environment works across a range of activities and develops interventions to address the environmental and social determinants of child development. These include: child-only vulnerability to indoor and outdoor air pollution, water pollution, lack of basic hygiene, toxic compounds, heavy metals, waste components and radiation exposure; mixed impact of factors related to the social environment, professional activities and nutrition, as well as the living conditions of children (home, school).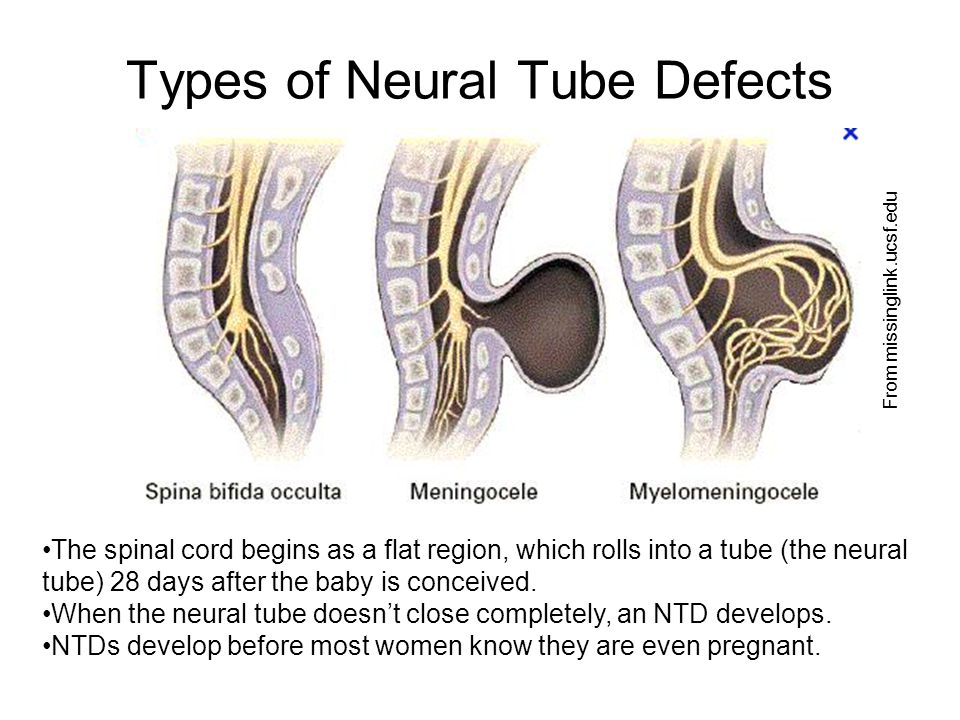
\n
","datePublished":"2022-02-28T22:52:00.0000000+00:00","image":"https://cdn.who.int/media/images/default -source/imported/preterm-birth-mother-jpg.jpg?sfvrsn=c5c1adf1_0","publisher":{"@type":"Organization","name":"World Health Organization: WHO","logo": {"@type":"ImageObject","url":"https://www.who.int/Images/SchemaOrg/schemaOrgLogo.jpg","width":250,"height":60}},"dateModified ":"2022-02-28T22:52:00.0000000+00:00","mainEntityOfPage":"https://www.who.int/ru/news-room/fact-sheets/detail/congenital-anomalies", "@context":"http://schema.org","@type":"Article"};
Key Facts
- It is estimated that 303,000 children die each year from malformations during the first 4 weeks of life.
- Developmental disabilities can lead to long-term disability, which has a significant impact on individuals, their families, health systems and society.
- The most severe malformations include heart defects, neural tube defects and Down's syndrome.
- Although malformations may be genetic, infectious or environmental in origin, the exact cause is often difficult to establish.
- Some birth defects can be prevented. The main elements of prevention are, inter alia, vaccination, adequate intake of folic acid or iodine through fortification of staple foods or provision of nutritional supplements, and proper prenatal care.
Malformations and preterm birth are major causes of childhood death, chronic disease and disability in many countries. In 2010, the World Health Assembly adopted a resolution calling on all Member States to promote primary prevention and health promotion for children with developmental disabilities through:
- development and strengthening of registration and surveillance systems;
- experience and capacity building;
- strengthening research and scientific work in the field of etiology, diagnosis and prevention;
- strengthening international cooperation.
Definition
Congenital malformations are also referred to as congenital malformations, congenital disorders or congenital deformities. Congenital malformations can be defined as structural or functional abnormalities (eg, metabolic disorders) that appear in utero and may be identified before birth, during birth, or later in life.
Causes and risk factors
Approximately 50% of all malformations cannot be attributed to any specific cause, but some causes or risk factors are known.
Socio-economic factors
While low income may be an indirect determinant, malformations are more likely to occur in under-resourced families and countries. It is estimated that approximately 94% of severe malformations occur in middle- and low-income countries, where women often do not have access to sufficient and good enough food and may be exposed to some agent or factor, such as infection or alcohol, that provokes or enhances deviations from the norm in prenatal development.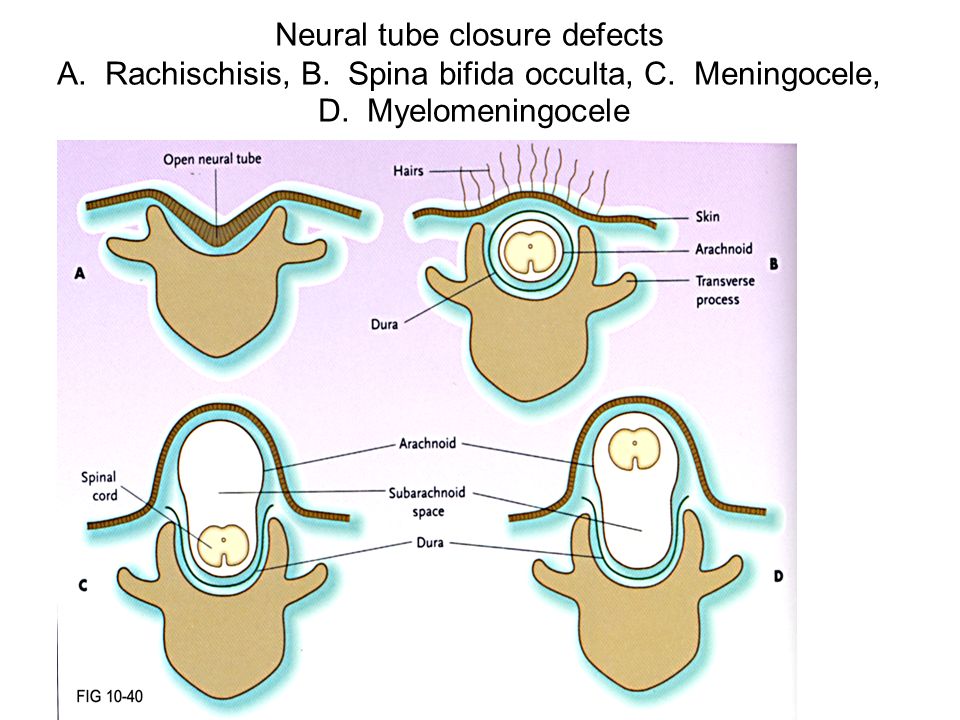 Moreover, motherhood in adulthood increases the risk of chromosomal abnormalities, including Down's syndrome, while motherhood at a young age increases the risk of certain congenital malformations.
Moreover, motherhood in adulthood increases the risk of chromosomal abnormalities, including Down's syndrome, while motherhood at a young age increases the risk of certain congenital malformations.
Genetic factors
Incest (consanguinity) increases the prevalence of rare genetic birth defects and almost doubles the risk of neonatal and infant mortality, mental retardation and severe birth defects in children born to first cousins. Some ethnic groups, such as Ashkenazi Jews and Finns, have a relatively high prevalence of rare genetic mutations that lead to an increased risk of malformations.
Infections
Maternal infections such as syphilis or measles are a common cause of birth defects in low- and middle-income countries.
Maternal nutrition
Deficiency of iodine, folic acid salts, obesity, or conditions such as diabetes mellitus are associated with some malformations. For example, folic acid deficiency increases the risk of having a baby with a neural tube defect.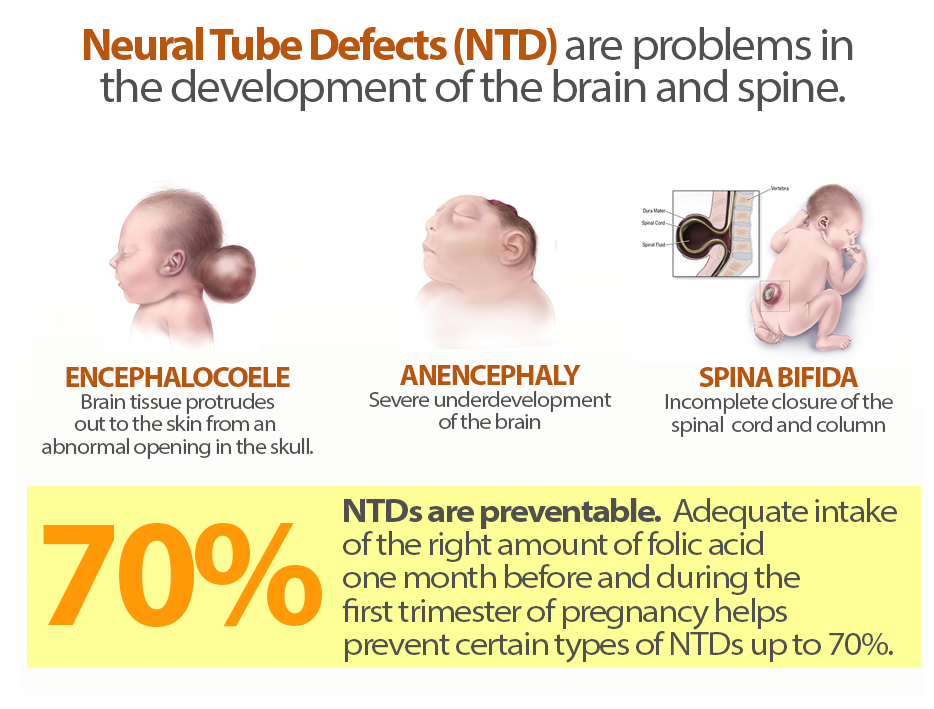 In addition, increased intake of vitamin A may affect the normal development of the embryo or fetus.
In addition, increased intake of vitamin A may affect the normal development of the embryo or fetus.
Environmental factors
Maternal exposure to certain pesticides and other chemicals, as well as certain drugs, alcohol, tobacco, psychoactive substances, or radiation during pregnancy may increase the risk of birth defects in the fetus or newborn. Working or living near or close to landfills, smelters, or mines can also be a risk factor, especially if the mother is exposed to other environmental risk factors or malnutrition.
Prevention
Preventive health care during pregnancy and conception, as well as antenatal care, reduce the incidence of some birth defects. Primary prevention of malformations includes the following:
- Improving the nutrition of women during the reproductive period by ensuring adequate intake of vitamins and minerals, especially folic acid, through daily oral supplementation or fortification of staple foods such as wheat or corn flour .
- Supervise that a pregnant woman does not consume or consume in a limited amount unhealthy foods, especially alcohol.
- Prevention of diabetes in pregnancy and during pregnancy through counseling, weight management, proper nutrition and, if necessary, insulin administration.
- Prevention during pregnancy of exposure to environmental hazardous substances (eg, heavy metals, pesticides, certain drugs).
- Ensuring that any exposure of a pregnant woman to drugs or radiation for medical purposes (such as x-rays) is justified and based on a careful analysis of the health risks and benefits.
- Increase vaccination coverage for women and children, especially against rubella virus. This disease can be prevented by vaccinating children. Rubella vaccine may also be given at least one month before pregnancy to women who did not receive the vaccine or who did not have rubella in childhood.
- Increase vaccination coverage for women and children, especially against rubella virus.
 This disease can be prevented by vaccinating children. Rubella vaccine may also be given to women who are not immune to the disease at least one month before pregnancy.
This disease can be prevented by vaccinating children. Rubella vaccine may also be given to women who are not immune to the disease at least one month before pregnancy. - Scaling up and strengthening training for health professionals and other staff involved in strengthening malformation prevention.
Detection
Medical care before conception (in the preconception period) and around the time of conception (in the periconceptional period) includes basic reproductive health care, as well as medical genetic screening and counseling. Screening can be carried out during the three periods listed below.
- Pre-pregnancy screening is designed to identify people who are at risk of developing certain health conditions or passing on any health conditions to their children. Screening includes family medical history and vector screening. Screening is especially important in countries where incestuous marriages are common.
- Preconception screening: maternal characteristics may increase risk and screening results should be used to provide appropriate care based on risk.
 During this period, screening of young and mature mothers, as well as screening for the use of alcohol, tobacco and other psychoactive substances, can be carried out. Ultrasound can be used to detect Down's syndrome during the first trimester of pregnancy and severe fetal malformations during the second trimester. Additional tests and amniocentesis help detect neural tube defects and chromosomal abnormalities during the first and second trimesters of pregnancy.
During this period, screening of young and mature mothers, as well as screening for the use of alcohol, tobacco and other psychoactive substances, can be carried out. Ultrasound can be used to detect Down's syndrome during the first trimester of pregnancy and severe fetal malformations during the second trimester. Additional tests and amniocentesis help detect neural tube defects and chromosomal abnormalities during the first and second trimesters of pregnancy. - Newborn screening includes clinical examination as well as screening for hematological, metabolic, and hormonal disorders. Screening for deafness and heart disease, and early detection of birth defects, can facilitate life-saving treatment and prevent progression of the defect, which could lead to some form of physical, mental, or visual or hearing disability. In some countries, all newborns are screened for thyroid and adrenal abnormalities before being discharged from the maternity ward.
Treatment and medical care
In countries with adequate health services, structural birth defects can be corrected with pediatric surgery and timely treatment can be provided for children with functional problems such as thalassemia (a recessive blood disorder), sickle cell disorders, and congenital hypothyroidism.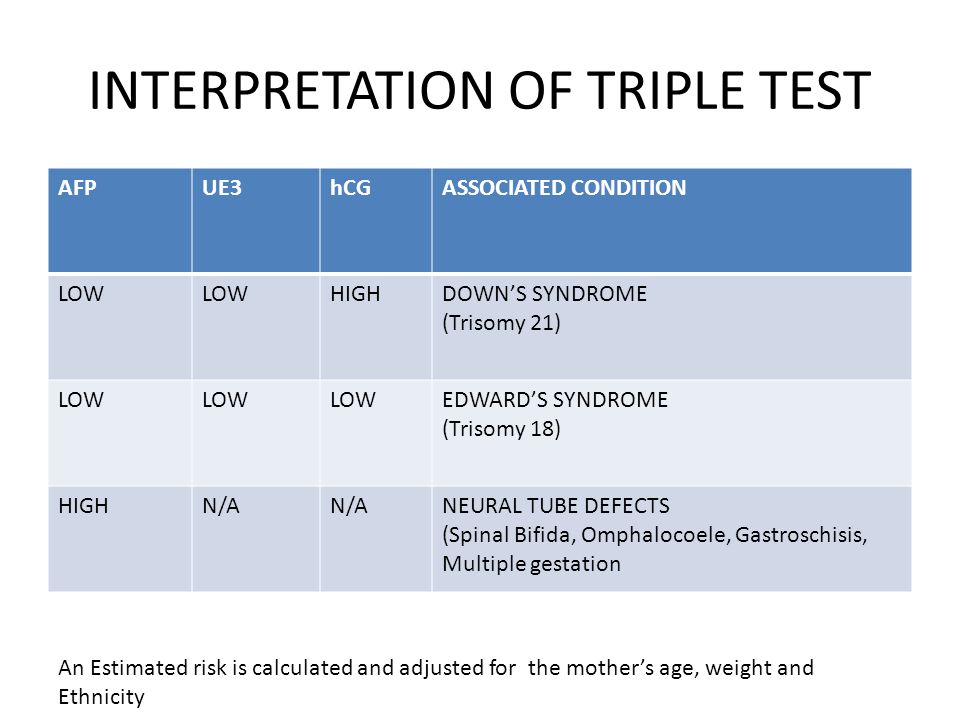
WHO activities
In 2010, the World Health Assembly published a report on birth defects. The report outlines the main components of establishing national programs for the prevention and care of birth defects before and after birth. The report also recommends priority actions for the international community to help establish and strengthen such national programs.
The Global Strategy for Women's and Children's Health, launched in September 2010 by the United Nations in collaboration with government leaders and other organizations such as WHO and UNICEF, plays a critical role in achieving effective and cost-effective action to improve newborn health and children.
WHO is also working with the National Center for Birth and Developmental Disorders, part of the US Centers for Disease Control and Prevention (CDC), and other partners to develop a global policy for folic acid fortification at the country level. In addition, WHO is working with partners to provide the necessary technical expertise to conduct surveillance of neural tube defects, monitor efforts to fortify foods with folic acid salts, and strengthen laboratory capacity to assess risks for birth defects prevented by folic acid salts.
The International Clearing House for Surveillance and Research on Birth Defects is a voluntary, non-profit international organization in official relations with WHO. This organization collects surveillance data on birth defects and research programs around the world to study and prevent birth defects and mitigate their effects.
The WHO Departments of Reproductive Health and Research and Nutrition for Health and Development, in collaboration with the International Clearing House for Surveillance and Research on Birth Defects and the CDC National Center for Birth Defects and Development, organize annual workshops on surveillance and prevention of birth defects and premature birth. The WHO Department of HIV/AIDS is collaborating with these partners to strengthen surveillance for malformations among women receiving antiretroviral drugs during pregnancy as an integral part of the monitoring and evaluation of national HIV programs.
The GAVI Alliance, with WHO among its partners, is helping developing countries to accelerate the control and elimination of rubella and congenital rubella syndrome through immunization.
WHO is developing normative tools, including guidelines and a global action plan to strengthen health care and rehabilitation services in support of the implementation of the Convention on the Rights of Persons with Disabilities. Similarly, WHO is helping countries integrate health care and rehabilitation services into general primary health care, supporting the development of community-based rehabilitation programs and strengthening specialized rehabilitation centers and their links with community-based rehabilitation centers.
UN Convention on the Rights of Persons with Disabilities
The WHO Department of Public Health and Environment works across a range of activities and develops interventions to address the environmental and social determinants of child development. These include: child-only vulnerability to indoor and outdoor air pollution, water pollution, lack of basic hygiene, toxic compounds, heavy metals, waste components and radiation exposure; mixed impact of factors related to the social environment, professional activities and nutrition, as well as the living conditions of children (home, school).