How to check for meningitis in a child
Meningitis - Symptoms - NHS
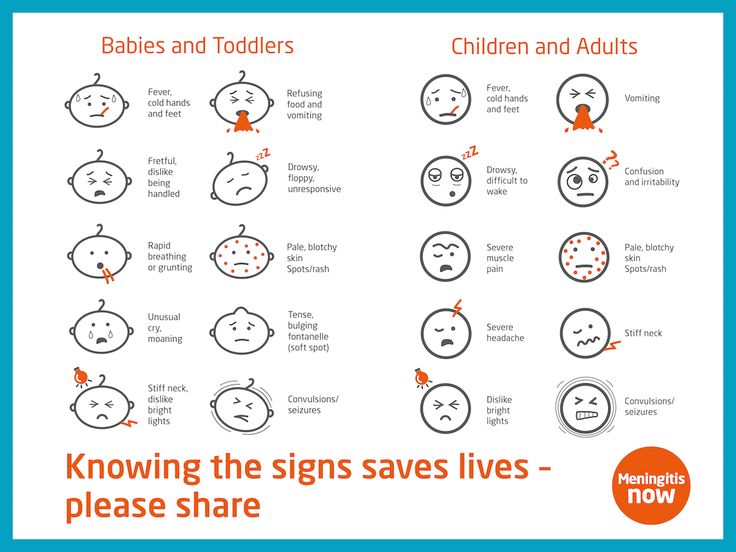
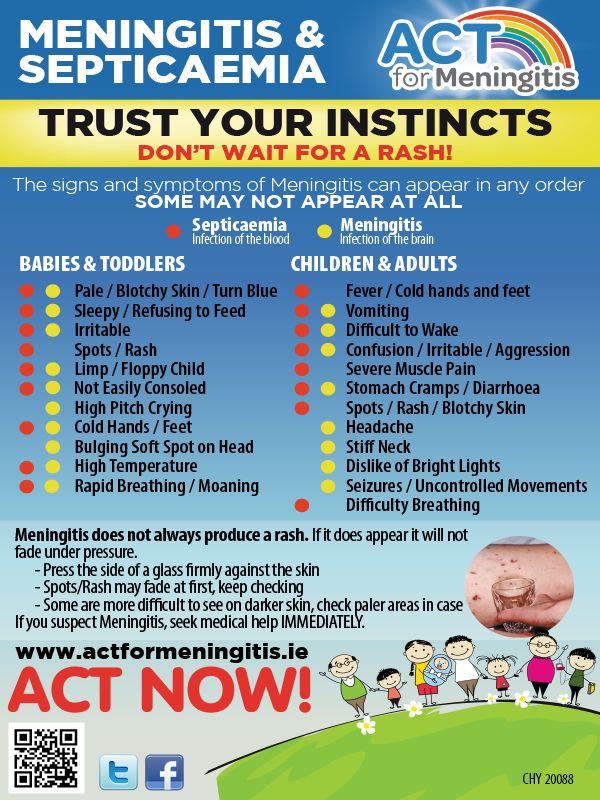
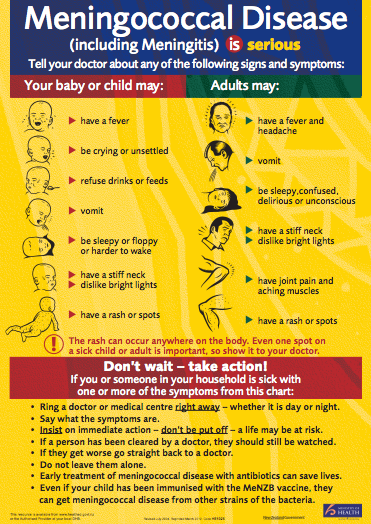
Symptoms of meningitis can appear in any order. Some may not appear at all. In the early stages, there may not be a rash, or the rash may fade when pressure is applied.
You should get medical help immediately if you're concerned about yourself or your child.
Trust your instincts and do not wait for all the symptoms to appear or until a rash develops.
Symptoms of meningitis and sepsis include:
- a high temperature
- cold hands and feet
- vomiting
- confusion
- breathing quickly
- muscle and joint pain
- pale, mottled or blotchy skin (this may be harder to see on brown or black skin)
- spots or a rash (this may be harder to see on brown or black skin)
- headache
- a stiff neck
- a dislike of bright lights
- being very sleepy or difficult to wake
- fits (seizures)
Babies may also:
- refuse feeds
- be irritable
- have a high-pitched cry
- have a stiff body or be floppy or unresponsive
- have a bulging soft spot on the top of their head
Someone with meningitis or sepsis can get a lot worse very quickly.
Call 999 for an ambulance or go to your nearest A&E immediately if you think you or someone you look after could have meningitis or sepsis.
Call NHS 111 for advice if you're not sure if it's anything serious.
If you’ve had medical advice and are still worried or any symptoms get worse, get medical help again.
The rash usually starts as small, red pinpricks before spreading quickly and turning into red or purple blotches.Credit:
Mediscan / Alamy Stock Photo https://www.alamy.com/meningococcal-rash-image1683649.html?pv=1&stamp=2&imageid=83D4AFC7-AC4B-4271-B09C-727E90532943&p=17774&n=0&orientation=0&pn=1&searchtype=0&IsFromSearch=1&srch=foo%3dbar%26st%3d0%26pn%3d1%26ps%3d100%26sortby%3d2%26resultview%3dsortbyPopular%26npgs%3d0%26qt%3dATB0C2%26qt_raw%3dATB0C2%26lic%3d3%26mr%3d0%26pr%3d0%26ot%3d0%26creative%3d%26ag%3d0%26hc%3d0%26pc%3d%26blackwhite%3d%26cutout%3d%26tbar%3d1%26et%3d0x000000000000000000000%26vp%3d0%26loc%3d0%26imgt%3d0%26dtfr%3d%26dtto%3d%26size%3d0xFF%26archive%3d1%26groupid%3d%26pseudoid%3d788068%26a%3d%26cdid%3d%26cdsrt%3d%26name%3d%26qn%3d%26apalib%3d%26apalic%3d%26lightbox%3d%26gname%3d%26gtype%3d%26xstx%3d0%26simid%3d%26saveQry%3d%26editorial%3d1%26nu%3d%26t%3d%26edoptin%3d%26customgeoip%3d%26cap%3d1%26cbstore%3d1%26vd%3d0%26lb%3d%26fi%3d2%26edrf%3d0%26ispremium%3d1%26flip%3d0%26pl%3d
It does not fade if you press the side of a clear glass firmly against the skin.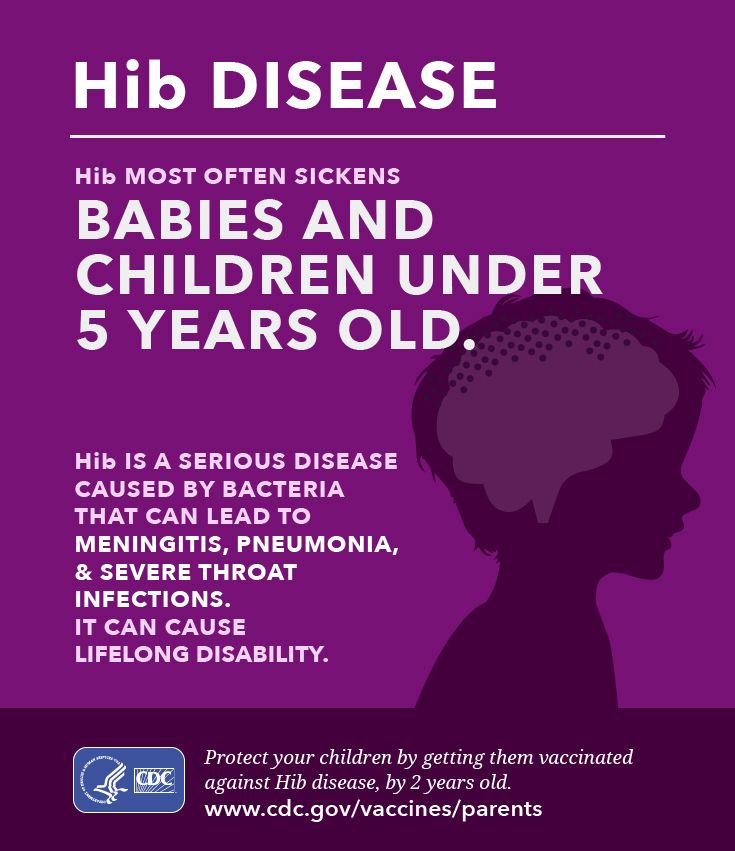
Credit:
Alamy Stock Photo https://www.alamy.com/testing-of-meningococcal-rash-image589611.html?pv=1&stamp=2&imageid=6C8D2A33-C874-43AF-A58B-398C0D9552AF&p=17774&n=0&orientation=0&pn=1&searchtype=0&IsFromSearch=1&srch=foo%3dbar%26st%3d0%26pn%3d1%26ps%3d100%26sortby%3d2%26resultview%3dsortbyPopular%26npgs%3d0%26qt%3dA8FF2B%26qt_raw%3dA8FF2B%26lic%3d3%26mr%3d0%26pr%3d0%26ot%3d0%26creative%3d%26ag%3d0%26hc%3d0%26pc%3d%26blackwhite%3d%26cutout%3d%26tbar%3d1%26et%3d0x000000000000000000000%26vp%3d0%26loc%3d0%26imgt%3d0%26dtfr%3d%26dtto%3d%26size%3d0xFF%26archive%3d1%26groupid%3d%26pseudoid%3d195878%26a%3d%26cdid%3d%26cdsrt%3d%26name%3d%26qn%3d%26apalib%3d%26apalic%3d%26lightbox%3d%26gname%3d%26gtype%3d%26xstx%3d0%26simid%3d%26saveQry%3d%26editorial%3d1%26nu%3d%26t%3d%26edoptin%3d%26customgeoip%3d%26cap%3d1%26cbstore%3d1%26vd%3d0%26lb%3d%26fi%3d2%26edrf%3d0%26ispremium%3d1%26flip%3d0%26pl%3d
The rash can be harder to see on brown or black skin.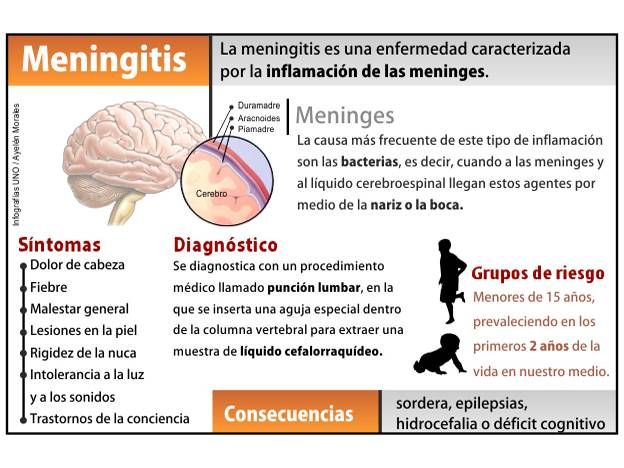 Check paler areas, such as the palms of the hands, soles of the feet, roof of the mouth, tummy, whites of the eyes or the inside of the eyelids.
Check paler areas, such as the palms of the hands, soles of the feet, roof of the mouth, tummy, whites of the eyes or the inside of the eyelids. Credit:
Meningitis Research UK https://hscic365.sharepoint.com/sites/Pilot/NHSUK/Health%20AZ/Forms/AllItems.aspx?id=%2Fsites%2FPilot%2FNHSUK%2FHealth%20AZ%2FHealth%20A%2DZ%2FA%2DZ%20content%20audit%2FM%2FMeningitis%2FImage%20and%20section%20review%2007%202019%2FRe%5FPhotography%20of%20the%20meningitis%20rash%2Eeml&parent=%2Fsites%2FPilot%2FNHSUK%2FHealth%20AZ%2FHealth%20A%2DZ%2FA%2DZ%20content%20audit%2FM%2FMeningitis%2FImage%20and%20section%20review%2007%202019
If a rash does not fade under a glass, it can be a sign of sepsis (sometimes called septicaemia or blood poisoning) caused by meningitis and you should call 999 straight away.
Page last reviewed: 25 October 2022
Next review due: 25 October 2025
Meningitis in Children | Cedars-Sinai
ABOUT CAUSES DIAGNOSIS TREATMENT NEXT STEPS
What is meningitis in children?
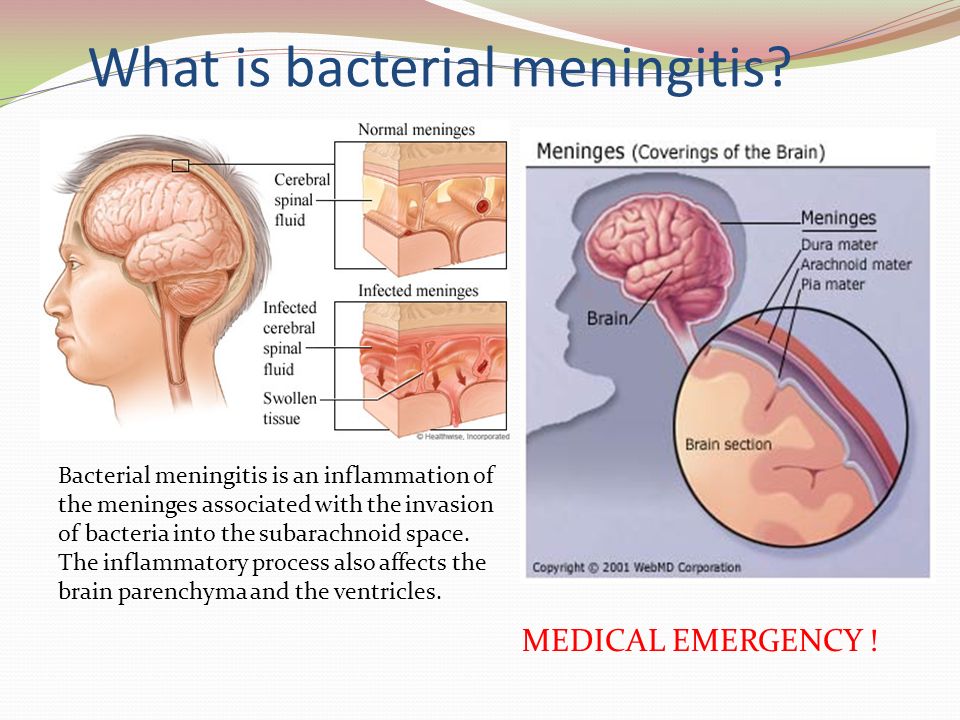
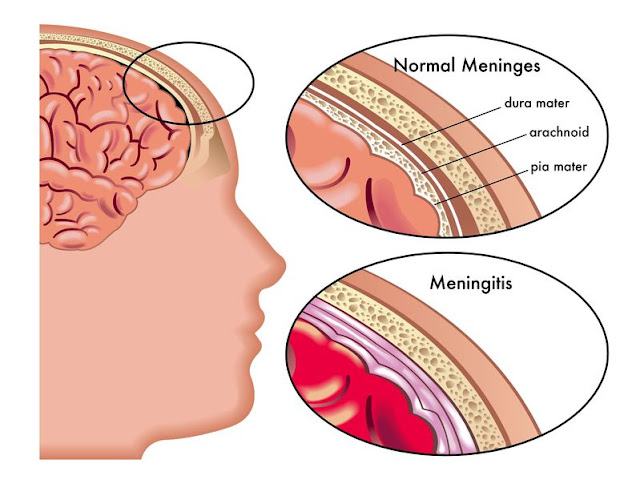
Meningitis is a swelling (inflammation) of the thin membranes that cover the brain and the spinal cord.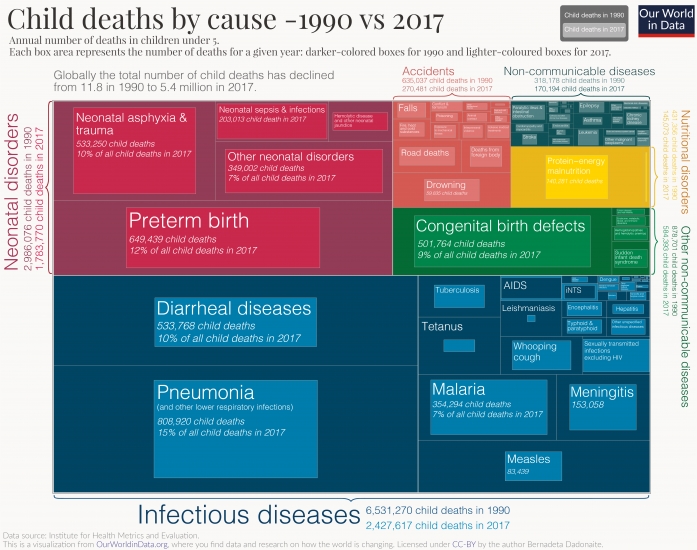 These membranes are called the meninges.
These membranes are called the meninges.
What causes meningitis in a child?
Meningitis is most often caused by a bacterial or viral infection that moves into the cerebral spinal fluid (CSF). CSF is the fluid that protects and cushions the brain and spinal cord. A fungus or parasite may also cause meningitis. This is more common only in children with a weak immune system.
Meningitis caused by a virus is more common and usually less severe. Bacterial meningitis is usually more severe and may lead to long-term complications or death.
Viruses that can cause meningitis include polioviruses, the mumps virus (paramyxovirus), the flu virus, and West Nile virus.
Bacteria that can cause meningitis include group B streptococcus, E. coli, Haemophilus influenzae type b (Hib), and a strep bacteria that causes pneumonia. Syphilis, tuberculosis, and Lyme disease bacteria can also cause meningitis. The bacteria, viruses, and fungi that cause meningitis usually grow in a person’s respiratory tract. A child may have no symptoms at all, but may carry the organism in his or her nose and throat. They may be spread by:
A child may have no symptoms at all, but may carry the organism in his or her nose and throat. They may be spread by:
- Close contact with someone carrying the infection
- Touching infected objects, such as doorknobs, hard surfaces, or toys, and then touching nose, mouth, or eyes
- Droplets from a sneeze, close conversation, or kissing
An infection usually starts in the respiratory tract. In a child, it may first cause a cold, sinus infection, or ear infection. It can then go into the bloodstream and reach the brain and spinal cord.
Which children are at risk for meningitis?
A child is more at risk for meningitis if he or she has an infection caused by a number of viruses, bacteria, or fungi. Children with a weakened immune system are at great risk.
What are the symptoms of meningitis in a child?
The symptoms of meningitis vary depending on what causes the infection. The symptoms may start several days after your child has had a cold and runny nose, or diarrhea and vomiting. Symptoms can occur a bit differently in each child. Symptoms may appear suddenly. Or they may develop over several days.
Symptoms can occur a bit differently in each child. Symptoms may appear suddenly. Or they may develop over several days.
In babies, symptoms may include:
- Irritability
- Fever
- Sleeping more than usual
- Poor feeding
- Crying that can’t be soothed
- High-pitched cry
- Arching back
- Bulging soft spots on the head (fontanelles)
- Changed temperament
- Purple-red splotchy rash
- Seizures
- Vomiting
In children age 1 or older, symptoms may include:
- Neck pain
- Back pain
- Headache
- Sleepiness
- Confusion
- Irritability
- Fever
- Refusing to eat
- Reduced level of consciousness
- Seizures
- Eyes sensitive to light (photophobia)
- Nausea and vomiting
- Neck stiffness
- A purple-red splotchy rash
The symptoms of meningitis can be like other health conditions. Make sure your child sees his or her healthcare provider for a diagnosis.
Make sure your child sees his or her healthcare provider for a diagnosis.
How is meningitis diagnosed in a child?
The healthcare provider will ask about your child’s symptoms and health history. He or she may also ask about your family’s health history. He or she will give your child a physical exam. Your child may also have tests, such as:
- Lumbar puncture (spinal tap). This is the only test that diagnoses meningitis. A needle is placed into the lower back, into the spinal canal. This is the area around the spinal cord. The pressure in the spinal canal and brain is measured. A small amount of cerebral spinal fluid (CSF) is removed and sent for testing to see if there is an infection or other problems.
- Blood tests. These can help diagnose infections that cause meningitis.
- CT scan or MRI. These are tests that show images of the brain.
 A CT scan is sometimes done to look for other conditions that may cause similar symptoms as meningitis. An MRI may show inflammatory changes in the meninges. These tests give more information. But meningitis can’t be diagnosed using these tests alone.
A CT scan is sometimes done to look for other conditions that may cause similar symptoms as meningitis. An MRI may show inflammatory changes in the meninges. These tests give more information. But meningitis can’t be diagnosed using these tests alone. - Nasal, throat, or rectal swabs. These tests help diagnose viral infections that cause meningitis.
How is meningitis treated in a child?
Treatment will depend on your child’s symptoms, age, and general health. It will also depend on how severe the condition is.
Treatment varies by type of meningitis. The treatments by type include:
- Bacterial meningitis. Treatment is started as quickly as possible. The healthcare provider will give your child IV (intravenous) antibiotics, which kill bacteria. Your child will also get a corticosteroid medicine. The steroid works by decreasing the swelling (inflammation) and reducing pressure that can build up in the brain.
 Steroids also reduce the risk for hearing loss and brain damage.
Steroids also reduce the risk for hearing loss and brain damage. - Viral meningitis. Most children get better on their own without treatment. In some cases, treatment may be done to help ease symptoms. There are no medicines to treat the viruses that cause viral meningitis. The only exception is herpes simplex virus, which is treated with IV antiviral medicine. Babies and children with a weakened immune system may need to stay in the hospital.
- Fungal meningitis. Your child may get IV antifungal medicine.
- Tuberculous (TB) meningitis. Your child will be treated with a course of medicines over 1 year. Treatment is done with several medicines for the first few months. This is followed by other medicines for the remaining time.
While your child is recovering from meningitis, he or she may also need:
- Bed rest
- Increased fluid intake by mouth or IV fluids in the hospital
- Medicines to reduce fever and headache.
 Don’t give aspirin or medicine that contains aspirin to a child younger than age 19 unless directed by your child’s provider. Taking aspirin can put your child at risk for Reye syndrome. This is a rare but very serious disorder. It most often affects the brain and the liver.
Don’t give aspirin or medicine that contains aspirin to a child younger than age 19 unless directed by your child’s provider. Taking aspirin can put your child at risk for Reye syndrome. This is a rare but very serious disorder. It most often affects the brain and the liver. - Supplemental oxygen or breathing machine (respirator) if your child has trouble breathing
Talk with your child’s healthcare providers about the risks, benefits, and possible side effects of all treatments.
What are the possible complications of meningitis in a child?
Bacterial meningitis is usually more severe and may lead to long-term complications. Some children may have long-term problems with seizures, brain damage, hearing loss, and disability. Bacterial meningitis can also cause death.
How can I help prevent meningitis in my child?
Several vaccines are available to prevent some of the bacterial infections that can cause meningitis. These include:
- H.
 influenzae type b vaccine (Hib). This is given as a 3- or 4-part series during your child's routine vaccines starting at 2 months old.
influenzae type b vaccine (Hib). This is given as a 3- or 4-part series during your child's routine vaccines starting at 2 months old. - PCV13 pneumococcal vaccine. The American Academy of Pediatrics recommends this vaccine for all healthy children younger than age 2. PCV13 can be given along with other childhood vaccines. It is recommended at ages 2 months, 4 months, 6 months, and 12 to 15 months. One dose is also advised for older children who did not get the 4-dose series, and for those at high risk for pneumococcal disease.
- PPSV23 pneumococcal vaccine. This vaccine is also recommended for older children at high risk for pneumococcal disease.
- Meningococcal vaccine. This vaccine is part of the routine vaccine schedule. It is given to children ages 11 to 12, with a booster given at age 16.
 It is given to teens entering high school if they were not vaccinated at age 11 or 12. A booster is also given at age 16 to 18, or up to 5 years later. Babies and young children at increased risk may also have this vaccine. Ask your child's healthcare provider about the number of doses and when they should be given.
It is given to teens entering high school if they were not vaccinated at age 11 or 12. A booster is also given at age 16 to 18, or up to 5 years later. Babies and young children at increased risk may also have this vaccine. Ask your child's healthcare provider about the number of doses and when they should be given.
Vaccines that protect against viruses such as measles, mumps, chickenpox, and the flu can prevent viral meningitis.
Talk with your child’s healthcare provider if you have questions about the vaccines.
You and your child can do other things to prevent the spread of infections. Proper handwashing and staying away from people who are sick can help prevent meningitis.
When should I call my child’s healthcare provider?
Call the healthcare provider if your child has:
- Not received vaccines
- Contact with someone who has meningitis
- Symptoms that don’t get better, or get worse
- New symptoms
Key points about meningitis in children
- Meningitis is an inflammation of the thin membranes that cover the brain and the spinal cord.

- It is most often caused by a bacterial or viral infection that moves into the cerebral spinal fluid. A fungus or parasite may also cause meningitis.
- Meningitis caused by a virus is more common and usually less severe. Bacterial meningitis is usually more severe and may lead to long-term complications or death.
- An infection usually starts in the respiratory tract. In a child, it may first cause a cold, sinus infection, or ear infection. It can then go into the bloodstream and reach the brain and spinal cord.
- A lumbar puncture (spinal tap) is the only test that diagnoses meningitis. A needle is placed into the lower back, into the spinal canal.
- Several vaccines are available to prevent some of the bacterial and viral infections that can cause meningitis.
Next steps
Tips to help you get the most from a visit to your child’s healthcare provider:
- Know the reason for the visit and what you want to happen.
- Before your visit, write down questions you want answered.
- At the visit, write down the name of a new diagnosis, and any new medicines, treatments, or tests. Also write down any new instructions your provider gives you for your child.
- Know why a new medicine or treatment is prescribed and how it will help your child. Also know what the side effects are.
- Ask if your child’s condition can be treated in other ways.
- Know why a test or procedure is recommended and what the results could mean.
- Know what to expect if your child does not take the medicine or have the test or procedure.
- If your child has a follow-up appointment, write down the date, time, and purpose for that visit.
- Know how you can contact your child’s provider after office hours. This is important if your child becomes ill and you have questions or need advice.

How to recognize meningitis and diagnose the disease in the Optimum medical laboratory in Sochi (Adler)
- Home
- How to recognize the disease
- Diseases of the nervous system
- Meningitis
More about the doctor
Symptoms, diagnosis and prevention of meningitis
Meningitis is an inflammation of the membranes of the brain or spinal cord, which can be triggered by infections of viral and bacterial etiology. Pathology is accompanied by a severe headache, a typical body position in bed, hemorrhagic rashes on the skin and stiffness of the muscles of the occipital zone. Children and adolescents, as well as elderly people with weakened immune systems, are especially susceptible to this disease.
Causes of meningitis
The main cause of meningitis are infections of viral and bacterial etiology.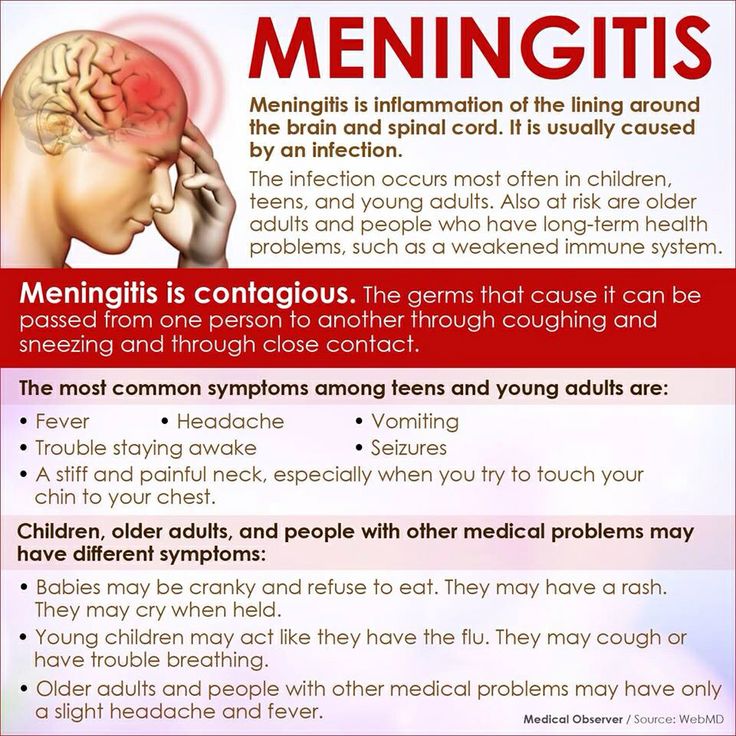 The causative agent of the inflammatory process can be:
The causative agent of the inflammatory process can be:
- pneumococci;
- Haemophilus influenzae;
- Escherichia coli;
- streptococci;
- amoeba.
In childhood, the main cause of the development of pathology is enteroviruses that enter the body by airborne droplets. Infection can occur during childbirth, through contaminated food, dirty water, and insect bites. The main causes of non-infectious meningitis are trauma and damage to the skull, as well as tumor processes occurring in the brain.
Mechanism of development
For the development of pathology, the pathogen must penetrate the cranial cavity and provoke an inflammatory process in the brain. In some cases, this is observed when foci of infection occur in tissues located near the meninges. Pathologies such as purulent otitis media or sinusitis can provoke meningitis.
In some cases, craniocerebral trauma becomes a provoking factor in the development of pathology, but the infection mainly penetrates into the cranial cavity along with the blood flow. The very process of entering the pathogen into the blood and its further spread to the meninges is associated with a poor state of immunity.
The very process of entering the pathogen into the blood and its further spread to the meninges is associated with a poor state of immunity.
Symptoms
Meningitis causes the following clinical picture:
- rise in body temperature;
- photophobia;
- muscle tension in the occipital region;
- confusion;
- convulsive syndrome;
- strabismus;
- muscle pain syndrome;
- mental disorders;
- tachycardia;
- rashes on the skin.
If these symptoms develop, seek medical attention as soon as possible because meningitis has a high mortality rate.
Diagnostic methods
The main method for diagnosing meningitis is lumbar puncture with further examination of cerebrospinal fluid. This diagnostic method is used in all cases when there is a suspicion of a disease.
In addition, the doctor analyzes the patient's complaints and collects an anamnesis, as well as conducts a neurological examination. With the help of a blood test, it is possible to diagnose signs of inflammation, and PCR of blood and cerebrospinal fluid helps to identify the pathogen.
Computed and magnetic resonance imaging allows to assess the structure of the brain and diagnose indirect manifestations of the pathological process in the meninges of the brain.
Prevention
Some forms of meningitis can be prevented by vaccination, which is effective for several years. As a preventive measure, it is recommended to treat chronic and acute pathologies of an infectious nature in a timely manner and take courses of immunostimulating drugs in the foci of meningococcal disease. In addition, you should harden the body, avoid visiting places with large crowds of people and severe hypothermia. In the autumn-winter period, you need to drink multivitamin complexes or vitamin C.
INVITRO. Meningococcal infection, find out the prices for tests and pass in Moscow
- Invitro
- Analyzes
- Diagnostics ...
- meningococcal ...
-
- COVID-19,0005
- Surveys for office employees 9000 9000 9000 personnel
- Assessment of the risk of developing diseases of the cardiovascular system
- Diagnosis of antiphospholipid syndrome (APS)
- Assessment of liver function
- Diagnostics of the state of the kidneys and urogenital system
- Diagnostics of the state of the gastrointestinal tract
- Diagnostics of connective tissue diseases
- Diabage diabetes
- Diagnosis of anemia 9000 glands
- Hospital profiles
- Healthy you - healthy country
- Gynecology, reproduction
- A healthy child: for children from 0 to 14 years old
- infections transmitted by sexually (STPP)
- Problems of weight
- VIP examinations
- Diseases of the respiratory system
- Determination of microelements in the body
- Beauty
- Vitamins
- Diets
- Pre-diet laboratory tests
- Sports profiles
- Hormonal tests for men
- Differential diagnosis of depression
- Evaluation of the blood coagulation system
- Covid-19
- Biochemical studies
- Glucose and carbohydrate metabolites
- proteins and amino acids
- Gilles and acid
- 9000 9000 9000 9000 9000 9000
- Inorganic substances/electrolytes:
- Vitamins
- Proteins involved in iron metabolism
- Cardiospecific proteins
- Laboratory assessment of the state of the Increte function of the gastrointestinal tract
- Laboratory assessment of hormonal regulation of erythropoiesis
- Laboratory assessment of the Epiphyse function
- Analysis for healthy Immunogematological studies Immunogematological studies )
- Immunological studies
- technology Immunocap
- technology Alkorbio
- Markers of autoimmune diseases
- Systemic diseases of the connective tissue
- rheumatoid arthritis, joint damage
- Antifolipid Permanum and kidney lesions
- ,0004000 9000
- 000mapon Celiac disease
- Autoimmune liver diseases
- Neurological autoimmune diseases
- Autoimmune endocrinopathies
- silicon
- Lantan
- Litius
- Magnesium
- Marganese
- Copper
- Molybden
- Nickel
9000 Silver - Strontium
- Antimony
- Thallium
- Phosphorus
- Chromium
- Zinc
- Zirconium
- Clinical urine analysis
- Biochemical Analysis of urine
- Clinical analysis of feces
- Biochemical analysis of feces
- Light-optical study microscopic examination of semen
- Antisperm antibodies
- Viral infections
- Bacterial infections
- fungal infections
- Parasitic infections
- Streptococcal infection
- Examination of newborns to identify hereditary metabolism diseases
- Additional studies (after screening and consultation of a specialist)
- Study of water quality
- Study of soil quality
- Settlement tests performed according to the results of steatoskrin without blood taking
- Blood
- 9000 diagnostics
- ultrasound
-
- Examinations we do not do
- New tests
- Obtaining results
- Additional research orders
- Medical consultant service
- Professional position
- Venous blood for analysis
- Tumor markers.