How to care for cracked nipples
Cracked Nipples: Natural Remedies
Overview
If you’re a breast-feeding mother, you’ve probably had the unpleasant experience of sore, cracked nipples. It’s something that many nursing moms endure. It’s usually caused by a bad latch. This results from improper positioning of your baby at the breast.
Try these five natural remedies to treat sore, cracked nipples. Then learn what you can do to prevent this problem from happening again.
What Causes Cracked Nipples?
Traumatized nipples are described as nipples that are:
- sore
- oozing
- bleeding
- throbbing
- cracked
There are two frequent causes of traumatized nipples: poor latch at the breast and suction trauma as a result of improper positioning.
There are a number of possible reasons for incorrect positioning. Breast-feeding is a learned skill for moms and babies alike. It takes a bit of practice to properly position the nipple in a baby’s mouth and their body against the mother.
Babies who aren’t latched well may protect themselves from forceful letdown reflexes by pinching off the nipple. If a baby has a shallow latch, they may also nurse more frequently. This is because they aren’t getting as much milk at each breast-feeding session.
La Leche League International notes that, in other cases, a baby will pinch their mother’s nipple because of anatomical issues, including a:
- tongue-tie
- small mouth
- receding chin
- short frenulum
- high palate
Other possible causes include:
- nipple confusion (a possibility if you’re breast-feeding, bottle-feeding, or offering pacifiers)
- sucking problems
- baby retracting or improperly positioning their tongue during nursing
It’s important to determine what’s causing your cracked, sore nipples so you can avoid a recurring problem. Speak to a certified lactation consultant. They will be able to assess both your breast-feeding and latch techniques.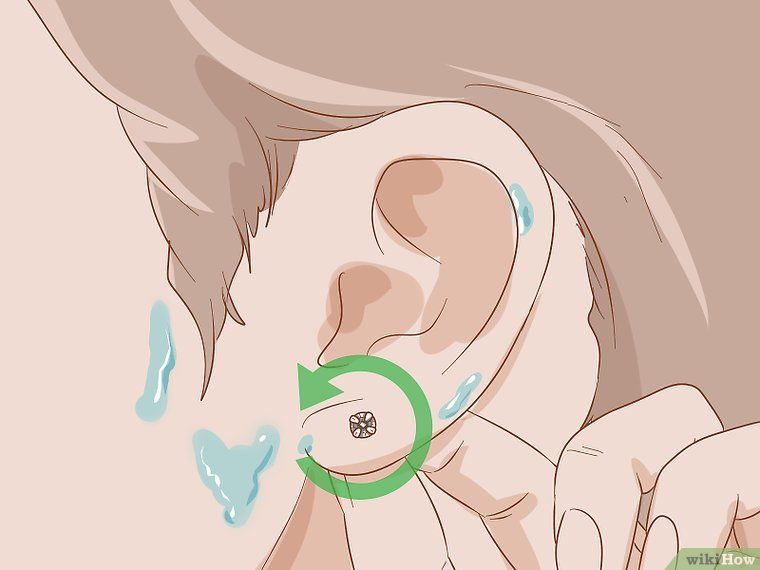 They can also look at your baby’s sucking patterns and strength.
They can also look at your baby’s sucking patterns and strength.
How Can I Treat Cracked Nipples?
Proper positioning is essential for preventing future trauma to your nipples. But how can you treat cracked nipples if you have them?
There are several home and store-bought options for treatment.
Apply Freshly Expressed Breast Milk
Smoothing freshly expressed breast milk onto cracked nipples may help them heal by offering antibacterial protection. If you’re a nursing mother, you’ll have breast milk on hand, making it easy to apply after breast-feeding sessions.
Make sure to wash your hands before gently applying a few drops of breast milk to your nipples. Allow the milk to air-dry before covering up.
Note: If you have thrush, this remedy should be avoided. Any breast milk should be rinsed off the nipple after feeding your baby. Yeast grows quickly in human milk.
Warm Compress
This is another readily available and inexpensive treatment option. While there aren’t any antibacterial benefits, you may find using warm, damp compresses after breast-feeding to be soothing on sore, cracked nipples.
While there aren’t any antibacterial benefits, you may find using warm, damp compresses after breast-feeding to be soothing on sore, cracked nipples.
- To apply, dip a washcloth in warm water.
- Wring out excess liquid.
- Place the washcloth over your nipple and breast for a few minutes.
- Gently pat dry.
Salt Water Rinse
This homemade saline solution will help hydrate the skin and promote healing:
- Mix 1/2 teaspoon of salt in 8 ounces of warm water.
- Soak the nipples in a small bowl of this warm saline solution for about one minute after breast-feeding.
- You can also use a squirt bottle to apply the solution to all areas of the nipple.
- Pat gently to dry.
Be sure to make a fresh supply of saline solution daily to reduce the chances of bacterial contamination. If your baby doesn’t seem to like the taste of the dried solution, rinse your nipples before feeding.
Apply Medical Grade Lanolin Ointment
Using a lanolin ointment specifically designed for breast-feeding mothers will help promote moist wound healing. Apply to nipples after breast-feeding. It doesn’t need to be removed before nursing your baby.
Apply to nipples after breast-feeding. It doesn’t need to be removed before nursing your baby.
Change Nursing Pads Frequently
Change nursing pads as soon as they become damp. Leaving the moisture against your nipples can delay healing. Also avoid nursing pads made with plastic linings. They can obstruct airflow. Look for pads made from 100 percent cotton.
Remedies to avoid
You may hear of other remedies for cracked, sore nipples. But some of these can be counter-effective and should be avoided.
- Wet tea bags: This is a popular remedy in many locations around the world. While they’re inexpensive, the tannic acid from the tea can have an astringent effect on the nipple. This can dry out the nipple or even cause cracking. If the moist warmth is appealing, stick with a plain water compress.
- Using ointments or creams that aren’t 100 percent lanolin, or shouldn’t be ingested:Some products marketed to breast-feeding mothers can prevent air circulation and dry out the skin.
 Avoid products that shouldn’t be ingested. These could be harmful to your baby. If you must wash your nipples before every feeding, you’ll lose the benefit of natural lubrication.
Avoid products that shouldn’t be ingested. These could be harmful to your baby. If you must wash your nipples before every feeding, you’ll lose the benefit of natural lubrication.
Takeaway
Remember, cracked nipples are often a symptom of breast-feeding. While it’s important to help cracked nipples heal, it’s also important to address the cause of the problem.
If you have questions or concerns about cracked nipples, see your pediatrician or a certified lactation consultant.
Share on Pinterest
Healing Tips for Nipple Cracks or Abrasions • KellyMom.com
By Kelly Bonyata, BS, IBCLC
The following measures can be very helpful if the skin on the nipple is broken for any reason (cracked nipple due to shallow latch, tongue-tie/lip-tie or other anatomical variations, thrush, a bite, milk blister, etc.).
Keep in mind that one of the most important factors in healing is to correct the source of the problem.
Now infants can get
all their vitamin D
from their mothers’ milk;
no drops needed with
our sponsor's
TheraNatal Lactation Complete
by THERALOGIX. Use PRC code “KELLY” for a special discount!
Use PRC code “KELLY” for a special discount!
Continue to work on correct latch and positioning, thrush treatment, etc. as you treat the symptoms, and talk to a La Leche League Leader and/or board certified lactation consultant (IBCLC) if what you’re doing is not working.
During the nursing session | After nursing | Between nursings | Additional information
- Breastfeed from the uninjured (or less injured) side first. Baby will tend to nurse more gently on the second side offered.
- The initial latch-on tends to hurt the worst – a brief application of ice right before latching can help to numb the area.
- Experiment with different breastfeeding positions to determine which is most comfortable.
- If breastfeeding is too painful, it is very important to express milk from the injured side to reduce the risk of mastitis and to maintain supply. If pumping is too painful, try hand expression.
After nursing
Salt water rinse
This special type of salt water, called normal saline, has the same salt concentration as tears and should not be painful to use.
To make your own normal saline solution:
Mix 1/2 teaspoon of salt in one cup (8 oz) of warm water. Make a fresh supply each day to avoid bacterial contamination. You may also buy individual-use packets of sterile saline solution.
- After breastfeeding, soak nipple(s) in a small bowl of warm saline solution for a minute or so–long enough for the saline to get onto all areas of the nipple. Alternately, put the saline solution into a squeeze bottle and squirt it on gently; use plenty of saline, making sure to get it on all areas of broken skin.
- Avoid prolonged soaking (more than 5-10 minutes) that “super” hydrates the skin, as this can promote cracking and delay healing.
- Pat dry very gently with a soft paper towel.
- If baby objects to the taste of the residual salt from the saline rinse, rinse directly before nursing by dipping nipple(s) into a bowl of plain water. Pat dry gently.
After the salt water rinse
- Apply expressed breastmilk to the nipples to promote healing–this can be done in addition to other treatments.
- To promote “moist wound healing” (this refers to maintaining the internal moisture of the skin, not keeping the exterior of the skin wet) apply a medical grade lanolin ointment (e.g., Lansinoh, Purelan), soft paraffin/vaseline or a hydrogel dressing (e.g., ComfortGel, Soothies).
- If you have thrush, follow the saline soak with an antifungal ointment or other thrush treatment.
- If needed, apply an antibiotic ointment (e.g. Bactroban/mupirocin, Polysporin) or Dr. Jack Newman’s All Purpose Nipple Ointment(APNO; an antibiotic/anti-inflammatory/anti-yeast combo) sparingly after each feeding.
- Per Hale, Bactroban ointment (mupirocin; lactation risk category L1/safest), available only by prescription, may be the best choice for nursing mothers.
- Of the over-the-counter treatments, Polysporin (Polymyxin B Sulfate and Bacitracin Zinc) may be preferred for topical use in the nipple area of nursing moms over antibiotic ointments containing neomycin (such as Neosporin or triple antibiotic ointment).
 Neomycin carries a small risk (1-2% of the general population) of contact dermatitis (see The Role of Topical Antibiotics in Dermatologic Practice by J.J. Leyden, MD).
Neomycin carries a small risk (1-2% of the general population) of contact dermatitis (see The Role of Topical Antibiotics in Dermatologic Practice by J.J. Leyden, MD). - It is not necessary to wash small amounts of antibiotic or APNO ointment from the nipple prior to nursing, even if baby nurses again within minutes (see Dr. Jack Newman’s Sore Nipples info). If too much ointment was used and there is an obvious amount remaining when baby is ready to nurse again, gently wipe the excess off with a damp cloth.
Between nursings
- Keep nipples exposed to air when possible. When wearing a bra, use fresh disposable pads (change when damp). Some mothers use breast shells to protect the nipple from the dampness and friction of the bra.
- If there is a specific injury–like a bite–cold compresses (ice packs over a layer of cloth) may help: 20 minutes on, 20 minutes off; repeat as needed.
- Ibuprofen (Advil, Motrin) or acetaminophen (Tylenol) is compatible with breastfeeding.

- Once a day, use a non-antibacterial, non-perfumed soap to gently clean the wounded area, then rinse well under running water. Using soap on the nipple area is not recommended unless the skin is broken.
| Contact your health care provider if you notice:Fever, inflammation/redness, swelling, oozing, pus, or other signs of infection. It is possible to have multiple infections (both fungal and bacterial). If the nipple is obviously infected, then talk to your health care provider about the possibility of using an oral (systemic) antibiotic. One study indicated that topical antibiotics and good breastfeeding techniques might not be sufficient if infection is present. (See Livingstone V, Stringer LJ. The treatment of Staphyloccocus aureus infected sore nipples: a randomized comparative study. J Hum Lact. 1999 Sep;15(3):241-6.) See also Oral antibiotic use for sore, cracked nipples and Staphylococcus aureus and sore nipples. |
Additional information
Treatment of Sore, Cracked, or Bleeding Nipples by Becky Flora, IBCLC
Sore Nipples by Jack Newman, MD, FRCPC
Nipple Pain by Paula Yount
Sore Nipples in the Breastfeeding Mother from Lactation Education Resources
Barton A. Oral Antibiotics and Positioning Are Effective in Decreasing Morbidity in Breastfeeding Mothers. Critically-Appraised Topic from University of Michigan Evidence-Based Pediatrics Web Site, February 14, 2000.
Buchanan P, Hands A, Jones W. Assessing the evidence: Cracked Nipples and Moist Wound Healing. Paisley, Scotland: The Breastfeeding Network, March 2002.
Livingstone V, Stringer LJ. The treatment of Staphyloccocus aureus infected sore nipples: a randomized comparative study. J Hum Lact. 1999 Sep;15(3):241-6.
Martin J. Nipple Pain: Causes, Treatments, and Remedies. Leaven. February-March 2000;36(1):10-11.
Morland-Schultz K, Hill PD. Prevention of and therapies for nipple pain: a systematic review. J Obstet Gynecol Neonatal Nurs. 2005 Jul-Aug;34(4):428-37.
J Obstet Gynecol Neonatal Nurs. 2005 Jul-Aug;34(4):428-37.
Cracked nipple Wikipedia
Nursing nipple care | Breast Care
Breastfeeding is good for you and your baby, but it can be a real challenge for the nipples. Check out our tips and tricks to help reduce the pain.
Share this information
Sioned Hilton, health visitor, neonatal nurse and lactation consultant:
A mother of three, Sioned Hilton has been supporting families with newborns and young children for over 30 years. She provides advice on breastfeeding and pumping, both in clinics and at home. In addition, Schoned writes articles for parenting magazines, attends conferences, and conducts seminars for attending physicians.
New mothers often hear: "Breastfeeding doesn't have to be painful." However, in the early days, many are faced with the opposite.
In most women during pregnancy, the nipples enlarge and become more sensitive. When a newborn baby begins to suckle, it creates a certain pressure, and this is a completely new and unfamiliar sensation for a woman (at least for a first-time mother).
Feedings can be prolonged for a long time, sometimes up to an hour, and the child may ask to be breastfed up to 13 times a day. 1 This sucking, pressure and saliva of the baby can cause sore nipples.
Remember how your lips crack in the wind and sun. The more often you lick them, the more they will dry and become inflamed. Therefore, lips require good hydration to soften, protect and speed up the healing of cracks. The same thing happens with nipples.
However, sore nipples usually don't last more than a couple of weeks and go away as your baby and your breasts get used to breastfeeding. It is important to start nipple care as early as possible to prevent the situation from worsening. Therefore, if your nipples become very inflamed, crack or bleed, contact your doctor as soon as possible. 2
Prevention is better than cure, so check out our tips.
Check your baby's latch-on
Correct latch is the key to pain-free breastfeeding. When putting the baby to the breast, point the nipple towards his palate. This will allow him to grab the nipple and the part of the areola (the darker skin around the nipple) underneath. When the nipple and part of the breast is in the baby's mouth, feeding is taking place correctly. 3
When putting the baby to the breast, point the nipple towards his palate. This will allow him to grab the nipple and the part of the areola (the darker skin around the nipple) underneath. When the nipple and part of the breast is in the baby's mouth, feeding is taking place correctly. 3
For the first few days, see a lactation consultant or specialist to check for proper latch. He will be able to give you advice on how to solve problems and recommend other feeding positions that will make it less painful for you to feed your baby.
Check tongue tie
Tongue tie (ankyloglossia) occurs in 4-11% of
newborns. 4 At the same time, the strip of skin that attaches the tongue to the bottom of the mouth - the so-called frenulum - is too short. A child with a shortened frenulum will not be able to open his mouth wide enough to latch onto the breast well, and his tongue will not cover the lower gum when sucking. As a result, the baby will be nervous, and your nipples may become inflamed.
The doctor or lactation consultant must examine the baby to make this diagnosis. The problem of a shortened bridle is solved by a simple undercutting procedure. It is performed by a doctor, and is usually done without blood and does not require anesthesia. Cutting the bridle allows you to restore the normal feeding mechanism almost instantly. 5
Less common in children is a short frenulum of the upper lip. In this case, it is necessary to dissect the skin that connects the upper lip to the gum. A shortened frenum of the tongue or upper lip in a newborn is not always detected during the examination conducted immediately after birth, so if you think that this is what is causing your nipples pain, seek medical advice as soon as possible. 4
Breastfeeding Tips
- Wash your breasts with water only when you shower or bathe. Small bumps on the areola (Montgomery's glands) secrete oil that moisturizes and protects your nipples. Soaps and shower gels can strip away this natural defense, causing dryness and irritation.
 6
6 - Pat the nipples gently with a soft towel or simply let them air dry. In the past, women were often advised to rub their nipples to make them stiffer, but thankfully, such advice is a thing of the past!
- Do not wash breasts or nipples before feeding. The bacteria found on the surface of the breast actually help the baby's intestinal microflora to develop. 7
- Fresh breast milk helps to heal cracked nipples, 8 so rub a few drops of milk into them before and after feeding.
- Change your bra pads often if they get wet. This will reduce the risk of bacterial and fungal infections, including thrush. 6
- It is not necessary to increase the intervals between feedings to give the nipples a "rest". For a baby to be healthy and grow well, it needs to be fed on demand. Remember, frequent feeding stimulates and maintains milk production, so keep feeding despite the pain. 9
Healthy teat care products
- Pure lanolin teat cleaner, a natural product derived from sheep's wool.
 It moisturizes and promotes healing of the nipples. This cream is safe for the baby, so it does not need to be washed off before feeding.
It moisturizes and promotes healing of the nipples. This cream is safe for the baby, so it does not need to be washed off before feeding. - Hydrogel Pads* can be applied to sore nipples to relieve pain while feeding and help promote healing. They can even be stored in the refrigerator to enhance the soothing cooling effect.
- Breast pads* fit into the bra. They help prevent nipple irritation from clothing and have air holes to help nipples heal.
- Nursing Bras** are made from breathable material such as cotton or a special fabric that dries quickly and wicks moisture away from sore nipples.
- Nursing pads* are special silicone pads that fit over the nipples. They have small holes through which milk flows when you are breastfeeding. The pads help to protect the skin underneath and help the baby to better latch on to the nipple by making the nipple stiffer. Do not use nursing pads for a long time. If you have problems or pain, contact your healthcare professional or lactation consultant.

When to Seek Medical Care
The soreness should go away as your nipples and baby get used to breastfeeding. It is worth repeating that the main cause of sore nipples is improper grip. If your lactation consultant has not been able to resolve your pain while feeding, see another specialist and a third if necessary.
If nipple pain persists or if you notice unusual symptoms, talk to your doctor. The appearance of white spots or flakes on the nipples may be a sign of thrush, whitish or bluish nipples may indicate a circulation disorder such as Raynaud's disease (vasospasm), and pus and redness indicate an infection. 2
Literature
1 Kent JC et al. Volume and frequency of breastfeedings and fat content of breast milk throughout the day. Pediatrics. 2006;117(3): e 387-395. - Kent J.S. et al., "Amount and frequency of breastfeeding and fat content of breast milk during the day." Pediatrix (Pediatrics). 2006;117(3):e387-95.
2006;117(3):e387-95.
2 Berens P et al. Academy of Breastfeeding Medicine. ABM Clinical Protocol#26: Persistent pain with breastfeeding. Breastfeeding Medicine. 2016;11(2):46-53. - Behrens, P. et al., Academy of Breastfeeding Medicine, AVM Clinical Protocol #26: Persistence of Breastfeeding Pain. Brestfeed Med (Breastfeeding Medicine). 2016;11(2):46-53.
3 Cadwell K. Latching - On and Suckling of the Healthy Term Neonate: Breastfeeding Assessment. J Midwifery & Women's Health. 2007;52(6):638-42. — Cadwell, K., "Latching and sucking in healthy newborns: evaluation of breastfeeding." F Midwifery Women Health. 2007;52(6):638-642.
4 Segal LM et al. Prevalence, diagnosis, and treatment of ankyloglossia: methodological review. Canadian Family Physician. 2007;53(6):1027-1033. - Segal L.M. et al., Incidence, Diagnosis, and Treatment of Ankyloglossia: A Methodological Review. Canadian Family Physic. 2007;53(6):1027-1033.
Canadian Family Physic. 2007;53(6):1027-1033.
5 O'Shea JE et al. Frenotomy for tongue - tie in newborn infants. The Cochrane Library. 2017. - O'Shea J.I. et al., "Dissection of the frenulum in the newborn", The Cochrane Labrery (Cochrane Library), 2017.
6 Jacobs A et al. S3-guidelines for the treatment of inflammatory breast disease during the lactation period. Geburtshilfe und Frauenheilkunde. 2013;73(12):1202-1208. - Jacobs A. et al., "Recommendations S -3 for the treatment of inflammatory diseases of the breast during breastfeeding. Geburtskhilfe und Frauenheilkünde. milk bacterial communities and establishment and development of the infant gut microbiome JAMA pediatrics 2017;171(7):647-654 - P. S. Pannaraj et al. development of the neonatal gut microbiome." JAMA pediatric. 2017;171(7):647-654.
8 Mohammadzadeh A et al. The effect of breast milk and lanolin on sore nipples. Saudi medical journal. 2005;26(8):1231-1234. — Mohammedzade A. et al., "Effects of breast milk and lanolin on sore nipples." Saudi Medical Journal. 2005;26(8):1231-1234.
The effect of breast milk and lanolin on sore nipples. Saudi medical journal. 2005;26(8):1231-1234. — Mohammedzade A. et al., "Effects of breast milk and lanolin on sore nipples." Saudi Medical Journal. 2005;26(8):1231-1234.
9 Kent JC et al. Principles for maintaining or increasing breast milk production. J Obstet , Gynecol , & Neonatal Nurs . 2012;41(1):114-121. - Kent J.S. et al., "Principles for Maintaining and Increasing Milk Production". J Obstet Ginecol Neoneutal Nurs. 2012;41(1):114-121.
Read instructions before use. Consult a specialist about possible contraindications.
* RC № № ФСЗ 2010/07352 dated 19.07.2010
** RC No. FZZ 2009/05592 dated 11.25.2009
Teat cracks | Medela
Amir, L.H. ABM Clinical Protocol #4: Mastitis, Revised March 2014. Breastfeed Med 9, 239–243 (2014). - Amir L.Kh., "AVM Clinical Protocol #4: Mastitis", revised March 2014 Brestfeed Med 9 (Breastfeeding Medicine) 239–243 (2014).
Breastfeed Med 9, 239–243 (2014). - Amir L.Kh., "AVM Clinical Protocol #4: Mastitis", revised March 2014 Brestfeed Med 9 (Breastfeeding Medicine) 239–243 (2014).
Jacobs, A. et al. S3-Guidelines for the Treatment of Inflammatory Breast Disease during the Lactation Period: AWMF Guidelines, Registry No. 015/071 (short version) AWMF Leitlinien-Register Nr. 015/071 (Kurzfassung). Geburtshilfe Frauenheilkd . 73, 1202–1208 (2013). - Jacobs, A. et al., "Guideline S -3 for the management of inflammatory breast disease during breastfeeding: AWMF Guideline , registration number 015/071 (abbreviated version)" 2 Leitlinjen- Registration number 015/071 (Kurzfassung).
American Academy of Pediatrics and The American College of Obstetricians and Gynecologists. Breastfeeding handbook for physicians 2006). - American Academy of Pediatrics and American College of Obstetrics and Gynecology. "Medical Guide to Breastfeeding", 2006.
- American Academy of Pediatrics and American College of Obstetrics and Gynecology. "Medical Guide to Breastfeeding", 2006.
Lawrence , R . A . & Lawrence , R . M . Breastfeeding : a guide for the medical profession ( Elsevier Mosby , Maryland Heights , MO , 2011). - Lawrence R.A., Lawrence R.M., "Breastfeeding: A guide for healthcare professionals." (Publisher Maryland Heights , Missouri, USA: Elsevier Mosby; 2011.)
McClellan, H.L. et al. Infants of mothers with persistent nipple pain exert strong sucking vacuums. Paediatica 97, 1205–1209 (2008). — McClellan H.L. et al., "Babies of mothers suffering from persistent nipple pain create extremely high sucking vacuums." Pediatrics 97, 1205–1209 (2008).
Paediatica 97, 1205–1209 (2008). — McClellan H.L. et al., "Babies of mothers suffering from persistent nipple pain create extremely high sucking vacuums." Pediatrics 97, 1205–1209 (2008).
McClellan, H.L. et al. Breastfeeding frequency, milk volume, and duration in mother-infant dyads with persistent nipple pain. Breastfeed Med 7, 275–281 (2012). — McClellan H.L. et al., "Breastfeeding frequency, milk quantity and duration of feedings in case of persistent maternal nipple soreness", Brestfeed Med (Breastfeeding Medicine) 7, 275–281 (2012).
McClellan, H.L. et al. Nipple pain during breastfeeding with or without visible trauma. J Hum Lact 28, 511–521 (2012). — McClellan H.L. et al., "Nipple pain during breastfeeding with or without visible lesions." J Hum Lakt (Journal of the International Association of Lactation Consultants" 28, 511–521 (2012).
Learn more
 )
)