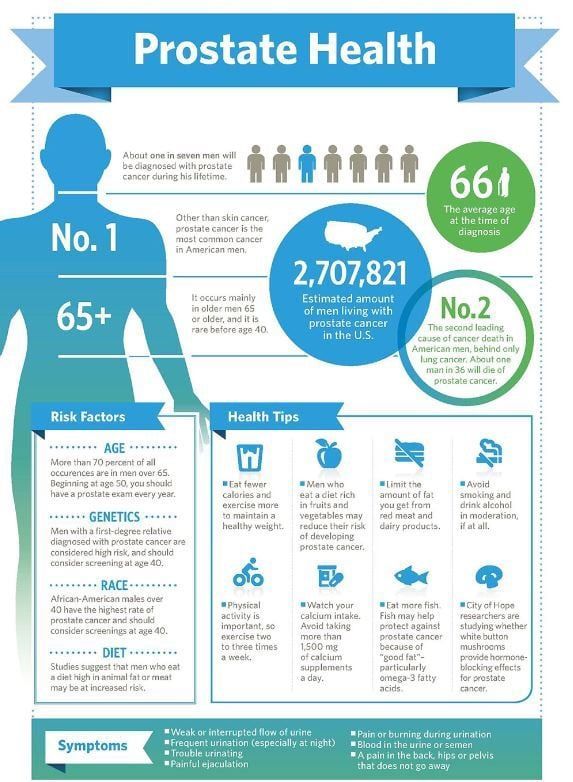
30 weeks pelvic pain
Pelvic pain in pregnancy - NHS
Some women may develop pelvic pain in pregnancy. This is sometimes called pregnancy-related pelvic girdle pain (PGP) or symphysis pubis dysfunction (SPD).
PGP is a collection of uncomfortable symptoms caused by a stiffness of your pelvic joints or the joints moving unevenly at either the back or front of your pelvis.
Symptoms of PGP
PGP is not harmful to your baby, but it can be painful and make it hard to get around.
Women with PGP may feel pain:
- over the pubic bone at the front in the centre, roughly level with your hips
- across 1 or both sides of your lower back
- in the area between your vagina and anus (perineum)
- spreading to your thighs
Some women may feel or hear a clicking or grinding in the pelvic area.
The pain can be worse when you're:
- walking
- going up or down stairs
- standing on 1 leg (for example, when you're getting dressed)
- turning over in bed
- moving your legs apart (for example, when you get out of a car)
Most women with PGP can have a vaginal birth.
Non-urgent advice: Call your midwife or GP if you have pelvic pain and:
- it's hard for you to move around
- it hurts to get out of a car or turn over in bed
- it's painful going up or down stairs
These can be signs of pregnancy-related pelvic girdle pain.
Treatments for PGP
Getting diagnosed as early as possible can help keep pain to a minimum and avoid long-term discomfort.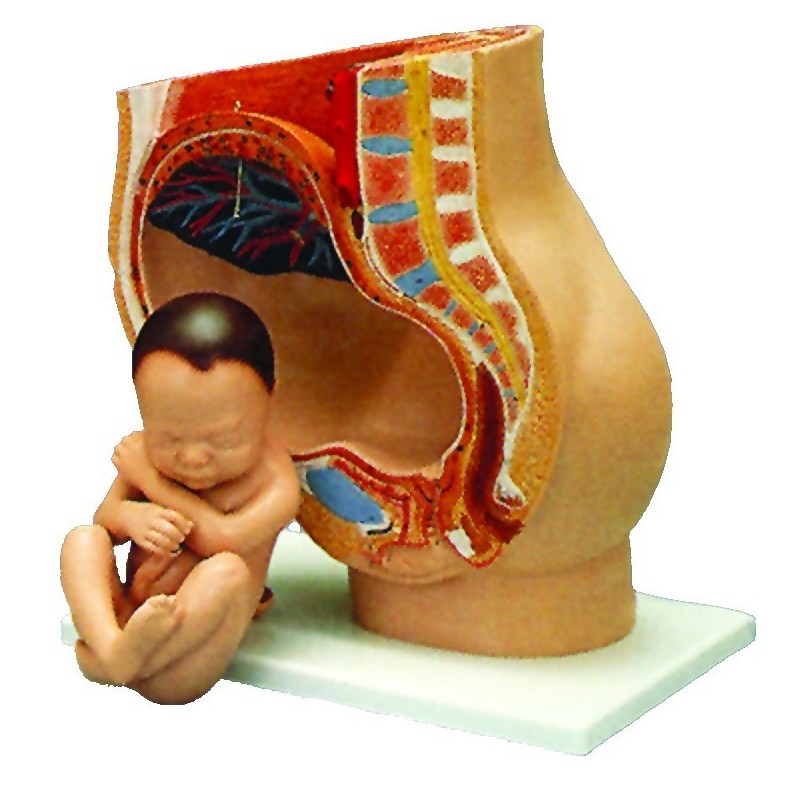
You can ask your midwife for a referral to a physiotherapist who specialises in obstetric pelvic joint problems.
Physiotherapy aims to relieve or ease pain, improve muscle function, and improve your pelvic joint position and stability.
This may include:
- manual therapy to make sure the joints of your pelvis, hip and spine move normally
- exercises to strengthen your pelvic floor, stomach, back and hip muscles
- exercises in water
- advice and suggestions, including positions for labour and birth, looking after your baby and positions for sex
- pain relief, such as TENS
- equipment, if necessary, such as crutches or pelvic support belts
These problems tend not to get completely better until the baby is born, but treatment from an experienced practitioner can improve the symptoms during pregnancy.
You can contact the Pelvic Partnership for information and support.
Coping with pelvic pain in pregnancy
Your physiotherapist may recommend a pelvic support belt to help ease your pain, or crutches to help you get around.
It can help to plan your day so you avoid activities that cause you pain. For example, do not go up or down stairs more often than you have to.
The Pelvic, Obstetric & Gynaecological Physiotherapy (POGP) network also offers this advice:
- be as active as possible within your pain limits, and avoid activities that make the pain worse
- rest when you can
- ask your family, friends or partner, if you have one, to help with everyday activities
- wear flat, supportive shoes
- sit down to get dressed – for example, do not stand on 1 leg when putting on jeans
- keep your knees together when getting in and out of the car – a plastic bag on the seat can help you swivel
- sleep in a comfortable position – for example, on your side with a pillow between your legs
- try different ways of turning over in bed – for example, turning over with your knees together and squeezing your buttocks
- take the stairs 1 at a time, or go upstairs backwards or on your bottom
- if you're using crutches, have a small backpack to carry things in
- if you want to have sex, consider different positions, such as kneeling on all fours
POGP suggests that you avoid:
- standing on 1 leg
- bending and twisting to lift, or carrying a baby on 1 hip
- crossing your legs
- sitting on the floor, or sitting twisted
- sitting or standing for long periods
- lifting heavy weights, such as shopping bags, wet washing or a toddler
- vacuuming
- pushing heavy objects, such as a supermarket trolley
- carrying anything in only 1 hand (try using a small backpack)
The physiotherapist should be able to provide advice on coping with the emotional impact of living with chronic pain, such as using relaxation techniques. If your pain is causing you considerable distress, then you should let your GP or midwife know. You may require additional treatment.
If your pain is causing you considerable distress, then you should let your GP or midwife know. You may require additional treatment.
Download the POGP leaflet Pregnancy-related pelvic girdle pain for mothers-to-be and new mothers.
You can get more information on managing everyday activities with PGP from the Pelvic Partnership.
Labour and birth with pelvic pain
Many women with pelvic pain in pregnancy can have a normal vaginal birth.
Plan ahead and talk about your birth plan with your birth partner and midwife.
Write in your birth plan that you have PGP, so the people supporting you during labour and birth will be aware of your condition.
Think about birth positions that are the most comfortable for you, and write them in your birth plan.
Being in water can take the weight off your joints and allow you to move more easily, so you might want to think about having a water birth. You can discuss this with your midwife.
You can discuss this with your midwife.
Your 'pain-free range of movement'
If you have pain when you open your legs, find out your pain-free range of movement.
To do this, lie on your back or sit on the edge of a chair and open your legs as far as you can without pain.
Your partner or midwife can measure the distance between your knees with a tape measure. This is your pain-free range.
To protect your joints, try not to open your legs wider than this during labour and birth.
This is particularly important if you have an epidural for pain relief in labour, as you won't be feeling the pain that warns you that you're separating your legs too far.
If you have an epidural, make sure your midwife and birth partner are aware of your pain-free range of movement of your legs.
When pushing in the second stage of labour, you may find it beneficial to lie on one side.
This prevents your legs from being separated too much. You can stay in this position for the birth of your baby, if you wish.
Sometimes it might be necessary to open your legs wider than your pain-free range to deliver your baby safely, particularly if you have an assisted delivery (for example, with the vacuum or ventouse).
Even in this case, it's possible to limit the separation of your legs. Make sure your midwife and doctor are aware that you have PGP.
If you go beyond your pain-free range, your physiotherapist should assess you after the birth.
Take extra care until they have assessed and advised you.
Who gets pelvic pain in pregnancy?
It's estimated that PGP affects up to 1 in 5 pregnant women to some degree.
It's not known exactly why pelvic pain affects some women, but it's thought to be linked to a number of issues, including previous damage to the pelvis, pelvic joints moving unevenly, and the weight or position of the baby.
Factors that may make a woman more likely to develop PGP include:
- a history of lower back or pelvic girdle pain
- previous injury to the pelvis (for example, from a fall or accident)
- having PGP in a previous pregnancy
- a physically demanding job
- being overweight
- having a multiple birth pregnancy
healthtalk.org has interviews with women talking about their experiences of pelvic pain in pregnancy.
Read more about coping with common pregnancy problems, including nausea, heartburn, tiredness and constipation.
Find maternity services or physiotherapy services near you.
Community content from HealthUnlockedPelvic pain in pregnancy (SPD)
Tommy's PregnancyHub
Pelvic pain is common in pregnancy and is known as Symphysis Pubis Dysfunction (SPD) or Pelvic Girdle Pain (PGP). The pain is caused by stiffness or uneven movements of the pelvic joints in pregnancy, which affects up to 1 in 5 women.
The pain is caused by stiffness or uneven movements of the pelvic joints in pregnancy, which affects up to 1 in 5 women.
Pelvic pain in pregnancy was originally called Symphysis Pubis Dysfunction (SPD) but health professionals now call it Pelvic Girdle Pain (PGP) because it affects all the joints of the pelvis not just the one called the Symphysis Pubis.
Symptoms of PGP
- pain deep in the pubic area and groin (between the vagina and anus)
- the pain can be manageable or severe
- it can be brought on by some types of activity, such as walking, climbing stairs and turning over in bed
- you may also have pain across your lower back
- you might have a grinding or clicking sensation in your pubic area
- the pain can be made worse by parting your legs or by leaning on one leg.
Causes of PGP
For some women in pregnancy the pelvic joints become stiff or less stable. This can cause inflammation and pain, which varies in severity. The pain can range from a dull ache to severe pain. Most sufferers are in the mild to moderate category.
The pain can range from a dull ache to severe pain. Most sufferers are in the mild to moderate category.
It is usually possible to successfully treat PGP, though the earlier a diagnosis is made and treatment is started, the better.
Certain types of movement, such as widening the legs or leaning on one leg, can make the pain worse.
For those with bad to severe pain, the condition can make it difficult to continue doing normal day to day activities. Pain can also affect your sleep, causing your emotional health to suffer too.
As PGP doesn’t affect the baby, sometimes women feel as if they should just put up with it and that it is not a priority. This is not the case and if you’re suffering from it, talk to your midwife or GP. They should be able to refer you to a physiotherapist who has experience of treating pelvic joint pain.
"I have had SPD since around 22 weeks pregnant. I thought it was sciatica at first and just struggled on but after a few days I found myself bed bound and went to the GP.
She referred me to physio who gave me some exercises to do.” Mollie
Watch our Facebook live about pelvic pain in pregnancy
Treatment for PGP
Physiotherapy
Physiotherapy treatment for pelvic pain might be different depending on your physiotherapist, but it is likely to include the following:
- hands-on therapy to restore normal movement of muscles and joints in the pelvis
- exercises to strengthen your pelvic floor, stomach, back and hip muscles
- exercises in water
- advice around labour and birth
- they may give you a pelvic support belt or crutches if they think these may help you.
Medication
Many people worry about taking pain medication during pregnancy, but there are some safe options for you and your baby. Ask for advice from your GP, midwife or a pharmacist to find out what pain medicine you can take.
Alternative therapies
You can also try to manage pain with alternative therapies, which could include things like:
- a TENS machine
- acupuncture
- hypnosis
- meditation, for example mindfulness or yoga
- complementary therapies such as massage or reflexology.
Review dates
Reviewed: 06 December 2018 | Next review: 06 December 2021
This content is currently being reviewed by our team. Updated information will be coming soon.
Back to top
Pain in the pubic region during pregnancy
Subscribe to our Instagram! Useful information about pregnancy and childbirth from leading obstetricians and gynecologists in Moscow and foreign experts: https://www.instagram.com/roddompravda/
Tips and opinions from leading child professionals: https://www.instagram.com/emc.child/
The pubic bone is one of the three bones that make up the pelvic bone. Two pubic bones, forming the pubic articulation (symphysis), form the anterior wall of the pelvis. The pubic bone in women with a regular physique has the form of a roller about the thickness of the thumb, which is curved and forms a pubic eminence. This bone hangs in a kind of arch over the entrance to the vagina.
This bone hangs in a kind of arch over the entrance to the vagina.
The main cause of pain in the pubic bone is the divergence and increased mobility of the pubic symphysis. To refer to pathological changes in the pubic symphysis of the pelvis during pregnancy and after childbirth, the following terms are used: symphysiopathy, symphysitis, arthropathy of pregnant women, divergence and rupture of the pubic symphysis, dysfunction of the pubic symphysis. The most commonly used terms are "symphysitis" or "symphysiopathy".
So, symphysiopathy is a disease associated with a pronounced softening of the pubic joint under the influence of the hormone relaxin, which is produced during pregnancy. The process of softening the interosseous joints is natural, it helps the child to pass more easily through the bone pelvis during childbirth. The diagnosis of "symphysiopathy" is made when severe pain appears, the pubic joint swells, greatly stretches, becomes mobile, and the pubic bones diverge excessively. One of the striking, characteristic symptoms of this pathology is that it is impossible to raise the leg in the prone position. In addition to acute pain in the pubis, there are difficulties when walking up the stairs, it becomes difficult to turn from side to side on the bed and get up from the sofa, and the gait changes and becomes like a "duck". According to most doctors, the cause of symphysiopathy is a lack of calcium, an increased concentration of the hormone relaxin, and increased physical activity on the bones of the pelvic region. In addition, the development of symphysiopathy can be provoked by a serious sports injury or a fracture of the pelvic bones.
One of the striking, characteristic symptoms of this pathology is that it is impossible to raise the leg in the prone position. In addition to acute pain in the pubis, there are difficulties when walking up the stairs, it becomes difficult to turn from side to side on the bed and get up from the sofa, and the gait changes and becomes like a "duck". According to most doctors, the cause of symphysiopathy is a lack of calcium, an increased concentration of the hormone relaxin, and increased physical activity on the bones of the pelvic region. In addition, the development of symphysiopathy can be provoked by a serious sports injury or a fracture of the pelvic bones.
At what stage of pregnancy do they occur?
The disease begins gradually or suddenly during pregnancy, childbirth or after childbirth. Most often, women begin to feel pain in the area of the pubic joint in the third trimester of pregnancy. This is due to the fact that the places of adhesions of the pubic bones, their ligaments and cartilage, soften under the influence of the hormone relaxin. This hormone of pregnancy naturally softens the bony joints, which is necessary to facilitate the passage of the child's bone pelvis and birth canal at the time of childbirth.
This hormone of pregnancy naturally softens the bony joints, which is necessary to facilitate the passage of the child's bone pelvis and birth canal at the time of childbirth.
Some women begin to complain of pain in the pelvic bones some time after giving birth. This may be the result of traumatic childbirth (imposition of obstetrical forceps, shoulder dystocia, excessive separation of the hips during childbirth, etc.) or physical exertion (lifting a heavy baby stroller up the stairs, prolonged motion sickness in the arms of a well-fed baby, etc.). It is recommended to limit physical activity, wear an orthopedic bandage, consult a traumatologist. Complaints usually recur after the next pregnancy. In a small proportion of patients, pain persists for a long time.
When can this be considered the norm, and when not?
Obstetricians-gynecologists do not consider a slight soreness of the pubic joint to be a pathology, but if the pain is acute, restricting the movements of the pregnant woman, accompanied by edema, then we can talk about pathology. Pain can be quite strong and especially manifest itself while walking, turning the body to the right and left in a sitting position and even lying down. In this case, you need to urgently consult a doctor and undergo an ultrasound diagnosis (ultrasound) to determine the size of the divergence of the pubic bones. Magnetic resonance imaging (MRI) is also used, which allows assessing the state of the symphysis, the state of the bone tissue, as well as soft tissues.
Pain can be quite strong and especially manifest itself while walking, turning the body to the right and left in a sitting position and even lying down. In this case, you need to urgently consult a doctor and undergo an ultrasound diagnosis (ultrasound) to determine the size of the divergence of the pubic bones. Magnetic resonance imaging (MRI) is also used, which allows assessing the state of the symphysis, the state of the bone tissue, as well as soft tissues.
With ultrasound, the degree of divergence (diastasis) of the pubic bones is determined. The severity of the clinical picture largely depends on the degree of divergence of the pubic bones, and therefore there are three degrees of divergence of the pubic branches: in the first degree - by 6-9 mm, in the second - by 10-20 mm, in the third - more than 20 mm. The severity of the symptoms of the disease varies from mild discomfort to unbearable pain.
How can pain be relieved?
There are some recommendations that will help reduce bone pain during pregnancy, if the cause of its occurrence is the divergence of the pubic bones. Be sure to wear a bandage, especially in later pregnancy. The bandage takes on most of the load, thereby releasing pressure from the pubic joint. Limitation of heavy physical exertion is indicated for any manifestations of pain, lying down more often, walking less and being in a sitting position for no longer than 30-40 minutes. In severe cases, before and sometimes after childbirth, a woman may be shown strict bed rest. Moreover, the bed should not be hard and flat.
Be sure to wear a bandage, especially in later pregnancy. The bandage takes on most of the load, thereby releasing pressure from the pubic joint. Limitation of heavy physical exertion is indicated for any manifestations of pain, lying down more often, walking less and being in a sitting position for no longer than 30-40 minutes. In severe cases, before and sometimes after childbirth, a woman may be shown strict bed rest. Moreover, the bed should not be hard and flat.
Since the appearance of symphysiopathy is associated not only with a large production of the hormone relaxin, but also with a lack of calcium in the body, the expectant mother is prescribed calcium preparations and complex vitamins for pregnant women, which contain all the necessary vitamins and trace elements in the right amount and proportions. There is evidence that pain is reduced during acupuncture and physiotherapy.
In especially severe cases of symphysiopathy, the pregnant woman is hospitalized.
What is the danger of this condition?
The occurrence of symphysiopathy is due to several reasons. This is a lack of calcium in the body of the future mother, and an excess amount of the hormone relaxin, and the individual structural features of the woman's body, and possible hereditary or acquired problems of the musculoskeletal system.
With an unexpressed clinical picture of the disease, with an expansion of the pubic fissure up to 10 mm, normal pelvic sizes, a small fetus, childbirth can be carried out through the birth canal, avoiding the use of physical force, such as the Christeller maneuver. With a pronounced stretching of the pubic symphysis, pain syndrome, especially with anatomical narrowing of the pelvis, a large fetus, there is a danger of rupture of the pubic symphysis, and the method of choice in this case is caesarean section. This is due to the fact that during natural delivery, the bones can disperse even more and the woman subsequently will not be able to walk at all.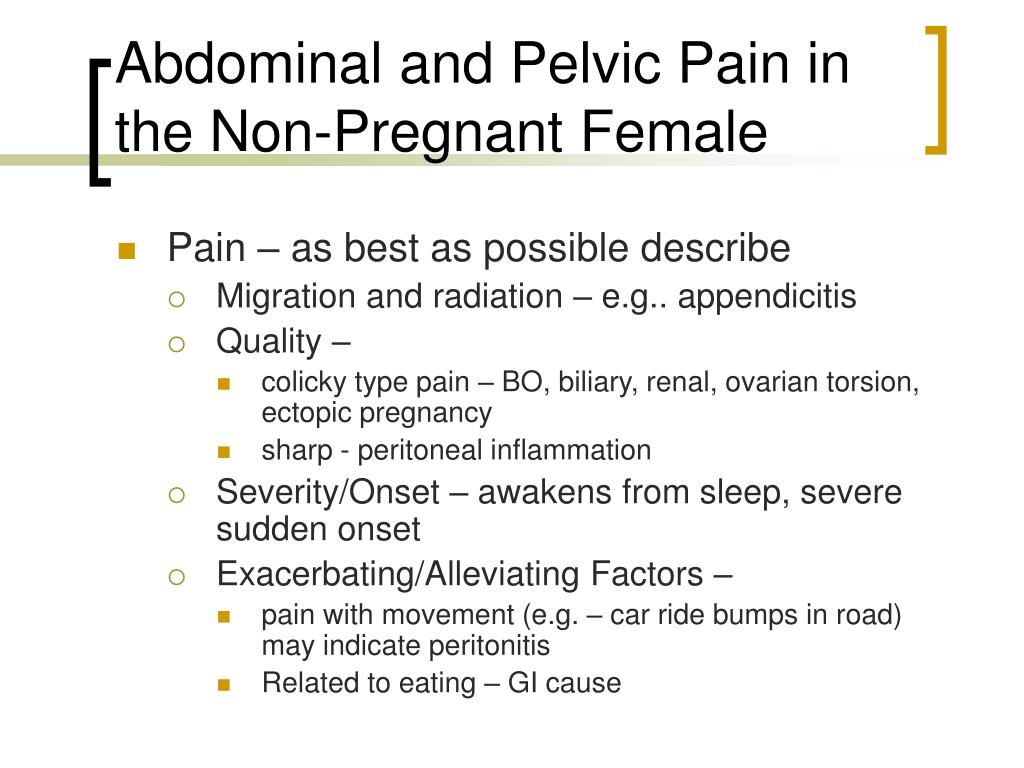
Prevention
The body of a healthy woman is able to independently cope with all the difficulties of the pregnancy period. First of all, the expectant mother should include enough foods containing calcium in her diet, as well as take vitamins for pregnant women.
For the prevention of symphysiopathy, the use of a prenatal bandage is recommended, which supports the abdomen and prevents excessive stretching of the ligaments and muscles. Prophylactic antenatal bandage is usually recommended from 25 weeks of gestation, when the abdomen begins to actively grow.
In order to ensure the plasticity of the ligaments and muscles, as well as the flexibility of the joints, special exercises must be done even during the planning of pregnancy. Yoga gives good results.
Prevention and treatment of low back and pelvic pain during pregnancy
Survey question
We were looking for evidence of the effect of any treatment used to prevent or treat low back pain, pelvic pain, or both during pregnancy.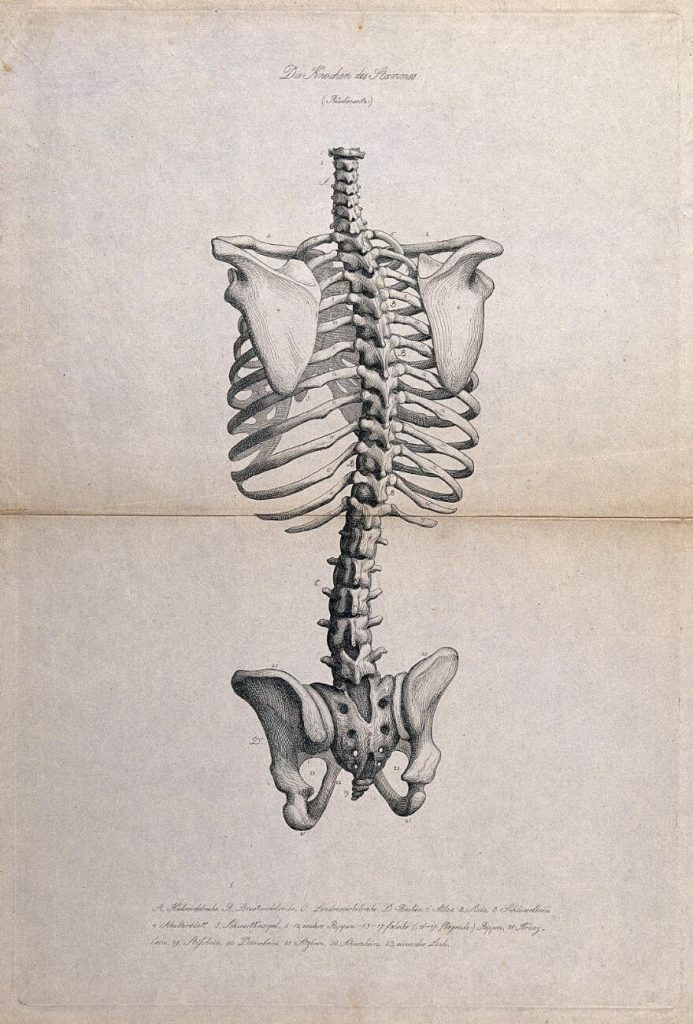 We would also like to know if the treatment reduced disability or sick leave, and if the treatment caused any side effects for pregnant women.
We would also like to know if the treatment reduced disability or sick leave, and if the treatment caused any side effects for pregnant women.
Relevance
Pain in the lumbar region, pelvic region, or both is a common complaint during pregnancy, often progressing as the pregnancy progresses. This pain can interfere with the daily activities, work, and sleep of pregnant women. We wanted to find out which treatment or combination of treatment options would be better than conventional prenatal care for pregnant women with these complaints.
Study profile
This evidence is current to 19 January 2015. We included 34 randomized trials with 5,121 pregnant women aged 16 to 45 in this updated review. The women were between 12 and 38 weeks pregnant. Studies have looked at various treatments for pregnant women with low back pain, pelvic pain, or both types of pain. All treatments were added to routine antenatal care and only compared to routine antenatal care in 23 studies. Symptoms in women in the studies were assessed in many ways, from self-reported pain to sick leave with the results of special tests.
Symptoms in women in the studies were assessed in many ways, from self-reported pain to sick leave with the results of special tests.
Main results
Pain in the lumbar region
When we combined the results of seven studies (645 women) that compared any form of physical exercise with routine prenatal care, exercise (lasting five to 20 weeks), we found that women with low back pain improved and disability rates decreased .
Pelvic pain
Less evidence is available for the treatment of pelvic pain. Two studies showed that women who participated in group exercise and received training in pain management reported no difference in pelvic pain compared to women who received routine prenatal care.
Pain in the lumbar region and pelvis
Results from four studies (1,176 women) when combined showed that an 8 to 12 week exercise program reduced the number of women who complained of low back and pelvic pain.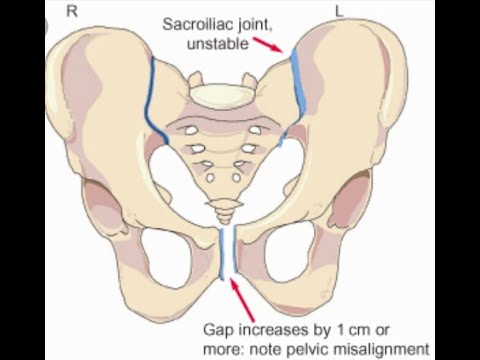 In two studies (1,062 women), ground exercises of various formats also reduced sick leave-related low back and pelvic pain.
In two studies (1,062 women), ground exercises of various formats also reduced sick leave-related low back and pelvic pain.
However, two other studies (374 women) found that group exercise and education was no better in preventing pain, both in the pelvic region and in the lumbar region, compared with conventional prenatal care.
There have been a number of separate studies that have evaluated different treatment options. These results confirm that craniosacral therapy, osteomanipulation therapy, or multimodal intervention (manual therapy, exercise, and education) may be beneficial.
When side effects were reported, there were no long-term side effects in any of the studies.
Quality of evidence and conclusions
There is low-quality evidence that exercise reduces pain and disability in women with low back pain, and moderate-quality evidence for the effect of exercise on reducing sick leave and reducing the number of women with both lower back and pelvic pain complaints.