How to help child with ear infection
What's the Best Ear Infection Treatment for Kids?
Five tips to help relieve ear infection symptoms at home
Five tips to help relieve ear infection symptoms at home
If your little one is cranky, unusually fussy and tugging at his or her ear or is feverish and having difficulty sleeping, chances are it may be due to an ear infection.
Ear infections in children often go away on their own or in some cases with antibiotic treatment. The challenge for many parents is knowing what to do, what to watch for and when to call their pediatrician.
Five out of six children experience an ear infection by the time they are 3 years old, according to the National Institutes of Health. The odds are that your child will have an ear infection before kindergarten.
What causes an ear infection?
Ear infections can be caused by either bacteria or a virus, often following a cold. The common cold can cause the middle ear to become inflamed and fluid to build up behind the eardrum. The Eustachian tube, which connects the ears, nose and throat, can also become swollen.
“Children are more susceptible to ear infections than adults because they have shorter and narrower Eustachian tubes, and it is easier for germs to reach the middle ear and for fluid to get trapped there,” says Kara Hutton, MD, a pediatrician at Scripps Clinic Rancho Bernardo. “Babies and children also have weaker immune systems, so it is more difficult for their bodies to fight an infection.”
The onset of ear infections is often on day three of a cold. Ear infections peak at age 6 months to 2 years, and are a common problem until age 8, according to the American Academy of Pediatrics.
What is the best treatment for ear infection?
Some ear infections require antibiotic treatment, but many can get better without this medicine.
If you suspect your child has an ear infection, your pediatrician can diagnose it and determine the appropriate treatment.
“Common ear infections often do not require antibiotics, except in severe cases or in infants younger than six months,” says Dr. Hutton. “Many ear infections will resolve on their own within a week.”
Hutton. “Many ear infections will resolve on their own within a week.”
For mild cases, your doctor might recommend watchful waiting to give your child’s immune system time to fight off the infection or delayed antibiotic prescribing, which gives you time to see if your child is still sick before filling it.
Five tips for ear infection treatment at home
Even when antibiotics are prescribed, they won’t take effect for 24 to 48 hours. Your child need not suffer needlessly. There are simple, effective ways to reduce your child’s discomfort and pain during an ear infection.
1. Fever and pain medicine: based it on age, consult with doctor
Over-the-counter medications can help reduce pain and fever in your child. Based it on age and weight and consult with your pediatrician if necessary.
Read labels and instructions carefully when giving fever-reducing medications. “It’s very important to follow instructions and give the appropriate dosage according to your child’s weight and age,” says Dr. Hutton.
Hutton.
- For children younger than 6 months, give only acetaminophen, such as Tylenol.
- For children older than 6 months, you may give also give an ibuprofen product, such as Advil, for fever and pain.
- Infants younger than 3 months old who have a fever need immediate medical attention even if they appear well and show no other signs of being ill.
- Do not give aspirin to children because it can cause Reye’s syndrome, a rare but very serious illness that harms the liver and brain, according to the Centers for Disease Control and Prevention (CDC).
2. Place a cold pack or warm compress over your child’s ear
Put a cold wet washcloth on the outer ear for 20 minutes to help with pain until the pain medicine starts to work.
Some children prefer a warm compress to help alleviate pain. Use a warm washcloth and apply until it becomes cool. “Make sure that the compress is only warm, not hot,” says Dr. Hutton.
3. Keep child hydrated
Make sure to keep your child well hydrated. Give lots of cold fluids.
Give lots of cold fluids.
4. Elevate your child’s head
“Keeping your child’s head elevated can ease some of the pressure,” says Dr. Hutton.
If your child is older than 2 and no longer sleeps in a crib, use a pillow, but never use a pillow with an infant. You can keep an infant upright in a car seat to alleviate pressure.
5. Watch for ear discharge
Pus discharge can be normal with an ear infection. Most often, this heals after the ear infection is treated. Wipe the discharge away. Careful not to plug the ear with cotton as retained pus can cause an infection of the lining of the ear canal.
When to call your doctor
Pediatricians recommend calling your doctor if:
- Fever lasts more than two days on antibiotics
- Ear pain becomes severe or crying becomes nonstop
- Ear pain lasts more than three days on antibiotics
- Ear discharge is not better after three days on antibiotics
- Your child becomes worse
Talk with your pediatrician if your child suffers recurrent ear infections, especially if you have a family history of allergies and asthma
Preventing ear infections
While you can’t fend off every germ, there are steps you can take to reduce the risk of an ear infection, including by:
- Breastfeeding your infant to pass along immunities
- Avoiding secondhand smoke
- Washing your hands
- Keeping immunizations up to date
Ear infections | Caring for kids
Middle ear infections are also called otitis media. They are very common, especially in children between 6 months and 3 years of age. They are usually not serious. Although not contagious, the viral illness that caused the infection can be. Most ear infections happen when a child has already had a cold for a few days.
They are very common, especially in children between 6 months and 3 years of age. They are usually not serious. Although not contagious, the viral illness that caused the infection can be. Most ear infections happen when a child has already had a cold for a few days.
What causes an ear infection?
Viruses or bacteria (germs) cause middle ear infections. The eustachian tube connects the middle ear with the back of the throat. Germs travel from the back of the throat when the eustachian tube is swollen from a cold, causing infection in the middle ear.
Who is at higher risk for ear infections?
- Children less than 5 years old, because they have shorter eustachian tubes.
- Children who attend daycare, because they tend to have more colds.
- Children with allergies.
- Children who are exposed to cigarette smoke. Smoke causes inflammation of the eustachian tube, making ear infections more likely.
- Children who were not breastfed.
 Breast milk has antibodies that help fight infections.
Breast milk has antibodies that help fight infections. - Babies who are being bottle-fed, especially if they swallow milk while lying too flat. Milk can enter the eustachian tube and cause inflammation, which increases the risk of an ear infection. Children should be held upright while drinking a bottle. When they are old enough to hold their own bottle well, they should be taught to drink from a regular cup (not a “sippy cup”) and no longer given a bottle.
- Children with cleft palates, as their eustachian tubes are often inflamed.
- Children of First Nations and Inuit descent, though it’s not clear why.
- Children with Down syndrome.
How do I know if my child has an ear infection?
Older children will usually complain of an earache. While younger children might not be able to say they have an earache, they may:
- have an unexplained fever,
- be fussy,
- have trouble sleeping,
- tug or pull at their ears, or
- have trouble hearing quiet sounds.
Some children with an ear infection may also have fluid draining from the ear.
How is an ear infection diagnosed?
Doctors diagnose ear infections by looking at the ear drum (tympanic membrane) with a special light called an otoscope. They look for fluid in the middle ear, at the colour and position of the ear drum, and monitor the pressure in the middle ear. Common viral infections can make the ear drum look red, but antibiotics are not needed.
How is an ear infection treated?
- If a child doesn’t have too much discomfort or a high fever, the doctor will likely wait 24 to 48 hours (1 to 2 days) to see if the ear infection gets better on its own. If the child does not improve or gets worse, contact the doctor again.
- You child’s doctor will prescribe antibiotics if:
- your child is moderately to severely ill with a high fever (more than 39◦C),
- your child has severe pain,
- the condition has not improved for 48 hours, or
- the ear canal has new fluid.

-
For an uncomplicated ear infection, children between 6 months and 2 years usually take an antibiotic for 10 days. Children over 2 years of age will take an antibiotic for 5 days.
-
The doctor might suggest acetaminophen or ibuprofen to reduce the child’s pain. Only give ibuprofen if your child is drinking reasonably well. Do not give ibuprofen to babies under 6 months old without first talking to your doctor.
-
Do not give over-the-counter medications (ones you can buy without a prescription) to babies and children under 6 years without first talking to your doctor. The only exceptions are medications used to treat fever, such as ibuprofen and acetaminophen.
Children usually feel better within 1 day of starting an antibiotic, but make sure to finish it. Your doctor might want to see your child again to be sure the infection has cleared up completely. Fluid can remain in the middle ear without inflammation for a few weeks.
When do children need tubes in their ears?
If your child has frequent ear infections, or if they have trouble hearing because of ongoing fluid in the middle ear, they may need a tube inserted through the eardrum and into the middle ear. The tube helps to keep air pressure normal on both sides of the ear drum and helps fluid drain from the middle ear.
Putting tubes in requires a brief operation by an ear, nose and throat surgeon. Children can usually go home the same day.
When should I call the doctor?
Call your doctor if you think your child has an ear infection AND:
- has other serious medical problems,
- seems ill,
- vomits over and over,
- is younger than 6 months old,
- is older than 6 months old and has had a fever for more than 48 hours,
- has redness and swelling behind the ear,
- is very sleepy,
- is very irritable,
- has a skin rash,
- isn’t hearing well or at all,
- remains in a lot of pain despite at least one dose of acetaminophen or ibuprofen, or
- still has an earache after 2 days of treatment with acetaminophen or ibuprofen.
How can I prevent my child from getting an ear infection?
- Wash your child’s hands and your own often to keep germs away.
- If possible, breastfeed your baby.
- Avoid bottle-feeding your baby when they are lying down. Never put your baby to bed with a bottle.
- Transition your baby from a bottle to a cup by 1 year of age.
- Don’t smoke, and keep your child away from any second-hand smoke. Exposure to smoke can increase the risk of ear infections.
- Ensure your child gets the pneumococcal vaccine (if they are at least 2 months of age, and have not already had this shot).
- Ensure your child gets a flu shot every year.
- If your child has had many ear infections, try reducing the use of pacifiers (soothers). Using a pacifier may increase the risk of repeated ear infections.
More information from the CPS
Additional resources
Reviewed by the following CPS committees
- Community Paediatrics Committee
Last updated: March 2022
Ear inflammation in a child: how to prevent complications
Otitis media is one of the most common diseases in childhood. According to international statistics, 98% of children suffer from ear inflammation at least once, 60% experience the disease twice. What is effective prevention and how otitis is treated, said the otorhinolaryngologist of the Morozov Children's Hospital, Candidate of Medical Sciences, holder of the status of "Moscow Doctor" Alexander Mikhailovich Ivanenko.
According to international statistics, 98% of children suffer from ear inflammation at least once, 60% experience the disease twice. What is effective prevention and how otitis is treated, said the otorhinolaryngologist of the Morozov Children's Hospital, Candidate of Medical Sciences, holder of the status of "Moscow Doctor" Alexander Mikhailovich Ivanenko.
Why does otitis occur?
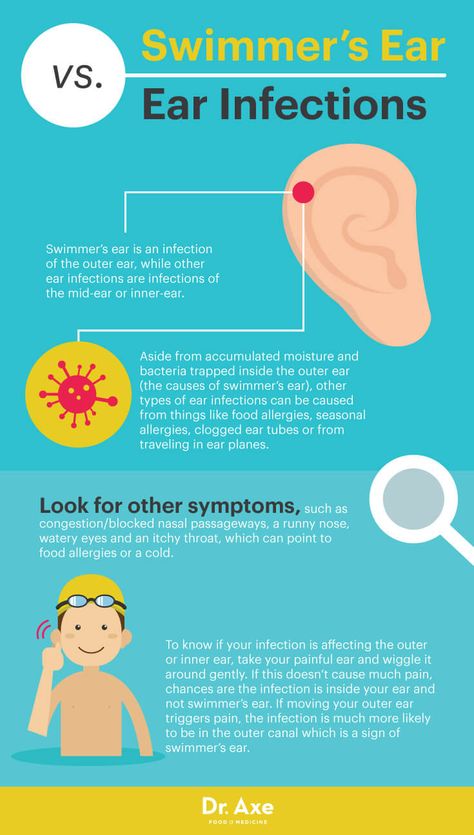
Depending on the location of the inflammatory process, otitis can be external, medial or internal. Otitis externa is caused by microbes and fungi, most often manifested by damage to the skin of the ear canal and boils in the auricle.
Acute otitis media is an acute inflammation of the mucous membrane of the middle ear cavity. It develops against the background of respiratory infections. Ear infection occurs through the auditory tube, when mucus from the nasopharynx enters the middle ear and viruses, bacteria, fungal flora freely penetrate from the nasopharynx through the mouth of the auditory tube into the tympanic cavity.
Due to anatomical features, the smaller the child, the shorter and wider the auditory tube connecting the ear cavity with the nasopharynx. Therefore, in an infant who spends most of his time lying down, and in a younger child who does not know how to clean his nose, mucus can flow at any time. In adolescent children, the auditory tube is a tortuous narrow tube, so the infection from the nasopharynx to the middle ear is less likely to pass.
Adenoid vegetations also contribute to the development of ear inflammation. This is an overgrowth of the nasopharyngeal tonsil, which is the main focus of bacterial infection in the nasopharynx.
How does the disease manifest itself?
The main symptom of otitis media is pain in the ear. Children under one year old, as a rule, refuse to eat, because sucking movements cause pain. Babies often touch their ears, rub them, and cry. You can suspect otitis media by pressing on the tragus of the child's auricle.
The key method for diagnosing otitis media is otoscopy - an examination by a doctor of the external auditory canal and eardrum using a special instrument.
How to treat otitis?
If the inflammatory process is at the initial stage, outpatient treatment is carried out. The therapy is selected by a pediatrician or an otorhinolaryngologist depending on the child's condition. Be sure to use vasoconstrictor drops in the nose.
If medical assistance is not provided in a timely manner, the inflammatory process turns into acute catarrhal otitis media, and then into acute purulent otitis media, characterized by the appearance of purulent discharge from the ear. In some cases, with inadequate outflow of contents or its absence, the child in the hospital undergoes paracentesis - an incision in the eardrum. The intervention is performed under anesthesia. Then medical conservative treatment continues.
Which preventive measures are most effective?
There is an opinion among many parents that otitis media can be prevented by “covering the ears with cotton wool in the street” or “putting a few hats on the child”. Such recommendations will not insure against otitis media.
Such recommendations will not insure against otitis media.
Due to the fact that ear infection occurs through the auditory tube that communicates with the nasopharynx, it is necessary to carefully care for the nasal cavity if the child has a runny nose. Otherwise, mucus flows from the nasopharynx into the middle ear, which leads to an inflammatory process in the ear.
In case of excessive growth of the nasopharyngeal tonsil, its removal is recommended.
Otitis in a child: symptoms, first aid
Children often get ARVI. Most infections pass quickly due to the protective functions of the baby's body, proper care, as well as adequate treatment. However, in some cases SARS occur with complications. Otitis media is one of the most common complications of viral respiratory infections in children. This is facilitated by the features of the anatomical structure in young children - a short, wide and more horizontal auditory tube, which connects the nasopharyngeal cavity and the middle ear, which means that the infection can easily penetrate from the nasopharynx. Otitis can cause infectious diseases such as measles, rubella. Sometimes it happens that frequent profuse regurgitation of the baby becomes the cause of otitis media, while the remnants of food can enter the middle ear through the auditory tube and cause inflammation. The cause of repeated otitis often becomes adenoiditis.
Otitis can cause infectious diseases such as measles, rubella. Sometimes it happens that frequent profuse regurgitation of the baby becomes the cause of otitis media, while the remnants of food can enter the middle ear through the auditory tube and cause inflammation. The cause of repeated otitis often becomes adenoiditis.
What is otitis media
In young children, the onset is usually sudden, with a sharp pain in the ear. Older children may complain of hearing loss. Pain in the ear may be accompanied by a rise in temperature up to 40 0 C. It is more difficult to suspect otitis in infants, because. they can't complain about the pain. Parents may suspect otitis in a baby by the following signs:
- Crying, crying.
- Anxiety, capriciousness, sleep disturbances, refusal of the breast.
- Attempts to finger the ear, rolling the head on the pillow.
- Increased screaming and crying on pressure on the tragus of the ear.
Discharge from the ear is another sign of otitis media. They can be serous or purulent, have an admixture of blood. Discharge from the ears with otitis occurs as a result of perforation (rupture) of the eardrum. Lack of treatment for this condition can lead to a persistent hearing loss in a baby, which once again confirms the need for immediate medical attention at the first sign of otitis media.
Treatment of otitis media and first aid
Treatment of otitis media must be prescribed by a physician. No need to get involved in treatment without an examination by an otorhinolaryngologist. Usually otitis is treated with antibiotics, the course of treatment is 7-10 days. The toilet of the external auditory canal, the restoration of the patency of the Eustachian tube and the normalization of pressure in the tympanic cavity, local and general anti-inflammatory therapy, antibiotic therapy are among the main areas of treatment for otitis media.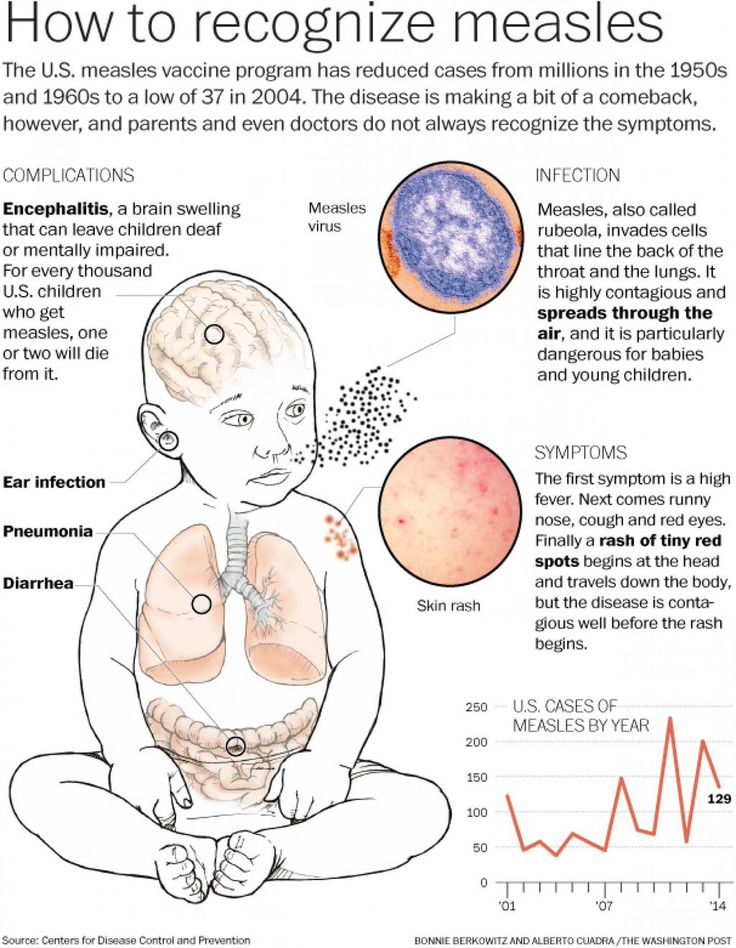 In some cases, the patient is shown paracentesis - a therapeutic puncture of the eardrum. Again, please note that only a doctor can prescribe specific drugs for your child.
In some cases, the patient is shown paracentesis - a therapeutic puncture of the eardrum. Again, please note that only a doctor can prescribe specific drugs for your child.
Help at home:
The use of vasoconstrictor nasal drops is an essential component of the treatment of otitis media. These drugs restore the patency of the auditory tube, which helps to normalize the pressure in the tympanic cavity.
- Put vasoconstrictor drops in your child's nose. Choose a drug that you have already taken.
- For fever and/or severe pain, give your child an age-appropriate antipyretic. Paracetamol and ibuprofen preparations effectively relieve pain in otitis media.
- Dry heat is indicated for otitis media. It is enough to put on a hat or a scarf that covers the ears. Do not use hot compresses or heating pads unless directed by a doctor. Remember! Any thermal procedures are CONTRAINDICATED for suppuration and elevated temperature.
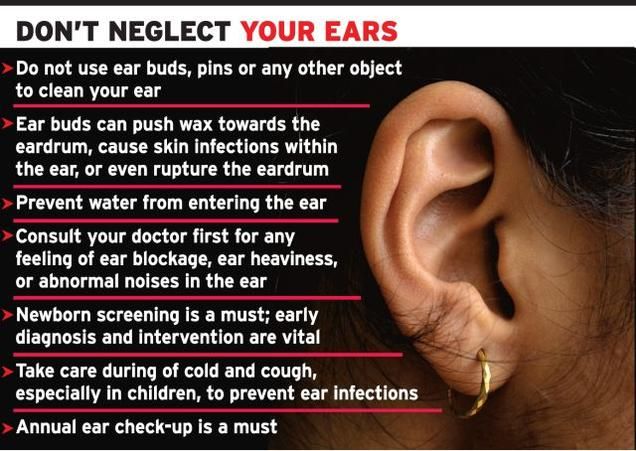
- If purulent or serous fluid is discharged from the ear, remove it with a cotton turunda soaked in 3% hydrogen peroxide solution.
Prophylaxis
It is necessary to treat the nose, nasopharynx and pharynx in time in children. This is especially true for enlarged adenoids. If the child is breathing heavily through his nose, sleeping with his mouth open, snoring, you need to contact an ENT doctor. If the doctor insists on removing the adenoids, consider and agree to this procedure. Treat other viral and bacterial diseases in a timely manner. For infants, the best prevention of otitis media is breastfeeding.
The following tips for caring for a child with SARS will help you reduce your chances of developing otitis media:
- Never force your child to blow his nose. When you blow your nose, mucus enters the Eustachian tubes, which directly contributes to the development of otitis media.
- The Eustachian tube is usually blocked by thick mucus.