Down syndrome blood test results explained
Prenatal Testing for Down Syndrome | Patient Education
Down syndrome is a genetic condition caused by extra genes from the 21st chromosome. It results in certain characteristics, including some degree of cognitive disability and other developmental delays. Common physical traits include an upward slant of the eyes; flattened bridge of the nose; single, deep crease on the palm of the hand; and decreased muscle tone. A child with Down syndrome, however, may not have all these traits.
The incidence of Down syndrome in the United States is about 1 in 1,000 births. There is no association between Down syndrome and culture, ethnic group, socioeconomic status or geographic region.
Age-Related Risks
Generally, the chance of having a Down syndrome birth is related to the mother's age. Under age 25, the odds of having a child with Down syndrome are about 1 in 1,400. At age 35, the odds are about 1 in 350. At age 40, the odds are about 1 in 100.
Causes of Down Syndrome
There are three causes of Down syndrome:
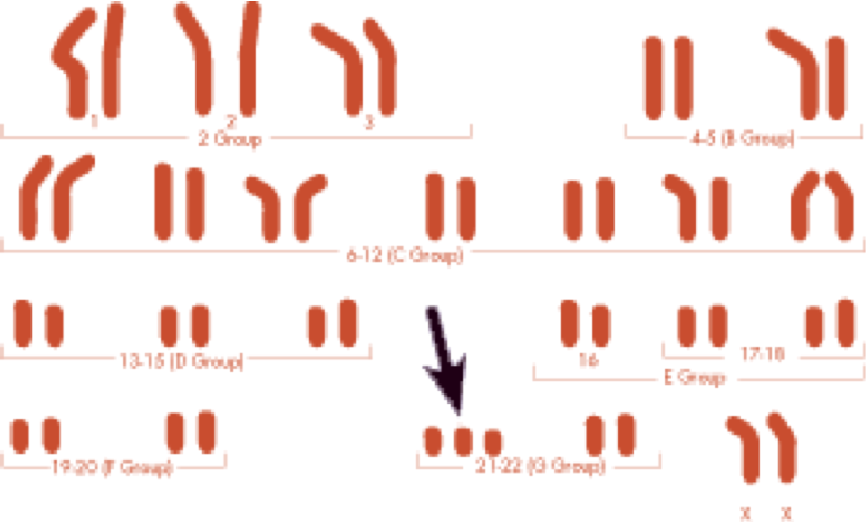
Trisomy 21
An estimated 95 percent of people with Down syndrome have trisomy 21, meaning they have three number 21 chromosomes instead of two. We normally have 23 pairs of chromosomes, each made up of genes. During the formation of the egg and the sperm, a woman's or a man's pair of chromosomes normally split so that only one chromosome is in each egg or sperm. In trisomy 21, the 21st chromosome pair does not split and a double dose goes to the egg or sperm. An estimated 95 to 97 percent of the extra chromosome is of maternal origin.
Translocation
Translocation occurs in about 3 to 4 percent of people with Down syndrome. In this type, an extra part of the 21st chromosome gets stuck onto another chromosome. In about half of these situations, one parent carries the extra 21st chromosome material in a "balanced" or hidden form.
Mosaicism
In mosaicism, the person with Down syndrome has an extra 21st chromosome in some of the cells but not all of them. The other cells have the usual pair of 21st chromosomes. About 1 to 2 percent of people with Down syndrome have this type.
Prenatal Testing
Screening tests can identify women at increased risk of having a baby with Down syndrome.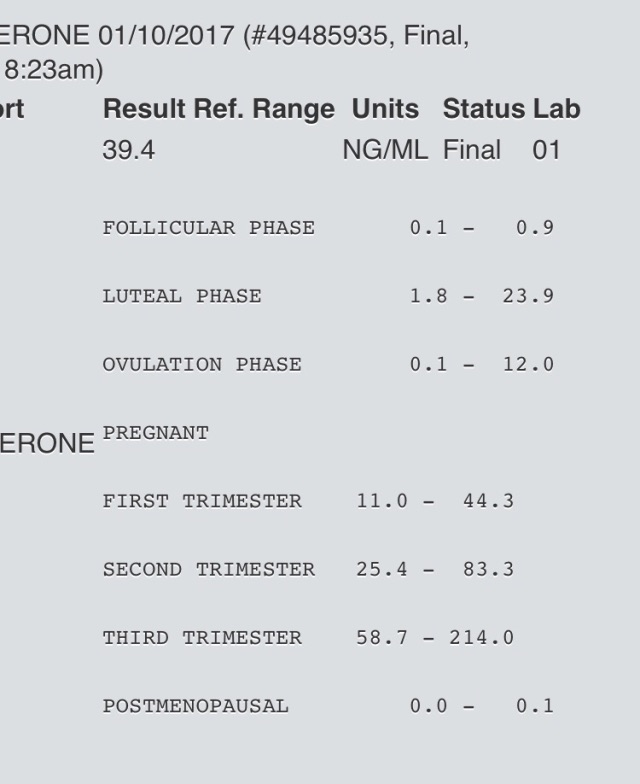 These tests have no risks of miscarriage, but can't determine with certainty whether a fetus is affected. Diagnostic tests, on the other hand, are extremely accurate at identifying certain abnormalities in the fetus, but carry a small — generally less than 1 percent — risk of miscarriage. We offer options for both screening and diagnostic testing.
These tests have no risks of miscarriage, but can't determine with certainty whether a fetus is affected. Diagnostic tests, on the other hand, are extremely accurate at identifying certain abnormalities in the fetus, but carry a small — generally less than 1 percent — risk of miscarriage. We offer options for both screening and diagnostic testing.
Continue reading
Screening Tests
Sequential Integrated Screening — Sequential integrated screening is offered to all pregnant women by the state of California. This non-invasive screening is performed in two steps.
In the first step, which is performed between 10 and 14 weeks of pregnancy, a blood sample is taken from the mother and a nuchal translucency ultrasound is performed to measure the amount of fluid at the back of the baby's neck. If the blood test is scheduled prior to the ultrasound, we can provide the results at the end of the ultrasound appointment. The results of the blood test, the nuchal translucency measurement and the mother's age are used to estimate the risk for Down syndrome and trisomy 18.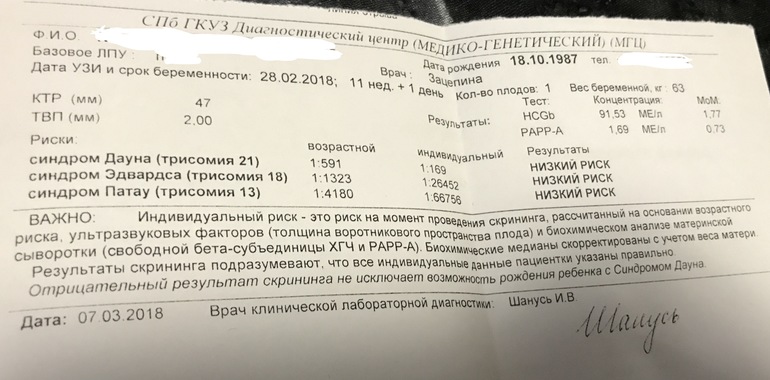
The second step is a maternal blood test between 15 to 20 weeks of pregnancy. When the results of this blood test are combined with the results from the first trimester blood test and nuchal translucency ultrasound, the detection rate for Down syndrome increases. This test also provides a personal risk assessment for having a fetus with trisomy 18, Smith-Lemli-Opitz syndrome, an open neural tube defect or an abdominal wall defect.
Diagnostic Tests
Amniocentesis, chorionic villus sampling (CVS) and ultrasound are the three primary procedures for diagnostic testing.
Amniocentesis — Amniocentesis is used most commonly to identify chromosomal problems such as Down syndrome. When the fetus is known to be at risk, it can detect other genetic diseases like cystic fibrosis, Tay-Sachs disease and sickle cell disease.
An amniocentesis procedure for genetic testing is typically performed between 15 and 20 weeks of pregnancy. Under ultrasound guidance, a needle is inserted through the abdomen to remove a small amount of amniotic fluid.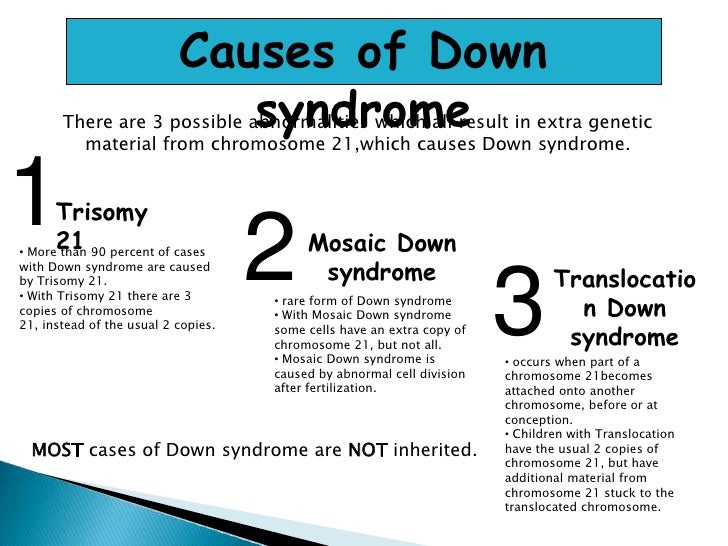 The cells from the fluid are then cultured and a karyotype analysis — an analysis of the chromosomal make-up of the cells — is performed. It takes about two weeks to receive the results of the test.
The cells from the fluid are then cultured and a karyotype analysis — an analysis of the chromosomal make-up of the cells — is performed. It takes about two weeks to receive the results of the test.
Amniocentesis detects most chromosomal disorders, such as Down syndrome, with a high degree of accuracy. Testing for other genetic diseases, such as Tay-Sachs disease, is not routinely performed but can be detected through specialized testing if your fetus is known to be at risk. Testing for neural tube defects, such as spina bifida, also can be performed.
There is a small risk of miscarriage as a result of amniocentesis — about 1 in 100 or less. Miscarriage rates for procedures performed at UCSF Medical Center are less than 1 in 350.
Chorionic Villus Sampling (CVS) — Like amniocentesis, chorionic villus sampling is used most commonly to identify chromosomal problems such as Down syndrome. It can detect other genetic diseases like cystic fibrosis, Tay-Sachs disease and sickle cell disease in at-risk fetuses. The main advantage of CVS over amniocentesis is that it is done much earlier in pregnancy, at 10 to 12 weeks rather than 15 to 20 weeks.
The main advantage of CVS over amniocentesis is that it is done much earlier in pregnancy, at 10 to 12 weeks rather than 15 to 20 weeks.
CVS involves removing a tiny piece of tissue from the placenta. Under ultrasound guidance, the tissue is obtained either with a needle inserted through the abdomen or a catheter inserted through the cervix. The tissue is then cultured and a karyotype analysis of the chromosomal make-up of the cells is performed. It takes about two weeks to receive the results.
The advantage of CVS over amniocentesis is that the test is performed much earlier in pregnancy, so results are typically available by the end of the third month. A disadvantage is that spinal cord defects cannot be detected. Expanded alpha fetoprotein (AFP) blood testing or ultrasound can be performed later in the pregnancy to screen for spinal cord defects.
There is a small risk of miscarriage as a result of CVS — 1 in 100 or less. Miscarriage rates for procedures performed at UCSF Medical Center are less than 1 in 350.
Ultrasound — The primary purpose of ultrasound is to determine the status of a pregnancy — the due date, size of the fetus and if the mother is carrying multiples. Ultrasound also can provide some information about possible birth defects in a fetus. All patients at UCSF Medical Center undergo a comprehensive ultrasound examination before any invasive tests are performed. Results of the ultrasound are explained at the time of the visit.
In some patients, an ultrasound raises concern of a possible abnormality in the fetus. We have extensive experience in performing and interpreting ultrasounds in pregnancy.
If You Receive a Positive Result
If you receive positive results on a screening test, we recommend that you discuss this with your doctor and a genetic counselor. Options for further diagnostic testing will be explained. The decision as to whether to have invasive genetic testing is up to you.
If a diagnostic test finds a genetic abnormality, the significance of such results should be discussed with experts familiar with the condition, including a medical geneticist and a genetic counselor, as well as your own doctor.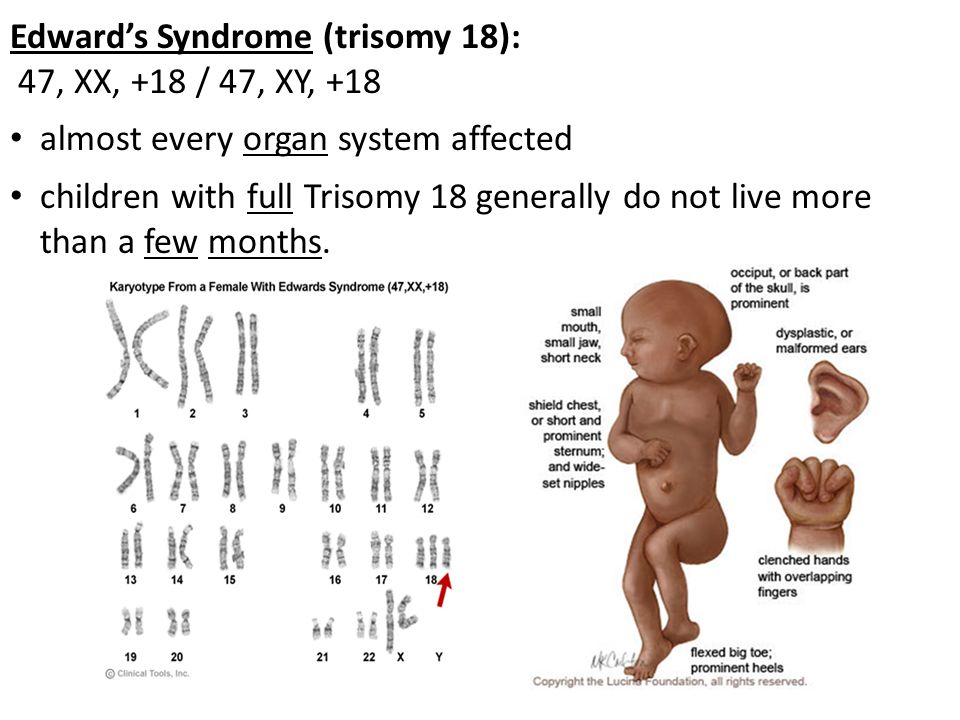
Screening for Down's syndrome, Edwards' syndrome and Patau's syndrome
You will be offered a screening test for Down's syndrome, Edwards' syndrome and Patau's syndrome between 10 and 14 weeks of pregnancy. This is to assess your chances of having a baby with one of these conditions.
Down's syndrome is also called trisomy 21 or T21. Edwards' syndrome is also called trisomy 18 or T18, and Patau's syndrome is also called trisomy 13 or T13.
If a screening test shows that you have a higher chance of having a baby with Down's syndrome, Edwards' syndrome or Patau's syndrome, you'll be offered further tests to find out for certain if your baby has the condition.
What are Down's syndrome, Edwards' syndrome and Patau's syndrome?
Down's syndrome
Down's syndrome causes some level of learning disability.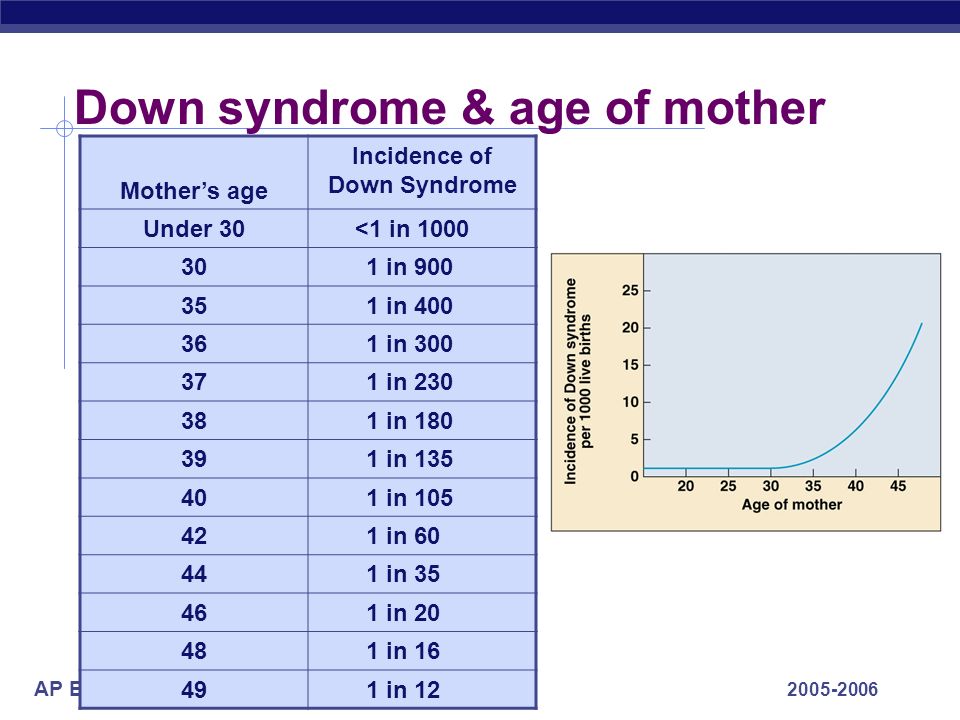
People with Down's syndrome may be more likely to have other health conditions, such as heart conditions, and problems with the digestive system, hearing and vision. Sometimes these can be serious, but many can be treated.
Read more about Down's syndrome
Edwards' syndrome and Patau's syndrome
Sadly, most babies with Edwards' syndrome or Patau's syndrome will die before or shortly after birth. Some babies may survive to adulthood, but this is rare.
All babies born with Edwards' syndrome or Patau's syndrome will have a wide range of problems, which can be very serious. These may include major complications affecting their brain.
Read more about Edwards' syndrome and Patau's syndrome.
What does screening for Down's syndrome, Edwards' syndrome and Patau's syndrome involve?
Combined test
A screening test for Down's syndrome, Edwards' syndrome and Patau's syndrome is available between weeks 10 and 14 of pregnancy.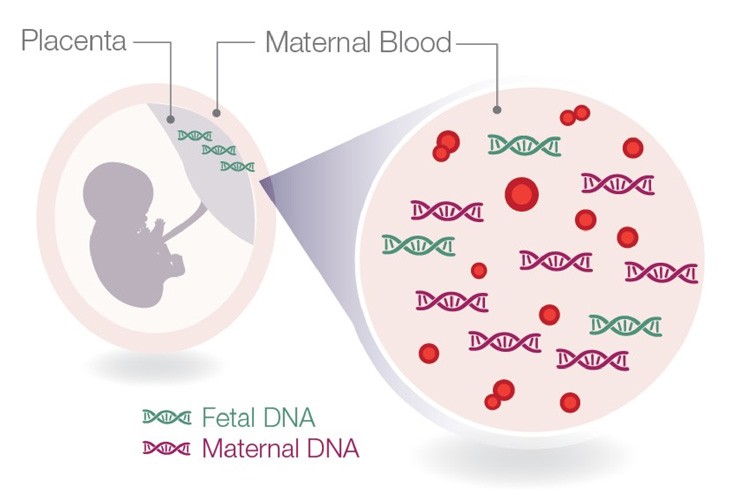 It's called the combined test because it combines an ultrasound scan with a blood test. The blood test can be carried out at the same time as the 12-week scan.
It's called the combined test because it combines an ultrasound scan with a blood test. The blood test can be carried out at the same time as the 12-week scan.
If you choose to have the test, you will have a blood sample taken. At the scan, the fluid at the back of the baby's neck is measured to determine the "nuchal translucency". Your age and the information from these 2 tests are used to work out the chance of the baby having Down's syndrome, Edwards' syndrome or Patau's syndrome.
Obtaining a nuchal translucency measurement depends on the position of the baby and is not always possible. If this is the case, you will be offered a different blood screening test, called the quadruple test, when you're 14 to 20 weeks pregnant.
Quadruple blood screening test
If it was not possible to obtain a nuchal translucency measurement, or you're more than 14 weeks into your pregnancy, you'll be offered a test called the quadruple blood screening test between 14 and 20 weeks of pregnancy. This only screens for Down's syndrome and is not as accurate as the combined test.
This only screens for Down's syndrome and is not as accurate as the combined test.
20-week screening scan
For Edwards' syndrome and Patau's syndrome, if you are too far into your pregnancy to have the combined test, you'll be offered a 20-week screening scan. This looks for physical conditions, including Edwards' syndrome and Patau's syndrome.
Can this screening test harm me or my baby?
The screening test cannot harm you or the baby, but it's important to consider carefully whether to have this test.
It cannot tell you for certain whether the baby does or does not have Down's syndrome, Edward's syndrome or Patau's syndrome, but it can provide information that may lead to further important decisions. For example, you may be offered diagnostic tests that can tell you for certain whether the baby has these conditions, but these tests have a risk of miscarriage.
Do I need to have screening for Down's syndrome, Edwards' syndrome and Patau's syndrome?
You do not need to have this screening test – it's your choice. Some people want to find out the chance of their baby having these conditions while others do not.
You can choose to have screening for:
- all 3 conditions
- Down's syndrome only
- Edwards' syndrome and Patau's syndrome only
- none of the conditions
What if I decide not to have this test?
If you choose not to have the screening test for Down's syndrome, Edwards' syndrome or Patau's syndrome, you can still choose to have other tests, such as a 12-week scan.
If you choose not to have the screening test for these conditions, it's important to understand that if you have a scan at any point during your pregnancy, it could pick up physical conditions.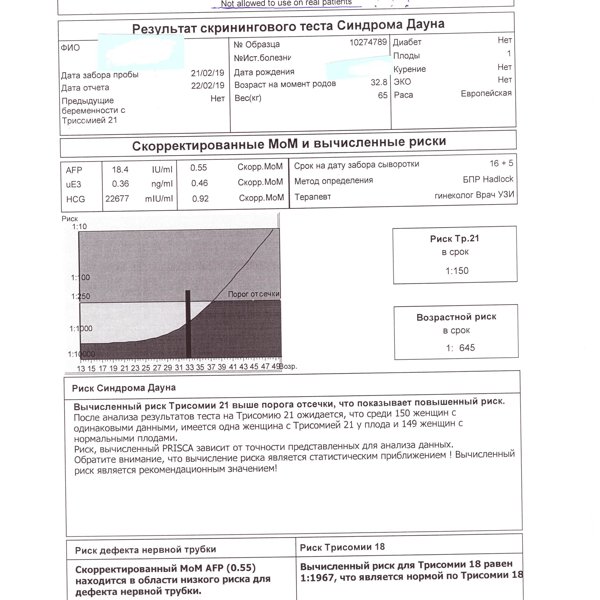
The person scanning you will always tell you if any conditions are found.
Getting your results
The screening test will not tell you whether your baby does or does not have Down's, Edwards' or Patau's syndromes – it will tell you if you have a higher or lower chance of having a baby with one of these conditions.
If you have screening for all 3 conditions, you will receive 2 results: 1 for your chance of having a baby with Down's syndrome, and 1 for your joint chance of having a baby with Edwards' syndrome or Patau's syndrome.
If your screening test returns a lower-chance result, you should be told within 2 weeks. If it shows a higher chance, you should be told within 3 working days of the result being available.
This may take a little longer if your test is sent to another hospital. It may be worth asking the midwife what happens in your area and when you can expect to get your results.
You will be offered an appointment to discuss the test results and the options you have.
The charity Antenatal Results and Choices (ARC) offers lots of information about screening results and your options if you get a higher-chance result.
Possible results
Lower-chance result
If the screening test shows that the chance of having a baby with Down's syndrome, Edwards' syndrome and Patau's syndrome is lower than 1 in 150, this is a lower-chance result. More than 95 out of 100 screening test results will be lower chance.
A lower-chance result does not mean there's no chance at all of the baby having Down's syndrome, Edwards' syndrome or Patau's syndrome.
Higher-chance result
If the screening test shows that the chance of the baby having Down's syndrome, Edwards' syndrome or Patau's syndrome is higher than 1 in 150 – that is, anywhere between 1 in 2 and 1 in 150 – this is called a higher-chance result.
Fewer than 1 in 20 results will be higher chance. This means that out of 100 pregnancies screened for Down's syndrome, Edwards' syndrome and Patau's syndrome, fewer than 5 will have a higher-chance result.
A higher-chance result does not mean the baby definitely has Down's syndrome, Edwards' syndrome or Patau's syndrome.
Will I need further tests?
If you have a lower-chance result, you will not be offered a further test.
If you have a higher-chance result, you can decide to:
- not have any further testing
- have a second screening test called non-invasive prenatal testing (NIPT) – this is a blood test, which can give you a more accurate screening result and help you to decide whether to have a diagnostic test or not
- have a diagnostic test, such as amniocentesis or chorionic villus sampling (CVS) straight away – this will tell you for certain whether or not your baby has Down's syndrome, Edwards' syndrome or Patau's syndrome, but in rare cases can cause a miscarriage
You can decide to have NIPT for:
- all 3 conditions
- Down's syndrome only
- Edwards' syndrome and Patau's syndrome only
You can also decide to have a diagnostic test after NIPT.
NIPT is completely safe and will not harm your baby.
Discuss with your healthcare professional which tests are right for you.
Whatever results you get from any of the screening or diagnostic tests, you will get care and support to help you to decide what to do next.
If you find out your unborn baby has Down's syndrome, Edwards' syndrome or Patau's syndrome
If you find out your baby has Down's syndrome, Edwards' syndrome or Patau's syndrome a specialist doctor (obstetrician) or midwife will talk to you about your options .
You can read more about what happens if antenatal screening tests find something.
You may decide to continue with the pregnancy and prepare for your child with the condition.
Or you may decide that you do not want to continue with the pregnancy and have a termination.
If you are faced with this choice, you will get support from health professionals to help you make your decision.
For more information see GOV.UK: Screening tests for you and your baby
The charity Antenatal Results and Choices (ARC) runs a helpline from Monday to Friday, 10am to 5.30pm on 020 7713 7486.
The Down's Syndrome Association also has useful information on screening.
The charity SOFT UK offers information and support through diagnosis, bereavement, pregnancy decisions and caring for all UK families affected by Edwards' syndrome (T18) or Patau's syndrome (T13).
Interpretation of the results of 1 pregnancy screening
Combined prenatal screening is carried out at 11-14 weeks of gestation with an embryo size of at least 45 mm and not more than 84 mm. This is a comprehensive examination of the fetus to assess the parameters of its development.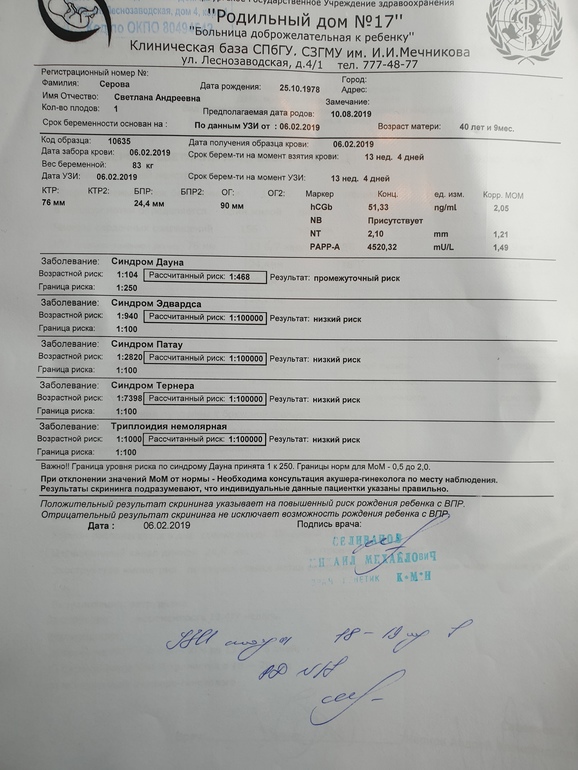 Its main task is the early detection of fetal malformations, the prevention of childhood disability, and the reduction of infant and child mortality.
Its main task is the early detection of fetal malformations, the prevention of childhood disability, and the reduction of infant and child mortality.
The first screening consists of an instrumental part - an ultrasound scan and a laboratory one - a blood test to determine the concentration of chorionic gonadotropin (βhCG) and pregnancy-associated protein A (PAPP-A). The cumulative results of these indicators allow you to plan the tactics of pregnancy management.
Why is the examination carried out at 11-14 weeks
The first trimester is the period of formation of all organs and structures of the body. By the end of the first trimester, the embryonic period ends and the fetal period of fetal development begins. It is in the period from 11 weeks 1 day to 13 weeks 6 days of pregnancy that echographic markers of chromosomal abnormalities are best visualized.
Who needs to be examined
According to the results of the study, it is possible to judge the risk of giving birth to children with chromosomal diseases and congenital malformations, therefore it is recommended to carefully consider the issue and examine all pregnant women.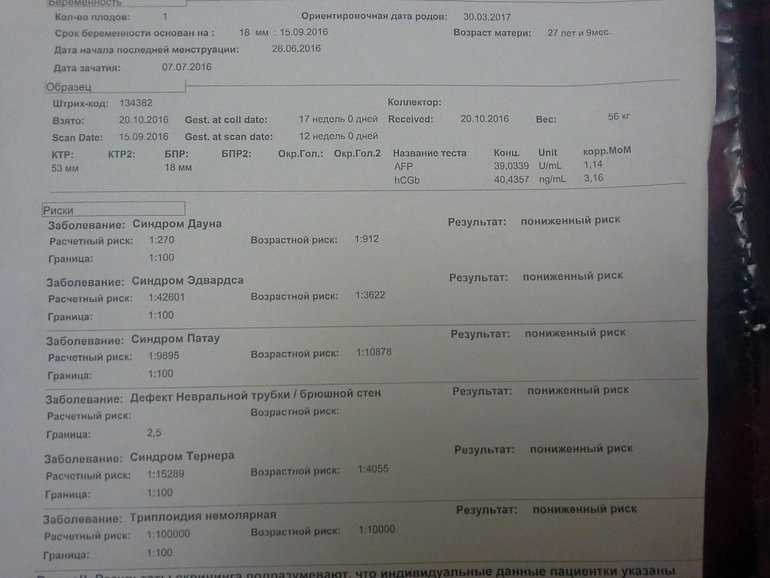 Indications for mandatory prenatal screening of the first trimester are:
Indications for mandatory prenatal screening of the first trimester are:
- Women with a history of spontaneous abortions, ectopic and missed pregnancies, premature birth, stillbirth, birth of a child with developmental anomalies.
- Hereditary diseases in the family of the mother or father of the child
- First trimester illness treated with antibiotics or drugs contraindicated during pregnancy.
- Marriage between relatives.
- The woman is over 35 years of age.
- Presence of occupational hazards
How to prepare
Preparation for the first screening is expressed in a sparing diet. Nutritional errors can affect the general condition of a woman and reduce the accuracy of the results. One week before the examination:
- Salty, spicy, fatty, fried foods should be excluded from the diet.
- Do not eat allergenic foods.
- Avoid carbonated drinks.
One day before screening:
- Do not eat chocolate, seafood, fatty meat, flour, limit sweets.
- If the study is scheduled for the morning, eat a light dinner no later than 20:00 hours.
It is advisable to observe moderate physical activity, if there are no contraindications for this. Walking and proper rest are also important.
Survey
A blood test and ultrasound are performed on the same day to avoid errors due to time differences.
- Ultrasound screening is performed first, as its results allow you to determine the exact gestational age, which affects the normative values of hormone levels. The study is carried out both transabdominally and transvaginally. The procedure is painless, safe for women and children, has no contraindications.
- Blood is donated from a vein on an empty stomach or 4 hours after a meal. The material is taken on the day of the ultrasound. The study determines the concentration of hormones and compares with standard indicators.
Only by deciphering the results of ultrasound and hormone analysis, a conclusion is made about possible risks.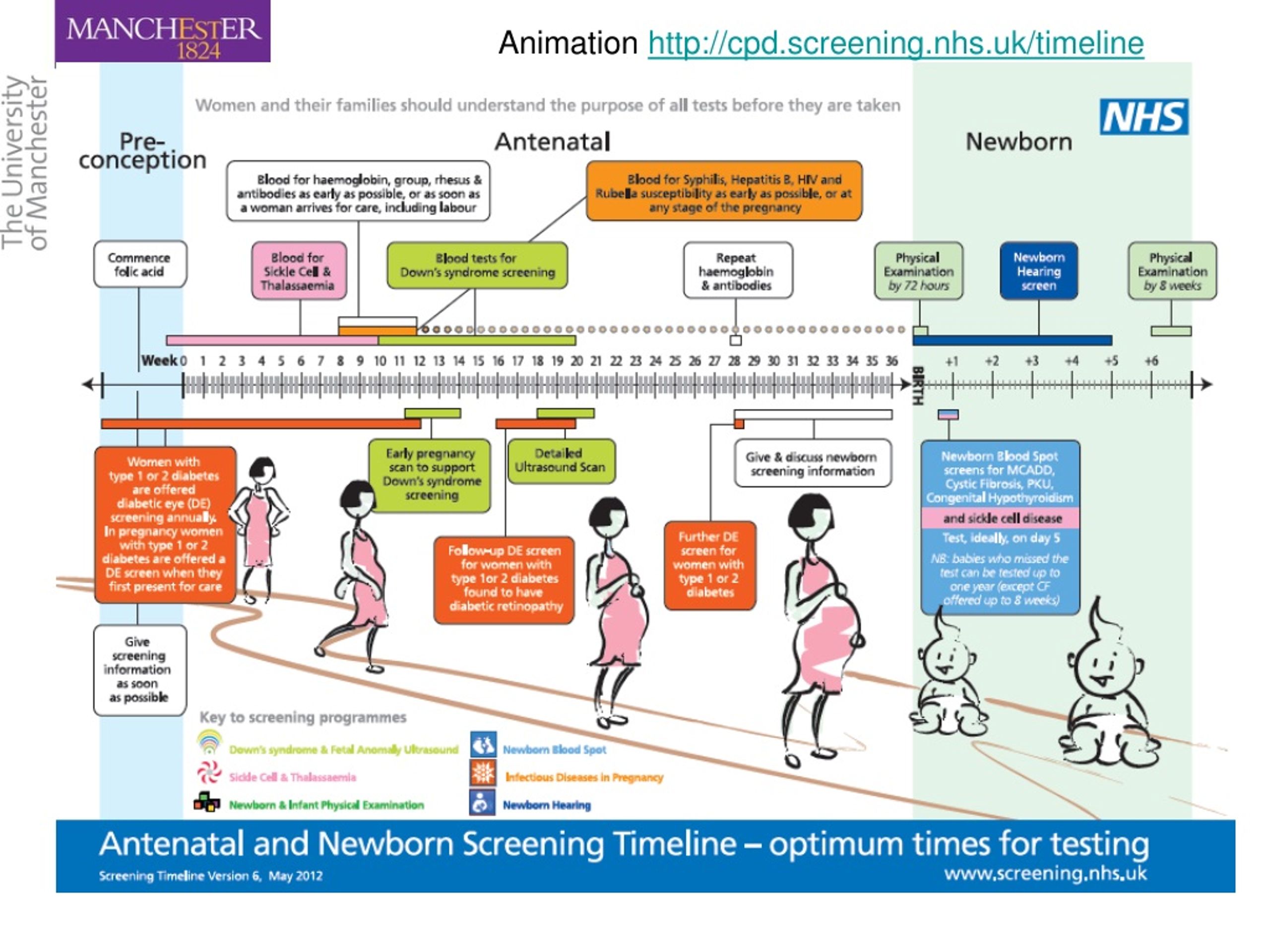
What ultrasound shows
At screening during pregnancy, fetometry of the fetus is performed - determination of the size of body parts and all anatomical structures are evaluated.
The results obtained are compared with a statistical table, which indicates the percentile of falling into the sample of standard values. With indicators less than 5 and more than 95 additional examinations are scheduled.
During an ultrasound examination in the 1st trimester, the following parameters are evaluated: the bones of the cranial vault and the brain, the spine, the anterior abdominal wall, the limbs of the fetus, the structures of the face, the organs of the chest and abdominal cavity, as well as the main echographic markers of chromosomal abnormalities.
Collar space thickness (NTP)
The area between the inner surface of the skin of the fetus and the outer surface of the soft tissues covering the cervical spine. TVP is considered the most important marker of chromosomal abnormalities.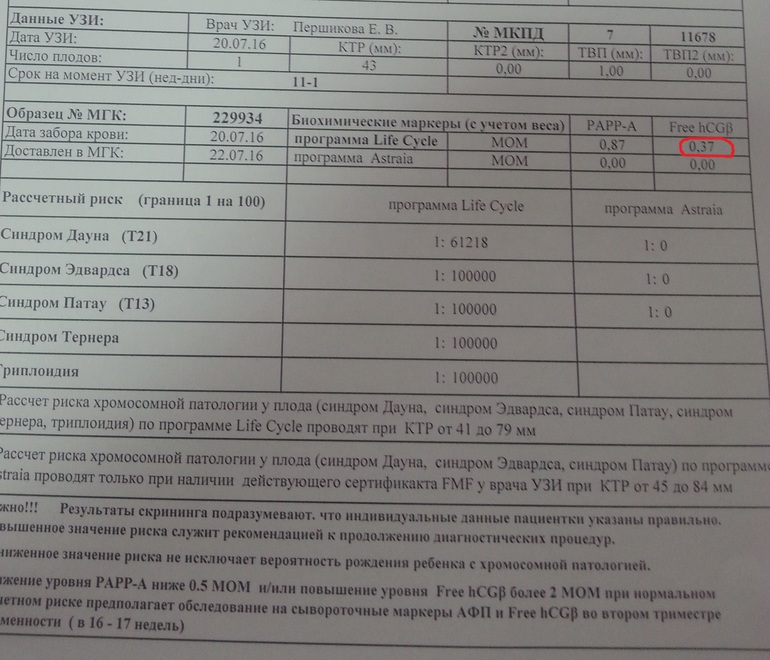
This space begins to decrease after 13 weeks, so it can only be assessed at the first screening.
| Gestational age | Collar thickness in mm | |||
| Percentile 5 | 50 percentile | 95 percentile | ||
| 11 weeks | 0.8 | 1.6 | 2.4 | |
| 12 weeks | 0.7 | 1.6 | 2.5 | |
| 13 weeks | 0. 7 7 | 1.7 | 2.7 | |
The discrepancy between the results and the normative values indicates an increased risk of developing chromosomal pathologies. Depending on the formed set of chromosomes, it can be Down syndrome, Patau, Edwards, Shereshevsky-Turner. To clarify the diagnosis in this case, a biopsy of the chorion or placenta, an analysis of cord blood, and amniotic fluid may be prescribed. Only after additional research can an accurate diagnosis be made.
Coccyx-parietal size (KTR)
Shows the distance between the coccygeal and parietal bones. According to this parameter, the exact gestational age is determined on ultrasound, and the ratio of the mass of the fetus to its CTE is also established.
A slight deviation from the norm indicates the features of the physique and is not a cause for concern.
| Gestational age | Coccyx-parietal size in mm | |||
| Percentile 5 | 50 percentile | 95 percentile | ||
| 11 weeks | 34 | 42 | fifty | |
| 12 weeks | 42 | 51 | 59 | |
| 13 weeks | 51 | 63 | 75 | |
If screening during pregnancy showed results that exceed the norm, this indicates that the fetus is quite large.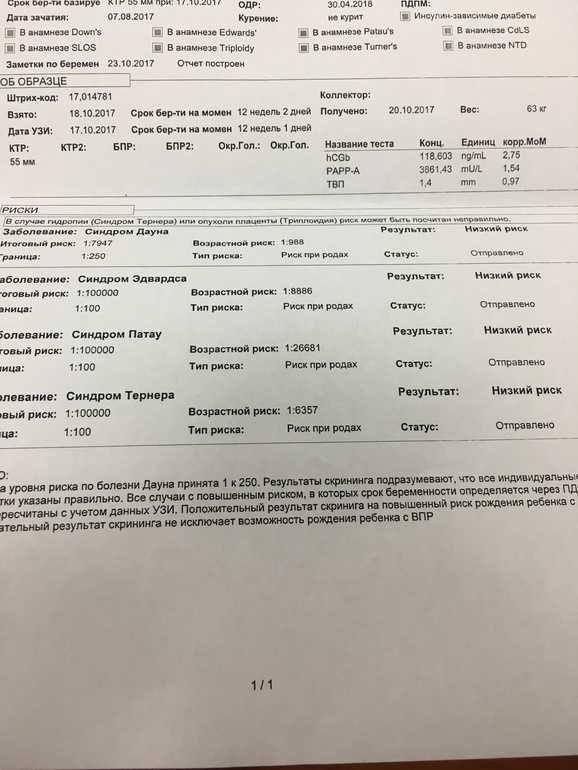 The indicator says much less either about an incorrectly determined gestational age (in this case, a re-examination is carried out after 1-1.5 weeks), or about a slowdown in development due to intrauterine death, impaired hormonal levels or an infectious disease of the mother, genetic abnormalities.
The indicator says much less either about an incorrectly determined gestational age (in this case, a re-examination is carried out after 1-1.5 weeks), or about a slowdown in development due to intrauterine death, impaired hormonal levels or an infectious disease of the mother, genetic abnormalities.
Skull bones and brain
Already from the 11th week, ultrasound examination can detect defects in the bones of the skull, which indicates severe fetal malformations that are incompatible with life. The evaluation of the brain is based on the study of the so-called "butterfly" - the choroid plexus of the lateral ventricles. A clear visualization and its symmetry indicates the normal development of the brain.
| Gestational age | BPR, LZR in mm | |||
| Percentile 5 | 50 percentile | 95 percentile | ||
| 11 weeks | 13.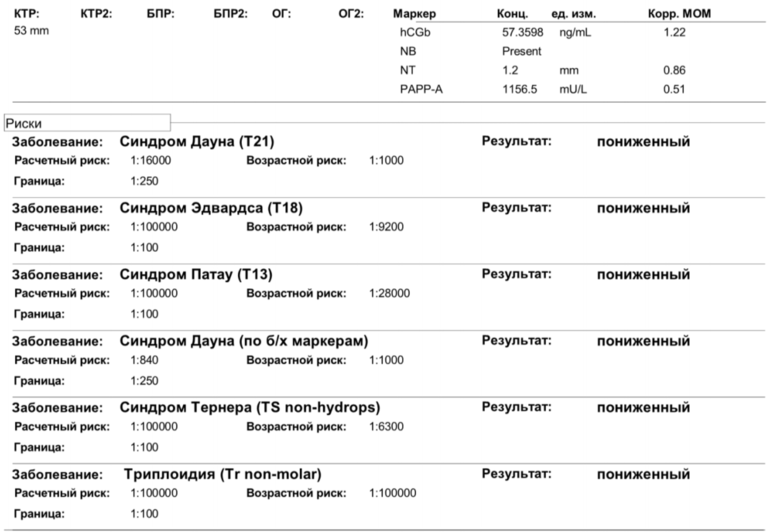 19 19 | 17.21 | 21.23 | |
| 12 weeks | 19.22 | 21.24 | 24.26 | |
| 13 weeks | 20.26 | 24.29 | 28.32 | |
Nasal bone
By the end of the trimester, it should be formed, clearly visualized.
| Gestational age | Nasal bone in mm | |||
| Percentile 5 | 50 percentile | 95 percentile | ||
| 11 weeks | visualized, not measured | visualized, not measured | visualized, not measured | |
| 12 weeks | 2 | 3.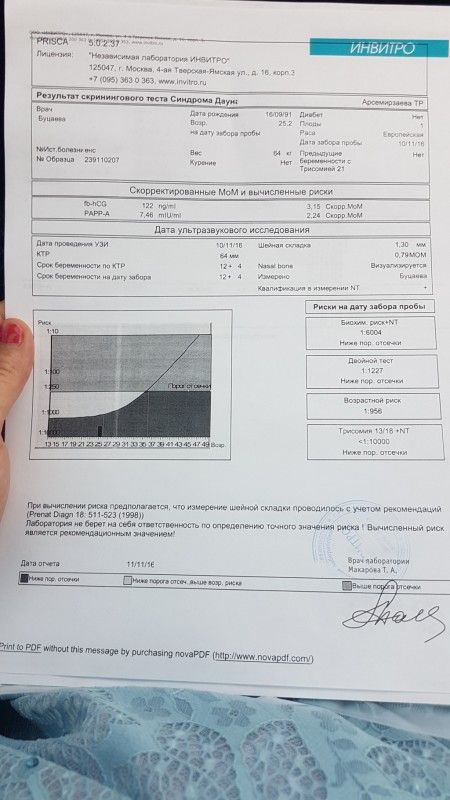 1 1 | 4.2 | |
| 13 weeks | 2 | 3.1 | 4.2 | |
The pathology of the nasal bone is its absence, hypoplasia (very small size) and a change in its echogenicity.
The diameter of the chest, the circumference of the head and abdomen, the length of the femur also make it possible to judge the proportionality of development.
Heart condition
When examining the heart, its location is assessed, the presence of four chambers of the heart is established - two atria and two ventricles, and their symmetry is assessed. The heart rate is measured.
| Gestational age | Heart rate in beats per minute | |||
| Percentile 5 | 50 percentile | 95 percentile | ||
| 11 weeks | 153 | 165 | 177 | |
| 12 weeks | 150 | 162 | 174 | |
| 13 weeks | 147 | 159 | 171 | |
The venous duct (VP) is a direct communication between the umbilical vein and the central venous system.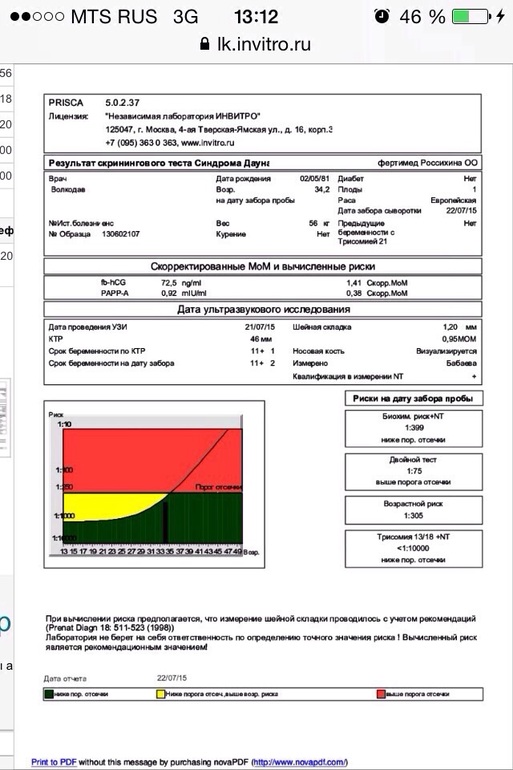 In a normally developing pregnancy, the blood flow in the EP is a three-phase curve. The appearance of reverse blood flow may indicate the presence of fetal pathology.
In a normally developing pregnancy, the blood flow in the EP is a three-phase curve. The appearance of reverse blood flow may indicate the presence of fetal pathology.
What a blood test shows
Ultrasound results are compared with maternal plasma pregnancy-associated protein A (PAPP-A) and human chorionic gonadotropin (hCG). The values are given in the table:
| Gestational age | hCG in ng/ml | PAPP-A in mU/l |
| 11 weeks | 17.4 - 130.4 | 0.46 - 3.73 |
| 12 weeks | 13.4 - 128.5 | 0.79 - 4.76 |
| 13 weeks | 14.2 - 114.7 | 1. 03 - 6.01 03 - 6.01 |
Differences from the reference values \u200b\u200bmay indicate pathologies of the mother or fetus.
| Deviation | hCG | PAPP-A |
| Above normal |
|
|
| Below normal |
|
|
Survey interpretation
The first study is evaluated only by the totality of all indicators. A single parameter cannot be the basis for an accurate conclusion. The protocol records ultrasound data, hormone analysis, the risks of probable diseases and the complex median coefficient MoM. It indicates the cumulative deviation of the obtained results from the average values. The coefficient must be in the range from 0.5 to 2.5. It is calculated by specialized programs.
What can affect the result
- Incorrect preparation, peculiarities of the woman's condition.
- Obsolete equipment with poor measurement accuracy and insufficient resolution.
- Qualification of the doctor of the ultrasound room, errors in decoding.
- Correctness of MoM calculation algorithms.
Modern diagnostic equipment makes it possible to evaluate more than 15 fetal parameters, build its volumetric reconstruction for examining organs in the early stages of development, and calculate possible risks with high accuracy.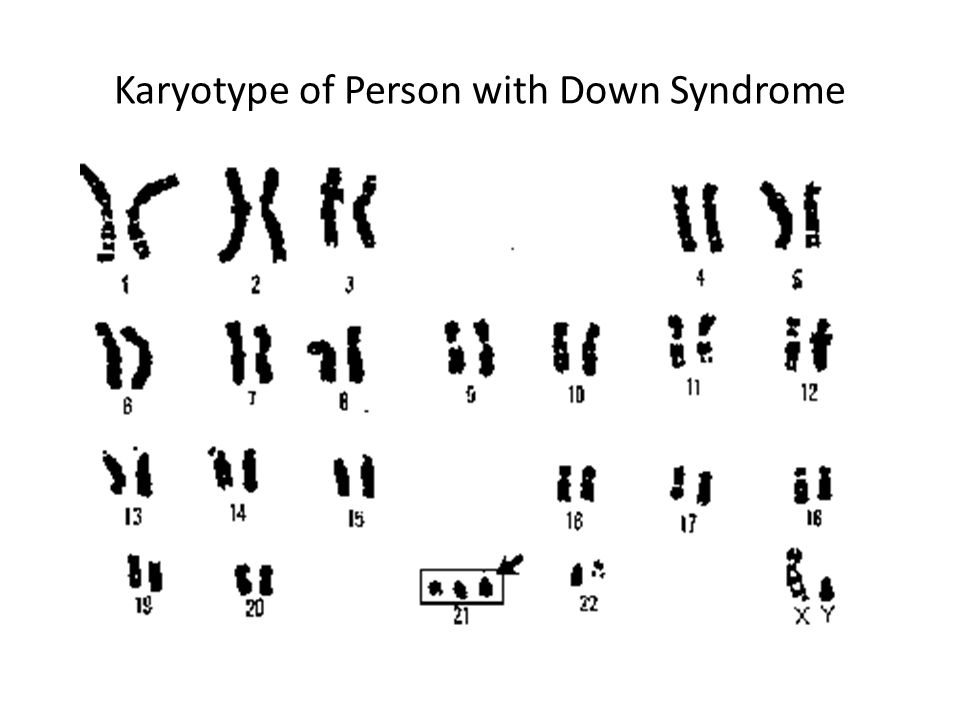 Contact well-equipped clinics and trust specialists with proven qualifications.
Contact well-equipped clinics and trust specialists with proven qualifications.
Reliability of 1st trimester screening - an article from the Lek-Diagnostic clinic network
1st trimester screening: what is it?
Screening of the 1st trimester is a comprehensive examination aimed at assessing the rate of intrauterine development of the baby by comparing the indicators of a specific gestational age. At this stage, the probability of congenital pathological abnormalities, including Down syndrome, is determined. Screening of the 1st trimester includes two procedures: a biochemical blood test and an ultrasound examination.
Biochemical blood test
Using biochemistry, you can determine the level of hormones that affect the development of genetic abnormalities:
1. B-hCG - is produced from the beginning of pregnancy, from the 9th week the indicator begins to decline. The norm is 50 thousand-55 thousand. mIU/ml.
2. PAPP-A is an A-plasma protein.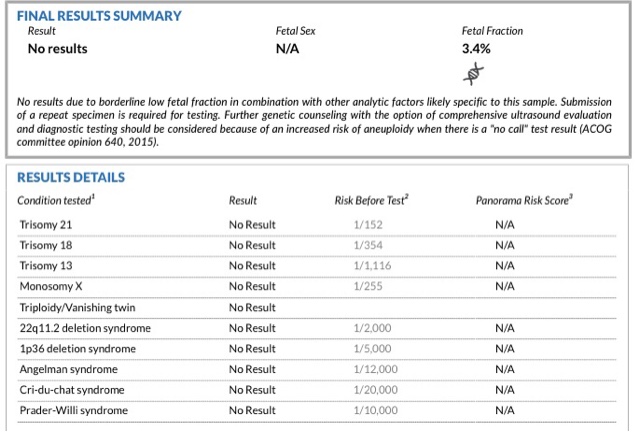 A natural indicator is 0.79-6.00 mU / l. during the 1st trimester screening period.
A natural indicator is 0.79-6.00 mU / l. during the 1st trimester screening period.
The procedure is carried out in the period from 11 to 13 weeks. A woman donates venous blood in the morning on an empty stomach. Among the contraindications: signs of multiple pregnancy, weight problems, diabetes. Biochemistry is mandatory for women after 35 years of age, with genetic anomalies in the family, with miscarriages or infectious diseases in the past.
Ultrasound examination
Ultrasound is a safe and informative diagnostic method. It allows you to localize the location of the fetus, its physique, compliance with the size of the norm, and also to identify how correctly the limbs of the unborn child are located.
According to the results of the first ultrasound, the doctor:
Determines the date of conception, and also corrects the gestational age;
Establishes or refutes the fact of the presence of congenital pathologies;
Estimates the likelihood of pathological pregnancy.
Ultrasound is performed in two ways: transvaginally (the sensor is inserted into the vagina) or abdominally (the sensor is driven along the abdomen). It is optimal to perform the procedure at the 12th week of pregnancy.
Why are parents afraid of Down syndrome?
Down syndrome is a common genetic syndrome. Normally, a set of chromosomes in humans contains 23 pairs. With a genetic anomaly, a mutation of chromosome 21 leads to trisomy - the presence of an extra 21 chromosome. The pathology was first diagnosed in 1866 by John Down. At the moment, the probability of developing the syndrome is 1 in 700 children.
Why can't Down syndrome be seen on ultrasound?
It is impossible to make an accurate diagnosis of Down syndrome using ultrasound. Based on the results of the procedure, the specialist evaluates the condition of the fetus according to the following parameters:
1. Thickened neck fold. Normally, it is 1.6-1.7 mm. A thickness of 3 mm indicates the likelihood of chromosomal abnormalities.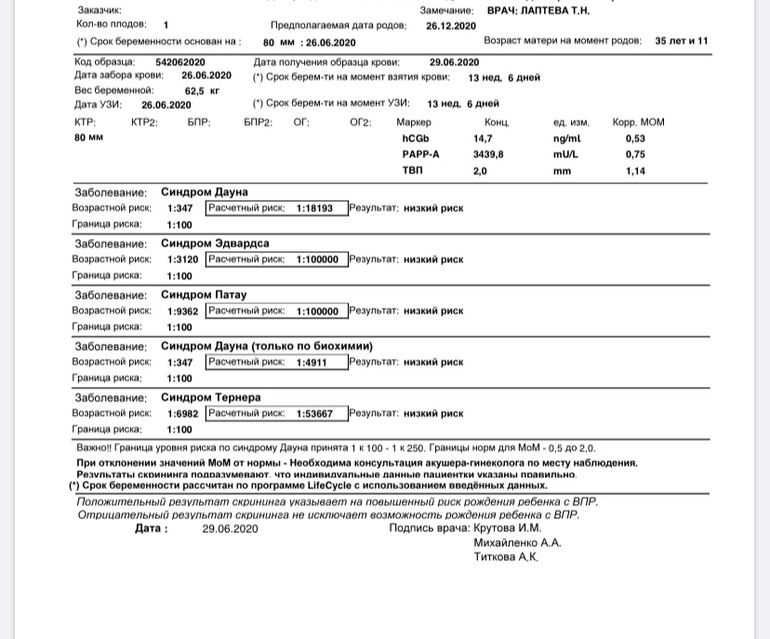
2. KTR (fetal length). The normal figure varies from 43 to 65 mm (for a period of 12-13 weeks).
At the next stage, calculations are carried out, the risk of genetic abnormalities is examined. A probability higher than 1:360 is high - however, this is not a diagnosis, but an assumption.
What to do if you are at high risk of Down syndrome?
According to statistics, 70% of women carrying a child with Down syndrome are at risk. In this case, the woman is invited to undergo an additional examination at the medical genetic center. The specialist prescribes a series of tests and amniocentesis is practiced as an invasive diagnosis.
Features of invasive diagnostics
Amniocentesis is the analysis of amniotic fluid. The procedure is performed by puncturing the abdomen in the area of the embryonic membrane. Its result is a sample of amniotic fluid, which contains fetal cells.
Amniocentesis is performed by one of two methods:
1.