How many babies are born stillborn
What is Stillbirth? | CDC
The loss of a baby due to stillbirth remains a sad reality for many families and takes a serious toll on families’ health and well-being. Learn more about stillbirth below.
A stillbirth is the death or loss of a baby before or during delivery. Both miscarriage and stillbirth describe pregnancy loss, but they differ according to when the loss occurs. In the United States, a miscarriage is usually defined as loss of a baby before the 20th week of pregnancy, and a stillbirth is loss of a baby at or after 20 weeks of pregnancy.
Stillbirth is further classified as either early, late, or term.
- An early stillbirth is a fetal death occurring between 20 and 27 completed weeks of pregnancy.
- A late stillbirth occurs between 28 and 36 completed pregnancy weeks.
- A term stillbirth occurs between 37 or more completed pregnancy weeks.
View and print fact sheet » [482 KB / 2 pages]
How Many Babies Are Stillborn?
Stillbirth affects about 1 in 175 births, and each year about 21,000 babies are stillborn in the United States. 1 That is about the same as the number of babies that die during the first year of life. Because of advances in medical technology over the last 30 years, prenatal care (medical care during pregnancy) has improved, which has dramatically reduced the number of late and term stillbirths. However, the rate of early stillbirth has remained about the same over time.
What Increases the Risk of Stillbirth?
Stillbirth with an unknown cause is called “unexplained stillbirth.” The further along a woman is in her pregnancy the more likely it is that the stillbirth will be unexplained. Having an autopsy on the baby and other laboratory tests is important in trying to understand why the baby died before birth. Your health care provider can share more information about this.
Stillbirth occurs in families of all races, ethnicities, and income levels, and to women of all ages. However, stillbirth occurs more commonly among certain groups of people including women who:
- are of black race
- are 35 years of age or older
- are of low socioeconomic status
- smoke cigarettes during pregnancy
- have certain medical conditions, such as high blood pressure, diabetes and obesity
- have multiple pregnancies such as triplets or quadruplets
- have had a previous pregnancy loss
This does not mean that every individual of black race or older age is at higher risk for having a stillbirth. It simply means that overall as a group, more stillbirths occur among all mothers of black race or older age when compared to white mothers and mothers under 35 years of age. Some factors that might contribute to these stillbirth disparities include differences in maternal preconception health, socioeconomic status, access to quality health care, and stress.2 More research is needed to determine what is underlying reason why some of these factors are associated with stillbirths.
It simply means that overall as a group, more stillbirths occur among all mothers of black race or older age when compared to white mothers and mothers under 35 years of age. Some factors that might contribute to these stillbirth disparities include differences in maternal preconception health, socioeconomic status, access to quality health care, and stress.2 More research is needed to determine what is underlying reason why some of these factors are associated with stillbirths.
Many of these factors are also associated with other poor pregnancy outcomes, such as preterm birth.
What Can Be Done?
CDC works to learn more about who might have a stillbirth and why. CDC does this by tracking how often stillbirth occurs and researching what causes stillbirth and how to prevent it. Knowledge about the potential causes of stillbirth can be used to develop recommendations, policies, and services to help prevent stillbirth. While we continue to learn more about stillbirth, much work remains. To learn more about CDC’s activities, visit the Stillbirth CDC Activities page.
To learn more about CDC’s activities, visit the Stillbirth CDC Activities page.
References
- Gregory ECW, Valenzuela CP, Hoyert DL. Fetal mortality: United States, 2020. National Vital Statistics Reports; vol 71 no 4. Hyattsville, MD: National Center for Health Statistics. 2022. [Read report]
- Pruitt SM, Hoyert DL, Anderson KN, et al. Racial and Ethnic Disparities in Fetal Deaths — United States, 2015–2017. MMWR Morb Mortal Wkly Rep 2020;69:1277–1282.
- MacDorman MF, Kirmeyer SE, Wilson EC. Fetal and perinatal mortality, United States, 2006. National vital statistics reports; vol 60 no 8. Hyattsville, MD: National Center for Health Statistics. 2012. [Read data brief pdf icon[432 KB / 23 pages]
Stillbirth
What is stillbirth?
Stillbirth is when a baby dies in the womb after 20 weeks of pregnancy. Most stillbirths happen before a pregnant person goes into labor, but a small number happen during labor and birth. Stillbirth affects about 1 in 160 pregnancies each year in the United States.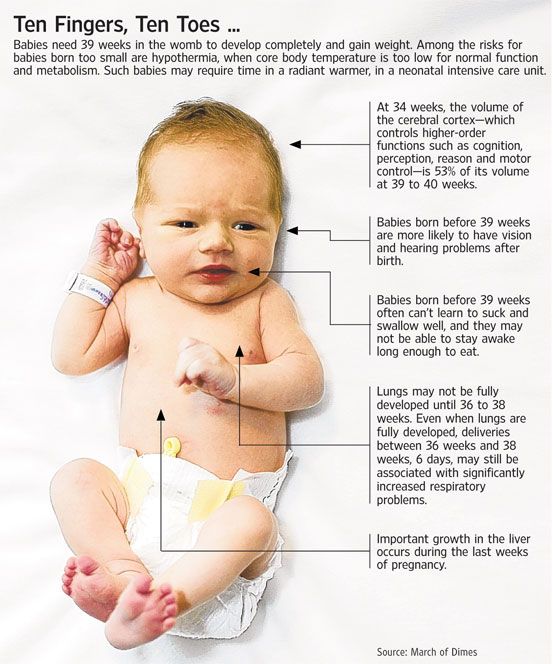
Who is at risk for stillbirth?
Stillbirth can happen in any family. We don’t always know why stillbirth affects certain families more than others. Researchers are working to learn more about risk factors for stillbirth.
Risk factors are things that make you at risk for (more likely than others to have) a condition. Having a risk factor for stillbirth doesn’t mean for sure that you will have a stillbirth. But knowing about and reducing your risk factors may help prevent a stillbirth from happening to your baby. Some risk factors are things you can’t change, such as having a stillbirth in a previous pregnancy. Other risk factors are things you can do something about, like quitting smoking. Talk to your health care provider about what you can do to help reduce your risk factors for stillbirth.
According to the Centers for Disease Control and Prevention (also called CDC) and other experts, risk factors for stillbirth include:
Medical conditions
- Being obese.
 If you’re obese, you have an excess amount of body fat and your body mass index (also called BMI) is 30 or higher. BMI is a measure of body fat based on your height and weight. To find out your BMI, go to www.cdc.gov/bmi.
If you’re obese, you have an excess amount of body fat and your body mass index (also called BMI) is 30 or higher. BMI is a measure of body fat based on your height and weight. To find out your BMI, go to www.cdc.gov/bmi. - Diabetes. Diabetes is a condition in which your body has too much sugar (called glucose) in the blood.
- High blood pressure. Blood pressure is the force of blood that pushes against the walls of your arteries. Arteries are blood vessels that carry blood away from your heart to other parts of the body.
- Substance abuse. Using certain harmful substances increase the risk of having a stillbirth. For example, smoking, drinking alcohol or using street drugs or prescription painkillers, such as opioids.
Pregnancy conditions and pregnancy history
- You’re pregnant with multiples (twins, triplets or more).
- You have intrahepatic cholestasis of pregnancy (also called ICP). This is the most common liver condition that happens during pregnancy.

- You had complications in a previous pregnancy, like premature birth, preeclampsia or fetal growth restriction. Preterm birth is a birth that happens too early, before 37 weeks of pregnancy. Preeclampsia is a condition that can happen after the 20th week of pregnancy or right after pregnancy. It’s when a pregnant person has high blood pressure and signs that some of her organs, like her kidneys and liver, may not be working properly. Fetal growth restriction is when a baby doesn’t gain enough weight in the womb before birth.
- You’ve never given birth before.
- You had a miscarriage or stillbirth in a previous pregnancy. Miscarriage is when a baby dies in the womb before 20 weeks of pregnancy.
- You’re pregnant after the age of 35. According to the American College of Obstetricians and Gynecologists (ACOG), studies show that a large number of stillbirths that happen among pregnant people 35 or older are related to congenital or chromosomal conditions.
- You have little social support.
 Many unmarried people have strong social networks of families and friends who help them. However, some studies have reported a higher risk of stillbirth among unmarried people. Researchers think that this may be because they have less social support.
Many unmarried people have strong social networks of families and friends who help them. However, some studies have reported a higher risk of stillbirth among unmarried people. Researchers think that this may be because they have less social support.
Health Disparities and Racism
We do not know exactly why, but stillbirth happens more often in some groups compared with others. We call this a health disparity (difference). To understand why these groups are at a higher risk of having a stillbirth we need to look at the social factors affecting them, this is what we call social determinants of health. These are the conditions in which you are born, grow, work, live and age. These conditions affect your health throughout your life. In many cases, social determinants of health and health disparities are related to racism.
Racism refers to the false belief that certain groups of people are born with qualities that make them better than other groups of people.
Racism isn’t limited to personal attacks such as ethnic slurs, bullying, or physical assault.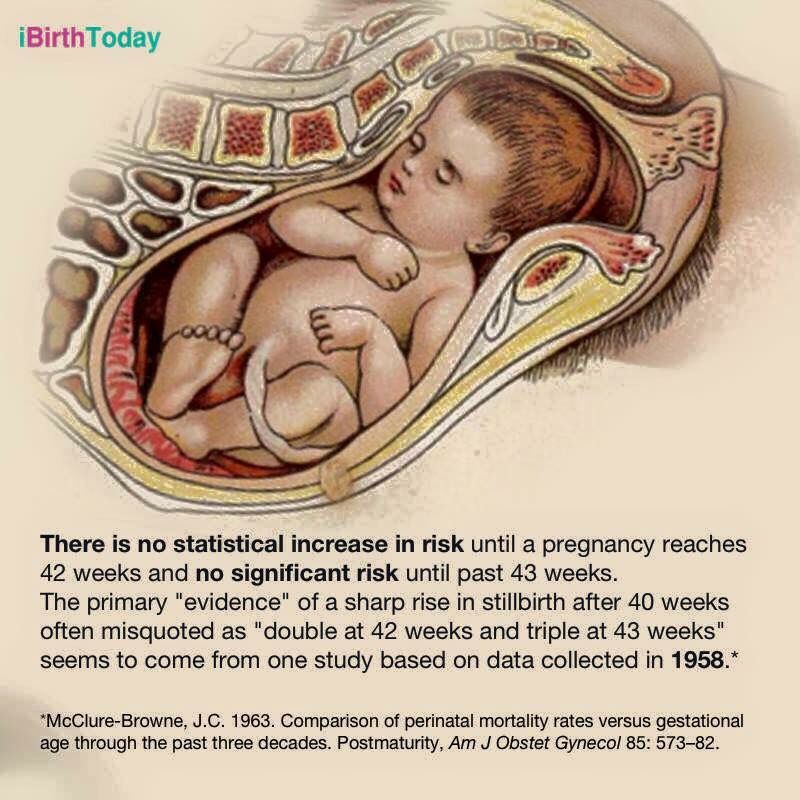 In a racist culture, one group of people has more power than other groups. People in the dominant racial or ethnic group make important decisions that affects everyone’s lives. For example, they have a lot of control over the way that schools, health care, housing, laws and law enforcement work. This control means that people in the dominant group are more likely to:
In a racist culture, one group of people has more power than other groups. People in the dominant racial or ethnic group make important decisions that affects everyone’s lives. For example, they have a lot of control over the way that schools, health care, housing, laws and law enforcement work. This control means that people in the dominant group are more likely to:
- Have better education and job opportunities
- Live in safer environmental conditions
- Be shown in a positive light by media, such as television shows, movies, and news programs.
- Be treated with respect by law enforcement
- Better access to health care
In contrast, people from racial or ethnic minority groups who live in a racist society are more likely to:
- Experience chronic stress
- Live in an unsafe neighborhood
- Live in areas that have higher amounts of environmental toxins, such as air, water, and soil pollution
- Go to a low-performing school
- Have limited access to healthy foods
- Have little or no access to health insurance and quality medical care
- Have less access to well-paying jobs
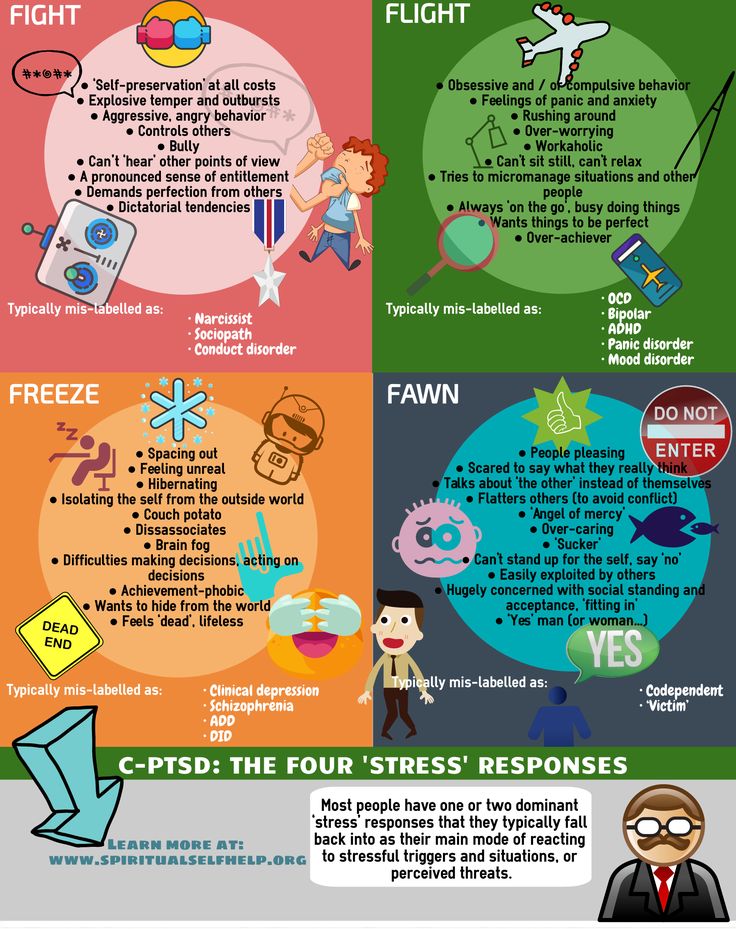
The Role of Chronic Stress
Studies have shown that the chronic stress caused by living in a racist culture is a factor in many health conditions, including having a preterm or low-birthweight baby. While some studies and statistics mention race as a risk factor for these conditions, we can’t say that race itself the cause. More research is needed to understand the connections between racism, stress, and health problems.
While some studies and statistics mention race as a risk factor for these conditions, we can’t say that race itself the cause. More research is needed to understand the connections between racism, stress, and health problems.
Rates of Stillbirth
According to data from the CDC (2017), there are there are major differences in stillbirth rates among different groups. For Black people, the stillbirth rate is more than double the rate than other groups, except when compared with American Indian/Alaskan Native people. These are rates per 1,000 live births and stillbirths. See the data below:
- Non-Hispanic Black, 10.32
- American Indian/Alaska Native people, 7.22
- Hispanic, 5.01
- Non-Hispanic white, 4.89
- Asian or Pacific Islander, 4.29
Being a person of color is not a cause for having a stillbirth. However, communities of color are disproportionately affected by racism. Racism and unequal living conditions affect their health and well-being and puts them at higher risk of pregnancy complications, such as stillbirth.
March of Dimes recognizes that racism and its effects are factors in the health disparities in pregnancy outcomes and babies’ health. We must work together to bring fair, just and full access to health care for all moms and babies.
How do you know if your baby is stillborn?
Signs of a condition are things someone else can see or know about you, like you have a rash or you’re coughing. Symptoms are things you feel yourself that others can’t see, like having a sore throat or feeling dizzy.
The most common symptom of stillbirth is when you stop feeling your baby moving and kicking. Others include cramps, pain or bleeding from the vagina. Call your health care provider right away or go to the emergency room if you have any of these conditions.
Your provider uses ultrasound to see if your baby’s heart has stopped beating. An ultrasound uses sound waves and a computer screen to show a picture of your baby in the womb.
What are your options for giving birth if your baby is stillborn?
If your baby is stillborn, your provider talks with you about options for giving birth. When and how you give birth depends on how far along you are in your pregnancy, your medical condition and what you think is best for you and your family. Some women need to give birth right away for medical reasons, but it’s often safe to wait until you go into labor on your own. Labor usually starts within 2 weeks after a baby dies in the womb.
When and how you give birth depends on how far along you are in your pregnancy, your medical condition and what you think is best for you and your family. Some women need to give birth right away for medical reasons, but it’s often safe to wait until you go into labor on your own. Labor usually starts within 2 weeks after a baby dies in the womb.
Your provider may recommend:
- Dilation and evacuation (also called D&E). During this surgical procedure, your provider dilates (opens) the cervix to remove tissue from the lining of the uterus. The cervix is the opening to the uterus (womb) that sits at the top of the vagina. Having a D&E may limit the information your provider can get about your baby’s condition. For example, if you have a D&E, your baby’s provider can’t do an autopsy on your baby.
- Inducing labor. This is when your provider gives you medicine or breaks your water (amniotic sac) to make your labor start. Most pregnant people with a stillbirth have their providers induce labor soon after they learn of their baby’s death.
 If you decide to wait to go into labor on your own and it doesn’t happen by 2 weeks after your baby’s death, your provider may induce labor to help prevent dangerous blood clots from developing.
If you decide to wait to go into labor on your own and it doesn’t happen by 2 weeks after your baby’s death, your provider may induce labor to help prevent dangerous blood clots from developing. - Cesarean birth (also called c-section). This is surgery in which your doctor makes a cut in your belly and uterus to deliver your baby.
What tests do you get after a stillbirth?
Your provider checks your baby, the placenta and the umbilical cord to try to find out why your baby died. The placenta grows in your uterus and supplies the baby with food and oxygen through the umbilical cord. Your provider may ask to do certain tests to try find out what caused the stillbirth. Tests may include:
- Amniocentesis (also called amnio). In this test, your provider takes some amniotic fluid from around your baby in the uterus. If your provider thinks a genetic condition or an infection in your baby may have caused the stillbirth, she may recommend an amnio before you give birth.
 Genetic conditions are health conditions that are passed from parents to children through genes.
Genetic conditions are health conditions that are passed from parents to children through genes. - Autopsy. This is a physical exam of your baby’s body after death. During an autopsy, a provider checks your baby’s organs for signs of birth defects or other conditions. This may help your provider find out what caused your baby’s death and if you may be at risk of having another stillbirth in the future. It’s common for a provider not to find a cause for stillbirth. Birth defects are health conditions that are present at birth. They change the shape or function of one or more parts of the body. Birth defects can cause problems in overall health, how the body develops or how the body works.
- Genetic tests. Genetic tests to check for genetic conditions in your baby
- Tests for infections on your baby or on the placenta
In addition to checking your baby for medical and genetic conditions, your provider reviews your family health history and any problems or illnesses you had during pregnancy. Your family health history is a record of any health conditions you, your partner and members of both your families have had. Your provider may want to test you for infections, genetic conditions and other medical conditions, like lupus or thyroid problems.
Your family health history is a record of any health conditions you, your partner and members of both your families have had. Your provider may want to test you for infections, genetic conditions and other medical conditions, like lupus or thyroid problems.
Information from tests on you and your baby may help you if you’re thinking about getting pregnant again. Test results may help your provider find out if there’s a chance that you could have another stillbirth. Even if your provider doesn’t find out what caused your stillbirth, having the tests may help you better understand and cope with your baby’s death. If you have questions about the tests, including their cost, talk to your health care provider.
If you’ve had a stillbirth, can you have a healthy baby in another pregnancy?
Yes. For most women, the chances of having another stillbirth are very low. Less than 1 in 100 women (less than 1 percent) who’ve had a stillbirth go on to have another stillbirth.
If you had a stillbirth and are thinking about having another baby, give yourself time to heal physically and emotionally. Your provider may recommend that you have medical tests to try to find out more about what caused your stillbirth. You may need to wait until after you’ve had these tests to try to get pregnant again.
Your provider may recommend that you have medical tests to try to find out more about what caused your stillbirth. You may need to wait until after you’ve had these tests to try to get pregnant again.
If you had a stillbirth that was caused by a genetic condition, a genetic counselor can help you understand the condition and the chances of you having another stillbirth. A genetic counselor is a person who is trained to help you understand about how genes, birth defects and other medical conditions run in families, and how they can affect your health and your baby’s health. Your health care provider can help you find a genetic counselor.
Here’s what you can do help to lower your risk of having a stillbirth in another pregnancy:
- Get a preconception checkup. This is a medical checkup you get before pregnancy. It helps make sure you’re healthy when you get pregnant.
- Get treatment for any medical conditions you have.
- Get to a healthy weight before getting pregnant.
 Your provider can recommend ways to get to a weight that’s right for you.
Your provider can recommend ways to get to a weight that’s right for you. - Don’t smoke, drink alcohol, use marijuana or other drugs that can be harmful to your pregnancy. Tell your provider if you need help to quit.
- If you have any pain or bleeding from the vagina during pregnancy, call your provider right away.
If you get pregnant again, your provider monitors you and your baby closely. At around 32 weeks of pregnancy, she may ask you to do kick counts to help you keep track of how often your baby moves. Your provider also may do medical tests to check your baby’s heart rate and movements.
What causes stillbirth?
We don’t know what causes many stillbirths, but common causes include:
Infections in the mother or baby. Some infections may not cause signs or symptoms and may not be diagnosed until they cause serious complications, like premature birth or stillbirth. Infections that can cause stillbirth include:
- Cytomegalovirus (also called CMV).
 This is a kind of herpes virus that you can get by coming in contact with body fluid (like saliva, semen, mucus, urine or blood) from a person who carries the virus. It’s a common infection in young children, but if you get it during pregnancy, it can cause serious problems, like stillbirth.
This is a kind of herpes virus that you can get by coming in contact with body fluid (like saliva, semen, mucus, urine or blood) from a person who carries the virus. It’s a common infection in young children, but if you get it during pregnancy, it can cause serious problems, like stillbirth. - Fifth disease. This is a common childhood illness that’s caused by a virus called parvovirus B19. It usually spreads through the air from an infected person’s cough or sneeze.
- Genital and urinary tract infections. These infections affect the urinary tract and genitals (also called sex organs), like the vagina or ovaries. The urinary tract is the system of organs (like the kidneys and bladder) that helps your body get rid of waste and extra fluids. Getting infected with genital herpes for the first time during pregnancy can lead to stillbirth. Genital herpes is a sexually transmitted infection (also called STI) you can get from having sex with someone who’s infected.
- Listeriosis.
 This is a type of food poisoning.
This is a type of food poisoning. - Syphilis. This is an STI.
- Toxoplasmosis. This is an infection you can get from eating undercooked meat or touching cat poop.
Problems with the placenta or umbilical cord. Placental problems include infections, blood clots, inflammation (redness, pain and swelling), problems with blood vessels and other conditions, like placental abruption. Placental abruption is a serious condition in which the placenta separates from the wall of the uterus before birth. Placental problems cause about 24 in 100 stillbirths (24 percent). Problems with the umbilical cord include having a knot in the cord or the cord being pinched so that your baby doesn’t get enough oxygen. Problems with the umbilical cord may lead to about 10 in 100 stillbirths (10 percent).
Complications during pregnancy, including:
- Being pregnant longer than 42 weeks
- Diabetes, obesity, high blood pressure and preeclampsia
- Health conditions like lupus, thrombophilias and thyroid disorders.
 Lupus is an autoimmune disorder. Autoimmune disorders are health conditions that happen when antibodies (cells in the body that fight off infections) attack healthy tissue just about anywhere in the body by mistake. Thyroid disorders affect your thyroid, a gland in your neck that makes hormones that help your body store and use energy from food. Thrombophilias increase your chances of making abnormal blood clots.
Lupus is an autoimmune disorder. Autoimmune disorders are health conditions that happen when antibodies (cells in the body that fight off infections) attack healthy tissue just about anywhere in the body by mistake. Thyroid disorders affect your thyroid, a gland in your neck that makes hormones that help your body store and use energy from food. Thrombophilias increase your chances of making abnormal blood clots. - Preterm labor and preterm premature rupture of the membranes (also called PPROM). Preterm labor is labor that begins early, before 37 weeks of pregnancy. PPROM is when the sac around the baby breaks early, causing labor to start.
- Fetomaternal hemorrhage. This is when your baby’s blood mixes with your blood during pregnancy or birth.
- Trauma or injuries (like from a car accident)
Conditions in the baby, including:
- Birth defects and genetic conditions. About 14 in 100 stillborn babies (14 percent) have one or more birth defects, including genetic conditions like Down syndrome.
- Fetal growth restriction
- Not getting enough oxygen during labor and birth
- Rh disease. Rh factor is a protein on the surface of red blood cells. Rh disease happens when a woman who doesn’t have the protein (called Rh-negative) is pregnant with a baby who does have the protein (called Rh-positive). Rh disease can be prevented.
How can you deal with feelings of grief after a stillbirth?
Grief is all the feelings you have when someone close to you dies. Having a stillborn baby is a painful loss for a family. But there are things you can do to help you grieve, heal and remember your baby.
After birth, do what feels right for you and your family. You may want to spend time alone with your baby and other family members. You can name your baby, hold your baby, bathe and clothe her and take part in cultural or religious traditions, like baptism. Some families take pictures of their baby, make footprints or save locks of hair. You may be able to keep things from the hospital, like blankets, that were used with your baby. Keepsakes like these can help you and your family remember your baby.
Keepsakes like these can help you and your family remember your baby.
Parents who have a stillbirth need time to grieve. You and your partner may cope with grief in different ways, and you may need help dealing with others as you grieve.
After you leave the hospital, certain things, like hearing names you were thinking of for your baby, seeing the baby’s nursery at home or having your breast milk come in can be painful reminders of your loss. You may need help learning how to deal with these situations and the feelings they create. Ask your health care provider to help you find a grief counselor to help you cope with your baby’s death. Or your hospital may have a loss and grief program for families. Getting counseling can be really helpful to you and your family.
Talking about your feelings with other parents who have had a stillbirth may help you deal with your grief. Visit shareyourstory.org, the March of Dimes online community where families who have lost a baby can talk to and support each other. Sharing your story may ease your pain and help you heal.
Sharing your story may ease your pain and help you heal.
Having a stillbirth may make you at risk for postpartum depression (also called PPD). PPD is a kind of depression that some women get after having a baby. Tell your provider if you have signs or symptoms of PPD, like feeling depressed most of the day every day, having little interest in things you normally like to do, or having trouble eating or sleeping.
More information
- From hurt to healing (free booklet from the March of Dimes for grieving parents)
- Share Your Story (March of Dimes online community for families to share experiences with prematurity, birth defects or loss)
- Centering Corporation (grief information and resources)
- Compassionate Friends (support for families after the death of a child)
- First Candle (support for families with children who died of SIDS or preventable stillbirth)
- International Stillbirth Alliance
- Journey Program of Seattle Children’s Hospital (support for families after the death of a child)
- Now I Lay Me Down to Sleep (remembrance photography)
- Perinatal Hospice & Palliative Care (resources for parents who find out during pregnancy that their baby has a life-limiting condition
- Share Pregnancy & Infant Loss Support (resources for families with pregnancy or infant loss)
- Star Legacy Foundation (support for families who have had a stillbirth)
Last reviewed: October, 2020
No name, no benefits: stillborn parents have no rights | Estonia
Parents of stillborn children consider it unfair that they cannot give the child an official name and are not entitled to benefits and compensation. Minister of Social Affairs Signe Riisalo promises to bring the issue of childbirth allowance to the government for discussion.
Minister of Social Affairs Signe Riisalo promises to bring the issue of childbirth allowance to the government for discussion.
Agnes' second pregnancy went well. She was glad that her son Bjorn would have a brother. “I immediately felt pregnant,” says Agnes Pitka.
"We were very calm, prepared, told our son that he was already an adult and would soon have a brother. There were no hints that something was wrong," adds Agnes' husband Matti Orav.
Their baby was due on Mother's Day, May 10th.
"Last Mother's Day was wonderful. The sun was shining, it was warm. That was the last day I felt the baby move," Agnes recalls.
Then she took a picture of her belly, but the sensations were not the same. She now realizes that by then the baby was dead.
“I went to bed that evening and didn’t feel him. It was unusual, he always moved before I fell asleep. The next day I put my eldest son to bed and realized that everything was bad,” the woman recalls.
At that time, Agnes still hoped that she was just tired of the long wait, but she called the midwife, and she told her to urgently come for a check-up. In May, the state of emergency was still in effect, and she had to travel alone.
"She looked and didn't tell me anything, got up and left. The second doctor came and they mentioned that the heart was not working. I asked if the baby was dead and they said yes," continues Agnes.
She was sent home. The next day, she had to return to the hospital to give birth to her dead baby.
"The next day I took Agnes to the hospital, and I went with my son to the village. The child fell asleep on the way. I thought about what Agnes was doing, how difficult it was for her, but there was nothing I could do. And then I cried" , - Matti admits.
They talked to Agnes by phone. After the birth, the father named the boy Miykael.
Only a few photographs now remind parents of him: one photograph was secretly taken by his mother during an ultrasound examination, and the second after his birth, as the crisis counselor advised her to do. My father was able to see Miikael and say goodbye to him only in the crematorium. The parents have not yet committed the ashes of the boy to the ground.
My father was able to see Miikael and say goodbye to him only in the crematorium. The parents have not yet committed the ashes of the boy to the ground.
Doctors investigated the causes of death, but received no answers. It is worth noting that in about half of the cases, the cause of intrauterine fetal death remains unknown.
Matti and Agnes are not alone in their tragedy. Last year, 28 children were born dead in Estonia, in previous years their number reached 50.
After the death of a child, grieving and shocked parents find themselves in a labyrinth of incredible bureaucracy, unexpected and unfair. For example, a stillborn child cannot be officially given a name, is not entered in the Population Register and is not assigned a personal code.
Many of these children are buried in the so-called Silence Cemetery in Harju Risti. The gravestone is the only place where you can write the name of the child.
Comrades in misfortune are united by the NGO "Children of Silence", led by Triina Tints, who also survived the death of her child before his birth.
"Sounds like a small thing, but it's important for parents to have their child's name officially recorded. Not just on the gravestone," Tints says.
Marika Lass, a social worker at the Ida-Tallinn Central Hospital, who helps families through the period of grief, also faces the desire of parents to give a name to a stillborn child every time. These parents have virtually no rights.
"Every time we see helplessness and confusion. We explain that the name of the child can be written on the monument, but it will not be in the registers" - Lass believes that this state of affairs cannot be given any reasonable explanation.
Agnes Pitka also calls this circumstance the most unpleasant. “I wanted to register the birth of my child, that I have two children. But he is not in the Population Register,” she states.
If her son had had time to take at least one breath after the birth, then he would have been given a name and a personal code, and the family would have received state childbirth benefits.
In case of intrauterine death of the fetus, a death certificate is not issued, as this requires a personal code. In such cases, only a death notice is issued, and even officials do not navigate their bureaucracy.
"When I went for a death notice, they asked me what the child's name was. I had to explain that my child did not have a name, and I came for a death notice. They looked like a fool, because I came for a death certificate of a child, What was your name? I eventually received this piece of paper, my name and gender of the child were written on it, "says Agnes.
The next surprise was the fact that the father's name is also not written anywhere. “That is, it was as if the father did not exist. I was not the only one who made this child,” Agnes is indignant.
"Such nuances come to light, a person should not do this. To prove whether you had a child or not. And it's so difficult, why complicate people's life even more," Matti wonders.
Ten years ago, stillborn children could be given a name, given a personal code and entered in the Population Register. Then the law was changed, and stillborn children officially became nameless.
Then the law was changed, and stillborn children officially became nameless.
"This was due to the fact that if a stillborn child is allowed to be entered in the Population Register, then this possibility should be from the 22nd week of pregnancy. But parents of very premature babies may not want to give a name or draw up any other documents ", - explains the head of the department of population and family policy of the Ministry of the Interior Lea Danilson-Yarg.
According to international standards, birth is the birth of a child after the 22nd week of pregnancy. It is by this time that all vital organs are formed in the fetus. Otherwise, we are talking about abortion. In Estonia, about half of stillborn babies are full-term, and parents want them to have a name.
It was Danilson-Jarg's department that began to look into the matter after ERR raised the issue of unequal treatment of families last November. Then the process was headed by the Minister of Population Riina Solman, who recognized the shortcomings and promised to look for a solution. But the government changed, and the post of Minister of Population was abolished.
But the government changed, and the post of Minister of Population was abolished.
Unnamed children
The Population Register is administered by the Ministry of the Interior. According to Danilson-Yarg, the issue of the names of stillborn children can be solved in a different way, without the Population Register.
"The population register is not the only way to give a baby a name. Currently, stillborn babies after the 22nd week of pregnancy are given a death notice. And it has a name and a unique code in its data set. So, according to the Naming Law , parents can always give their child a name, the only question is where this name is documented,” says Danilson-Yarg.
It is noteworthy that last year, when the notorious Naming Law was being approved, the Ministry of the Interior clearly wanted to deprive stillborn children of the right to a name, but the Ministry of Social Affairs did not approve it. The controversial law has not yet been adopted, last week the new government returned it to the Ministry of the Interior.
And if an official claims that it is possible to give a name, then in practice everything is not so.
"The systems are inflexible. We tried in our system to give the child a name and put it on the death notice, but the system doesn't allow it," says social worker Marika Lass.
"The name does not appear on the death certificate, because the deceased does not have a personal code and connection with the Population Register. However, a name can be added to the notice of the cause of perinatal death and to the notice of death using the instructions. Such an opportunity for parents is a health worker must offer before filling out the death notice, because the name does not automatically appear on it. The second nuance is that even if the name is written in the notice, this information does not fall into any databases, "explains the head of the Department of Child Welfare of the Ministry social affairs Hanna Vseviov.
The absence of a name in the register and a personal code is not just a matter of emotions. Numerous practical problems of families are connected with this.
Numerous practical problems of families are connected with this.
"If a child lives for some time after birth, then parents can give him a name, receive a birth allowance, apply for a funeral allowance. Families in which a child was born dead become victims of gaps in the law and bureaucracy," states Triinu Tints from NGO "Children of Silence".
Benefits - for the living
The question is also about money. Families who, in anticipation of the birth of a child, bought the necessary things and counted on benefits when planning the budget, are left with nothing.
"Of course, we counted on the birth allowance and the maternity salary. Financially, it was a blow," admits Matti Orav.
"Most of the rights, various vacations, benefits, are related to the existence of the child. If the child is born dead, then the parents do not have rights to receive most benefits," Hanna Vseviov confirms.
The government encourages families to have children less than three years apart. In this case, the mother's salary remains at the level at which it was after the birth of the first child. If the child is born dead, then it does not affect the calculation of benefits. This means that if the family, after a traumatic experience, decides to have a child again, then the calculation of the three-year period will begin from the time of the birth of a living child, and not a dead one. It turns out that families who have lost a child are punished doubly.
In this case, the mother's salary remains at the level at which it was after the birth of the first child. If the child is born dead, then it does not affect the calculation of benefits. This means that if the family, after a traumatic experience, decides to have a child again, then the calculation of the three-year period will begin from the time of the birth of a living child, and not a dead one. It turns out that families who have lost a child are punished doubly.
The situation should change in April next year, when amendments come into force to correct gaps in the law, and time can again be taken into account from the moment of the birth of a dead child.
At the same time, the state gives with one hand and takes with the other. If now maternity and birth leave lasts 140 days, then the new law will not have such a concept and it will be replaced by the term "parental leave". The mother's right to leave in the event of the death of the child will end 30 days after the tragic event.
"It's not fair. If a child is stillborn or dies late, then the family needs time to recover. If the law requires the mother to return to work after 30 days, then this is an unfair law," Lass said.
At the same time, the Ministry of Social Affairs says that the families were simply met halfway, and according to the law, the right to 140-day leave should not apply to them at all.
"In fact, at present there are no legal grounds for paying maternity benefits to these families and providing leave. That is, if there is no ground, then there is a child, but there is no right either. We tried to mitigate this purely for practical reasons, so as not demand the return of benefits, but in fact there are no legal grounds for this at all," Vseviov said.
When a child is stillborn, the family does not receive state benefits, even if they have incurred the costs.
"I loaned my first child's stroller to a friend of mine, so I won't have to see it again. I just gave away the rest of the things," says Agnes.
The topic was passed from the Minister of Population to the Minister of Social Affairs, Signe Riisalo. According to Vseviov, the new minister promised to bring the issue to the discussion of the government.
Missing Fathers
By law, families with a stillborn child cannot take 30 days of paternity leave. Such amendments to the law came into force in July last year. After the news portal ERR highlighted the problem at the end of last year, the Department of Social Insurance, which deals with the payment of benefits and compensations, decided to review the current practice and pay benefits also to the fathers of stillborn children. Last July, 11 dead babies were born in Estonia. Since the state does not have data on them, the search for fathers turned out to be a difficult task.
"We managed to contact three fathers out of 11, they were paid compensation. For the Social Insurance Department, the situation is complicated by the fact that there is no information about these children and fathers," says Vseviov, adding that the only way to find the fathers is to go to hospitals .
From April next year, fathers of stillborn children will also be entitled to 30 days' leave and appropriate compensation.
Various solutions
For parents, it is not a matter of principle for benefits, but for the right to a name. In the ministries involved in the issue, the vision of solving the problem differs.
"We proposed to the Ministry of Social Affairs to supplement the data set with the name of the father. We do not see the possibility of restoring such a mark in the Population Register. The issue should be resolved as soon as possible through a death notice so that the unique code that is entered in it would be the basis for the payment of various benefits and compensation," a spokeswoman for the Interior Ministry said.
"It seems to me that we are now going in circles, looking for a solution and reviewing various registers and ways of transmitting data, but in fact we have a place that allows us to solve all these problems. We will definitely come up with a proposal to enter data on such children in the Register population,” says Vseviov of the Ministry of Social Affairs, referring to the restoration of the old order.
We will definitely come up with a proposal to enter data on such children in the Register population,” says Vseviov of the Ministry of Social Affairs, referring to the restoration of the old order.
Agnes Pitka and Matti Orav most of all want their child to receive an official name - Miikael Orav - at least in hindsight.
"He was born at 41 weeks. He was human," explains Agnes.
The Ministry of Social Affairs promises to listen to the wishes of the parents.
"I don't see any reason why it would be impossible. After all, we write laws for the people," says Vseviov.
“Given in a box. Buried themselves ”Why dead babies are considered biological garbage in Russia: Society: Russia: Lenta.ru
The #necessary_words project is gaining popularity in Russian social networks. Its mission is to support women who have lost a child before, during and shortly after childbirth. According to the Light in Hands charity foundation, in 2016, 17,000 stillbirths were registered in Russia. Approximately the same number of pregnancies were terminated for medical reasons. For a woman, the news that she will have to have an abortion because doctors doubt the viability of the fetus becomes a tragedy. A family in such a situation is often left alone with their grief, and in dealing with doctors, instead of receiving support, they receive additional psychological trauma. Why is this happening and is it possible to help them - Lenta.ru found out.
Approximately the same number of pregnancies were terminated for medical reasons. For a woman, the news that she will have to have an abortion because doctors doubt the viability of the fetus becomes a tragedy. A family in such a situation is often left alone with their grief, and in dealing with doctors, instead of receiving support, they receive additional psychological trauma. Why is this happening and is it possible to help them - Lenta.ru found out.
The editors intentionally chose a harsh tone in the presentation of this material in order to draw attention to the problem of ethical treatment of mothers who have lost their children during childbirth.
Lenta.ru
Newborn waste
Three years ago, Natalia and Vladimir Skripin (surname changed) from Yekaterinburg died in a hospital during childbirth. The doctors refused to release the body for burial. Legally, they did not violate anything, because according to Russian laws, a fetus born no earlier than the 22nd week of pregnancy, weighing at least 500 grams and at least 25 centimeters tall is considered a person. Everything else is biological waste and must be disposed of as sanitary waste.
Everything else is biological waste and must be disposed of as sanitary waste.
“The pregnancy was long-awaited,” Natalia recalls. “At first everything went well. Even toxicosis did not torment. And then I went with my husband for an ultrasound. He wanted to know the gender and get a photo of the baby. I can still see the expression with which the doctor looks at the computer screen and hides his eyes from me. And I have a smile on my face. Because it is clear that something terrible has happened. And then the verdict: "The fetus is not viable."
Photo: Alexander Ryumin / TASS
The deadline was already long — five months. Doctors insisted on artificial childbirth. During this manipulation, the pregnant woman is given special pills that cause contractions. Parents did not agree and ran from one local luminary of gynecology to another with a crazy hope: suddenly a mistake.
“You have no idea how much pressure the doctors put on us when they found out that we didn't want to terminate the pregnancy,” Natalia sobs. - It's very scary. And this squeamish tone - as if a threat to all mankind is growing in my stomach!
- It's very scary. And this squeamish tone - as if a threat to all mankind is growing in my stomach!
According to Natalia, everything ended naturally - a spontaneous miscarriage. Natalya really wanted to look at her son, but in the first minutes after the birth she was almost unconscious. And then no one allowed. They also refused to give out the body for burial with the wording: “You will give birth again. Everything is for your own good, so that at night you don’t dream of horrors later. ”
Despite the fact that several years have passed, Natalya says that she cannot forget her failed son.
— My mother-in-law and even my mother erased everything from memory and pretend that the child didn’t exist, — continues Natalya. — I really want to, but I can’t reset my memory. I often think about who my boy would look like. I didn't even see him. I dream about how it is thrown into a landfill, like biological garbage.
At family forums, the topic “Should embryos be buried” is constantly discussed. Tragedy survivors share experiences. Since the law does not endow the fetus with human rights, a birth and death certificate is not issued for it - therefore, it is impossible to officially arrange a burial. But many do it bypassing bureaucratic procedures.
Tragedy survivors share experiences. Since the law does not endow the fetus with human rights, a birth and death certificate is not issued for it - therefore, it is impossible to officially arrange a burial. But many do it bypassing bureaucratic procedures.
“My baby, who was born at the 20th week of pregnancy, died,” says Irina, a Muscovite. - The hospital did not want to give the body, they said that the state buries the stillborn. But then the husband informally agreed. Issued in a box. They buried themselves in grandfather's grave. For a long time I could not decide to come to the cemetery. And now I go there often. It helps to let go of grief.
The writer Anna Starobinets was one of the first to raise the topic of pain from failed parenthood in the public space. In the autobiographical story “Look at him,” she told how, at the 16th week of pregnancy, she found out that her child was terminally ill. The book details what the mother-to-be faces if something goes wrong. A woman is treated like an inanimate object that is not supposed to have an opinion. For example, if a rare pathology is found in an embryo, then the doctor, without even asking permission from the patient, may invite students to look at the “interesting object” for educational purposes.
A woman is treated like an inanimate object that is not supposed to have an opinion. For example, if a rare pathology is found in an embryo, then the doctor, without even asking permission from the patient, may invite students to look at the “interesting object” for educational purposes.
Photo: Sergey Venyavsky / RIA Novosti
Against the background of global problems in Russian healthcare, the lack of ethics does not seem to be something terrible, but recently Ekaterina Nekrasova, an ultrasound diagnostician from St. Petersburg, published an article in a professional journal in which she expressed her thoughts about how to properly counsel couples with "problem" pregnancies. The doctor gives specific recommendations on the tactics of conducting a conversation.
“Giving bad news to a patient is a certain test for a doctor,” explains Nekrasova. - A defensive reaction in a morally difficult situation is the desire to end an unpleasant conversation as quickly as possible, since it is difficult not only for the patient, but also for the doctor.
Dr. Nekrasova is now working on the details of a practical training on "Breaking bad news" for doctors of prenatal (prenatal) diagnostics, in which professional actors will participate.
“Parents should have a chance to say goodbye”
In Russia, people are just beginning to talk about the need for perinatal palliative care, including psychological help for parents. And in Europe and America, this direction has been developing for a long time. At the Palliative Care for Children conference organized by the Vera Charitable Foundation, Joan Wolf, Head of the Department of Palliative Care at the Boston Children's Hospital (USA), spoke about this. Later, she answered questions from Lenta.ru.
Lenta.ru: Why is the US concerned about this problem?
Joan Wolf: A number of scientific papers have been published in which neonatologists have pointed out that many newborns die in agony without receiving any help, and their parents are left without support. This problem was widely discussed, and about 10 years ago, at the request of society, a new service appeared.
This problem was widely discussed, and about 10 years ago, at the request of society, a new service appeared.
The main task of the perinatal palliative care is to help the mother and family when it is discovered that the fetus has serious pathologies. We are talking about conditions when a child can die in the womb, live a short time or remain disabled. Usually the starting point is the office of an obstetrician-gynecologist who understands that the fetus has serious problems. The doctor talks about the diagnosis, and then, if necessary, calls the palliative care team. Experts come and discuss different options.
Photo: China Stringer Network / Reuters
Could there be more than one? In Russia, in case of serious malformations, doctors strongly recommend terminating the pregnancy.
In the US, the situation is similar: most families reported that doctors persuaded them to have an abortion. Most often this happens with identified genetic disorders. In such cases, many gynecologists for some reason are sure in advance that the woman will want to have an abortion. But it all depends on what values the family professes. Do not forget that the United States is a religious country, there are many Catholics here. Under no circumstances can they have an abortion. Often mothers, even fully aware of the difficulties ahead, decide to give birth and wait for the natural development of events.
But it all depends on what values the family professes. Do not forget that the United States is a religious country, there are many Catholics here. Under no circumstances can they have an abortion. Often mothers, even fully aware of the difficulties ahead, decide to give birth and wait for the natural development of events.
Who is the palliative team?
Usually a pediatrician with a year of training in palliative care, a nurse and a social worker.
What exactly do they do?
The most important thing is that they provide complete information about how the disease will develop, what to expect. If the family decides not to terminate the pregnancy, they prepare the parents in advance for difficulties. The issue of resuscitation is being discussed - with the help of a ventilator, life can be maintained for a long time. If the natural path is chosen, the doctor decides how to alleviate the child's condition from the first seconds of life so that he does not feel discomfort. Parents should have a chance to hold their child in their arms, to say goodbye. We always suggest doing this, even in case of premature birth, when the baby is very young.
Parents should have a chance to hold their child in their arms, to say goodbye. We always suggest doing this, even in case of premature birth, when the baby is very young.
But why? In Russia, doctors, on the contrary, believe that this can negatively affect the psyche of a woman. Long send-offs are extra tears...
Previously, the US adhered to exactly the same position. But there are scientific studies that in the long term, for many, such alleged “care for the psyche” led to serious mental problems. The woman has an unprocessed psychotrauma. She does not understand - there was something or not. The rite of farewell, as it were, puts an end to it. Therefore, now all mothers are asked the question: do you want to? Most agree.
“We remember your child”
And if the child has obvious physical deformities, won't this aggravate the mother's condition?
Doctors warn relatives what to expect, what to prepare for. Even a child with developmental anomalies is always useful for mothers to hold in their hands. For many parents, this baby, despite all the shortcomings, is a favorite, he is a part of them. The child is usually cooked before being handed over to the hands of relatives. They swaddle him, put on a hat. And he doesn't look terrible. We also always offer to make prints of arms and legs so that parents have something to remember. We partner with a professional association of volunteer photographers who, as volunteers, invite families to take professional photographs of a child before or after death. This remains later as evidence that their child was, he did not disappear without a trace. We invite all family members and close friends to participate in the farewell ceremony.
For many parents, this baby, despite all the shortcomings, is a favorite, he is a part of them. The child is usually cooked before being handed over to the hands of relatives. They swaddle him, put on a hat. And he doesn't look terrible. We also always offer to make prints of arms and legs so that parents have something to remember. We partner with a professional association of volunteer photographers who, as volunteers, invite families to take professional photographs of a child before or after death. This remains later as evidence that their child was, he did not disappear without a trace. We invite all family members and close friends to participate in the farewell ceremony.
Photo: Valery Sharifulin / TASS
Even older children, if they are in this family?
If a brother or sister is over four years old, it is right for them to have this experience. That is, it is better to participate in a family tragedy than to remain in the dark. Children still feel that something bad is happening, and can draw terrible pictures in their imagination. At such moments, they are given less attention, and some take it personally - they think that bad things happened because they did not obey. Others suddenly decide that they are no longer loved. And when they themselves see what is happening, it also has a psychotherapeutic effect on them.
At such moments, they are given less attention, and some take it personally - they think that bad things happened because they did not obey. Others suddenly decide that they are no longer loved. And when they themselves see what is happening, it also has a psychotherapeutic effect on them.
In Russia, the bodies of premature babies are often not allowed to be buried because it is legally considered "bio-waste".
Our family decides everything. Parents are guided by their traditions. Usually such a child is buried in the same way as everyone else.
Have there been cases when terrible forecasts of doctors turned out to be erroneous and an absolutely healthy child was born?
Misdiagnosis can be made, but it mainly concerns chromosomal abnormalities. For example, Down syndrome, Edwards. A couple of days ago we had almost a miracle. At the stage of pregnancy, the child was diagnosed with a serious pathology of the skeleton. It was seen that the fetus had abnormally short limbs and a very small chest. Doctors were sure that the girl would die in the process of childbirth. However, a normal baby was born. Of course, we are not talking about absolute health, the skeleton is underdeveloped, but the most important thing is that the child can breathe on his own. And it's practically a miracle. A gynecologist at one time recommended an abortion to the family.
Doctors were sure that the girl would die in the process of childbirth. However, a normal baby was born. Of course, we are not talking about absolute health, the skeleton is underdeveloped, but the most important thing is that the child can breathe on his own. And it's practically a miracle. A gynecologist at one time recommended an abortion to the family.
Do you have any recommendations on how exactly a doctor should tell a woman bad news, what expressions can be used?
Of course, there are no pre-prepared scenarios where all the replicas are registered. But on this topic, trainings are necessarily held, where different situations are played out with the actors. A doctor of any specialty can participate. However, there are many specialists in the same palliative who are trying to do this work without proper training. They make a lot of mistakes in communicating with families.
What, for example?
I can give an example not from the perinatal palliative, but the situation is similar. I interviewed the parents of children who died of cancer. Among others, the questionnaire included the question: “What is your impression of how you were told the tragic news?”. Parents often recalled that doctors and nurses were too emotional in these situations. Sometimes they even felt some anger towards the families of the sick.
I interviewed the parents of children who died of cancer. Among others, the questionnaire included the question: “What is your impression of how you were told the tragic news?”. Parents often recalled that doctors and nurses were too emotional in these situations. Sometimes they even felt some anger towards the families of the sick.
Doctors were angry because they could not cure the patient, could not help?
This happened, for example, when the parents refused the solutions recommended by the doctor. And in perinatal medicine, a doctor can often say rudely: “Don't you understand that your child will be born dead? Why don't you terminate the pregnancy?" If a woman even once heard this, she will never forget it.
Photo: Yury Martyanov / Kommersant
Are those who work in palliative care required to undergo training in the ethics of communication with patients?
We don't have a supervisory body to keep track of this. But our system is set up in such a way that over time everything will normalize itself.