Whooping cough vaccination for pregnant women
Whooping Cough Vaccines Are Safe
Whooping cough vaccines are safe, but side effects can occur. CDC continually monitors the safety of all vaccines, which CDC holds to the highest standards of safety. Learn more about how new vaccines get licensed and how their safety is monitored.
The whooping cough vaccine is very safe for you and your baby
The whooping cough vaccine is very safe for pregnant women and their babies. Doctors and midwives who specialize in caring for pregnant women agree that the whooping cough vaccine is important to get during the third trimester of each pregnancy. Getting the vaccine during your pregnancy will not put you at increased risk for pregnancy complications.
CDC and a panel of experts who make vaccine recommendations (Advisory Committee on Immunization Practices) have studied the whooping cough vaccine recommended for pregnant women (called Tdap vaccine). They have concluded that it is very safe for pregnant women and their babies. These experts carefully reviewed the available safety data before recommending that women get the vaccine during every pregnancy. See the publications page for a list of published safety studies.
- Vaccine Adverse Event Reporting System
The Vaccine Adverse Event Reporting System (VAERS), a national vaccine safety surveillance program, receives information from the public about possible side effects from various vaccines. CDC and the Food and Drug Administration (FDA) monitor VAERS to look for new safety concerns or trends (also called safety signals) after Tdap vaccination. Published studies that include VAERS data support the safe use of Tdap vaccine during pregnancy. To date, VAERS has not found any safety signals among pregnant women or their babies after Tdap vaccination. - Manufacturer Pregnancy Registries
Both manufacturers of Tdap vaccine (Sanofi Pasteur for Adacel® and GlaxoSmithKline for Boostrix®) created pregnancy registries to collect information from pregnant women who got Tdap vaccine.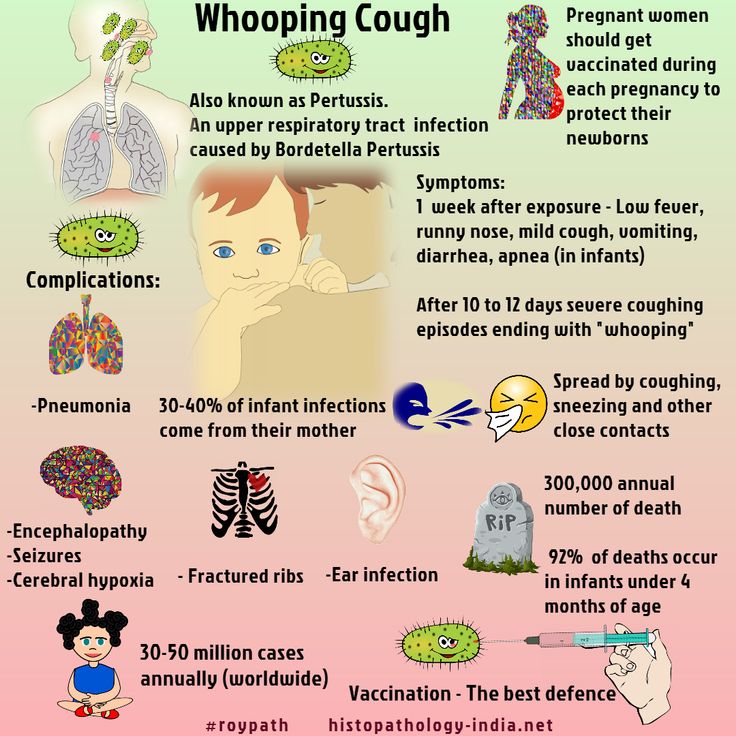 The manufacturers have not reported any safety signals to FDA.
The manufacturers have not reported any safety signals to FDA. - Safety History for Tetanus and Diphtheria Vaccines
Tdap vaccine combines protection against tetanus and diphtheria, in addition to whooping cough. Vaccines that protect against tetanus and diphtheria are commonly associated with local reactions, such as redness, swelling, pain, and tenderness where the shot is given. Pregnant women have been getting both tetanus and diphtheria toxoids (Td) and tetanus toxoid (TT) vaccines worldwide since the 1960s to prevent tetanus among newborns. This long history provides researchers a lot of data to understand their safety. Getting tetanus vaccine during pregnancy is very safe for you and your baby.
Top of Page
You may experience side effects from the Tdap vaccine
Most side effects are mild, meaning they do not affect daily activities. They also get better on their own in a few days. The most common side effects from the Tdap vaccine include
- Redness, swelling, pain, and tenderness where you got the shot
- Body-ache
- Fatigue
- Fever
In adults who have received 2 doses of the Tdap vaccine, the most commonly reported side effect was pain where they got the shot.
Severe side effects are extremely rare, especially in adults.
There is a low risk of severe side effects from multiple Tdap doses
The Tdap vaccine combines protection against tetanus and diphtheria, in addition to whooping cough. Researchers have done studies on tetanus vaccines that do not contain protection against pertussis. These studies found that adults who receive 2 tetanus shots in a short time period (within 2 years) were no more likely than adults getting their first Tdap vaccine to have severe side effects. CDC and the American College of Obstetricians and Gynecologists consider the benefits of Tdap vaccination in multiple pregnancies to outweigh theoretical (potential) risks.
Studies looked at the safety of giving multiple Tdap doses because there is a theoretical risk for severe local reactions (called hypersensitivity) if the tetanus component of the vaccine is given too often. An example of severe hypersensitivity would be the arm swelling from the shoulder to the elbow within 4 to 12 hours of getting the shot (the swelling goes away within 4 to 7 days). Manufacturers now make these vaccines with lower doses of the tetanus component than tetanus vaccines in the past. Experts believe this change likely reduced the risk of severe local reactions.
Manufacturers now make these vaccines with lower doses of the tetanus component than tetanus vaccines in the past. Experts believe this change likely reduced the risk of severe local reactions.
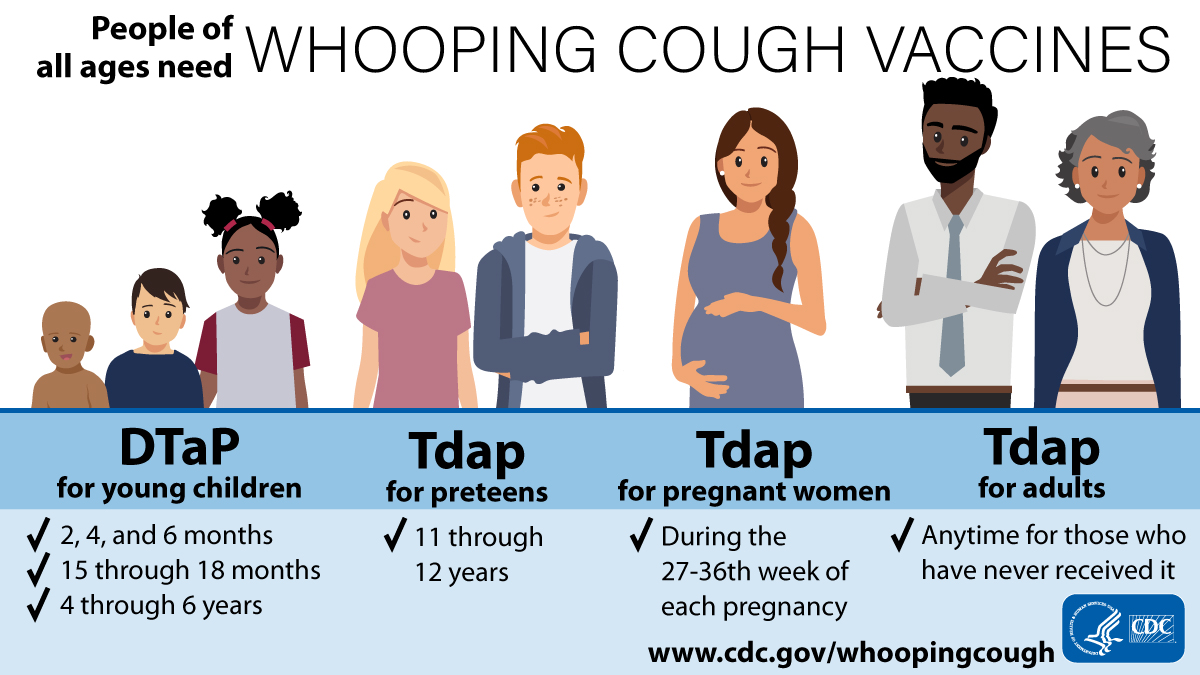
The whooping cough vaccine for children is very safe for your baby
DTaP is the name of the whooping cough vaccine for children (2 months through 6 years). The DTaP vaccine combines protection against diphtheria, tetanus and whooping cough. Currently, there are 3 licensed formulations of the DTaP vaccine. Researchers conducted many different clinical trials on each vaccine to make sure of its safety. Results from clinical trials showed that these vaccines are very safe for infants and children. Doctors can safely give the DTaP vaccine at the same time as other vaccines.
Top of Page
Your baby may experience side effects from the DTaP vaccine
The most common side effects from the DTaP vaccine include:
- Fever (up to about 1 out of 4 children)
- Redness or swelling where the shot was given (up to about 1 out of 4 children)
- Soreness or tenderness where the shot was given (up to about 1 out of 4 children)
These problems occur more often after the 4th and 5th doses of the DTaP series than after earlier doses. Some children get swelling of the entire arm or leg in which the shot was given (up to about 1 out of 30 children) following the 4th or 5th dose of DTaP vaccine. If swelling occurs, it generally lasts for 1 to 7 days after the shot is given.
Some children get swelling of the entire arm or leg in which the shot was given (up to about 1 out of 30 children) following the 4th or 5th dose of DTaP vaccine. If swelling occurs, it generally lasts for 1 to 7 days after the shot is given.
Other mild problems include:
- Fussiness (up to about 1 out of 3 children)
- Tiredness or poor appetite (up to about 1 out of 10 children)
- Vomiting (up to about 1 out of 50 children)
These problems generally occur 1 to 3 days after the shot is given.
Severe side effects are extremely rare. Learn more about side effects of the DTaP vaccine.
You cannot get whooping cough from whooping cough vaccines
Whooping cough vaccines cannot give you whooping cough since they do not contain any live bacteria. The whooping cough vaccines we use today for children and adults in the United States contain purified, inactivated parts of the bacterium that causes whooping cough (Bordetella pertussis).
Learn more about different types of vaccines and which CDC recommends for pregnant women.
Top of Page
Breastfeeding is safe after getting the whooping cough vaccine
Getting the whooping cough vaccine while breastfeeding is very safe for you and your baby. You can and should get the whooping cough vaccine if you plan to breastfeed or are currently breastfeeding. There are, however, some vaccines that CDC does not recommend for you to get while breastfeeding.
Learn more about breastfeeding.
You can safely get the whooping cough and flu vaccine at the same time
You can get the whooping cough and flu vaccines at the same time during your pregnancy. You can also get them at different visits. If you are pregnant during flu season, you should get the flu vaccine by the end of October, if possible. But you can get the flu vaccine at any point during pregnancy. You do not have to wait until later in your pregnancy for the flu shot, like CDC recommends for the whooping cough vaccine.
You can safely get the Tdap vaccine even if you recently got a tetanus shot
It does not matter when you got your last tetanus shot (Td or Tdap vaccine) — you still need the Tdap vaccine during each pregnancy.
Whooping cough vaccines do not contain thimerosal
None of the whooping cough vaccines (Tdap and DTaP) currently used in the United States contain thimerosal.
Top of Page
Whooping cough vaccination in pregnancy
Whooping cough (pertussis) rates have risen sharply in recent years and babies who are too young to start their vaccinations are at greatest risk.
Young babies with whooping cough are often very unwell and most will be admitted to hospital because of their illness. When whooping cough is particularly severe, they can die.
Pregnant women can help protect their babies by getting vaccinated – ideally from 16 weeks up to 32 weeks pregnant. If for any reason you miss having the vaccine, you can still have it up until you go into labour.
Why are pregnant women advised to have the vaccine?
Getting vaccinated while you're pregnant is highly effective in protecting your baby from developing whooping cough in the first few weeks of their life.
The immunity you get from the vaccine will pass to your baby through the placenta and provide passive protection for them until they are old enough to be routinely vaccinated against whooping cough at 8 weeks old.
When should I have the whooping cough vaccine?
The best time to get vaccinated to protect your baby is from 16 weeks up to 32 weeks of pregnancy. This maximises the chance that your baby will be protected from birth, through the transfer of your antibodies before he or she is born.
If for any reason you miss having the vaccine, you can still have it up until you go into labour. However, this is not ideal, as your baby is less likely to get protection from you. At this stage of pregnancy, having the vaccination may not directly protect your baby, but would help protect you from whooping cough and from passing it on to your baby.
Is the vaccine safe in pregnancy?
It's understandable that you might have concerns about the safety of having a vaccine during pregnancy, but there's no evidence to suggest that the whooping cough vaccine is unsafe for you or your unborn baby.
Pertussis-containing vaccine (whooping cough vaccine) has been used routinely in pregnant women in the UK since October 2012, and the Medicines and Healthcare products Regulatory Agency (MHRA) is carefully monitoring its safety. The MHRA's study of around 20,000 vaccinated women has found no evidence of risks to pregnancy or babies.
To date, around 69% of eligible pregnant women have received the whooping cough vaccine with no safety concerns being identified in the baby or mother.
A number of other countries, including the US, Argentina, Belgium, Spain, Australia and New Zealand, currently recommend vaccination against whooping cough in pregnancy.
Is whooping cough vaccination in pregnancy working?
Yes, it is. Published research from the UK vaccination programme shows that vaccinating pregnant women against whooping cough has been highly effective in protecting young babies until they can have their first vaccination when they are 8 weeks old.
Published research from the UK vaccination programme shows that vaccinating pregnant women against whooping cough has been highly effective in protecting young babies until they can have their first vaccination when they are 8 weeks old.
Babies born to women vaccinated at least a week before birth had a 91% reduced risk of becoming ill with whooping cough in their first weeks of life, compared to babies whose mothers had not been vaccinated.
An additional benefit is that the protection the mother receives from the vaccination will lower her own risk of infection and of passing whooping cough on to her baby.
Which whooping cough vaccine will I be given?
As there is no whooping cough-only vaccine, the vaccine you'll be given also protects against polio, diphtheria and tetanus. The vaccine is called Boostrix IPV.
Boostrix IPV is similar to the 4-in-1 vaccine – the pre-school booster that's routinely given to children before they start school.
You can read the manufacturer's patient information leaflet for Boostrix IPV (PDF, 91kb).
The manufacturer's leaflet says there's no information on the use of Boostrix IPV in pregnancy. Should it be used in pregnancy?
The licence for Boostrix IPV allows for its use in pregnancy when clearly needed, and when the possible benefits outweigh the possible risks.
It is standard practice with most medicines not to test them on pregnant women. This is why the manufacturer's information leaflet includes this statement, and not because of any specific safety concerns or evidence of harm in pregnancy.
Whooping cough-containing vaccine has been used routinely in pregnant women in the UK since October 2012, and the Medicines and Healthcare products Regulatory Agency (MHRA) is carefully monitoring its safety. The MHRA's study of around 20,000 women vaccinated with Repevax, the whooping cough vaccine previously offered to pregnant women, found no evidence of risks to pregnancy or pregnancy outcome.
Boostrix (similar to Boostrix IPV, but without the polio component) is one of the vaccines routinely recommended in the US for immunisation of pregnant women. There have been no reported safety concerns in the US with the use of the vaccine in pregnancy.
There is no evidence of risk to the pregnant woman or unborn child with inactivated vaccines like Boostrix IPV. An inactivated vaccine is one that does not contain "live" vaccine.
Read more about why vaccines are safe and important.
What are the side effects of the whooping cough vaccine?
You may have some mild side effects such as swelling, redness or tenderness where the vaccine is injected in your upper arm, just as you would with any vaccine. These only last a few days. Other side effects can include fever, irritation at the injection site, swelling of the vaccinated arm, loss of appetite, irritability and headache. Serious side effects are extremely rare.
What is whooping cough?
Whooping cough (medically known as pertussis) is a serious infection that causes long bouts of coughing and choking, making it hard to breathe.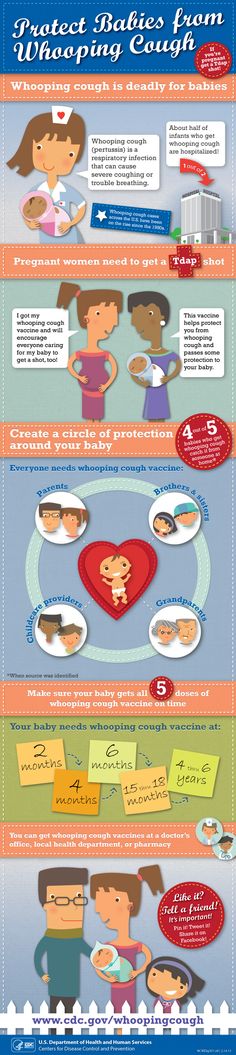 The "whoop" is caused by gasping for breath after each bout of coughing, though babies do not always make this noise.
The "whoop" is caused by gasping for breath after each bout of coughing, though babies do not always make this noise.
Read more about whooping cough symptoms.
Should I be concerned about whooping cough?
Whooping cough is a highly infectious, serious illness that can lead to pneumonia and brain damage, particularly in young babies. Most babies with whooping cough will need hospital treatment, and when whooping cough is very severe they may die.
Research from the vaccination programme in England shows that vaccinating pregnant women against whooping cough has been highly effective in protecting young babies until they can receive their own vaccinations from 8 weeks of age.
In keeping with usual disease patterns, which see cases increasing every 3 to 4 years in England, whooping cough cases have fallen in all age groups since 2012. The greatest fall has been in young babies targeted by the pregnancy vaccination programme.
Cases of whooping cough in older age groups are still high compared to pre-2012 levels.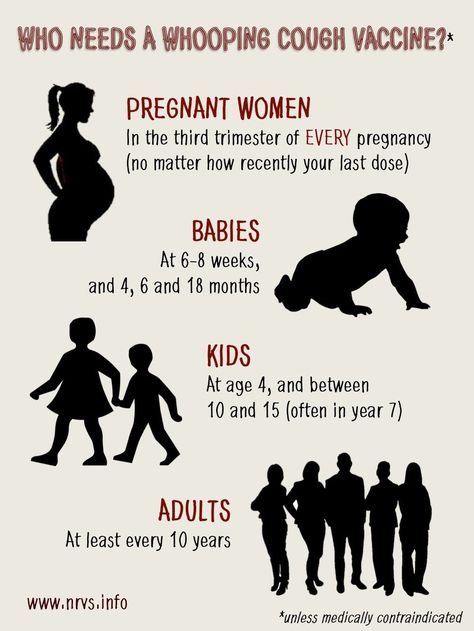 The number of cases was particularly high in 2016, in line with the typical 3- to 4-yearly peak in disease rates.
The number of cases was particularly high in 2016, in line with the typical 3- to 4-yearly peak in disease rates.
Babies can be infected by people with whooping cough in these older age groups, so it is still important for pregnant women to be vaccinated to protect their babies.
But are babies not vaccinated against whooping cough to protect them?
Yes, they are, but the babies that have been getting whooping cough are generally too young to have started their normal vaccinations, so they are not protected against the disease.
So, how can I protect my baby?
The only way you can help protect your baby from getting whooping cough in their first few weeks after birth is by having the whooping cough vaccination yourself while you are pregnant.
After vaccination, your body produces antibodies to protect against whooping cough. You will then pass some immunity to your unborn baby.
Will the whooping cough vaccine in pregnancy give me whooping cough?
No. The whooping cough vaccine is not a "live" vaccine. This means it does not contain whooping cough (or polio, diphtheria or tetanus), and cannot cause whooping cough in you, or in your baby.
The whooping cough vaccine is not a "live" vaccine. This means it does not contain whooping cough (or polio, diphtheria or tetanus), and cannot cause whooping cough in you, or in your baby.
Will my baby still need to be vaccinated at 8 weeks if I've had the vaccine while pregnant?
Yes. Whenever you have the whooping cough vaccine, your baby will still need to be vaccinated according to the normal NHS vaccination schedule when they reach 8 weeks old. Babies are protected against whooping cough by the 6-in-1 vaccine.
Can I have the whooping cough vaccine at the same time as the flu jab?
Yes, you can have the whooping cough vaccine when you get the flu vaccine, but do not delay your flu jab so that you can have both at the same time.
How can I get the whooping cough vaccination?
The vaccine is available from your GP, though some antenatal clinics also offer it. You may be offered the vaccination at a routine antenatal appointment from around 16 weeks of your pregnancy.
If you are more than 16 weeks pregnant and have not been offered the vaccine, talk to your midwife or GP and make an appointment to get vaccinated.
I was vaccinated against whooping cough as a child, do I need to get vaccinated again?
Yes, because any protection you may have had through either having whooping cough or being vaccinated when you were young is likely to have worn off and will not provide sufficient protection for your baby.
I was vaccinated against whooping cough in a previous pregnancy, do I need to be vaccinated again?
Yes, you should get re-vaccinated from 16 weeks in each pregnancy to maximise protection for your baby.
How do I spot whooping cough in my baby?
Be alert to the signs and symptoms of whooping cough, which include severe coughing fits that may be accompanied by difficulty breathing (or pauses in breathing in young infants) or vomiting after coughing, and the characteristic "whoop" sound.
If you are worried your baby may have whooping cough, contact your doctor immediately.
Read more about whooping cough vaccination in the leaflet Whooping cough and pregnancy (PDF, 183kb) from Public Health England.
Fomin's clinic - a network of multidisciplinary clinics
You probably know that in the modern world there is a fierce struggle. And this is not about military conflicts or political strife, but about clashes between supporters of vaccination and anti-vaccinationists who claim that vaccination is a real universal evil that causes irreparable consequences - pathologies and disorders. Nevertheless, pregnant women and newborns are the most vulnerable groups, which can be taken care of by timely vaccination.
What diseases should a pregnant woman be vaccinated against?
Pregnancy is stressful for the body, and therefore it functions differently than before or after it. It is because of a weakened immune system that the risk of severe influenza in pregnant women is much higher than in non-pregnant women. Influenza can not only cause premature birth, but also harm the health of the unborn baby.
Influenza can not only cause premature birth, but also harm the health of the unborn baby.
Influenza vaccination is strongly recommended by all world medical organizations (including the well-known World Health Organization). There are controversial opinions about vaccination in the first trimester, therefore, if it does not fall in autumn or winter - the most dangerous months for the active spread of the disease, it is better to get vaccinated in the II-III trimester.
Get vaccinated
When you get vaccinated against influenza, it primarily has a preventive effect directly for you - the expectant mother, but the whooping cough vaccine is about taking care of the baby's health. The woman who received the vaccine will pass antibodies to the child in utero - and this will save him from the disease in the first months of life, because for the newborn it can be fatal.
Whooping cough is difficult to recognize immediately, because it does not always manifest itself with a characteristic cough - at one moment breathing can simply stop, although there were no visible symptoms. For your baby's safety, you should get the whooping cough vaccine (along with diphtheria and tetanus) during every pregnancy - best done in the third trimester.
For your baby's safety, you should get the whooping cough vaccine (along with diphtheria and tetanus) during every pregnancy - best done in the third trimester.
No, not dangerous.
There is a myth that you can get the flu after vaccination. It is impossible to catch the flu from a vaccine, since the vaccine does not contain the whole virus, but only its parts - antigens. Antibodies are produced against these antigens, our defending cells. And the next time our body encounters a virus, already real, our antibodies will actively destroy the viral particles.
Many people do not consider it necessary to get vaccinated because they think that the vaccine protects against only a few strains of influenza, and there are many. But every year the vaccine contains precisely the actual strains for this season and this territory. So mass vaccination forms a stable herd immunity. Immunity after vaccination lasts for a year, so the flu shot is annual.
In some cases, pregnant women need additional vaccinations:
Vaccination against hepatitis B. The immunobiological preparation does not contain live or whole virus. According to medical research and statistics, this hepatitis shot is safe for a child. However, the vaccine is recommended for expectant mothers who are at risk of infection with this type of hepatitis (for example, if a loved one is infected). If the likelihood of the disease increases, then the pregnant woman is given emergency vaccination and a specific immunoglobulin is administered.
The immunobiological preparation does not contain live or whole virus. According to medical research and statistics, this hepatitis shot is safe for a child. However, the vaccine is recommended for expectant mothers who are at risk of infection with this type of hepatitis (for example, if a loved one is infected). If the likelihood of the disease increases, then the pregnant woman is given emergency vaccination and a specific immunoglobulin is administered.
Vaccination against hepatitis A. Hepatitis A can be contracted through contact with objects that contain the virus, after drinking contaminated water or food. The immunobiological preparation contains an inactivated virus, and therefore the likelihood of its negative effect on the fetus is minimal. Vaccination is carried out if the risk of infection increases. This is possible if a pregnant woman enters a region unfavorable for hepatitis A or doctors suspect that contact with the virus has already taken place. In some cases, human normal immunoglobulin is given with the vaccine.
Rabies vaccination. Infection usually occurs after the bite of a sick animal. The rabies virus is quite strong and dangerous, with the development of the disease provokes death. It is for this reason that rabies vaccination is an urgent and necessary measure. The vaccine contains an inactivated virus, so the drug is considered safe for the fetus. If the bites and injuries are severe, then the victim is injected with a specific immunoglobulin.
Meningococcal vaccination may also be recommended by a doctor during pregnancy in the event of a meningococcal outbreak or if traveling to an area endemic for meningococcal disease.
The possibility of vaccinating a pregnant woman against pneumococcal infection may be considered by a doctor for women who have chronic respiratory diseases during the II-III trimesters of pregnancy.
Pregnant women are not vaccinated if the vaccine contains live attenuated
cultures of pathogens. These drugs include vaccines: measles, rubella, chicken pox, mumps, BCG.
In order to protect yourself and your baby from possible infectious dangers, it is necessary to get the necessary vaccinations before pregnancy.
If the risk of getting sick appeared during pregnancy (the pregnant woman was not vaccinated on time and there was contact with the patient), then specific prophylaxis is carried out with immunoglobulins.
In our clinic, also, when planning a pregnancy, it is possible to vaccinate MMR (measles, mumps, rubella vaccine) - a combined attenuated live vaccine against infections: mumps, rubella and measles.
Follow us
Vaccination of pregnant women
When planning a pregnancy, you need to review the vaccination history of the expectant mother. If not, tests to determine the level of protective antibodies are necessary. Based on the vaccination history and test results, the doctor will prescribe the necessary immunizations before pregnancy. If you need measles, mumps, rubella, or chickenpox vaccines, be sure to get them at least 1 month before pregnancyRecommended vaccines during pregnancy
The CDC (US Centers for Disease Control and Prevention) recommends that all pregnant women receive the inactivated influenza vaccine at any time during pregnancy and the pertussis vaccine (Tdap Adacel) at the beginning of the third trimester during each pregnancy.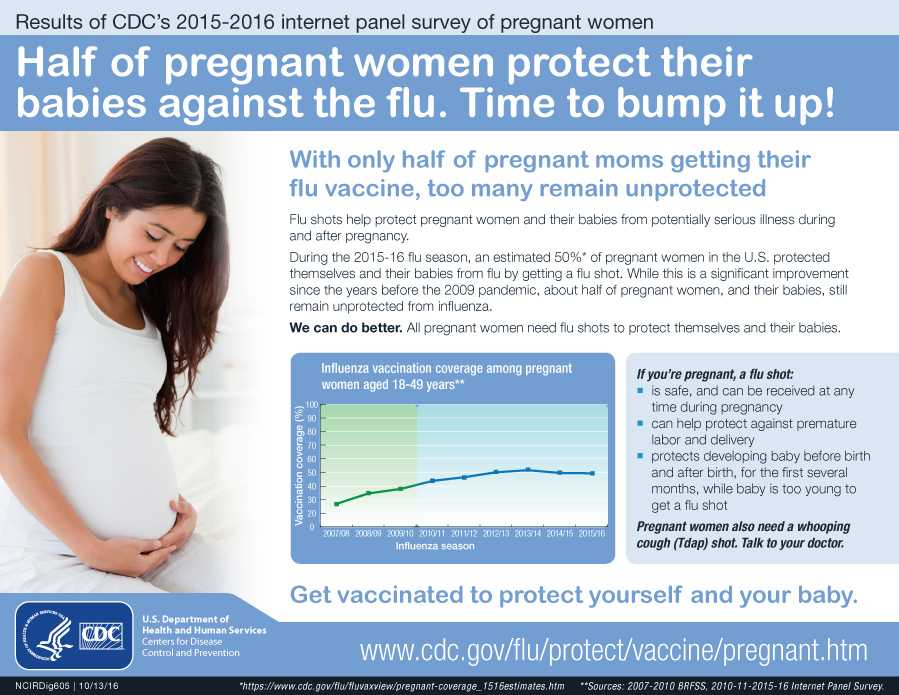 The flu and whooping cough can be fatal, especially in the first few months of a child's life. Vaccinating women against these diseases during each pregnancy helps protect both themselves and their babies. Studies show flu and whooping cough vaccines are safe for pregnant women and developing children
The flu and whooping cough can be fatal, especially in the first few months of a child's life. Vaccinating women against these diseases during each pregnancy helps protect both themselves and their babies. Studies show flu and whooping cough vaccines are safe for pregnant women and developing children Vaccination of pregnant women in special cases
The decision to vaccinate in special cases is made by the attending physician and the pregnant woman based on an assessment of the likelihood of infection and the risk to the mother and fetus from both the disease and vaccination. This should be guided by international recommendations on immunization of pregnant women (for example, the Advisory Committee on Immunization Practices)Basic information on vaccination of pregnant women under special conditions
Hepatitis A Data on the safety of vaccination during pregnancy have not been established. The theoretical risk to the fetus is low, it is necessary to compare the risk of vaccination and the risk of infection (it is necessary to discuss with your doctor if you are at risk)Hepatitis B
There is limited data on the safety of hepatitis B vaccination during pregnancy. If there is a risk of infection during pregnancy, vaccination is necessary (need to discuss with your doctor if you are at risk)
If there is a risk of infection during pregnancy, vaccination is necessary (need to discuss with your doctor if you are at risk) Human papillomavirus (HPV)
HPV vaccines are not recommended for pregnant women. However, if the vaccine dose was administered during pregnancy, no intervention is required. Next, the series of vaccines should be postponed until the end of pregnancy.Measles, mumps, rubella
Vaccines should not be given to women who are pregnant or trying to become pregnant. Pregnancy should also be avoided for 28 days after vaccinationMeningococcal disease
There is limited data on the safety of meningococcal vaccination during pregnancy. Pregnant women who are at risk of infection during pregnancy may be vaccinated (need to discuss with your doctor if you are at risk)Pneumococcal infection
There is limited data on the safety of pneumococcal vaccine (PPSV23) during the second and third trimesters of pregnancy.
 Pregnant women who are at risk may be vaccinated (need to discuss with your doctor if you are at risk). There are no recommendations for the use of pneumococcal conjugate vaccine (PCV13) in pregnant women.
Pregnant women who are at risk may be vaccinated (need to discuss with your doctor if you are at risk). There are no recommendations for the use of pneumococcal conjugate vaccine (PCV13) in pregnant women. Hemophilus vaccination
There is limited data on the safety of Haemophilus influenzae vaccination during the third trimester of pregnancy. Pregnant women who are at risk may be vaccinated (need to discuss with your doctor if you are at risk)Poliomyelitis (IPV/OPV) In theory, vaccination of pregnant women should be avoided, although no side effects of IPV have been reported in pregnant women and their fetuses. If there is an increased risk of infection and immediate protection against polio is needed, IPV can be given according to the recommended schedules for adults (need to discuss with your doctor if you are at risk)
Chickenpox
Chickenpox vaccines should not be given to women who are pregnant or trying to get pregnantYellow fever
Live yellow fever vaccine is not contraindicated during pregnancy.