Baby average body temperature
Fever (0-12 Months)
Is this your child's symptom?
- An abnormal high body temperature
- Fever is the only symptom. Your child has a true fever if:
- Rectal (bottom), Ear or Forehead temperature: 100.4° F (38.0° C) or higher
- Under the arm (armpit) temperature: 99° F (37.2° C) or higher
- Caution: Ear temperatures are not accurate before 6 months of age
- Caution: Forehead temperatures must be digital. Forehead strips are not accurate.
Causes of Fever
- Overview. Almost all fevers are caused by a new infection. Viruses cause 10 times more infections than bacteria. The number of germs that cause an infection are in the hundreds. Only a few common ones will be listed.
- Viral Infections. Colds, flu and other viral infections are the most common cause. Fever may be the only symptom for the first 24 hours. The start of viral symptoms (runny nose, cough, loose stools) is often delayed.
Roseola is the most extreme example. Fever may be the only symptom for 3 to 5 days. Then a rash appears.
- Bacterial Infections. A bladder infection is the most common cause of silent fever in girls.
- Vaccine Fever. Fever with most vaccines begins within 12 hours. It lasts 2 to 3 days. This is normal and harmless. It means the vaccine is working.
- Newborn Fever (Serious). Fever that occurs during the first 3 months of life can be serious. All of these babies need to be seen as soon as possible. The fever may be due to sepsis (a bloodstream infection). Bacterial infections in this age group can get worse quickly. They need rapid treatment.
- Meningitis (Very Serious). A bacterial infection of the membrane that covers the spinal cord and brain. The main symptoms are a stiff neck, headache and confusion. Younger children are lethargic or so irritable that they can't be consoled. If not treated early, can suffer brain damage.
- Overheated. The fever is usually low grade. Can occur during heat waves or from being overdressed. The temp becomes normal in a few hours after moving to a cooler place. Fever goes away quickly with rest and drinking extra fluids.
- Not Due to Teething. Research shows that "getting teeth" does not cause fevers.
Fever and Crying
- Fever on its own shouldn't cause much crying.
- Frequent crying in a child with fever is caused by pain until proven otherwise.
- Hidden causes can be ear infections, kidney infections, sore throats and meningitis.
Normal Temperature Range
- Rectal. A reading of 98.6° F (37° C) is just the average rectal temp. A normal low can be 96.8° F (36° C) in the morning. It can change to a high of 100.3° F (37.9° C) late in the day. This is a normal range.
When to Call for Fever (0-12 Months)
Call 911 Now
- Not moving
- Can't wake up
- Severe trouble breathing (struggling for each breath; can barely speak or cry)
- Purple or blood-colored spots or dots on skin
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Trouble breathing, but not severe
- Great trouble swallowing fluids or spit
- Fever in baby less than 12 weeks old.
 Caution: Do NOT give your baby any fever medicine before being seen.
Caution: Do NOT give your baby any fever medicine before being seen. - Fever over 104° F (40° C)
- Shaking chills (shivering) lasting more than 30 minutes
- Nonstop crying or cries when touched or moved
- Won't move an arm or leg normally
- Dehydration suspected. No urine in over 8 hours, dark urine, very dry mouth and no tears.
- Weak immune system. Examples are sickle cell disease, HIV, cancer, organ transplant, taking oral steroids.
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Contact Doctor Within 24 Hours
- Age 3-6 months old with fever
- Age 6-12 months old with fever that lasts more than 24 hours. There are no other symptoms (such as cough or diarrhea).
- Fever lasts more than 3 days
- Fever returns after gone for more than 24 hours
- You think your child needs to be seen, but the problem is not urgent
Contact Doctor During Office Hours
- You have other questions or concerns
Self Care at Home
- Fever with no other symptoms and your child acts mildly ill
Seattle Children's Urgent Care Locations
If your child’s illness or injury is life-threatening, call 911.
- Bellevue
- Everett
- Federal Way
- Seattle
Care Advice for Fever
- What You Should Know About Fever:
- Having a fever means your child has a new infection.
- It's most likely caused by a virus.
- You may not know the cause of the fever until other symptoms develop. This may take 24 hours.
- For infants more than 3 months old, most fevers are good for sick children. They help the body fight infection.

- Use the ranges below to help put your child's level of fever into perspective:
- 100° - 102° F (37.8° - 39° C) Low grade fever: helpful, good range. Don't treat.
- 102° - 104° F (39 - 40° C) Average fever: helpful. Treat if causes discomfort.
- Over 104° F (40° C) High fever: causes discomfort, but harmless. Always treat.
- Over 106° F (41.1° C) Very high fever: important to bring it down. Rare to go this high.
- Over 108° F (42.3° C) Dangerous fever: fever itself can be harmful.
- Treatment for All Fevers - Extra Fluids:
- Fluids alone can lower the fever. Reason: being well hydrated helps the body give off heat through the skin.
- For shivering (or the chills), give your child a blanket. Make them comfortable.
- Offer your child extra water or other fluids by mouth. Cold fluids are better. Until 6 months old, only give extra formula or breastmilk.
- For all children, dress in 1 layer of light weight clothing, unless shivering.
 Reason: also helps heat loss from the skin.
Reason: also helps heat loss from the skin. - For shivering (or the chills), give your child a blanket. Make them comfortable.
- Caution: if a baby under 1 year has a fever, never overdress or bundle up. Reason: Babies can get over-heated more easily than older children.
- Fever Medicine:
- Caution: Do not give a baby under 3 months any fever medicine. Most of these babies will need to be seen.
- For fevers 100°-102° F (37.8° - 39°C), fever meds are not needed. Reason: fevers in this range help the body fight the infection. Fevers turn on the body's imune system. Fevers don't cause any discomfort. Fever meds are mainly needed for fevers higher than 102° F (39° C).
- Give an acetaminophen product (such as Tylenol).
- Another choice is an ibuprofen product (such as Advil) if over 6 months old.
- Goal of treatment: keep the fever at a helpful level. Most often, the fever meds lower the fever by 2° to 3° F (1 - 1.
 5° C). They do not bring it down to normal. It takes 1 or 2 hours to see the effect.
5° C). They do not bring it down to normal. It takes 1 or 2 hours to see the effect. - Do not use aspirin. Reason: Risk of Reye syndrome, a rare but serious brain disease.
- Do not use both acetaminophen and ibuprofen together. Reason: Not needed and a risk of giving too much.
- Pain: fever does not cause pain. If your child also has pain, it's from the infection. It may be a sore throat or muscle pain. Treat the pain, if it's more than mild.
- Return to Child Care:
- Your child can return to child care after the fever is gone. Your child should feel well enough to join in normal activities.
- What to Expect:
- Most fevers with viral illnesses range between 101° and 104° F (38.4° and 40° C).
- They may last for 2 or 3 days.
- They are not harmful.
- Call Your Doctor If:
- Your child looks or acts very sick
- Any serious symptoms occur such as trouble breathing
- Fever goes above 104° F (40° C)
- Any fever occurs if less than 12 weeks old
- Fever without other symptoms lasts more than 24 hours
- Fever lasts more than 3 days (72 hours)
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.

Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Last Reviewed: 10/20/2022
Last Revised: 09/18/2022
Copyright 2000-2022 Schmitt Pediatric Guidelines LLC.
Normal Body Temperature: Babies, Kids, Adults
You may have heard that the “normal” body temperature is 98.6°F (37°C). But this number is only an average. Your body temperature may be slightly higher or lower.
A body temperature reading above or below the average doesn’t automatically mean you’re sick. Several factors can influence your body temperature, including your age, sex, time of day, and activity level.
Read on to learn more about healthy body temperature ranges for babies, kids, adults, and older adults.
Your body’s ability to regulate temperature changes as you get older.
People over the age of 64 generally have more trouble adjusting to sudden changes in temperature as quickly as younger people. In general, older people have more difficulty conserving heat. They’re also more likely to have lower body temperatures.
In general, older people have more difficulty conserving heat. They’re also more likely to have lower body temperatures.
Below are average body temperatures based on age, according to a review of studies and older research:
| Age | Oral | Rectal/Ear | Armpit |
|---|---|---|---|
| 0–12 months | 95.8–99.3°F (36.7–37.3°C) | 96.8–100.3°F (37–37.9°C) | 94.8–98.3°F (36.4–37.3°C) |
| Children | 97.6–99.3°F (36.4–37.4°C) | 98.6–100.3°F (37–37.9°C) | 96.6–98.3°F (35.9–36.83°C) |
| Adults | 96–98°F (35.6–36.7°C) | 97–99°F (36.1–37.2°C) | 95–97°F (35–36.1°C) |
| Adults over age 65 | 93–98.6°F (33.9–37°C) | 94–99.6°F (34.4–37.6°C) | 92–97.6°F (33.3–36.4°C) |
Identifying your normal range can make it easier to know when you have a fever.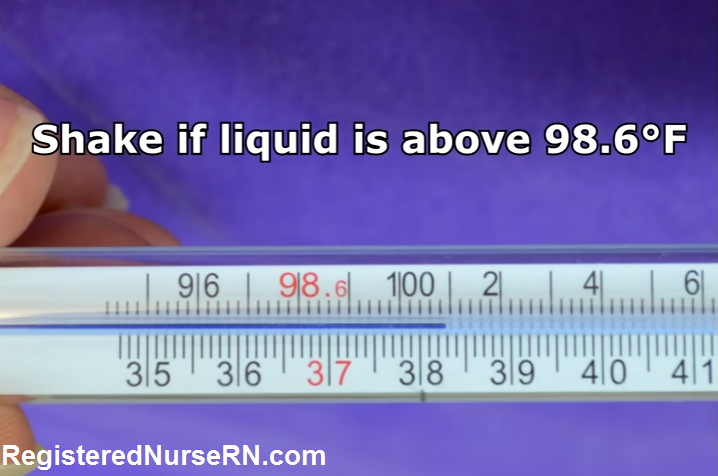
Keep in mind that average body temperature varies from person to person. Your body temperature might be up to 1°F (0.6°C) higher or lower than the guidelines above.
There are four different ways to take your or a family member’s temperature. However, the reading can vary from one method to the next.
The chart below shows which method is recommended for each age group:
| Age | Rectal | Temporal (forehead) | Oral | Tympanic (ear) |
|---|---|---|---|---|
| Under 3 months | X | |||
| 3–6 months | X | X | ||
| 6 months–3 years | X | X | X | |
| 4 years–teens | X | X | X | |
| Adults | X | X | X | |
| Older adults | X | X | X |
You may have had your temperature checked under your arm, in the armpit. This method isn’t as accurate and not recommended.
This method isn’t as accurate and not recommended.
German doctor Carl Wunderlich identified the average body temperature of 98.6°F (37°C) during the 19th century. However, many studies have since determined that that isn’t always the case.
A 2019 study found that the average body temperature is 97.86°F (36.59°C). That’s a little lower than initially thought so many years ago.
However, it’s best to take this information with a grain of salt since no single number defines your average body temperature. Instead, it’s best to look at a temperature range that may be higher or lower than the average.
Here are some of the factors that affect body temperature:
- Our bodies tend to warm up throughout the day.
- Older adults have lower body temperatures since our ability to regulate body temperature lessens as we age.
- Younger people have higher body temperatures.
- The level of physical activity affects temperature because the more you move your body, the warmer your core body becomes.

- Hotter and colder weather can also mirror your body temperature — it rises when in a warm environment and lowers in the cold.
- Temperature readings from the armpit are lower than the thermometer read from the mouth.
- Thermometer readings from the mouth are lower than if taken in the ear or rectum.
- Hormone levels can affect body temperature.
- Excess weight can also be associated with lower body temperatures.
A higher-than-normal thermometer reading can be a sign of a fever.
The American College of Critical Care Medicine identifies a temperature of 100.9°F (38.3°C) or higher as a fever. As mentioned previously, the exact reading is dependent upon a few factors. If your temperature’s elevated above the normal range described earlier in the article, you may have a fever.
In general, a reading that’s 2°F (1.1°C) above your normal temperature is usually a sign of a fever.
Fevers can be accompanied by other signs and symptoms, including:
- sweating or feeling flushed
- chills
- aches and pains
- headache
- lack of appetite
- dehydration
- weakness or lack of energy
Our bodies have a built-in temperature control system. This operation raises the body temperature in response to disease and infection that you can sometimes fight without any intervention. With time and rest, your body temperature will likely return to normal without treatment.
This operation raises the body temperature in response to disease and infection that you can sometimes fight without any intervention. With time and rest, your body temperature will likely return to normal without treatment.
When should I call my doctor if I have a fever?
On many occasions, a fever will go away on its own without treatment. However, you’ll want to seek medical advice if you have a fever and any of the following:
- trouble breathing
- skin rash
- persistant cough
- confusion or sleepiness
- unexplained bleeding or bruising
- persistent diarrhea, vomiting, or both
- headache with stiff neck
- feeling unwell
- fever that has lasted for more than 2 days
With babies and younger children, it can be hard to know when to speak with a doctor. Call your pediatrician if:
- your baby is less than 3 months old and has a fever.
- your baby is between 3 months and 3 years old and has a temperature of 102°F (38.
 9°C).
9°C). - your child is 3 years or older and has a temperature of 103°F (39.4°C).
Seek medical care if your baby or child has a fever and:
- has difficulty breathing
- struggles to drink liquids
- is under 3 months old
- has a temperature over 104°F (40°C)
- is shivering for more than 30 minutes
- is inconsolable, especially when touched or moved
- is unable to move an arm or leg as normal
- appears dehydrated by low urine amounts, dry mouth, and no tears with crying
- has pain with urination
- appears very ill
If you feel your child should be seen by a medical professional, then trust your gut and have them checked out.
Hypothermia is a serious condition that occurs when you lose too much body heat. For adults, a body temperature that dips below 95°F (35°C) is a sign of hypothermia.
Most people associate hypothermia with being outside in cold weather for long periods of time. But hypothermia can occur indoors, too.
Babies and older adults are more susceptible. For babies, hypothermia can occur when their body temperature is 97°F (36.1°C) or lower.
Hypothermia can also be a concern in a poorly heated house in winter or an air-conditioned room in summer.
Other signs and symptoms of hypothermia include:
- shivering
- slow, shallow breath
- slurred or mumbled speech
- a weak pulse
- poor coordination or clumsiness
- low energy or sleepiness
- confusion or memory loss
- loss of consciousness
- bright red skin that’s cold to the touch (in babies)
See a doctor if you have a low body temperature with any of the symptoms above.
A fever isn’t usually a cause for concern. The fever goes away with a few days of rest most of the time.
However, seek treatment when your fever climbs too high, lasts too long, or is accompanied by more severe symptoms.
Your doctor will ask questions about your symptoms. They might perform or order tests to determine the cause of the fever. Treating the cause of the fever can help your body temperature return to normal.
Treating the cause of the fever can help your body temperature return to normal.
On the other hand, a low body temperature can also cause concern. Hypothermia can be life threatening if left untreated. Seek medical assistance as soon as you notice signs of hypothermia.
Your doctor will use a standard clinical thermometer to diagnose hypothermia and check for physical signs. In addition, they may use a low-reading rectal thermometer if needed.
In some cases, your doctor may order a blood test to confirm the cause of your hypothermia or to check for infection.
In mild cases, hypothermia may be harder to diagnose but easier to treat. Heated blankets and warm fluids can restore heat. Other treatments include blood rewarming and warmed intravenous fluids for more severe cases.
Read this article in Spanish.
Normal values of body temperature in children, measurement of the child's body temperature
It is believed that a healthy child should have a body temperature of 36. 6 °C. And its increase over 37 degrees is regarded as a sign of illness. But it is not so.
6 °C. And its increase over 37 degrees is regarded as a sign of illness. But it is not so.
Body temperature depends on age and measurement area. It can increase after physical exertion, emotional arousal and feeding.
Devices and time for measuring body temperature
To determine the temperature, the following types of thermometers are used:
-
digital;
-
mercury;
-
infrared.
The optimal time for thermometry is 7-9 am and 17-19 pm. As prescribed by the doctor, the determination of the temperature during the day in children can be performed 3-4 times.
What temperature is considered normal for a child?
Immediately after the birth of a newborn, the temperature of his body decreases by 1-2 ° C, then within 24 hours it rises to 36-37 ° C. In the first 3 months of a baby's life, its indicators are unstable and depend on external factors: air temperature in the room, sleep, food intake. Normally, these fluctuations do not exceed 0.6 °C per day. For children of the first year of life, a temperature of 37.7 is the norm.
Normally, these fluctuations do not exceed 0.6 °C per day. For children of the first year of life, a temperature of 37.7 is the norm.
The average body temperature for a child is 37°C. Usually in the morning - 36.3 ° C, and in the evening it can rise to 37.6 ° C.
In what areas can the temperature of children be taken?
Underarm
The temperature measurement time under the arm is 5-10 minutes and depends on the type of device.
In the rectum
It is used in children under 5 years of age and in debilitated patients. For this method, it is desirable to use medical electronic thermometers with a soft tip. It will take 1-1.5 minutes to determine the rectal temperature.
Oral
The procedure is performed both under the tongue and behind the cheek. Contraindications to the use of this method are: children under 4-5 years of age, increased excitability and impaired nasal breathing. The duration of temperature measurement by the oral method is from 10 seconds to 3 minutes.
The duration of temperature measurement by the oral method is from 10 seconds to 3 minutes.
In the ear
The temperature in the ear is measured with an infrared sensor. The tip of the thermometer is inserted into the ear canal and the result appears on the display.
On forehead
Forehead temperature can be measured with a contact and non-contact thermometer. It will take 3 to 5 seconds to get the result. If the baby is sleeping or excited, then it is more convenient to use a non-contact method for measuring temperature.
Crotch
Mainly used in infants. The measurement time in the inguinal fold is 5 minutes. The method is inconvenient because the baby is not easy to keep in one position during this time.
Ranges of normal temperature in children depending on age and area of measurement are presented in the following table:
| 0-2 years | 3-10 years | 11-18 years old | |
|---|---|---|---|
| In the armpit | 34. 7 - 37.2 7 - 37.2 | 35.8 - 36.6 | 35.1 - 36.8 |
| On the forehead | 36.7 - 37.5 | 36.7 - 37.5 | 36.5 - 37.4 |
| in the ear | 36.3 - 37.7 | 36.3 - 37.7 | 36.7 - 37.8 |
Fever in children - NCCH
36.6˚ is the average normal body temperature for an adult. In children, the average body temperature is 0.3-0.4˚ C higher than in adults. In addition, the temperature in children is characterized by significant lability and its average fluctuations in newborns can be about 0.4 ° C, and in older children up to 1 ° C. Factors such as food intake, hunger, movement, restlessness, alternation of sleep and wakefulness. It must be remembered that there are daily fluctuations in temperature, in the evening it is usually slightly higher. In young children with insufficient maturity of thermoregulation processes, environmental factors have a significant impact, it is important to remember that children are very easy to both overcool and overheat, so the air temperature in the room, the quantity and quality of clothes on the child, etc. are important. If the child seemed hot to you, and you decided to measure the temperature, you must wait 15-20 minutes after sleep or physical activity, uncover the child. The temperature should not be measured in the hands of the mother, but in a calmly sitting or lying child. When measuring the temperature in the armpit, you just need to hold the child's hand with a thermometer with your hand or use an ear infrared thermometer.
are important. If the child seemed hot to you, and you decided to measure the temperature, you must wait 15-20 minutes after sleep or physical activity, uncover the child. The temperature should not be measured in the hands of the mother, but in a calmly sitting or lying child. When measuring the temperature in the armpit, you just need to hold the child's hand with a thermometer with your hand or use an ear infrared thermometer.
Fever is an increase in body temperature ≥38˚ C, in most cases it is not dangerous, it is a normal physiological reaction of the body to infectious and non-infectious diseases. In young children, febrile illnesses are common and are usually caused by viral infections.
In the body, the role of the thermoregulation center is performed by the hypothalamus, its mechanism of action is based on achieving a balance between heat production and heat loss.
Febrile convulsions are genetically determined, develop in 3-4% of children, as a rule, are not accompanied by epileptic activity of the brain, do not affect the further development of the child and do not recur after 6 years. In almost 50% of cases, febrile convulsions are single, however, if they are present in the history of the child, antipyretics are recommended for him at lower fever figures.
In almost 50% of cases, febrile convulsions are single, however, if they are present in the history of the child, antipyretics are recommended for him at lower fever figures.
Of course, one can understand the excitement of parents and grandparents when a child has a fever, but they need to remember that by lowering the temperature, especially low values, they calm themselves more than help the child. So, in most viral infections, only during an increase in temperature, antibodies to the virus and various active substances are produced that are responsible for the immune response and immunological memory. Therefore, an artificial decrease in temperature can lengthen the period of the disease. If a child has started antibiotic therapy for a bacterial infection, it is important to evaluate the effectiveness of the antibiotic, which can be seen primarily by self-reduction of body temperature. Against the background of antipyretics, this is quite difficult to do, and the sooner the child receives the correct treatment, the lower the risk of possible complications. Taking into account all of the above, international recommendations have been developed for the appointment of antipyretics. They are indicated in initially healthy children under the age of 3 months with an increase in body temperature above 38 °C. For children older than 3 months, antipyretics are prescribed at a temperature above 39-39.5˚С. For children at risk (with congenital heart defects, diseases of the central nervous system, etc.), as well as with previously identified febrile convulsions, the temperature is reduced to a lower temperature - 37.5-38 ° C. If the child feels unwell with a fever, refuses to eat and drink, parents can begin to lower the temperature to a lower temperature. No guideline for the management of children with fever recommends the use of antipyretics solely to reduce fever.
Taking into account all of the above, international recommendations have been developed for the appointment of antipyretics. They are indicated in initially healthy children under the age of 3 months with an increase in body temperature above 38 °C. For children older than 3 months, antipyretics are prescribed at a temperature above 39-39.5˚С. For children at risk (with congenital heart defects, diseases of the central nervous system, etc.), as well as with previously identified febrile convulsions, the temperature is reduced to a lower temperature - 37.5-38 ° C. If the child feels unwell with a fever, refuses to eat and drink, parents can begin to lower the temperature to a lower temperature. No guideline for the management of children with fever recommends the use of antipyretics solely to reduce fever.
Temperature reduction is carried out by physical cooling methods and, if necessary, medication. If the child does not have chills, marbling of the skin, the room should be ventilated, the child is open. With cold hands and feet, they must be rubbed to redness or given a no-shpu in order to expand the peripheral vessels for an adequate heat transfer process. The drugs of choice among antipyretics for children are paracetamol and ibuprofen with many convenient dosage forms for the child. A single dose is calculated on body weight and is 10-15 mg / kg (every 6 hours, if necessary) for paracetamol and 5-10 mg / kg (every 6 hours, if necessary) for ibuprofen. If the dose of antipyretics is insufficient, the effect of them may not be. In the presence of vomiting, the form in candles is convenient. A decrease in temperature, as a rule, can be expected 30-60 minutes after taking the drug (somewhat longer with rectal use) and the effect lasts up to 3-8 hours. If the temperature is very high, physical cooling methods can be used until the antipyretic begins to take effect or until the time of the next dose of the drug. Vinegar and vodka, when rubbed, can have both a local irritant effect and a toxic effect when absorbed through the skin.
With cold hands and feet, they must be rubbed to redness or given a no-shpu in order to expand the peripheral vessels for an adequate heat transfer process. The drugs of choice among antipyretics for children are paracetamol and ibuprofen with many convenient dosage forms for the child. A single dose is calculated on body weight and is 10-15 mg / kg (every 6 hours, if necessary) for paracetamol and 5-10 mg / kg (every 6 hours, if necessary) for ibuprofen. If the dose of antipyretics is insufficient, the effect of them may not be. In the presence of vomiting, the form in candles is convenient. A decrease in temperature, as a rule, can be expected 30-60 minutes after taking the drug (somewhat longer with rectal use) and the effect lasts up to 3-8 hours. If the temperature is very high, physical cooling methods can be used until the antipyretic begins to take effect or until the time of the next dose of the drug. Vinegar and vodka, when rubbed, can have both a local irritant effect and a toxic effect when absorbed through the skin.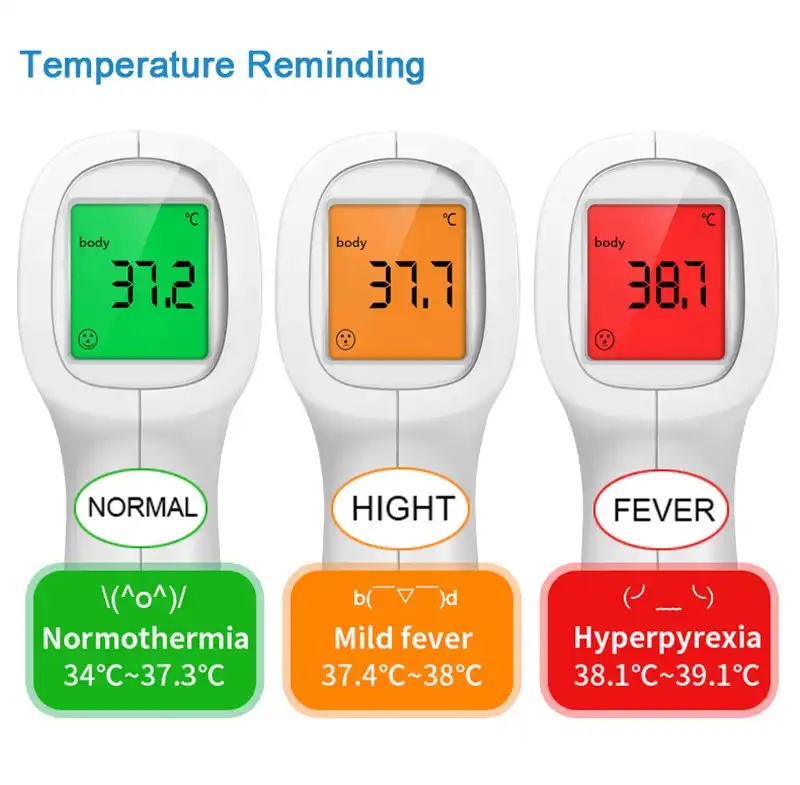 Therefore, the simplest and safest way is to wipe the child with ordinary water at 25-30˚ C. It is necessary to wipe the neck, back of the head, inguinal and axillary folds, forehead, and then other surfaces.
Therefore, the simplest and safest way is to wipe the child with ordinary water at 25-30˚ C. It is necessary to wipe the neck, back of the head, inguinal and axillary folds, forehead, and then other surfaces.
It is not recommended to alternate paracetamol and ibuprofen, as well as to give their combined preparations, this combination is no more effective than monotherapy, but is fraught with serious side effects and can lead to acute renal failure. Also, nimesulide, acetylsalicylic acid preparations are not used in children with an antipyretic purpose, and metamizole (analgin) can only be administered intramuscularly in order to quickly reduce the temperature. All of these drugs can cause serious side effects that are incomparable to their antipyretic effect.
Usually a decrease in temperature by 0.5-1˚ C is sufficient to improve the child's well-being, it is not necessary to achieve a decrease in temperature to normal numbers. Large diurnal fluctuations in temperature may have a more significant negative effect than the fever itself.
We have already said above that fever in children is most often accompanied by acute infectious diseases, which can be both viral and bacterial etiology. In the vast majority of cases, a viral infection does not require the appointment of an antibiotic (antibiotics do not act on viruses), children are treated with symptomatic agents and, if necessary, reduce the temperature. In the case of a proven bacterial etiology of the disease, it is necessary to prescribe antibiotic therapy. It is up to the doctor to decide what exactly the child is sick with, and, accordingly, how to treat him. However, if the disease begins with fever, runny nose and cough, the child's condition suffers slightly, with a high degree of probability one can think about the development of a respiratory viral infection and treat the child symptomatically. If the temperature persists for more than 3 days, of course, it is necessary to consult a doctor, control a blood test, if urine is needed, with a decision on the advisability of prescribing an antibiotic.