Ultrasound reading pregnancy
Fetal ultrasound - Mayo Clinic
Overview
2D fetal ultrasound
2D fetal ultrasound
A 2D fetal ultrasound can help your health care provider evaluate your baby's growth and development.
A fetal ultrasound (sonogram) is an imaging technique that uses sound waves to produce images of a fetus in the uterus. Fetal ultrasound images can help your health care provider evaluate your baby's growth and development and monitor your pregnancy. In some cases, fetal ultrasound is used to evaluate possible problems or help confirm a diagnosis.
The first fetal ultrasound is usually done during the first trimester to confirm the pregnancy and estimate how long you've been pregnant. If your pregnancy remains uncomplicated, the next ultrasound is typically offered during the second trimester, when anatomic details are visible. If a problem is suspected, a follow-up ultrasound or additional imaging tests, such as an MRI, might be recommended.
There are two main types of fetal ultrasound exams:
- Transvaginal ultrasound. With this type of fetal ultrasound, a wandlike device called a transducer is placed in your vagina to send out sound waves and gather the reflections. Transvaginal ultrasounds are used most often during early pregnancy. This type of ultrasound also might be done if a transabdominal ultrasound didn't provide enough information.
- Transabdominal ultrasound. A transabdominal fetal ultrasound is done by moving a transducer over your abdomen.
Various other types of transabdominal ultrasounds are available, including:
- Specialized sonographic evaluation. This type of exam might be needed in specific circumstances, such as when a fetal abnormality is known or suspected. In this situation, a more detailed evaluation can provide additional information about the abnormality.
- 3D ultrasound. This exam provides a two-dimensional display of three-dimensional data.
 This type of ultrasound is sometimes used to help health care providers detect facial abnormalities or neural tube defects.
This type of ultrasound is sometimes used to help health care providers detect facial abnormalities or neural tube defects. - Doppler ultrasound. A Doppler ultrasound measures slight changes in the ultrasound waves as they bounce off moving objects, such as blood cells. It can provide details about a baby's blood flow.
- Fetal echocardiography. This exam provides a detailed picture of a baby's heart. It might be used to confirm or rule out a congenital heart defect.
Products & Services
- Book: Mayo Clinic Guide to a Healthy Pregnancy
- Book: Obstetricks
Why it's done
First trimester ultrasound examination is done to evaluate the presence, size and location of the pregnancy, determine the number of fetuses, and estimate how long you've been pregnant (gestational age). Ultrasound can also be used for first trimester genetic screening, as well as screening for abnormalities of your uterus or cervix.
In the second or third trimester a standard ultrasound is done to evaluate several features of the pregnancy, including fetal anatomy. This exam is typically done between weeks 18 and 20 of pregnancy. However, the timing of this ultrasound might be altered for reasons such as obesity, which could limit visualization of the fetus.
During the second and third trimesters, limited ultrasound evaluation might be needed when a specific question requires investigation. Examples include the evaluation of fetal growth and the estimation of amniotic fluid volume. A specialized or detailed exam is done when an anomaly is suspected based on your history or other prenatal exam results.
Your health care provider might use fetal ultrasound to:
- Confirm the pregnancy and its location. Some fetuses develop outside of the uterus, in the fallopian tube. A fetal ultrasound can help your health care provider detect a pregnancy outside of the uterus (ectopic pregnancy).

- Determine your baby's gestational age. Knowing the baby's age can help your health care provider determine your due date and track various milestones throughout your pregnancy.
- Confirm the number of babies. If your health care provider suspects a multiple pregnancy, an ultrasound might be done to confirm the number of babies.
- Evaluate your baby's growth. Your health care provider can use ultrasound to determine whether your baby is growing at a normal rate. Ultrasound can be used to monitor your baby's movement, breathing and heart rate.
- Study the placenta and amniotic fluid levels. The placenta provides your baby with vital nutrients and oxygen-rich blood. Too much or too little amniotic fluid — the fluid that surrounds the baby in the uterus during pregnancy — or complications with the placenta need special attention. An ultrasound can help evaluate the placenta and amniotic fluid around the baby.

- Identify birth defects. An ultrasound can help your health care provider screen for some birth defects.
- Investigate complications. If you're bleeding or having other complications, an ultrasound might help your health care provider determine the cause.
- Perform other prenatal tests. Your health care provider might use ultrasound to guide needle placement during certain prenatal tests, such as amniocentesis or chorionic villus sampling.
- Determine fetal position before delivery. Most babies are positioned headfirst by the end of the third trimester. That doesn't always happen, though. Ultrasound imaging can confirm the baby's presentation so that your health care provider can discuss options for delivery.
Fetal ultrasound should be done only for valid medical reasons. Fetal ultrasound isn't recommended only to determine a baby's sex. Similarly, fetal ultrasound isn't recommended solely for the purpose of producing keepsake videos or pictures.
If your health care provider doesn't suggest a fetal ultrasound but you'd like the reassurance an ultrasound can provide, share your wishes with your care provider so that you can work together to determine what's best for you and your baby.
More Information
- Prenatal testing: Quick guide to common tests
- Hypoplastic left heart syndrome
- Preeclampsia
Request an Appointment at Mayo Clinic
Risks
Diagnostic ultrasound has been used during pregnancy for many years and is generally considered safe when used appropriately. The lowest amount of ultrasound energy that provides an accurate assessment should be used.
Fetal ultrasound also has limitations. Fetal ultrasound might not detect all birth defects — or might incorrectly suggest a birth defect is present when it's not.
How you prepare
You might be asked to drink a certain amount of fluid or avoid urinating before a fetal ultrasound, depending on the type of ultrasound. When scheduling your ultrasound, ask your health care provider for instructions.
When scheduling your ultrasound, ask your health care provider for instructions.
Also be aware that fetal ultrasound can be done through the vagina (transvaginal) or over the abdomen (transabdominal), depending on why it's being done or the stage of your pregnancy. If you're having a transabdominal ultrasound, consider wearing loosefitting clothing so that you can easily expose your abdomen.
What you can expect
During the procedure
During a transabdominal fetal ultrasound, you'll recline on an exam table and expose your abdomen. Your health care provider or technician will apply a special gel to your abdomen. This will improve the conduction of sound waves and eliminate air between your skin and the transducer.
Your health care provider or technician will move or scan the transducer back and forth over your abdomen. The sound waves reflected off your bones and other tissues will be converted into images on a monitor.
Your health care provider or technician will measure your baby's anatomy. He or she might print or store certain images to document important structures. You'll likely be given copies of some of the images.
He or she might print or store certain images to document important structures. You'll likely be given copies of some of the images.
Depending on your baby's position and stage of development, you might be able to make out a face, hands and fingers, or arms and legs. Don't worry if you can't "see" your baby. Ultrasound images can be hard for an untrained observer to decipher. Ask your health care provider or technician to explain what's on the screen.
The procedure for other types of fetal ultrasound exams is similar. If you're having a transvaginal ultrasound, however, you'll be asked to change into a hospital gown or undress from the waist down. You'll recline on an exam table and place your feet in stirrups. The transducer will be covered in a plastic sheath, like a condom, and be lubricated with gel. Your health care provider or technician will place the transducer in your vagina.
After the procedure
You can wipe off any residual gel or lubricant. If you had a full bladder during the ultrasound, you can urinate after the exam.
Results
3D fetal ultrasound
3D fetal ultrasound
A 3D fetal ultrasound can detect facial abnormalities or neural tube defects.
Typically, a fetal ultrasound offers reassurance that a baby is growing and developing normally. If your health care provider wants more details about your baby's health, he or she might recommend additional tests.
By Mayo Clinic Staff
Related
Products & Services
Pregnancy tests - ultrasound - Better Health Channel
Summary
Read the full fact sheet- Ultrasound is used during pregnancy to check the baby’s development, the presence of a multiple pregnancy and to help pick up any abnormalities.
- The ultrasound scan isn’t 100 per cent accurate, but the advantages of the test are that it’s non-invasive, painless and safe for both mother and unborn baby.
- If fetal abnormalities are detected, you may be offered further tests to confirm the diagnosis, such as amniocentesis and chorionic villus sampling.

What is an ultrasound?
Ultrasound is a scan that uses high frequency sound waves to study internal body structures. The sound waves are emitted from a vibrating crystal in a handheld scanner. The reflected sound waves or ‘echoes’ are then translated into a grainy, two-dimensional (or sometimes three-dimensional) image on a monitor.
Ultrasound is used during pregnancy to check the baby’s development and to help pick up any abnormalities such as Down syndrome. Since the procedure can’t produce high quality images, any suspected abnormalities need to be confirmed with other tests. The ultrasound scan isn’t 100 per cent accurate, but the advantages of the test are that it’s non-invasive, painless and safe for both mother and unborn baby.
Uses of the ultrasound
Ultrasound may be used at various points during pregnancy, including:
- First trimester - ultrasound performed within the first 3 months of pregnancy is used to check that the embryo is developing inside the womb (rather than inside a fallopian tube, for example), confirm the number of embryos, and calculate the gestational age and the baby’s due date.

- Second trimester - ultrasound performed between weeks 18 and 20 is used to check the development of fetal structures such as the spine, limbs, brain and internal organs. The size and location of the placenta is also checked. The baby’s sex can be established, if the parents wish to know.
- Third trimester - ultrasound performed after 30 weeks is used to check that the baby is continuing to grow at a normal rate. The location of the placenta is checked to make sure it isn’t blocking the cervix.
Medical issues to consider
Ultrasound is a safe, painless and non-invasive procedure. Many parents consider the ultrasound as an opportunity to see their unborn child, and perhaps discover its sex. However, you should remember that the ultrasound is a diagnostic procedure and, in some cases, it may suggest that a fetus has an abnormality. Further tests are usually needed to confirm the diagnosis.
Ultrasound procedure
The procedure depends on the type of ultrasound used, but may include:
- Transabdominal ultrasound – sound waves pass very well through water.
 The sonographer uses your full bladder as a ‘porthole’ to your uterus, so you will have to drink plenty of water before the test. You lie down on an examination table or bed. Gel is applied to your abdomen (to provide better contact between your skin and the scanner) and the sonographer moves the scanner in various positions. Pictures are sent instantly to a nearby monitor. The sonographer may have to push quite firmly at times in order to see the deeper structures. The scan usually takes about 30 minutes.
The sonographer uses your full bladder as a ‘porthole’ to your uterus, so you will have to drink plenty of water before the test. You lie down on an examination table or bed. Gel is applied to your abdomen (to provide better contact between your skin and the scanner) and the sonographer moves the scanner in various positions. Pictures are sent instantly to a nearby monitor. The sonographer may have to push quite firmly at times in order to see the deeper structures. The scan usually takes about 30 minutes. - Vaginal ultrasound – in some cases, a transabdominal ultrasound can’t produce clear enough pictures. There may be too much air in your bowel, for instance, and air is a poor conductor of sound waves. In these cases, a slender scanner is inserted into your vagina. The scan usually takes about 30 minutes.
Immediately after the ultrasound
Once the ultrasound is finished, you are given tissues to wipe away the gel, and you can go to the toilet. The report is sent to your doctor, so you will have to make an appointment to get the result.
The report is sent to your doctor, so you will have to make an appointment to get the result.
Possible complications
There are no known risks, complications or side effects for either the mother or her unborn baby.
Taking care of yourself at home
An ultrasound scan is safe, painless and non-invasive, so there is no need to take any special precautions afterward. You are free to go about your normal business.
Long term outlook
What happens next depends on the results of your ultrasound. Note that a normal result doesn’t guarantee that your baby is normal, because some abnormalities cannot be found using this test. If fetal abnormalities were detected, you may need further tests to confirm the diagnosis. These tests, including amniocentesis and chorionic villus sampling, are optional. Discuss the benefits, risks and complications of these tests with your doctor before deciding whether or not to go ahead.
Other types of pregnancy tests
Other types of pregnancy tests you may be offered could include:
- Amniocentesis – a small amount of amniotic fluid is taken using a slender needle inserted through the abdomen.
 The needle is guided with the help of ultrasound. The fluid sample contains cells, which are then examined in a laboratory for chromosomal abnormalities. The risk of miscarriage following amniocentesis is around one in 250.
The needle is guided with the help of ultrasound. The fluid sample contains cells, which are then examined in a laboratory for chromosomal abnormalities. The risk of miscarriage following amniocentesis is around one in 250. - Chorionic villus sampling – a slender needle is inserted through the abdomen or cervix to take a small sample of placenta. The needle is guided with the help of ultrasound. The chorionic villi are then tested in the laboratory for chromosomal abnormalities. The risk of miscarriage following chorionic villus sampling is one in 100.
Where to get help
- Your GP (doctor)
- Obstetrician and gynaecologist
- Any ultrasound or medical imaging department
This page has been produced in consultation with and approved by:
How to prepare for an ultrasound during pregnancy and other frequently asked questions from expectant mothers. Answered by a doctor with more than 40 years of experience
Rating: 4 / 5 (2)
Article reading time: 2 minutes trust only professionals. Most often, women who become mothers for the first time ask more questions related to all 9 months: how to prepare for an ultrasound of the fetus, is it safe for the baby, why is such a study needed, etc.
Most often, women who become mothers for the first time ask more questions related to all 9 months: how to prepare for an ultrasound of the fetus, is it safe for the baby, why is such a study needed, etc.
In this post, I've collected a number of frequently asked questions from moms-to-be of different ages to give you the most detailed answers.
How many times do you need to visit a doctor during pregnancy?
It all depends on how the expectant mother feels. And speaking in general, then at least 7 times for the entire period of bearing a baby.
The scheme is as follows:
- I trimester - once a month;
- II trimester - 1 time in 2-3 weeks;
- 36th week and before delivery - once a week.
An ultrasound was prescribed during pregnancy, it's scary, I think, is it safe?
Ultrasound is an absolutely safe examination method for both the baby and the mother, so it can be performed as many times as the specialist prescribes. And most importantly: a timely examination with the appointment of the necessary treatment, if necessary, gives every chance for the birth of a healthy child.
And most importantly: a timely examination with the appointment of the necessary treatment, if necessary, gives every chance for the birth of a healthy child.
Therefore, do not neglect the doctor's recommendations. At IdealMed, we perform ultrasound of the fetus during pregnancy at different stages, using only modern equipment for this, thanks to which the mother can clearly examine the baby, and the doctors can identify intrauterine development anomalies, if any.
How many times can I have an ultrasound during pregnancy?
Routine ultrasound during pregnancy is performed 3 times at different times: 11-13 weeks, 18-22 weeks and 32-34 weeks.
Preparing for ultrasound during pregnancy in the early stages and throughout all 9 months in general
In the early stages, both a transvaginal examination using a special probe and an abdominal examination can be performed, where a convex probe is used and driven over the abdomen from above. In the II and III trimesters, only abdominal ultrasound is performed.
The preparation is as simple as possible. Before performing a transvaginal ultrasound, it is important that the bladder and bowels are emptied. In addition, it is better not to eat food that causes flatulence the day before.
Abdominal preparation is not needed in principle, only personal hygiene the day before.
What is checked by ultrasound?
It all depends on the trimester, as the fetus grows, new changes appear, etc.
- I trimester
When examining up to 11 weeks, little information can be obtained, only whether there is a pregnancy in principle, the number of fetal eggs and their placement.
For example, in the period from 11 to 14 weeks - the period when it is possible to assess the violation of the formation of the fetal egg (missed pregnancy, hydatidiform mole), recognize gross congenital malformations (absence of a limb or part of it, underdevelopment and aplasia of the brain and spine), signs of genetic abnormalities (Down's disease), determine the localization of the placenta.
IMPORTANT! If gross external and chromosomal pathologies are observed, the woman is advised to terminate the pregnancy.
- II trimester
Ultrasound is performed at 18-22 weeks. At this time, you can study the development of the baby in more detail. The doctor analyzes the structure and function of the heart, determines the overall development, whether there are any minor defects in the internal organs.
In addition, it examines the amount of amniotic fluid, the length of the umbilical cord, the condition of its vessels, the thickness of the placenta, etc. It determines the tone of the uterus, the size of the pelvis, the state of the isthmic-cervical region (function of the cervix). As a result of the examination, the specialist can draw conclusions whether there is a threat of miscarriage, malformations, late toxicosis, etc.
- III trimester
The baby is preparing for the birth, so at this stage it is important for the doctor to decide whether the birth will be natural or whether a caesarean section will be needed.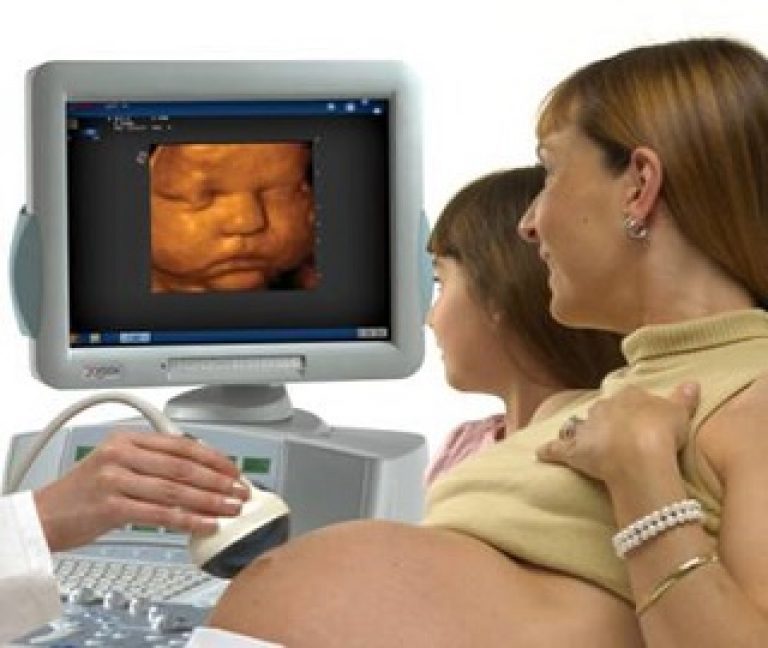 In addition, assess the readiness of the fetus for birth, whether there is an entanglement of the umbilical cord, placenta previa, congenital organ defects, etc.
In addition, assess the readiness of the fetus for birth, whether there is an entanglement of the umbilical cord, placenta previa, congenital organ defects, etc.
By the way, in the third trimester, a mother can see the baby's movements and even his facial expressions on ultrasound.
Are you expecting a baby? Sign up for an ultrasound of the fetus during pregnancy at IdealMed: we have no queues, only an individual appointment, as well as modern equipment and qualified specialists.
You can sign up by phone: +375 (17) 395-55-77, +375 (29) 144-22-22, +375 (29) 88-88-195.
Author: Nikitin Boris Nikolaevich
Ultrasound doctor of the highest category, experience - 43 years
Date of publication: 09/15/2021
Number of reviews in the article: 0
Write your review
90,000 ultrasounds at 35 weeks pregnant; norms, photo, video
Contents
- Children's body, main changes
- How the mother's body has changed
- Ultrasound of this period
- Normal indicators of the child's development
Contents
Now 8. 5 months of pregnancy are behind moments. There is not much time left before the birth of the long-awaited baby. By the 35th week, the coordinated functioning of all the organs of the child is noted. The adrenal glands of the fetus actively secrete hormones that regulate the water-salt balance of the tiny organism.
5 months of pregnancy are behind moments. There is not much time left before the birth of the long-awaited baby. By the 35th week, the coordinated functioning of all the organs of the child is noted. The adrenal glands of the fetus actively secrete hormones that regulate the water-salt balance of the tiny organism.
In the last weeks of pregnancy, very important processes in the development of the fetus take place. Ultrasound at 35 weeks of gestation is usually not prescribed. It can be carried out as an additional diagnosis, the need for which arises if any pathologies are detected. Sometimes the reason for an ultrasound examination is the desire of a pregnant woman.
Children's body, main changes
Starting from the 35th week, the baby's body begins to actively gain fat mass. There is a smoothing of the child's facial features, his individuality is already being drawn. The skin becomes more pink. On the monitor during ultrasound, the disappearance of the gun from the body of the baby is noted. When diagnosing, you can consider the position of the fetus in which it is to be born.
When diagnosing, you can consider the position of the fetus in which it is to be born.
The baby's nails have become longer, due to their considerable length they cover the fingertips. The eyes at this time for all babies are the same - a gray-blue hue. The length of the hair is about 5 cm. The sucking reflex is well developed, therefore, at this gestational age, premature birth is no longer terrible. The baby will easily adapt to breastfeeding.
The lungs are not yet fully formed at this stage, they are still developing. The production of an enzyme that prevents the alveoli from sticking together continues. During childbirth with this stage of development, the child will need artificial respiratory support.
Ultrasound will show fetal presentation. Norm is the key. If it is pelvic, gluteal, a caesarean section is possible. Thus, the mother and child will be able to avoid injury to the ligaments and joints.
The way of the upcoming birth will also be affected by:
- Baby's health;
- Fetal development level;
- Localization of the umbilical cord;
- Mater's condition.

In the last weeks of development, the fetus has a weight gain of about 220 grams for each week of pregnancy. The approximate size of the fetus by 35 weeks is 47 cm, and the weight during this period is approximately 2,500 g.
How the mother's body has changed
From this moment on, the baby moves head down (normally) towards the birth canal. A pregnant woman may feel contractions of the cervix. There is a periodic contraction / expansion of the cervix. The opening of this organ sometimes reaches 10 cm. Contractions are accompanied by very unpleasant sensations.
From the 35th week of pregnancy, Braxton Higgs contractions occur. They indicate the preparation of the mother's body for an early birth. These contractions are quite noticeable, but not painful. Their duration is approximately 2 minutes, then attenuation is noted.
Increased contractions may indicate an imminent delivery. In this case, you need to call an ambulance or go to the maternity ward that you have chosen in advance.
At 35 weeks there is a high position of the upper wall of the uterus. Its height above the level of the navel is 15 cm. The expectant mother has difficulty breathing due to compression of the lungs by a significantly enlarged uterus. Soon the uterus will descend and this phenomenon will disappear. To prevent difficulty breathing, you can use this exercise: get on all fours, relax as much as possible, take a deep breath, and then exhale the same way. We perform the exercise until you feel relief when breathing.
In the third trimester, diet is very important for the expectant mother. The size of the child became large, the pressure on the internal organs increased. It became more difficult for the stomach to digest large amounts of food. Doctors advise to eat food 5-6 times a day and, importantly, in small portions.
Heartburn is very common at this stage of pregnancy. It is very important to adhere to a healthy diet, exclude fatty, fried, sour, overly salty foods from your diet.
It is very important to adhere to a healthy diet, exclude fatty, fried, sour, overly salty foods from your diet.
Pregnant women often suffer from insomnia at 35 weeks. Its reasons may be:
- Uncomfortable position;
- Soreness of the hips;
- Urinary frequency;
- Excessive excitement.
To normalize sleep, you can use comfortable pillows for pregnant women, reduce the amount of fluid you drink before bedtime, avoid sleeping on your back, it is recommended to sleep on your side. Walking before bed can also help fight insomnia. In the evening, it is recommended to perform soothing, relaxing activities (reading books, listening to calm music).
The activity of the baby is increasing. This affects the maternal organs, because he, turning over, squeezes them. From next week, the lowering of the abdomen will be noted. The strip from the navel down became darker, there is itching of the skin due to stretching.
The mother's body is gradually preparing for childbirth, the expansion of the pelvis is fixed. This process causes pain, cramps in the lower abdomen, on the pubis, in the sides.
This process causes pain, cramps in the lower abdomen, on the pubis, in the sides.
There is swelling, swelling of the legs, caused by an increased load on the body. Back pain and seizures are often noted. It is necessary to provide the body with active recreation in the form of walks in the fresh air. Do not forget about the implementation of light exercises, necessary for the prevention of blood stasis.
From now on, special attention should be paid to emerging secretions. Transparent, odorless - the norm. Mucous discharge occurs as a result of exfoliation of the mucous plug.
If there are inclusions of pus, blood, smell in the discharge, this may indicate an infection. Watery discharge indicates leakage of amniotic fluid. With such secretions, a pregnant woman may be prescribed an ultrasound, recommend hospitalization.
Ultrasound of this period
An ultrasound is required at 35 weeks of gestation to ensure that the baby is well prepared for birth.
The fetus, uterus, placenta, umbilical cord, amniotic fluid are subject to inspection:
Placenta from the 35th week of pregnancy is characterized by the second degree of maturity. The resources of this organ decrease with increasing maturity. With the help of dopplerography, an assessment of this organ is carried out.
Diagnostics helps to determine the presence/absence of pathologies, defects in the development of the baby. The sonologist makes sure that the child's presentation is in accordance with the norm (it should be head).
Normal indicators of development of the child
By 35 weeks the baby has reached a high degree of development. After 2 weeks, the baby will be considered full-term. Ultrasound examination reveals the nuclei of ossification that occurred in children's bones. The child continues to develop the brain. 90% of children born with this degree of development survive without medical assistance from attendants.