Heel stick test
Why Do They Prick Your Newborn Baby’s Heel? – Cleveland Clinic
When your baby is born, there are many firsts: a first breath, a first touch. If your baby is born in a hospital, they’ll also receive their first series of health screenings.
Every state in the United States requires newborns to have certain health tests. A hearing test is required by law in certain states, for example, and a pulse oximetry test determines the level of oxygen in an infant’s blood. An abnormal oxygen level can indicate a critical heart malformation.
About 24 hours after your baby is born before you’re discharged from the hospital, a nurse will administer a “heel prick” test to look for indications in the blood of rare medical conditions, such as phenylketonuria or PKU. We asked pediatrician Thomas Phelps, MD, what else parents need to know about the newborn screening panel.
Why does your newborn need a blood test?
Newborn screening got its start in the 1960s when scientists developed a blood test for PKU, an amino acid disorder. “Babies with PKU appear perfectly healthy at first,” says Dr. Phelps. “But if their condition isn’t treated soon after birth by changing their milk supply, they will eventually experience a host of serious health issues including the possibility for developmental delays, brain damage and even death,” he says.
Over time, states added tests for other conditions besides PKU to this heel prick test. In particular, they test for conditions that aren’t obvious at birth and are treatable before it is too late and symptoms appear.
Advertising Policy
“Knowing whether your baby has one of these conditions before symptoms appear can make a huge difference in your baby’s health,” Dr. Phelps says. “In fact, early treatment, which can sometimes involve something as simple as a change in diet, can prevent how the disease affects your child as an infant and throughout their whole life,” he says.
How does newborn screening work?
In general, doctors arrange for testing when a newborn is between 24 and 48 hours old. If your baby is born in a hospital, the staff will test your baby before you’re released to go home. If you give birth at home, a midwife should do the test at home 24 hours from birth. “If you have a home birth, you can also take your newborn to a local hospital for the screening 24 hours after they’re born and within two to three days,” says Dr. Phelps.
If your baby is born in a hospital, the staff will test your baby before you’re released to go home. If you give birth at home, a midwife should do the test at home 24 hours from birth. “If you have a home birth, you can also take your newborn to a local hospital for the screening 24 hours after they’re born and within two to three days,” says Dr. Phelps.
A nurse or medical technician will draw blood from your baby’s heel and send it off to a state lab for testing. “Ideally your infant should be fed prior to the test,” says Dr. Phelps. Your pediatrician will let you know if the screening results show any issues, usually within a week.
But the screening is not a diagnostic tool, Dr. Phelps says. “If anything shows up as abnormal, the test will be repeated to confirm,” says Dr. Phelps. He clarifies: “Some tests will be normal on repeat testing. After the child’s physician or specialist verifies the test results, the specialist will set up a care plan for treatment and close follow up. ”
”
Advertising Policy
What conditions are they looking for in newborn screenings?
Each state determines which conditions the newborn screenings will test for, Dr. Phelps says. Health officials typically take into account both national health recommendations and what conditions are most common in each region based on population genetics. Most states test for PKU (present in 1 in 10,000 to 15,000 births), but many also test for:
- Primary congenital hypothyroidism. This is an endocrine disorder in which your baby’s body doesn’t produce enough of the thyroid hormone. Without treatment within four weeks of age, CH can lead to developmental delays and slow growth.
- Maple syrup urine disease. Like PKU, maple syrup urine disease is an amino acid disorder that can lead to developmental delays. As the name suggests, babies with the disease have a distinctive, sweet-smelling, or maple-syrup like, odor to their urine.
 With this condition, the body is unable to break down certain proteins. Babies with this condition may seem listless or lethargic, exhibit vomiting or poor feeding habits due to nausea and if left untreated, can develop seizures. This condition can eventually be fatal if left untreated.
With this condition, the body is unable to break down certain proteins. Babies with this condition may seem listless or lethargic, exhibit vomiting or poor feeding habits due to nausea and if left untreated, can develop seizures. This condition can eventually be fatal if left untreated. - Cystic fibrosis. This condition affects the mucus glands and causes mucus to be thick and sticky. The mucus prevents certain organs from working properly, including the lungs, liver and intestines. This condition also hinders a baby’s ability to retain nutrients and grow normally. There is no cure, but early awareness and treatment can help you manage the condition, so your child can live a longer, healthier life.
- Sickle cell anemia. This condition affects people of African descent, as well as families from South or Central America, the Caribbean Islands, Mediterranean countries, India and Saudi Arabia. This condition can cause anemia (low red blood cells), fatigue, pain, organ damage and death.
 Your child’s doctor will also test for other possible problems with their hemoglobin (a protein in your red blood cells). This may include thalassemia (either alpha or beta types), which is genetically passed down to children as sickle cell.
Your child’s doctor will also test for other possible problems with their hemoglobin (a protein in your red blood cells). This may include thalassemia (either alpha or beta types), which is genetically passed down to children as sickle cell.
That tiny heel prick can reveal so many illnesses that can potentially be life-threatening or can potentially be physically and intellectually damaging. Regardless of what conditions your state screens for, hospitals offer the newborn screening panel to help all babies get the best start possible. “The conditions screenings look for are rare, but sometimes serious,” says Dr. Phelps. “Finding them early offers the best chance for your baby to grow and thrive.”
Newborn blood spot test - NHS
Every baby is offered newborn blood spot screening, also known as the heel prick test, ideally when they're 5 days old.
What is the blood spot test?
Newborn blood spot screening involves taking a blood sample to find out if your baby has 1 of 9 rare but serious health conditions.
Most babies won't have any of these conditions but, for the few who do, the benefits of screening are enormous.
Early treatment can improve their health, and prevent severe disability or even death.
What does the blood spot test involve?
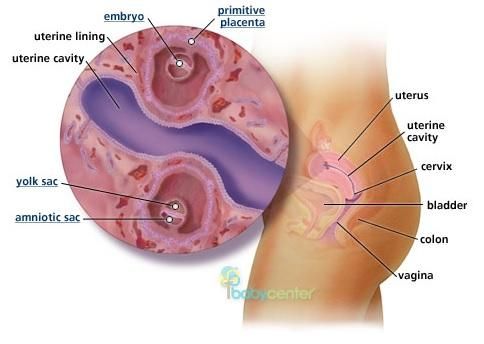
When your baby is 5 days old, a healthcare professional will prick their heel and collect 4 drops of blood on a special card.
You can ease any distress for your baby by cuddling and feeding them, and making sure they're warm and comfortable.
Occasionally, the sample may need to be taken when your baby is 6, 7 or 8 days old.
Sometimes a second blood spot sample is needed. The reason for this will be explained to you. It doesn't necessarily mean there's something wrong with your baby.
The test doesn't carry any known risks for your baby.
Which conditions is the blood spot test for?
The blood spot test screens for the following 9 rare but serious conditions.
If you, your partner or a family member already has one of these conditions (or a family history of it), tell your healthcare professional straight away.
Sickle cell disease
About 270 babies are born with sickle cell disease in the UK each year. This is a serious inherited blood disease.
Sickle cell disease affects haemoglobin, the iron-rich protein in red blood cells that carries oxygen around the body.
Babies who have this condition will need specialist care throughout their lives.
People with sickle cell disease can have attacks of severe pain and get serious, life-threatening infections. They're usually anaemic because their blood cells have difficulty carrying oxygen.
The blood spot screening test means that babies with sickle cell disease can receive early treatment to help them live healthier lives. This may include vaccinations and antibiotics to prevent serious illnesses.
Pregnant women are also routinely tested for sickle cell disease early in pregnancy.
Read more about sickle cell disease.
GOV.UK also has a factsheet about sickle cell disease
Cystic fibrosis
About 1 in 2,500 babies born in the UK has cystic fibrosis. This inherited condition affects the digestion and lungs.
Babies with cystic fibrosis may not gain weight well and are prone to chest infections.
Babies with the condition can be treated early with a high-energy diet, medicines and physiotherapy.
Although children with cystic fibrosis may still become very ill, early treatment can help them live longer, healthier lives.
Read more about cystic fibrosis.
GOV.UK also has a leaflet for parents whose baby has suspected cystic fibrosis
Congenital hypothyroidism
About 1 in every 2,000 to 3,000 babies born in the UK has congenital hypothyroidism. Babies with congenital hypothyroidism don't have enough of the hormone thyroxine.
Without thyroxine, babies don't grow properly and can develop learning disabilities.
Babies who have the condition can be treated early with thyroxine tablets, and this allows them to develop normally.
The British Thyroid Foundation has more information about congenital hypothyroidism
Inherited metabolic diseases
It's important to let your healthcare professional know if you have a family history of a metabolic disease (a disease that affects your metabolism).
Babies are screened for 6 inherited metabolic diseases. These are:
- phenylketonuria (PKU)
- medium-chain acyl-CoA dehydrogenase deficiency (MCADD)
- maple syrup urine disease (MSUD)
- isovaleric acidaemia (IVA)
- glutaric aciduria type 1 (GA1)
- homocystinuria (pyridoxine unresponsive) (HCU)
About 1 in 10,000 babies born in the UK has PKU or MCADD. The other conditions are rarer, occurring in 1 in 100,000 to 150,000 babies.
Without treatment, babies with inherited metabolic diseases can become suddenly and seriously ill. The diseases all have different symptoms.
Depending on which one affects your baby, the condition may be life threatening or cause severe developmental problems.
They can all be treated with a carefully managed diet and, in some cases, medicines as well.
Severe combined immunodeficiency (SCID)
In some areas of England, screening for a condition called severe combined immunodeficiency (SCID) is also being offered as part of the newborn blood spot test. This is to help the NHS decide if screening for SCID should be offered to all babies in England.
SCID causes problems with the immune system. It makes it very hard for a baby to fight off infections like meningitis and pneumonia, which can be life-threatening. About 14 babies born each year in England have SCID.
Ask your midwife if screening for SCID is being offered in your area.
Great Ormond Street Hospital for Children has more information on severe combined immunodeficiency
Does my baby have to have the blood spot test?
The blood spot test is not compulsory, but it's recommended because it could save your baby's life.
You can choose to have screening for sickle cell disease, cystic fibrosis or congenital hypothyroidism individually, but you can only choose to have screening for all 6 inherited metabolic diseases or none at all.
If you don't want your baby to be screened for any of these conditions, discuss it with your midwife.
You should be given information about the blood spot test and the diseases it screens for in advance so you can make an informed decision for your baby.
If you change your mind, babies can be screened up to the age of 12 months for all the conditions except cystic fibrosis. Cystic fibrosis can only be screened for up to 8 weeks of age.
If you have any concerns about the tests, speak to your midwife, health visitor or GP.
When will we get the results?
You should receive the results either by letter or from a healthcare professional by the time your baby is 6 to 8 weeks old.
The results should be recorded in your baby's personal child health record (red book). It's important to keep this safe and take it with you to all your baby's appointments.
If you haven't received your baby's results, speak to your health visitor or GP.
You'll be contacted sooner if your baby screens positive. This means they're more likely to have one of the conditions tested for.
You'll be contacted:
- the day the result is available, or the next working day, if your baby is thought to have congenital hypothyroidism (CHT) – you'll be given an appointment to see a specialist
- before your baby's 4 weeks old if they're thought to have cystic fibrosis
- before your baby's 6 weeks old if they're thought to have sickle cell disease
Screening for cystic fibrosis finds some babies who may be genetic carriers of the condition. These babies may need further testing.
These babies may need further testing.
Screening for sickle cell disease also finds babies who are carriers of this or other red blood cell diseases.
Carriers are healthy, although they can experience problems in situations where their bodies aren't getting much oxygen – for example, if they're having an anaesthetic.
Parents of babies who are found to be carriers should be told by the time they're 6 to 8 weeks old.
What do the results mean?
Most babies will have a normal result, which means it's unlikely that they have any of the conditions.
A small number of babies will screen positive for one of the conditions. This doesn't mean they have the condition, but they're more likely to have it. They'll be referred to a specialist for more tests.
It's important to know that screening isn't 100% certain. A baby with a negative screening result may later turn out to have the disease screened for. This is known as a false negative.
A baby with a negative screening result may later turn out to have the disease screened for. This is known as a false negative.
Babies with a positive result sometimes turn out not to have the disease – what's known as a false positive.
Occasionally, other medical conditions are picked up by blood spot test screening. For example, babies with beta thalassaemia major, a serious blood disease, will usually be detected. These babies also need to be referred for early treatment.
More information
- Frequently asked questions about blood spot screening
- Find out what happens to your baby's blood spot card
- GOV.UK: screening tests for you and your baby
Baby Heel Test | Bezzia
If you're a new mom or dad, one of the hardest things you'll have to go through when you have a baby is the popular heel test. With this test, they analyze your baby's blood to treat metabolic diseases such as hypothyroidism or cystic fibrosis as soon as possible. If these diseases are diagnosed late, they can cause serious health problems for the baby and even endanger his life.
With this test, they analyze your baby's blood to treat metabolic diseases such as hypothyroidism or cystic fibrosis as soon as possible. If these diseases are diagnosed late, they can cause serious health problems for the baby and even endanger his life.
The test consists of a heel prick and this is usually done within a few days of birth. Then I will tell you a little more about this so that you know more specifically what this test consists of.
Index
- 1 Diseases detected by the heel test
- 2 What is the heel test?
Diseases detected by the heel test
The heel test aims to prevent and treat future metabolic diseases that negatively affect important organs such as the heart or lungs, or the good development of the child. The vast majority of these diseases are genetic in nature and are usually passed on from parents to children. As I mentioned above, due to this analysis of the child's blood, diseases such as congenital hypothyroidism, cystic fibrosis, tyrosinemia or congenital adrenal hyperplasia can be detected. That's why it's so important to do this test on a newborn.
As I mentioned above, due to this analysis of the child's blood, diseases such as congenital hypothyroidism, cystic fibrosis, tyrosinemia or congenital adrenal hyperplasia can be detected. That's why it's so important to do this test on a newborn.
What is a heel test?
The heel test consists of a small, shallow prick in the heel that allows a small amount of blood to be dripped to soak paper, which is sent to a laboratory and analyzed to rule out any of the diseases mentioned above. In most cases, the baby feels pain from the injection and cries from the discomfort, so it is advisable to constantly caress the baby to calm him down and prevent him from having a very bad time. Experts in the field advise to perform this test in the first days of a child's life, especially in the first 48 and 72 hours, and thus as soon as possible to identify any type of condition or disease that the child may have.
In addition to the blood in this test, the child's data is usually collected along with the family's data in order to facilitate the sending of the data obtained in the tests, and the parents can know the results of the specified blood test as soon as possible. If the heel test is positive, it must be repeated to ensure that there were no failures and that the test is completely valid. If it remains positive and the child is confirmed to have some type of metabolic disease, treatment should be started as soon as possible to avoid possible health complications. Parents will receive advice from a specialist so that they know how to cope with the problem in the best possible way, and the child can cope with this disease every day.
If the heel test is positive, it must be repeated to ensure that there were no failures and that the test is completely valid. If it remains positive and the child is confirmed to have some type of metabolic disease, treatment should be started as soon as possible to avoid possible health complications. Parents will receive advice from a specialist so that they know how to cope with the problem in the best possible way, and the child can cope with this disease every day.
As you have seen, the heel test is necessary and very important, as it allows you to identify other metabolic disorders and save the baby's life. This is a free test that all hospitals must take. And although this is a very difficult time for any parent, because the child cries a lot, it is important to do this as soon as possible. I hope it's perfectly clear to you what the famous heel test is and why it's so important.
The content of the article complies with our principles of editorial ethics. To report a bug, click here.
To report a bug, click here.
Neonatal screening | BPH 91
Neonatal screening
Immediately after birth, the child may not have clinical symptoms of a genetic disease. However, with age, clinical symptoms can increase, leading to a critical situation, serious illness and even death.
Neonatal screening is carried out for early detection, timely treatment, prevention of disability and the development of severe clinical consequences, as well as reducing child mortality from hereditary diseases.
Neonatal screening is a mass examination of newborns for hereditary diseases (adrenogenital syndrome, galactosemia, congenital hypothyroidism, cystic fibrosis, phenylketonuria).
When is newborn screening done?
Neonatal screening is carried out on:
- 4 days of life in a full-term baby;
- 7 days of life in a premature baby.
Where is newborn screening done?
Blood sampling is carried out in the maternity hospital. At the same time, in the extract, the neonatologist puts a mark “Neonatal screening taken”.
If, for some reason, screening was not carried out, then it is carried out at the polyclinic at the place of residence.
How are newborns screened?
A blood sample is taken from the heel of a newborn baby 3 hours after feeding.
Blood sampling is carried out on special filter paper test forms from the heel of the newborn.
Before taking a blood sample, the heel of a newborn child must be washed, wiped with a sterile cloth moistened with 70-degree alcohol, then moistened with a dry sterile cloth. The heel puncture of a newborn child is carried out with a disposable scarifier, the first drop of blood is removed with a sterile dry swab.
To collect a second drop of blood, apply gentle pressure to the heel of a newborn baby. The test form is applied perpendicularly and soaked with blood completely and through and through in accordance with the circle dimensions indicated on the test form. The appearance of blood spots should be the same on both sides of the test form.
The test form is applied perpendicularly and soaked with blood completely and through and through in accordance with the circle dimensions indicated on the test form. The appearance of blood spots should be the same on both sides of the test form.
The study of blood samples is carried out in the Medical Genetic Department (Moscow Center for Neonatal Screening).
Since 2006, in Russia, by order of the Ministry of Health and Social Development of Russia dated March 22, 2006 No. 185 "On mass screening of newborn children for hereditary diseases" , neonatal screening for five hereditary diseases has been carried out: 90 hypothyroidism14 Congenital.
1. Phenylketonuria.
2. Cystic fibrosis.
3. Galactosemia.
4. Andrenogenital syndrome.
5. Congenital hypothyroidism.
Congenital hypothyroidism is a disease in which thyroid insufficiency is manifested, so the physical and mental condition of the child does not develop. Timely hormonal treatment will prevent the disease and lead to the full development and recovery of the baby. The dose of the hormone is selected individually.
Timely hormonal treatment will prevent the disease and lead to the full development and recovery of the baby. The dose of the hormone is selected individually.
Phenylketonuria is a rare hereditary disease of the group of fermentopathies associated with impaired metabolism of amino acids, mainly phenylalanine. The disease is associated with serious mental and neurological disorders. If a disease is detected, the doctor prescribes a long-term diet for the recovery and normal development of the young organism. The diet is selected individually.
Cystic fibrosis ( also known as cystic fibrosis ) is a common genetic disease that is transmitted only by inheritance. Its specific feature is the formation of viscous mucus throughout the body, as a result of which, first of all, the functioning of organs covered with a mucous membrane is disrupted: the digestive system, lungs and other vital organs. Most often, the disease manifests itself in infancy and requires well-coordinated interaction between the family and medical specialists in order to provide the child with timely, and therefore effective treatment.
Most often, the disease manifests itself in infancy and requires well-coordinated interaction between the family and medical specialists in order to provide the child with timely, and therefore effective treatment.
Galactosemia is a cause that occurs when feeding with milk or dairy products, while internal organs (nervous system, liver) are affected. Following the doctor's instructions, treatment and a dairy-free diet will help to avoid consequences.
Adrenogenital syndrome - increased production of androgen hormones by the adrenal glands. If left untreated, then the reproductive system develops rapidly in children, and the overall growth stops, in the future - the person is infertile. The use of the necessary hormonal drugs restores development and removes the signs of the manifestation of the disease.
-Genetic Department (Moscow Center for Neonatal Screening).