Group b strep culture pregnancy
Group B Strep and Pregnancy (for Parents)
What Is Group B Strep?
Group B Streptococcus (group B strep, GBS) is a type of
bacteriaoften found in the urinary tract, digestive system, and reproductive tracts. The bacteria come and go from our bodies, so most people who have it don't know that they do. GBS usually doesn't cause health problems.
What Problems Can Group B Strep Cause?
Health problems from GBS are not common. But it can cause illness in some people, such as the elderly and those with some medical conditions. GBS can cause infections in such areas of the body as the blood, lungs, skin, or bones.
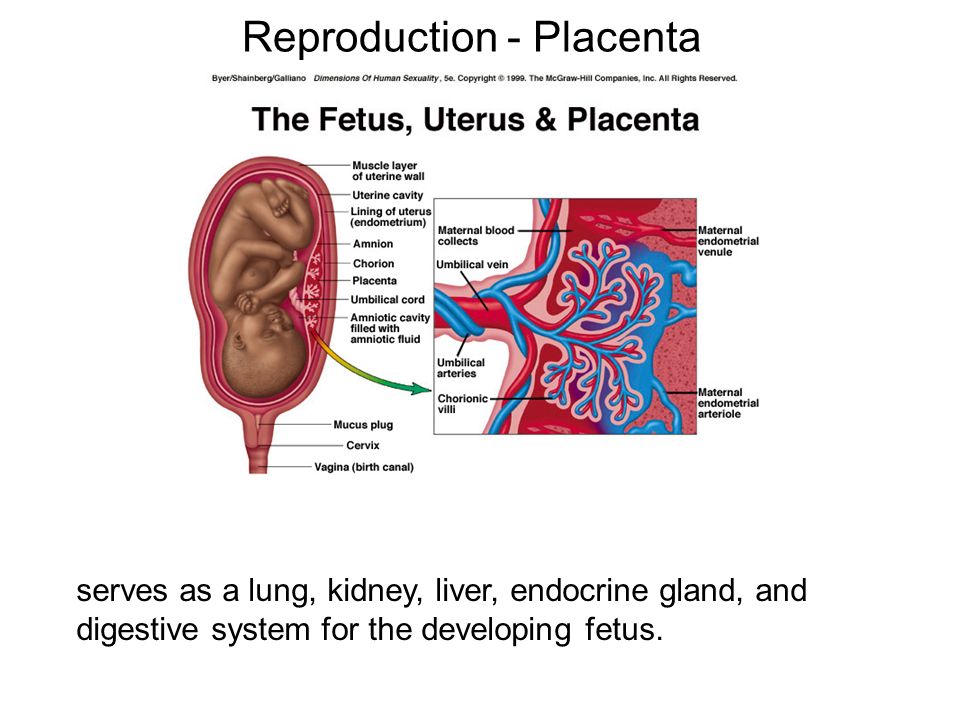
About 1 out of every 4 women have GBS. In pregnant women, GBS can cause infection of the urinary tract, placenta, womb, and amniotic fluid.
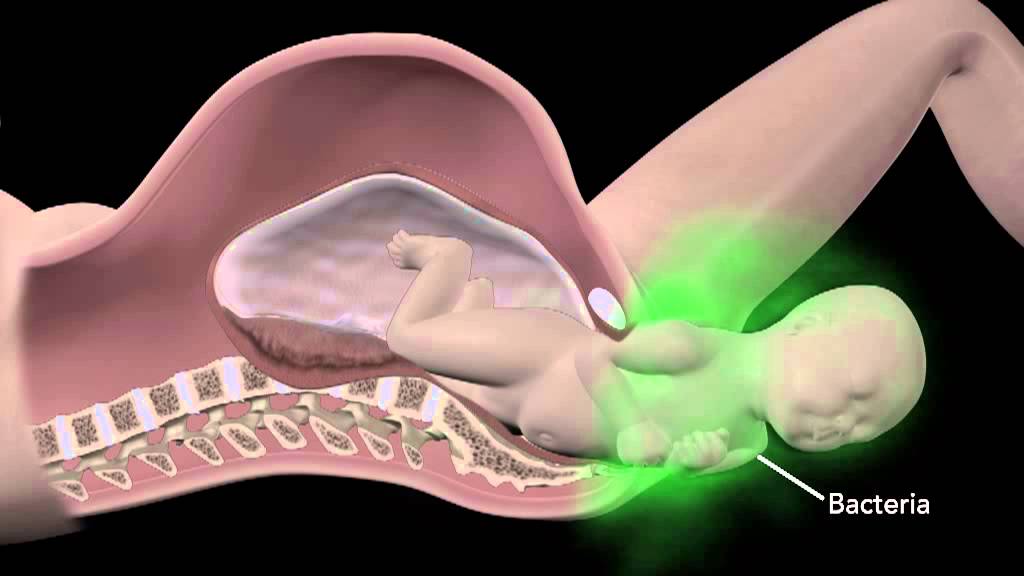
Even if they haven't had any symptoms of infection, pregnant women can pass the infection to their babies during labor and delivery.
How Does Group B Strep Affect Babies?
When women with GBS are treated with antibiotics during labor, most of their babies do not have any problems. But some babies can become very sick from GBS. Premature babies are more likely to be infected with GBS than full-term babies because their bodies and immune systems are less developed.
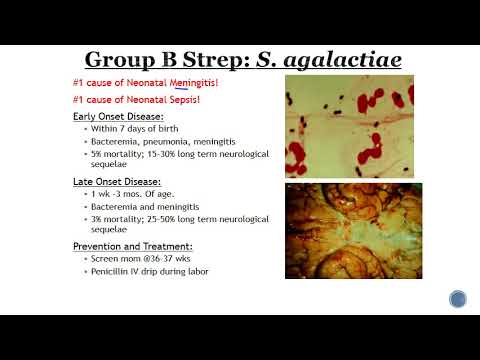
The two types of GBS disease in babies are:
- Early-onset infections, which happen during the first week of life. Babies often have symptoms within 24 hours of birth.
- Late-onset infections, which develop weeks to months after birth. This type of GBS disease is not well understood.
What Are the Signs & Symptoms of GBS Disease?
Newborns and infants with GBS disease might show these signs:
- a fever
- feeding problems
- breathing problems
- irritability or fussiness
- inactivity or limpness
- trouble keeping a healthy body temperature
Babies with GBS disease can develop serious problems, such as:
- pneumonia
- sepsis
- meningitis (infection of the fluid and lining around the brain).
 Meningitis is more common with late-onset GBS disease and, in some cases, can lead to hearing loss, vision loss, learning disabilities, seizures, and even death.
Meningitis is more common with late-onset GBS disease and, in some cases, can lead to hearing loss, vision loss, learning disabilities, seizures, and even death.
How Is Group B Strep Diagnosed?
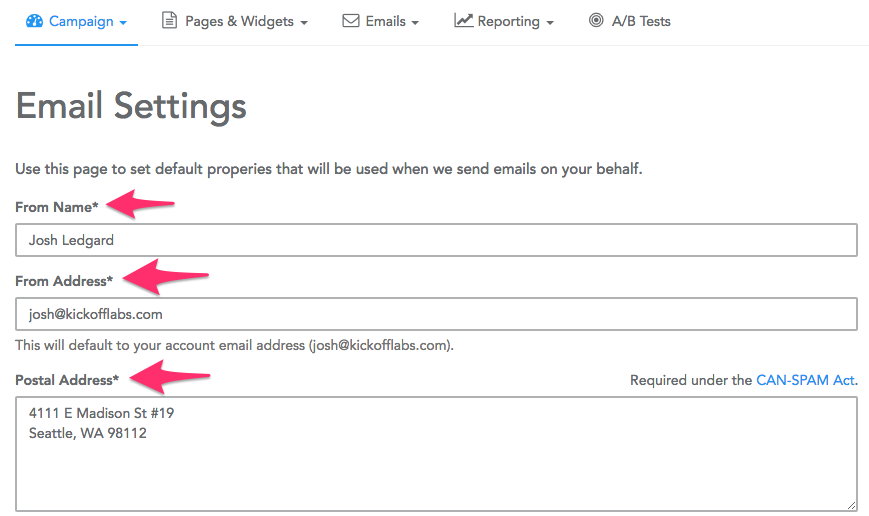
Pregnant women are routinely tested for GBS late in the pregnancy, usually between weeks 35 and 37. The test is simple, inexpensive, and painless. Called a culture, it involves using a large cotton swab to collect samples from the vagina and rectum. These samples are tested in a lab to check for GBS. The results are usually available in 1 to 3 days.
If a test finds GBS, the woman is said to be "GBS-positive." This means only that she has the bacteria in her body — not that she or her baby will become sick from it.
GBS infection in babies is diagnosed by testing a sample of blood or spinal fluid. But not all babies born to GBS-positive mothers need testing. Most healthy babies are simply watched to see if they have signs of infection.
How Is Group B Strep Treated?
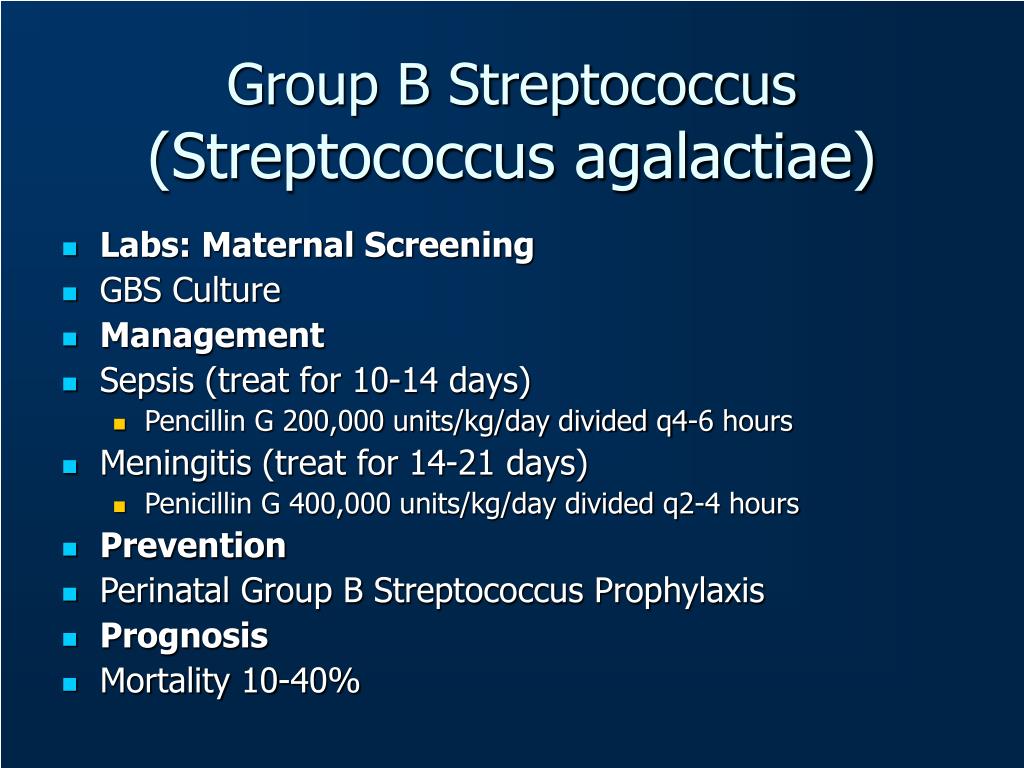
Doctors will test a pregnant woman to see if she has GBS. If she does, she will get intravenous (IV) antibiotics during labor to kill the bacteria. Doctors usually use penicillin, but can give other medicines if a woman is allergic to it.
If she does, she will get intravenous (IV) antibiotics during labor to kill the bacteria. Doctors usually use penicillin, but can give other medicines if a woman is allergic to it.
It's best for a woman to get antibiotics for at least 4 hours before delivery. This simple step greatly helps to prevent the spread of GBS to the baby.
Doctors also might give antibiotics during labor to a pregnant woman if she:
- goes into labor prematurely, before being tested for GBS
- hasn't been tested for GBS and her water breaks 18 or more hours before delivery
- hasn't been tested for GBS and has a fever during labor
- had a GBS bladder infection during the pregnancy
- had a baby before with GBS disease
Giving antibiotics during labor helps to prevent early-onset GBS disease only. The cause of late-onset disease isn't known, so no method has yet been found to prevent it. Researchers are working to develop a vaccine to prevent GBS infection.
Babies who get GBS disease are treated with antibiotics. These are started as soon as possible to help prevent problems. These babies also may need other treatments, like breathing help and IV fluids.
How Can I Help Prevent Group B Strep Infection?
Because GBS comes and goes from the body, a woman should be tested for it during each pregnancy. Women who are GBS-positive and get antibiotics at the right time during labor do well, and most don't pass the infection to their babies.
If you are GBS-positive and begin to go into labor, go to the hospital rather than laboring at home. By getting IV antibiotics for at least 4 hours before delivery, you can help protect your baby against early-onset GBS disease.
Reviewed by: Thinh Phu Nguyen, MD
Date reviewed: July 2022
Group B Strep In Pregnancy: Test, Risks & Treatment
Overview
What is group B strep?
Group B strep infection (also GBS or group B Streptococcus) is caused by bacteria typically found in a person's vagina or rectal area. About 25% of pregnant people have GBS, but don't know it because it doesn't cause symptoms. A pregnant person with GBS can pass the bacteria to their baby during vaginal delivery. Infants, older adults or people with a weakened or underdeveloped immune system are more likely to develop complications from group B strep.
About 25% of pregnant people have GBS, but don't know it because it doesn't cause symptoms. A pregnant person with GBS can pass the bacteria to their baby during vaginal delivery. Infants, older adults or people with a weakened or underdeveloped immune system are more likely to develop complications from group B strep.
Most newborns who get GBS don't become sick. However, the bacteria can cause severe and even life-threatening infections in a small percentage of newborns. Healthcare providers screen for group B strep as part of your routine prenatal care. If you test positive, your provider will treat you with antibiotics.
How do you get group B strep?
GBS bacteria naturally occur in areas of your body like your intestines and genital and urinary tracts. Adults can't get it from person-to-person contact or from sharing food or drinks with an infected person. Experts aren't entirely sure why the bacteria spreads, but they know that it’s potentially harmful in babies and people with weakened immune systems.
When do you get tested for group B strep?
The Centers for Disease Control and Prevention (CDC) recommends routine screening for group B strep in all pregnancies. You're screened for GBS between 36 and 37 weeks of pregnancy. Group B strep testing involves your provider taking a swab of your vagina and rectum and then sending it to a lab for analysis.
Can Group B strep affect a developing fetus?
GBS doesn't affect the fetus baby while it's still inside your uterus. However, your baby can get GBS from you during labor and delivery. Taking antibiotics for GBS reduces your chances of passing it to your baby.
How does a baby get GBS?
There are two main types of Group B strep in babies:
- Early-onset infection: Most (75%) babies with GBS become infected in the first week of life. GBS infection is usually apparent within a few hours after birth. Premature babies face greater risk if they become infected, but most babies who get GBS are full-term.
- Late-onset infection: GBS infection can also occur in infants one week to three months after birth. Late-onset infection is less common and is less likely to result in a baby's death than early-onset infection.
How common is GBS?
Group B strep screening during pregnancy has decreased the number of cases. According to the CDC, about 930 babies get early-onset GBS, and 1,050 get late-onset GBS. About 4% of babies who develop GBS will die from it.
Symptoms and Causes
What are the symptoms of group B strep?
Most adults don't experience symptoms of group B strep. It can cause symptoms in older people or people with certain medical conditions, but this is rare. These symptoms include:
- Fever, chills and fatigue.
- Difficulty breathing.
- Chest pains.
- Muscle stiffness.
Newborns with GBS have symptoms like:
- Fever.
- Difficulty feeding.
- Irritability.
- Breathing difficulties.

- Lack of energy.
These symptoms can become serious quickly because newborns lack immunity. Group B strep infection can lead to severe problems like sepsis, pneumonia and meningitis in infants.
Can I pass group B strep to my partner?
Other people that live with you, including other children, aren't at risk of getting sick.
Diagnosis and Tests
Will I be tested for group B strep?
Yes, your healthcare provider will test you for GBS late in your pregnancy, around weeks 36 to 37.
Your obstetrician uses a cotton swab to obtain samples of cells from your vagina and rectum. This test doesn't hurt and takes less than a minute. Then, the sample is sent to a lab where it's analyzed for group B strep. Most people receive their results within 48 hours. A positive culture result means you're a GBS carrier, but it doesn't mean that you or your baby will become sick.
If you’re using a midwife, you might be given instructions on how to test yourself at home and submit the swab to a lab.
Is Group B strep an STD?
No, group B strep isn't an STD (sexually transmitted disease). The type of bacteria that causes GBS naturally lives in your vagina or rectum. It doesn't cause symptoms for most people.
Management and Treatment
What happens if you test positive for group B strep during pregnancy?
Healthcare providers prevent GBS infection in your baby by treating you with intravenous (IV) antibiotics during labor and delivery. The most common antibiotic to treat group B strep is penicillin or ampicillin. Giving you an antibiotic at this time helps prevent the spread of GBS from you to your newborn. It's not effective to treat GBS earlier than at delivery. The antibiotics work best when given at least four hours before delivery. About 90% of infections are prevented with this type of treatment.
One exception to the timing of treatment is when GBS is detected in urine. When this is the case, oral antibiotic treatment begins when GBS is identified (regardless of the stage of pregnancy). Antibiotics should still be given through an IV during labor.
Antibiotics should still be given through an IV during labor.
Any pregnant person who has previously given birth to a baby who developed a GBS infection or who has had a urinary tract infection in this pregnancy caused by GBS will also be treated during labor.
How is group B strep treated in newborns?
Some babies still get GBS infections despite testing and antibiotic treatment during labor. Healthcare providers might take a sample of the baby's blood or spinal fluid to see if the baby has GBS infection. If your baby has GBS, they're treated with antibiotics through an IV.
Prevention
How can I reduce my risk of group B strep?
Anyone can get GBS. Some people are at higher risk due to certain medical conditions or age. The following factors increase your risk for having a baby born with group B strep:
- You tested positive for GBS.
- You develop a fever during labor.
- More than 18 hours pass between your water breaking and your baby being born.
- You have medical conditions like diabetes, heart disease or cancer.
Getting screened for GBS and taking antibiotics (if you're positive) is the best way to protect your baby from infection.
Outlook / Prognosis
What are long term problems of Group B strep in newborns?
Infants with GBS can develop meningitis, pneumonia or sepsis. These illnesses can be life-threatening. Most infants don't develop any long-term issues; however, about 25% of babies with meningitis caused by GBS develop cerebral palsy, hearing problems, learning disabilities or seizures.
Can I get tested for group B strep again?
No, once you test positive for GBS, you're considered positive for the rest of your pregnancy. You will not get re-tested.
Do I need treated for group B strep if I am having a c-section?
No, you don't need antibiotics if you're having a c-section delivery. However, you'll still be tested for GBS because labor could start before your scheduled c-section. If your water breaks and you're GBS positive, your baby is at risk of contracting the disease.
If your water breaks and you're GBS positive, your baby is at risk of contracting the disease.
Living With
When should I see my healthcare provider if I’m positive for group B strep?
In some cases, GBS causes infections during pregnancy. Symptoms of infection include fever, pain and increased heart rate. Let your provider know if you have any of those symptoms as it could lead to preterm labor.
GBS can also cause urinary tract infection (UTI), which requires oral antibiotics.
Talk to your provider about what you can expect during labor and delivery if you have group B strep.
A note from Cleveland Clinic
Try not to panic if your healthcare provider tells you you're positive for group B strep during pregnancy. It's caused by bacteria that occur naturally in your body, not by anything you did wrong. The chances of you passing group B strep to your baby are quite low, especially if you take antibiotics during labor. Talk to your provider about group B strep and share any concerns you have.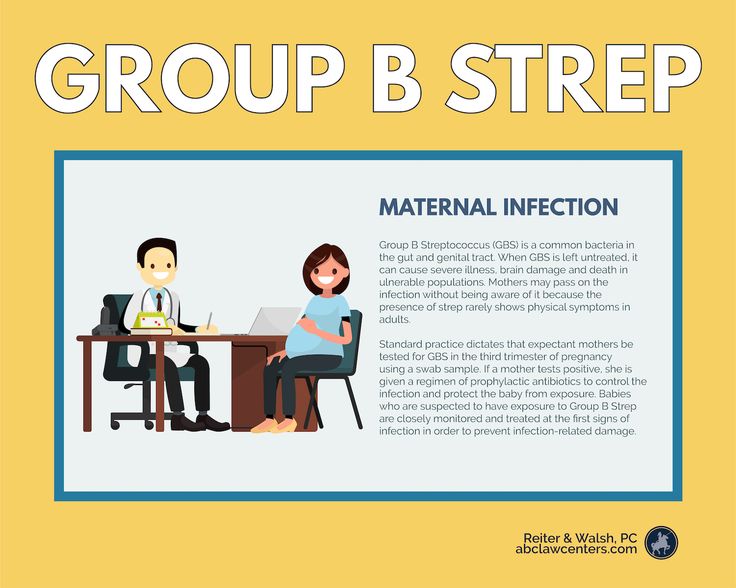 In most cases, testing positive for GBS causes no problems, and your baby is healthy.
In most cases, testing positive for GBS causes no problems, and your baby is healthy.
Article "Streptococcus B - danger during pregnancy"
Clinic of Gynecology and Oncogynecology
Moscow, st. Shchepkina, 35
Moscow, Spiridonievsky per., 5/1
Moscow, st. Pravdy, 15 building 1
Write to WhatsApp
Streptococcus B (Strept. Agalactiae) is a bacteria that is very often found in the vagina and/or lower intestines of women. They do not pose any danger to a non-pregnant woman, because. these bacteria may be part of the normal flora. In addition, even if this disease is treated, it may appear again after a few days.
It is also quite common during pregnancy - about 10% of pregnant women are thought to carry Streptococcus B.
The problem is that these bacteria can cause serious illness in newborns. It does not help the situation and the fact that the risk of disease in newborns is very small. Although streptococcus B is transmitted from every second mother to a child at birth, only 1% of infected babies will develop a neonatal infection.
It does not help the situation and the fact that the risk of disease in newborns is very small. Although streptococcus B is transmitted from every second mother to a child at birth, only 1% of infected babies will develop a neonatal infection.
Thus, we are talking about a banal and often occurring microbe, which, some time after the treatment of its carrier, will return again, which makes the treatment useless and dangerous. This microbe is very often transmitted to newborns, without bringing the latter any harm, not counting 1% of babies.
Taking into account these features of the disease, the scientific community recommends the following recommendations:
Systematic diagnosis of Streptococcus B is recommended at the end of pregnancy, between 34 and 38 weeks amenorrhea;
Treatment of asymptomatic disease in women in early and mid-pregnancy is not justified. This means that you should not treat Streptococcus B during pregnancy, except for the presence of infectious signs or a dangerous condition of the patient (rupture of the amniotic membranes).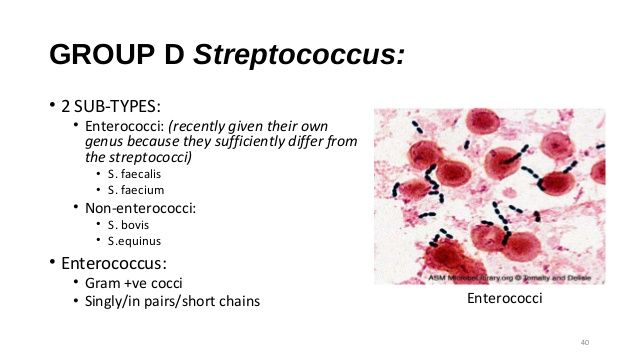
But in case of a positive test result during childbirth, it is necessary to carry out antibiotic prophylaxis. It is carried out with antibiotics of the penicillin series (penicillin or amoxicillin).
Rate
Average: 3.95 (20 ratings)
Clinic of Gynecology and Oncogynecology
Moscow, st. Shchepkina, 35
Moscow, Spiridonievsky per., 5/1
Moscow, st. Pravdy, 15 building 1
Write to WhatsApp
Doctors and staff
IMPORTANT QUESTIONS ABOUT PREGNANCY | About vitamins, nutrition, shoes, etc...
November 02
All videos
Clinic of Gynecology and Oncogynecology
Dear Vladimir Borisovich! Thank you from the bottom of my heart. You are truly a doctor from God with a capital letter. Thanks to your professionalism, kindness, tact, charm and talent, I believed in the success of the upcoming operation immediately at the first meeting at your appointment, you explained everything so intelligibly and convincingly that there was complete confidence in success. The operation you have done is fantastic! The very next day it was possible to sit, get up and groom, and on the third day I was discharged home. Just great. A month later, I completely forgot about the problems that I had before the operation. Once again, many thanks to you and your team, God bless you with health, well-being and success. You are a miracle doctor!!! Best regards, Antonina
You are truly a doctor from God with a capital letter. Thanks to your professionalism, kindness, tact, charm and talent, I believed in the success of the upcoming operation immediately at the first meeting at your appointment, you explained everything so intelligibly and convincingly that there was complete confidence in success. The operation you have done is fantastic! The very next day it was possible to sit, get up and groom, and on the third day I was discharged home. Just great. A month later, I completely forgot about the problems that I had before the operation. Once again, many thanks to you and your team, God bless you with health, well-being and success. You are a miracle doctor!!! Best regards, Antonina
Antonina, Moscow
All reviews
Borderline ovarian tumors
02 November 2022
All stories
Infections during pregnancy.
 Detection of group B streptococcus
Detection of group B streptococcus 05/16/2017
Infections during pregnancy that can be transmitted from mother to fetus deserve great attention, as they carry a potential risk of infection of the fetus or newborn and may lead to undesirable consequences. In addition, the diagnosis of infections during pregnancy has certain characteristics due to the asymptomatic course of most maternal infections or non-specific signs and symptoms.
Group B Streptococcus (GBS, Streptococcus agalactiae ) - Causes severe neonatal illness and poses a risk to certain patients in other age groups.
It has been estimated that GBS in 30% of pregnant women can be found in the vagina and often in the urethra of their sexual partners. Despite the fact that GBS can occur as part of the normal intestinal microflora of a woman, their colonization of the urogenital tract of a pregnant woman poses a significant risk to the fetus due to the possibility of ascending infection. There is a significant relationship between the carriage of GBS in the vagina, not only with early infection of newborns (sepsis, pneumonia and meningitis), but also with premature birth, premature discharge of amniotic fluid, urinary infection in pregnant women, development of chorioamnionitis during childbirth, endometritis.
There is a significant relationship between the carriage of GBS in the vagina, not only with early infection of newborns (sepsis, pneumonia and meningitis), but also with premature birth, premature discharge of amniotic fluid, urinary infection in pregnant women, development of chorioamnionitis during childbirth, endometritis.
In the USA, Canada and European countries, regulated National programs for the prevention and treatment of GBS infections have been adopted, which are mandatory for all medical institutions.
From 01.05.17, DILA ML introduces a new study “Identification of group B streptococcus (streptococcus agalactiae) with sensitivity to antibiotics”.
| Prompt identification of pregnant women who are positive for group B streptococcus and who have risk factors for an increased chance of infection in the newborn allows to conduct intravenous antibiotic prophylaxis with the onset of labor and prevent early infection of the newborn with group B streptococcus:
|
Rules for preparation : 24 hours before the use of intravaginal and rectal drugs, do not clean the external genitalia before taking the biomaterial.
The biomaterial is taken from two points: the lower third of the vagina and the next - the rectum, the overall result is evaluated.
Detection of group B streptococcus is carried out by a cultural method with the determination of sensitivity to antibiotics.
Research period: 6 days (Kyiv), 7.5 days (Regions).
Adequate assessment of the risk of infection of the newborn with group B streptococcus will significantly reduce the possibility of complications and ensure a favorable pregnancy outcome.
Literature:
1. Australasian society for infectious diseases, 2014
2. Antibiotic Prevention for Maternal Group B Streptococcal Colonization on Neonatal GBS-Related Adverse Outcomes: A Meta-Analysis, Shunming Li, Jingya Huang, 2017.