Giving birth dilation
The stages of labour and birth
1st stage of labour
During the 1st stage of labour, contractions make your cervix gradually open (dilate). This is usually the longest stage of labour.
At the start of labour, your cervix starts to soften so it can open. This is called the latent phase and you may feel irregular contractions. It can take many hours, or even days, before you're in established labour.
Established labour is when your cervix has dilated to about 4cm and regular contractions are opening your cervix.
During the latent phase, it's a good idea to have something to eat and drink because you'll need energy for when labour is established.
If your labour starts at night, try to stay comfortable and relaxed. Sleep if you can.
If your labour starts during the day, stay upright and gently active. This helps your baby move down into your pelvis and helps your cervix to dilate.
Breathing exercises, massage and having a warm bath or shower may help ease pain during this early stage of labour.
When to contact a midwife
Contact your midwifery team if:
- your contractions are regular and you're having about 3 in every 10-minute period
- your waters break
- your contractions are very strong and you feel you need pain relief
- you're worried about anything
If you go into hospital or your midwifery unit before your labour has become established, they may suggest you go home again for a while.
Once labour is established, your midwife will check on you from time to time to see how you're progressing and offer you support, including pain relief if you need it.
You can either walk around or get into a position that feels comfortable to labour in.
Your midwife will offer you regular vaginal examinations to see how your labour is progressing. If you do not want to have these, you do not have to – your midwife can discuss with you why she's offering them.
Your cervix needs to open about 10cm for your baby to pass through it. This is what's called being fully dilated.
In a 1st labour, the time from the start of established labour to being fully dilated is usually 8 to 12 hours. It's often quicker (around 5 hours), in a 2nd or 3rd pregnancy.
When you reach the end of the 1st stage of labour, you may feel an urge to push.
Monitoring your baby in labour
Your midwife will monitor you and your baby during labour to make sure you're both coping well.
This will include using a small handheld device to listen to your baby's heart every 15 minutes. You'll be free to move around as much as you want.
You'll be free to move around as much as you want.
Your midwife may suggest electronic monitoring if there are any concerns about you or your baby, or if you choose to have an epidural.
Electronic monitoring involves strapping 2 pads to your bump. One pad is used to monitor your contractions and the other is used to monitor your baby's heartbeat. These pads are attached to a monitor that shows your baby's heartbeat and your contractions
Sometimes a clip called a foetal heart monitor can be attached to the baby's head instead. This can give a more accurate measurement of your baby's heartbeat.
You can ask to be monitored electronically even if there are no concerns. Having electronic monitoring can sometimes restrict how much you can move around.
If you have electronic monitoring with pads on your bump because there are concerns about your baby's heartbeat, you can take the monitor off if your baby's heartbeat is shown to be normal.
A foetal scalp monitor will usually only be removed just as your baby is born, not before.
Speeding up labour
Labour can sometimes be slower than expected. This can happen if your contractions are not coming often enough, are not strong enough, or if your baby is in an awkward position.
If this is the case, your doctor or midwife may talk to you about 2 ways to speed up your labour: breaking your waters or an oxytocin drip.
Breaking your waters
Breaking the membrane that contains the fluid around your baby (your waters) is often enough to make contractions stronger and more regular. This is also known as artificial rupture of the membranes (ARM).
Your midwife or doctor can do this by making a small break in the membrane during a vaginal examination. This may make your contractions feel stronger and more painful, so your midwife will talk to you about pain relief.
Oxytocin drip
If breaking your waters does not work, your doctor or midwife may suggest using a drug called oxytocin (also known as syntocinon) to make your contractions stronger. This is given through a drip that goes into a vein, usually in your wrist or arm.
Oxytocin can make your contractions stronger and more regular and can start to work quite quickly, so your midwife will talk to you about your options for pain relief.
You will also need electronic monitoring to check your baby is coping with the contractions, as well as regular vaginal examinations to check the drip is working.
2nd stage of labour
The 2nd stage of labour lasts from when your cervix is fully dilated until the birth of your baby.
Finding a position to give birth in
Your midwife will help you find a comfortable position to give birth in. You may want to sit, lie on your side, stand, kneel, or squat, although squatting may be difficult if you're not used to it.
You may want to sit, lie on your side, stand, kneel, or squat, although squatting may be difficult if you're not used to it.
If you've had lots of backache while in labour, kneeling on all fours may help. It's a good idea to try some of these positions before you go into labour. Talk to your birth partner so they know how they can help you.
Find out what your birth partner can do.
Pushing your baby out
When your cervix is fully dilated, your baby will move further down the birth canal towards the entrance to your vagina. You may get an urge to push that feels a bit like you need to poo.
You can push during contractions whenever you feel the urge. You may not feel the urge to push immediately. If you have had an epidural, you may not feel an urge to push at all.
If you're having your 1st baby, this pushing stage should last no longer than 3 hours. If you've had a baby before, it should take no more than 2 hours.
If you've had a baby before, it should take no more than 2 hours.
This stage of labour is hard work, but your midwife will help and encourage you. Your birth partner can also support you.
What happens when your baby is born
When your baby's head is almost ready to come out, your midwife will ask you to stop pushing and take some short breaths, blowing them out through your mouth.
This is so your baby's head can be born slowly and gently, giving the skin and muscles in the area between your vagina and anus (the perineum) time to stretch.
Sometimes your midwife or doctor will suggest an episiotomy to avoid a tear or to speed up delivery. This is a small cut made in your perineum.
You'll be given a local anaesthetic injection to numb the area before the cut is made. Once your baby is born, an episiotomy, or any large tears, will be stitched closed.
Find out about your body after the birth, including how to deal with stitches.
Once your baby's head is born, most of the hard work is over. The rest of their body is usually born during the next 1 or 2 contractions.
You'll usually be able to hold your baby immediately and enjoy some skin-to-skin time together.
You can breastfeed your baby as soon as you like. Ideally, your baby will have their 1st feed within 1 hour of birth.
Read more about skin-to-skin contact and breastfeeding in the first few days.
3rd stage of labour
The 3rd stage of labour happens after your baby is born, when your womb contracts and the placenta comes out through your vagina.
There are 2 ways to manage this stage of labour:
- active – when you have treatment to make it happen faster
- physiological – when you have no treatment and this stage happens naturally
Your midwife will explain both ways to you while you're still pregnant or during early labour, so you can decide which you would prefer.
There are some situations where physiological management is not advisable. Your midwife or doctor can explain if this is the case for you.
What is active management?
Your midwife will give you an injection of oxytocin into your thigh as you give birth, or soon after. This makes your womb contract.
Evidence suggests it's better not to cut the umbilical cord immediately, so your midwife will wait to do this between 1 and 5 minutes after birth. This may be done sooner if there are concerns about you or your baby – for example, if the cord is wound tightly around your baby's neck.
Once the placenta has come away from your womb, your midwife pulls the cord – which is attached to the placenta – and pulls the placenta out through your vagina. This usually happens within 30 minutes of your baby being born.
Active management speeds up the delivery of the placenta and lowers your risk of having heavy bleeding after the birth (postpartum haemorrhage), but it increases the chance of you feeling and being sick. It can also make afterpains (contraction-like pains after birth) worse.
It can also make afterpains (contraction-like pains after birth) worse.
Read about preventing heavy bleeding on our page What happens straight after the birth.
What is physiological management?
No oxytocin injection is given, and the 3rd stage of labour happens naturally.
The cord is not cut until it has stopped pulsing. This means blood is still passing from the placenta to your baby. This usually takes around 2 to 4 minutes.
Once the placenta has come away from your womb, you should feel some pressure in your bottom and you'll need to push the placenta out. It can take up to an hour for the placenta to come away, but it usually only takes a few minutes to push it out.
If the placenta does not come away naturally or you begin to bleed heavily, you'll be advised by your midwife or doctor to switch to active management. You can do this at any time during the 3rd stage of labour.
You can do this at any time during the 3rd stage of labour.
Read more about what happens straight after you give birth.
Video: What positions are best for giving birth?
In this video, a midwife talks through some of the best positions to give birth.
Media last reviewed: 20 March 2020
Media review due: 20 March 2023
Cervix Dilation Chart: Stages of Labor
The cervix, which is the lowest portion of the uterus, opens when a woman has a baby, through a process called cervical dilation. The process of the cervix opening (dilating) is one way that healthcare staff track how a woman’s labor is progressing.
During labor, the cervix opens to accommodate the passage of baby’s head into the vagina, which is around 10 centimeters (cm) dilated for most term babies.
If your cervix is dilated with regular, painful contractions, you’re in active labor and getting closer to delivering your baby.
The first stage of labor is divided into two parts: the latent and active phases.
Latent phase of laborThe latent phase of labor is the first stage of labor. It can be thought of more as the “waiting game” stage of labor. For first-time moms, it can take a while to move through the latent phase of labor.
In this stage, contractions aren’t yet strong or regular. The cervix is essentially “warming up,” softening, and shortening as it prepares for the main event.
You might consider picturing the uterus as a balloon. Think of the cervix as the neck and opening of the balloon. As you fill that balloon up, the neck of the balloon draws up with the pressure of the air behind it, similar to the cervix.
The cervix is simply the bottom opening of the uterus drawing up and opening wider to make room for the baby.
Active stage of laborA woman is considered to be in the active stage of labor once the cervix dilates to around 5 to 6 cm and contractions begin to get longer, stronger, and closer together.
The active stage of labor is characterized more by the rate of regular cervical dilation per hour. Your doctor will expect to see your cervix opening at a more regular rate during this stage.
How long does stage 1 of labor last?There’s no scientific hard and fast rule for how long the latent and active phases last in women. The active stage of labor can range from a woman dilating anywhere from 0.5 cm per hour up to 0.7 cm per hour.
How fast your cervix dilates will also depend on if it’s your first baby or not. Mothers who have delivered a baby before tend to move more quickly through labor.
Some women will simply progress more quickly than others. Some women may “stall” at a certain stage, and then dilate very quickly.
In general, once the active stage of labor kicks in, it’s a safe bet to expect a steady cervical dilation every hour. Many women don’t start really dilating more regularly until closer to around 6 cm.
The first stage of labor ends when a woman’s cervix is fully dilated to 10 cm and fully effaced (thinned out).
The second stage of labor begins when a woman’s cervix is fully dilated to 10 centimeters. Even though a woman is fully dilated, it doesn’t mean that the baby is necessarily going to be delivered immediately.
A woman may reach full cervical dilation, but the baby may still need time to move down the birth canal fully to be ready for birth. Once the baby is in prime position, it’s time to push. The second stage ends after the baby is delivered.
How long does stage 2 of labor last?In this stage, there’s again a wide range for how long it can take for the baby to come out. It can last anywhere from minutes to hours. Women may deliver with only a few hard pushes, or push for an hour or more.
Pushing occurs only with contractions, and the mother is encouraged to rest between them. At this point, the ideal frequency of contractions will be about 2 to 3 minutes apart, lasting 60 to 90 seconds.
In general, pushing takes longer for first-time pregnant people and for women who have had epidurals. Epidurals can reduce the woman’s urge to push and interfere with her ability to push. How long a woman is allowed to push depends on:
Epidurals can reduce the woman’s urge to push and interfere with her ability to push. How long a woman is allowed to push depends on:
- the hospital’s policy
- the doctor’s discretion
- the health of the mom
- the health of the baby
The mother should be encouraged to change positions, squat with support, and rest between contractions. Forceps, vacuum, or cesarean delivery is considered if the baby isn’t progressing or the mother is becoming exhausted.
Again, every woman and baby is different. There’s no universally accepted “cut-off time” for pushing.
The second stage ends with the birth of the baby.
The third stage of labor is perhaps the most forgotten phase. Even though the “main event” of birth has occurred with the birth of the baby, a woman’s body still has important work to do. In this stage, she’s delivering the placenta.
A woman’s body actually grows an entirely new and separate organ with the placenta. Once the baby is born, the placenta no longer has a function, so her body must expel it.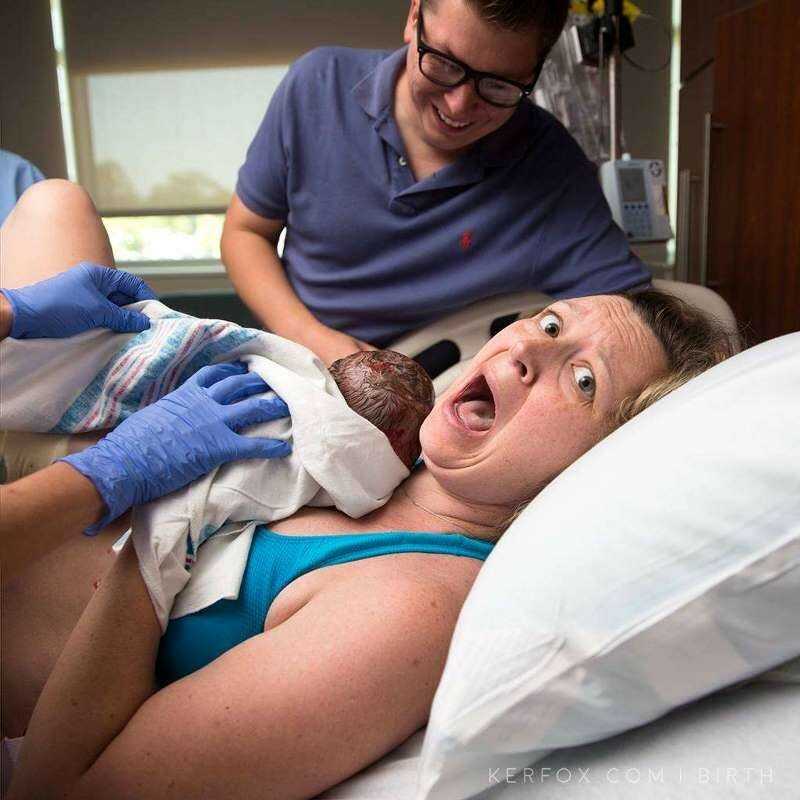
The placenta is delivered the same way as the baby, through contractions. They may not feel as strong as the contractions that are needed to expel the baby. The doctor directs the mother to push and the delivery of the placenta is typically over with one push.
How long does stage 3 of labor last?The third stage of labor can last anywhere from 5 to 30 minutes. Putting the baby on the breast for breastfeeding will hasten this process.
Postpartum recovery
Once the baby is born and the placenta has been delivered, the uterus contracts and the body recovers. This is often referred to as the fourth stage of labor.
After the hard work of moving through the stages of labor is finished, a woman’s body will need time to return to its nonpregnant state. On average, it takes about 6 weeks for the uterus to return to its nonpregnant size and for the cervix to return to its prepregnancy state.
Induction of labor or induction of labor
The purpose of this informational material is to familiarize the patient with the induction of labor procedure and to provide information on how and why it is performed.
In most cases, labor begins between the 37th and 42nd weeks of pregnancy. Such births are called spontaneous. If drugs or medical devices are used before the onset of spontaneous labor, then the terms "stimulated" or "induced" labor are used in this case.
Labor should be induced when further pregnancy is for some reason unsafe for the mother or baby and it is not possible to wait for spontaneous labor to begin.
The purpose of stimulation is to start labor by stimulating uterine contractions.
When inducing labor, the patient must be in the hospital so that both mother and baby can be closely monitored.
Labor induction methods
The choice of labor induction method depends on the maturity of the cervix of the patient, which is assessed using the Bishop scale (when viewed through the vagina, the position of the cervix, the degree of its dilatation, consistency, length, and the position of the presenting part of the fetus in the pelvic area are assessed). Also important is the medical history (medical history) of the patient, for example, a past caesarean section or operations on the uterus.
Also important is the medical history (medical history) of the patient, for example, a past caesarean section or operations on the uterus.
The following methods are used to induce (stimulate) labor:
- Oral misoprostol is a drug that is a synthetic analogue of prostaglandins found in the body. It prepares the body for childbirth, under its action the cervix becomes softer and begins to open.
- Balloon Catheter - A small tube is placed in the cervix and the balloon attached to the end is filled with fluid to apply mechanical pressure to the cervix. When using this method, the cervix becomes softer and begins to open. The balloon catheter is kept inside until it spontaneously exits or until the next gynecological examination.
- Amniotomy or opening of the fetal bladder - in this case, during a gynecological examination, when the cervix has already dilated sufficiently, the fetal bladder is artificially opened. When the amniotic fluid breaks, spontaneous uterine contractions will begin, or intravenous medication may be used to stimulate them.

- Intravenously injected synthetic oxytocin - acts similarly to the hormone of the same name produced in the body. The drug is given by intravenous infusion when the cervix has already dilated (to support uterine contractions). The dose of the drug can be increased as needed to achieve regular uterine contractions.
When is it necessary to induce labor?
Labor induction is recommended when the benefits outweigh the risks.
Induction of labor may be indicated in the following cases:
- The patient has a comorbid condition complicating pregnancy (eg, high blood pressure, diabetes mellitus, preeclampsia, or some other condition).
- The duration of pregnancy is already exceeding the norm - the probability of intrauterine death of the fetus increases after the 42nd week of pregnancy.
- Fetal problems, eg, problems with fetal development, abnormal amount of amniotic fluid, changes in fetal condition, various fetal disorders.

- If the amniotic fluid has broken and uterine contractions have not started within the next 24 hours, there is an increased risk of inflammation in both the mother and the fetus. This indication does not apply in case of preterm labor, when preparation of the baby's lungs with a special medicine is necessary before delivery.
- Intrauterine fetal death.
What are the risks associated with labor induction?
Labor induction is not usually associated with significant complications.
Occasionally, after receiving misoprostol, a patient may develop fever, chills, vomiting, diarrhea, and too frequent uterine contractions (tachysystole). In case of too frequent contractions to relax the uterus, the patient is injected intravenously relaxing muscles uterus medicine. It is not safe to use misoprostol if you have had a previous caesarean section as there is a risk of rupture of the uterine scar.
The use of a balloon catheter increases the risk of inflammation inside the uterus.
When using oxytocin, the patient may rarely experience a decrease in blood pressure, tachycardia (rapid heartbeat), hyponatremia (lack of sodium in the blood), which may result in headache, loss of appetite, nausea, vomiting, abdominal pain, depression strength and sleepiness.
Induction of labor, compared with spontaneous labor, increases the risk of prolonged labor, the need for instrumentation
(use of vacuum or forceps), postpartum hemorrhage, uterine rupture, the onset of too frequent uterine contractions and the associated deterioration of the fetus, prolapse umbilical cord, as well as premature detachment of the placenta.
If induction of labor is not successful
The time frame for induction of labor varies from patient to patient, on average labor begins within 24-72 hours. Sometimes more than one method is required.
The methods used do not always work equally quickly and in the same way on different patients. If the cervix does not dilate as a result of induction of labor, your doctor will tell you about your next options (which may include inducing labor later, using a different method, or delivering by caesarean section).
If the cervix does not dilate as a result of induction of labor, your doctor will tell you about your next options (which may include inducing labor later, using a different method, or delivering by caesarean section).
ITK833
This informational material was approved by the Women's Clinic on 01/01/2022.
Stages of childbirth - disclosure, expulsion, birth of the placenta.
Catalog of maternity hospitals
Perinatal center MMCC Kommunarka — childbirth under the compulsory medical insurance policy
Everything about the new Perinatal Center in Kommunarka: conditions of stay, features, photo, address, phone.
Catalog of maternity hospitals
Perinatal center GKB №67 named after. L.A. Vorokhobov — childbirth under the MHI policy
Perinatal Center City Clinical Hospital No. 67 named after. L.A. Vorokhobova - reviews, doctors, registration for childbirth free of charge under compulsory medical insurance.
Catalog of maternity hospitals
Family Planning and Reproduction Center – childbirth free of charge under compulsory health insurance
TsPSiR on Sevastopolskaya - about the center, reviews, doctors, an appointment for childbirth under the MHI policy.
Catalog of maternity hospitals Bauman - childbirth under the MHI policy
Perinatal Center of the City Clinical Hospital No. 29 named after N.E. Bauman on Hospital Square, 2. Registration for childbirth is free of charge under the compulsory medical insurance policy.
Catalog of maternity hospitals
O.M. Filatov - childbirth under the MHI policy
Maternity hospital GKB No. 15 named after. O.M. Filatov on Vykhino, st. Veshnyakovskaya, d.
Catalog of maternity hospitals
Perinatal center S.S. Yudina - childbirth under the MHI policy
Maternity hospital No. 7 GKB im. S.S. Yudina on Kolomensky passage, 4, building 2. Registration for childbirth is free of charge under the MHI policy.
Catalog of maternity hospitals
Maternity ward №2 A.K. Yeramishantseva (Maternity Hospital No. 40) - childbirth under the compulsory medical insurance policy
Maternity Ward No. 2 of the City Clinical Hospital named after. A.K. Eramishantseva (Maternity Hospital No. 40) on Taimyrskaya, 6. Registration for childbirth is free of charge under the compulsory medical insurance policy.
A.K. Eramishantseva (Maternity Hospital No. 40) on Taimyrskaya, 6. Registration for childbirth is free of charge under the compulsory medical insurance policy.
Catalog of maternity hospitals
Maternity ward No. 1 A.K. Yeramishantseva - childbirth under the policy of OMS
Maternity Ward No. 1 of the City Clinical Hospital named after. A.K. Yeramishantsev. Registration for childbirth is free of charge under the compulsory medical insurance policy.
Catalog of maternity hospitals
Maternity hospital №3 GKB №67 named after. L.A. Vorokhobova (previously RD No. 3 TsPSiR Branch No. 4) - childbirth under the MHI policy
Maternity hospital No. 3 GKB No. 67 named after. L.A. Vorokhobov on Nezhinskaya, 3 (formerly RD No. 3 TsPSiR Branch No. 4). Registration for childbirth is free of charge under the compulsory medical insurance policy.
Catalog of maternity hospitals
Maternity hospital No. 52 - childbirth under the compulsory medical insurance policy
Maternity hospital No. 26 at the city clinical hospital No. 52 on Sosnovaya, 11. Registration for childbirth is free of charge under the compulsory medical insurance policy.
26 at the city clinical hospital No. 52 on Sosnovaya, 11. Registration for childbirth is free of charge under the compulsory medical insurance policy.
Catalog of maternity hospitals
Perinatal center GKB im. M.P. Konchalovsky - childbirth under the policy of compulsory medical insurance
Perinatal Center of the City Clinical Hospital named after. M.P. Konchalovsky in Zelenograd. Registration for childbirth is free of charge under the compulsory medical insurance policy.
Catalog of maternity hospitals
Maternity hospital №2 GKB im. F. I. Inozemtseva (formerly maternity hospital No. 20 of the D. D. Pletnev City Clinical Hospital) - childbirth under the compulsory medical insurance policy
Maternity hospital No. 2 GKB im. F.I. Inozemtseva (formerly the Maternity Hospital No. 20 of the Pletnev City Clinical Hospital) on Verkhnaya Pervomaiskaya, 57. Registration for childbirth is free of charge under the CHI policy.
Catalog of maternity hospitals
F. I. Inozemtseva — childbirth under the compulsory medical insurance policy
I. Inozemtseva — childbirth under the compulsory medical insurance policy
Maternity hospital No. 36 GKB im. F.I. Inozemtseva on Fortunatovskaya, 1, bldg. 2. Registration for childbirth is free of charge under the CHI policy.
Catalog of maternity hospitals
Maternity hospital №4 GKB im. V.V. Vinogradova - childbirth under the MHI policy
Maternity hospital No. 4 GKB im. V.V. Vinogradova on the street. Novatorov, d. 3. Registration for childbirth is free of charge under the compulsory medical insurance policy.
Catalog of maternity hospitals
Maternity hospital GKB im. V.V. Veresaeva - childbirth under the policy of compulsory medical insurance
Maternity hospital No. 17 GKB im. V.V. Veresaeva on the 800th anniversary of Moscow, house 22. Registration for childbirth is free of charge under the compulsory medical insurance policy.
Catalog of maternity hospitals
Maternity hospital №27 V.V. Veresaeva (formerly RD No.