Embryo one week
Fetal development: Month-By-Month Stages of Pregnancy
When does a pregnancy start?
The start of pregnancy is actually the first day of your last menstrual period. This is called the gestational age, or menstrual age. It’s about two weeks ahead of when conception actually occurs. Though it may seem strange, the date of the first day of your last period will be an important date when determining your due date. Your healthcare provider will ask you about this date and will use it to figure out how far along you are in your pregnancy.
How does conception work?
Each month, your body goes through a reproductive cycle that can end in one of two ways. You will either have a menstrual period or become pregnant. This cycle is continuously happening during your reproductive years — from puberty in your teen years to menopause around age 50.
In a cycle that ends with pregnancy, there are several steps. First, a group of eggs (called oocytes) gets ready to leave the ovary for ovulation (release of the egg). The eggs develop in small, fluid-filled cysts called follicles. Think of these follicles as small containers for each immature egg. Out of this group of eggs, one will become mature and continue on through the cycle. This follicle then suppresses all the other follicles in the group. The other follicles stop growing at this point.
The mature follicle now opens and releases the egg from the ovary. This is ovulation. Ovulation generally happens about two weeks before your next menstrual period begins. It’s generally in the middle of your cycle.
After ovulation, the opened (ruptured) follicle develops into a structure called the corpus luteum. This secretes (releases) the hormones progesterone and estrogen. Progesterone helps prepare the endometrium (lining of the uterus). This lining is the place where a fertilized egg settles to develop. If you don’t become pregnant during a cycle, this lining is what is shed during your period.
On average, fertilization happens about two weeks after your last menstrual period. When the sperm penetrates the egg, changes occur in the protein coating of the egg to prevent other sperm from entering.
When the sperm penetrates the egg, changes occur in the protein coating of the egg to prevent other sperm from entering.
At the moment of fertilization, your baby’s genetic make-up is complete, including its sex. The sex of your baby depends on what sperm fertilizes the egg at the moment of conception. Generally, women have a genetic combination of XX and men have XY. Women provide each egg with an X. Each sperm can be either an X or a Y. If the fertilized egg and sperm is a combination of an X and Y, it’s a boy. If there are two Xs, it’s a girl.
What happens right after conception?
Within 24 hours after fertilization, the egg begins rapidly dividing into many cells. It remains in the fallopian tube for about three days after conception. Then the fertilized egg (now called a blastocyte) continues to divide as it passes slowly through the fallopian tube to the uterus. Once there, its next job is to attach to the endometrium. This is called implantation.
Before implantation though, the blastocyte breaks out of its protective covering.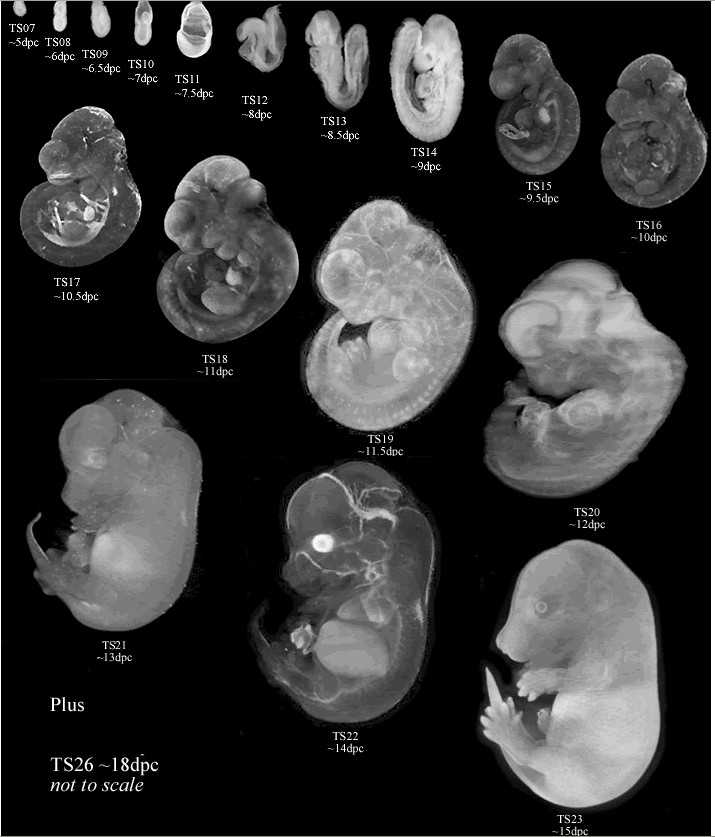 When the blastocyte makes contact with the endometrium, the two exchange hormones to help the blastocyte attach. Some women notice spotting (slight bleeding) during the one or two days when implantation happens. This is normal and isn’t something you should worry about. At this point, the endometrium becomes thicker and the cervix (the opening between your uterus and birth canal) is sealed by a plug of mucus.
When the blastocyte makes contact with the endometrium, the two exchange hormones to help the blastocyte attach. Some women notice spotting (slight bleeding) during the one or two days when implantation happens. This is normal and isn’t something you should worry about. At this point, the endometrium becomes thicker and the cervix (the opening between your uterus and birth canal) is sealed by a plug of mucus.
Within three weeks, the blastocyte cells ultimately form a little ball, or an embryo. By this time, the first nerve cells have formed.
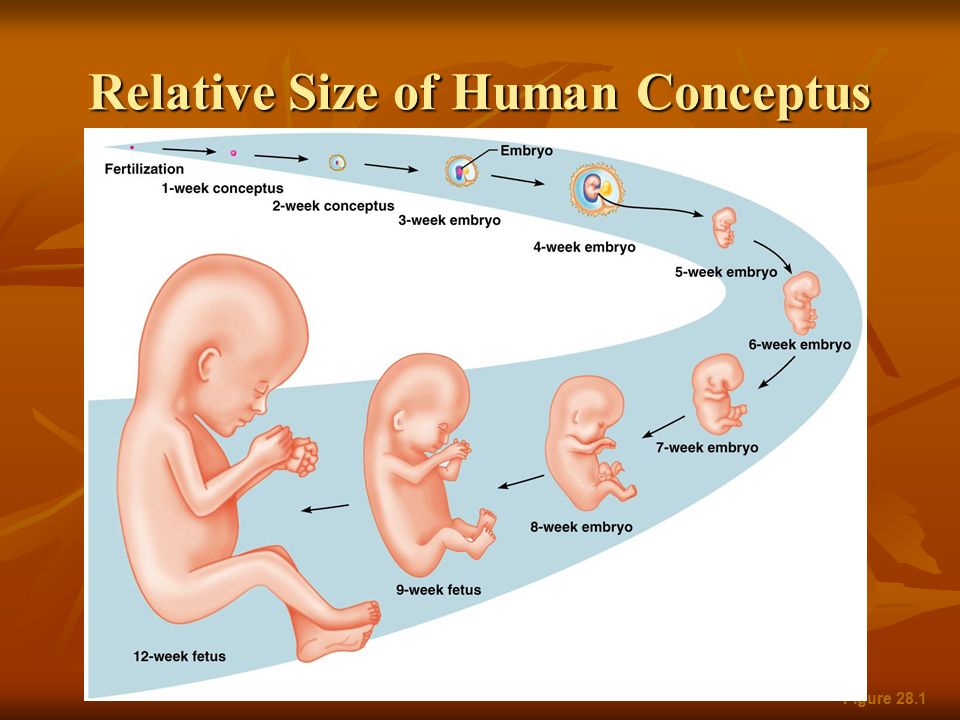
Your developing fetus has already gone through a few name changes in the first few weeks of pregnancy. Generally, it's called an embryo from conception until the eighth week of development. After the eighth week, it's called a fetus until it’s born.
How early can I know I’m pregnant?
From the moment of conception, the hormone human chorionic gonadotrophin (hCG) will be present in your blood. This hormone is created by the cells that form the placenta (food source for the growing fetus).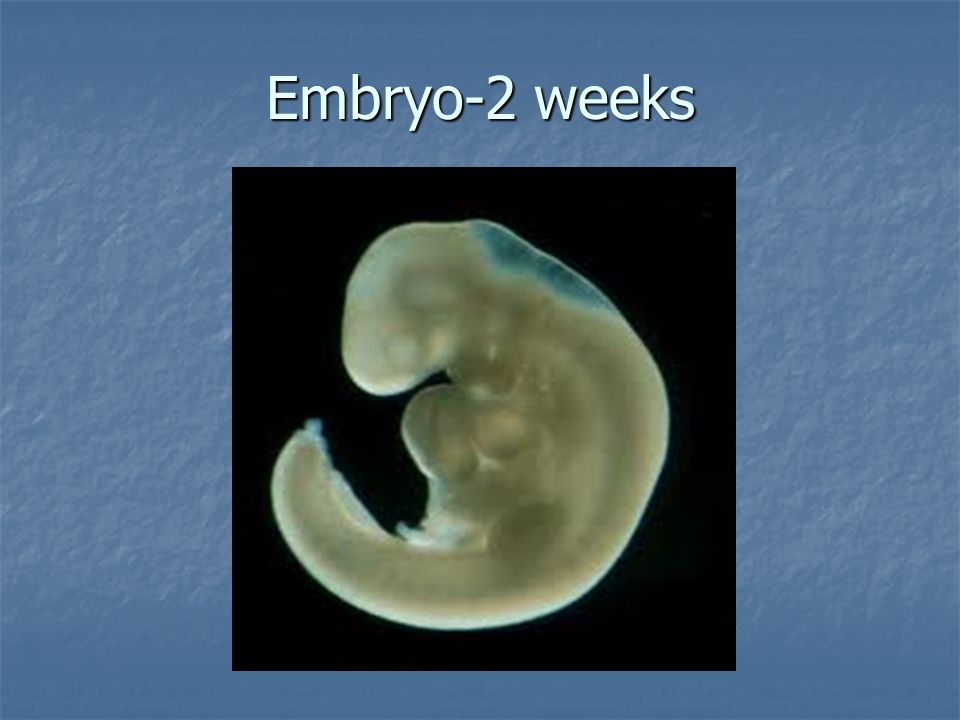 It’s also the hormone detected in a pregnancy test. Even though this hormone is there from the beginning, it takes time for it to build within your body. It typically takes three to four weeks from the first day of your last period for the hCG to increase enough to be detected by pregnancy tests.
It’s also the hormone detected in a pregnancy test. Even though this hormone is there from the beginning, it takes time for it to build within your body. It typically takes three to four weeks from the first day of your last period for the hCG to increase enough to be detected by pregnancy tests.
When should I reach out to my healthcare provider about a new pregnancy?
Most healthcare providers will have you wait to come in for an appointment until you have had a positive home pregnancy test. These tests are very accurate once you have enough hCG circulating throughout your body. This can be a few weeks after conception. It’s best to call your healthcare provider once you have a positive pregnancy test to schedule your first appointment.
When you call, your healthcare provider may ask you if you are taking a prenatal vitamin. These supplements contain folic acid. It’s important that you get at least 400mcg of folic acid each day during a pregnancy to make sure the fetus's neural tube (beginning of the brain and spine) develops correctly. Many healthcare providers suggest that you take prenatal vitamins with folic acid even when you aren’t pregnant. If you weren’t taking prenatal vitamins before your pregnancy, your provider may ask you to start as early as possible.
Many healthcare providers suggest that you take prenatal vitamins with folic acid even when you aren’t pregnant. If you weren’t taking prenatal vitamins before your pregnancy, your provider may ask you to start as early as possible.
What’s the timeline for fetal development?
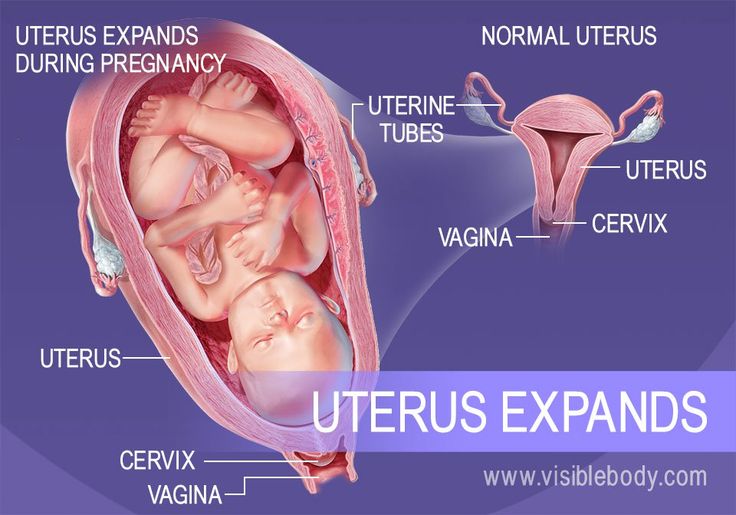
The fetus will change a lot throughout a typical pregnancy. This time is divided into three stages, called trimesters. Each trimester is a set of about three months. Your healthcare provider will probably talk to you about fetal development in terms of weeks. So, if you are three months pregnancy, you are about 12 weeks.
You will see distinct changes in the fetus, and yourself, during each trimester.
Traditionally, we think of a pregnancy as a nine-month process. However, this isn’t always the case. A full-term pregnancy is 40 weeks, or 280 days. Depending on what months you are pregnant during (some are shorter and some longer) and what week you deliver, you could be pregnant for either nine months or 10 months.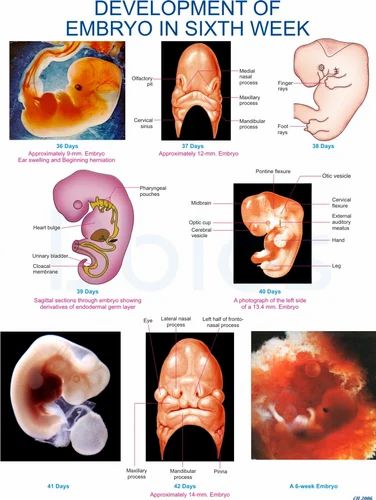 This is completely normal and healthy.
This is completely normal and healthy.
Once you get close to the end of your pregnancy, there are several category names you might hear regarding when you go into labor. These labels divide up the last few weeks of pregnancy. They’re also used to look out for certain complications in newborns. Babies that are born in the early term period or before may have a higher risk of breathing, hearing or learning issues than babies born a few weeks later in the full term time frame. When you’re looking at these labels, it’s important to know how they’re written. You may see the week first (38) and then you’ll see two numbers separated by a slash mark (6/7). This stands for how many days you currently are in the gestational week. So, if you see 38 6/7, it means that you are on day 6 of your 38th week.
The last few weeks of pregnancy are divided into the following groups:
- Early term: 37 0/7 weeks through 38 6/7 weeks.
- Full term: 39 0/7 weeks through 40 6/7 weeks.

- Late term: 41 0/7 weeks through 41 6/7 weeks.
- Post term: 42 0/7 weeks and on.
Talk to your healthcare provider about any questions you may have about gestational age and due date.
Stages of Growth Month-by-Month in Pregnancy
First trimester
The first trimester will span from conception to 12 weeks. This is generally the first three months of pregnancy. During this trimester, the fertilized egg will change from a small grouping of cells to a fetus that is starting to have a baby’s features.
Month 1 (weeks 1 through 4)
As the fertilized egg grows, a water-tight sac forms around it, gradually filling with fluid. This is called the amniotic sac, and it helps cushion the growing embryo.
During this time, the placenta also develops. The placenta is a round, flat organ that transfers nutrients from the mother to the fetus, and transfers wastes from the fetus. Think of the placenta as a food source for the fetus throughout your pregnancy.
In these first few weeks, a primitive face will take form with large dark circles for eyes. The mouth, lower jaw and throat are developing. Blood cells are taking shape, and circulation will begin. The tiny "heart" tube will beat 65 times a minute by the end of the fourth week.
By the end of the first month, the fetus is about 1/4 inch long – smaller than a grain of rice.
Month 2 (weeks 5 through 8)
Facial features continue to develop. Each ear begins as a little fold of skin at the side of the head. Tiny buds that eventually grow into arms and legs are forming. Fingers, toes and eyes are also forming.
The neural tube (brain, spinal cord and other neural tissue of the central nervous system) is well formed now. The digestive tract and sensory organs begin to develop too. Bone starts to replace cartilage.
The head is large in proportion to the rest of the body at this point. At about 6 weeks, a heartbeat can usually be detected.
After the 8th week, healthcare providers refer to it as a fetus instead of an embryo.
By the end of the second month, the fetus is about 1 inch long and weighs about 1/30 of an ounce.
Month 3 (weeks 9 through 12)
The arms, hands, fingers, feet and toes are fully formed. At this stage, the fetus is starting to explore a bit by doing things like opening and closing its fists and mouth. Fingernails and toenails are beginning to develop and the external ears are formed. The beginnings of teeth are forming under the gums. The reproductive organs also develop, but sex is still difficult to distinguish on ultrasound.
By the end of the third month, the fetus is fully formed. All the organs and limbs (extremities) are present and will continue to develop in order to become functional. The circulatory and urinary systems are also working and the liver produces bile.
At the end of the third month, the fetus is about 4 inches long and weighs about 1 ounce.
Since the most critical development has taken place, your chance of miscarriage drops considerably after three months.
Second trimester
This middle section of pregnancy is often thought of as the best part of the experience. By this time, any morning sickness is probably gone and the discomfort of early pregnancy has faded. The fetus will start to develop facial features during this month. You may also start to feel movement as the fetus flips and turns in the uterus. During this trimester, many people find out whether their baby will be designated male or female at birth. This is typically done during an anatomy scan (an ultrasound that checks physical development) around 20 weeks.
Month 4 (weeks 13 through 16)
The fetal heartbeat may now be audible through an instrument called a doppler. The fingers and toes are well-defined. Eyelids, eyebrows, eyelashes, nails and hair are formed. Teeth and bones become denser. The fetus can even suck his or her thumb, yawn, stretch and make faces.
The nervous system is starting to function. The reproductive organs and genitalia are now fully developed, and your doctor can see on ultrasound if the fetus will be designated male or female at birth.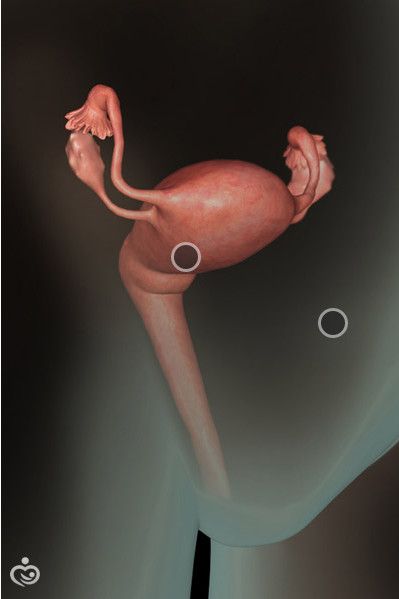
By the end of the fourth month, the fetus is about 6 inches long and weighs about 4 ounces.
Month 5 (weeks 17 through 20)
At this stage, you may begin to feel the fetus moving around. The fetus is developing muscles and exercising them. This first movement is called quickening and can feel like a flutter.
Hair begins to grow on the head. The shoulders, back and temples are covered by a soft fine hair called lanugo. This hair protects the fetus and is usually shed at the end of your baby's first week of life.
The skin is covered with a whitish coating called vernix caseosa. This "cheesy" substance is thought to protect fetal skin from the long exposure to the amniotic fluid. This coating is shed just before birth.
By the end of the fifth month, the fetus is about 10 inches long and weighs from 1/2 to 1 pound.
Month 6 (weeks 21 through 24)
If you could look inside the uterus right now, you would see that the fetus's skin is reddish in color, wrinkled and veins are visible through translucent skin.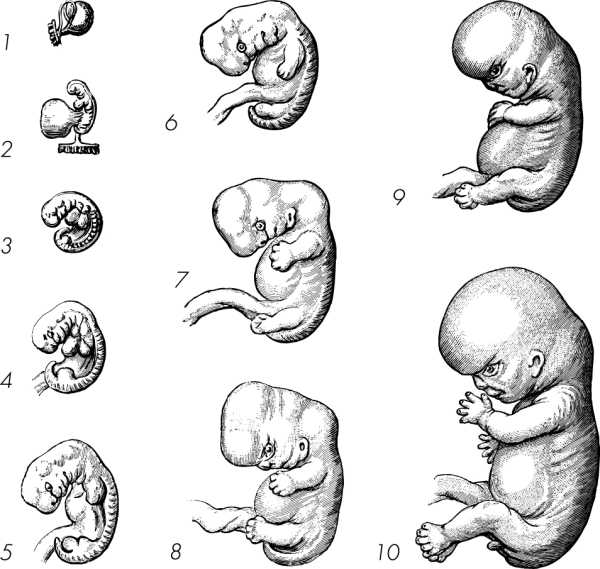 The finger and toe prints are visible. In this stage, the eyelids begin to part and the eyes open.
The finger and toe prints are visible. In this stage, the eyelids begin to part and the eyes open.
The fetus responds to sounds by moving or increasing the pulse. You may notice jerking motions if the fetus hiccups.
If born prematurely, your baby may survive after the 23rd week with intensive care.
By the end of the sixth month, the fetus is about 12 inches long and weighs about 2 pounds.
Month 7 (weeks 25 through 28)
The fetus continues to mature and develop reserves of body fat. At this point, hearing is fully developed. The fetus changes position frequently and responds to stimuli, including sound, pain and light. The amniotic fluid begins to diminish.
If born prematurely, your baby would be likely to survive after the seventh month.
At the end of the seventh month, the fetus is about 14 inches long and weighs from 2 to 4 pounds.
Third trimester
This is the final part of your pregnancy. You may be tempted to start the countdown till your due date and hope that it would come early, but each week of this final stage of development helps the fetus prepare for birth. Throughout the third trimester, the fetus gains weight quickly, adding body fat that will help after birth.
Throughout the third trimester, the fetus gains weight quickly, adding body fat that will help after birth.
Remember, even though popular culture only mentions nine months of pregnancy, you may actually be pregnant for 10 months. The typical, full-term pregnancy is 40 weeks, which can take you into a tenth month. It’s also possible that you can go past your due date by a week or two (41 or 42 weeks). Your healthcare provider will monitor you closely as you approach your due date. If you pass your due date, and don’t go into spontaneous labor, your provider may induce you. This means that medications will be used to make you go into labor and have the baby. Make sure to talk to your healthcare provider during this trimester about your birth plan.
Month 8 (weeks 29 through 32)
The fetus continues to mature and develop reserves of body fat. You may notice more kicking. The brain developing rapidly at this time, and the fetus can see and hear. Most internal systems are well developed, but the lungs may still be immature.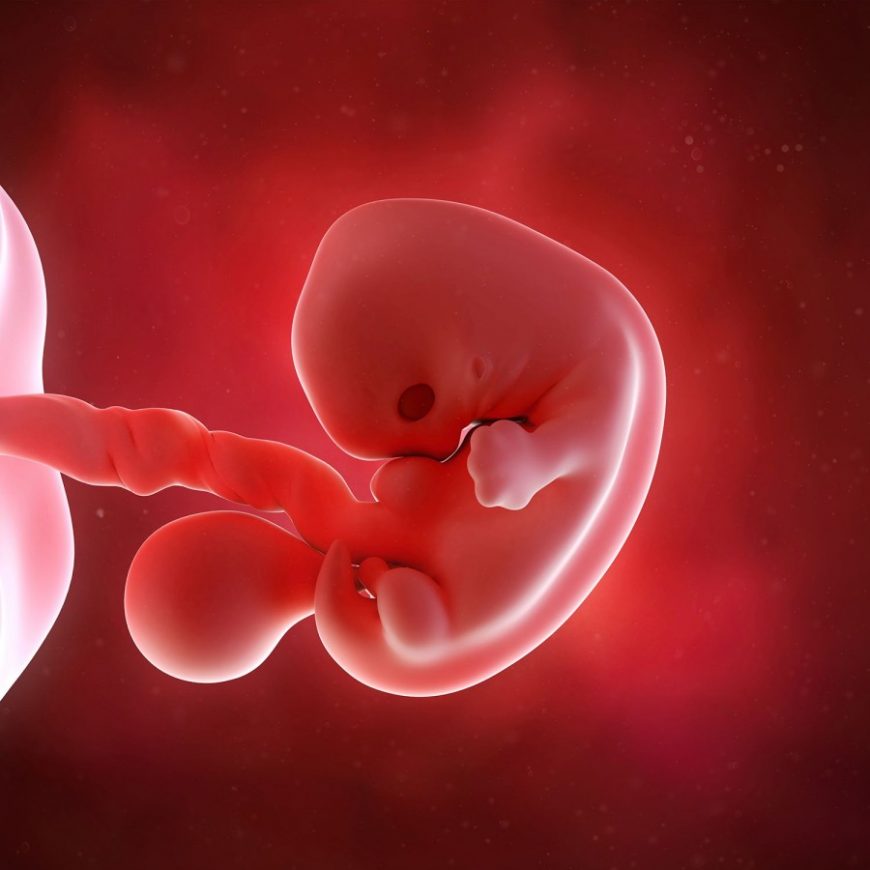
The fetus is about 18 inches long and weighs as much as 5 pounds.
Month 9 (weeks 33 through 36)
During this stage, the fetus continues to grow and mature. The lungs are close to being fully developed at this point.
The fetus has coordinated reflexes and can blink, close the eyes, turn the head, grasp firmly, and respond to sounds, light and touch.
The fetus is about 17 to 19 inches long and weighs from 5 ½ pounds to 6 ½ pounds.
Month 10 (Weeks 37 through 40)
In this final month, you could go into labor at any time. You may notice that less movement because space is tight. At this point, The fetus's position may have changed to prepare for birth. Ideally, it's head down in your uterus. You may feel very uncomfortable in this final stretch of time as the fetus drops down into your pelvis and prepares for birth.
Your baby is ready to meet the world at this point. They are about 18 to 20 inches long and weigh about 7 pounds.
Stages of Fetal Development - First Trimester
Stages of Fetal Development - First TrimesterStages of Fetal Development - First Trimester
One - 13 Weeks
| FERTILIZATION Biologically speaking, fertilization (or conception) is the beginning of human development. Fertilization normally occurs within several hours of ovulation (some authors report up to 24 hours) when a man's sperm combines with a woman's egg | |
| WEEK 2
| |
| WEEK 4
| |
| WEEK 6
| |
| WEEK 8
| |
| WEEK 10
| |
| WEEK 12
| |
Selective transfer of one embryo - articles from the specialists of the clinic "Mother and Child"
How often do we, reproductologists, hear from our patients: “I want twins”; “Please transfer me 2 or 3 embryos”; “I’m afraid not to get pregnant when transferring one embryo”; “My friend had 3 embryos transferred at another clinic and she got pregnant, I want that too.”
And today I would like to talk about indications, contraindications, risks and features of the transfer of 2-3 embryos .
We will talk about embryo transfer at the blastocyst stage (5-6 days of development), since at this stage the implantation potential of the embryo is higher than at the early stages of 1-4 days. It has been shown that a good quality early embryo showing even logical cleavage has a chance of implantation of about 50% (Van Royen et al., 2001; Denis et al. 2006). Whereas a morphologically correct blastocyst (categories AA, AB, BA, BC) can be implanted with a probability of 70% or more (Gardner D.K. 2000, Criniti A. 2005).
It has been shown that a good quality early embryo showing even logical cleavage has a chance of implantation of about 50% (Van Royen et al., 2001; Denis et al. 2006). Whereas a morphologically correct blastocyst (categories AA, AB, BA, BC) can be implanted with a probability of 70% or more (Gardner D.K. 2000, Criniti A. 2005).
Multiple pregnancy is a chance to become parents of two or three children of the same age. The family immediately becomes bigger and happier. However, such a family acquires a number of features, including psychological ones.
The process of gaining individuality in twins is more difficult. Due to their special relationship with twins, they grow up in a somewhat unusual atmosphere from early childhood. All the problems associated with raising a child are more pronounced in "twin" families, and their resolution requires much more effort from parents. And the point here is not only that the problems are multiplied by two.
But even if future parents are ready for this, then there are other aspects.
However, multiple pregnancy often :
· Premature multiple births
· Children with low birth weight
· High perinatal morbidity and mortality
The frequency of hospitalization for pregnancy in patients with singleton pregnancy is 12-13%, and with multiple pregnancy - 50-60%
Frequency of cerebral palsy with multiple pregnancy up to 13%
According to the results of numerous foreign and Russian studies, with the transfer of one embryo, the pregnancy rate is 50-60%. The transfer of two embryos increases the chance of pregnancy by 15%, and the birth rate of a full-term baby drops by 40%.
It is well known that multiple pregnancy after IVF can be avoided if no more than 1 embryo is transferred. Although in some cases, even with the transfer of 1 embryo, a multiple pregnancy may occur, as a result of the separation of blastomeres from each other.
Although in some cases, even with the transfer of 1 embryo, a multiple pregnancy may occur, as a result of the separation of blastomeres from each other.
In determining the number of embryos transferred into the uterine cavity, the reproductologist takes into account many factors: the age of the patient, the number of IVF attempts, the presence of concomitant gynecological (uterine fibroids, decreased ovarian reserve, scar on the uterus, in patients with a history of miscarriage, APS, etc.) and somatic pathology (hypertension, bronchial asthma, diabetes mellitus, etc.), the quality of the embryos, even the physique, weight and height of the patient are taken into account.
Indications for 1 embryo transfer:
- First IVF attempt
- Previous successful IVF attempts
- Age up to 35 years
- Program with donor oocytes
- More than 1 embryo at the blastocyst stage
Selective (that is, when there are several embryos at the blastocyst stage and there is an opportunity to choose) single embryo transfer is indicated for patients under the age of 35 with tubal-peritoneal and / or male factor infertility, with normal ovarian reserve, fertile and / or subfertile sperm of the spouse, who have no more than two ineffective IVF cycles in history. The effectiveness of the IVF program in this category of couples with selective transfer of one embryo is comparable to that with the transfer of 2 embryos with a 10-fold reduction in the risk of multiple pregnancy!!!
The effectiveness of the IVF program in this category of couples with selective transfer of one embryo is comparable to that with the transfer of 2 embryos with a 10-fold reduction in the risk of multiple pregnancy!!!
There are a number of clinical and embryological factors that reduce the effectiveness of the IVF procedure in patients of older reproductive age - the presence of a "weak response" of the ovaries due to a decrease in the ovarian reserve, respectively, a smaller number of oocytes received, a decrease in their ability to fertilize, the state of somatic and gynecological health. It has been shown that with the age of a woman, the rate of embryo cleavage decreases, the frequency of their fragmentation increases, the proportion of embryos with cytogenetic defects increases, and, in general, the number of embryos with normal morphology decreases. Despite the improvement of ovulation stimulation schemes, the use of technological embryological methods (ooplasma replacement, auxiliary "hatching"), the effectiveness of ART in older women remains quite low (using their own eggs). In this regard, an increase in the number of embryos transferred into the uterine cavity improves the chances of becoming pregnant in this group of women.
In this regard, an increase in the number of embryos transferred into the uterine cavity improves the chances of becoming pregnant in this group of women.
However, there are a number of contraindications for the transfer of two embryos in any group of patients:
- Scar on the uterus (after caesarean section, myomectomy, plastic surgery on the uterus)
- Malformations of the uterus (saddle/bicorn uterus)
- Severe mutations of the hemostasis system (Leiden, mutations in the prothrombin gene, antithrombin 3)
- Miscarriage
- Operations on the cervix (conization, amputation of the cervix)
- Severe somatic pathology
- Height less than 155 cm
Even taking into account the economic cost, the IVF protocol, the frozen embryo transfer protocol and two consecutive births after IVF are equal to the cost of carrying, nursing and having twins after IVF.
And in conclusion, I would like to say, dear patients, listen to the recommendations of your fertility doctors, because a “successful” protocol is not just a positive pregnancy test, not twins born at 24 weeks who spent several months in the pediatric intensive care unit; A “successful” protocol is a healthy baby born at term .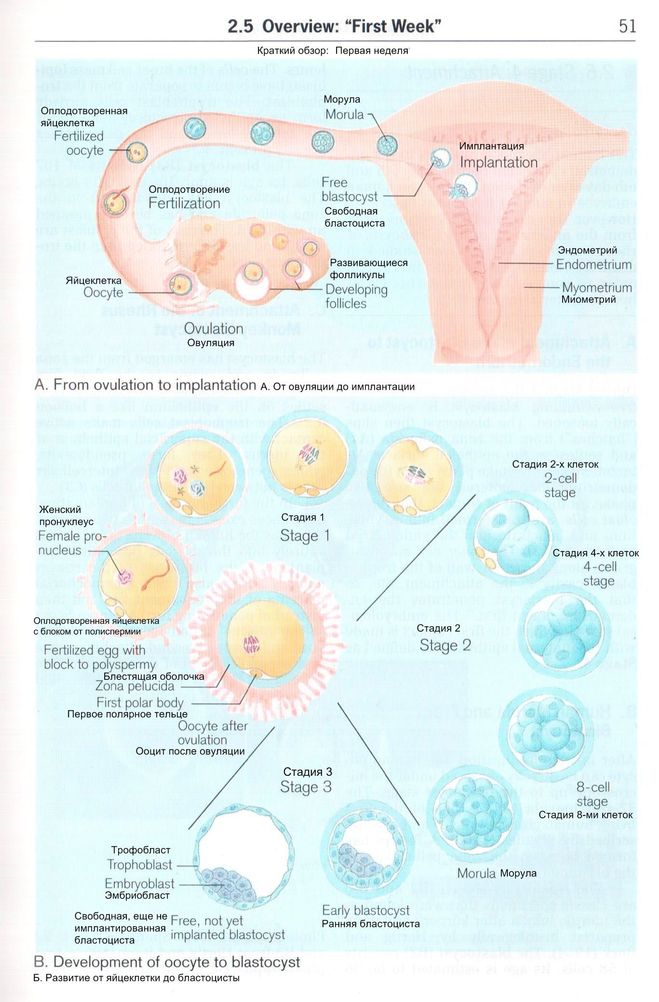
1-4 weeks of pregnancy
From a tiny fetus to a small person, a child's body develops in just 9 months. What changes are happening to the expectant mother and what changes are observed inside her during this difficult and joyful period of life?
Each new life begins with the union of the egg and sperm. Conception is the process by which a sperm enters an egg and fertilizes it.
It should be noted that the fetal and obstetric periods are different. The thing is that among specialists it is customary to consider the period from the first day of the last menstruation, that is, the obstetric period includes the period of preparation for pregnancy. So it turns out that the embryo has just appeared, and the gestation period is already two weeks. It is the obstetric period that is indicated in all the documents of a woman and is the only reporting period for specialists.
Until the moment of the meeting, the spermatozoon and the ovum lived for a certain time, being in the stage of development and maturation. The development of the future fetus significantly depends on the quality of these processes.
The development of the future fetus significantly depends on the quality of these processes.
First week
Growth and maturation of the egg starts from the first day of the cycle. A mature egg contains 23 chromosomes as the genetic material for the future embryo, and also contains all the nutrients necessary to start its development. It contains reserves of carbohydrates, proteins and fats, designed to support the embryo during the first days after its occurrence.
A certain number of eggs are laid in each ovary of a girl before she is born. During the childbearing period, they only grow and develop, the process of their formation does not occur. By the time a girl is born, the number of cells from which eggs can develop in the future reaches a million, but this number decreases significantly over the course of life. So, by the time of puberty, there are several hundred thousand of them, and by maturity - about 500.
The ovary each month gives the opportunity to develop, most often one egg, the maturation of which occurs inside a fluid-filled vesicle called a follicle. From the first day of the cycle, the uterine mucosa begins to prepare for a possible pregnancy. For implantation, i.e., the introduction of the resulting embryo into the wall of the uterus, an optimal environment is created. To do this, due to the influence of hormones, the endometrium thickens, it becomes covered with a network of vessels and accumulates the nutrients necessary for the future embryo.
From the first day of the cycle, the uterine mucosa begins to prepare for a possible pregnancy. For implantation, i.e., the introduction of the resulting embryo into the wall of the uterus, an optimal environment is created. To do this, due to the influence of hormones, the endometrium thickens, it becomes covered with a network of vessels and accumulates the nutrients necessary for the future embryo.
Male reproductive cells are formed in the gonads - in the testicles or testes. The maturation of spermatozoa occurs in the epididymis, into which they move after formation. The liquid structure of semen is formed due to the secretion of the seminal vesicles and the prostate gland. A liquid medium is necessary for storing mature spermatozoa and creating favorable conditions for their life.
The number of spermatozoa is quite large: tens of millions in one milliliter. Despite such a significant number, only one of them will be able to fertilize the egg. In spermatozoa, there is exclusively genetic material - 23 chromosomes, which are necessary for the appearance of the embryo.
Spermatozoa are characterized by high motility. Once in the female genital tract, they begin their movement towards the egg. Only half an hour or an hour passes from the moment of ejaculation, when sperm enter the uterine cavity. It takes one and a half to two hours for spermatozoa to penetrate into the widest part, which is called the ampulla. Most spermatozoa die on the way to the egg, meeting the folds of the endometrium, getting into the vaginal environment, cervical mucus.
Second week
In the middle of the cycle, the egg fully matures and leaves the ovary. It enters the abdominal cavity. This process is called ovulation. With a regular cycle of 30 days, ovulation occurs on the fifteenth. The egg is unable to move on its own. When she leaves the follicle, the fimbriae of the fallopian tube ensure her penetration inside. The fallopian tubes are characterized by longitudinal folding, they are filled with mucus. The muscular movements of the tubes have a wave-like character, which, with a significant number of cilia, creates optimal conditions for transporting the egg.
Through the tubes, the egg enters their widest part, which is called the ampulla. This is where fertilization takes place. If there is no meeting with the sperm, the egg dies, and the female body receives the appropriate signal to start a new cycle. There is a rejection of the mucous membrane, which was created by the uterus. The manifestation of such rejection is bloody discharge, which is called menstruation.
The waiting period for fertilization by the egg is short. On average, it takes no more than a day. Fertilization is likely on the day of ovulation and maximum on the next. Sperm have a longer lifespan, averaging three to five days, in some cases seven. Accordingly, if a spermatozoon enters the female genital tract before ovulation, there is a possibility that it will be able to wait for the appearance of an egg.
When the egg is in a state of waiting for fertilization, certain substances are released that are designed to detect it. If spermatozoa find an egg, they begin to secrete special enzymes that can loosen its shell. As soon as one of the spermatozoa penetrates the egg, the others can no longer do this due to the restoration of the density of its shell. Thus, one egg can only be fertilized by one sperm.
As soon as one of the spermatozoa penetrates the egg, the others can no longer do this due to the restoration of the density of its shell. Thus, one egg can only be fertilized by one sperm.
After fertilization, the chromosome sets of the parents merge - 23 chromosomes from each. As a result, one cell is formed from two different cells, which is called a zygote. The sex of the unborn child depends on which of the chromosomes, X or Y, was in the sperm. Eggs contain only X chromosomes. When XX is combined, girls are born. If the spermatozoon contains a Y chromosome, that is, with a combination of XY, boys are born. As soon as a zygote is formed in the body, a mechanism is launched in it aimed at maintaining pregnancy. There are changes in the hormonal background, biochemical reactions, immune mechanisms, and the receipt of nerve signals. The female body creates all the necessary conditions for the safe development of the fetus.
Third week
As soon as a day has passed after the formation of the embryo, he will need to make his first journey. The movements of the cilia and the contraction of the muscles of the tube direct it into the uterine cavity. During this process, inside the egg, fragmentation into identical cells occurs.
The movements of the cilia and the contraction of the muscles of the tube direct it into the uterine cavity. During this process, inside the egg, fragmentation into identical cells occurs.
After four days, the appearance of the egg changes: it loses its round shape and becomes vine-shaped. This stage is called morula, embryogenesis begins - an important stage in the development of the embryo, during which the formation of the rudiments of organs and tissues occurs. Cleavage of cells continues for several days, on the fifth day their complexes are formed, which have different functions. The central cluster forms directly the embryo, the outer one, called the trophoblast, is designed to melt the endometrium - the inner layer of the uterus.
It takes 5-7 days for the embryo to reach the uterus. When implantation occurs in its mucous membrane, the number of cells reaches one hundred. The term implantation refers to the process of implantation of the embryo into the endometrial layer.
After fertilization on the seventh or eighth day, implantation takes place. The first critical period of pregnancy is this stage, since the embryo will have to demonstrate its viability for the first time.
During implantation, the outer cells of the embryo actively divide, and the process itself takes about forty hours. The number of cells outside the embryo increases dramatically, they stretch, they penetrate into the uterine mucosa, and the thinnest blood vessels are formed inside, which are necessary for the supply of nutrients to the embryo. Time will pass, and these vessels will be transformed first into the chorion, and subsequently into the placenta, which will be able to supply the fetus with everything necessary until the baby is born.
The embryo at this stage of life is called a blastocyst. It contacts with the endometrium, melts the cells of the endometrium with its activity, creates a path for itself to the deeper layers. The blood vessels of the embryo intertwine with the mother's body, which allows it to immediately begin to extract useful and necessary substances for development. This is vital, because by this time the stock that the mature egg carried in itself is exhausted.
This is vital, because by this time the stock that the mature egg carried in itself is exhausted.
Next, the production of the trophoblast cells, i.e., the outer cells of human chorionic gonadotropin, the hCG hormone, begins. The distribution of this hormone throughout the body notifies it of the onset of pregnancy, which causes the launch of active hormonal changes and the beginning of corresponding changes in the body.
After fertilization and before the start of hCG, it usually takes eight or nine days. Therefore, already from the tenth day after fertilization, it becomes possible to determine this hormone in the mother's blood. Such an analysis is the most reliable confirmation of the onset of pregnancy. The tests that are offered today to determine pregnancy are based on the detection of this hormone in the urine of a woman. After the first day of delayed menstruation with its regular cycle, it is already possible to determine pregnancy using a test on your own.
What happens to a woman in the third week of pregnancy
If a woman is planning a pregnancy, 21-24 days, subject to a regular cycle, should be important for her. This is a period of possible implantation, when you should pay special attention to your own lifestyle. During this period, thermal effects and excessive physical exertion are undesirable, and the influence of various kinds of radiation should also be prevented.
This is a period of possible implantation, when you should pay special attention to your own lifestyle. During this period, thermal effects and excessive physical exertion are undesirable, and the influence of various kinds of radiation should also be prevented.
The woman does not feel anything at this stage, because implantation has no external signs. If you adjust your lifestyle in accordance with the simple rules listed above, you will be able to create optimal conditions for successful implantation.
Fourth week
In the fourth obstetric week or the second week of the fetus's life, its body consists of two layers. Endoblast - cells of the inner layer - will become the beginning of the digestive and respiratory systems, ectoblast - cells of the outer layer - will start the development of the nervous system and skin.
The size of the embryo at this stage is 1.5 mm. The flat arrangement of the cells determined the name of the embryo of this age - the disc.