Down syndrome lab test
Prenatal Testing for Down Syndrome | Patient Education
Down syndrome is a genetic condition caused by extra genes from the 21st chromosome. It results in certain characteristics, including some degree of cognitive disability and other developmental delays. Common physical traits include an upward slant of the eyes; flattened bridge of the nose; single, deep crease on the palm of the hand; and decreased muscle tone. A child with Down syndrome, however, may not have all these traits.
The incidence of Down syndrome in the United States is about 1 in 1,000 births. There is no association between Down syndrome and culture, ethnic group, socioeconomic status or geographic region.
Age-Related Risks
Generally, the chance of having a Down syndrome birth is related to the mother's age. Under age 25, the odds of having a child with Down syndrome are about 1 in 1,400. At age 35, the odds are about 1 in 350. At age 40, the odds are about 1 in 100.
Causes of Down Syndrome
There are three causes of Down syndrome:
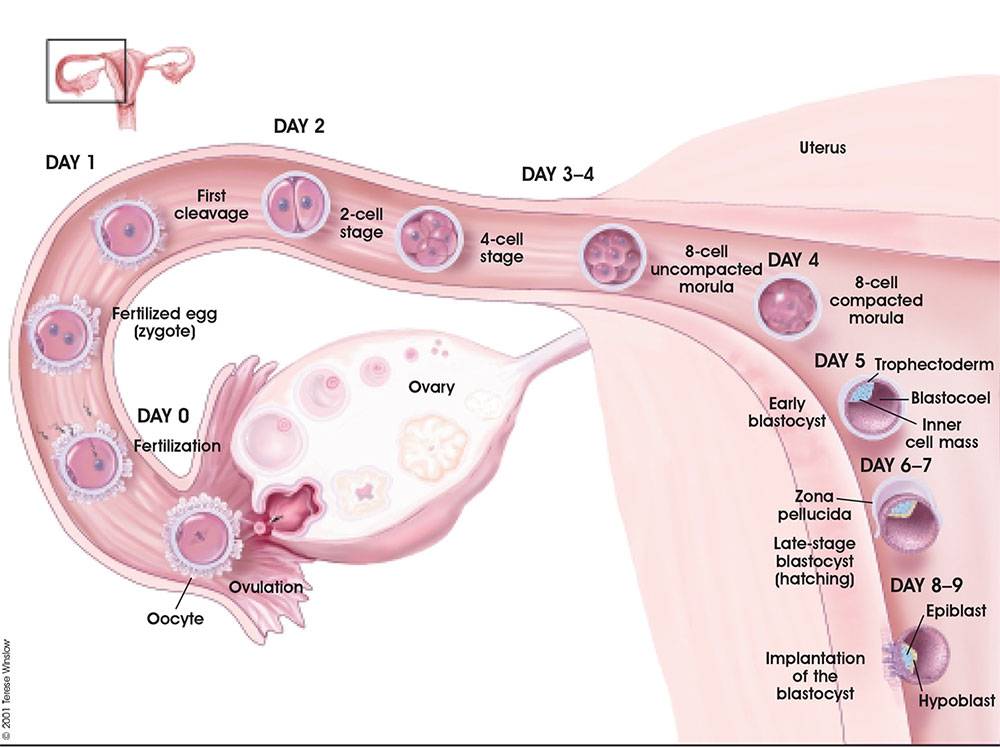
Trisomy 21
An estimated 95 percent of people with Down syndrome have trisomy 21, meaning they have three number 21 chromosomes instead of two. We normally have 23 pairs of chromosomes, each made up of genes. During the formation of the egg and the sperm, a woman's or a man's pair of chromosomes normally split so that only one chromosome is in each egg or sperm. In trisomy 21, the 21st chromosome pair does not split and a double dose goes to the egg or sperm. An estimated 95 to 97 percent of the extra chromosome is of maternal origin.
Translocation
Translocation occurs in about 3 to 4 percent of people with Down syndrome. In this type, an extra part of the 21st chromosome gets stuck onto another chromosome. In about half of these situations, one parent carries the extra 21st chromosome material in a "balanced" or hidden form.
Mosaicism
In mosaicism, the person with Down syndrome has an extra 21st chromosome in some of the cells but not all of them. The other cells have the usual pair of 21st chromosomes. About 1 to 2 percent of people with Down syndrome have this type.
Prenatal Testing
Screening tests can identify women at increased risk of having a baby with Down syndrome. These tests have no risks of miscarriage, but can't determine with certainty whether a fetus is affected. Diagnostic tests, on the other hand, are extremely accurate at identifying certain abnormalities in the fetus, but carry a small — generally less than 1 percent — risk of miscarriage. We offer options for both screening and diagnostic testing.
These tests have no risks of miscarriage, but can't determine with certainty whether a fetus is affected. Diagnostic tests, on the other hand, are extremely accurate at identifying certain abnormalities in the fetus, but carry a small — generally less than 1 percent — risk of miscarriage. We offer options for both screening and diagnostic testing.
Continue reading
Screening Tests
Sequential Integrated Screening — Sequential integrated screening is offered to all pregnant women by the state of California. This non-invasive screening is performed in two steps.
In the first step, which is performed between 10 and 14 weeks of pregnancy, a blood sample is taken from the mother and a nuchal translucency ultrasound is performed to measure the amount of fluid at the back of the baby's neck. If the blood test is scheduled prior to the ultrasound, we can provide the results at the end of the ultrasound appointment. The results of the blood test, the nuchal translucency measurement and the mother's age are used to estimate the risk for Down syndrome and trisomy 18.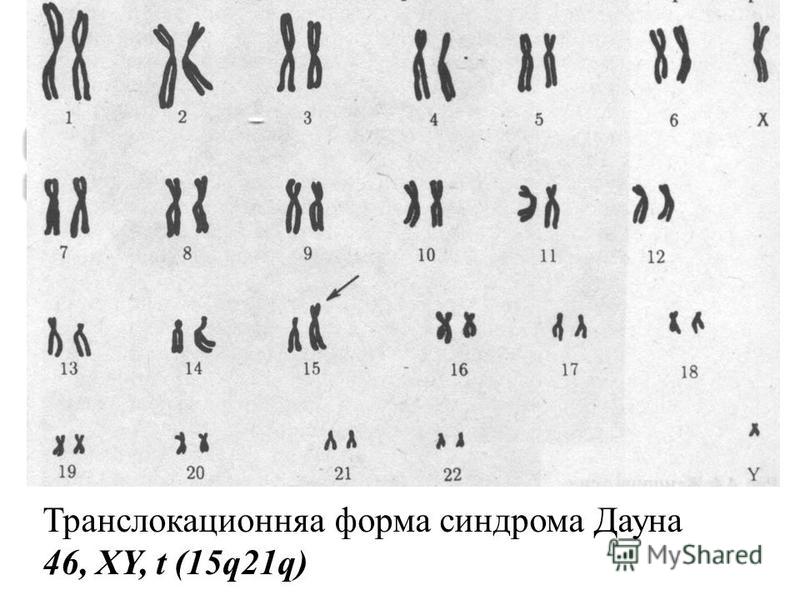
The second step is a maternal blood test between 15 to 20 weeks of pregnancy. When the results of this blood test are combined with the results from the first trimester blood test and nuchal translucency ultrasound, the detection rate for Down syndrome increases. This test also provides a personal risk assessment for having a fetus with trisomy 18, Smith-Lemli-Opitz syndrome, an open neural tube defect or an abdominal wall defect.
Diagnostic Tests
Amniocentesis, chorionic villus sampling (CVS) and ultrasound are the three primary procedures for diagnostic testing.
Amniocentesis — Amniocentesis is used most commonly to identify chromosomal problems such as Down syndrome. When the fetus is known to be at risk, it can detect other genetic diseases like cystic fibrosis, Tay-Sachs disease and sickle cell disease.
An amniocentesis procedure for genetic testing is typically performed between 15 and 20 weeks of pregnancy. Under ultrasound guidance, a needle is inserted through the abdomen to remove a small amount of amniotic fluid. The cells from the fluid are then cultured and a karyotype analysis — an analysis of the chromosomal make-up of the cells — is performed. It takes about two weeks to receive the results of the test.
The cells from the fluid are then cultured and a karyotype analysis — an analysis of the chromosomal make-up of the cells — is performed. It takes about two weeks to receive the results of the test.
Amniocentesis detects most chromosomal disorders, such as Down syndrome, with a high degree of accuracy. Testing for other genetic diseases, such as Tay-Sachs disease, is not routinely performed but can be detected through specialized testing if your fetus is known to be at risk. Testing for neural tube defects, such as spina bifida, also can be performed.
There is a small risk of miscarriage as a result of amniocentesis — about 1 in 100 or less. Miscarriage rates for procedures performed at UCSF Medical Center are less than 1 in 350.
Chorionic Villus Sampling (CVS) — Like amniocentesis, chorionic villus sampling is used most commonly to identify chromosomal problems such as Down syndrome. It can detect other genetic diseases like cystic fibrosis, Tay-Sachs disease and sickle cell disease in at-risk fetuses. The main advantage of CVS over amniocentesis is that it is done much earlier in pregnancy, at 10 to 12 weeks rather than 15 to 20 weeks.
The main advantage of CVS over amniocentesis is that it is done much earlier in pregnancy, at 10 to 12 weeks rather than 15 to 20 weeks.
CVS involves removing a tiny piece of tissue from the placenta. Under ultrasound guidance, the tissue is obtained either with a needle inserted through the abdomen or a catheter inserted through the cervix. The tissue is then cultured and a karyotype analysis of the chromosomal make-up of the cells is performed. It takes about two weeks to receive the results.
The advantage of CVS over amniocentesis is that the test is performed much earlier in pregnancy, so results are typically available by the end of the third month. A disadvantage is that spinal cord defects cannot be detected. Expanded alpha fetoprotein (AFP) blood testing or ultrasound can be performed later in the pregnancy to screen for spinal cord defects.
There is a small risk of miscarriage as a result of CVS — 1 in 100 or less. Miscarriage rates for procedures performed at UCSF Medical Center are less than 1 in 350.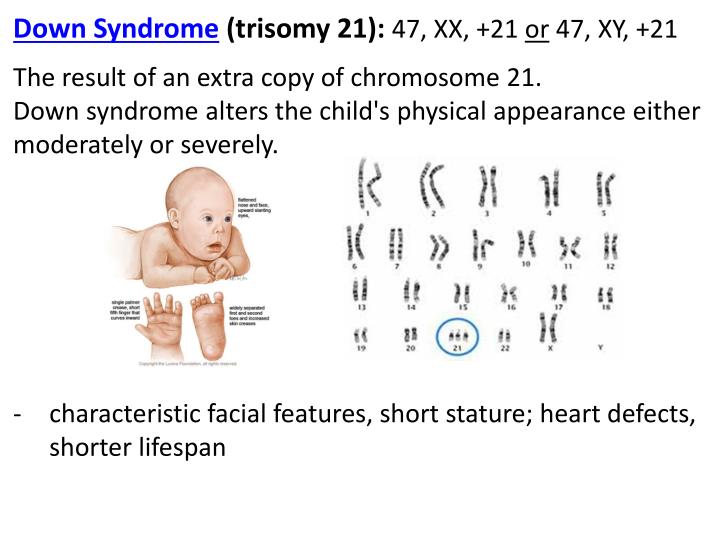
Ultrasound — The primary purpose of ultrasound is to determine the status of a pregnancy — the due date, size of the fetus and if the mother is carrying multiples. Ultrasound also can provide some information about possible birth defects in a fetus. All patients at UCSF Medical Center undergo a comprehensive ultrasound examination before any invasive tests are performed. Results of the ultrasound are explained at the time of the visit.
In some patients, an ultrasound raises concern of a possible abnormality in the fetus. We have extensive experience in performing and interpreting ultrasounds in pregnancy.
If You Receive a Positive Result
If you receive positive results on a screening test, we recommend that you discuss this with your doctor and a genetic counselor. Options for further diagnostic testing will be explained. The decision as to whether to have invasive genetic testing is up to you.
If a diagnostic test finds a genetic abnormality, the significance of such results should be discussed with experts familiar with the condition, including a medical geneticist and a genetic counselor, as well as your own doctor.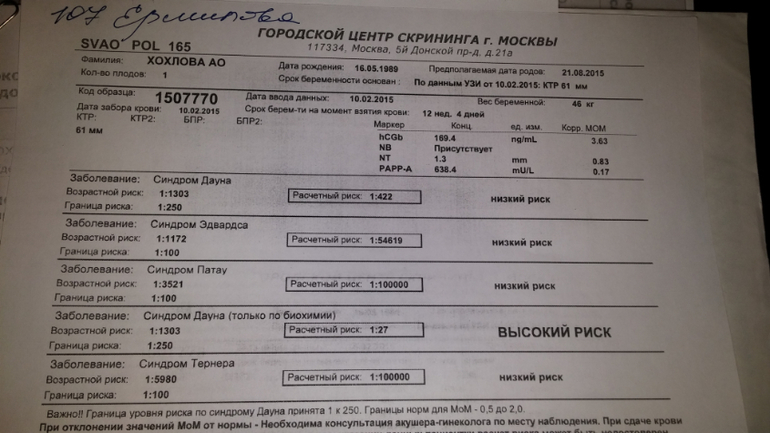
Down syndrome - Diagnosis and treatment
Diagnosis
The American College of Obstetricians and Gynecologists recommends offering the option of screening tests and diagnostic tests for Down syndrome to all pregnant women, regardless of age.
- Screening tests can indicate the likelihood or chances that a mother is carrying a baby with Down syndrome. But these tests can't tell for sure or diagnose whether the baby has Down syndrome.
- Diagnostic tests can identify or diagnose whether your baby has Down syndrome.
Your health care provider can discuss the types of tests, advantages and disadvantages, benefits and risks, and the meaning of your results. If appropriate, your provider may recommend that you talk to a genetics counselor.
Screening tests during pregnancy
Screening for Down syndrome is offered as a routine part of prenatal care. Although screening tests can only identify your risk of carrying a baby with Down syndrome, they can help you make decisions about more-specific diagnostic tests.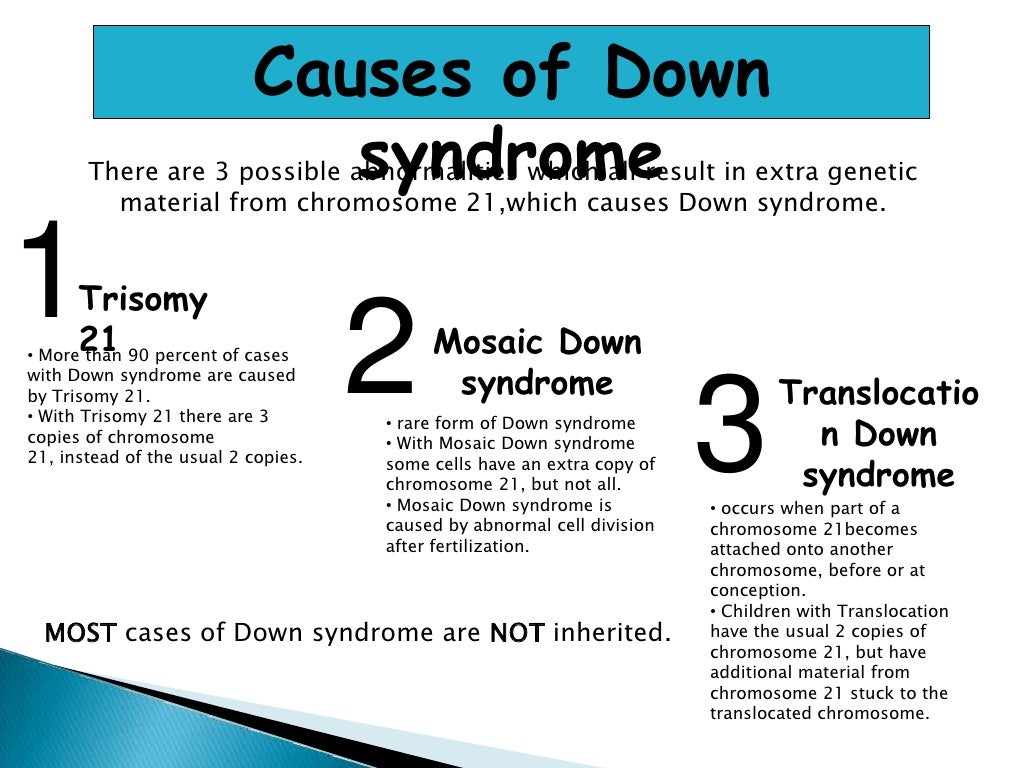
Screening tests include the first trimester combined test and the integrated screening test.
The first trimester combined test
The first trimester combined test, which is done in two steps, includes:
- Blood test. This blood test measures the levels of pregnancy-associated plasma protein-A (PAPP-A) and the pregnancy hormone known as human chorionic gonadotropin (HCG). Abnormal levels of PAPP-A and HCG may indicate a problem with the baby.
- Nuchal translucency test. During this test, an ultrasound is used to measure a specific area on the back of your baby's neck. This is known as a nuchal translucency screening test. When abnormalities are present, more fluid than usual tends to collect in this neck tissue.
Using your age and the results of the blood test and the ultrasound, your doctor or genetic counselor can estimate your risk of having a baby with Down syndrome.
Integrated screening test
The integrated screening test is done in two parts during the first and second trimesters of pregnancy.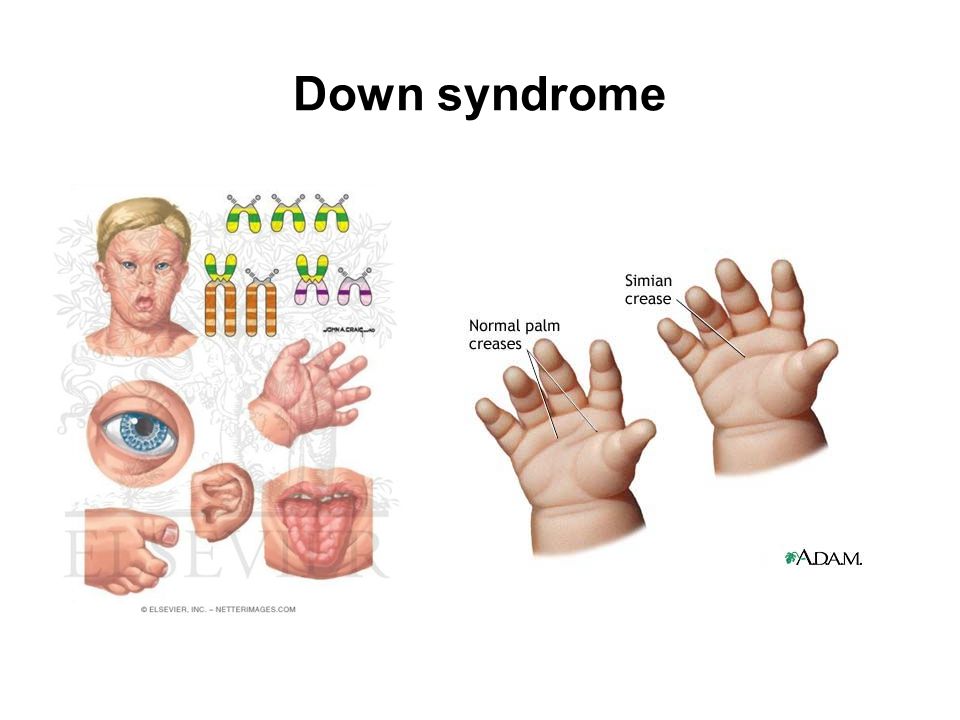 The results are combined to estimate the risk that your baby has Down syndrome.
The results are combined to estimate the risk that your baby has Down syndrome.
- First trimester. Part one includes a blood test to measure PAPP-A and an ultrasound to measure nuchal translucency.
- Second trimester. The quad screen measures your blood level of four pregnancy-associated substances: alpha fetoprotein, estriol, HCG and inhibin A.
Diagnostic tests during pregnancy
If your screening test results are positive or worrisome, or you're at high risk of having a baby with Down syndrome, you might consider more testing to confirm the diagnosis. Your health care provider can help you weigh the pros and cons of these tests.
Diagnostic tests that can identify Down syndrome include:
- Chorionic villus sampling (CVS). In CVS, cells are taken from the placenta and used to analyze the fetal chromosomes. This test is typically performed in the first trimester, between 10 and 13 weeks of pregnancy.
 The risk of pregnancy loss (miscarriage) from a CVS is very low.
The risk of pregnancy loss (miscarriage) from a CVS is very low. - Amniocentesis. A sample of the amniotic fluid surrounding the fetus is withdrawn through a needle inserted into the mother's uterus. This sample is then used to analyze the chromosomes of the fetus. Doctors usually perform this test in the second trimester, after 15 weeks of pregnancy. This test also carries a very low risk of miscarriage.
Preimplantation genetic diagnosis is an option for couples undergoing in vitro fertilization who are at increased risk of passing along certain genetic conditions. The embryo is tested for genetic abnormalities before it's implanted in the womb.
Diagnostic tests for newborns
After birth, the initial diagnosis of Down syndrome is often based on the baby's appearance. But the features associated with Down syndrome can be found in babies without Down syndrome, so your health care provider will likely order a test called a chromosomal karyotype to confirm diagnosis.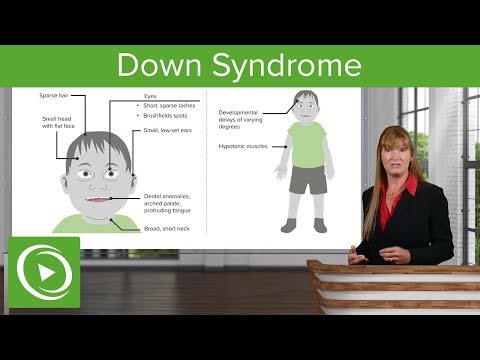 Using a sample of blood, this test analyzes your child's chromosomes. If there's an extra chromosome 21 in all or some cells, the diagnosis is Down syndrome.
Using a sample of blood, this test analyzes your child's chromosomes. If there's an extra chromosome 21 in all or some cells, the diagnosis is Down syndrome.
More Information
- Amniocentesis
- Chorionic villus sampling
- Cordocentesis
- Genetic testing
- Ultrasound
Treatment
Early intervention for infants and children with Down syndrome can make a major difference in improving their quality of life. Because each child with Down syndrome is unique, treatment will depend on individual needs. Also, different stages of life may require different services.
Team care
If your child has Down syndrome, you'll likely rely on a team of specialists that can provide medical care and help him or her develop skills as fully as possible. Depending on your child's particular needs, your team may include some of these experts:
- Primary care pediatrician to coordinate and provide routine childhood care
- Pediatric cardiologist
- Pediatric gastroenterologist
- Pediatric endocrinologist
- Developmental pediatrician
- Pediatric neurologist
- Pediatric ear, nose and throat (ENT) specialist
- Pediatric eye doctor (ophthalmologist)
- Audiologist
- Speech pathologist
- Physical therapist
- Occupational therapist
You'll need to make important decisions about your child's treatment and education. Build a team of health care providers, teachers and therapists you trust. These professionals can help evaluate the resources in your area and explain state and federal programs for children and adults with disabilities.
Build a team of health care providers, teachers and therapists you trust. These professionals can help evaluate the resources in your area and explain state and federal programs for children and adults with disabilities.
Request an Appointment at Mayo Clinic
Coping and support
When you learn your child has Down syndrome, you may experience a range of emotions, including anger, fear, worry and sorrow. You may not know what to expect, and you may worry about your ability to care for a child with a disability. The best antidote for fear and worry is information and support.
Consider these steps to prepare yourself and to care for your child:
- Ask your health care provider about early intervention programs in your area. Available in most states, these special programs offer infants and young children with Down syndrome stimulation at an early age (typically until age 3) to help develop motor, language, social and self-help skills.
- Learn about educational options for school.
 Depending on your child's needs, that may mean attending regular classes (mainstreaming), special education classes or both. With your health care team's recommendations, work with the school to understand and choose appropriate options.
Depending on your child's needs, that may mean attending regular classes (mainstreaming), special education classes or both. With your health care team's recommendations, work with the school to understand and choose appropriate options. - Seek out other families who are dealing with the same issues. Most communities have support groups for parents of children with Down syndrome. You can also find internet support groups. Family and friends can also be a source of understanding and support.
- Participate in social and leisure activities. Take time for family outings and look in your community for social activities such as park district programs, sports teams or ballet classes. Although some adaptations may be required, children and adults with Down syndrome can enjoy social and leisure activities.
- Encourage independence. Your child's abilities may be different from other children's abilities, but with your support and some practice your child may be able to perform tasks such as packing lunch, managing hygiene and dressing, and doing light cooking and laundry.

- Prepare for the transition to adulthood. Opportunities for living, working, and social and leisure activities can be explored before your child leaves school. Community living or group homes, and community employment, day programs or workshops after high school require some advance planning. Ask about opportunities and support in your area.
Expect a bright future. Most people with Down syndrome live with their families or independently, go to mainstream schools, read and write, participate in the community, and have jobs. People with Down syndrome can live fulfilling lives.
By Mayo Clinic Staff
Related
Associated Procedures
Products & Services
Get tested for Down syndrome in the 2nd trimester of pregnancy
Description
Study material Blood Serum
Home visit available
The study is performed for screening examination of pregnant women in order to assess the risk of fetal chromosomal abnormalities - trisomy 21 (Down syndrome), trisomy 18 (Edwards syndrome), as well as neural tube defect (NTD). Quantification of research results is carried out using PRISCA software.
Quantification of research results is carried out using PRISCA software.
Attention! For this study, the results of ultrasound are required!
Biochemical screening of the second trimester of pregnancy "triple test" of the second trimester consists of the following studies:
- Human chorionic gonadotropin (hCG, beta-hCG, b-hCG, Human Chorionic gonadotropin, HCG), test No. 66;
- Alpha-fetoprotein (AFP, a-Fetoprotein), test No. 92;
- Free estriol (unconjugated estriol, unconjugated estriol), test No. 134.
Determination of the concentration of these markers is used for screening examination of pregnant women in the second trimester of pregnancy in order to assess the risk of chromosomal abnormalities and fetal neural tube defects. The study is carried out between 15 and 20 weeks of pregnancy. The optimal timing for 2nd trimester screening is between 16 and 18 weeks of pregnancy.
Conducting a comprehensive examination at 11-14 weeks of gestation, including ultrasound and determination of maternal serum markers (hCG free beta subunit and PAPP-A), followed by a complex software calculation of the individual risk of giving birth to a child with a chromosomal pathology, is recommended for all pregnant women by order of the Ministry of Health of the Russian Federation dated November 01, 2012 No. 572n (“Procedure for the provision of medical care in the field of obstetrics and gynecology”). With normal 1st trimester screening results, a separate AFP determination can be used in the 2nd trimester to rule out a neural tube defect (see Test #92 AFP) or complete PRISCA profile 2nd trimester. A triple biochemical test with a complex software calculation of risks in the 2nd trimester may be especially appropriate for borderline risk assessment results during 1st trimester screening, and also if for some reason the 1st trimester screening was not carried out on time.
PRISCA (developed by Typolog Software, distributed by Siemens) is an EU-certified (CE-certified) and registered for use in the Russian Federation program that supports risk calculation for screening examinations of the 1st and 2nd trimesters of pregnancy. The risk calculation is carried out using a combination of biochemical markers informative for the corresponding period and ultrasound indicators. 1st trimester ultrasound data performed at 11-13 weeks of gestation can be used to calculate risks in the PRISCA program during 2nd trimester biochemical screening. At the same time, the PRISCA program will carry out an integrated calculation of risks, taking into account the value of NT (thickness of the nuchal space of the fetus) relative to the median values of this indicator for the gestational age on the date of its measurement in the 1st trimester.
Critical to correct calculations are the accuracy of the individual data provided, the qualifications of the ultrasound provider in performing prenatal screening ultrasound measurements, and the quality of the laboratory tests.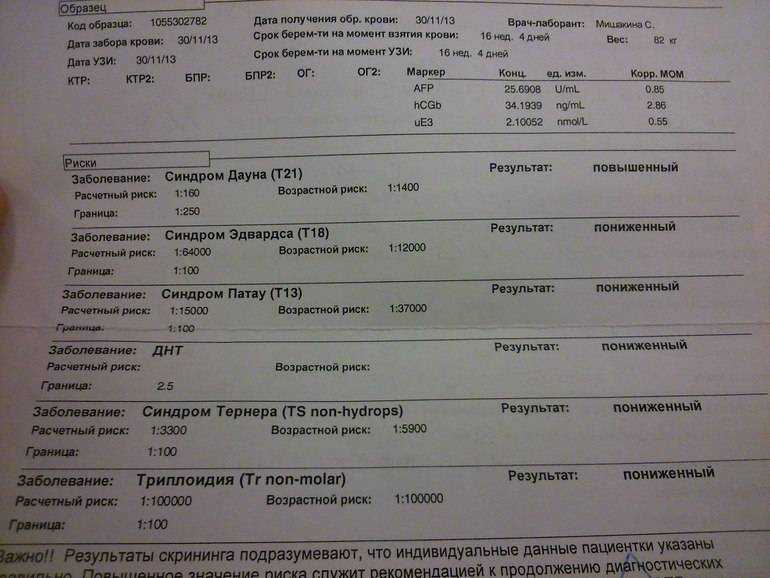
Preparation
Blood sampling is preferably carried out in the morning on an empty stomach, after 8-14 hours of overnight fasting (you can drink water), it is permissible in the afternoon 4 hours after a light meal.
On the eve of the study, it is necessary to exclude increased psycho-emotional and physical activity (sports training), alcohol intake, and smoking an hour before the study.
First trimester screening is optimal at 11-13 weeks, second trimester screening at 16-18 weeks. 1st trimester ultrasound data can be used to calculate risk in 2nd trimester biochemical screening.
General guidelines for exam preparation can be found here >>.
See instructions.
Indications for prescribing
Screening of pregnant women in the second trimester of pregnancy to assess the risk of chromosomal abnormalities and a defect in the neural tube of the fetus, especially appropriate for borderline results of the estimated risk of chromosomal abnormalities during screening of the 1st trimester, and also if there was no screening examination of the 1st trimester carried out on time.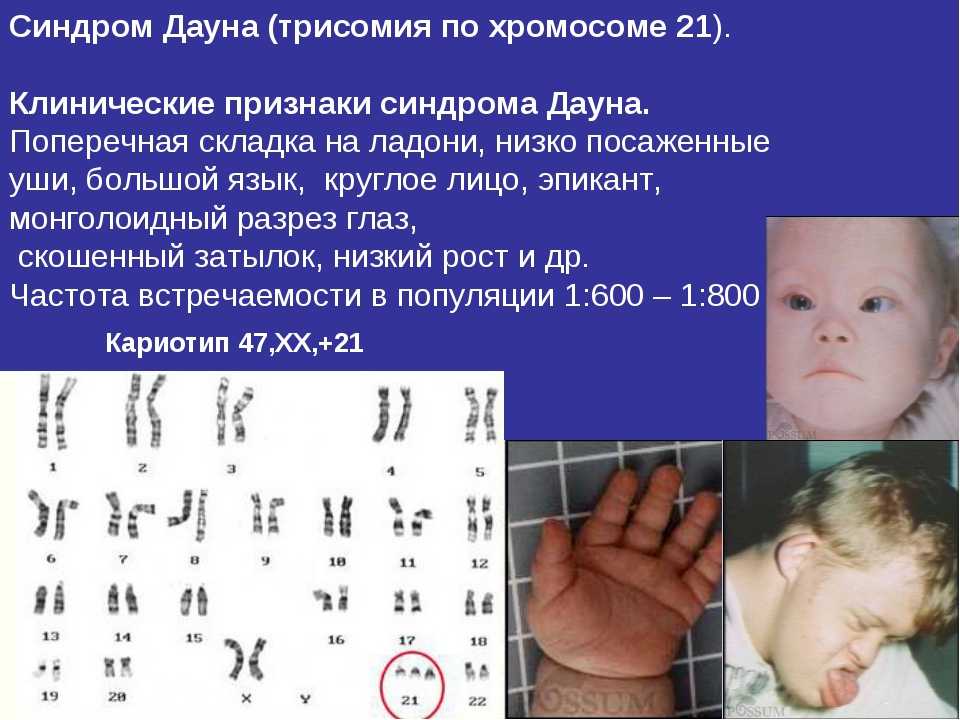
A referral form must be completed in order to complete the examination.
Interpretation of results
Interpretation of test results contains information for the attending physician and is not a diagnosis. The information in this section should not be used for self-diagnosis or self-treatment. An accurate diagnosis is made by the doctor, using both the results of this examination and the necessary information from other sources: history, results of other examinations, etc.
Triplets cannot be calculated (there are no corresponding statistical algorithms in the PRISCA program)
The results of the examination are issued in the form of a report form. It indicates the data used in the calculations, provides the results of the studies, adjusted values of MoM. In the conclusion, quantitative indicators of the risk degree for trisomy 21 (Down syndrome), trisomy 18 (Edwards syndrome) and neural tube defect (NTD) are indicated, which reflect the frequency of occurrence of the corresponding types of pathology with similar examination results and individual data. For example, a risk ratio of 1:6250 means that the statistical probability of having a child with the corresponding pathology is one in 6250 pregnancies with similar individual data. The PRISCA program sets conditional thresholds for identifying a high-risk group - a frequency above 1/250 for trisomy 21 (Down syndrome), above 1/100 - for trisomy 18, AFP MoM above 2.5 - for a neural tube defect.
For example, a risk ratio of 1:6250 means that the statistical probability of having a child with the corresponding pathology is one in 6250 pregnancies with similar individual data. The PRISCA program sets conditional thresholds for identifying a high-risk group - a frequency above 1/250 for trisomy 21 (Down syndrome), above 1/100 - for trisomy 18, AFP MoM above 2.5 - for a neural tube defect.
The results of calculating the risk of fetal chromosomal abnormalities based on screening biochemical studies and ultrasound indicators are only statistical probabilistic indicators that are not the basis for making a diagnosis, but may serve as an indication for the appointment of further special research methods. According to the current recommendations of the Ministry of Health of the Russian Federation, when a pregnant woman is found to have a high estimated risk of chromosomal abnormalities in the fetus (individual risk of 1/100 and higher), the obstetrician-gynecologist sends her to a medical genetic consultation (center) for medical genetic counseling and establishing or confirmation of the diagnosis using invasive examination methods to establish the fetal karyotype.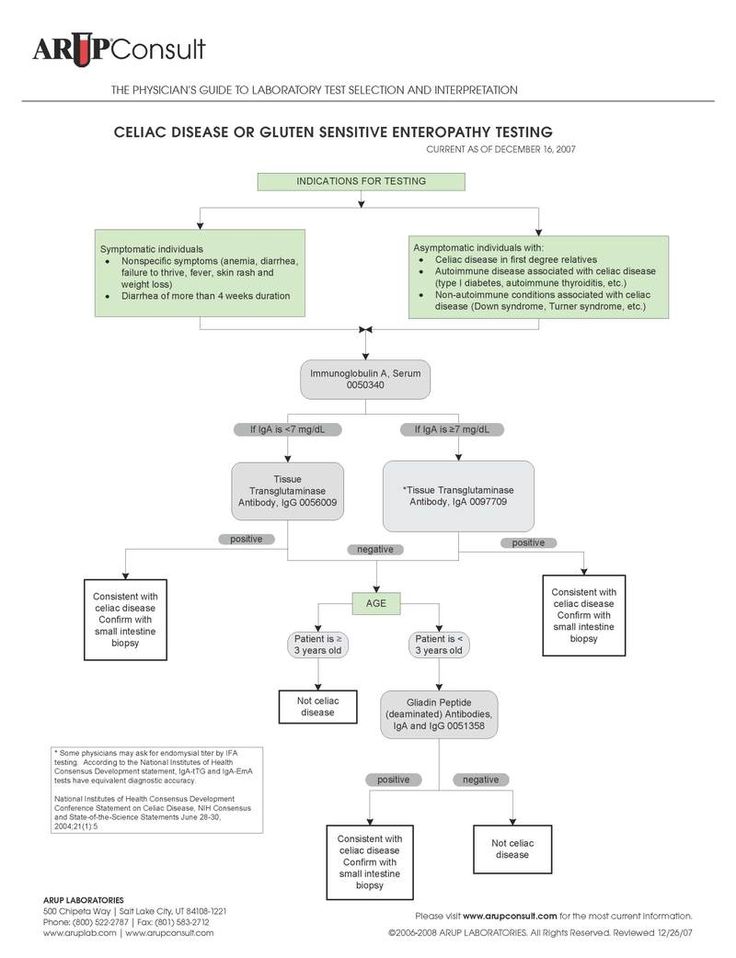
The use of complex (ultrasound + biochemical) screening, according to a number of studies, makes it possible to detect Down's syndrome in the fetus of pregnancy in 85 - 90% of cases with 5% of false positive results. Comprehensive screening helps to identify not only the risk of a fetal chromosomal abnormality, but also the overall risk of pregnancy pathology.
ᐈ Analysis for the presence of Down syndrome (trisomy 21 chromosomes), sex determination in Kyiv, prices
A non-invasive study that allows you to reliably determine the presence of Down syndrome in the fetus and determine its gender. The clinical test is completely safe for both the fetus and the expectant mother. Down syndrome is the most well-known chromosomal disorder - it is diagnosed in one in 700-900 babies born worldwide. A medical diagnosis is made on the basis of a laboratory test and a doctor.
Each human cell contains 46 chromosomes, whose DNA determines appearance and development. Down syndrome results when there is an extra partial or complete copy of chromosome 21 (trisomy 21).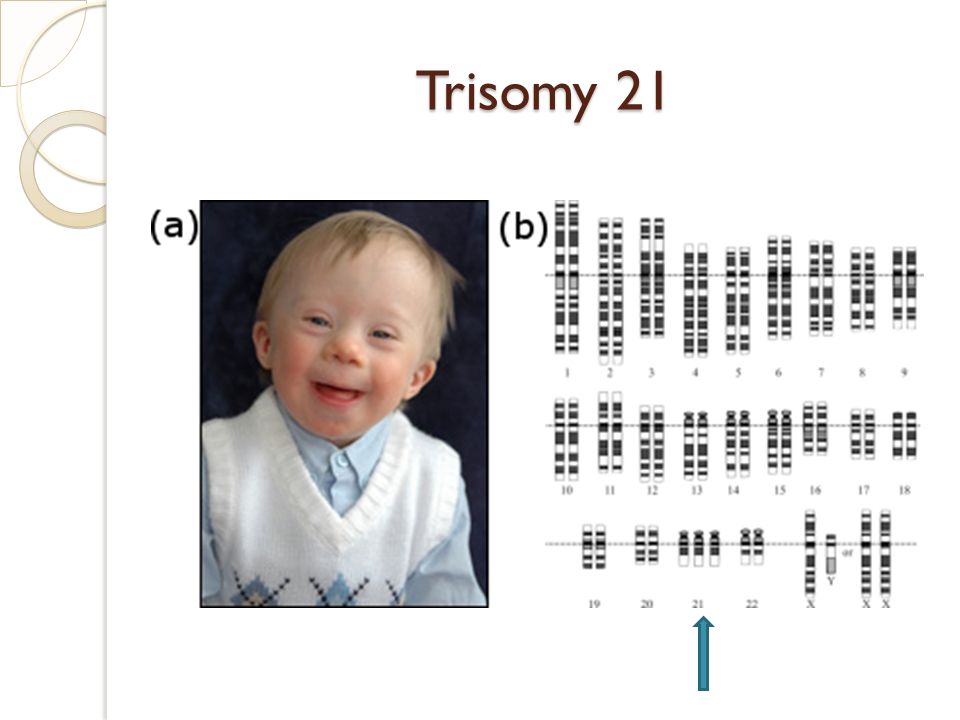 There may be several reasons for this, the most common of which is an error in cell distribution, which results in an embryo with three copies of chromosome 21 instead of the usual two, which is why a laboratory test for this syndrome is so important.
There may be several reasons for this, the most common of which is an error in cell distribution, which results in an embryo with three copies of chromosome 21 instead of the usual two, which is why a laboratory test for this syndrome is so important.
As the embryo develops, an extra chromosome is replicated in every cell of the body. This type of development of Down syndrome is 95% of cases. About 4% of cases of this disease are due to translocation - while the total number of chromosomes in cells is 46, but an additional complete or partial copy of chromosome 21 is attached to another chromosome. Sometimes an additional examination is required to make a diagnosis. In addition, in very rare cases, there may be mosaic Down syndrome. It is diagnosed if there are two types of cells in the body: some contain the usual chromosomes 46, and some 47 (in them they find an additional chromosome 21). An additional partial or complete copy of the 21st chromosome, the embryo most often receives from the mother.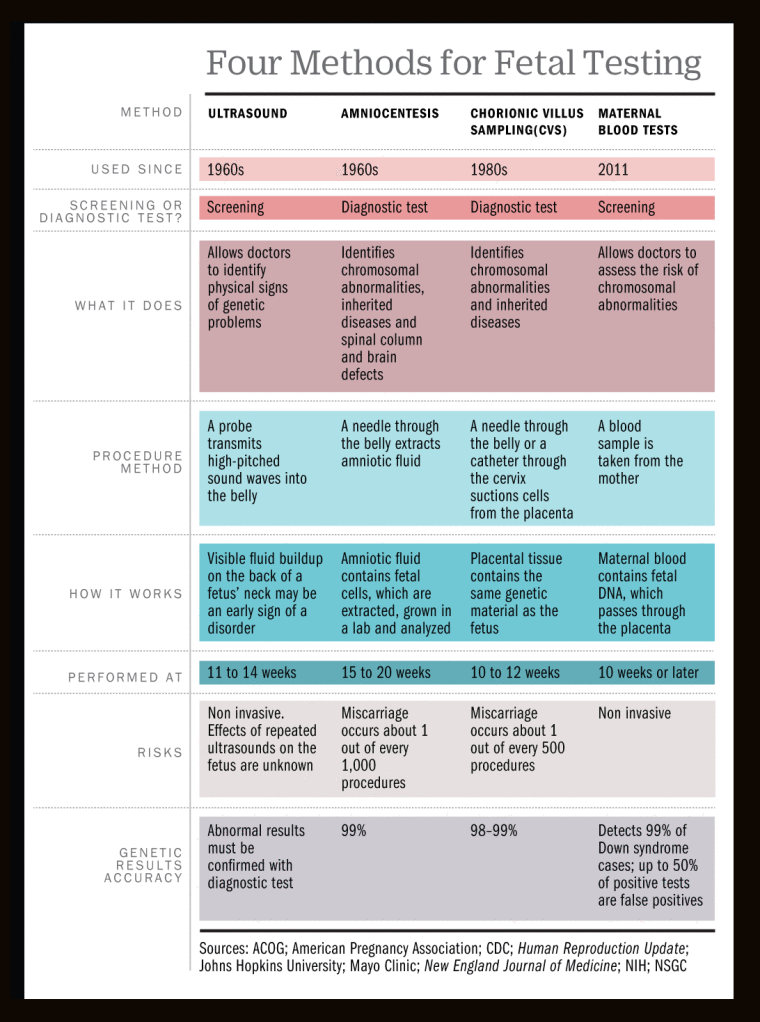 If a woman gave birth to a child with trisomy 21, then it is believed that the probability of her having a second child with the same pathology is 1 to 100. By carefully studying the biological material of the study, it is possible to determine the exact indicators of the analysis. The non-invasive prenatal test for trisomy 21 in a fetus is a new and improved prenatal test capable of detecting the chromosomal material of a fetus circulating in the maternal blood. Also, this test determines the sex of the child with an accuracy of> 99.9%. Gender is optional. The possibility of passing the test with a quality guarantee is provided by the ADONIS clinic, where you can take the material in any convenient laboratory.
If a woman gave birth to a child with trisomy 21, then it is believed that the probability of her having a second child with the same pathology is 1 to 100. By carefully studying the biological material of the study, it is possible to determine the exact indicators of the analysis. The non-invasive prenatal test for trisomy 21 in a fetus is a new and improved prenatal test capable of detecting the chromosomal material of a fetus circulating in the maternal blood. Also, this test determines the sex of the child with an accuracy of> 99.9%. Gender is optional. The possibility of passing the test with a quality guarantee is provided by the ADONIS clinic, where you can take the material in any convenient laboratory.
Non-invasive prenatal test for the presence of Down's syndrome, sex determination, is prescribed for the diagnosis of women over 35 years of age with chromosomal abnormalities in relatives, with a history of reproductive losses, with 2 or more IVF failures, with changes in biochemical markers by screening.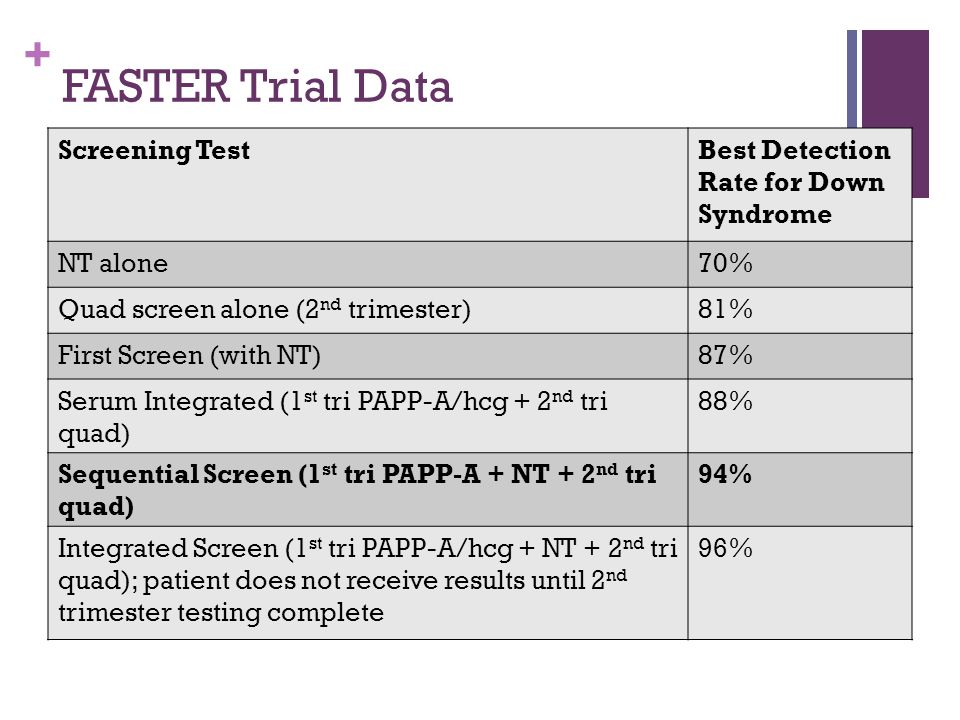 The exact diagnosis is determined by the doctor.
The exact diagnosis is determined by the doctor.
The conclusion of the study can be presented in two versions:
"Low risk" - the child is unlikely to have Down syndrome.
"High risk" - evidence of trisomy 21 was found. This test result may indicate that the fetus has Down syndrome.
The price of the study is indicated on the website.
DNA sex determination reveals the Y chromosome. When a Y chromosome is found, you will be given the conclusion that your unborn child will be a boy. If the Y-chromosome marker is not found, then you will get the conclusion that you will have a girl. You can take a test in Kyiv at any ADONIS department.
Biomaterial type
Venous blood
Patient preparation rules
30 minutes - no smoking. Medicines, alcohol, coffee, excessive physical activity can affect the results of laboratory tests and their diagnostic value.