Chance of getting pregnant before ovulation
Right Time For Sex , When Do You Ovulate ?
When are you more likely to conceive?
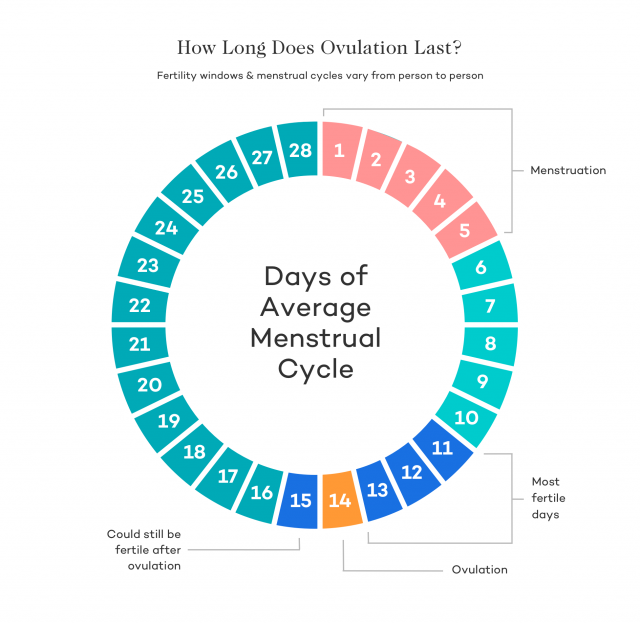
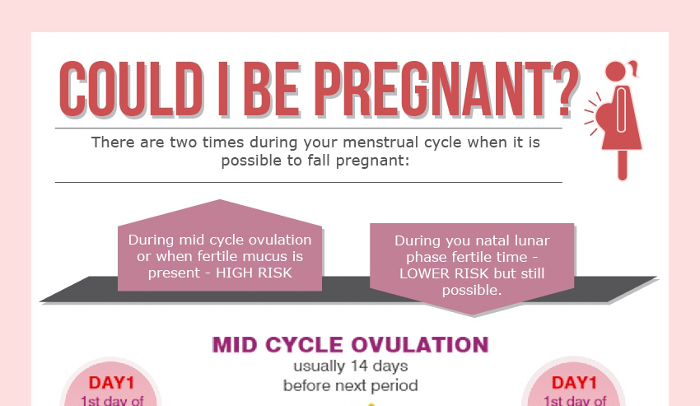
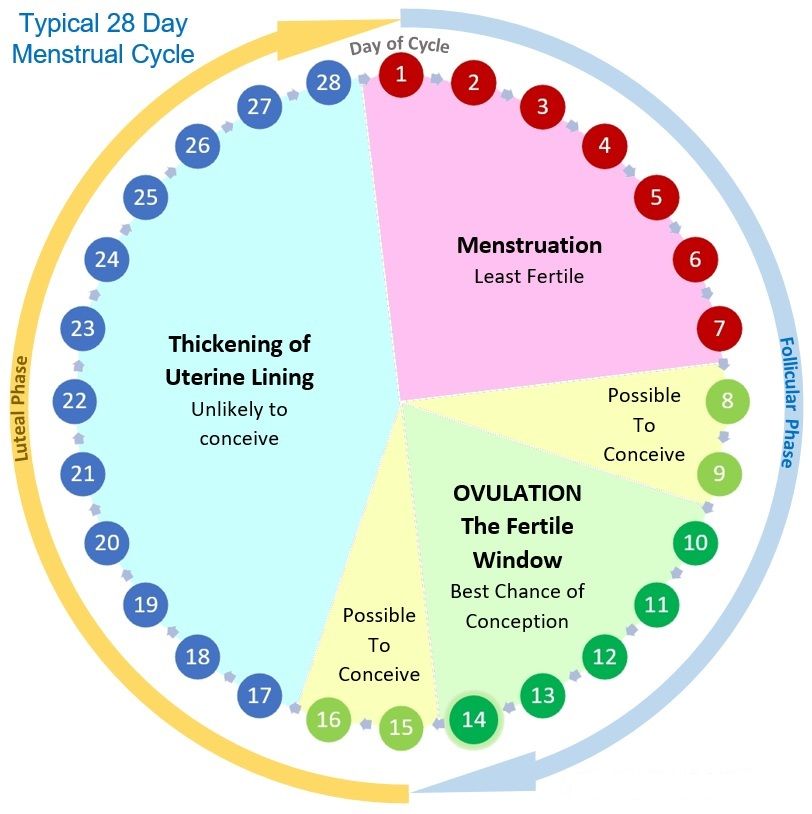
We’re talking about the 'fertile window’ – the days in a woman’s menstrual cycle when pregnancy is possible. The ‘fertile window’ depends on the length of the menstrual cycle, which varies among women.
The ‘fertile window’ is the day an egg is released from the ovary (ovulation) and the five days beforehand. Having sex (intercourse) during this time gives you the best chance of getting pregnant.
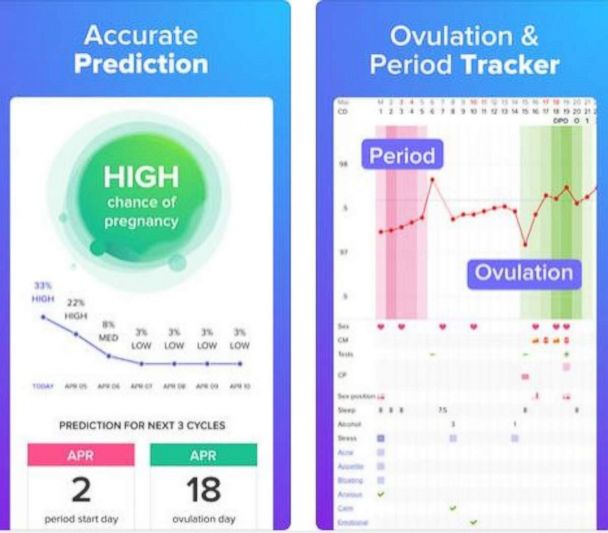
Ovulation Calculator
What day did you your most recent period start?
Number of days in your cycle Please select20 Days21 Days22 Days23 Days24 Days25 Days26 Days27 Days28 Days29 Days30 Days31 Days32 Days33 Days34 Days35 Days36 Days37 Days38 Days39 Days40 Days41 Days42 Days43 Days44 Days45 Days
Your ovulation day
Most fertile time
-
What is an ovulation calculator and how does it help you get pregnant?
This ovulation calculator or ovulation calendar can help you work out your most fertile time.
These are the days you are most likely to get pregnant.
It can also estimate your due date if you do become pregnant during your next fertile days.
Others ways to help you work out when you're ovulating:
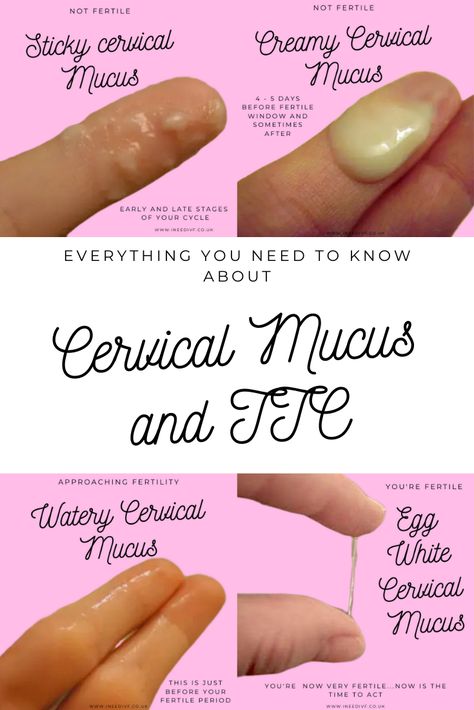
- Notice changes in vaginal mucus
A few days before ovulation, you may notice your vaginal mucus becomes clear, slick and slippery, and feels a bit like egg white.
This is a sign that ovulation is about to happen. It’s the best time to have sex, as sperm travel more easily in this kind of mucus.
- Use an ovulation predictor kit
You can use a predictor kit from a supermarket or pharmacy, to test your urine for signs of ovulation. If you start testing your urine a few days before the day you next expect to ovulate, a positive result means you are going to ovulate within the next 24 to 36 hours (one to two days).
-
Facts about timing
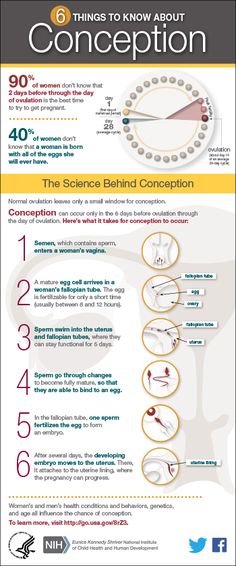
Ovulation is when a mature egg is released from the ovary. The egg then moves down the fallopian tube where it can be fertilised. If sperm are in the fallopian tube when the egg is released, there is a good chance that the egg will be fertilised, creating an embryo, which can grow into a baby.
Pregnancy is technically only possible if you have sex during the five days before ovulation or on the day of ovulation. But the most fertile days are the three days leading up to and including ovulation. Having sex during this time gives you the best chance of getting pregnant.
By 12-24 hours after ovulation, a woman is no longer able to get pregnant during that menstrual cycle because the egg is no longer in the fallopian tube.
There’s almost no chance of getting pregnant if you have sex before or after the fertile window (but if you’re not trying to get pregnant, don’t rely on this – contraception is your best option!).
-
How to know when you’re ovulating
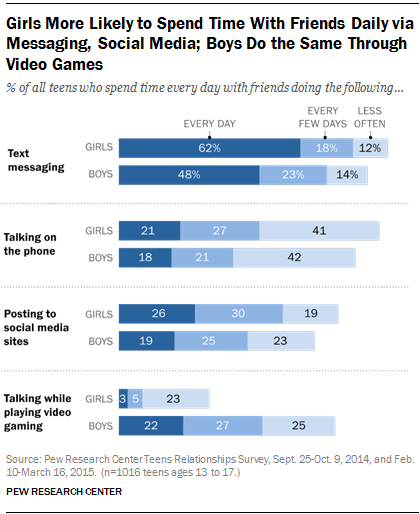
Knowing when you ovulate can help you plan for sex at the right time and improve your chance of getting pregnant. You can keep track of your menstrual cycles on a chart, in a diary, or on a free period-tracker app on your smartphone.
To work out the length of your menstrual cycle, record the first day you start bleeding (first day of your period). This is day 1. The last day of your cycle is the day before your next period begins.
- What is a ‘menstrual cycle’ and a ‘period’?
Some people think the ‘menstrual cycle’ and a ‘period’ are the same thing.
A period is when you bleed (or menstruate).
A menstrual cycle starts on the day when a period starts (day 1) and ends the day before the next period. A cycle’s length is considered normal if it’s between 21 and 35 days. They can vary between women and from one cycle to the next.
- Working out your ‘average’ menstrual cycle length
If your menstrual cycles are different lengths (most women’s cycles are) you can work out your average cycle length.
The number of days in a woman’s menstrual cycle can vary month to month. Periods are not always regular. It can be useful to work out an ‘average’ cycle length, based on the length of three menstrual cycles, to estimate when you’re most likely to be ovulating.
If you add the number of days in three cycles and divide the total number by three, it gives you your average cycle length.
Example
Sarah tracked her last three menstrual cycles by counting the time from the first day of one period, to the day before the next period.

Cycle 1 was 28 days; Cycle 2 was 32 days; Cycle 3 was 27 days
28 + 32 + 27 = 87
87 divided by 3 = 29
So the average length of Sarah’s menstrual cycles is 29 days.
- Working out your most fertile days
When you know your average menstrual cycle length, you can work out when you ovulate.
Ovulation happens about 14 days before your period starts.
- If your average menstrual cycle is 28 days, you ovulate around day 14, and your most fertile days are days 12, 13 and 14.
- If your average menstrual cycle is 35 days ovulation happens around day 21 and your most fertile days are days 19,20 and 21.
- If you have shorter cycles, say 21 days, ovulation happens around day 7 and your most fertile days are days 5, 6 and 7.
Your most fertile days are the three days leading up to and including the day of ovulation.

Some women have very irregular cycles or find it difficult to work out an average cycle length. This can make it hard to work out when ovulation happens. If it’s all too hard, having sex every 2-3 days covers all bases and improves your chance of getting pregnant.
Myth busting
- MYTH
A woman can get pregnant any time of the month.
- FACT
A woman can only get pregnant on a few days during her menstrual cycle.
Why?
Because eggs and sperm only live for a short time:
- Sperm live for around five days.
- Eggs can only be fertilised for around 24 hours (one day) after being released from the ovary.
Eggs and sperm need to come together at the right time for fertilisation to happen to create an embryo.
Getting the timing right
If you're trying to get pregnant, timing is everything. Dr Karin Hammarberg explains how to work out when you are ovulating and the right time to have sex to improve your chance of pregnancy.
-
What are the chances?
Having sex as close as possible to the time of ovulation increases the chance of pregnancy.
If a woman has sex six or more days before she ovulates, the chance she will get pregnant is virtually zero.
If she has sex five days before she ovulates, her probability of pregnancy is about 10 percent.
If she has sex on the day of ovulation, or the two days before, the chance of getting pregnant is around 30 percent.
These are average figures and depend on a woman’s age.
When does preconception health begin?
Professor Sarah Robertson, Director of Robinson Research Institute, University of Adelaide, highlights the key time before pregnancy that your health is most important to ensure your child has the best start to life.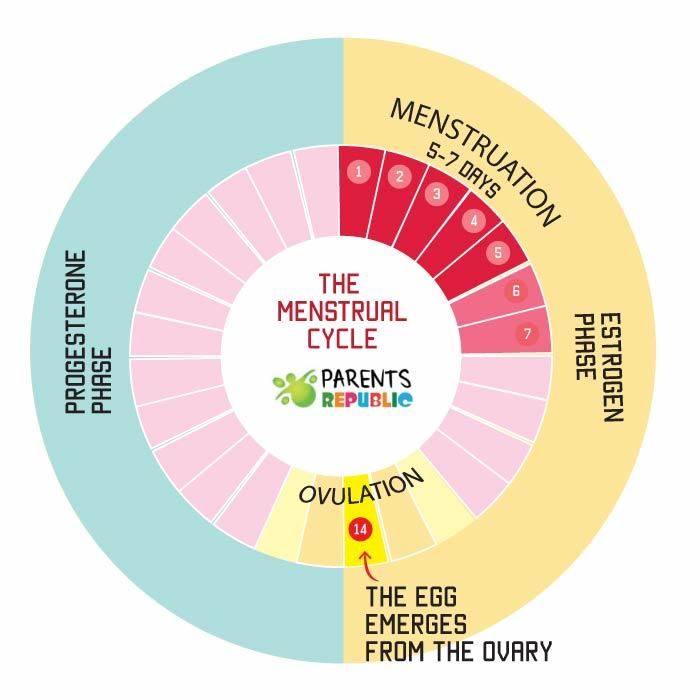
How to know you are ovulating
Kerry Hampton, a registered nurse and fertility specialist, discusses the importance of fertility awareness, and how to determine your fertile window to improve your chances of conceiving.
- References
- American Society for Reproductive Medicine, Optimizing natural fertility, https://www.reproductivefacts.org/news-and-publications/patient-fact-sheets-and-booklets/documents/fact-sheets-and-info-booklets/optimizing-natural-fertility/
- Berglund Scherwitzl, et al. (2015). Identification and prediction of the fertile window using Natural Cycles. The European Journal of Contraception and Reproductive Health Care, 20(5), 403-408. doi:10.3109/13625187.2014.988210
- Ecochard, R., et al. (2015). Self-identification of the clinical fertile window and the ovulation period.
 Fertility and Sterility, 103(5), 1319-1325.e1313. doi: http://dx.doi.org/10.1016/j.fertnstert.2015.01.031
Fertility and Sterility, 103(5), 1319-1325.e1313. doi: http://dx.doi.org/10.1016/j.fertnstert.2015.01.031 - Pfeifer, S., et al. (2017). Optimizing natural fertility: a committee opinion. Fertility and Sterility, 107(1), 52-58. doi: 10.1016/j.fertnstert.2016.09.029
- Stanford, J. B. (2015). Revisiting the fertile window. Fertility and Sterility, 103(5), 1152-1153. doi: http://dx.doi.org/10.1016/j.fertnstert.2015.02.015
- Stanford, et al. (2002). Timing intercourse to achieve pregnancy: current evidence. Obstetrics and Gynecology, 100(6), 1333-1341.
- Stephenson, J., et al. (2018). Before the beginning: nutrition and lifestyle in the preconception period and its importance for future health. The Lancet, 10.1016/S0140-6736(18)30311-8 doi: 10.1016/S0140-6736(18)30311-8
- Vélez, M. Pet al. (2015). Female exposure to phenols and phthalates and time to pregnancy: the Maternal-Infant Research on Environmental Chemicals (MIREC) Study. Fertility and Sterility.
 doi: 10.1016/j.fertnstert.2015.01.005
doi: 10.1016/j.fertnstert.2015.01.005 - Verón, G. L., et al. (2018). Impact of age, clinical conditions, and lifestyle on routine semen parameters and sperm kinematics. Fertility and Sterility, 110(1), 68-75.e64. https://doi.org/10.1016/j.fertnstert.2018.03.016
- Waylen, A. Let al. (2009). Effects of cigarette smoking upon clinical outcomes of assisted reproduction: a meta-analysis. Hum Reprod Update, 15(1), 31-44.
- Zenzes, M. T. (2000). Smoking and reproduction: gene damage to human gametes and embryos. Hum Reprod Update, 6(2), 122-131.
Page created on: 28/08/2018 | Last updated: 09/12/2022
Chances of getting pregnant after ovulation
This article was last updated on Friday, February 28, 2021.
Depending on what state, county, or school district you grew up in, what you were taught about reproduction and conception varies greatly. Though 39 states and DC require some sort of sex education, only 44% of states mandating sex ed require that content be medically accurate.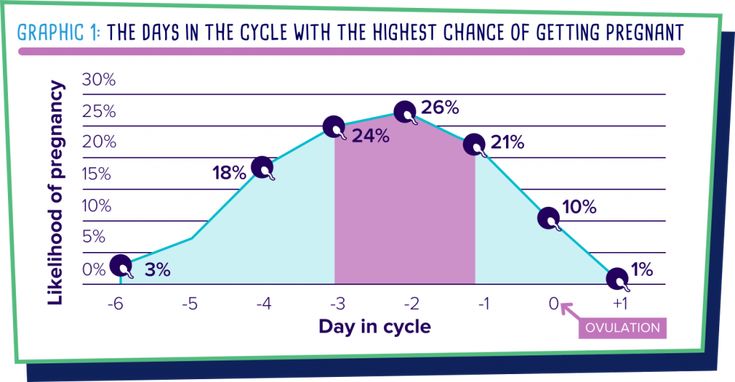 (It's a real head-scratcher.) While some teens learn that abstinence is the only way to avoid conceiving, it turns out that abstinence-only education actually harms teens by leading to increased rates of teen pregnancy and sexually transmitted infections.
(It's a real head-scratcher.) While some teens learn that abstinence is the only way to avoid conceiving, it turns out that abstinence-only education actually harms teens by leading to increased rates of teen pregnancy and sexually transmitted infections.
In this post, we'll go way beyond your high school sex ed to give you the (medically accurate) summary on your chances of getting pregnant, and how those chances are affected by things like your cycle, age, previous and current birth control use, conditions like polycystic ovary syndrome (PCOS), and more.
Whether you're actively trying to conceive (TTC) or actively avoiding conception, we want you to have the info required to help you achieve your reproductive goals — whatever they may be.
The conception and ovulation data, in a nutshell
- There's a 42% (max) chance of conception on the day before ovulation, the most fertile day of your cycle. (Source)
- Most medical experts cite that around 85% of couples achieve a pregnancy after 12 months of trying.
 But this estimate varies significantly across studies.
But this estimate varies significantly across studies. - Compared to women who've never used birth control, there is a 0% difference in pregnancy rates after 12 months for ex-pill and ex-IUD users. (Source)
- The failure rate (how many women get pregnant over the course of a year) for long-acting reversible contraceptives like IUDs is 1%.
- 10% of women have PCOS, a condition that is associated with irregular and infrequent ovulation, making natural conception trickier.
Back to basics: What is conception, anyway?
Conception is a little more nuanced than the love story of egg meets sperm, sperm meets egg, and — voila! — conception. Of course, it's true that the meeting of eggs and sperm is a necessary prerequisite to a pregnancy, but let's get into why it's a bit more complicated than that:
- While we're born with all the eggs we'll ever have (over one million!) and have approximately 400,000 eggs left by the time we hit puberty, almost all of these eggs are suspended in an undeveloped state — it's only in the few months before an egg is ovulated that it grows and develops into an egg that can be fertilized.
- Around ovulation, typically one egg is released from the follicle it grew and developed in. It takes an egg about 30 hours to travel from ovary to the end of the tube. The egg rests there, and then it waits another 30 hours. After 24 hours, if fertilization doesn't occur, RIP to that egg.
- If any sperm were waiting around in the reproductive tract before ovulation occurred (they can survive in the female reproductive tract for up to ~5 days after all), or if sperm make their way into the reproductive tract and all the way to the egg when it's released, fertilization can occur.
Most medical professionals agree that a fertilized egg does not equal successful conception. It takes about six days for a fertilized egg to travel down into the uterus where it then digs its heels into the uterine lining (on average, fertilized eggs implant 6-10 days after conception in the fallopian tube).
It's only at that point that it can start further developing and receiving the nutrients it needs to result in a pregnancy. Only about 40% of fertilized eggs will make it past this implanting-in-the-uterine-lining hurdle (caveat: this data is hard to come by, so estimates of this statistic may vary widely), and it's after that point that most medical professionals would consider it a pregnancy.
Only about 40% of fertilized eggs will make it past this implanting-in-the-uterine-lining hurdle (caveat: this data is hard to come by, so estimates of this statistic may vary widely), and it's after that point that most medical professionals would consider it a pregnancy.
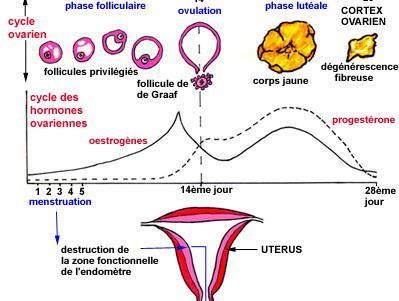
How your hormones change before, during, and after ovulation
Here we’ll explain how estradiol, luteinizing hormone (LH), and progesterone levels all fluctuate — and what tracking each of these hormones can tell you about ovulation.
Talia ShiraziModern Fertility Blog
What are the chances of getting pregnant during your cycle? Can you get pregnant after ovulation or while you're on your period?
If you get your period regularly and don't have any conditions (like PCOS) that influence ovulation, you'll ovulate around the middle of your cycle (days 10-14) in about 92% to 96% of cycles; in the remaining 4%-6% of cycles, ovulation never occurs (this is perfectly normal).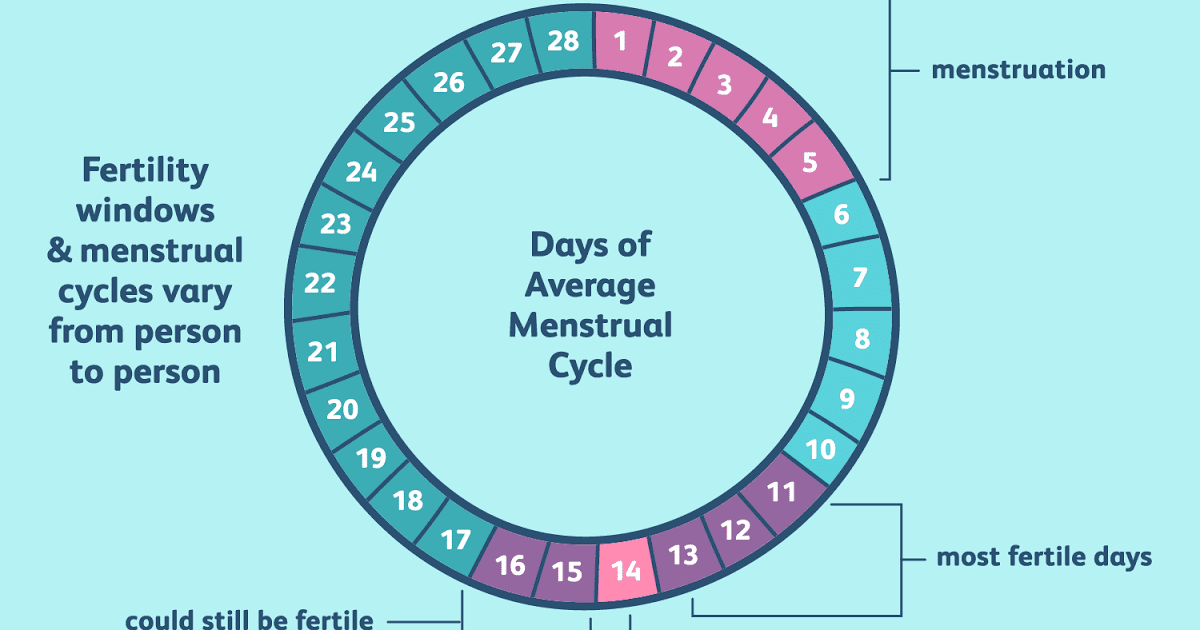
In a cycle where ovulation occurs, recent estimates suggest the chances of conception are between 3% seven days before ovulation and 42% the day before ovulation. Estimates from other studies suggest peak chances of conception are a bit lower — closer to 38% according to some, or 20% according to others. Differences in study methodology and the demographics of the women who are in their sample (e.g., age, if women with any reproductive conditions were screened out) may in part explain the variation in estimates among studies.
Because sperm can live up to five days in the female reproductive tract, it *is* completely possible to get pregnant if you have sex on the days leading up to ovulation and not on the day of ovulation itself, if those five days overlaps at all with the 24 hours that an egg can be fertilized. Having sex on the days leading up to ovulation, even though ovulation has not yet occurred, makes it likely that there will be some sperm waiting around for the egg once it's released.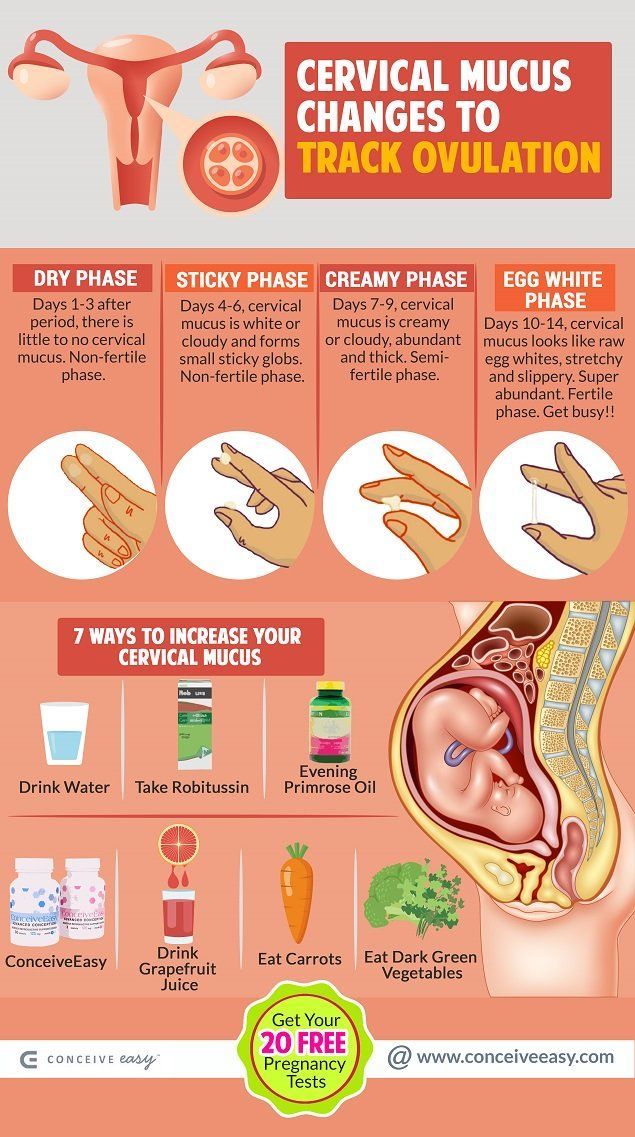 That being said, chances of conception get higher the closer you get to ovulation.
That being said, chances of conception get higher the closer you get to ovulation.
But can you get pregnant after ovulation or during your period? Outside the “fertile window” (i.e., the five days before ovulation and the day of ovulation), it is not physiologically possible to conceive if you have regular-length cycles and periods. This means that you can't get pregnant while on your period, nor can you get pregnant the day after ovulation (or in the following days). This changes if your follicular phase is abnormally short. Having said that, remember that not everyone ovulates on day 14. If you ovulate on day 9 or 10, that means you can get pregnant from sex you had on day 4 or 5 of your period (#math).
How long, on average, does it take to conceive?
This is such an important question that many different studies have attempted to answer. Leading medical experts and organizations (like the American Society for Reproductive Medicine and the American Pregnancy Association) cite 85% as the percentage of couples who conceive within 12 months of trying.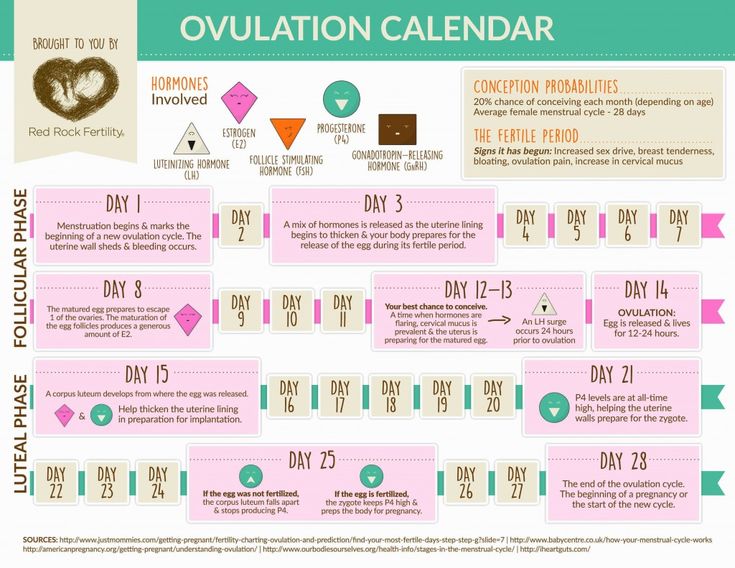 But that statistic is based on a review of studies published in a book from 1956 — meaning what was accurate back then doesn't necessarily reflect the average time to pregnancy today. What we know from the more recent peer-reviewed articles on this topic is that the average time to conceive varies from study to study, and really depends on who is included and how the study was designed.
But that statistic is based on a review of studies published in a book from 1956 — meaning what was accurate back then doesn't necessarily reflect the average time to pregnancy today. What we know from the more recent peer-reviewed articles on this topic is that the average time to conceive varies from study to study, and really depends on who is included and how the study was designed.
In a study of almost 3,000 US couples trying to conceive:
- Pregnant within six months: ranged from 62% for women between 28 and 30 to 28% for women between 40 and 45. (The average across the entire study was 58%.)
- Pregnancy rates within 12 months: ranged from 79% in women between 25 and 27 to 56% in women between 40 and 45. (The average across the entire study was 75%.)
Because participants in this study weren't explicitly instructed what to do when trying to conceive, the data from this study is likely more representative of what we'd expect to see in the real world.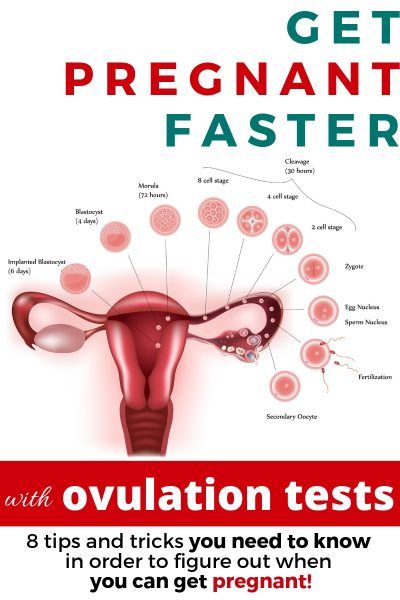
However, if you've been cycle tracking and timing intercourse, this next study might be more relevant. In this study, women between the ages of 20 and 44 were taught how to use natural family planning (e.g., monitoring cervical mucus and basal body temperature) when they started trying to conceive. You can think of this study as the most optimistic estimates.
They found that 38% will conceive within one month of TTC, 68% within three months, 81% within six months, and 92% within 12 months. This means that among couples who are TTC and have not conceived in the first six months, only half (50%) of these couples will conceive in the next six months. Let's illustrate this data a bit: Let's say you have 100 couples trying to get pregnant. This study shows that 81 get pregnant within six months. Of the 19 remaining couples who did not get pregnant in the first six months of trying, only 50% will conceive in months 7-12 of trying.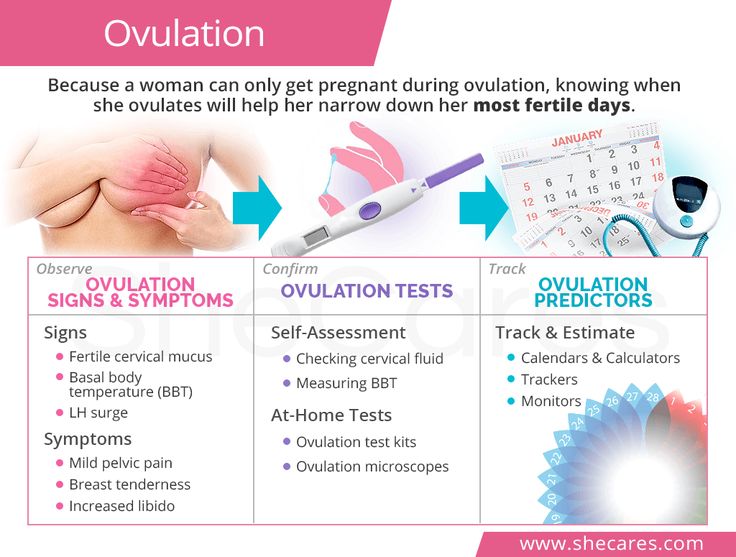
How does birth control impact the time it takes to conceive?
If you've recently stopped using a non-barrier-based method of birth control (i.e., not spermicide or condoms), these numbers may look a bit different depending on what you were using.
A team of researchers recently did a systematic review of the existing work on how different methods of birth control impacted the likelihood of getting pregnant within 12 months of TTC. Here's what they found:
- 74.7% for ex-implant users
- 77.74% for ex-injectable users
- 87.04% for ex-oral contraception users
- 84.75% for ex-IUD users (no difference between hormonal and nonhormonal IUDs)
Among women using different formulations of oral contraception, times to conception are similar — meaning how soon you're likely to get pregnant after stopping the pill isn’t affected by whether the pill was a combined oral contraceptive or the progestin-only pill, or by the pill dose. Time to pregnancy is also likely not affected by the duration of oral contraceptive use.
The main takeaway here? There's no delay in the resumption of fertility for women coming off of the most popular methods of birth control, but women coming off of the implant and injection-based methods may see a slight delay. This no-delay-in-resumption-of-fertility also doesn’t seem to be affected by how long contraception methods were used for. For more info, you can check out this post that covers birth control’s impact on fertility.
Is there a chance of conceiving if you're currently on birth control?
Chances are, if you're currently using birth control, you're not TTC — but how successful your birth control method is at preventing pregnancy differs significantly based on what you're using.
The effectiveness of birth control methods are measured in two ways:
- One way focuses on perfect use (i.e., how effective is this method if people use it exactly how it is meant to be used?).
- The other focuses on typical use (i.e., how effective is this method given how people use it in the real world?).
 Below, we'll focus on this way of measuring because of its real-world relevance.
Below, we'll focus on this way of measuring because of its real-world relevance.
According to the Centers for Disease Control and Prevention (CDC), the least effective birth control method is spermicide — of couples who only use this method over the course of a year, 28 out of 100 will experience an unintended pregnancy within the first year of typical use.
This number falls to 18 out of 100 over the course of a year for condoms, and further drops to 9 out of 100 for the pill, the patch, and the ring. While a 9 in 100 failure rate seems high for these hormone-based methods, it's important to remember that this rate takes into account user error. Because women don't always take the pill as directed or replace their patches and rings on schedule, failure rates for these methods are higher than they would be with perfect use.
There are some birth control methods that require less action on the part of women; for example, once you get an IUD, there's nothing you have to do to make sure it's doing its thang, except for remembering to get it replaced every 3-10 years (depending on the type you get).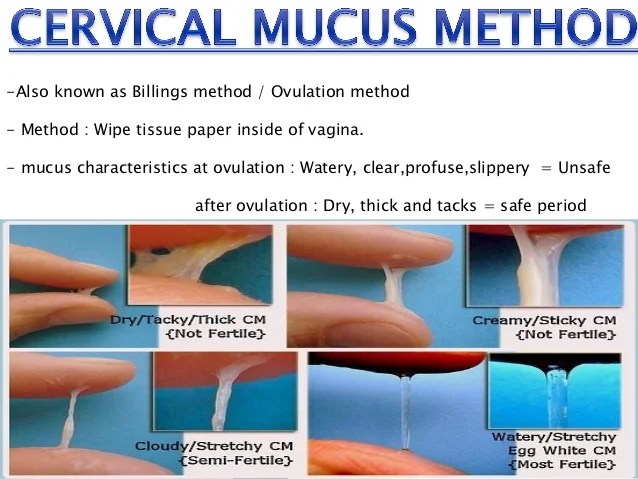 These methods, called long-acting reversible contraceptives (LARCs for short), have failure rates of less than 1%.
These methods, called long-acting reversible contraceptives (LARCs for short), have failure rates of less than 1%.
How are cycle-based conception rates and time to pregnancy affected by age?
If you've read some of our previous blog posts on aging and fertility or have used our Timeline Tool, you likely know that fertility decreases as people with ovaries (and those with sperm!) age. These changes in fertility are a function of both how many eggs we have left and how healthy those eggs are. Together, the changes in egg quality and quantity make it trickier to conceive as age goes up.
There is some data from large-scale studies investigating the effect of age on cycle-based conception rates:
- According to one study from 2002, the chances of getting pregnant during the fertile window decrease as age increases. For example, while this study estimated the chance of conception at two days before ovulation to be roughly 50% for women between the ages of 19 and 26, it was less than 30% for women between the ages of 35 and 39.
- Other studies have mirrored these findings, showing that cycle day-specific conception probabilities in the fertile window are lower among older women.
- Research shows that time to pregnancy may also differ among women of different ages. While the exact estimates differ across studies, one thing remains constant: Time to pregnancy tends to get longer as age goes up.
- For example, one study with almost 3,000 couples found that whereas 62% of women between 28 and 30 will conceive within six cycles, this drops to 56% for women between 34 and 36, and 28% for women between 40 and 45. (For other examples of good studies that also find a longer time to pregnancy as age goes up, check out here and here.)
The main takeaway here? Your chances of conceiving on each day of your fertile window change as you age, and this may in part explain why time to pregnancy is longer among older people.
How do medical conditions impact your chances of getting pregnant?
Different medical conditions may (or may not!) impact how often you ovulate, how likely a fertilized egg is to implant, and how likely a pregnancy is to be carried to term.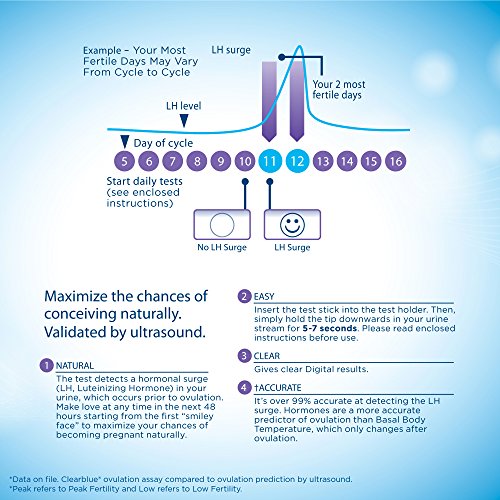
PCOS and conception
PCOS affects 1 in 10 people with ovaries, and is one of the leading culprits of infertility among couples seeking treatment at fertility clinics. In people with PCOS, ovulation is irregular and occurs less frequently. This means that people with PCOS ovulate infrequently (if at all), and ovulation doesn't always occur at predictable intervals.
There are science-backed, FDA-approved options for people with PCOS to boost their chances of conception that work by improving the frequency and regularity of ovulation. Clomid administration increases the chances of ovulation in people with PCOS, and metformin may, too. People with PCOS are at increased risk of adverse pregnancy outcomes which means they may need additional visits with their doctor when trying to conceive and after conception has occurred.
Endometriosis and conception
Endometriosis is a condition characterized by the growth of tissue that's similar to uterine lining outside of the uterus, and may manifest as excessive cramping, pressure, bloating, headaches, and bleeding. Somewhere between 6 and 10% of people with ovaries have endometriosis, and among those with infertility, up to 50% may have endometriosis (whether it be diagnosed or undiagnosed). According to the American Society of Reproductive Medicine (ASRM), the hypothesis that endometriosis causes infertility is controversial. What's not as controversial? That the reproductive hormone-based medications prescribed to help deal with the symptoms of endometriosis may not be an option for people who are TTC, as they'll disrupt your ability to conceive. In these cases, surgery or assisted reproductive technology may be the way to go, though a recent ASRM committee opinion has highlighted that there are mixed findings about how effective these options are.
Somewhere between 6 and 10% of people with ovaries have endometriosis, and among those with infertility, up to 50% may have endometriosis (whether it be diagnosed or undiagnosed). According to the American Society of Reproductive Medicine (ASRM), the hypothesis that endometriosis causes infertility is controversial. What's not as controversial? That the reproductive hormone-based medications prescribed to help deal with the symptoms of endometriosis may not be an option for people who are TTC, as they'll disrupt your ability to conceive. In these cases, surgery or assisted reproductive technology may be the way to go, though a recent ASRM committee opinion has highlighted that there are mixed findings about how effective these options are.
Thyroid dysfunction and reproductive health
Your thyroid gland is regulated by the hypothalamus-pituitary axis (HPA) — a dynamic duo featuring the hypothalamus (a part of the brain that produces hormones) and the pituitary gland (which waits for its cue from the hypothalamus). When something happens in one area of the HPA, it often triggers a chain reaction in other areas. What this means: When there are higher or lower levels of thyroid hormones, it can alter our reproductive hormones and disrupt the menstrual cycle — which makes conception trickier. But just because you have hypo- or hyperthyroidism doesn't mean you can't get pregnant. In one study of a group of almost 400 women suffering from infertility, 24% of participants were found to have hypothyroidism — but within a year of treatment, 76% were able to conceive.
When something happens in one area of the HPA, it often triggers a chain reaction in other areas. What this means: When there are higher or lower levels of thyroid hormones, it can alter our reproductive hormones and disrupt the menstrual cycle — which makes conception trickier. But just because you have hypo- or hyperthyroidism doesn't mean you can't get pregnant. In one study of a group of almost 400 women suffering from infertility, 24% of participants were found to have hypothyroidism — but within a year of treatment, 76% were able to conceive.
Prescription medications and conception
It's also possible to have a medical condition that doesn't affect ovulation or fertility, but to be on medications for that condition that do affect ovulation or fertility. For example, there's no reason to think that people with mild musculoskeletal pain would have issues with ovulation. But a recent study showed that the medication used to treat pain in a group of these women — nonsteroidal anti-inflammatory drugs (NSAIDs) — decreased progesterone levels and impaired ovulation, both of which negatively impact chances of conception.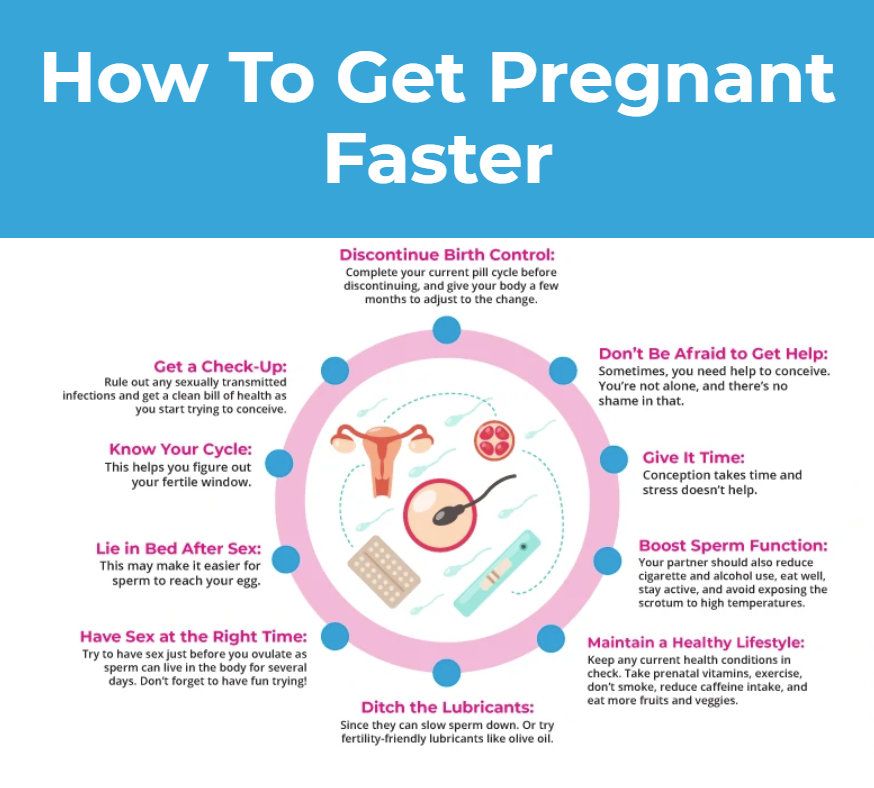 There's also evidence that medication for mental health conditions, like antidepressants, can have an effect on fertility.
There's also evidence that medication for mental health conditions, like antidepressants, can have an effect on fertility.
If you have a diagnosed medical condition or are taking prescription meds, talk to your doctor before TTC. They will be able to give you crucial insight into how your diagnoses and meds may impact your chances of conception (if at all), and suggest steps to help you maximize those chances.
How can you increase your chances of natural conception?
Ah yes, the million-dollar question. Because there are many factors that influence your chances of conceiving, there are several different things you can do to tip the scales in your favor.
Arguably the most important thing you can do to boost your odds is to track your cycles and time intercourse or insemination around ovulation. After all, if you aren't having sex or inseminating during the fertile window, your chances of conception are zero. Because the chances of conception increase in the five days before ovulation and peak the day before ovulation, you should be having sex within this window if you're looking to conceive. While some sources suggest you should be having intercourse every other day in this window, there aren’t empirical studies suggesting what the optimal intercourse frequency is, but it’s likely that more frequent = better.
While some sources suggest you should be having intercourse every other day in this window, there aren’t empirical studies suggesting what the optimal intercourse frequency is, but it’s likely that more frequent = better.
To figure out where in your cycle you are, using ovulation predictor kits (OPKs) is a good idea to better understand when you're ovulating — they measure your hormones (specifically, luteinizing hormone) to give you a heads up (via a positive result) on that egg's release. You can also use so-called “sympto-thermal” methods of cycle tracking, which involve taking your basal temperature (the “thermal”) and examining certain symptoms (the “sympto”) like your cervical mucus consistency to pinpoint when your fertile window starts and ends. Previous work has shown that cycle tracking using these symptoms can increase chances of pregnancy among TTC people with ovaries, both who have and have not had difficulty conceiving.
Certain lifestyle factors may also modulate how likely you are to conceive because they affect how regularly you ovulate, your egg quality, and your ovarian reserve. For example, having a very low or high body-fat percentage might make conception trickier. Another thing that makes it tricker? Smoking (that includes vaping!) and THC affects the gametes (another word for sex cells; eggs for those assigned “female” at birth, sperm for those assigned “male” at birth) of both people with ovaries and people with sperm.
For example, having a very low or high body-fat percentage might make conception trickier. Another thing that makes it tricker? Smoking (that includes vaping!) and THC affects the gametes (another word for sex cells; eggs for those assigned “female” at birth, sperm for those assigned “male” at birth) of both people with ovaries and people with sperm.
Summing it all up
There are so many factors that affect the likelihood of conception that sometimes it may seem like a miracle it happens at all. Putting it all together, here's what we know about chances of conception:
- Because of how long sperm can live in the female reproductive tract and how long an egg can be fertilized, it's possible to conceive only during a specific time of the cycle. The chances of conception increase as you get closer to ovulation.
- The chances of conceiving on each day of the cycle differ a bit based on your age, with younger age → higher chances. Because of this, time to pregnancy changes with age too.

- Used pills, injections, patches, IUDs in the past? There's no evidence that these should affect your odds of conceiving in the long run, but time to pregnancy is slightly longer in those who recently stopped using injections or implants.
- Certain medical conditions like PCOS and endometriosis make conception trickier. If you think you may have one of these conditions, it’s best to see an OB-GYN or REI.
While we can't control things like our age or diagnoses, there are steps you can take to boost your chances of getting pregnant: testing your fertility hormones to see whether underlying conditions like PCOS may be a factor affecting your fertility, using ovulation predictor kits or tracking cervical mucus to pinpoint ovulation (and timing intercourse accordingly), and embracing healthy habits.
This article was medically reviewed by Dr. Jane van Dis, MD, FACOG. Dr. van Dis is an OB-GYN, co-founder and CEO of Equity Quotient, and Medical Director for Ob Hospitalist Group.
When is a woman most fertile?
If you are a woman taking precautions to prevent pregnancy, or if you are thinking about pregnancy in some way in the future, the issue of fertility usually remains in the background.
The question of when a woman is most fertile has two aspects.
First, is the menstrual monthly cycle and the period when a woman is most fertile.
To figure out the arithmetic, a fertility calendar or an ovulation calculator will help. The second aspect of the question concerns biological age and the stage of life at which women are most fertile. In our article, we will look at the monthly cycle, the days that are the most fertile during this cycle, and various means of monitoring and predicting ovulation. This makes it possible to predict the time of maximum fertility with some accuracy.
Second , we look at the stages of fertility at various times in a woman's life and their impact on her ability to conceive.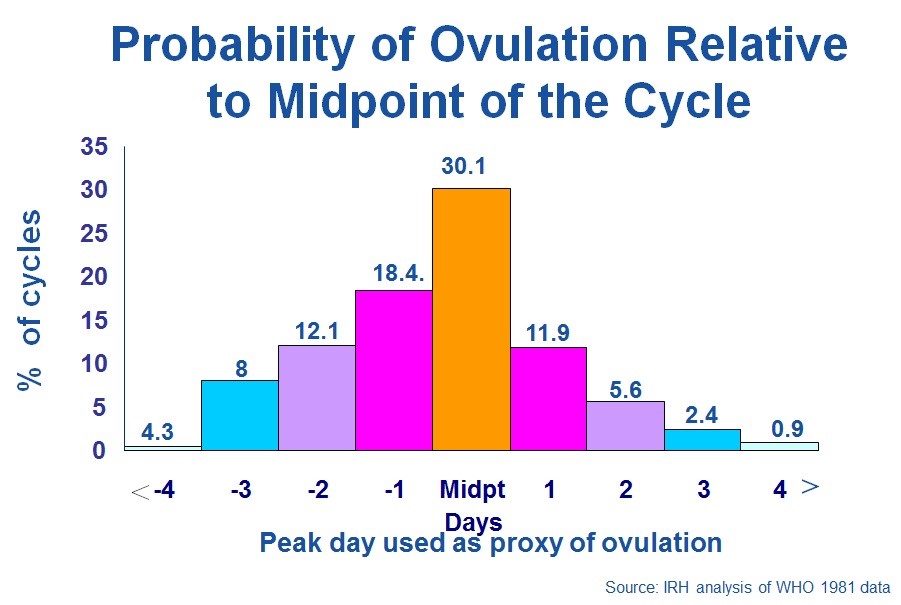
It is well known that fertility peaks at age 20 and begins to decline after age 30; after 35 years, natural conception rates begin to drop sharply. However, in today's society, many women, for understandable financial and social reasons, choose to delay childbearing until the age of thirty. Thus, we are faced with the paradoxical situation where many women, who have long sought to prevent pregnancy in their younger years, find themselves in a situation where they begin to look for ways to increase their chances of conceiving.
When is a woman most fertile? What does the menstrual cycle show?
In a woman, the ability to conceive is maximum a day or two before and after ovulation. This is when the egg is released from the ovaries. You can calculate with a reasonable degree of accuracy when ovulation will occur, especially if your cycle is regular, anywhere between 24 and 35 days. Consider the start of your period (bright spotting) as the first day of your cycle, and the day before the next as the end of your cycle.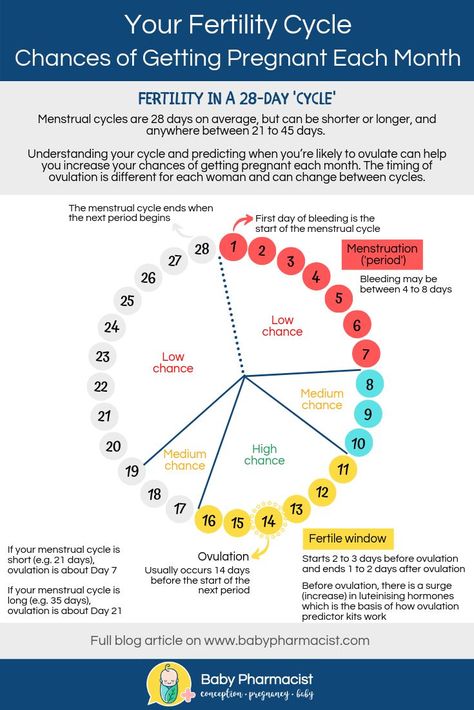 Ovulation usually occurs 12-16 days before the start of the next cycle. Thus, if you have a regular 28-day cycle, then the indicator remains the same: ovulation occurs on the 12th-16th day. However, fertile time is not limited to these few days. Remember that you can get pregnant if you have unprotected sex at any time during the week before ovulation, as sperm can live in a woman's genital tract for up to seven days.
Ovulation usually occurs 12-16 days before the start of the next cycle. Thus, if you have a regular 28-day cycle, then the indicator remains the same: ovulation occurs on the 12th-16th day. However, fertile time is not limited to these few days. Remember that you can get pregnant if you have unprotected sex at any time during the week before ovulation, as sperm can live in a woman's genital tract for up to seven days.
Fertility specialists generally advise that if you are hoping to get pregnant, it is advisable to specifically schedule contacts around this time, as it can be difficult to calculate the exact day of ovulation, and trying to have sex on a schedule can cause unnecessary stress and anxiety. For the best chance of getting pregnant as long as there are no underlying fertility problems, it is recommended to have intercourse every 2-3 days during your cycle. In addition, fertility calendars, an ovulation test, and self-monitoring for signs of ovulation can help predict the ideal time to conceive.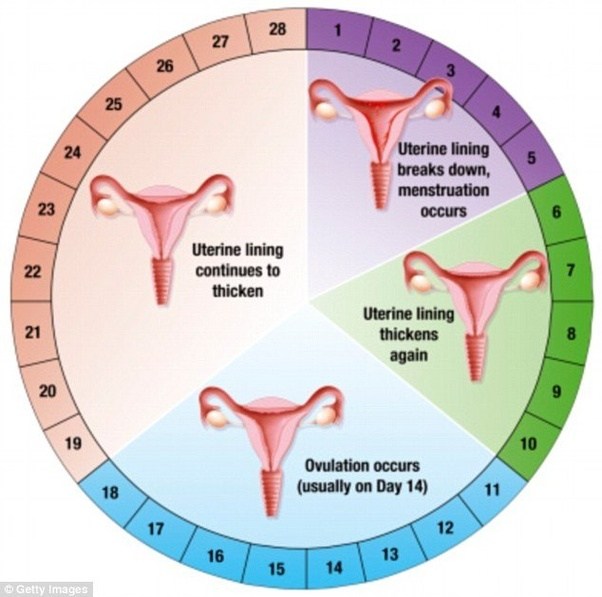
Menstrual calendar
It could be an old-fashioned pen and paper, a spreadsheet, or one of the many online calendars available. They are also known as ovulation calendars or ovulation calculators. They all do the same thing: keep track of your menstrual cycle dates and use the 12-16 day calculation outlined above to determine the days on which you are most likely to conceive.
Ovulation Tests
These are test kits that measure the level of luteinizing hormone (LH) in your urine. The essence of the measurement is to capture the surge in LH levels that occurs during your cycle a couple of days before ovulation. There are also tests that measure the same hormone pulsation but use a saliva sample. In these tests, saliva takes on the appearance of a fern-like pattern when it dries on glass. However, the most accurate analysis that allows you to track the LH peak is a urinalysis (rarely used in routine practice).
Self-monitoring for signs of impending ovulation
Self-monitoring includes taking temperature every morning after waking up, as well as monitoring the quality and consistency of vaginal mucus secretions. This must continue for several months so that ovulation can be tracked. This is the least reliable of the methods, because there can be many different causes of body temperature fluctuations (night rises, colds, blood sugar fluctuations), and in fact, many girls rightly find this procedure tedious and difficult to perform.
This must continue for several months so that ovulation can be tracked. This is the least reliable of the methods, because there can be many different causes of body temperature fluctuations (night rises, colds, blood sugar fluctuations), and in fact, many girls rightly find this procedure tedious and difficult to perform.
Fomin's clinic — a network of multidisciplinary clinics
Today's world is full of information: literally with one click, each of us can open the Universe and learn everything - from string theory to concert posters for the next week. It is all the more interesting that, having unlimited access to knowledge, we still live in myths - and sometimes they arise, including thanks to the Internet, replicating untruth and absurdity.
We have prepared for you a short “blitz” of six questions or myths about pregnancy and conception, so that you are fully equipped and do not believe the tales on the Internet.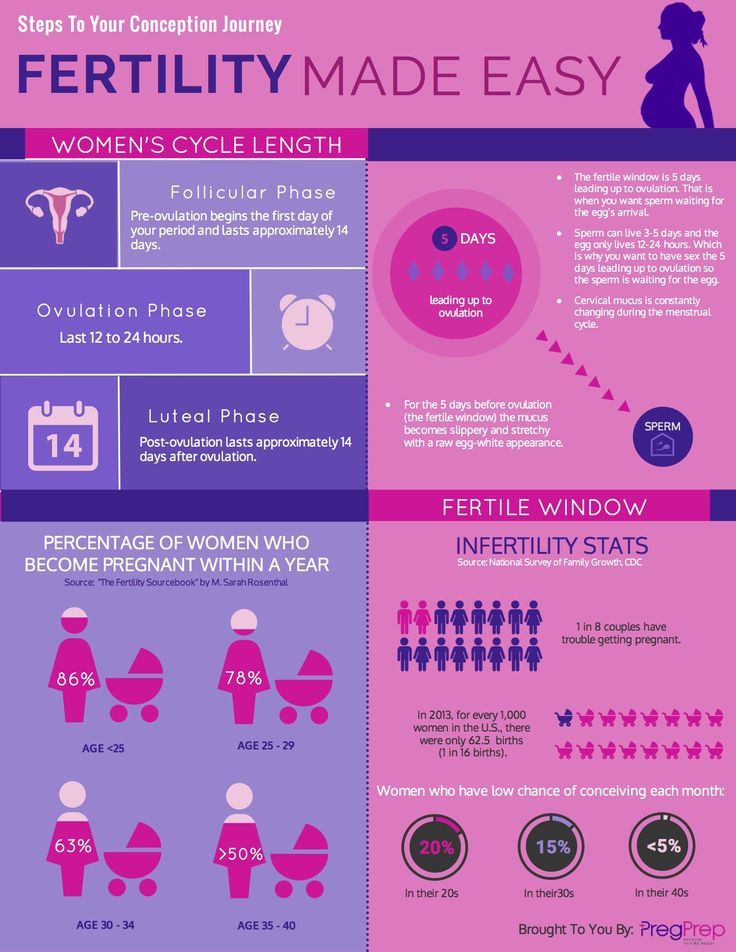
Well... not exactly. Firstly, the idea of a “full examination” is a clear exaggeration, because there is no single list of tests that an expectant mother needs to pass. Ideally, visit a doctor three months before the end of contraception, get tested for STIs and antibodies to rubella. If additional examinations are required, you will be individually prescribed everything you need - including, probably, vaccinations that should be “updated”. As for alcohol and smoking, they are really contraindicated at the stage of pregnancy planning, so if you have these addictions, you will have to give them up. However, it should be remembered that smoking cessation applies to both electronic cigarettes and “passive smoking”, which can lead to dangerous consequences for the fetus.
Spoiler: no big deal. Do not panic and blame yourself for all mortal sins because of a glass of wine. With the recognized insecurity of alcohol, scientists have proven that a woman drinking 1-2 servings a couple of times a week should not harm the unborn child. For men, the allowable figures are slightly higher - 3-4 doses of alcohol per week. The main thing is to know the measure and not to overdo it.
For men, the allowable figures are slightly higher - 3-4 doses of alcohol per week. The main thing is to know the measure and not to overdo it.
There is, of course, a simplified formula for calculating the estimated due date: plus 7 days and minus 3 months from the date of the last period, but to be honest, it doesn’t work like that: the fact is that it is very difficult to “program” pregnancy and make sure that the child is born when you want. If you have a plan and are going to stick to it, be prepared for the fact that things can go wrong, if only because:
- the duration of pregnancy is not 40 weeks, but 37-42 weeks, which means that you can easily get into a five-week “loop”, which will reduce the chances of fulfilling the plan to zero;
- with regular sex, the probability of conception is not 1 time per month (exactly when you guessed it), but 1 time per year.
Nothing is impossible. .. However, it is worth clarifying the question a little: you can get pregnant only during ovulation (more precisely, shortly after it), but you can have sex, which will lead to a long-awaited pregnancy, on different days. Of course, on the days of menstruation, the probability is lower than on the days that precede ovulation, but on none of the days of the menstrual cycle this probability is not zero.
.. However, it is worth clarifying the question a little: you can get pregnant only during ovulation (more precisely, shortly after it), but you can have sex, which will lead to a long-awaited pregnancy, on different days. Of course, on the days of menstruation, the probability is lower than on the days that precede ovulation, but on none of the days of the menstrual cycle this probability is not zero.
Let's just say that trying multiple times a day is a bad idea. Why? At least because ejaculation more than once a day worsens the quality of sperm, as a maximum - such perseverance and zeal can create tension in the relationship of partners. Doctors advise to have sex every 2-3 days throughout the cycle, and not try to guess the moment and throw all your strength into this short period.
Planning the sex of a child is an extremely prolific topic for myth-makers. Some believe that with the help of a special table that takes into account such indicators as the age of the father and mother, the month of conception, it is possible to accurately calculate the sex of the child.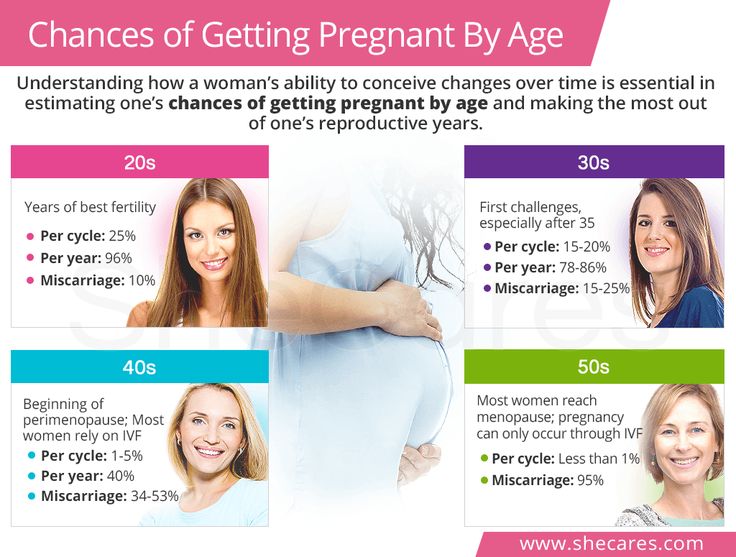 This "method" is anti-scientific and has nothing to do with reality.
This "method" is anti-scientific and has nothing to do with reality.
Another myth is that you have to get pregnant on the day you ovulate to have a boy. Previously, scientists really believed that X and Y spermatozoa differ from each other (Y are faster), and the sex of the child is formed due to the first one that broke through the defenses of the female egg. If you want to conceive a boy, you need to have sex on the day of ovulation so that the Y-sperms responsible for the "male sex" have more time to get to the egg located farthest from the entrance to the uterus.
However, this myth does not stand up to criticism: the fact is that there is no difference between the X and Y chromosomes, which means that the sex of the child does not depend on which of the sperm reaches the egg first. Moreover, not the fastest fertilizes the egg: thousands of spermatozoa simultaneously break its shell.
From this follows the conclusion: modern science does not know how to determine the sex of the child during natural conception, and therefore there is no universal recipe.