Breech baby at 38 weeks problems
Everything You Should Know About Breech Babies
When it comes to giving birth, one common concern for new mums is their baby laying bottom up, and the impact it can have on their birthing plan. Breech is very common in early pregnancy, but by weeks 36-37, most babies will turn themselves into the head-first position as a natural movement. If your baby remains in this breech position, it can mean that your birth may be considered a little more high risk.
As healthcare professionals working within maternity, we encounter women who have a breech baby at term on a fairly regular basis and so are used to answering the questions that you may have. To put your mind at ease, we thought it might be helpful to answer the common questions, which often arise about breech babies.
Why Might a Baby Lay Breech?
Approximately 3-4% of babies lie bottom down towards the end of pregnancy, known as a breech position, rather than the usual cephalic or head down position.
It may just be a matter of chance that your baby has not turned and remains in a breech position, however there are some factors which may make breech positioning more likely. These include:
If this is your first pregnancy
- You have a uterine abnormality
- You go in to labour prematurely
- If the edge of your placenta is close to or covering your cervix (also known as a placenta praevia)
- When there is too little, or too much, amniotic fluid, making turning difficult
- If you are having more than one baby (twins, triplets etc.)
Babies who are breech in the last trimester are more likely to have developmental hip dysplasia (DDH), also known as congenital hip dislocation, due to the position they lie in. You’ll be offered an ultrasound scan of their hips a few weeks after birth to check for this, and it will be treated if necessary.
What Are My Options for Birth if My Baby is Breech?
If your baby hasn’t shown any sign of moving into a head-down birth position on their own, your medical team will usually discuss a procedure called an external cephalic version (ECV), with you.This can be done any time from 36 weeks right up until the early stages of labour, but is more successful when there’s more space for your baby to move around 36-37 weeks. We’ll cover this in more detail a little later.
We’ll cover this in more detail a little later.
If you do not opt for an ECV or it’s unsuccessful, your options will include:
- Planned caesarean section
- Planned vaginal breech birth
Both methods of birth carry there own risks and benefits, which should be discussed in more detail with your healthcare professional. Giving birth to a breech baby vaginally is not usually any more painful than a head-down position, as you’ll have the same pain relief options available to you, although it does carry a higher risk of perinatal morbidity (2:1000 compared to 1:1000 with a cephalic baby). This is mainly due to the risk of something called head entrapment. In a cephalic baby, the hard skull of the head, paves the way for the rest of the body, the risk is in a breech birth, is that the body delivers and then the head gets stuck. The key to a successful vaginal breech birth, is having it in a unit that have healthcare professionals, who are experienced in managing this kind of birth.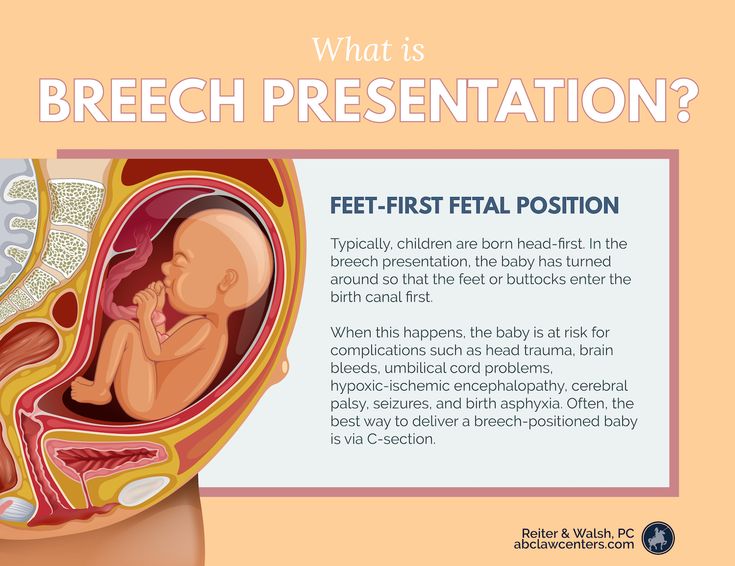
Between 20% and 30% of these 3-4% of births will not be diagnosed until the late stages of labour and as a result, many babies in the breech position are delivered via emergency caesarean section. While this may not fit in with your original birth plan, your medical team will make recommendations based around what is safest for you and your baby.
Turning a Breech Baby with ECV
External cephalic version, also known as ECV, is the process of turning a breech baby in the womb. This involves applying firm but gentle pressure on your abdomen in order to encourage your baby to do a somersault in the uterus to lie head-first.
You will normally be offered a medication which can help to relax the muscle of your uterus before the ECV, which can help to improve the chances of turning your baby. Before the EVC, you will have an ultrasound scan to confirm that your baby is in breech. You will also have your blood pressure and pulse checked and your baby’s heart beat will be monitored throughout the duration of the procedure to make sure you’re both okay. You will then have a second ultrasound scan after the procedure to see if the baby has turned.
You will then have a second ultrasound scan after the procedure to see if the baby has turned.
An ECV can be uncomfortable and sometimes painful, however the procedure will be stopped if you are experiencing any pain. The procedure itself only lasts for a few minutes and the experience for women is hugely varied with 5% to 1/3 reporting significant pain. The most important thing to remember is that you are in charge and can ask for it to stop at any point. If you experience any bleeding, abdominal pain, contractions or reduced fetal movements after the ECV then you should contact your doctor, midwife or hospital immediately.
It is important to note that an EVC would not be carried out in any of the following circumstances:
- You need a caesarean section for any other reason
- You have recently experienced vaginal bleeding
- Your baby’s heart rate tracing is abnormal
- Your waters have broken
- You are pregnant with more than one baby
An EVC is successful for approximately 50% of women, and it is typically more successful if you have previously had a natural, vaginal birth. Risks are low, with studies suggesting a small increased chance at 0.5% of emergency caesarean in the 24 hours following a successful ECV, and no difference in Apgar scores in babies.
Risks are low, with studies suggesting a small increased chance at 0.5% of emergency caesarean in the 24 hours following a successful ECV, and no difference in Apgar scores in babies.
What Other Options Do I Have To Help Turn My Baby?
There are a number of other options to consider aside from an ECV, including:
- Moxibustion – the traditional Chinese practice of burning dried mugwort, which is thought to increase fetal activity.
- Acupuncture – TCM practitioners advocate the benefits of acupuncture to turn your baby, although there are no studies which support this.
- Yoga – there’s not enough evidence to determine if postural modifications increase the chance of your baby turning. However, putting yourself into a forwards and open position may give your baby more space to turn.
Our Complete Birth Preparation Course can offer more insight into complicated labour and birth, including assisted vaginal delivery, complications of labour and caesarean section.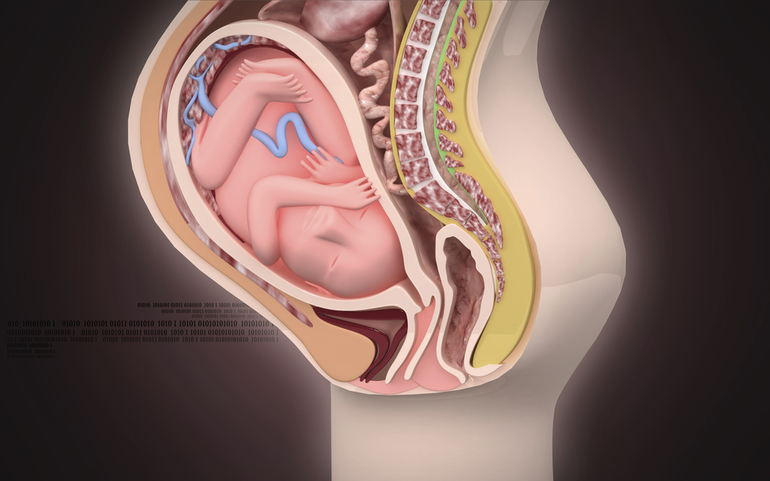 To find out more about breech babies, don’t hesitate to get in touch with a member of our team, or sign up to our newsletter for regular top tips on all things birthing.
To find out more about breech babies, don’t hesitate to get in touch with a member of our team, or sign up to our newsletter for regular top tips on all things birthing.
Sources –
https://www.kcl.ac.uk/news/new-algorithm-to-increase-breech-birth-safety
https://www.rcog.org.uk/globalassets/documents/pat…
Causes, Complications, Turning & Delivery
Overview
Types of breech positions during pregnancy.What is a breech baby?
A breech baby, or breech birth, is when your baby’s feet or buttocks are positioned to come out of your vagina first. Your baby’s head is up closest to your chest and its bottom is closest to your vagina. Most babies will naturally move so their head is positioned to come out of the vagina first during birth. Breech is common in early pregnancy and most babies will move to a head-first position by 36 weeks of pregnancy. This head-first position is called vertex presentation and is the safest position for birth.
How common is a breech baby?
There is a small chance that your baby will not move into a head-first position before 37 weeks of pregnancy. Breech babies account for about 3% to 4% of all full-term pregnancies.
What are the types of breech position a baby can be in?
There are several fetal positions your baby may present in. Ideally, your baby is positioned head-down, facing your back, with their chin tucked to their chest.
Breech babies can be in a few different positions:
- Frank breech: The baby’s buttocks are aimed at the vaginal canal with its legs sticking straight up in front of their body and the feet near their head.
- Complete breech: The baby’s buttocks are pointing downward and both the hips and the knees are flexed (folded under themselves).
- Footling breech: One or both of the baby’s feet point downward and will deliver before the rest of their body.
- Transverse lie: This is a form of breech presentation where your baby is positioned horizontally across your uterus instead of vertically.
 This would make their shoulder enter the vagina first.
This would make their shoulder enter the vagina first.
How does a breech baby affect pregnancy?
Your pregnancy is usually not affected. Most breech babies are born healthy, although there is a slightly elevated risk for certain birth defects. Your baby’s movements may feel a little different. You will feel your baby’s kicks lower in your belly. You may feel a hard lump closer to your ribs. This is your baby’s head.
If you planned a vaginal delivery, a breech baby could change these plans. When your baby is breech, a vaginal delivery can be complicated and dangerous. Your healthcare provider may feel comfortable attempting a vaginal breech delivery, but in most cases, they will recommend a Cesarean birth (C-section).
How does a breech baby affect delivery?
If your baby presents in a breech position after 36 weeks of pregnancy, your birthing plan will likely change. It's usually unsafe for a breech baby to be born vaginally due to risks of injury.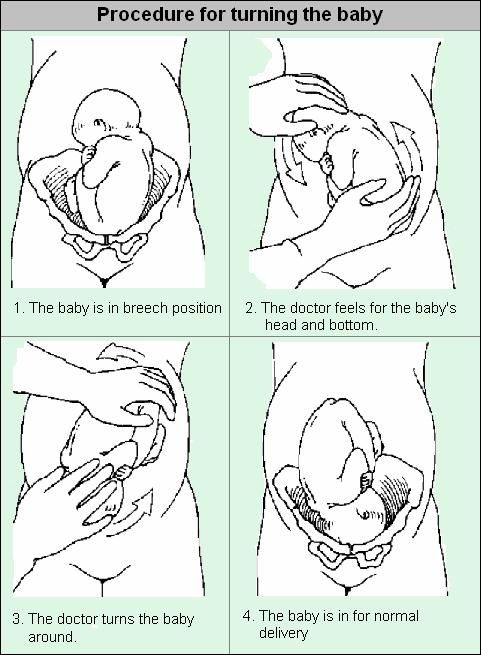 In most cases, a planned C-section is the safest way to deliver your baby. Some healthcare providers may be comfortable with a vaginal breech birth. In some cases, turning your baby to a head-down position while they are still inside your uterus is an option. Your baby is then born head first.
In most cases, a planned C-section is the safest way to deliver your baby. Some healthcare providers may be comfortable with a vaginal breech birth. In some cases, turning your baby to a head-down position while they are still inside your uterus is an option. Your baby is then born head first.
Symptoms and Causes
How can you tell if your baby is breech?
You may be able to tell if your baby is breech, especially if you have had past pregnancies where your baby was head-first. The places where you feel lumps and kicks might indicate that your baby is breech. Let your healthcare provider know where you feel movement. They will feel your belly or do an ultrasound to confirm that your baby is breech.
What causes a baby to be breech?
It’s not always known why a baby is breech. Some factors that may contribute to this position are:
- You are expecting multiples (twins or more). This makes it harder for each baby to get into the right position.
- There is too much or too little amniotic fluid.

- The uterus is not normal in shape or has abnormal growths such as fibroids. Most of the time, the uterus is shaped like an upside-down pear. If it's shaped differently, there might not be enough room for a full-grown baby to move into position.
- The placenta covers all or part of the cervix (a condition called placenta previa).
- The baby is preterm. This means they are less than 37 weeks gestation and may not have turned to a head-first position.
- Your baby has a birth defect that causes them to not turn head-down.
Diagnosis and Tests
How is a breech baby diagnosed?
Your healthcare provider may be able to tell which way your baby is facing by placing their hands at certain places on your abdomen. By feeling where the baby’s head, back and buttocks are, it’s usually possible to find out what part of the baby is positioned to come out of the vagina first. An ultrasound may be used to confirm the baby’s position.
When is a breech baby diagnosed?
Almost all babies are breech at some point.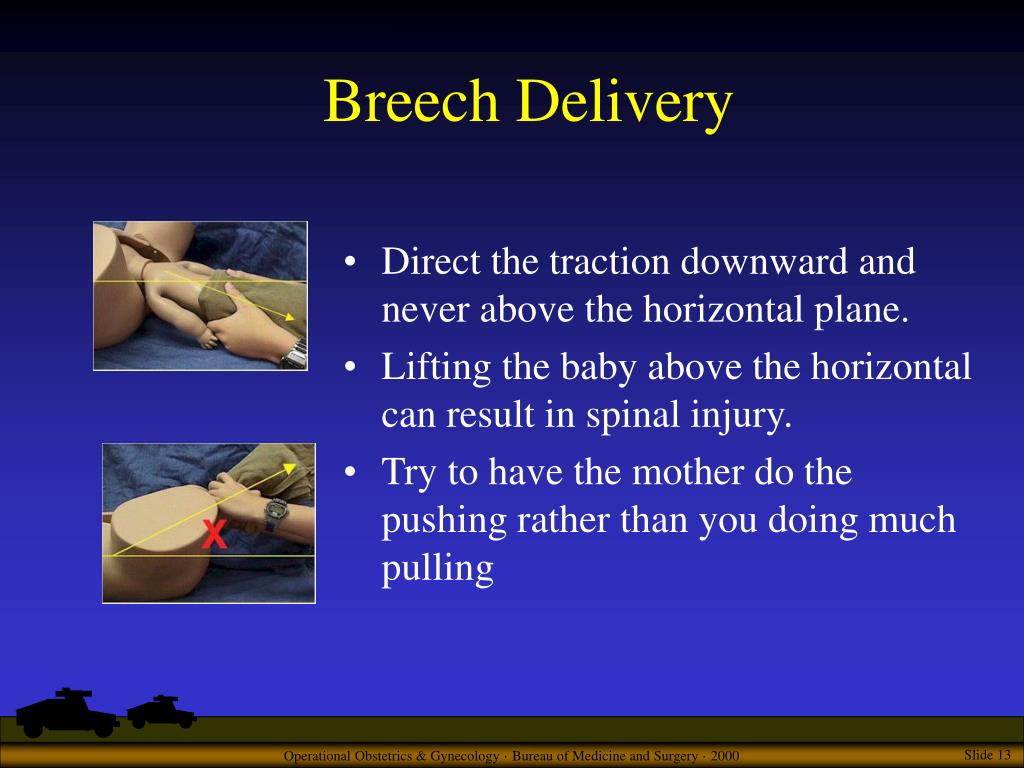 As your pregnancy progresses, your baby will naturally move to a head-down position — probably between 32 and 36 weeks. Your healthcare provider will feel your belly and determine where your baby is positioned. This will happen during most of your appointments in the third trimester. After 37 weeks, a breech baby usually does not turn on their own. Your healthcare provider will discuss delivery options with you.
As your pregnancy progresses, your baby will naturally move to a head-down position — probably between 32 and 36 weeks. Your healthcare provider will feel your belly and determine where your baby is positioned. This will happen during most of your appointments in the third trimester. After 37 weeks, a breech baby usually does not turn on their own. Your healthcare provider will discuss delivery options with you.
Management and Treatment
What are the options for treating a breech baby?
If your baby is breech at 37 weeks of pregnancy, your healthcare provider may:
- Try turning your baby in your uterus into the head-first position.
- Plan a C-section birth.
- Plan a vaginal breech birth.
What are some complications of having a breech baby?
The complications of having a breech baby usually do not occur until it's time to deliver. Some breech babies can be safely delivered through the vagina.
The risks of attempting a vaginal breech birth are:
- Injuries to your baby’s legs or arms such as dislocated or broken bones.

- Umbilical cord problems. The umbilical cord can be flattened or twisted during delivery. This can cause nerve or brain damage due to a lack of oxygen.
Will my doctor try to flip my baby if it's breech?
If your baby is breech, your healthcare provider may consider turning your baby so that you can have a vaginal delivery. In some cases, trying to turn your baby may not be safe or the risks outweigh the benefits.
Flipping your baby may not be safe if you have any of the following:
- Bleeding from your vagina.
- Placenta previa. This is when your placenta covers all or part of your cervix.
- A nonreactive nonstress test.
- An abnormally small baby.
- Low level of amniotic fluid.
- Low or high fetal heart rate.
- Premature rupture of the membranes.
- Twins or multiples.
The most common method used to turn a breech baby is called external cephalic version (ECV). It's performed by your healthcare provider around 37 weeks of pregnancy. This procedure is performed in the hospital just in case an emergency occurs. It involves placing hands on your abdomen and applying firm pressure to turn your baby to a head-down position while your baby is still in your uterus. It is about 65% effective and carries some risks.
This procedure is performed in the hospital just in case an emergency occurs. It involves placing hands on your abdomen and applying firm pressure to turn your baby to a head-down position while your baby is still in your uterus. It is about 65% effective and carries some risks.
What are the risks of turning my breech baby?
The risks of ECV include the following:
- Premature labor.
- Premature rupture of the amniotic sac.
- Blood loss for either you or your baby.
- Emergency C-section.
- Your baby might turn back to the breech position.
Although the risk of having these complications is small, some healthcare providers prefer not to try to flip a breech baby.
Will my breech baby flip on their own?
Most babies will flip to a head-down position before they reach full term (37 weeks). If your baby is still in a breech position at this time, your healthcare provider will determine if you can deliver vaginally or if you will need a C-section.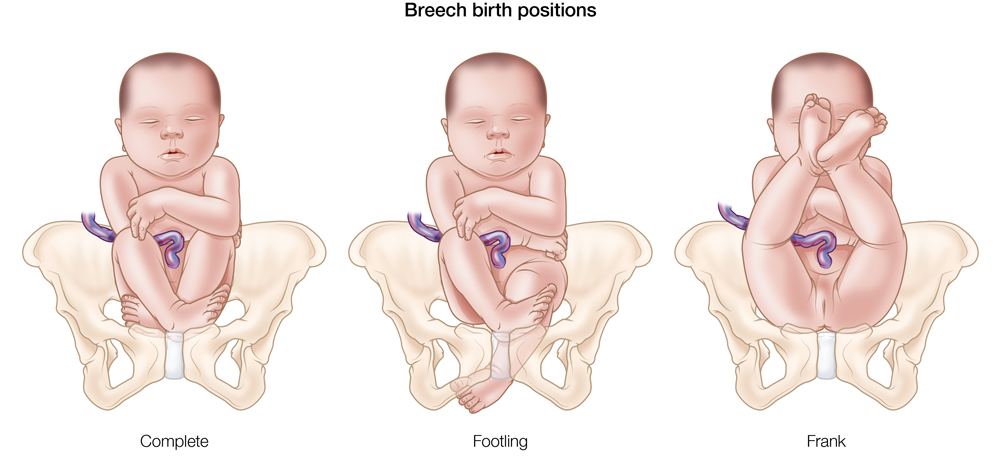
How can I flip my baby if it's breech?
Some women will try at-home methods to flip their baby to a head-first position. They may help, but there is no scientific evidence that they work.
- Bridge position: Lie on the floor with your legs bent and your feet flat on the ground. Raise your hips and pelvis into a bridge position. Hold this position for 10 or 15 minutes several times a day.
- Child’s pose: Rest in the child’s pose for 10 to 15 minutes. It can help relax your pelvic muscles and uterus. You can also rock back and forth on your hands and knees or make circles with your pelvis to promote activity.
- Music: Place headphones or a speaker at the bottom of your uterus to encourage your baby to turn.
- Temperature: Try placing something cold at the top of your stomach where your baby’s head is. Then, place something warm at the bottom of your stomach.
A chiropractic technique, called the Webster technique, can also help your uterus relax.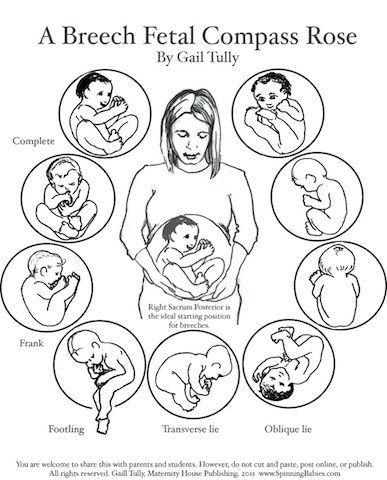 Some providers even recommend acupuncture. Both of these techniques need to be done by a professional that your healthcare provider has recommended.
Some providers even recommend acupuncture. Both of these techniques need to be done by a professional that your healthcare provider has recommended.
Prevention
How can I reduce my risk of having a breech baby?
There is nothing you can do to prevent your baby from being in a breech position. If your baby is in a breech position, it’s not because you did anything wrong.
Outlook / Prognosis
Can you deliver vaginally with a baby breech?
It's possible to deliver a breech baby vaginally. It can be more dangerous for the baby and the risk of injury is much higher. If the umbilical cord is compressed during birth, the baby could be deprived of oxygen and this could harm their brain and nerves. The cord could also slip around the baby’s neck or arms, causing injury. Healthcare providers have various levels of comfort with vaginal deliveries of breech babies. Talk to your provider about the risks and benefits of different types of birth for a breech baby.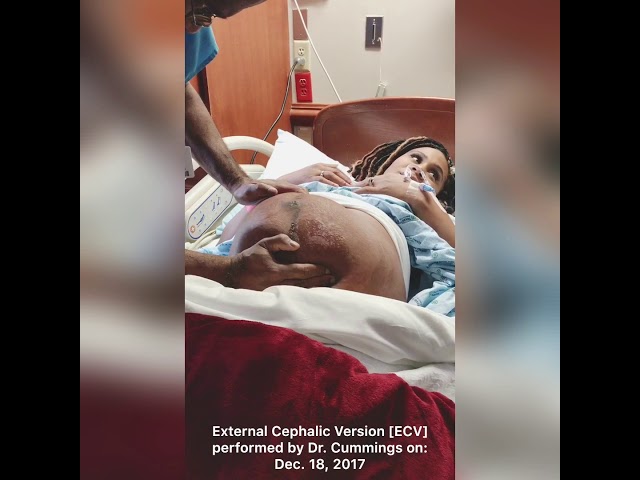
Living With
When should I see my healthcare provider?
Contact your healthcare provider if you experience any of the following symptoms during pregnancy:
- Severe cramping or contractions.
- Vaginal bleeding.
What questions should I ask my doctor?
Learning your baby is breech may give you concerns about your delivery. It’s completely natural to have questions. Some questions to ask your doctor can include:
- How can I tell if my baby is breech?
- Is my baby OK?
- What are the benefits and risks of turning my baby?
- What are my options for delivery if my baby remains in the breech position?
- What are the health risks to my baby and me if they are born breech?
Frequently Asked Questions
Do birth defects cause breech position?
Birth defects are slightly more common in breech babies. It might be the reason that the baby didn’t move to the head-down position. Most babies who are breech at delivery are born without any health complications.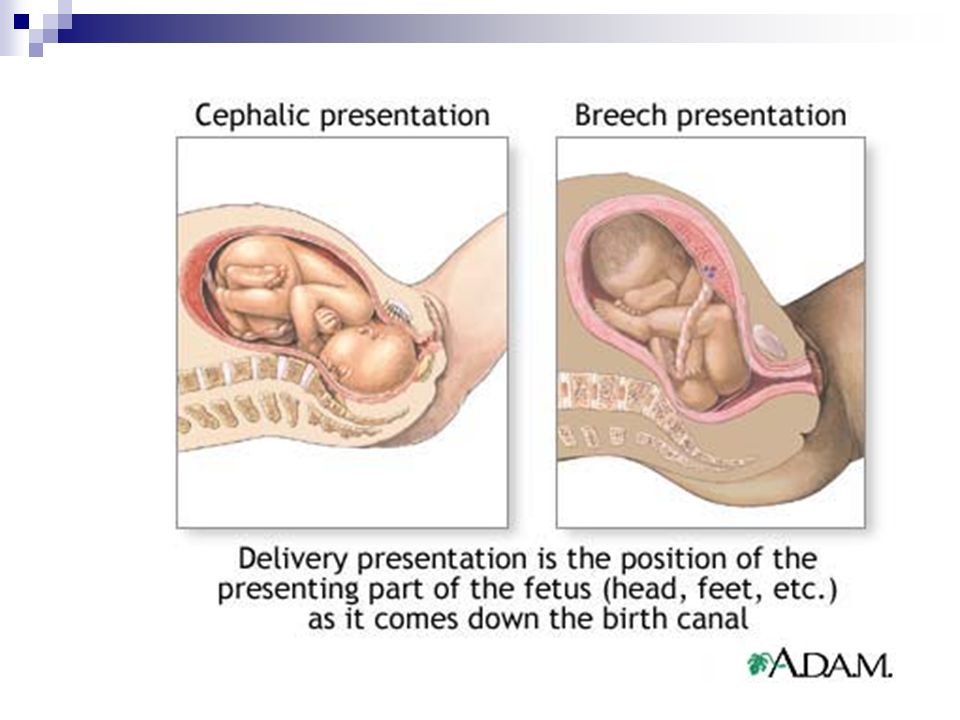
Will I need a C-section if my baby is breech?
Most of the time, a C-section is the safest way to deliver a breech baby. Your risks of developing complications are much higher if you try to deliver a breech baby through the vagina. However, some healthcare providers may feel comfortable performing a vaginal breech birth.
How does labor start if your baby is breech?
Having a breech baby doesn’t change some of the first signs of labor like contractions or rupturing of your membranes. In most cases, your healthcare provider will recommend a planned C-section. If your delivery is planned, you may not have any labor symptoms.
If you are in labor and go to the hospital for delivery, your provider will confirm your baby’s position a final time. Your provider could attempt a vaginal delivery, but it's more likely they will proceed with a C-section to be safe.
A note from Cleveland Clinic
Having a breech baby can be unexpected and change the vision you had for childbirth.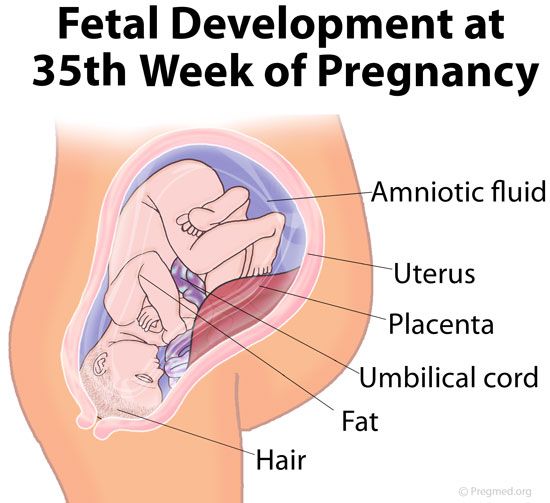 Talk to your healthcare provider about what to expect during a breech delivery. They can help you understand the risks and benefits of a breech birth so that you and your baby are kept safe.
Talk to your healthcare provider about what to expect during a breech delivery. They can help you understand the risks and benefits of a breech birth so that you and your baby are kept safe.
The problem of breech presentation of the fetus. External obstetric rotation of the fetus on the head.
Breech presentation of the fetus occurs in 3% -5% of cases at full-term pregnancy. Vaginal delivery with breech presentation is associated with high risks both on the mother's side and on the fetus's side. Thus, breech presentation is currently considered pathological, even if the conditions necessary for childbirth through the birth canal are ideally met, and the fetus is relatively small relative to the size of the mother's pelvis. During vaginal delivery, the arms and head of the fetus may tilt back, which can lead to injury.
Currently the most common method of delivery in breech presentation is a caesarean section (90%). Among the indications for the use of caesarean section, breech presentation ranks third among others in the world. However, this the operation does not make it possible to completely eliminate the risk of trauma to the fetus, since when it is removed, it is also possible to tilt the arms and head of the fetus, and their release requires the use of complex manipulations.
However, this the operation does not make it possible to completely eliminate the risk of trauma to the fetus, since when it is removed, it is also possible to tilt the arms and head of the fetus, and their release requires the use of complex manipulations.
To correct breech presentation today, the world is using EXTERNAL OBTETAL TURNING OF THE FETUS ON THE HEAD proposed at the end the century before last by the Russian obstetrician Arkhangelsky B.A.
External obstetric cephalic rotation (EFRT) is a procedure during which the doctor turns the fetus from the outside through the wall of the uterus breech presentation in the head. A successful attempt at NAPP allows women to give birth on their own, avoiding a caesarean section.
What is required for external cephalic fetal rotation?
External obstetric rotation of the fetus on the head is performed before the onset of labor, usually starting from 36 weeks of pregnancy.
It is necessary to consult a doctor and conduct an ultrasound examination to confirm the fact breech presentation of the fetus and determine the conditions for NAPP, starting from 34-35 weeks of pregnancy.
| The operation of external rotation of the fetus on the head in breech presentation |
When NAPP is possible:
- From 36 to 37 weeks, since with earlier use, it is likely that it will return to the breech presentation.
- In the presence of a singleton pregnancy.
- Subject to the mobility of the buttocks of the fetus (if they are tightly pressed against the entrance to the mother's pelvis, it will be extremely difficult to change the position of the fetus).
- Sufficient amount of amniotic fluid. With oligohydramnios, this manipulation can be traumatic for the fetus, while with polyhydramnios there is a high probability of a reverse rotation of the fetus in a breech presentation.

- Sufficient amount of amniotic fluid. With oligohydramnios, this manipulation can be traumatic for the fetus, while with polyhydramnios there is a high probability of a reverse rotation of the fetus in a breech presentation.
- Fetal head flexed
When NAPP is not possible:
- With the outflow of amniotic fluid.
- If the patient has contraindications to the use of drugs used to relax the uterus (tocolysis).
- In the presence of obstetric indications or indications from the health of the mother for delivery by caesarean section.
- With the extensor position of the fetal head.
- If the fetus has congenital developmental features.
- With multiple pregnancy.
- In the presence of structural features of the uterus in a pregnant woman
However, in addition to this, there are a number of factors that may favor or, on the contrary, serve as a contraindication to external obstetric turning the fetus on the head, and which can only be determined by a doctor during a direct examination of a pregnant woman.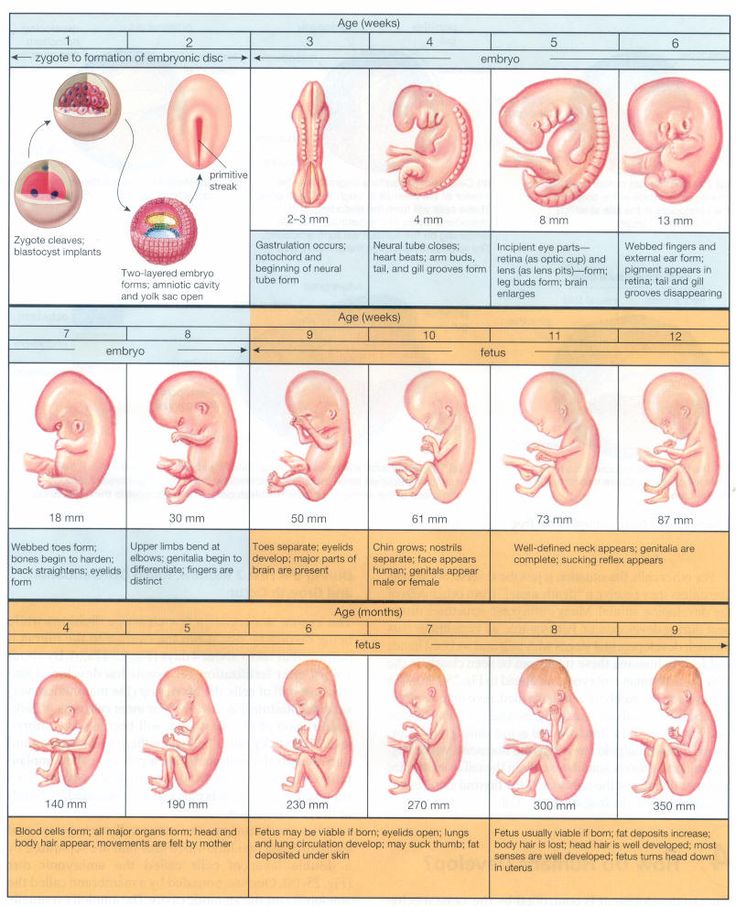
How NAPP is conducted
For manipulation, hospitalization in the maternity hospital is necessary. Preliminarily, an additional examination of the pregnant woman is carried out in the required volume, including ultrasound.
During the NAPP:
Immediately before the start of the manipulation, a CTG is recorded to assess the condition of the fetus.
Drugs are administered to prevent uterine contractions (tocolytics).
Further, under constant ultrasound and KGT control, as well as the continued administration of drugs that relax the uterus, the doctor performs a turn.
Holding both hands on the surface of the pregnant woman's abdomen, one on the head of the fetus, and the other on the buttocks of the fetus, the doctor pushes and rotates the fetus to the upside down position. A pregnant woman may feel some discomfort during the procedure. The degree of discomfort depends on the individual sensitivity of each patient.
The degree of discomfort depends on the individual sensitivity of each patient.
After the procedure is successfully completed, the CTG is recorded again, to make sure that the fetus feels well and has successfully undergone the procedure. Usually during the day, the condition of the mother and fetus is monitored, after which the patient is discharged and continues the pregnancy until spontaneous delivery occurs.
If the doctor notices a deterioration in the condition of the fetus according to the monitoring data, then the procedure is immediately stopped.
If the first attempt was not successful, your doctor may suggest another attempt if the fetus is in good health.
APP is performed ONLY in a maternity ward where there is an opportunity for an emergency delivery, if necessary.
Risks associated with NAPP
Subject to constant monitoring of the condition of the fetus, constant tocolysis (administration of drugs that relax the uterus) The risks associated with this procedure are minimal. Complications from its use occur in less than 1-2% of cases.
Complications from its use occur in less than 1-2% of cases.
Complications of NAPP include:
- compression or "twisting" of the umbilical cord. In this case, constant monitoring of the condition of the fetus allows you to immediately fix its deterioration and stop the procedure.
- discharge of amniotic fluid or the development of labor. This complication can be considered relative, since the rotation in most cases is carried out at full-term pregnancy.
Any deviation from the normal course of the procedure serves as a reason to stop the manipulation and decide on the choice of further management tactics.
Carrying out NAPP with Rh-negative mother's blood.
The presence of Rh isoimmunization (that is, the presence of anti-Rh antibodies in the mother's blood) is a contraindication to this procedure, as it increases the risk of anemia in the fetus.
In the absence of isoimmunization (absence of anti-Rhesus antibodies) it is possible to carry out NAPP with prophylaxis by introducing anti-Rhesus immunoglobulin.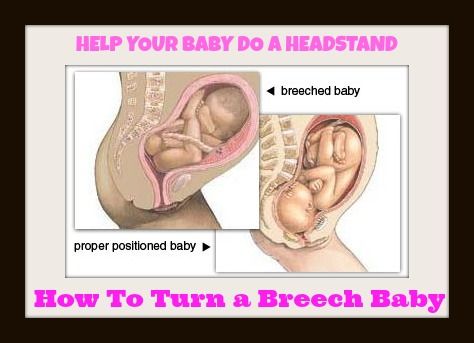
If you have a breech presentation of the fetus and you want to know about further options for pregnancy management, delivery, external obstetric rotation of the fetus on the head, the presence of indications and contraindications for its implementation, please consult our specialists.
harbingers of labor in multiparous and primiparas, what happens, fetal movement, baby's weight, ultrasound
What happens to the baby during this period?
Now the baby's weight is 3000-3200 g. Sometimes a mother can feel in the abdomen not only the fetus moving, but also rhythmic tremors - this is the baby hiccups, swallowing amniotic fluid. It is believed that hiccups are a kind of training before the start of spontaneous breathing. By this time, the baby has already taken its final position in the uterine cavity - head down, towards the exit from the uterus.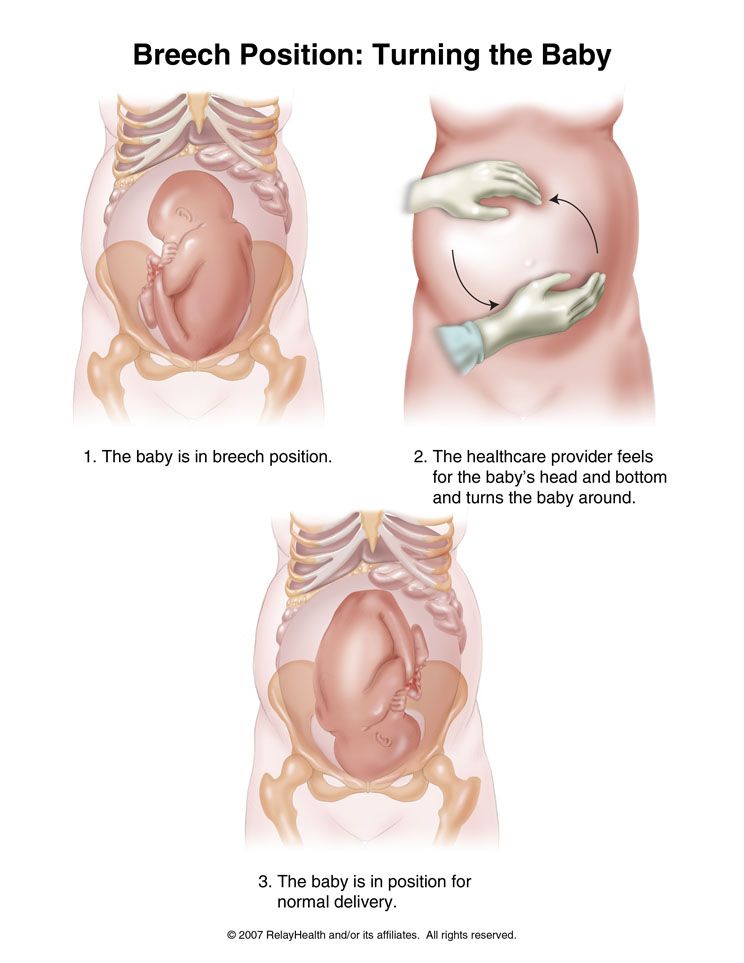 The obstetrician determines the presentation of the fetus by probing the abdomen of the expectant mother. But sometimes doctors detect breech presentation, in this case, an examination is performed, ultrasound is performed and the tactics of childbirth are determined.
The obstetrician determines the presentation of the fetus by probing the abdomen of the expectant mother. But sometimes doctors detect breech presentation, in this case, an examination is performed, ultrasound is performed and the tactics of childbirth are determined.
Index
Norm
Weight gain of the mother
From 8.6 (with initial excess weight) to 14.5 kg (with initial weight deficit), average gain 10-12 kg
Fundal height03
35-38 cm
Fetal weight
3000-3200 g
Fetal height
48-52 cm
Important!
During the 38th week of pregnancy, the body of the expectant mother is actively preparing for the upcoming birth. It is important to know in advance, read the necessary information about this process (if you have not already done so) in order to clarify how to behave with the onset of contractions.
The first harbingers of childbirth appear in multiparous and primiparas. These are body changes, certain processes that set up the body and reproductive system for the birth of a child.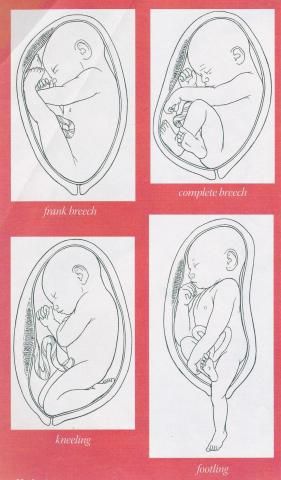 The signs differ slightly depending on whether the mother is expecting her first baby or if this is her second and subsequent pregnancies.
The signs differ slightly depending on whether the mother is expecting her first baby or if this is her second and subsequent pregnancies.
Many mothers are afraid to miss or not recognize these important "calls". Don't worry about that - we've put together a handy labor checklist to help you figure out when it's time to go to the hospital.
During this period, drops of a yellowish-whitish liquid - colostrum - can periodically be released from the nipples of the breast. So the mammary glands prepare for childbirth and subsequent feeding of the baby. In order not to stain the linen, you can use special absorbent pads for the chest. They are sold in pharmacies and children's stores, they are a small circle of absorbent materials that is inserted into a bra. If colostrum is absent, this is not a sign of pathology. In some women, the work of the mammary glands starts only after the birth of the crumbs.
Harbingers of childbirth in women who are expecting their first child
One of the first signs that labor is coming is easier breathing due to the fact that the stomach has dropped. This feeling is not always so vivid that the pregnant woman herself notices it, sometimes others focus on it. Although the child is also actively moving, the mother's shortness of breath decreases, breathing becomes easier, heartburn and mild nausea after eating less often occur or completely disappear. But due to the fact that the fetal head sank lower into the small pelvis, the uterus is increasingly in good shape, urination becomes more frequent due to pressure on the bladder.
This feeling is not always so vivid that the pregnant woman herself notices it, sometimes others focus on it. Although the child is also actively moving, the mother's shortness of breath decreases, breathing becomes easier, heartburn and mild nausea after eating less often occur or completely disappear. But due to the fact that the fetal head sank lower into the small pelvis, the uterus is increasingly in good shape, urination becomes more frequent due to pressure on the bladder.
Sometimes the mother-to-be suddenly notices that the child is not moving much, his movements are not so sharp and active, he seems to calm down. This is a completely natural process, since every day there is less and less space inside the uterine cavity, the walls of its temporary “house” put more and more pressure on the arms and legs, tightly cover, and the amniotic fluid becomes a little less.
If the baby began to move less, he is also preparing for childbirth, gaining strength, but if for 10-12 hours you have not felt a single push or movement, it is better to consult a doctor. He will check if everything is fine with the baby.
He will check if everything is fine with the baby.
Important!
If the mother feels the fetal movement is too active, a doctor's consultation is necessary. This is necessary to make sure that the baby does not have oxygen starvation, and the volume of amniotic fluid is normal.
If at earlier times the fetal movements were felt as various movements, pushes, kicks and even somersaults, then by this time it is more and more often pandiculation or slight movements. The baby already has little space, sometimes his movements are very noticeable - the woman notes that she is pulling her stomach in the area where the fetal activity is felt.
Preparing the body for childbirth
The 38th week of pregnancy is a period of active restructuring of the body. Under the influence of hormones, the body prepares for hard work: there is pain in the lower back, pulling the lower abdomen, there is an ache in the area of the pubic joint (the place where the pelvic bones are closed). The lower abdomen hurts due to the descent of the fetal head and its tight fit to the pelvic bones, the occurrence of more and more frequent training uterine contractions and the gradual loosening of the ligaments. Sometimes there is a feeling that the stomach is turning to stone - this is the tone of the uterus, muscle training for subsequent contractions. If these contractions are irregular, occur occasionally, they are not intense, you just need to lie on your side, rest, and they pass. If the same time passes between contractions, they become more and more sensitive, the interval is reduced - this is the beginning of labor, it's time to go to the maternity hospital.
The lower abdomen hurts due to the descent of the fetal head and its tight fit to the pelvic bones, the occurrence of more and more frequent training uterine contractions and the gradual loosening of the ligaments. Sometimes there is a feeling that the stomach is turning to stone - this is the tone of the uterus, muscle training for subsequent contractions. If these contractions are irregular, occur occasionally, they are not intense, you just need to lie on your side, rest, and they pass. If the same time passes between contractions, they become more and more sensitive, the interval is reduced - this is the beginning of labor, it's time to go to the maternity hospital.
There is one easy way to tell if contractions are false or true. You just need to count the number of contractions and the interval between them. Use a stopwatch on your smartphone, noting how long the contraction of the uterus lasts and how long the period of relaxation, rest, will then be. If the contractions of the uterus gradually increase, intensify, and the time intervals between them gradually decrease, this is a sign of the onset of labor.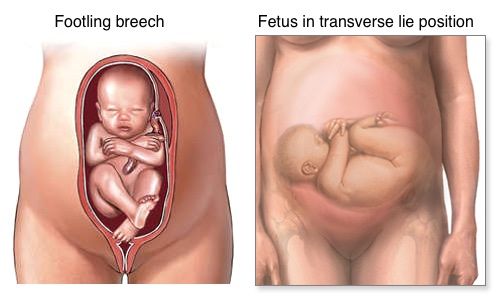 Then it was time to go to the maternity hospital.
Then it was time to go to the maternity hospital.
Mucous discharge from the genital tract may occur during the 38th week. By the nature of the discharge, they look like lumps of dense transparent or whitish mucus with streaks of blood without any smell. This is the discharge of the mucous plug, which closed the cervix and prevented the penetration of pathogenic bacteria to the fetal membranes. The cervix gradually softens, opens slightly and the mucus gradually leaves.
Good to know
In nulliparous women, the harbingers of imminent labor may appear approximately one to two weeks before the onset of labor. It's about 38 or 39th weeks of pregnancy.
In some cases, the mother-to-be may have loose stools at 38 weeks of gestation, although no changes in the woman's diet have occurred. This is an acceptable bowel reaction to changing hormone levels and preparing the body for childbirth. The intestines are gradually cleared of the contents. However, not always different sensations and changes in the work of digestion are explained precisely by prenatal changes.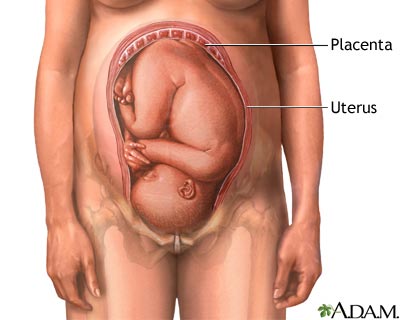 Diarrhea at this gestational age may also be the result of nutritional errors, food poisoning, or other influences.
Diarrhea at this gestational age may also be the result of nutritional errors, food poisoning, or other influences.
A particularly alarming situation is when nausea and even vomiting occur against the background of diarrhea. In this case, you should immediately consult a doctor.
Harbingers of childbirth when expecting a second and subsequent children
If this is not the first pregnancy and childbirth for a woman, and the family is expecting a second, third baby, then the birth may come a little earlier. The body already knows what will happen and it takes less time for the preparatory phase. Thus, the appearance of the crumbs into the world can be expected in the period from the beginning of the 38th week of pregnancy. The processes themselves, which are associated with the preparation for childbirth, may not be so pronounced, sometimes they are absent or appear just a couple of days before the baby is born.
So, with repeated pregnancy, there may not be a pronounced and significant lowering of the abdomen.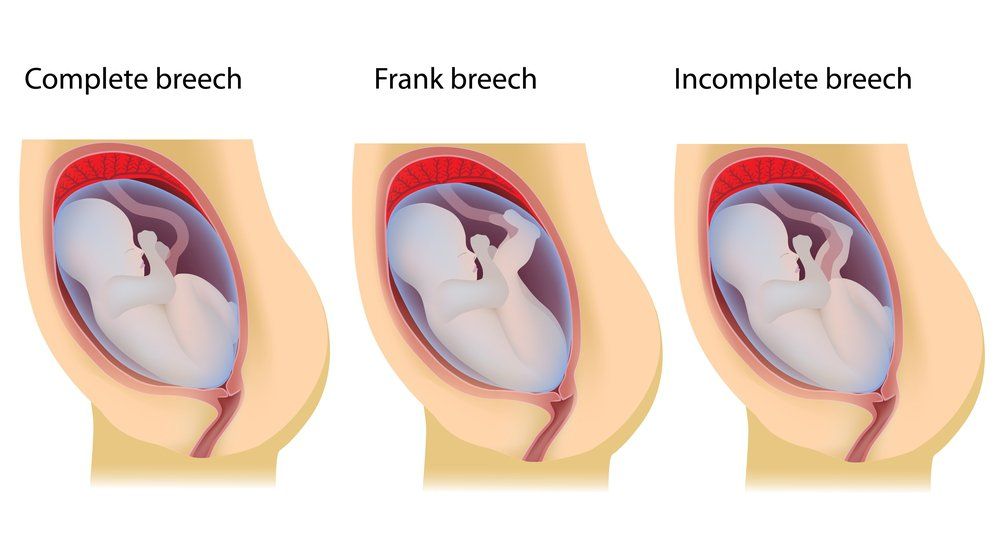 Often, the baby is initially located lower than during the first pregnancy, or the cervix relaxes just before the onset of childbirth. Then the woman feels that it has become easier to breathe, the pressure on the bladder has increased.
Often, the baby is initially located lower than during the first pregnancy, or the cervix relaxes just before the onset of childbirth. Then the woman feels that it has become easier to breathe, the pressure on the bladder has increased.
Important!
It is worth emphasizing that in multiparous mothers, the harbingers of childbirth may be completely absent. The birth process can begin suddenly, and the contractions will be stronger, the duration of labor will be shorter. Therefore, by the time of 38 weeks, you need to collect everything you need to go to the maternity hospital, all the necessary things and documents should be in an accessible place.
Childbirth is unique, it takes place differently in women, and even in the same woman childbirth is different. If this is the third birth or the fourth, often the precursors can be barely perceptible or completely absent. And the birth act itself proceeds quite quickly and sometimes even a little earlier than the date of birth, which is determined by the doctor. But, as for the second birth, this fact is not a strict pattern, childbirth is possible almost the same day with a pre-calculated date.
But, as for the second birth, this fact is not a strict pattern, childbirth is possible almost the same day with a pre-calculated date.
In any case, by the 38th week of pregnancy, it is necessary to collect everything necessary for a trip to the maternity hospital and, at the first contractions, immediately seek medical help.
Is it worth it to speed up labor at this time?
Many women experience fatigue towards the end of their pregnancy and want to have a baby as soon as possible. Therefore, they ask one question - how to speed up the onset of childbirth, is it possible to stimulate this process in order to meet the baby faster and return home, accept congratulations and raise the baby. But you don't need to think about inducing labor before the full term of 40 weeks. Although by the 38th week the baby is already full-term, he is still gaining weight, continues to develop, and nature knows better when he needs to be born.
- 1. Normal pregnancy (clinical recommendations) // Obstetrics and Gynecology: News.