Can you use miconazole while pregnant
Answers to 6 burning questions about yeast infection during pregnancy | Your Pregnancy Matters
×
What can we help you find?Refine your search: Find a Doctor Search Conditions & Treatments Find a Location
Appointment New Patient Appointment
or Call214-645-8300
MedBlog
Your Pregnancy Matters
September 20, 2022
Your Pregnancy Matters
Robyn Horsager-Boehrer, M. D. Obstetrics and Gynecology
Vaginal candidiasis, also known as a yeast infection, can be a real pain. The itching, burning, and discharge can be especially worrisome during pregnancy.
In most cases, though, vaginal yeast infections and most treatment options pose minimal risk to the patient or pregnancy.
After bacterial vaginal infections, yeast infections are the second most common cause of vaginal inflammation, and 75% of women will have at least one in their lifetime. Common symptoms can include redness, itching, or irritation on the external genital area (vulva), an increase in white or tan vaginal discharge, and a burning sensation during urination or intercourse.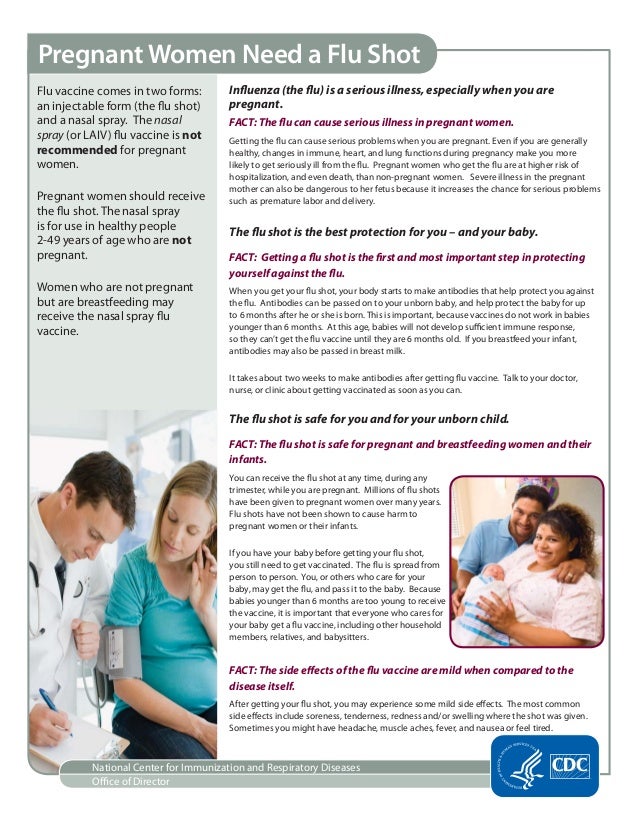
There are a range of over-the-counter and prescription treatments, and an Ob/Gyn or gynecologist can help you choose the safest, most effective option during pregnancy.
I’ve invited Meredith McClure, M.D., a UT Southwestern gynecologist, to answer the top questions pregnant and breastfeeding patients ask about yeast infection treatment and prevention.
Meredith McClure, M.D.Q: How common are yeast infections during pregnancy?
A: Studies have found that 20%-30% of women develop a yeast infection during pregnancy. An increase in the hormone estrogen creates a more hospitable climate for yeast to colonize the vagina because it binds to the protein factor H on the surface of the cells that cause vulvovaginal candidiasis.
Some women are more likely to develop yeast infections due to their genetics. Mutations of several genes can interfere with the immune system’s ability to defend against candida yeast, resulting in recurring infections for some people. This inherited predisposition is called familial candidiasis.
This inherited predisposition is called familial candidiasis.
Q: Can a yeast infection harm my pregnancy?
A: No. A yeast infection won’t affect your developing baby – that’s why we don’t treat yeast infections that don’t have symptoms. However, most symptomatic yeast infections get worse when left untreated. This means more itching, redness, and inflammation. If the skin becomes cracked or torn from repeated scratching, a skin infection can result. In rare cases, an untreated yeast infection can lead to fatigue, oral thrush, or digestive problems.
Q: Do yeast infections appear throughout pregnancy?
A: Yeast infections can occur any time, but they are most common during the second trimester. Talk with your doctor if you notice signs of a yeast infection while pregnant, even if you have had one before. Some more serious infections have similar symptoms, so your doctor will perform a simple fungal culture swap in the office to check for the presence of yeast.
Q: What treatment options are available?
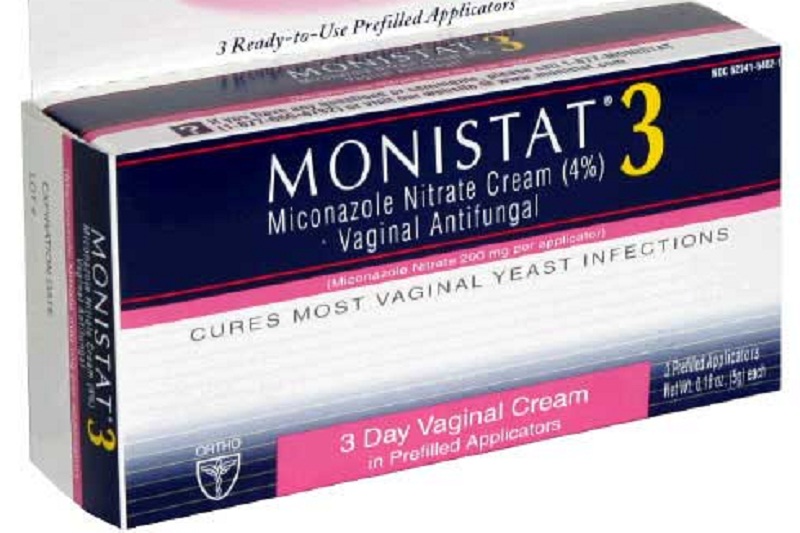
Talk with your doctor about the safest and most effective options for treating yeast infections during pregnancy.A: Topical creams or vaginal suppositories are the recommended yeast infection treatment options during pregnancy or while breastfeeding. Over-the-counter medications such as Miconazole, Clotrimazole, and Terconazole have been shown to eliminate a yeast infection safely and effectively. They are usually applied for three to seven days. It is important to finish the entire course of medication to prevent the infection from coming back. Studies have demonstrated these medications are safe to use during pregnancy.
The oral medication Diflucan (fluconazole) is not recommended for most patients during pregnancy. Though taking a single pill is simpler, quicker, and less messy, some studies suggest fluconazole carries a slightly increased risk of miscarriage, birth defects, or stillbirth, especially at high doses taken over long periods of time.
While the increase is small – approximately 12 incidents per 10,000 births – the convenience of single-pill treatment might not outweigh the risk. However, in the event you have already taken or need to take fluconazole while pregnant, the additional risk at a normal dose is unlikely to pose any problems for your baby.
Q: Are yeast infection treatments safe while breastfeeding?
A: Yeast infections are less common among breastfeeding patients because estrogen levels drop dramatically in the postpartum period, making it hard for yeast to thrive. But if they occur, fluconazole may be taken by women who are breastfeeding as the levels secreted into breast milk are small.
It is possible for a breastfeeding mother and baby to pass thrush, a fungal infection that typically grows in the mouth and throat, back and forth between nipple and mouth. If that happens, both must be treated to stop the infection. Thrush is usually minor and is often caused by the same fungus – and treated with a 7- to 14-day course of the same antifungal medicines – as a yeast infection in the vagina.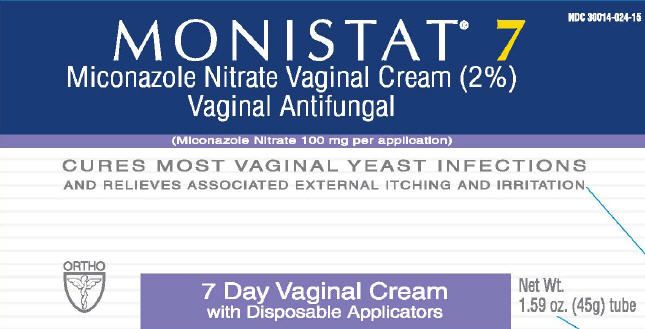
Q: What steps can reduce the risk of yeast infection?
A: During pregnancy and otherwise, take the following precautions:
- Wipe front to back after using the toilet.
- Avoid using scented tampons, pads, and pantyliners.
- Change tampons, pads, and pantyliners often.
- Avoid very hot baths and hot tubs.
- Wear underwear with a cotton lining to promote airflow.
- Do not douche, which removes healthy vaginal bacteria that prevent infection.
- Wear loose fitting clothing.
- Manage your blood sugar if you have diabetes or gestational diabetes.
- Remove wet workout clothes and swimsuits as soon as possible after activities.
If you’re pregnant and notice signs of a yeast infection, discuss treatment options with your doctor so you can eliminate these disruptive symptoms. To request an appointment, call 214-645-8300 or request online.
More in: Your Pregnancy Matters
Pediatrics; Your Pregnancy Matters
- Jessica Morse, M.
 D.
D.
December 6, 2022
Your Pregnancy Matters
- Shivani Patel, M.D.
November 22, 2022
Your Pregnancy Matters
- Robyn Horsager-Boehrer, M.D.
November 15, 2022
Your Pregnancy Matters
- Robyn Horsager-Boehrer, M.
 D.
D.
November 7, 2022
Mental Health; Your Pregnancy Matters
- Robyn Horsager-Boehrer, M.D.
October 11, 2022
Prevention; Your Pregnancy Matters
- Robyn Horsager-Boehrer, M.
 D.
D.
October 4, 2022
Mental Health; Your Pregnancy Matters
- Meitra Doty, M.D.
September 27, 2022
Men's Health; Women's Health; Your Pregnancy Matters
- Yair Lotan, M.
 D.
D.
September 6, 2022
Your Pregnancy Matters
August 29, 2022
More Articles
Yeast Infections During Pregnancy: What To Do
Written by Camille Peri
Reviewed by Dan Brennan, MD on August 09, 2022
In this Article
- What is a Yeast Infection During Pregnancy?
- Symptoms of a Yeast Infection During Pregnancy
- Causes of a Yeast Infection During Pregnancy
- Treating a Yeast Infection During Pregnancy
- Preventing a Yeast Infection During Pregnancy:
What is a Yeast Infection During Pregnancy?
Yeast infections (also known as candidiasis) are common in women, especially when you're pregnant. Increased estrogen in your pregnant body can throw off the normal balance of yeast and bacteria in your vagina. This may let the yeast overgrow. Most yeast infections during pregnancy result from the fungus candida albicans. Two other kinds of yeast that can also cause them are candida glabrata and candida tropicalis.
Increased estrogen in your pregnant body can throw off the normal balance of yeast and bacteria in your vagina. This may let the yeast overgrow. Most yeast infections during pregnancy result from the fungus candida albicans. Two other kinds of yeast that can also cause them are candida glabrata and candida tropicalis.
Yeast infections aren't pleasant, but they won't hurt you or your baby. And they can be safely treated, usually with a topical cream.
Symptoms of a Yeast Infection During Pregnancy
You might notice:
- Itching
- Burning
- Redness or swelling in your vulva, the area outside your vagina.
- Thick, white vaginal discharge that looks like cottage cheese.
Causes of a Yeast Infection During Pregnancy
- Taking antibiotics, which can cause that can change the balance of yeast and bacteria in your vagina.
- Diabetes that isn’t well controlled
- Conditions like HIV or medications, like corticosteroids that make it harder for your immune system to work well.
- If your sexual partner has a yeast infection, it can be passed to you during vaginal sex.
Treating a Yeast Infection During Pregnancy
It's safe to treat a yeast infection with over-the-counter (OTC) vaginal creams or suppositories that contain miconazole or clotrimazole.
Don’t take an oral fluconazole tablet to treat a yeast infection during pregnancy. It may cause birth defects.
If you think you have a yeast infection, call your doctor before using over-the-counter medications to treat it.
Preventing a Yeast Infection During Pregnancy:
- Wear cotton underwear and pantyhose with a cotton crotch to keep your vaginal area dry and let it "breathe."
- Always wipe from front to back after you go to the bathroom.
- Don't douche. It can upset the balance in your vagina. In late pregnancy, it may also cause your water to break.
- Avoid tight pants and pantyhose.
- Change out of a wet swimsuit or sweats immediately.
 This keeps the genital area dry.
This keeps the genital area dry. - Avoid toilet paper, feminine sprays, bubble bath, and sanitary pads that are scented.
- Keep good control of your blood sugar if you have diabetes.
- Eat yogurt with live cultures; some research suggests this can help.
| 📜 Instructions for use Mikozon ® 💊 Composition of the drug Mikozon ® ✅ Application of the drug Mikozon ® 📅 Storage conditions Mycoson ® ⏳ The shelf life of mycoson ® Save Search for analogues Description of the drug Mycosone ® (Micoson) Based on the approved prescribing information and prepared for the electronic edition of the Vidal 2014 handbook, last updated: 2021. Marketing authorization holder:AGIO PHARMACEUTICALS, Ltd. (India) ATX code: D01AC02 (Miconazole) Active substance: miconazole (miconazole) Rec.INN WHO registered Dosage form
Release form, packaging and composition preparation Mikozon®Cream for external use white or almost white, homogeneous, with a specific odor, not containing foreign particles.
Miconazole during pregnancy and lactation - Medum. ru Active substance ru Active substance Pay attention : the use of any medicines, including those containing the active substance miconazole, when planning and during periods of pregnancy, lactation (breastfeeding) must be agreed with the attending physician. Women of reproductive potential are encouraged to get tested for pregnancy. Use in pregnancyFDA fetal category C. There are no adequate and well-controlled studies on the safety of miconazole during pregnancy. Animal studies showed no evidence of embryotoxicity, fetotoxicity or teratogenicity during intravenous studies. The use of miconazole in pregnant women is contraindicated, unless absolutely necessary, when the expected benefit to the mother outweighs the potential risk to the fetus. During pregnancy, vaginal use of the drug (vaginal suppositories, capsules) is possible only in the first trimester. Use during breastfeedingSpecial studies on the safety of miconazole during breastfeeding have not been conducted. There are no data on the excretion of miconazole in breast milk. A risk to the infant cannot be ruled out. The decision to continue/stop breastfeeding or continue/stop miconazole therapy should be made taking into account the benefits of breastfeeding for the baby and the benefits of miconazole treatment for the mother. Important additional information
See more detailed information about the active substance Miconazole:
Didn't find what you were looking for? If you need to know more about the active ingredient Miconazole - ask your question. |
 06.06
06.06  10.19
10.19