How common is whooping cough in babies
Whooping Cough is Deadly for Babies
Whooping cough is a very contagious disease that can be deadly for babies. It spreads from person to person, usually by coughing or sneezing while in close contact with others.
Your baby could be at risk for getting whooping cough
People used to think of whooping cough as a disease of the past, but it’s still common in the U.S. Learn why reported cases of whooping cough are increasing.
Since 2010, CDC sees between 10,000 and 50,000 cases of whooping cough each year in the United States. In fact, there are cases reported in every state. 2012 was a record year with more than 48,000 cases, the most cases that CDC has seen in the past 60 years. Most of the deaths each year are in babies younger than 3 months of age. Since 2010, up to 20 babies die from it each year in the United States.
Even though it seems like these are a lot of cases, the United States no longer has the 200,000 cases per year like it did before whooping cough vaccines were available.
Even healthy babies get whooping cough
In the first 6 months of life, babies are at high risk for complications from whooping cough, even if they are healthy. This is because their immune systems are still developing. In fact, babies younger than 2 months of age only have the antibodies they get from their mother to help protect them. It is important for you to get the whooping cough vaccine during each pregnancy. This allows you to transfer the greatest number of protective antibodies to each of your babies.
Whooping cough can be serious for you, your baby, and your family
Whooping cough can cause serious and sometimes life-threatening complications in babies. This is especially true within the first 6 months of life. It is important to know that many babies with whooping cough don’t cough at all. Instead it causes them to stop breathing and turn blue. About half of babies who get whooping cough end up in the hospital. The younger the baby is when she gets whooping cough, the more likely it is that doctors will need to treat her in the hospital. Of those babies who get treatment for whooping cough in a hospital, about 1 out of 4 will get pneumonia and 1 or 2 out of 100 will die. Other complications include violent, uncontrolled shaking, life-threatening pauses in breathing, and brain disease.
Of those babies who get treatment for whooping cough in a hospital, about 1 out of 4 will get pneumonia and 1 or 2 out of 100 will die. Other complications include violent, uncontrolled shaking, life-threatening pauses in breathing, and brain disease.
View photos of a baby being treated for whooping cough.
Adolescents and adults can also have complications from whooping cough. They are usually less serious in this age group, especially in those who got vaccines against whooping cough. The cough itself often causes common complications in adolescents and adults, including loss of bladder control, fainting, and rib fractures.
View videos of a child and an adult with whooping cough.
Antibiotics are used to treat whooping cough
Doctors generally treat whooping cough with antibiotics (medications that help treat diseases caused by bacteria). Learn why early treatment is so important and get tips for caring for your baby.
Your doctor or local health department may recommend preventive antibiotics to close contacts of a whooping cough patient, including all household members. This might prevent or reduce the chance of getting whooping cough.
This might prevent or reduce the chance of getting whooping cough.
Whooping Cough: What Parents Need to Know
Pertussis, or whooping cough, is caused by bacteria that attack the lining of the breathing passages. Severe coughing is one of the major symptoms.
Because a child is short of breath, they inhale deeply and quickly between coughs. The breaths often make a "whooping" sounds, which is how this illness got its common name. The intense coughing scatters the pertussis bacteria into the air, and can spread the disease to others.
Pertussis on the rise
Many years ago, there were several hundred thousand cases of whooping cough each year in the United States. With the development of a vaccine for pertussis, that number dropped. But in recent years, U.S. cases have gone up. Because of this, giving the pertussis vaccine to children and their caregivers is more important than ever.
Infants under one year of age are at greatest risk of developing severe breathing problems and life-threatening illness from whooping cough.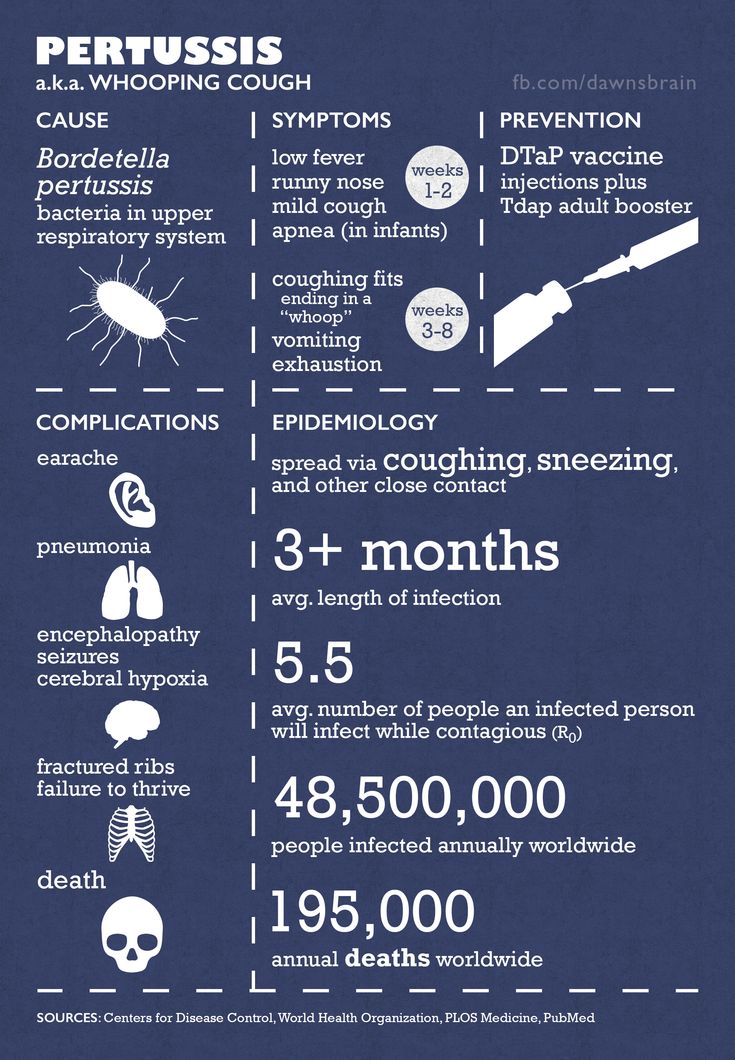
Symptoms of pertussis
Pertussis often acts like a common cold for a week or two. Then the cough gets worse (rather than better, as usually happens with a cold), and older children may start to have the characteristic "whoop." During this phase, which can last two weeks or more, your child may often be short of breath. They may look bluish around the mouth. In addition, they may tear, drool, and vomit.
Young infants with pertussis may have episodes where they appear to stop breathing or have vomiting after a long bout of coughs. Infants with pertussis become exhausted and develop complications, becoming more vulnerable to other infections, pneumonia, and seizures. Pertussis can be fatal in some infants, but the usual course is for recovery to begin after two to four more weeks.
The cough of pertussis, which has also been called the "100 day cough," may not disappear for months, and may return with future respiratory infections.
When to call the pediatrician
Pertussis infection starts out acting like a cold.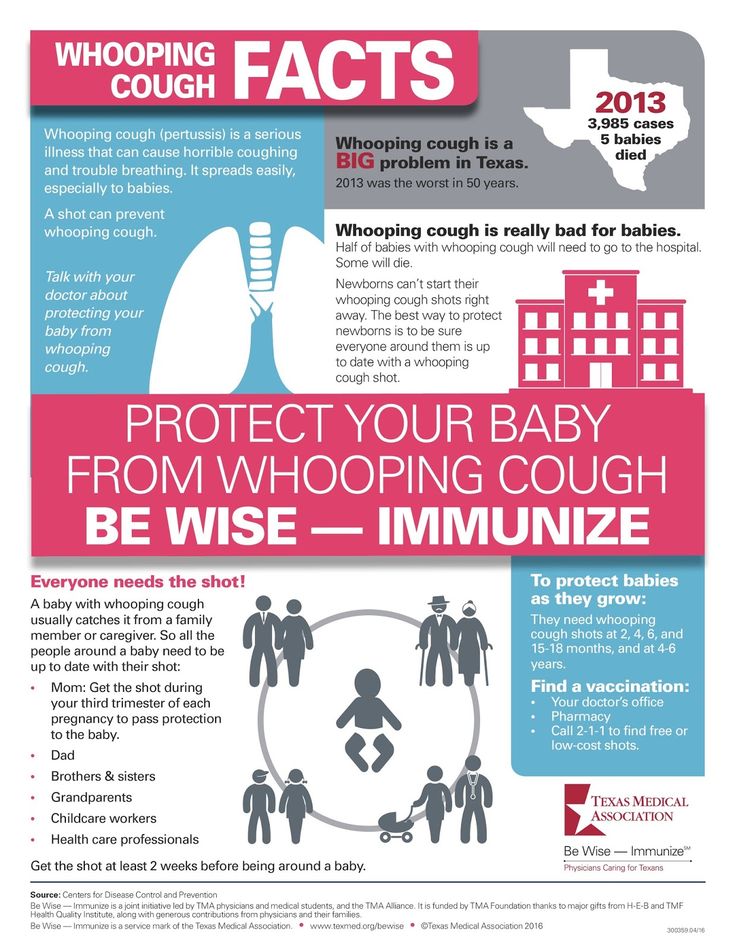 You should consider the possibility of whooping cough if:
You should consider the possibility of whooping cough if:
Your child is a very young infant who has not been fully immunized and/or has had exposure to someone with a chronic cough or the disease.
Their cough becomes more severe and frequent, or their lips and fingertips become dark or blue.
They become exhausted after coughing episodes, eat poorly, vomit after coughing, and look "sick."
When your child needs hospital care
Most infants who are less than six months old with whooping cough need to be initially treated in the hospital. Slightly less than half of older babies with the disease are initially treated in the hospital, too. This more intensive care can decrease the chances of complications. These complications can include pneumonia, which occurs in slightly less than one fourth of children under one year old who have whooping cough. If your child is older, they are more likely to be treated only at home.
While in the hospital, your child may need to have the thick respiratory secretions suctioned.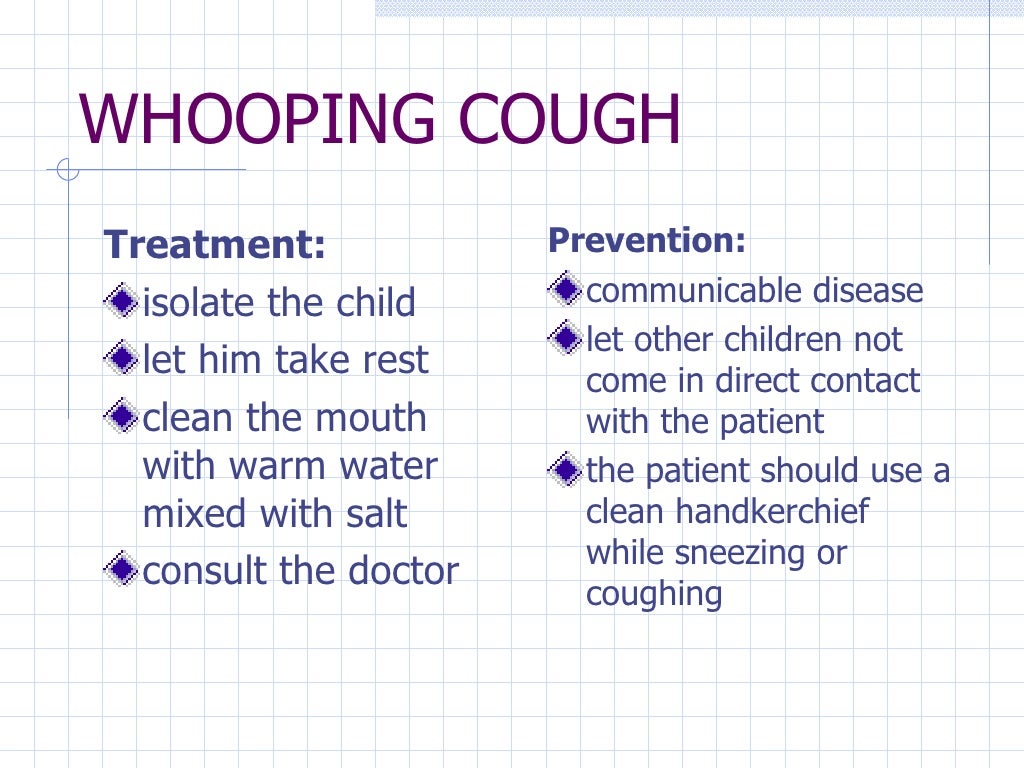 Their breathing will be monitored, and they may need to be given oxygen. Your child will be isolated from other patients to keep the infection from spreading to them.
Their breathing will be monitored, and they may need to be given oxygen. Your child will be isolated from other patients to keep the infection from spreading to them.
Treatment for pertussis
Whooping cough is treated with an antibiotic that is most effective when given in the first stage of illness, before the coughing spells begin. Although antibiotics can stop the spread of the whooping cough infection, they cannot prevent or treat the cough itself. Because cough medicines do not relieve the coughing spells, your pediatrician probably will recommend other forms of home treatment to help manage the cough.
Let your child rest in bed and use a cool-mist vaporizer to help soothe their irritated lungs and breathing passages. A vaporizer also will help loosen secretions in the respiratory tract.
Ask your pediatrician for instructions on the best position for your child to help drain those secretions and improve breathing. Also ask whether antibiotics or vaccine boosters need to be given to others in your household to prevent them from developing the disease.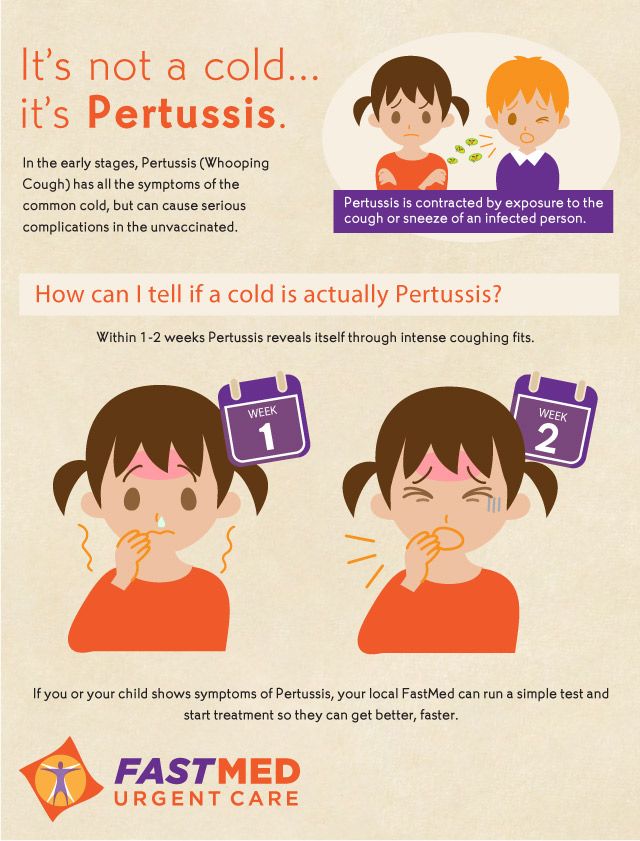 Your child should stay home from child care until finishing five days of antibiotics.
Your child should stay home from child care until finishing five days of antibiotics.
How to protect your baby against pertussis
The best way to protect your child against pertussis is with DTaP vaccination (immunizations at two months, four months, and six months of age, and booster shots at twelve to eighteen months and at four or five years of age or prior to starting school). See Recommended Immunization Schedules.
Parents or family members who will be in close contact with babies younger than one year old should also receive the Tdap booster. This lowers the risk of passing the infection to the infant.
In addition, all women who are pregnant should get the Tdap vaccine during each pregnancy. This allows mothers to pass on protection against pertussis to their newborns.
The information contained on this Web site should not be used as a substitute for the medical care and advice of your pediatrician. There may be variations in treatment that your pediatrician may recommend based on individual facts and circumstances.
There may be variations in treatment that your pediatrician may recommend based on individual facts and circumstances.
Whooping cough in children - all of a sudden out of nowhere
Whooping cough in children - all of a sudden, out of nowhere.
Whooping cough vaccines for children help control the infection.
Whooping cough is called a vaccine-preventable infection because its occurrence is related to how preventive vaccinations are administered. That is, if all children are vaccinated, then the probability of an outbreak of pertussis infection is practically zero. But when adults begin to refuse to vaccinate children, then the disease is right there.
By the way, doctors start vaccinating against whooping cough for babies from the age of three months. At the same time they are vaccinated against diphtheria and tetanus.
In this case, as a rule, a three-component DTP vaccine is used. Unfortunately, it is the whooping cough component that gives children the most trouble: fever, pain, and malaise. Therefore, sometimes doctors exclude it - an ADS is vaccinated. These are the children, vaccinated by a third, most often get sick with severe forms of whooping cough. In addition, this disease has another unpleasant feature - the lack of a person's innate immunity to it. Therefore, even a newly born child can get sick with whooping cough.
Vulnerability of the nervous system, development of allergies.
The germ that causes whooping cough dies very quickly in the environment. Therefore, it can only be picked up by airborne droplets. But for this you need to communicate quite closely with a sick person. Because even during a cough, the wand does not scatter more than two meters. By the way, it is not the causative agent of the disease that causes the symptoms of whooping cough, but the toxin that it produces.
Moreover, this poison gives a diverse effect. Specifically, it increases the permeability of the brain's defenses against circulating microbes and toxins. This makes the central nervous system vulnerable to dangerous infections. Pertussis toxin also increases the body's production of insulin. This prevents the flow of glucose into the brain and leads to its depletion. And also - increases the body's sensitivity to histamine, which entails the development of allergies.
Symptoms of whooping cough in children the very next day.
After infection with whooping cough, the first symptoms of the disease appear already on the second or third day. First, there is a dry and frequent cough. Sometimes there is also a slight runny nose, a slight increase in body temperature. That is, all the signs of the usual acute respiratory disease or mild bronchitis. Therefore, at first, neither doctors nor parents suspect that the cause of the child's illness is whooping cough.
However, after a while, the cough acquires a pronounced whooping cough character. That is, it usually starts at night, becomes barking and follows attacks. In this case, the patient coughs hoarsely several times without stopping, and then takes a deep breath, which is accompanied by a specific whistling sound. In addition, during an attack, the patient's face often turns red or even blue. And then he coughs up thick mucus or even vomits it. In general, the whooping cough cough is so special that anyone who has heard it once will immediately understand the reason for the child's ailment the second time. Interestingly, in the absence of coughing attacks, a patient with whooping cough feels quite well.
Thus, the severity of the disease is characterized primarily by the frequency and duration of coughing attacks. Moreover, after the peak of the disease, the cough begins to subside. But it lasts for quite a long time - about two months.
Whooping cough is most severe in children under the age of one year.
After coughing attacks, they often stop breathing for a few seconds, or even minutes. This leads to a lack of oxygen, due to which the baby can develop serious complications of the nervous system. And the most dangerous of them are pertussis encephalitis and cerebral hemorrhages, which can turn a child into an invalid. But most often whooping cough is complicated by pneumonia - inflammation of the lungs. Moreover, it is not at all caused by whooping cough, but by other bacteria: staphylococci, streptococci ... Even as a result of an illness, an infant may develop otitis media - inflammation of the middle ear.
Many parents believe that a child with whooping cough should definitely stay at home. However, with whooping cough it is very important how the patient breathes. Especially during the recovery period. After all, dry air provokes an increase in the amount of sputum and its thickening. As a result, it is more difficult to withdraw and clog the bronchi, causing complications.
Therefore, walk with your child more often. Moreover, in the summer it is better to go for a walk in the morning, while it is humid and cool, and also in the evening, when the heat subsides. Just avoid interacting with other children. Better yet, take the child to the grandmother in the village. There, the recovery period will be faster.
Head of the Pediatric Department DPO 72
St. Petersburg City Polyclinic No. 122 Dementieva M.V.
On alert » Medvestnik
In the first half of 2018, the incidence of whooping cough more than doubled compared to the same period last year. We discussed the next cyclic rise in this infection with the head of the department for the prevention of infectious diseases of the Children's Scientific and Clinical Center for Infectious Diseases FMBA Susanna Mikhailovna Kharit .
- Susanna Mikhailovna, what is the situation with the incidence of diphtheria, whooping cough and tetanus in Russia? How does it compare with global statistics?
– Fortunately, today we have practically no diphtheria and tetanus. Although there are still countries where the incidence of both diphtheria and tetanus persists. But if tetanus is a disease that is associated with the earth, with contamination of wounds, then diphtheria can cause epidemic outbreaks.
Although there are still countries where the incidence of both diphtheria and tetanus persists. But if tetanus is a disease that is associated with the earth, with contamination of wounds, then diphtheria can cause epidemic outbreaks.
As for whooping cough, it is a worldwide problem. Indeed, now there is a lot of this infection in different countries. The incidence in our country ranges from 4 to 6 per 100 thousand annually. It seems to be a small figure, but this is a general incidence. In children, of course, the incidence is many times higher, and the bulk of the diseased, approximately 93-95%, in different years in different ways, are children. And among them the leading role is played by small children. They are the most seriously ill and most often end up in a hospital, the infection often occurs with complications. In recent years, the system for detecting the disease has changed, and we began to talk about other age groups. It turned out that almost the same as small children, preschoolers and school-age children get sick.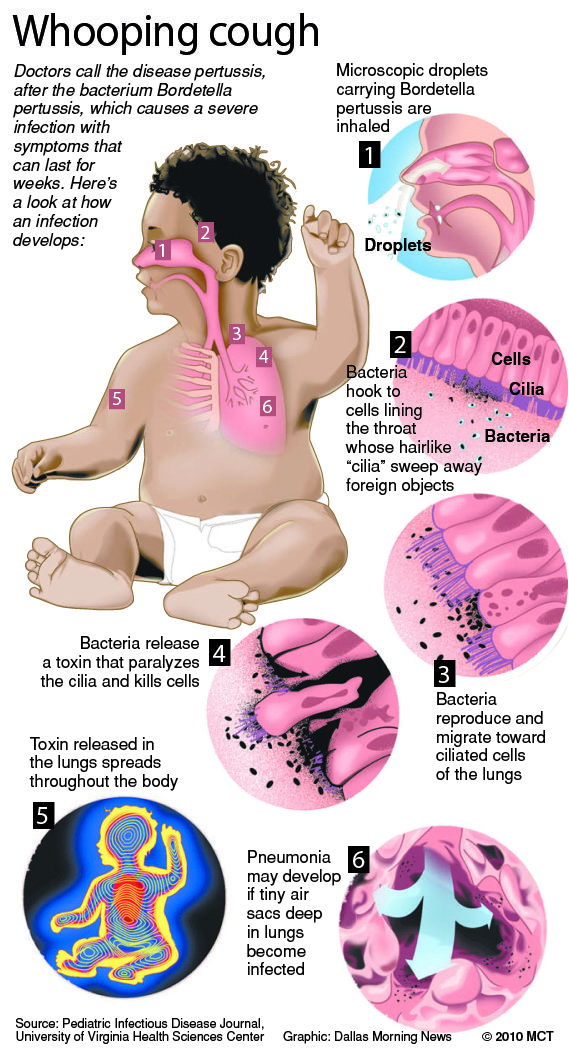
– What are the features of the course of infections (diphtheria, whooping cough, tetanus) at the present stage?
- Unfortunately, these three infections are just as dangerous, just as severe as in the old days. Let's start with diphtheria, young parents often refuse vaccinations because they simply do not understand how dangerous it is. Diphtheria in unvaccinated people is a deadly disease.
I also caught a diphtheria epidemic in our country at 90 years. Unvaccinated children died. Our parents were on their knees in front of the intensive care unit, praying that their children would be alive. Therefore, this terrible disease, which until now, if a person is not vaccinated, can lead to death in almost 20% of cases, gives severe complications.
The basis of this infection is not the germ itself, which can be killed with antibiotics, but the toxin that it produces. And when the microbe enters the nasopharynx, literally in the first 2-3 days it already produces this toxin.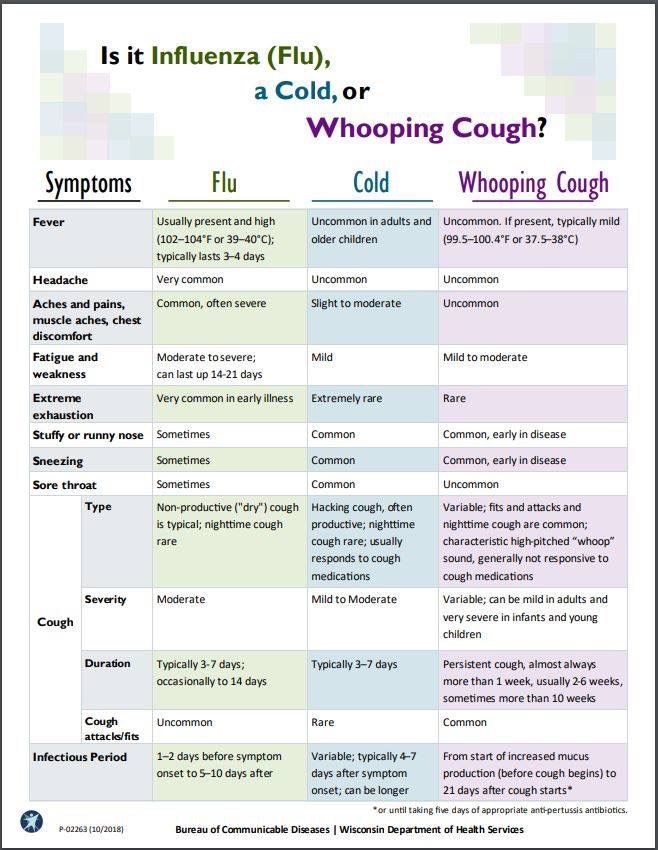 In turn, the toxin is absorbed into the blood and affects all our organs: primarily the heart, kidneys and nervous system. And now it is already very difficult to cope with this, to remove this toxin, which has already contacted the tissues. Therefore, unfortunately, the treatment remains a hundred years old, we cannot think of anything else. And the only means of prevention is vaccination.
In turn, the toxin is absorbed into the blood and affects all our organs: primarily the heart, kidneys and nervous system. And now it is already very difficult to cope with this, to remove this toxin, which has already contacted the tissues. Therefore, unfortunately, the treatment remains a hundred years old, we cannot think of anything else. And the only means of prevention is vaccination.
Speaking of tetanus, a few years ago at a conference, representatives from one region spoke about a case of tetanus in a 7-year-old girl who died. The child was given a medical exemption from vaccinations all the time, because something happened to her in the first year of life, some kind of perinatal encephalopathy was found, then the parents, frightened by vaccinations, did not vaccinate the child, the child developed normally, went to kindergarten, went to school . And she was riding a scooter and fell and hurt her leg, slightly, while she also got into a fight with a neighbor. And when she had neurological manifestations, they decided that it was a brain injury due to this fight.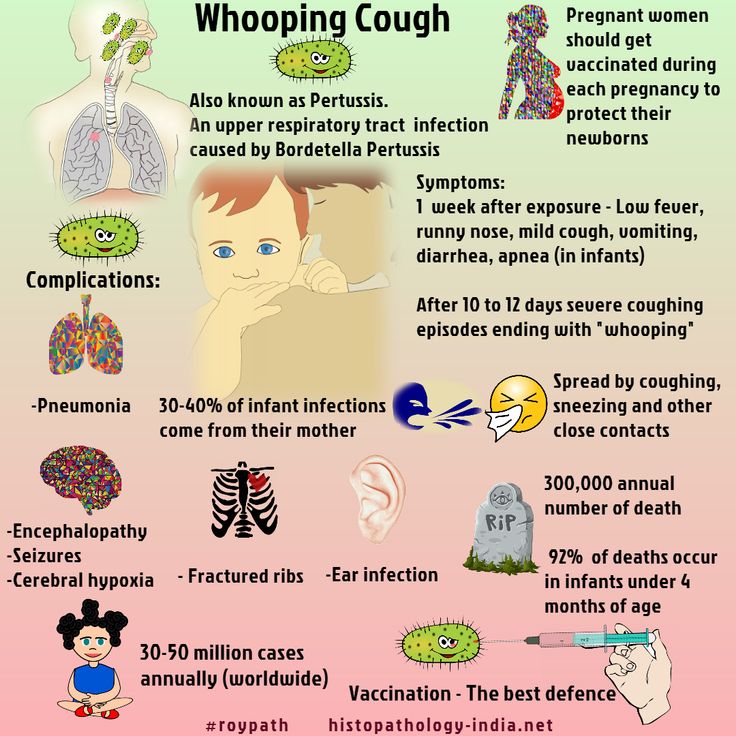 And only when the child stood in an arc, it became clear that it was tetanus. And treatment at this time is completely useless. It's so easy because of some nonsense you can lose your only beloved child.
And only when the child stood in an arc, it became clear that it was tetanus. And treatment at this time is completely useless. It's so easy because of some nonsense you can lose your only beloved child.
Finally, the third infection you asked about is whooping cough. The disease begins as if it were an acute respiratory disease. Cough, runny nose, low temperature, about 7-10 days, the child begins to cough more and a completely specific paroxysmal cough appears, that is, bouts of growing cough, then the breath is heavy, because he could not inhale, with a whistle due to the fact that that the glottis is narrowed, is called a reprise, and coughs again. In this case, there may be hemorrhages in the sclera, because the person is tense, small hemorrhages appear on the face. All this is really a very severe and clearly expressed clinical picture. At the same time, they cough day and night, and even more at night. It lasts for about 3-4 weeks, then it goes away, but if a person gets sick for six months, such an attack of coughing can resume again.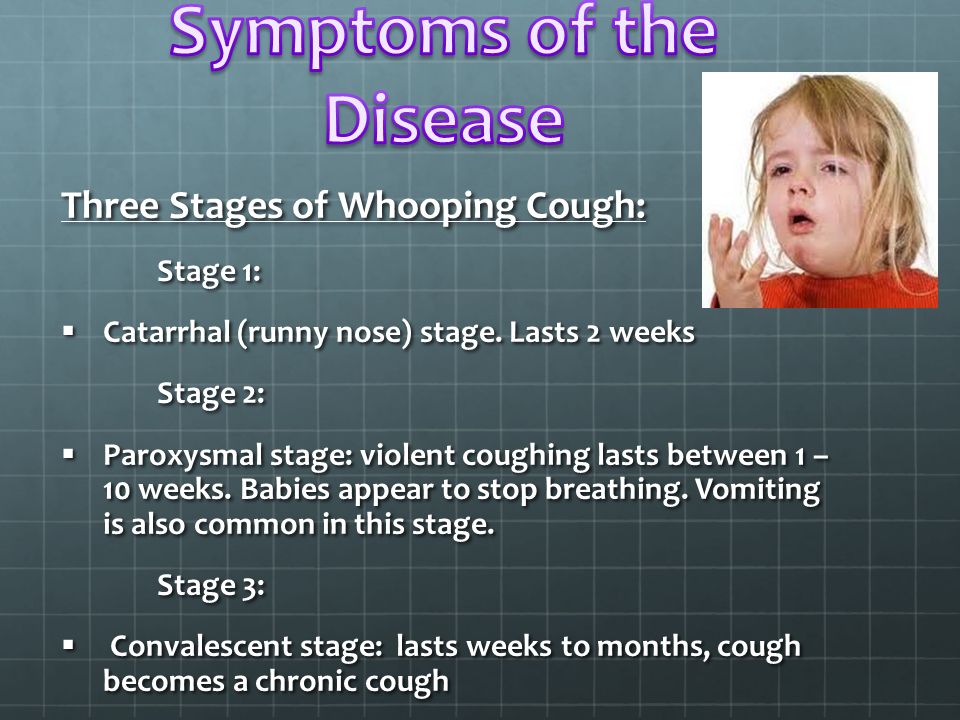 Because this cough is associated not so much with the infection itself, with the whooping cough microbe itself, but with the fact that a dominant excitation is created in the nervous system that supports this cough. Small children, unfortunately, do not know how to cough well, it is difficult for them to cough, they have a different structure, muscles, skeletal system is different for up to a year. Against the background of such attacks, which they still cannot realize well, how to cough, they develop so-called apnea, that is, respiratory arrest. Accordingly, this leads to convulsions, to what used to be called encephalosis, brain damage associated with hypoxia. Unfortunately, this can be fatal. Even in such developed countries as Australia, America, England. Children from pertussis of the first year of life die. Despite all the possibilities of our modern therapy.
Because this cough is associated not so much with the infection itself, with the whooping cough microbe itself, but with the fact that a dominant excitation is created in the nervous system that supports this cough. Small children, unfortunately, do not know how to cough well, it is difficult for them to cough, they have a different structure, muscles, skeletal system is different for up to a year. Against the background of such attacks, which they still cannot realize well, how to cough, they develop so-called apnea, that is, respiratory arrest. Accordingly, this leads to convulsions, to what used to be called encephalosis, brain damage associated with hypoxia. Unfortunately, this can be fatal. Even in such developed countries as Australia, America, England. Children from pertussis of the first year of life die. Despite all the possibilities of our modern therapy.
- Susanna Mikhailovna, tell me, has the quality of these vaccines changed in recent years?
- At the beginning of the 20th century there were no vaccines, there was serum, and these are different things. Serum is ready-made antibodies that must bind microorganisms or a toxin and remove them from the body. These ready-made antibodies are obtained by immunizing a horse, diphtheria and tetanus serum, horses are vaccinated, as it were, blood is taken from the horse, and the serum from this blood is used as a therapeutic drug. It has nothing to do with vaccination. Therefore, vaccines were still created much later than the serum was obtained, but also, of course, in the 20th century. And starting somewhere in the 1940s and 1950s, these drugs began to be used more actively in the world. There was a monopertussis vaccine, that is, a separate prevention of whooping cough. There was a separate diphtheria-tetanus notoxin, then it was combined into combined preparations, which our parents know very well.
Serum is ready-made antibodies that must bind microorganisms or a toxin and remove them from the body. These ready-made antibodies are obtained by immunizing a horse, diphtheria and tetanus serum, horses are vaccinated, as it were, blood is taken from the horse, and the serum from this blood is used as a therapeutic drug. It has nothing to do with vaccination. Therefore, vaccines were still created much later than the serum was obtained, but also, of course, in the 20th century. And starting somewhere in the 1940s and 1950s, these drugs began to be used more actively in the world. There was a monopertussis vaccine, that is, a separate prevention of whooping cough. There was a separate diphtheria-tetanus notoxin, then it was combined into combined preparations, which our parents know very well.
I must say that in our country, too, in the same years and later, the study of side effects. That is, it must be said that much attention has always been paid to this issue - the safety of vaccines.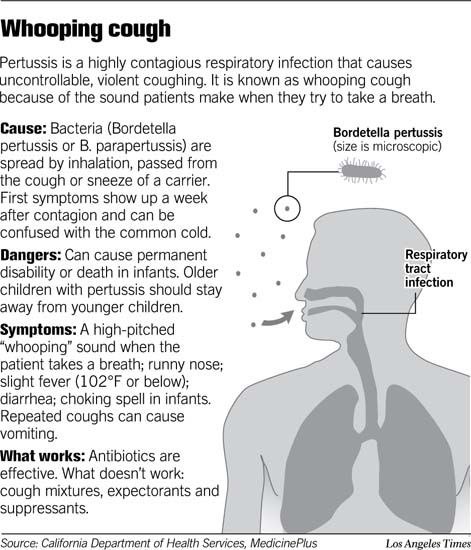 But it was well understood that the danger of infection or the risk of infection is significantly higher than the possible risk from vaccination. And this balance of risks, yes, weighing the risk of infection and the risk of vaccination, has always made it possible to say that it is better to be vaccinated. Therefore, over the past more than half a century, different pertussis vaccines have really appeared in the world. Two - whole-celled and acellular.
But it was well understood that the danger of infection or the risk of infection is significantly higher than the possible risk from vaccination. And this balance of risks, yes, weighing the risk of infection and the risk of vaccination, has always made it possible to say that it is better to be vaccinated. Therefore, over the past more than half a century, different pertussis vaccines have really appeared in the world. Two - whole-celled and acellular.
– What new approaches have emerged in the prevention of whooping cough, diphtheria and tetanus?
– Today, in our country, we have the opportunity to carry out infection prevention at almost any age. Since a vaccine is registered that contains a cell-free pertussis component, several reduced pertussis antigens and diphtheria-tetanus antitoxin. Also with a reduced content of their quantity, corresponding to the domestic vaccine of vaccination against diphtheria and tetanus. Therefore, today we can carry out revaccination, that is, maintain protection against diphtheria, whooping cough and tetanus with this new vaccine at all ages. Re-vaccinations are done every 10 years. This is most important for children going to school. And it is schoolchildren who very often give outbreaks of whooping cough, it is easy for them, they cough for a long time, they miss school, but this is not so scary. Although in children with bronchial asthma, this can lead to serious illness. And bringing this whooping cough home, a schoolboy can infect that small child who is at home. He will be seriously ill, as you have already discussed. Naturally, it is very important to protect young adults, so before leaving school, when we do a booster in 7th grade, you can also use this new vaccine that is now available, and thus extend the protection against whooping cough.
Re-vaccinations are done every 10 years. This is most important for children going to school. And it is schoolchildren who very often give outbreaks of whooping cough, it is easy for them, they cough for a long time, they miss school, but this is not so scary. Although in children with bronchial asthma, this can lead to serious illness. And bringing this whooping cough home, a schoolboy can infect that small child who is at home. He will be seriously ill, as you have already discussed. Naturally, it is very important to protect young adults, so before leaving school, when we do a booster in 7th grade, you can also use this new vaccine that is now available, and thus extend the protection against whooping cough.
– How often are doctors vaccinated against whooping cough?
- To date, we have only received such a vaccine. Because in our country for a long time there was no vaccine for age-related revaccinations. Yes, if the primary complex is called vaccination, then the second one is called revaccination. And we didn’t have the opportunity to revaccinate adults, unfortunately, it just appeared. A couple of years ago, a vaccine was registered, a vaccine for the prevention of pertussis-diphtheria-tetanus is allowed in Russia, this one combined in adults and in children older than 4 years. And starting this year, we can basically apply it.
And we didn’t have the opportunity to revaccinate adults, unfortunately, it just appeared. A couple of years ago, a vaccine was registered, a vaccine for the prevention of pertussis-diphtheria-tetanus is allowed in Russia, this one combined in adults and in children older than 4 years. And starting this year, we can basically apply it.
It contains just a cell-free pertussis component, that is, several pertussis antigens. At the same time, their number is reduced compared to the cell-free vaccine that young children receive. Today, vaccination with cell-free combined vaccines of young children is very common in our country. The calendar includes vaccinations for children, premature babies and risk groups, they just get such a cell-free vaccine according to the plan. And, by the way, they, too, will definitely need to be revaccinated before school with this vaccine. And it's meant for adults. This means that it contains a certain amount of whooping cough antigens, reduced compared to children's variants, it also contains diphtheria-tetanus antitoxin.
First, no vaccine enters clinical practice until it has undergone extensive preclinical and clinical research. First, vaccines are tested and studied for safety in animal models, if possible. And then already on adult volunteers , and only then on children. Already after clinical trials, the vaccine enters into life, it is registered and used in large quantities, and post-marketing surveillance is carried out. That is, after registration, it is mandatory to record all adverse events. So, the safety of this vaccine has been studied in practice for 20 years. That is, there are post-marketing observations.
- Susanna Mikhailovna, as an infectious disease specialist, do you have confidence that after the introduction of this vaccine, its active use, it will become , will the incidence decrease?
- In order for the incidence to decline, we must use several mechanisms, not just one vaccine. We must vaccinate young children very well, that is, children of the first year of life must be 90-95% vaccinated, for sure.