Baby red bumps all over body
Common childhood rashes | Pregnancy Birth and Baby
If your child has a seizure, call triple zero (000) immediately and ask for an ambulance.
If you think your child might have meningococcal rash, go to the nearest emergency department immediately.
Key facts
- There are many different types of childhood rashes. Many are not serious.
- If your child has a rash and fever, they should see their doctor.
- If your child has a meningococcal rash, go immediately to the emergency department.
Meningococcal rash
If you think your child might have meningococcal rash, go to the nearest emergency department immediately.
You can read more about serious childhood rashes here.
Rashes with no fever or itching
Milia (blocked oil glands)
Up to 1 in every 2 newborn babies develop small white spots called milia on their face, especially on the nose. These are just blocked pores, and they’re not itchy or contagious. They usually clear up without treatment within a few weeks.
Erythema toxicum
Many newborns develop a blotchy red skin reaction called erythema toxicum, which can appear between 2 days and 2 weeks after birth. Flat, red patches or small bumps often first appear on the face and spread to the body and limbs. The rash is harmless, not contagious, and will clear after a few days or a week.
Baby acne
Some babies get pimples on their cheeks and nose in the first three months of life. These pimples normally disappear without any treatment, usually within a few months.
Nappy rash
Nappy rash is inflammation of the skin in the nappy area. It can look red, sore and inflamed. Nappy rash is usually caused by urine (wee) or faeces (poo) irritating the skin.
To avoid nappy rash, keep the nappy area clean and dry with frequent nappy changes and nappy-free time. You can help protect the skin by putting on a barrier cream such as zinc or soft white paraffin at each nappy change.
Persistent nappy rash can be treated with a medicated cream. Don’t use talcum powder or antiseptics to treat nappy rash. If your baby develops a fungal infection, you’ll need to use an antifungal ointment. Ask your doctor or pharmacist for advice.
Erythema multiforme (minor)
Erythema multiforme is a rash triggered by an infection (most commonly herpes simplex virus), medicine or an illness. Your baby might feel unwell or have a mild fever before the rash appears. Red spots develop on the hands, feet, arms and legs and spread symmetrically across both sides of the body. The spots often become raised or blistered and then develop into classic target-like lesions.
Erythema multiforme is not contagious, and usually resolves without treatment in 3 to 6 weeks.
Keratosis pilaris (‘chicken skin’)
Keratosis pilaris is a harmless condition where the skin becomes rough and bumpy, as if permanently covered in goose pimples. These bumps most commonly occur on the upper arms and thighs. You can try several things to help the rash to clear up, including moisturising regularly.
You can try several things to help the rash to clear up, including moisturising regularly.
Rashes that might be itchy
Eczema (Atopic dermatitis)
Eczema is a very common skin condition affecting 1 in 3 Australians. It causes the skin to become itchy, red, dry and cracked, often in the creases at the knees and elbows.
Eczema commonly starts before a baby is 12 months old. Eczema follows a relapsing-remitting course. This means that there are flare-ups of the rash, followed by periods where there is no rash or a minimal rash.
Eczema management includes preventative treatment such as avoiding skin irritants, moisturising regularly and using bath oil. Treatment of flare-ups includes using steroid and anti-inflammatory creams.
Ringworm (tinea)
Ringworm is a common, contagious skin infection that causes a ring-like red rash with a clear centre. It commonly occurs on the scalp, feet and groin, but it can appear almost anywhere on the body.
Ringworm is caused by a fungus, not a worm, and is usually treated with over-the-counter antifungal creams. You should keep your child home from childcare or school until a day after you have started treatment to prevent spreading the infection.
You should keep your child home from childcare or school until a day after you have started treatment to prevent spreading the infection.
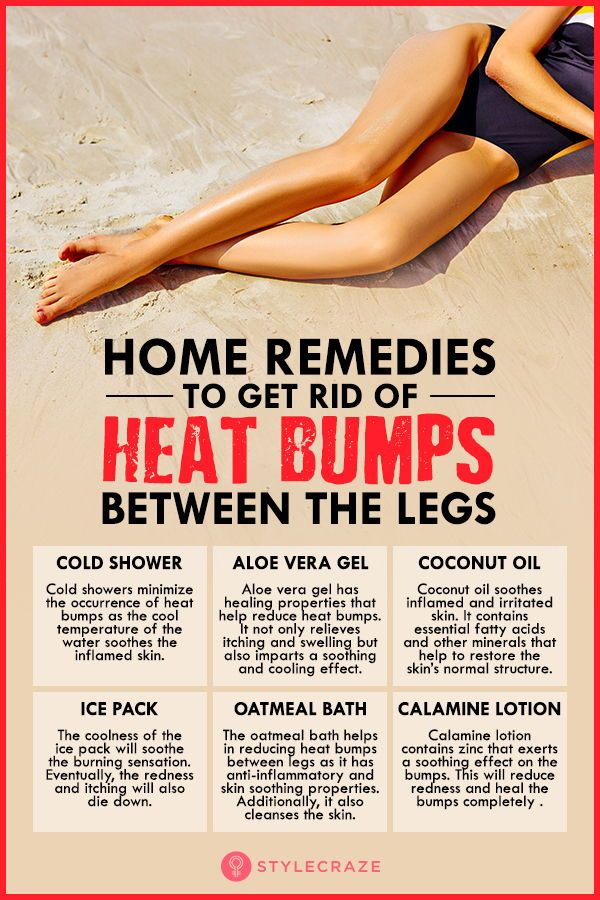
Prickly heat (heat rash)
Heat rash might appear if your baby gets hot in a humid environment. The rash shows as tiny red bumps or blisters on the skin, which can be very itchy. Cooling your baby down and avoiding humidity is the best way to prevent heat rash, which usually clears within 2 to 3 days without treatment.
Impetigo (school sores)
Impetigo is a highly contagious bacterial infection of the skin. It causes red sores and blisters that form a yellow crust. It is very common in children aged 2 to 6, and it is not usually serious in this age group, but it can be dangerous for newborn babies.
If your child has impetigo, you should see your doctor, who might prescribe an antibiotic cream, ointment or tablet. This should clear the infection within 7 to 10 days. Keep your child home from childcare or school and away from young babies until the sores have dried up, usually a few days after treatment starts.
Hives (urticaria)
Hives is a raised, red, itchy rash. It is common on the chest, stomach and back, as well as the throat and limbs, but it can appear on any part of the body. Hives usually disappears within a few days without any treatment. Antihistamines can be given to relieve itching. If the rash doesn't go away, you should see your doctor.
Hives isn’t usually serious, but it can be a sign of a more serious allergic reaction (anaphylaxis). If your child develops hives after eating, or together with other symptoms such as vomiting, dizziness or trouble breathing, you should seek urgent medical attention.
If your child has symptoms of a serious allergic reaction (anaphylaxis), call triple zero (000) immediately and ask for an ambulance.
Pityriasis rosea
Pityriasis rosea is a mild skin rash that sometimes appears after a sore throat, cold or fever. It begins with a single pink or tan-coloured patch on the chest or back. Red, oval-shaped patches, which may be itchy, then appear on the chest or back and limbs over the next weeks.
The exact cause of pityriasis rosea is unclear, and it is not thought to be contagious. The rash usually clears up within a couple of months without treatment.
If you are pregnant, pityriasis rosea can in rare cases lead to complications. See your doctor if you are pregnant and have contact with a child who has pityriasis rosea.
Molluscum contagiosum
Molluscum contagiosum is a viral skin infection that is spread by skin-to-skin contact or by sharing swimming pool water, bath water or towels.
Molluscum contagiosum spots look like pimples and grow into round pearly white lumps, usually 2 to 5 millimetres in size. They can be itchy. They usually heal without treatment within 6 months, but sometimes longer.
Rashes with fever
Slapped cheek disease (fifth disease)
Slapped cheek disease is a viral infection that mainly affects pre-school and school-age children. It typically causes a bright red rash on both cheeks that spreads as a ‘lacy’ rash on the body and limbs. Occasionally, it causes a fever.
Occasionally, it causes a fever.
Slapped cheek disease is usually mild and clears up in a few days without treatment. The child is contagious before the rash appears, but not once it has appeared.
If you are pregnant and catch the virus, it may cause a type of anaemia in your unborn baby. It can also cause miscarriage. If you suspect you or your child has slapped cheek disease, you should avoid contact with people who might be pregnant.
Hand, foot and mouth disease
Hand, foot and mouth disease is a mild but highly contagious viral illness. It causes a rash on the palms of the hands and soles of the feet and blisters in the mouth. It is not the same as the foot-and-mouth disease that affects farm animals.
The disease is common in childcare and kindergartens. Your child might feel unwell and have a fever and blisters on the hands and feet and in the mouth and in the nappy area. The illness usually lasts about 7 to 10 days. Children with hand, foot and mouth disease should stay away from childcare or school until all the blisters have dried up.
Hand, foot and mouth disease usually resolves on its own without complications. In rare cases, it can be more serious, especially if you have a weakened immune system or are pregnant. Complications can include infections of the brain and heart muscle and miscarriage.
Roseola infantum
Roseola infantum is a contagious viral infection that can cause cold-like symptoms and a high fever. The high fever may last for a few days. Roseola infantum can also cause some children to have a febrile convulsion (seizure).
Children with roseola infantum develop a rash after the fever has resolved. The rash looks like raised pink spots that start on the chest, stomach and back and spread to the limbs. The child is contagious before the rash appears, but not after. The rash usually lasts 3 to 5 days.
Febrile convulsions can look scary but are generally not harmful.
If your child has a seizure, call triple zero (000) immediately and ask for an ambulance.
When to seek help
Many babies develop a skin rash in their first days or weeks of life as their sensitive skin adapts to a new environment. Most rashes are harmless and go away on their own, but if your baby seems unwell, or if you’re worried, you should see your doctor. They can advise about the cause and whether treatment is necessary.
Most rashes are harmless and go away on their own, but if your baby seems unwell, or if you’re worried, you should see your doctor. They can advise about the cause and whether treatment is necessary.
Whatever their age, you should take your child to the doctor if they have a rash and persistent high temperature, cold or cough symptoms or swollen neck glands.
Treatment of common childhood rashes
If you think your child might be contagious, they should stay at home. Keep them away from school, childcare and other children. You should also keep them away from people who are pregnant, or who might be pregnant, since some childhood infections can cause serious problems in unborn babies.
You can use paracetamol or ibuprofen (in babies aged over 3 months) to reduce fever — read the packet instructions carefully to ensure your child receives the right amount for their age and weight.
Your pharmacist can advise you on treating the symptoms of common rashes. For example, you can use over-the-counter creams to prevent itchiness.
If you are concerned about your child’s rash, call Pregnancy, Birth and Baby on 1800 882 436 to talk to a maternal child health nurse, or call Healthdirect on 1800 022 022 to talk to a registered nurse. Alternatively, contact your doctor.
Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call. Available 7am to midnight (AET), 7 days a week.
Learn more here about the development and quality assurance of healthdirect content.
17 Most Common Types of Baby Rashes (With Pictures)
Are small red bumps popping up on your baby’s body? There are many possible reasons for baby rashes, so it can be difficult to know what causes them.
Chances are, it’s something completely harmless that will resolve itself within a few days. But it’s still important to keep an eye on any rashes that pop up on your little one.
Our medical team will give you the lowdown on the 17 most common types of baby rashes to help you identify those bumps and set your mind at ease.
Table of Contents
- 1. Baby Acne
- 2. Cradle Cap
- 3. Erythema Toxicum Neonatorum (ETN)
- 4. Atopic Eczema
- 5. Hives
- 6. Diaper Rash
- 7. Milia
- 8. Impetigo
- 9. Fifth Disease
- 10. Hand, Foot, and Mouth Disease
- 11. Measles
- 12. Miliaria
- 13. Scabies
- 14. Ringworm
- 15. Meningitis
- 16. Chickenpox
- 17. Molluscum Contagiosum
- When to Worry About a Rash
- Make a Rash Decision
1. Baby Acne
This rash is nothing to worry about. Most babies have experienced it. It usually shows up within the first couple of weeks of a baby’s life and can last from several days to several months (1).
Causes
Doctors are still not entirely sure why some babies develop acne. But it may be caused by the maternal hormones your baby is exposed to in the womb.
Symptoms
Baby acne is distinguished by tiny red or white pimples on a baby’s cheeks, nose, forehead, and chin. Basically, they look like a tiny teenager going through puberty.
Basically, they look like a tiny teenager going through puberty.
Treatment
The best way to get rid of baby pimples is to keep your baby’s skin clean. Gently wipe the area using soft materials like cotton balls or gentle washcloths.
Moisturizing the skin is essential, so try a mild baby lotion or baby oil. But don’t use too much since this could block the pores and worsen the acne. Most baby acne goes away on its own.
Your baby may need treatment for moderate to severe acne to prevent scarring. Never buy any over-the-counter acne treatment creams intended for teens or adults. These are not safe for newborns. Consult your pediatrician to find the appropriate treatment for the baby acne.
If the acne does not go away on its own, or if it worsens despite treatment, talk to your doctor immediately. Your baby may have a hormonal imbalance issue or other causes of rashes that would warrant a medical exam.
2. Cradle Cap
Cradle cap is easy to recognize and common in newborns. It results in greasy yellow or brown scales at the top of the baby’s head. In some cases, it will move down to the face or neck.
It usually develops within the first two or three months. Cradle cap is not contagious (2).
Causes
Nobody is 100% sure what causes cradle cap. However, it is linked to two common factors:
- Fungus: Some babies react to Malassezia, a fungus naturally found on the skin.
- High sebum levels in the affected area: Sebum is an oily substance consisting of fat, keratin, and cellular debris.
Symptoms
Cradle cap won’t cause fever or discomfort for your baby. However, it can cause large flakes to develop. As the scales fall off, you might notice a few hair strands following.
The skin around the scales can become red, and you might notice a smell in severe cases. I find it similar to the aroma of unwashed hair.
I find it similar to the aroma of unwashed hair.
Treatment
Cradle cap will often clear up on its own within a few weeks, although you can help to get rid of it faster. Treating cradle cap is relatively easy:
- Wash your baby’s hair: Using a mild shampoo, lather your baby’s head, and let the shampoo sit for a minute. Then brush the hair with a soft brush before rinsing.
- Apply baby oil: Baby oil or coconut oil will loosen the scales. Brush your baby’s hair with a soft brush to remove loose flakes.
- Soak overnight: Apply Vaseline, olive oil, coconut oil, or vegetable oil, and let it soak overnight. The following morning, wash your baby’s hair with a mild shampoo and rinse.
- Steroid cream and antifungal shampoo: In more severe cases, your physician may prescribe a low-potency steroid and antifungal cream to alleviate cradle cap.
There are special cradle cap shampoos available. These soften the scales quickly, making them easy to remove. The shampoo also prevents new scales from forming.
These soften the scales quickly, making them easy to remove. The shampoo also prevents new scales from forming.
You should never pick at the scales, although I know it can be very tempting. Removing them from the scalp in this way could result in an infection.
3. Erythema Toxicum Neonatorum (ETN)
ETN is a widespread rash that occurs within the first few days of a newborn’s life. It’s most common in full-term babies.
ETN appears as blotchy red bumps that can sometimes look pale and raised due to fluid buildup. If the fluid looks like pus, this can indicate an infection. But in most cases, it’s only a bodily fluid (3).
Causes
The cause of ETN is unknown but is thought to be related to immune system development.
Symptoms
ETN symptoms include a red rash with bumps that sometimes look white or yellow. It shouldn’t cause any discomfort or fever.
It shouldn’t cause any discomfort or fever.
This rash most commonly appears on the baby’s chest, neck, and face. It can develop anywhere except the palms and soles.
Treatment
There is no treatment necessary. However, if it becomes more severe, you should consult your doctor for advice.
4. Atopic Eczema
Eczema can be extremely uncomfortable as the affected area becomes red, itchy, and even cracked.
It could be a long-term, chronic condition that requires extensive treatment. However, it often clears over time as your little one grows (4).
Causes
Atopic eczema can be passed down by your parents. If you suffer from it or have previously, your newborn might also develop the condition.
If your baby is born with an increased risk, keep them away from specific triggers such as these:
- Soaps and detergents: Don’t use scented detergents or soaps. Make sure all soap residue is rinsed off your baby after a bath.

- Allergens: These could be cold, dry weather or a humid environment. Even dust mites, fur, pollen, mold, heat, sweat, and certain foods can cause an allergy.
- Certain fabrics: Wool and synthetic materials are known to trigger eczema.
Symptoms
The affected area will become red, dry, itchy, cracked, and sore. This could result in bleeding skin and inflammation, and secondary infections may occur.
The areas of skin affected might become darker or lighter after eczema has cleared, although this is only temporary.
Treatment
Keeping the skin hydrated is the best way to avoid a rash. Moisturizers, steroids, or eczema creams can help alleviate this. Consult your pediatrician for creams or ointments to help ease the symptoms.
Covering up the area with bandages might be necessary in some instances. However, damaging the skin could cause more eczema.
You may want to consider putting mittens on your baby. Newborns aren’t coordinated enough to scratch, but they might do some accidental damage. I had some great sleepsuits with integrated foldover mitts and found these worked much better than the loose mittens, which quickly fell off.
Newborns aren’t coordinated enough to scratch, but they might do some accidental damage. I had some great sleepsuits with integrated foldover mitts and found these worked much better than the loose mittens, which quickly fell off.
5. Hives
People of all ages can develop hives. The rash features red raised patches or bright red spots.
Hives can appear anywhere on the body. They’re often extremely itchy and are sometimes accompanied by a stinging or burning sensation (5).
Causes
When hives occur, it is because the body has been in contact with a trigger. This could be allergens, such as certain foods, pollen, latex, medications, or insect bites. Infections can also trigger hives.
The trigger causes the body to release histamines. These carry white blood cells to the affected area, which will repair the damage and eliminate the intruder (the trigger). The histamines cause swelling, redness, and itchiness.
Symptoms
The rash will be made up of swollen, red welts of different sizes. They will be well-defined with a pale center and red surrounding it (similar to mosquito bites but usually bigger).
They will be well-defined with a pale center and red surrounding it (similar to mosquito bites but usually bigger).
Hives can easily spread across the skin in different areas. They can last a few hours, days, or, on rare occasions, weeks.
Treatment
Antihistamines, such as Benadryl, are the best treatment for hives. However, you should never give your baby any medication without consulting a pediatrician first.
If your baby doesn’t seem too bothered by the rash and the size of it isn’t concerning, don’t worry. It should ease and disappear within a day or two.
You can always try different methods to ease the irritation. Wet a washcloth in water, similar to the temperature of a bath, and gently apply it to the affected area.
6. Diaper Rash
A diaper rash is something nearly all parents have to deal with at some point in their child’s life. The rash can be mild, with only a few red spots in one area. More severe rashes will look red and tender (6).
Causes
The leading cause of a diaper rash is prolonged exposure to urine or poop. Here are some other possible causes:
- Disposable diapers: These can sometimes contain chemicals or fragrances which might be causing the reaction.
- Fungal or yeast infection: Bacterias thrive in warm, moist environments, so they often cause rashes in the folds within the diaper area.
- Food: As your baby starts to have solid foods, their stools will change. Acidic foods are known to cause diaper rash in some babies.
- Antibiotics: These will increase the chance of a yeast infection.
Symptoms
The diaper area will be red, a little swollen, and warm to the touch. The rash can spread to the baby’s thighs, stomach, and back.
Some babies will seem troubled by it and uncomfortable during diaper changes. Older children may be holding themselves because it’s painful to pee.
Treatment and Prevention
A diaper rash can be difficult to deal with. But don’t worry, there are many effective ways to treat and prevent it:
But don’t worry, there are many effective ways to treat and prevent it:
- Keep the area dry and clean: Change your baby’s diaper frequently. Gently pat the area dry — never rub!
- Apply ointment or cream: Diaper rash ointments or creams will treat the area and create a barrier on the skin to protect it.
- Loosen the diaper: A good tip is to use a bigger diaper, as this allows for more airflow. You can even leave your baby without the diaper, but make sure to waterproof the surrounding area, particularly if you have a boy!
Cloth diapers are a great option and good for the environment. They need more work since you have to wash them. But they eliminate all the possible chemicals and harsh edges on disposable diapers.
My little one loves cloth diapers as they are softer than disposables. Just remember to wash them in fragrance-free detergent, and never use fabric softeners or dryer sheets.
7.
Milia is common among newborn babies. It looks like tiny white spots that usually form around a baby’s nose (7).
Causes
Milia is entirely harmless. It is the result of the baby’s pores being blocked by dead skin cells.
Symptoms
Small white bumps will appear on a baby’s face and sometimes even on the limbs or the upper body. They can also appear on the roof of the baby’s mouth or on their gums, looking like little teeth coming through. The spots shouldn’t be itchy or painful.
Treatment
The spots will usually clear up on their own within the first four weeks after birth. Never try to squeeze them.
8. Impetigo
Impetigo is a highly contagious infection that causes blisters and sores. Babies and adults can get it, though it’s most common in young children aged 2 to 6 years old. For newborns, it can be dangerous.
The sores and blisters grow quickly and then burst, leaving golden, crusty patches. These may grow and spread to other parts of the body. The patches can also be itchy and painful (8).
Causes
The rash occurs when bacteria enters the skin — this could be through a cut or a sore. If someone with impetigo comes into contact with your baby, there is a high risk of it being passed on.
Symptoms
Impetigo usually starts as a cluster of red blisters. These will grow, burst, ooze, and then spread. The rash is itchy, which increases the spreading.
The skin in the affected area will be red, and the lymph nodes may also become swollen.
Treatment
Mild cases of impetigo won’t require much treatment. By keeping the area clean, it should clear itself up.
A pediatrician might prescribe antibiotics to help your baby’s body fight off the bacteria. Depending on the child’s age, this could be given orally or as a cream.
Trim your baby’s nails and keep them clean to prevent the bacteria from spreading. Wash the scabs gently, twice a day, using warm water and soap. Dry with a towel that is only used for your baby.
9. Fifth Disease
Fifth disease, also known as slapped cheek syndrome or parvovirus B19, takes its unique name from how it looks. Any guesses on what it looks like?
It starts as small red patches on the child’s cheeks. It is most common in preschoolers, but babies can also contract the virus, and pregnant mothers can pass it on to their babies.
It’s highly contagious but not harmful. After recovery, most people develop an immunity to the virus (9).
Causes
The cause of fifth disease is the same as most other viruses. If your baby is in contact with another person carrying the virus, they are at risk.
Symptoms
Apart from the red cheeks, there are a few other symptoms you might notice:
- Fever before the rash appears.
- Stuffy or runny nose.
- Sore throat.
- Upset stomach.
- Headache.
- Fatigue.
- Anemia (lack of red blood cells).
The rash can be itchy and will start on the face, but it can also appear on the arms, legs, and buttocks.
Treatment
You should treat fifth disease like any other cold. Your child will need rest and lots of fluids. However, you should always see your pediatrician when a rash occurs. Though harmless, it’s best to rule out other diseases. In rare instances when anemia becomes severe, further medical interventions such as blood transfusion may be warranted.
10. Hand, Foot, and Mouth Disease
Hand, foot, and mouth disease (HFMD) is another widespread viral disease most common in those under 5 years of age.
The child will begin to develop sores around and inside the mouth. You might find them on the tongue, back of the mouth, or inside of the cheeks (10).
Causes
HFMD is due to the infection commonly caused by a coxsackie virus and is highly contagious. It will spread through sneezes, coughs, stool, and fluid from sores and blisters.
Like any other viral infection, children often pass it on to each other.
Symptoms
There are a few symptoms you might notice before the rash begins. These include the following:
- Fever.
- Loss of appetite.
- Sore throat.
- Fatigue.
After the fever starts, usually within a few days, the first sores or blisters will appear on the hands, feet, or mouth.
These can be extremely painful. Older children will surely complain, while younger children and babies will seem super irritated (because they can’t complain).
Sometimes, the rash appears on the buttocks as well.
Treatment
Mild cases only need observation. Make sure to check your baby’s temperature often. They should drink and eat plenty to give the body strength. However, more severe cases require doctor visits and hospitalization.
Your baby might be miserable, so comfort them as much as possible. Treat them with cold drinks or ice cream, which can ease the discomfort. Never give salty, spicy, or acidic foods.
Never give salty, spicy, or acidic foods.
11. Measles
Measles is another viral infection similar to fifth disease. It starts as small red bumps with white dots inside the cheeks, followed by a fever.
A rash will quickly appear and spread from the face down the back and torso, making its way to the arms and legs.
The rash will look like red patches at first, but it will soon develop into itchy raised bumps. Measles is most likely to occur in unvaccinated children (11).
Causes
Measles is highly contagious and is caused by a virus called paramyxovirus. When a person carrying the virus sneezes or coughs, the virus will spread. The droplets containing the virus stay active for up to two hours outside the body.
The United States was considered measles-free in the year 2000. But it has been appearing again mainly because some parents choose not to vaccinate their children (12).
Symptoms
As the first few bumps begin appearing, you might also notice these symptoms:
- Red and runny nose.

- Low energy levels.
- Loss of appetite.
- Nausea and vomiting.
- Diarrhea.
- Swollen lymph nodes.
Treatment
It is critical you contact a doctor immediately if you suspect your child has measles.
Once confirmed, it is crucial to keep your child away from others to prevent the disease from spreading.
Some studies have demonstrated that vitamin A and antiviral agent ribavirin can play roles in the recovery process (13).
Ensure your little one is as comfortable as possible and watch closely for signs of a fever. Measles can cause the temperature to rise to 105 degrees Fahrenheit, which is dangerous.
Talk with your doctor if your child hasn’t been vaccinated yet and is exposed to the virus. They can give an immune globulin injection, which may prevent or ease the symptoms.
The MMR vaccine is usually scheduled at the age of 12 to 15 months, with a booster vaccine at 4 to 6 years.
12. Miliaria
Miliaria, also called sweat rash, prickly heat, or heat rash, usually occurs if your baby has been sweating excessively.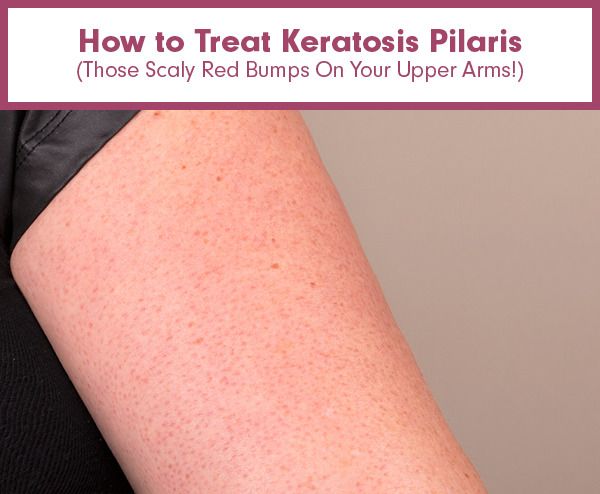 It normally occurs in hot, humid conditions (14).
It normally occurs in hot, humid conditions (14).
Causes
If you live in a hot environment, your baby might sweat quite a lot. The sweat glands can become blocked, resulting in a rash. This can also happen if your baby is dressed too warmly or if they are in an overly hot room, such as a room with a fireplace that has been burning all day.
Symptoms
The rash looks like tiny red bumps or blisters, as sweat is trapped under the skin. There will be a lack of sweat in the affected area, and your baby will experience a prickly feeling.
Treatment
Miliaria doesn’t require any treatment since it usually goes away on its own once your baby cools down. Moving your baby to a cooler environment helps. If the rash takes a little longer to clear, your pediatrician might recommend a cream or ointment.
13. Scabies
Scabies is an infestation of the skin. People of all ages can become infected. A baby with scabies will develop small, red spots all over the body (15).
Causes
Scabies is caused by tiny parasitic mites which burrow into the skin. (Eww!) It most often makes its way to your baby with the help of friends or other family members.
Symptoms
The rash will feature little bumps that can form a line. There will be extreme itchiness that is worse at night with potential sores and crusty areas. Scabies usually occurs on hands and arms but can develop anywhere on a baby’s skin.
Treatment
It’s necessary to contact your doctor and obtain treatment that will kill the mites. However, it’s not enough to only treat your child; it’s crucial to treat everyone who might also be infected. Some people choose to treat the whole house.
14. Ringworm
Ringworm is a common fungal infection. It causes a unique red rash in the form of a ring. Ringworm can develop anywhere on the body.
In babies, it is most often seen on the scalp, feet, and groin area (16).
Causes
Ringworm is actually caused by fungi — not a worm! It spreads as people come into contact with others who are infected — humans or animals. The fungi may also be present on bedsheets, towels, and even combs.
The fungi may also be present on bedsheets, towels, and even combs.
Symptoms
The rash will have round patches that are red or silver. It may be dry, scaly, itchy, and swollen. You might also notice blister-like lesions or some hair loss if the rash appears on the scalp.
Treatment
An antifungal cream, gel, or spray is an effective method. It’s essential to finish the whole course of treatment to make sure the infection is completely cleared.
15. Meningitis
Meningitis is a severe condition that affects the protective membranes surrounding the spinal cord and brain.
While meningitis can affect anyone, it’s most common in babies and children. The infection should be treated immediately. It could develop into life-threatening blood poisoning, called septicemia, which can lead to permanent brain and nerve damage.
Vaccines are available to protect against some forms of meningitis (17).
Causes
A viral or bacterial infection can cause meningitis. Viral infections are the most common cause, including the following :
Viral infections are the most common cause, including the following :
- Enteroviruses.
- Influenza.
- Herpes simplex viruses.
- Varicella-zoster virus.
- Measles and mumps.
- Haemophilus influenza type b (Hib).
- Group B Streptococcus.
- E. coli.
- Streptococcus pneumoniae.
- Listeria monocytogenes.
- Neisseria meningitis.
Symptoms
A patchy rash with lots of small red spots gathered in one area is the first sign. One way to tell if it’s a meningitis rash is by pressing a glass over it. If the rash doesn’t fade, it could be meningitis.
These are some other symptoms of meningitis:
- Fever of 100.4 degrees Fahrenheit or above.
- Lack of energy or extreme sleepiness.
- Rapid breathing.
- Cold hands and feet.
- Pale skin.
- A stiff neck and body.
- Swelling of the fontanelle (the soft spot on a baby’s head).
- Drowsiness or unresponsiveness.
- Seizures.
- Refusing to feed.
- Not wanting to be picked up.
- Unusual high-pitched cry.
- Shivering.
Treatment
If there are any signs of meningitis, it is vital you get your baby to a hospital immediately. This is a medical emergency.
Antibiotics may be given and fluids to treat dehydration. Some cases require steroid medication to reduce swelling around the brain.
Treatment in the hospital can take anywhere from a few days to several weeks. Your baby might also need some aftercare once home again.
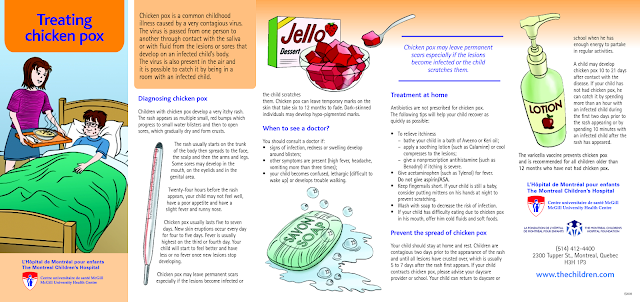
16. Chickenpox
Chickenpox is a rash due to the varicella-zoster virus (VZV) infection. The baby may first show flu-like symptoms before developing a rash, which appears as red, itchy spots over the body.
Babies are especially susceptible to chickenpox infection because they cannot get immunization until the age of one year old. Fortunately, the incidence of chickenpox has declined by 90% since 1995 with the introduction of the varicella vaccine. Since the prevalence of chickenpox decreased drastically in the general population, there are fewer carriers who can pass the disease on to infants, a phenomenon called “herd immunity” (18).
Since the prevalence of chickenpox decreased drastically in the general population, there are fewer carriers who can pass the disease on to infants, a phenomenon called “herd immunity” (18).
Causes
VZV infection occurs through viral transmission similar to that of measles. When a person coughs or sneezes, the air droplets containing the virus can spread to unvaccinated babies, leading to chickenpox. Transmission can also occur through physical contact with those who have a chickenpox rash. Vertical transmission can also occur when an infected pregnant mother transmits the virus directly to the fetus.
Symptoms
Flu-like symptoms can occur in infants infected with chickenpox days before the development of the rash. The flu-like symptoms include:
- Fever.
- Cough.
- Poor feeding.
- Fussiness.
- Fatigue.
- Sleepiness.
The rash starts at the torso and the head, then spreads to limbs over several days. The rash starts as itchy, red bumps, which later become fluid-filled blisters. The blisters burst to become open sores that scab over and heal. This whole process can last from five days to two weeks.
The rash starts as itchy, red bumps, which later become fluid-filled blisters. The blisters burst to become open sores that scab over and heal. This whole process can last from five days to two weeks.
Treatment
You should notify your pediatrician immediately if you suspect your baby has a chickenpox infection, even if the symptoms are mild. You should also let your physician know right away if your baby develops any of the following symptoms:
- High fever.
- Rash on the eyelid or around the eyes.
- Stiff neck.
- Vomiting.
- Severe cough.
- Difficulty breathing.
- Extreme sleepiness or difficulty waking up.
- Rash that has become warm and swollen.
Treatment of chickenpox is usually supportive. However, in more severe cases of chickenpox, or if a baby is born with chickenpox (congenital chickenpox) due to an infected mother, the physician may prescribe an antiviral agent called acyclovir.
To prevent chickenpox from infecting an unvaccinated baby, avoid contact with anyone who is infected with chickenpox.
17. Molluscum Contagiosum
Molluscum contagiosum is another viral infection that causes rashes in babies. The rashes consist of small pink bumps with indented centers. Molluscum contagiosum can occur anywhere on a baby’s body, but it is most commonly found on the head, neck, torso, and armpits.
Causes
The rash is caused by an infection with the molluscum contagiosum virus (MCV). Babies can get molluscum contagiosum rashes in a couple of ways, such as direct skin-to-skin contact with someone who has molluscum contagiosum or contact with objects, such as toys or towels, that have MCV on them.
Most of the time, the only symptom of MCV infection is the rash. The rash appears like pink, skin-colored dome-shaped bumps with central indentations. They can appear anywhere on the body except the palms of the hands, the soles of the feet, and very rarely on the oral mucosa. The bumps can occur in isolations or in groups.
Treatment
Treatment is optional, especially in immunocompetent infants and children, since MCV rashes usually go away on their own within 18 months. Some doctors may use a variety of methods such as freezing the bumps (cryotherapy), removal via sharp instruments (curettage), or application of wart removing chemicals or creams. However, many doctors prefer not to use these methods because they can cause burns and skin scarring.
Some doctors may use a variety of methods such as freezing the bumps (cryotherapy), removal via sharp instruments (curettage), or application of wart removing chemicals or creams. However, many doctors prefer not to use these methods because they can cause burns and skin scarring.
Since molluscum contagiosum can spread from one part of the body to another through contact, it is wise to cover up the areas of rash with small, watertight bandages. Caretakers should also wash their hands often to prevent the spread of the MCV.
When to Worry About a Rash
Babies have sensitive skin, so even the most minor thing can cause a reaction.
Most rashes are harmless and will improve or disappear within a few days. Always contact your pediatrician if a rash looks suspicious or is accompanied by a fever.
Rashes can sometimes be caused by an allergic reaction. With this comes the risk of anaphylactic shock.
These are some of the symptoms of a severe allergic reaction:
- Difficulty breathing.
- Hard for baby to feed or swallow.
- Baby is lethargic.
- Vomiting.
- Increased heart rate.
- Any swelling in the face, around the mouth or throat (19).
Make a Rash Decision
Always take good care of your baby’s precious skin. Don’t bathe your child too frequently using soap. Instead, choose a gentle cleaning product that is unperfumed and moisturizing. End the bath with a lotion or oil massage — this is when you can get a good look at your child’s skin and spot anything out of the ordinary.
Most rashes that appear in newborns are harmless. ETN, baby acne, and heat rash are the most common.
Knowing what to look for should help to ease your mind or let you know when to take action. If you’re ever unsure of a rash and what could be causing it, don’t hesitate to contact your child’s pediatrician.
Feedback: Was This Article Helpful?
Thank You For Your Feedback!
Thank You For Your Feedback!
What Did You Like?
What Went Wrong?
Rash in a child on the body, legs, back
We treat children according to the principles of evidence-based medicine: we choose only those diagnostic and treatment methods that have proven their effectiveness. We will never prescribe unnecessary examinations and medicines!
We will never prescribe unnecessary examinations and medicines!
Make an appointment via WhatsApp
Prices Doctors
The first children's clinic of evidence-based medicine in Moscow
No unnecessary examinations and medicines! We will prescribe only what has proven effective and will help your child.
Treatment according to world standards
We treat children with the same quality as in the best medical centers in the world.
The best team of doctors in Fantasy!
Pediatricians and subspecialists Fantasy - highly experienced doctors, members of professional societies. Doctors constantly improve their qualifications, undergo internships abroad.
Ultimate treatment safety
We made pediatric medicine safe! All our staff work according to the most stringent international standards JCI
We have fun, like visiting best friends
Game room, cheerful animator, gifts after the reception. We try to make friends with the child and do everything to make the little patient feel comfortable with us.
We try to make friends with the child and do everything to make the little patient feel comfortable with us.
You can make an appointment by calling or by filling out the form on the site
Other Pediatric services
- Pediatrician's consultation
- Child Health Management Program
Frequent calls
- Acute bronchiolitis in children: diagnosis and treatment
- SARS
- Angina streptococcal tonsillitis
- Frequently ill child
- Intestinal infections
- Pneumonia (pneumonia) in children
- Colic
- Feeding problems
- Prolonged cough in a child: diagnosis and treatment
- Acute bronchitis in children: diagnosis and treatment
- Pneumonia (pneumonia) in children: diagnosis and treatment
- False croup in a child
- Coxsackie virus in a child
- The child was bitten by a tick! What to do?
Online payment
Documents online
Online services
Rashes on the child's body
Many parents have noticed suspicious rashes on the body of their children. This symptom indicates the presence of any disease of the body or simply its painful condition. In any case, a rash on a child's body can be very dangerous. Therefore, if you notice a rash on the skin, you should immediately make an appointment with the child's pediatrician.
This symptom indicates the presence of any disease of the body or simply its painful condition. In any case, a rash on a child's body can be very dangerous. Therefore, if you notice a rash on the skin, you should immediately make an appointment with the child's pediatrician.
Rash help
Make an appointment with a doctor
Online appointment
Phones:
+7 (812) 30-888-03
+7 (812) 242-53-50 Clinic address: 900 900 50 Petersburg, Vyborgsky district, st. Asafiev, 9, building 2, lit. A (metro station Ozerki, metro station Prosveshcheniya)
Causes of rashes
A rash in children can appear for various reasons. The most “safe” case is when rashes appear due to poor hygiene. In addition, the cause of the rash is allergies, blood diseases, cardiovascular diseases, as well as infections and microbes. In the case of an infection, a rash is not the only symptom: fever, runny nose, sore throat, severe cough, chills, etc. are added to it. Often infections are accompanied by indigestion and vomiting. The rash in such cases does not occur immediately, but appears after a few days.
Often infections are accompanied by indigestion and vomiting. The rash in such cases does not occur immediately, but appears after a few days.
Rash most often occurs as a symptom of diseases that are commonly referred to as "children's". We are talking about chicken pox, rubella, measles, scarlet fever and some other infections that people get sick, mainly in childhood. Moreover, depending on the disease, the nature of the rash changes, so that doctors can diagnose only one type of rash. The most dangerous rash, which refers to the symptoms of meningitis.
Diseases causing rashes on the skin of children
Let's analyze the types of rash in a child in more detail, depending on the disease.
- Chicken pox. Perhaps the most famous disease that is accompanied by a rash. With chickenpox, reddish spots appear on the entire surface of the body, which grow and become bubbles filled with a clear liquid. The growth of the bubbles is accompanied by itching, but over time they dry out and fall off, sometimes leaving characteristic “pockmarks”.
 Chicken pox often causes fever, and doctors recommend treating blisters of the rash with brilliant green.
Chicken pox often causes fever, and doctors recommend treating blisters of the rash with brilliant green. - Measles. Initially, a rash in the form of large red spots appears on the face, but literally within 2-3 days it spreads “from top to bottom” along the body to the very legs. In addition, the child begins to have a sore throat, runny nose and cough, and the temperature rises. The largest spots merge into large inflamed areas.
- Meningococcal infection. The most dangerous infection, as it causes meningitis. It is very important to recognize the disease in time, as it develops very quickly. The rash is expressed in the form of large spots resembling bruises. If you see a doctor as soon as possible, the chances of a cure are very high.
- Rubella. The rash is accompanied by fever and inflammation of the lymph nodes. A rash on the body of a child in the form of small red spots appears mainly on the buttocks and in the places where the limbs are bent.
 After a few days, the rash disappears without leaving any consequences.
After a few days, the rash disappears without leaving any consequences. - Scarlet fever. With scarlet fever, a rash in the form of small pimples appears on the second day all over the body, but their highest concentration is noted in the groin, in the places of the folds of the arms and legs and in the lower abdomen. After a few days, the rash disappears, and the skin in these places begins to peel off strongly. Also during the peak of the disease, swelling, rash and redness of the entire skin are noted.
- Enteroviral infection. Redness and rash appear on the third day after infection and last for about two to three days. Their other symptoms, doctors note vomiting, diarrhea, fever and general weakness of the body.
- Parasites. In this case, the rash is not caused by infections, but by scabies mites or other parasites that live on the human body. The scabies mite "drills" holes in the skin, leaving entrances and exits in the form of dots. The most “attractive” parts of the body for a tick are places with thin skin: groin, wrists, areas between fingers, etc.
 Since the tick can be transmitted from one person to another, urgent treatment is necessary after the detection of this pathology.
Since the tick can be transmitted from one person to another, urgent treatment is necessary after the detection of this pathology. - Cardiovascular diseases. As a rule, these diseases are not typical for children, although they occur in them. Vascular disease can be recognized by small hemorrhages under the skin. Larger areas form bruises.
Other causes of rashes
Sometimes, even with all the rules of hygiene and the absence of diseases, a rash on the body of a child appears with enviable regularity. In this case, it is most likely an allergic reaction of the body to various substances. If this is true, then allergies can be recognized by other symptoms that will inevitably appear along with the rash: a runny nose, cough, tears, and itching. Also, a rash on the body of a child may appear from burns by plants or insect bites. Even a simple mosquito bite often causes a severe rash in children, which is accompanied by itching.
And, of course, very often a rash appears due to poor hygiene. Unlike adults, children's skin is much thinner and more delicate, so even a short-term lack of care for it can lead to a rash. Children, especially the smallest, should be washed and washed regularly. But wearing a lot of clothes on him or leaving him in wet diapers is not worth it - this can lead to diaper rash, irritation, and a rash.
Unlike adults, children's skin is much thinner and more delicate, so even a short-term lack of care for it can lead to a rash. Children, especially the smallest, should be washed and washed regularly. But wearing a lot of clothes on him or leaving him in wet diapers is not worth it - this can lead to diaper rash, irritation, and a rash.
Rash Help
If you find a rash on your child's body, you should see a doctor as soon as possible. You can make an appointment at our Poem Health clinic. In addition, you can call a doctor at home if the child is in a serious condition. Moreover, sometimes a doctor's house call is mandatory, since many diseases with symptoms in the form of a rash are easily transmitted to such children. You need to be especially careful with rubella, as it seriously affects the health of pregnant women. And if you suspect meningitis, you need to call not just a doctor, but an ambulance team.
Do not try to get rid of the rash on your own before seeing a doctor. Firstly, it will make it difficult for a doctor to determine the diagnosis. Secondly, it can lead to even more rashes in the child. It is best to wait for the examination of the doctor and listen to his recommendations for further treatment of the rash. Bacterial rashes are treated with antibiotics, scabies - with special means against ticks, allergies - with appropriate drugs with isolation from the source of allergies, etc. More complex treatment is needed for cardiovascular diseases, but, in the end, a rash on the body of a child is always treated successfully.
Firstly, it will make it difficult for a doctor to determine the diagnosis. Secondly, it can lead to even more rashes in the child. It is best to wait for the examination of the doctor and listen to his recommendations for further treatment of the rash. Bacterial rashes are treated with antibiotics, scabies - with special means against ticks, allergies - with appropriate drugs with isolation from the source of allergies, etc. More complex treatment is needed for cardiovascular diseases, but, in the end, a rash on the body of a child is always treated successfully.
Rash Prevention
To avoid a rash on the body, you need to take steps to prevent it. First of all, we are talking about the basic rules of personal hygiene. At the earliest age, parents should take care of this, later they should teach this to their child as early as possible. Compliance with hygiene helps to get rid of not only rashes, sweating and dirt, but also prevents many infectious diseases.
In addition, infections can be prevented by vaccination.