Constant vomiting while pregnant
Severe vomiting in pregnancy - NHS
Sickness in pregnancy (sometimes called morning sickness) is common. Around 8 out of every 10 pregnant women feel sick (nausea), are sick (vomiting) or both during pregnancy. This does not just happen in the morning.
For most women, this improves or stops completely by around weeks 16 to 20, although for some women it can last longer.
Some pregnant women experience very bad nausea and vomiting. They might be sick many times a day and be unable to keep food or drink down, which can impact on their daily life.
This excessive nausea and vomiting is known as hyperemesis gravidarum (HG), and often needs hospital treatment.
Exactly how many pregnant women get HG is not known as some cases may go unreported, but it's thought to be around 1 to 3 in every 100.
If you are being sick frequently and cannot keep food down, tell your midwife or doctor, or contact the hospital as soon as possible. There is a risk you may become dehydrated, and your midwife or doctor can make sure you get the right treatment.
Symptoms of hyperemesis gravidarum
HG is much worse than the normal nausea and vomiting of pregnancy.
Signs and symptoms of HG include:
- prolonged and severe nausea and vomiting
- being dehydrated. Symptoms of dehydration include, feeling thirsty, tired, dizzy or lightheaded, not peeing very much, and having dark yellow and strong-smelling pee
- weight loss
- low blood pressure (hypotension) when standing
Unlike regular pregnancy sickness, HG may not get better by 16 to 20 weeks. It may not clear up completely until the baby is born, although some symptoms may improve at around 20 weeks.
See your GP or midwife if you have severe nausea and vomiting. Getting help early can help you avoid dehydration and weight loss.
Getting help early can help you avoid dehydration and weight loss.
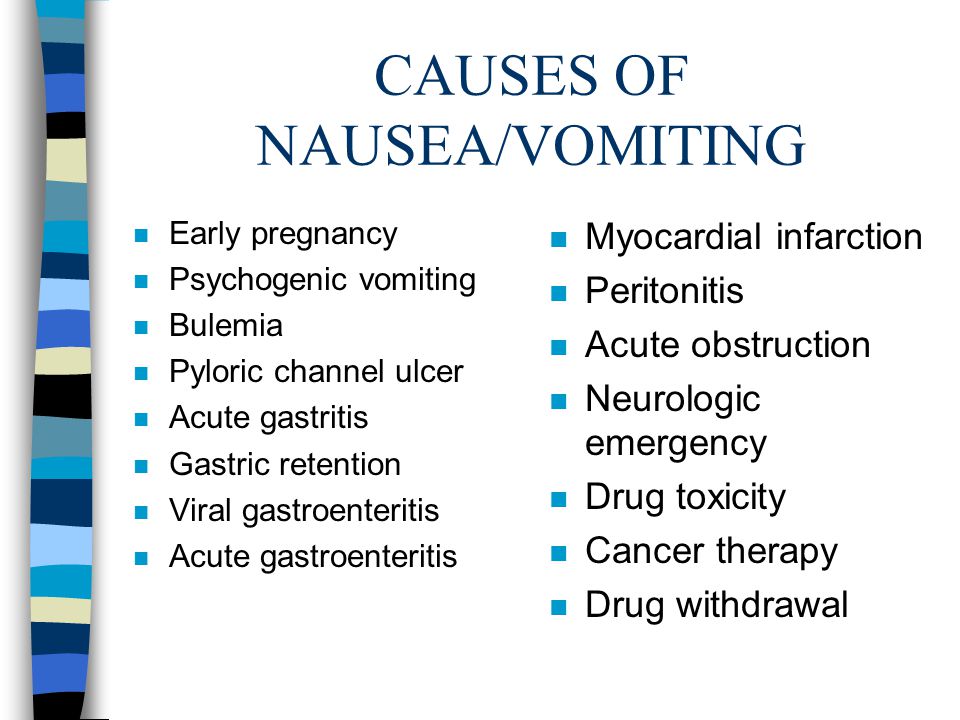
There are other conditions that can cause nausea and vomiting, and your doctor will need to rule these out first.
See the healthtalk.org website for videos and written interviews of women talking about their experiences of hyperemesis gravidarum and how they coped.
What causes hyperemesis gravidarum?
It's not known what causes HG, or why some women get it and others do not. Some experts believe it is linked to the changing hormones in your body that occur during pregnancy.
There is some evidence that it runs in families, so if you have a mother or sister who has had HG in a pregnancy, you may be more likely to get it yourself.
If you have had HG in a previous pregnancy, you are more likely to get it in your next pregnancy than women who have never had it before, so it's worth planning in advance.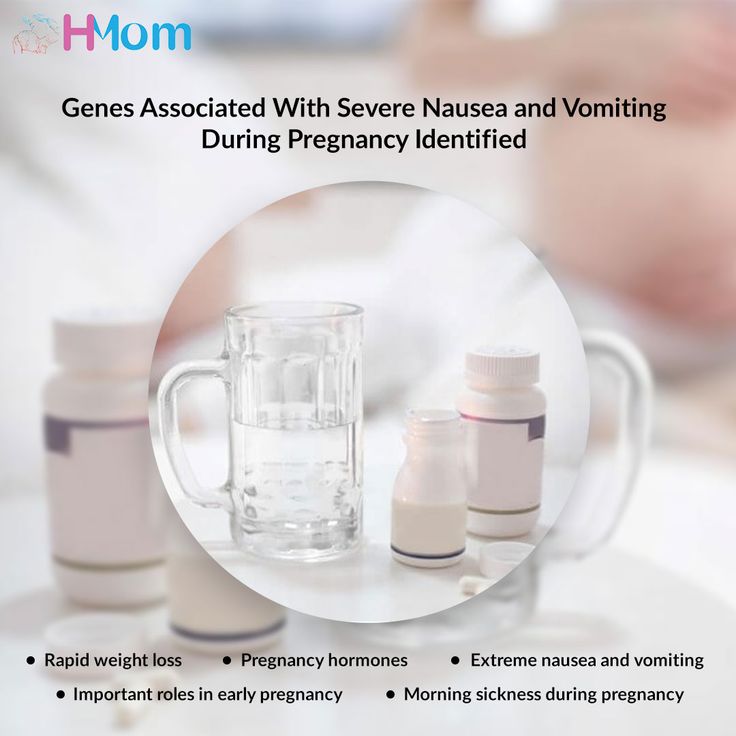
Treating hyperemesis gravidarum
There are medicines that can be used in pregnancy, including the first 12 weeks, to help improve the symptoms of HG. These include anti-sickness (anti-emetic) drugs, vitamins (B6 and B12) and steroids, or combinations of these.
You may need to try different types of medicine until you find what works best for you.
You can visit the Bumps website to find out which medicines are safe to use in pregnancy.
If your nausea and vomiting cannot be controlled, you may need to be admitted to hospital. This is so doctors can assess your condition and give you the right treatment to protect the health of you and your baby.
Treatment can include intravenous fluids, which are given directly into a vein through a drip. If you have severe vomiting, the anti-sickness drugs may also need to be given via a vein or a muscle.
The charity Pregnancy Sickness Support has information and tips on coping with nausea and vomiting, including HG.
Will hyperemesis gravidarum harm my baby?
HG can make you feel very unwell, but it's unlikely to harm your baby if treated effectively.
However, if it causes you to lose weight during pregnancy, there is an increased risk that your baby may be born smaller than expected (have a low birthweight).
Other symptoms you may experience
Pregnancy Sickness Support is in touch with many women who have had HG, and who report having some or all of the following symptoms in addition to the main symptoms listed above:
- extremely heightened sense of smell
- excessive saliva production
- headaches and constipation from dehydration
If you experience these symptoms, you are not alone. Many women have them and they will go away when the HG stops or the baby is born.
Many women have them and they will go away when the HG stops or the baby is born.
How you might feel
The nausea and vomiting of HG can impact your life at a time when you were expecting to be enjoying pregnancy and looking forward to the birth of your baby.
It can affect you both emotionally and physically. The symptoms can be hard to cope with. Without treatment HG may also lead to further health complications, such as depression or tears in your oesophagus.
Severe sickness can be exhausting and stop you doing everyday tasks, such as going to work or even getting out of bed.
In addition to feeling very unwell and tired, you might also feel:
- anxious about going out or being too far from home in case you need to vomit
- isolated because you do not know anyone who understands what it's like to have HG
- confused as to why this is happening to you
- unsure about how to cope with the rest of the pregnancy if you continue to feel very ill
If you feel any of these, do not keep it to yourself. Talk to your midwife or doctor, and explain the impact HG is having on your life and how it is making you feel. You could also talk to your partner, family and friends if you want to.
Talk to your midwife or doctor, and explain the impact HG is having on your life and how it is making you feel. You could also talk to your partner, family and friends if you want to.
If you want to talk to someone who has been through HG, you can contact Pregnancy Sickness Support's help section. They have a support network across the UK and can put you in touch with someone who has had HG.
Bear in mind that HG is much worse than regular pregnancy sickness. It is not the result of anything you have or have not done, and you do need treatment and support.
Another pregnancy
If you have had HG before, it's likely you will get it again in another pregnancy.
If you decide on another pregnancy, it can help to plan ahead, such as arranging child care so you can get plenty of rest.
You could try doing things that helped last time.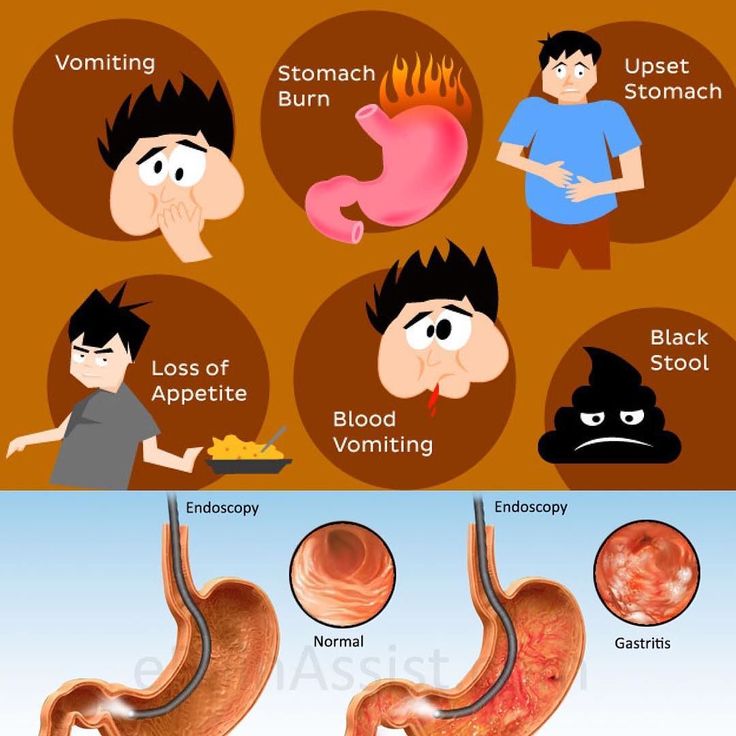
Talk to your doctor about starting medicine early.
Blood clots and hyperemesis gravidarum
Because HG can cause dehydration, there's also an increased risk of having a blood clot (deep vein thrombosis), although this is rare.
If you are dehydrated and immobile, there is treatment that you can be given to prevent blood clots.
Read more about how to prevent deep vein thrombosis.
Severe vomiting during pregnancy (hyperemesis gravidarum)
Severe vomiting during pregnancy (hyperemesis gravidarum) | Pregnancy Birth and Baby beginning of content6-minute read
Listen
Key facts
- Hyperemesis gravidarum is a complication of pregnancy in which sufferers experience severe nausea and vomiting.
- It is more severe than morning sickness.
- It can lead to other health problems including dehydration, malnutrition, depression, anxiety and difficulty doing day-to-day tasks.
- Most people with hyperemesis gravidarum need to go to hospital for intravenous (IV) fluids and treatment.
What is hyperemesis gravidarum?
Hyperemesis gravidarum is a complication of pregnancy in which sufferers experience severe nausea and vomiting. It makes eating and drinking difficult and leads to weight loss, malnutrition and dehydration if it is not treated.
How is hyperemesis gravidarum different to morning sickness?
Morning sickness refers to nausea and vomiting in pregnancy, even though it doesn't only occur in the morning. The majority of people who are pregnant have some level of morning sickness.
Hyperemesis gravidarum is more severe, affecting about 1 in 100 people who are pregnant. There isn’t a clear definition as to when morning sickness becomes severe enough to be called hyperemesis gravidarum.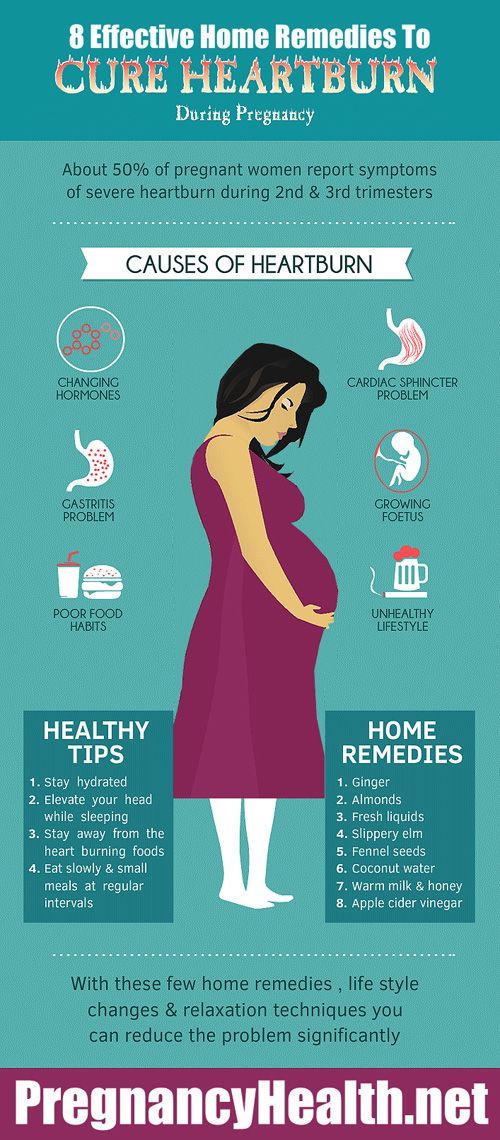
In general, people with morning sickness may feel put off by certain foods, but they can eat and drink and don’t lose much weight. Symptoms come and go and usually improve with dietary changes. Sometimes it may affect your mood and your ability to do your usual daily activities.
People with hyperemesis gravidarum have symptoms that are severe and constant. They have difficulty eating and drinking anything and usually need medicines and intravenous fluids. It often involves having to take time off work and needing help with your daily activities. It may affect your mood and in some cases could cause post-traumatic stress after your baby is born.
Both morning sickness and hyperemesis gravidarum usually start between 4 and 10 weeks of pregnancy and improve by 20 weeks. Some people continue to have symptoms throughout pregnancy.
What symptoms or problems could I have with hyperemesis gravidarum?
The main symptoms of hyperemesis gravidarum are severe nausea and vomiting, difficulty eating and drinking and weight loss. Some people have excessive saliva production.
Some people have excessive saliva production.
Hyperemesis gravidarum can lead to other health problems, such as:
- malnutrition and dehydration
- an imbalance of salts or acid in your body
- kidney damage
- low vitamin levels
- a tear in your oesophagus
- reflux
- constipation
- dental erosion
Other possible effects of hyperemesis gravidarum include:
- depression, anxiety and post-traumatic stress
- breastfeeding difficulties
- relationship problems
- financial problems
- difficulty with daily activities
- reluctance to have more children
How is hyperemesis gravidarum treated?
You should receive treatment from a doctor with special expertise in this area. You’ll be monitored closely, and may need to go to hospital for ongoing care.
There are many dietary and lifestyle measures that can reduce nausea and vomiting. These are worth trying, but more intensive treatment is usually needed if you suffer from hyperemesis gravidarum.
What treatment will I need?
There are several different medicines available to treat nausea and vomiting. Your symptoms might not disappear completely, but the aim is for you to manage to eat and drink some food or water during the day without vomiting.
Some people find that multivitamins make them feel sick. It’s fine to stop pregnancy multivitamins if this helps, if possible, try to continue taking folate.
If you’ve had hyperemesis gravidarum, in future pregnancies it can help to start taking medicine for nausea and vomiting as early as possible — even before you conceive.
Hydration
Try to drink fluids so you don’t get dehydrated. It can help to sip on a drink containing sugar or electrolytes every 15 minutes, or suck on ice blocks or icypoles.
If you can’t keep food or fluids down, go to your local emergency department. You will need intravenous (IV) fluids, which may help improve nausea and vomiting, and can help keep up your levels of electrolytes.
Nutrition
Try to eat small amounts regularly. Eat any food that you can keep down, as long as it’s safe in pregnancy — don’t worry about eating healthy foods right now.
You might need to see a dietitian. If you have low vitamin levels, you may need supplements.
In extreme cases, if you’re unable to eat, you may need to be fed through a tube. This can cause complications and requires careful monitoring.
Treatment of related conditions
Other treatments may include:
- antacids or other medicines to treat reflux
- laxatives for constipation
- medicines to reduce saliva production
Rinse your mouth out with water after vomiting, to protect your teeth from damage. If you can, add some baking soda to the water you rinse with.
Can hyperemesis gravidarum affect my baby?
If you have hyperemesis gravidarum, your placenta may not be working as it should. This can affect your baby. Your baby may be more likely to be small and to be born early. It’s not clear if you have a higher risk of stillbirth.
It’s not clear if you have a higher risk of stillbirth.
In severe cases, people with hyperemesis gravidarum may choose to have a termination of pregnancy (abortion) if they have tried intensive treatment without relief.
Where can I get support?
If you experience hyperemesis gravidarum, contact Hyperemesis Australia for information and support.
You can also call Pregnancy, Birth and Baby on 1800 882 436 to speak to a maternal child health nurse.
Other sources of support include:
- relatives or friends who may be able to help you with day-to-day tasks or prepare meals for your family
- services such as cleaners and supermarket delivery
- a social worker
- a psychologist or counsellor for help with depression and anxiety
- Perinatal Anxiety & Depression Australia (PANDA)
If you suffer from hyperemesis gravidarum, it’s likely that working will be difficult, talk to your employer about changing to another role, or about taking special parental leave if you need extended time off to take care of yourself.
Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call. Available 7am to midnight (AET), 7 days a week.
Sources:
Society of Obstetric Medicine of Australia and New Zealand (Guideline for the management of nausea and vomiting in pregnancy and hyperemesis gravidarum), Royal Hospital for Women (Hyperemesis gravidarum (HG) and nausea and vomiting in pregnancy (NVP) - management), Hyperemesis Australia (What is HG?), The Royal Hospital for Women (Nausea and vomiting of pregnancy (NVP)), King Edward Memorial Hospital (Looking after yourself), Hyperemesis Australia (House and family), Hyperemesis Australia (Oral hygeine), Hyperemesis Australia (Mental health), Hyperemesis Australia (Diet and nutrition), Hyperemesis Australia (Employment)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: August 2022
Back To Top
Related pages
- Morning sickness
- Healthy diet during pregnancy
Need more information?
Nausea and vomiting in pregnancy and Hyperemesis Gravidarum - Maternal, child and family health
While nausea and vomiting are both common symptoms of early pregnancy, if you are very sick and it’s impacting your normal life, you may have Hyperemesis Gravidarum or HG as it’s often known, which involves excessive nausea and vomiting during pregnancy
Read more on NSW Health website
Pregnancy - morning sickness - Better Health Channel
Morning sickness is typically at its worst early in the day but it can strike at any point during the day or night.
Read more on Better Health Channel website
Morning sickness - MyDr.com.au
Many women experience morning sickness (nausea and vomiting) in early pregnancy, and the symptoms can actually occur at any time of the day or night.
Read more on myDr website
Morning sickness
Morning sickness is a feeling of nausea or the experience of vomiting during pregnancy. Find out why some women get it and what you can do to relieve it.
Read more on Pregnancy, Birth & Baby website
Multiple pregnancy (triplets or more)
Learning you're pregnant with triplets or more can be a shock, but overall, most parents find having multiple babies to be a positive experience.
Read more on Pregnancy, Birth & Baby website
Blood tests during pregnancy
Find out more about the blood tests you be offered during your pregnancy. what they test for and when you’ll be offered them.
Read more on Pregnancy, Birth & Baby website
Glossary of pregnancy and labour
Glossary of common terms and abbreviations used in pregnancy and labour.
Read more on Pregnancy, Birth & Baby website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Early toxemia of pregnancy - causes and treatment
- When does early toxemia begin during pregnancy
- Manifestation of early toxicosis
- Causes of early toxicosis
- Severity of toxicosis during pregnancy
- How to manage morning sickness and relieve symptoms
- Principles of treatment of early toxicosis
Most women, having barely learned about the onset of pregnancy, expect to feel unwell, bouts of nausea and even vomiting. Indeed, early toxicosis often becomes a constant companion of many expectant mothers in the early stages of pregnancy. Is there any way to alleviate these unpleasant symptoms? nine0018
Indeed, early toxicosis often becomes a constant companion of many expectant mothers in the early stages of pregnancy. Is there any way to alleviate these unpleasant symptoms? nine0018
Toxicosis (and doctors call this condition gestosis) is a syndrome that is defined as a violation of a woman's adaptation to pregnancy. According to the time of occurrence, early preeclampsia is distinguished, which will be discussed in this article, and late preeclampsia, which appears in the last 2-3 months of pregnancy and is manifested by edema, increased blood pressure and the appearance of protein in the urine.
When early morning sickness begins in pregnancy
Early morning sickness usually occurs in the first half of pregnancy. As a rule, after the end of the formation of the placenta, that is, at 12-13 weeks of pregnancy, the phenomena of toxicosis stop. During a normal pregnancy, adaptive changes in the function of almost all organs and systems occur in a woman's body, which are regulated by the nervous system with the participation of endocrine glands. Toxicosis also occurs due to the impossibility of the adaptive mechanisms of the body of the expectant mother to adequately meet the needs of the developing fetus. nine0019
Toxicosis also occurs due to the impossibility of the adaptive mechanisms of the body of the expectant mother to adequately meet the needs of the developing fetus. nine0019
Manifestation of early toxicosis
The most common manifestation of toxicosis is vomiting. Other forms of early toxicosis are very rare:
- pregnancy dermatosis is a group of skin diseases that occur during pregnancy and disappear after it. When it occurs in early pregnancy, dermatosis is caused by immune disorders in the body of a pregnant woman, and is also most often found in patients with diseases of the digestive and endocrine systems. The most common form of dermatoses of pregnancy is pruritus gravidarum, which can be on a small area of the skin or spread throughout the body, including the feet and palms. nine0004
- tetany (chorea) of pregnant women. This condition occurs when the function of the parathyroid glands decreases, as a result of which calcium metabolism in the body is disturbed.
 Clinically, the disease is manifested by muscle cramps, more often cramps occur in the fingers, sometimes in the muscles of the face.
Clinically, the disease is manifested by muscle cramps, more often cramps occur in the fingers, sometimes in the muscles of the face. - salivation - increased secretion of saliva, in connection with which there is a large loss of fluid (up to 1 liter per day). Salivation can be an independent manifestation of toxicosis or accompany vomiting of pregnant women. In the development of salivation, not only changes in the central nervous system are important, but also local disturbances in the salivary glands and their ducts under the influence of hormonal changes. nine0004
- Pregnancy bronchial asthma is an extremely rare form of preeclampsia.
- osteomalacia of pregnancy - softening of the bones due to a violation of the metabolism of calcium and phosphorus, while the bones of the pelvis and spine are more often affected
- neuropathy and psychopathy of pregnant women.
Learn more about the services:
- Tests for pregnant women
- Ultrasound of the 1st trimester of pregnancy
Causes of toxicosis in the early stages
There are many theories trying to explain the causes and mechanisms of development of early toxicosis: the most recognized are the so-called neuro-reflex and immunological.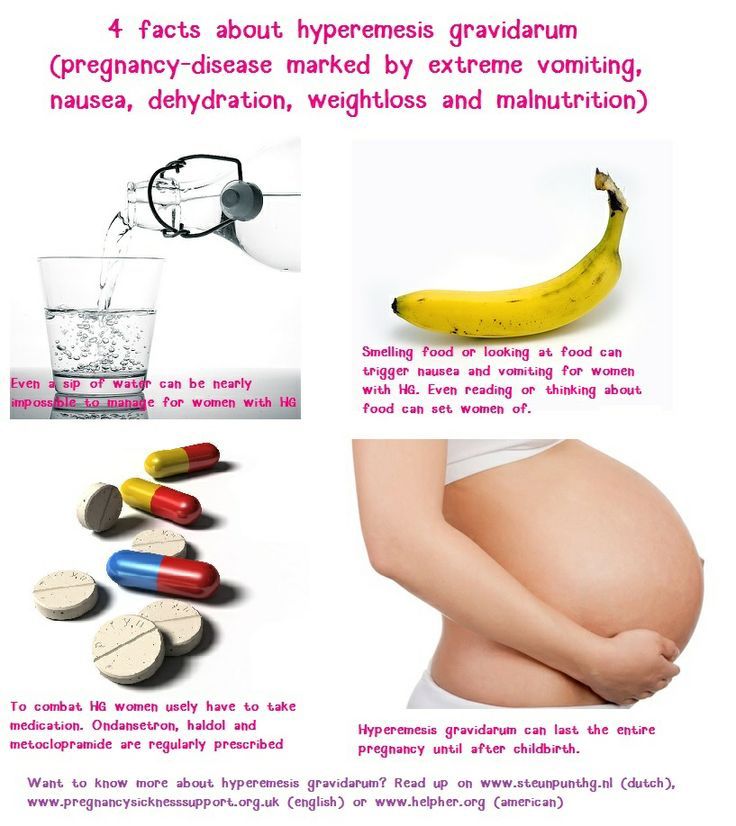
According to the neuro-reflex concept , vomiting occurs as a result of a violation of the relationship between the cerebral cortex and subcortical structures. During pregnancy, the subcortical centers of the brain begin to work more intensively than usual, which are responsible for most protective reflexes, including breathing and cardiac activity. In the same areas of the subcortical structures are the vomiting and salivary centers, the nuclei of the olfactory system of the brain. Excitation processes also capture them. Therefore, nausea and vomiting may be preceded by such phenomena as deepening of breathing, increased heart rate, an increase in the amount of saliva, pallor due to vasospasm, and a change in smell. nine0019
Immunological disorders play a certain role in the development of preeclampsia . The timing of the onset of vomiting usually coincides with the formation of blood circulation in the placenta, increased reproduction of white blood cells - lymphocytes, which are involved in immune reactions. The fetus is foreign to the mother's body, and her immune system reacts to it in this way. After the full maturation of the placenta, which accumulates all these immune cells, toxicosis usually disappears.
The fetus is foreign to the mother's body, and her immune system reacts to it in this way. After the full maturation of the placenta, which accumulates all these immune cells, toxicosis usually disappears.
Human chorionic gonadotropin (hCG) plays a certain role in the development of vomiting during pregnancy. This hormone is produced by the placenta during pregnancy. Its high concentration can provoke vomiting.
The severity of toxicosis during pregnancy
The main symptom of early toxicosis of pregnant women is vomiting. Depending on the frequency of its occurrence, as well as the degree of metabolic disorders in the body of the expectant mother, doctors distinguish three degrees of severity of vomiting during pregnancy. nine0019
How to manage morning sickness and relieve symptoms
Treatment for mild morning sickness is usually done at home. But, nevertheless, a pregnant woman should be under the supervision of doctors, take all the tests recommended by the doctor, and follow the appointments. This will allow the doctor to monitor the condition of the future mother's body and prevent possible complications in time. A woman needs to organize a normal sleep and rest regimen, walks in the fresh air, a calm atmosphere in the family are shown. nine0019
This will allow the doctor to monitor the condition of the future mother's body and prevent possible complications in time. A woman needs to organize a normal sleep and rest regimen, walks in the fresh air, a calm atmosphere in the family are shown. nine0019
Proper nutrition
You need to eat in small portions, fractionally, every 2-3 hours. Food should be easily digestible, high-calorie and fortified whenever possible. In connection with a decrease in appetite, they recommend varied and pleasant food for the expectant mother, that is, products are selected taking into account the desires of the pregnant woman, with the exception of spicy dishes and smoked meats. It is important to remember that very hot or very cold food often induces vomiting, so the dishes should be warm. Reception of alkaline mineral waters in small volumes 5-6 times a day is shown. nine0019
If nausea and vomiting occur in the morning, immediately after waking up, it is recommended to have breakfast while lying in bed without getting up.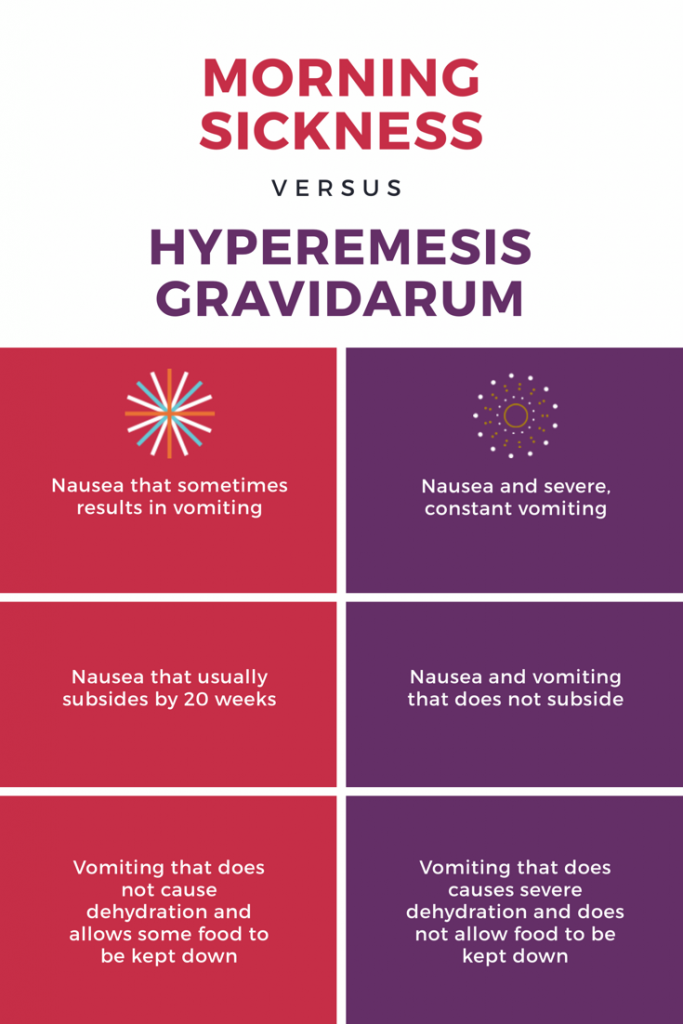 For breakfast, you can eat dry crackers, crackers, drink tea or water with lemon, light yogurt is allowed. It is better to put all this next to the bed in advance or ask someone to bring breakfast.
For breakfast, you can eat dry crackers, crackers, drink tea or water with lemon, light yogurt is allowed. It is better to put all this next to the bed in advance or ask someone to bring breakfast.
Every woman chooses for herself a remedy that helps to fight nausea. Someone helps a slice of orange, lemon or apple, some expectant mothers carry crackers or mint sweets with them to alleviate the symptoms of toxicosis. Pumpkin juice has a good antiemetic effect. Many pregnant women benefit from ginger tea. It is prepared very simply:
ginger root finely chopped or grated on a coarse grater is poured with boiling water and infused for 15-20 minutes. Tea can be drunk warm or chilled, adding lemon, mint or honey to it.
Fats and proteins of animal origin are recommended to be consumed in the morning, when pancreatic enzymes are more active. Dairy products are best eaten after dinner or before bed.
Do not use food with preservatives, broiler meat, fast food, fast food. nine0019
nine0019
To maintain metabolic processes in the body, it is advisable to drink 2-2.5 liters of fluid per day. With increased vomiting, it is not recommended to consume solid and liquid food at the same time. Liquids should not be drunk 30 minutes before and within 1.5 hours after eating, as this provokes vomiting by stretching the walls of the stomach and affecting the receptors.
Decoctions and infusions
Oat broth
As an enveloping agent, that is, a substance that forms a mucous film and prevents irritation of receptors on the walls of the stomach and intestines, oat broth is recommended. It is prepared as follows: 2-3 tbsp. spoons of oat grains are washed, pour 500-700 ml of water, boil over low heat under a lid for 30 minutes. The broth is drained, the grains are crushed and poured with new water and boiled until fully cooked. The resulting mass is crushed with a blender. You need to use the decoction on an empty stomach and in the evening before going to bed, but not earlier than 2 hours after dinner, and also throughout the day in small portions. nine0103 It has a particularly good effect in combination with rosehip infusion.
nine0103 It has a particularly good effect in combination with rosehip infusion.
Rosehip infusion
This infusion is a good source of vitamins and microelements - it contains vitamins C, K, P and PP, potassium, manganese, iron, and contributes to the normalization of the gallbladder function. To prepare it, you need 1 tbsp. pour a spoonful of crushed rose hips with 250 ml of boiling water and insist in a thermos for about 2 hours.
The following infusions and decoctions contribute to reducing nausea and improving the condition of the expectant mother. nine0019
Phytonast
Take equally: valerian root, common anise fruits, fireweed leaves, linden flowers, marigold flowers, common blueberry shoots, blood red hawthorn fruits. 1 st. Pour 500 ml of boiling water over a spoonful of the mixture ground in a coffee grinder and insist in a thermos for 2 hours, then strain. Take the infusion as needed, up to 6 times a day in a heated form, 1/3 cup.
Benediktov's collection
To prepare this collection you will need: common yarrow (10 g), peppermint herb (20 g), shepherd's purse herb (20 g), valerian officinalis rhizomes (10 g), calendula officinalis inflorescences (20 g) and inflorescences of chamomile officinalis (20 g). Pour 10 g of the mixture with 400 ml of water, soak in a water bath for 30 minutes, strain. Take 50 ml 6 times a day for 25 days, three courses with 15-day breaks. nine0019
Pour 10 g of the mixture with 400 ml of water, soak in a water bath for 30 minutes, strain. Take 50 ml 6 times a day for 25 days, three courses with 15-day breaks. nine0019
Viburnum with honey
Grind 2 tbsp. tablespoons of fresh viburnum berries, pour 250 ml of boiling water over them, heat for 10 minutes in a water bath, strain, add a little honey. Take 1/3 cup of warm infusion before meals 3-4 times a day.
Cranberries with mint, honey and lemon
Squeeze the juice from 250 g of cranberries, cool it, boil the pulp in 1 liter of water, add 1 tbsp. a spoonful of mint leaves and leave for 15 minutes under the lid. Strain, dissolve in a hot broth 2-3 tbsp. tablespoons of honey, let cool to room temperature, add chilled cranberry juice and a slice of lemon. Drink 0.5 cup after meals or when nausea occurs. nine0019
Rose hips with apples
Crushed rose hips (about 1 tbsp) pour 250 ml of boiling water, add 0.5 tbsp. tablespoons of dried apples, heat in a water bath for 15-20 minutes. This drink can be consumed throughout the day instead of tea.
This drink can be consumed throughout the day instead of tea.
Rosehip with garden berries
To make a drink you will need: 1 tbsp. a spoonful of rose hips, 1 tbsp. spoon of raspberries, 1 tbsp. spoon of blackcurrant leaves, 1 tbsp. a spoonful of lingonberry leaves. 2 tbsp. spoons of the mixture pour 500 ml of boiling water, boil for 5 minutes, leave for 1 hour, strain. Take 100 ml of decoction 3 times a day. nine0019
Therapeutic exercise
Among non-drug treatments, exercise therapy has a good effect. The complex of exercises includes walking, deep breathing with stretching of the muscles of the trunk and limbs. It is necessary to exclude inclinations, they can increase nausea. The complex includes dynamic exercises for training the muscles of the arms, legs, relaxation exercises. Remedial gymnastics also includes training in breathing techniques. As a result, the body is saturated with oxygen, the excitability of the vomiting center decreases - toxicosis is relieved. nine0019
nine0019
Physiotherapeutic procedures
Physiotherapeutic procedures for the treatment of early toxicosis include electrosleep, acupuncture, laser therapy . Electrosleep is a method that uses low frequency currents to induce sleep. The duration of the procedure is from 60 to 90 minutes, the course of treatment is 6-8 sessions.
Laser therapy
In the complex therapy of early toxicosis, blood is irradiated with a helium-neon laser through a light guide passed through a needle placed in the cubital vein. The procedure lasts 15-20 minutes. The therapeutic effect is achieved due to the influence of the laser on blood cells, changes in its properties, accumulation of biologically active substances in the blood. As a result, the metabolism in cells changes, the resistance of tissues and the body to adverse conditions increases, and the vitality increases. nine0019
Acupuncture, acupuncture
Treatment methods based on stimulation of biologically active points and zones on the body and face. With early toxicosis, such an effect changes the tone of the nervous system of a pregnant woman. A session of acupuncture is carried out 1-2 times a week and lasts 15-30 minutes.
With early toxicosis, such an effect changes the tone of the nervous system of a pregnant woman. A session of acupuncture is carried out 1-2 times a week and lasts 15-30 minutes.
Acupressure method is effective for morning sickness and vomiting of pregnant women. To do this, you need to press your finger on a point that is located on the inside of the wrist, in the middle, 3 transverse fingers above the palm. nine0019
Aromatherapy
The use of plant aromas has a positive effect on the expectant mother and baby. By inhaling pleasant aromas, you can achieve a good psychological effect, create a good mood, and reduce the effects of toxicosis. During pregnancy, aroma lamps, aroma medallions, pads - sachets are mainly used. To relieve nausea and vomiting, oils of noble laurel, lemon, lavender, cardamom present, dill, lemon balm, peppermint, anise, eucalyptus, ginger are suitable. To flavor the air, you can use the following mixture 0 3 drops of lavender oil, 1 drop of peppermint oil, 1 drop of eucalyptus oil. nine0019
nine0019
Principles of treatment of early toxicosis
Even with a mild course of early toxicosis of pregnant women, the attending physician will definitely prescribe a number of tests - a general blood test, a general urinalysis, a biochemical blood test, a hemostasiogram. This is necessary to control the condition of a pregnant woman and to timely prescribe medications to correct the changes that occur in the body.
If non-drug remedies are ineffective, the doctor prescribes medications that help fight toxicosis. First of all, these are herbal sedatives, homeopathic medicines for nausea, vitamin B6 preparations, antiemetics. nine0019
If, despite all the therapy, vomiting increases, the doctor detects changes in blood and urine tests, and body weight continues to progressively decrease, hospitalization is indicated.
An intravenous infusion of medicines is carried out in the hospital, which restores the fluid, microelements and proteins lost by the body. A pregnant woman receives at least 2-2.5 liters of fluid intravenously per day.
A pregnant woman receives at least 2-2.5 liters of fluid intravenously per day.
To improve blood flow through the placenta and improve oxygen supply to the fetus, oxygen therapy can be prescribed - inhalation of an oxygen-air mixture for 20-30 minutes twice a day. nine0019
Most often, the effects of toxicosis gradually decrease by 12-13 weeks of pregnancy.
Mild
Mild vomiting on an empty stomach or after meals occurs 3 to 5 times a day. Despite vomiting, part of the food is still retained and significant weight loss is not observed in such pregnant women. The general condition does not suffer significantly, there are no changes in blood and urine tests. Such vomiting is easily treatable with various non-drug means, and often resolves on its own after the normalization of the diet and rest. nine0019
Moderate vomiting
Moderate vomiting (or moderate vomiting) is expressed in the increase in vomiting up to 10 times a day, regardless of food intake. Characterized by persistent nausea. There comes dehydration of the body, a decrease in body weight by 3-5 kg (6% of the initial weight). The general condition of pregnant women worsens. Expectant mothers complain of weakness, apathy, tearfulness, sometimes depression. The skin is pale, dry, the tongue is covered with a white coating, yellowness of the skin may be noted.
Characterized by persistent nausea. There comes dehydration of the body, a decrease in body weight by 3-5 kg (6% of the initial weight). The general condition of pregnant women worsens. Expectant mothers complain of weakness, apathy, tearfulness, sometimes depression. The skin is pale, dry, the tongue is covered with a white coating, yellowness of the skin may be noted.
Excessive vomiting
The severe form (excessive pregnancy vomiting) is rare. The frequency of vomiting up to 20 times a day or more. Excessive vomiting is characterized by severe dehydration and intoxication. This condition can occur as a continuation of moderate vomiting of pregnant women or initially acquire a severe character. With excessive vomiting, body weight decreases rapidly, on average by 2-3 kg per week, the skin becomes dry and flabby, subcutaneous fat quickly disappears, the tongue and lips are dry, there is a smell of acetone from the mouth, body temperature can rise up to 38 degrees. Vomiting of moderate and severe degrees is treated in a hospital. nine0019
nine0019
Toxicosis and other difficulties of a pregnant woman - Motherhood in Khabarovsk
Toxicosis and other difficulties of a pregnant woman, 6-13 week
How to deal with nausea
Take the time to understand what makes you worse and what makes you better. Many women find that minimal additions to their lifestyle can help manage nausea.
If you feel sick in the morning, try eating cookies with a glass of water without getting out of bed. It may be better for you now to avoid rushing in the morning and get to work after rush hour. Distribute work in accordance with your well-being, and if some duties make you feel worse, change with colleagues. nine0019
If you can eat, eat whatever you want - you can focus on healthy eating later. Right now you might get better just from the high blood sugar, so peck at something, and then, when the nausea passes, you can eat properly. Eat little and often. Always carry apples, nuts, or sandwiches with you so you can have a snack before you start to feel sick.
If you cannot eat, try to drink more water, diluted juices or even broth. Try your luck with ice cream: very cold foods usually don't smell. nine0019
It is very important to drink plenty of fluids. If this is difficult for you, here are some tips:
- Keep a glass of water handy
- Drink through a straw
- Experiment: water - plain or sparkling - with lemon juice. Choose the right proportion.
Choose the right proportion.
- Change the temperature of liquids - ice water, warm lemon water, iced fruit teas.
- Sometimes it helps to eat and drink at the same time - drink something and try to eat after that. nine0019
Toxicosis and other difficulties of pregnancy, 5 day - 13 week
Nausea during pregnancy
Some women experience nausea and even vomiting very early, even before they discover they are pregnant. Nausea torments 85% of pregnant women, and approximately 50% suffer from vomiting. For some women, this is a slight temporary inconvenience. For very few, it is a dangerous condition that takes away the last of their strength. Fortunately, most women fall somewhere in between. nine0019
Nausea torments 85% of pregnant women, and approximately 50% suffer from vomiting. For some women, this is a slight temporary inconvenience. For very few, it is a dangerous condition that takes away the last of their strength. Fortunately, most women fall somewhere in between. nine0019
There are many theories to explain nausea and vomiting. It is known that pregnant women feel better when the formed placenta takes over the production of pregnancy hormones. Most doctors believe that it is the hormones, but some believe that this is a protective mechanism that prevents a pregnant woman from eating something that is harmful to the baby. One study links nausea to women eating a diet high in saturated fat before pregnancy. It's strange that Mother Nature would see fit to spoil the start of a pregnancy like this, but nauseated women all over the world, in all cultures and, it seems, at all times, so in that sense, nausea is a "normal" attribute of pregnancy. nine0019
Toxicosis and other difficulties of pregnancy, 4-13 week
When to Report Nausea to Your Doctor
Nausea can only become a serious problem if the body is dehydrated. Pernicious vomiting of pregnancy is an extremely rare but serious complication that must be treated in the hospital.
Pernicious vomiting of pregnancy is an extremely rare but serious complication that must be treated in the hospital.
You should tell your doctor even about ordinary nausea, but if you think that this is no longer “normal”, contact your doctor immediately. This should be done if:
- you have been unable to retain food in your body for two or three days;
- you cannot drink;
- you have a fever or pain;
- you have vomiting and diarrhea;
- you have other symptoms such as bleeding;
- nausea appeared suddenly, and before that you felt good (in this case, nausea may be caused by food poisoning, so it's better to clarify this).
Toxicosis and other difficulties of pregnancy, 4-13 week
Does toxicosis affect the child
Surely you wondered: "Is everything all right with my child?" Sometimes you feel so bad that it's hard to believe that the child does not feel anything. But at this stage, the baby is so small that even if you eat almost nothing, he still gets all the nutrients he needs.
But at this stage, the baby is so small that even if you eat almost nothing, he still gets all the nutrients he needs.
If a woman suffers from nausea during pregnancy, she is less likely to have a miscarriage or premature birth, and the risk of birth defects in the baby is not increased. So, while you can't be bothered, your child is probably doing great. nine0019
Toxicosis and other difficulties of pregnancy, 4-13 week
Metallic taste in the mouth and drooling
In early pregnancy, you may develop a strong metallic or bitter taste in your mouth, preventing you from eating certain foods and foods. It often starts very early, and disappears at 12-14 weeks.
It often starts very early, and disappears at 12-14 weeks.
Some say it's due to a lack of nutrients in your diet, others think it's due to bleeding gums, and still others attribute it to hormonal spikes that cause morning sickness. If you can, suck on a mint or swish lemon water in your mouth to ward off the aftertaste. nine0019
Another joy of early pregnancy is excessive salivation. Sometimes the amount of saliva is produced in such quantity that you have to spit all the time. Fortunately, things rarely go to this extreme. Try drinking water with lemon juice or, if you can, suck on a slice of fresh lemon. You may need to place a towel over your pillow. It is probably worth going to a homeopath, as there are no traditional remedies for this condition. If you haven't noticed any changes in your saliva, you're in luck. nine0019
Toxicosis and other difficulties of pregnancy, 4-13 week
How to deal with nausea at work
In the first trimester, when you feel sick all the time, it can be very difficult to go to work.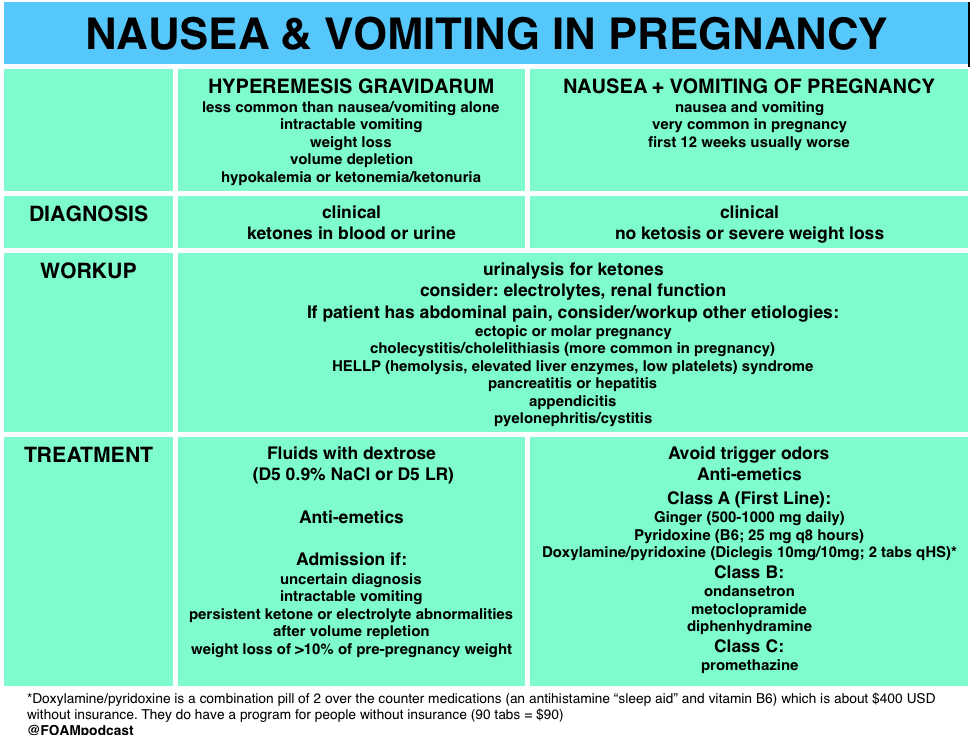 You will feel better if you have a light snack ready. Make yourself a "first aid kit" and keep it in your desk drawer or in your locker. These can be: apples and bananas, muesli bars in yogurt or chocolate, gingerbread cookies, a bag of mixed nuts, a bag of sour dried fruits, such as prunes or dried pineapple pieces. nine0019
You will feel better if you have a light snack ready. Make yourself a "first aid kit" and keep it in your desk drawer or in your locker. These can be: apples and bananas, muesli bars in yogurt or chocolate, gingerbread cookies, a bag of mixed nuts, a bag of sour dried fruits, such as prunes or dried pineapple pieces. nine0019
Don't forget to drink: stock up on small packets of juice and keep water bottles nearby. If you have a machine with drinking water at work, go to it more often - at the same time you will warm up.
If you've tried everything and the nausea still plagues your life, consider taking a week off and just relaxing. You will probably feel noticeably better if you can sleep for a few days and "recharge your batteries."
Toxicosis and other difficulties of pregnancy, 7-26 week
Harmful professions: working conditions
Your employer has an obligation to minimize any risk in the workplace and must make every effort to ensure that you can work safely during your pregnancy. If your job poses a threat to you and your child, you have the right to request a transfer to another job. To do this, you need to provide the boss or the personnel department with a written statement that you are pregnant. nine0019
If your job poses a threat to you and your child, you have the right to request a transfer to another job. To do this, you need to provide the boss or the personnel department with a written statement that you are pregnant. nine0019
The following work conditions do not suit you in your position:
- overtime, shift work, night work, business trips: you have every right to refuse such work. It is prescribed by the Labor Code;
- standing for a long time, heavy lifting: this can lead to miscarriage, premature birth, low birth weight;
- the need to sit for a long time on an uncomfortable cramped seat: this can cause problems with blood circulation. You must be provided with a chair with a high back, armrests and height adjustment, as well as a footstool; nine0019
- stepladder work: this can be dangerous, because during pregnancy your center of gravity shifts and you risk falling.
Toxicosis and other difficulties of pregnancy, 7-26 week
Harmful professions: working conditions
Working in a shop or office is not dangerous, but if you work in a laboratory or factory, it can be difficult.
The following working conditions are not suitable for pregnant women:
- shaking and vibration: for example, working on off-road vehicles increases the risk of miscarriage, so it is worth postponing participation in the rally for the time being; nine0019
- hot and cold;
- work with radioactive substances: including in the X-ray room, when welding plastic, when vulcanizing rubber. If you work near sources of radiation, tell your employer that you are pregnant;
- operation under pressure drops: including in air and under water;
- handling biologically active substances or very strong medicines: if you are a nurse or pharmacist who prepares these medicines, or if your job is to dispose of waste, you should take extra precautions; nine0019
- work in places where there is a risk of carbon monoxide poisoning: these are enclosed spaces in which internal combustion engines operate.
- working with animals: if you have to deal with lambs, you need to take special precautions to avoid infection, which can lead to miscarriage. By law, a pregnant woman must be released from work related to animal husbandry and crop production.
By law, a pregnant woman must be released from work related to animal husbandry and crop production.
Toxicosis and other difficulties of pregnancy, 7-26 week
Long road to work during pregnancy
The time you spend commuting to and from work is not covered by maternity safety laws, so your employer cannot help you. However, you can try to make traveling a more comfortable and less tiring part of your daily routine:
However, you can try to make traveling a more comfortable and less tiring part of your daily routine:
- find out if you can shift your work hours so you don't travel during rush hour, avoid crowding and be able to sit; nine0019
- think about whether you can take work home at least one day a week;
- write an ad at work - suddenly there is an employee who lives in your area and agrees to give you a lift to work and home.
- if you feel sick on public transport, do not take it into your head to endure it with gritted teeth: be sure to make it clear that you are pregnant and that you need to sit down.
- always carry water with you, as well as nuts, dried fruits or hard candies - so that you can eat and cope with nausea. nine0019
Toxicosis and other difficulties of pregnancy, 14-26 week
How to deal with heartburn during pregnancy
Pregnancy hormones affect the valve between the esophagus and the stomach, and it closes worse than usual.
Therefore, women feel a burning sensation in the upper part of the stomach. However, if you suffer from heartburn and it occurs several times a day, there are ways to cope with it:
- eat little and often; nine0019
- eat slowly and chew your food thoroughly;
- during and after eating, sit straight: wait until the food is digested, and only then move;
- avoid fatty foods and any foods that you find difficult to digest;
- do not drink with meals, but between meals.
Heartburn is usually aggravated by carbonated drinks, coffee, alcohol, spicy and fatty foods.
Toxicosis and other difficulties of pregnancy, 5-26 week
Thrush during pregnancy
During pregnancy, the immune system is suppressed and the chance of developing thrush increases. This is also affected by changes in the mucous membrane of the vagina and in the secretions. Usually, thrush does not cause any symptoms and only becomes a problem if it is too severe (irritation and itching of the vulva, burning, white cheesy discharge). For many women, thrush appears for the first time during pregnancy. Your doctor will likely prescribe you an antifungal cream or suppositories. However, you can try to cope with thrush without medication:
This is also affected by changes in the mucous membrane of the vagina and in the secretions. Usually, thrush does not cause any symptoms and only becomes a problem if it is too severe (irritation and itching of the vulva, burning, white cheesy discharge). For many women, thrush appears for the first time during pregnancy. Your doctor will likely prescribe you an antifungal cream or suppositories. However, you can try to cope with thrush without medication:
- eat less sugar;
- use "live" yoghurts - this way you will restore the level of "good" bacteria that will suppress thrush;
- wear cotton underwear;
- try not to wear pantyhose and tight clothes - in them this area overheats and becomes wet, and this is just what the thrush needs.
- do not wear panties - tanga and generally tight panties, as they can form tiny abrasions, and if they get an infection, it will be much more difficult to get rid of it. nine0019
Thrush does not harm your child.
Toxicosis and other difficulties of pregnancy, 14-26 week
What is cervical weakness
Sometimes the cervix is very soft and weak. This may be the result of surgery. As the baby grows, the uterus puts pressure on the cervix, and if the cervix is weak, it can lead to premature birth or very late miscarriage. This is called cervical weakness.
This is called cervical weakness.
Diagnosing cervical weakness is difficult, and many experts feel that the diagnosis is made too often. Usually it is based on the experience of previous pregnancies. If a woman had a miscarriage after 14 weeks, when spontaneous rupture of the membranes or painless opening of the cervix occurred, the cause of this was probably the weakness of the cervix. nine0019
Toxicosis and other difficulties of pregnancy, 1 day - 26 week
Contact lenses during pregnancy
During pregnancy, many women notice that their vision changes. That is why in the antenatal clinic they give a referral to an ophthalmologist.
That is why in the antenatal clinic they give a referral to an ophthalmologist.
If you wear glasses, you may not notice any deterioration in vision, but if you wear contact lenses, you may notice that your vision has become worse. This is due to the fact that fluid is retained in the body, the shape of the eyeball changes, so it becomes uncomfortable in the lenses. nine0019
It's smart to switch to lenses that need to be changed frequently, so you can quickly adapt to change without spending extra money.
If your eyes become very dry, you may need to limit the amount of time you wear lenses or switch back to glasses for a while.
Toxicosis and other difficulties of pregnancy, 7 month
7th month of pregnancy: weight and back pain
In the last three months you will gain approximately 300-500 grams per week. By the end of the seventh month, the total weight gain will reach 7-11 kg. We can say that now you have become quite clumsy. In late pregnancy, back pain is almost inevitable. Their cause is an increased level of the hormone relaxin, which relaxes all the ligaments and muscles, preparing them for childbirth. The action of relaxin is diverse. By loosening the muscles and ligaments of the pelvis, it changes the way a pregnant woman walks, making you waddle like a duck. Relaxing the muscular wall of the veins, relaxin leads to an increase in their varicose veins, the muscular sphincter of the esophagus - to the appearance of heartburn, and the muscles of the bladder - to the appearance of urinary incontinence. In order not to hurt your back, it is important to monitor your posture. Some happy women may not experience any discomfort, but this does not mean that their body is not preparing for the birth of a child. It all depends on various factors, including heredity and the level of physical fitness.
By the end of the seventh month, the total weight gain will reach 7-11 kg. We can say that now you have become quite clumsy. In late pregnancy, back pain is almost inevitable. Their cause is an increased level of the hormone relaxin, which relaxes all the ligaments and muscles, preparing them for childbirth. The action of relaxin is diverse. By loosening the muscles and ligaments of the pelvis, it changes the way a pregnant woman walks, making you waddle like a duck. Relaxing the muscular wall of the veins, relaxin leads to an increase in their varicose veins, the muscular sphincter of the esophagus - to the appearance of heartburn, and the muscles of the bladder - to the appearance of urinary incontinence. In order not to hurt your back, it is important to monitor your posture. Some happy women may not experience any discomfort, but this does not mean that their body is not preparing for the birth of a child. It all depends on various factors, including heredity and the level of physical fitness. nine0019
nine0019
Toxicosis and other difficulties of pregnancy, 1 day - 30 week
Linking gum disease to preterm birth
It seems incredible that gum disease is associated with the risk of preterm birth, but any infection during pregnancy increases the risk of having a premature or low birth weight baby.