Cancer while pregnant
Cancer During Pregnancy | Cancer.Net
Approved by the Cancer.Net Editorial Board, 08/2020
Cancer during pregnancy is uncommon. Cancer itself rarely affects the growing fetus (unborn baby). When it does happen, cancer during pregnancy can be more complex to diagnose and treat. This is because tests to diagnose cancer and treatments can affect the fetus, so each step in your medical care will be done carefully. It is important to work with a health care team that has experience treating cancer in pregnancy. Learn more about finding an oncologist.
Being diagnosed with cancer or starting cancer treatment during pregnancy can be very stressful and overwhelming. Throughout this experience, it is important to let your health care team know how you are feeling so they can help you find the support you need. This may include an in-person or online support group for other people who have or had cancer during their pregnancy.
What types of cancer occur in pregnancy?
Breast cancer is the most common cancer found during pregnancy. It affects about 1 in 3,000 women who are pregnant. Other cancers that tend to occur during pregnancy are also generally more common in younger people who are not pregnant, including:
-
Cervical cancer
-
Gestational trophoblastic disease
-
Hodgkin lymphoma
-
Melanoma
-
Non-Hodgkin lymphoma
-
Thyroid cancer
How is cancer during pregnancy diagnosed?
It can be more difficult to detect cancer when a person is pregnant. This is because some cancer symptoms, such as bloating, headaches, or rectal bleeding, are also common during pregnancy in general. Breasts typically get larger and change texture during pregnancy and these breast changes may appear normal. This means that cancer-related changes in pregnant women may be noticed later and therefore be diagnosed later than women who are not pregnant.
Pregnancy can also sometimes reveal cancer. For example, a Pap test done as a part of standard pregnancy care can find cervical cancer, or an ultrasound done during pregnancy can find ovarian cancer.
Some of the tests doctors use to find cancer are safe during pregnancy and for the fetus. Others could possibly be harmful. Always talk with your health care team about each recommended test and let the testing staff know you are pregnant. Common tests used in cancer diagnosis include:
X-ray. Research shows that the level of radiation in diagnostic x-rays is too low to harm the fetus. When possible, a shield is used to cover the abdomen during x-rays.
Computed tomography (CT or CAT) scans. CT scans are like x-rays but are much more exact because they use more radiation. They can find cancer or show the spread of cancer. CT scans of the head and chest are usually safe during pregnancy. This is because they do not expose the fetus to direct radiation. When possible, a shield should be used to cover a pregnant woman's abdomen during all CT scans. CT scans of the abdomen or pelvis should only be done if there is no other option. Talk with your health care team about the need for this scan and any risks.
Other tests. Magnetic resonance imaging (MRI), ultrasound, and a biopsy are usually safe during pregnancy.
How is cancer during pregnancy treated?
Planning cancer treatment during pregnancy requires a multidisciplinary team of different types of medical and health care providers working together. This includes cancer doctors called oncologists and high-risk obstetricians. An obstetrician, sometimes called an OB, is a doctor who cares for women during and after pregnancy.
Your cancer doctors and obstetricians will review and compare the best treatment options for you and any possible risks. This will involve looking at a number of factors. The stage of your pregnancy and the type, size, and stage of the cancer are important. Your doctors will also talk with you about your preferences as you make cancer treatment decisions. Throughout treatment, they will closely monitor you to make sure the baby is healthy.
Sometimes doctors may recommend delaying or avoiding certain treatments during pregnancy. For example:
For example:
-
During the first 3 months of pregnancy, some cancer treatments are more likely to harm a fetus. So, your doctors may recommend delaying treatment until the second or third trimester.
-
Some treatments can harm the fetus at any time during pregnancy. Doctors try to avoid using these treatments until after the baby is born. For example, radiation therapy is a powerful treatment that uses high-energy x-rays to destroy cancer cells. Depending on the radiation dose and which area of the body needs treatment, there may be risks to the fetus throughout pregnancy.
-
When doctors find cancer later in pregnancy, they may recommend starting treatment after the baby is born.
-
Doctors may recommend waiting to treat some specific types of cancer, such as early-stage cervical cancer, until after the baby is born.
What cancer treatments can I get during pregnancy?
Some cancer treatments are safer to use during pregnancy than others:
Surgery. During surgery, doctors remove the tumor and some of the healthy tissue around it. There is usually little risk to the fetus. In general, it is the safest cancer treatment during all stages of pregnancy.
During surgery, doctors remove the tumor and some of the healthy tissue around it. There is usually little risk to the fetus. In general, it is the safest cancer treatment during all stages of pregnancy.
Cancer medications. Your treatment plan may include the use of medications to destroy cancer cells, such as chemotherapy. Chemotherapy can only be used during certain times in pregnancy:
-
During the first 3 months of pregnancy, chemotherapy carries risk of birth defects or pregnancy loss. This is when the fetus's organs are still growing.
-
During the second and third trimesters, doctors can give several types of chemotherapy with low risk to the fetus. The placenta acts as a wall protecting the baby, so some drugs cannot pass through. Other drugs only pass through in small amounts. Studies suggest that children exposed to chemotherapy during pregnancy do not show more health issues than children who are not. This includes right after birth and during the child's growth and development.

-
Chemotherapy in the later stages of pregnancy may cause side effects like low blood counts. This can increase the risk of infection and indirectly harm the baby during birth or right after birth.
-
Your health care team may consider inducing labor early to protect the baby from your cancer treatment. This is a decision that will be made with you very carefully, with both your health and your baby's health considered.
-
If you receive chemotherapy after the baby is born, you should not breastfeed the baby. Chemotherapy can transfer to the infant through breast milk.
Does pregnancy affect cancer treatment?
Pregnancy itself does not seem to affect how well cancer treatment works. Finding cancer in a later stage or not starting treatment right away can affect the results of the cancer treatment. Talk with your health care team about how different factors may affect your risk from the cancer and how you recover from treatment.
Questions to ask the health care team
If you are pregnant and recently found out that you have cancer, ask your health care team these questions:
-
How much experience do you have treating pregnant women with cancer?
-
How will you work with my obstetrician?
-
Do I need to have any special tests done to learn more about the cancer? Could there be a risk to my baby in having each test?
-
What are my cancer treatment options?
-
Which treatment plan do you think is best? Why?
-
Do I need to start treatment right away, or should I wait?
-
Could a delay in my treatment affect how I recover from this cancer?
-
Is it safe to continue the pregnancy?
-
What are the short- and long-term risks of my treatment to me? To the baby?
-
How will my baby's health be monitored during my cancer treatment?
-
Will my cancer treatment affect how I give birth?
-
Will I be able to breastfeed?
-
Is there a counselor, oncology social worker, or other team member who can help me cope with the emotional side effects of my diagnosis?
-
What other support services and other resources are available to me? To my family?
Related Resources
Having a Baby After Cancer: Pregnancy
What to Do When You Are Diagnosed With Cancer During Pregnancy
Anxiety
Coping with Uncertainty
Finding Hope During Cancer and Pregnancy: "Your Stories" Podcast
More Information
Hope for Two: The Pregnant with Cancer Network
Pregnancy and Cancer Registry
MedlinePlus: Tumors and Pregnancy
National Cancer Institute: Breast Cancer Treatment During Pregnancy
What to Do When You Are Diagnosed With Cancer During Pregnancy
- Register
- Log In
Search
What to Do When You Are Diagnosed With Cancer During Pregnancy
Elyce Cardonick, MD
January 19, 2021
· Elyce Cardonick, MD
Elyce Cardonick, MD, is a professor in obstetrics and gynecology at Cooper Medical School at Rowan University in Camden, New Jersey. Dr. Cardonick closely follows a cohort study of over 450 pregnant women diagnosed with cancer since 1997, including evaluating outcomes for the mother and child long beyond the postpartum period. Dr. Cardonick has lectured at the American College of Obstetricians and Gynecologists, the Royal College of Obstetricians and Gynaecologists, and the Society for Maternal Fetal Medicine on the treatment of cancer during pregnancy. Dr. Cardonick is also a medical advisor for Hope for Two: The Pregnant with Cancer Network.
Dr. Cardonick closely follows a cohort study of over 450 pregnant women diagnosed with cancer since 1997, including evaluating outcomes for the mother and child long beyond the postpartum period. Dr. Cardonick has lectured at the American College of Obstetricians and Gynecologists, the Royal College of Obstetricians and Gynaecologists, and the Society for Maternal Fetal Medicine on the treatment of cancer during pregnancy. Dr. Cardonick is also a medical advisor for Hope for Two: The Pregnant with Cancer Network.
Receiving a cancer diagnosis during pregnancy can be scary. The excitement of the pregnancy is quickly replaced by the fear of the cancer. Then, the focus of the mother often shifts to wanting to protect the unborn child at all costs. Pregnant women with cancer will often stop focusing on the cancer and instead focus on getting well for the sake of their unborn child, as well as for other children they may have, their partner, or other members of the family who may need them.
Pregnant women also experience cancer differently from other people with the disease. On 1 hand, there is the terrible difference of having to worry about not only fighting for their own life with this new diagnosis, but also worrying about how their own life-saving treatment may affect the life inside of them. The more pleasant difference is that once treatment decisions are made and the initial shock of the diagnosis passes, there is the realization that at the end of treatment, there is the delivery of a baby to look forward to. It is unlike any other reward at the end of a cancer treatment course.
Breast cancer is the most common cancer diagnosed during pregnancy. In fact, approximately 7% to 10% of women diagnosed with breast cancer are younger than the age of 40. And when cancer is diagnosed in women age 30 or younger, an estimated 10% to 20% of cancers are detected either during pregnancy or within the first year after giving birth.
As women delay both marriage and childbearing for careers and other reasons, the average age of a woman’s first pregnancy is now older than it was for previous generations. This shift is likely the reason for the increased number of cases in which various types of cancers are being diagnosed during pregnancy.
This shift is likely the reason for the increased number of cases in which various types of cancers are being diagnosed during pregnancy.
Working with women who have been diagnosed with cancer during pregnancy has been the focus of my career. During my fellowship training in maternal fetal medicine and after completing my residency in obstetrics and gynecology, I met 3 women who helped set the course of my work and my life. One was diagnosed with melanoma on her thigh. Not only was she encouraged to terminate her pregnancy, but once she decided to continue the pregnancy, she also had difficulty finding a surgeon willing to perform the more extensive surgery that was required. Were she not pregnant, she also would have been able to avoid a full groin lymph node dissection. Instead, she would have been able to undergo a nuclear medicine injection to highlight any cancerous lymph nodes in her groin so the surgeon could remove only those. She was motivated to avoid the full groin dissection due to the possible side effect of lifelong leg swelling (called lymphedema), which could affect her ability to do her job. After speaking with both a nuclear medicine physician and surgeon during which we researched the potential risks to the baby, I was able to reassure them and the patient that performing this type of surgery in pregnancy was safe for the unborn child and vital for the mother. The surgery was successful, and her daughter was healthy and born at term. The placenta did not show any evidence of melanoma.
After speaking with both a nuclear medicine physician and surgeon during which we researched the potential risks to the baby, I was able to reassure them and the patient that performing this type of surgery in pregnancy was safe for the unborn child and vital for the mother. The surgery was successful, and her daughter was healthy and born at term. The placenta did not show any evidence of melanoma.
Next, I met a woman with Hodgkin lymphoma who was 10 weeks pregnant. Her oncologist sent her for a nuclear medicine study to evaluate her heart function before she could start chemotherapy. But the radiologist would not do the study unless she terminated the pregnancy. Her oncologist also felt it would be best for her to terminate the pregnancy, as did the hospital’s policies, but she did not wish to do so. I found a few case reports and a small series of cases showing that pregnant women with Hodgkin lymphoma did not have a worse chance of survival compared to non-pregnant women. How could I advise her to terminate the pregnancy if it most likely wouldn’t improve her chance of survival? However, I did not want her to save the pregnancy just to sacrifice herself by avoiding treatment at all costs, especially for such a treatable cancer. I realized that we really needed to convene the ethics board at the hospital to discuss with the oncologist the possibility that she could safely undergo chemotherapy during the later part of pregnancy after the baby’s organs were mostly done developing. After looking for a way to save both mother and child, I found a study that showed the woman could safely undergo chemotherapy during the second and third trimesters of pregnancy. The ethics board at the hospital agreed, and my patient underwent chemotherapy. I had the privilege of following her son’s normal growth and development; he has just graduated from college!
I realized that we really needed to convene the ethics board at the hospital to discuss with the oncologist the possibility that she could safely undergo chemotherapy during the later part of pregnancy after the baby’s organs were mostly done developing. After looking for a way to save both mother and child, I found a study that showed the woman could safely undergo chemotherapy during the second and third trimesters of pregnancy. The ethics board at the hospital agreed, and my patient underwent chemotherapy. I had the privilege of following her son’s normal growth and development; he has just graduated from college!
Because of the rarity of experience in diagnosing and treating pregnant women with cancer, no single institution would be able to collect enough cases to truly learn the safest way to treat cancer during pregnancy. This is when I started the Cancer and Pregnancy Registry, now an international collection of cases of women diagnosed with cancer during pregnancy and their children. The third influential patient for my career path was enrolled in the registry after she was diagnosed with breast cancer. She named her son David because he “fought Goliath,” as he was exposed to chemotherapy before he was born. He is followed annually in the registry, as is his beautiful mother. Both are healthy, and the work has come full circle. David just became a father, and his mother a grandmother. This was something I was told may not be possible for children who were exposed to chemotherapy while in the womb. It was feared their gonads could be affected by chemotherapy. Women diagnosed with cancer during pregnancy can be treated and remain healthy enough to become a mother—and even a grandmother, too!
The third influential patient for my career path was enrolled in the registry after she was diagnosed with breast cancer. She named her son David because he “fought Goliath,” as he was exposed to chemotherapy before he was born. He is followed annually in the registry, as is his beautiful mother. Both are healthy, and the work has come full circle. David just became a father, and his mother a grandmother. This was something I was told may not be possible for children who were exposed to chemotherapy while in the womb. It was feared their gonads could be affected by chemotherapy. Women diagnosed with cancer during pregnancy can be treated and remain healthy enough to become a mother—and even a grandmother, too!
How to cope when you are diagnosed with cancer during pregnancy
Although it is normal for pregnant women with cancer to focus on the unborn child and not themselves, know that the best way to have a healthy child is to take care of yourself during your pregnancy. Consider cancer treatment during pregnancy if that is advised by your doctor. Also take time for yourself, accept help from others, rest, and eat when you can between and during treatments. Know you are not alone; approximately 1 in 1,000 pregnant women are diagnosed with cancer each year.
Also take time for yourself, accept help from others, rest, and eat when you can between and during treatments. Know you are not alone; approximately 1 in 1,000 pregnant women are diagnosed with cancer each year.
If you are receiving cancer treatment while pregnant, be sure to have an open dialogue with your health care team about how the cancer treatment may impact you and your child. The most important question for those newly diagnosed with cancer to ask is, “How would I be treated if I were not pregnant?” The next question to ask should be, “Has this treatment been given before, and what were the risks and outcomes for the children?”
Finally, maybe the most helpful thing to do is to speak with another woman on the phone who has already experienced the same thing and hear her child’s voice in the background. Calling the wonderful support network Hope for Two can put each newly diagnosed woman in touch with a support woman who was also diagnosed with a similar cancer during pregnancy and who safely delivered their child. No one else can quite understand what it’s like to experience the fear of a cancer diagnosis while trying to be happy about a pregnancy like someone who has experienced the same thing.
No one else can quite understand what it’s like to experience the fear of a cancer diagnosis while trying to be happy about a pregnancy like someone who has experienced the same thing.
Tags:
- family
- expert information
- breast cancer
- decision making
- tips
Related Resources:
- Cancer During Pregnancy
- Having a Baby After Cancer: Pregnancy
- Having a Baby After Cancer: Fertility Assistance and Other Options
- Fighting for Henry: My Story of Cancer and Pregnancy
- Gestational Trophoblastic Disease
More Information:
Hope for Two
Cancer and Pregnancy Registry
Share your thoughts on this blog post on Cancer.Net's Facebook and Twitter.
Category:
Category
- Any -AnnouncementsCancer PreventionCancer ResearchCancer RiskFriends, Family, and CaregiversLiving With Cancer
Archives by Month:
Archives by Month:All EntriesDecember 2022November 2022October 2022September 2022August 2022July 2022June 2022May 2022April 2022March 2022February 2022January 2022December 2021November 2021October 2021September 2021August 2021July 2021June 2021May 2021April 2021March 2021February 2021January 2021December 2020November 2020October 2020September 2020August 2020July 2020June 2020May 2020April 2020March 2020February 2020January 2020December 2019November 2019October 2019September 2019August 2019July 2019June 2019May 2019April 2019March 2019February 2019January 2019December 2018November 2018October 2018September 2018August 2018July 2018June 2018May 2018April 2018March 2018February 2018January 2018December 2017November 2017October 2017September 2017August 2017July 2017June 2017May 2017April 2017March 2017February 2017January 2017December 2016November 2016October 2016September 2016August 2016July 2016June 2016May 2016April 2016March 2016February 2016January 2016December 2015November 2015October 2015September 2015August 2015July 2015June 2015May 2015April 2015March 2015February 2015January 2015December 2014November 2014October 2014September 2014August 2014July 2014June 2014May 2014April 2014March 2014February 2014January 2014December 2013Tags:
- breast cancer
- communication
- coping
- emotions
- español
- expert information
- meetings
- patient perspective
- podcast
- side effects
- survivorship
- tips
More
Cancer.
 Net Podcasts
Net Podcasts RSS Feed
Policies and Guidelines:
- Commenting Guidelines
- Guest Posting Policies
- Cancer.Net Terms and Conditions
Contact Us:
Email: [email protected]
ASCO's toll-free patient information line:
571-483-1780 or 888-651-3038
Recognition:
The Cancer.Net Blog was named one of Healthline's Best Cancer Blogs of 2020.
Timely. Trusted. Compassionate.
Comprehensive information for people with cancer, families, and caregivers, from the American Society of Clinical Oncology (ASCO), the voice of the world's oncology professionals.
Find a Cancer Doctor
treatment and outcome ➤ articles Oncogenotest
“Diagnosing cancer during pregnancy can be scary. The excitement of pregnancy is quickly replaced by fear of illness. The mother's attention then often shifts to the desire to protect the unborn child at all costs. Pregnant women with cancer often stop focusing on cancer and instead focus on getting well for their unborn child, as well as other children they may have, their partner, or other family members who may need them.
Pregnant women experience the disease differently than other people with cancer. You need to worry not only about how to fight for your life, but also about how the treatment can affect the life inside. A more pleasing difference is that once the treatment decision has been made and the initial shock of the diagnosis has passed, there is a realization that a baby should be expected at the end of the treatment. This is unlike any other award!
Breast cancer is the most common type of cancer diagnosed during pregnancy. In fact, approximately 7% to 10% of women who are diagnosed with breast cancer are under 40 years of age. And when cancer is diagnosed in women aged 30 and younger, 10% to 20% of cancers are detected either during pregnancy or within the first year after delivery.
As women delay marriage and childbearing due to career and other reasons, the average age of a woman's first pregnancy is now older than it was for previous generations. This shift is likely responsible for the increased incidence of cancer during pregnancy.
This shift is likely responsible for the increased incidence of cancer during pregnancy.
I have worked with women who were diagnosed with cancer during pregnancy. During my fellowship in fetal medicine and after completing my residency in obstetrics and gynecology, I met three women who helped set the course for my work and my life. One was diagnosed with melanoma on her thigh. She was offered to terminate the pregnancy. But, once she decided to continue with the pregnancy, it was difficult for her to find a surgeon willing to perform the extensive surgery that was required. Had she not been pregnant, she would have been able to avoid complete inguinal lymph node dissection. She could have had a nuclear test to pinpoint the cancerous lymph nodes in her groin, and the surgeon could have removed just those. She was worried about the upcoming surgery due to the possible side effect of lifelong leg swelling (lymphedema), which could affect her ability to bear a child. After talking with the doctors, during which the potential risks to the baby were explored, I was able to reassure them and the patient that performing this type of surgery during pregnancy is safe for the unborn baby and vital for the mother. The operation was successful, the daughter was healthy and was born at term. The placenta showed no signs of melanoma.
The operation was successful, the daughter was healthy and was born at term. The placenta showed no signs of melanoma.
Then I met a woman with Hodgkin's lymphoma who was 10 weeks pregnant. Her oncologist sent her to a nuclear medicine study to evaluate her heart function before she could start chemotherapy. But the radiologist did not conduct an examination until she terminated the pregnancy. Her oncologist also felt it would be best for her to terminate the pregnancy, but she didn't want to. I found several case reports showing that pregnant women with Hodgkin's lymphoma were no less likely to survive than non-pregnant women. How can I advise her to terminate the pregnancy if it would not likely increase her chances of survival? However, I didn't want her to save the pregnancy just to sacrifice herself, avoiding treatment at all costs, especially for such a curable cancer. I realized that we really need to convene an ethics committee at the hospital to discuss with the oncologist the possibility of safely administering chemotherapy in late pregnancy after the baby's organs have largely completed development.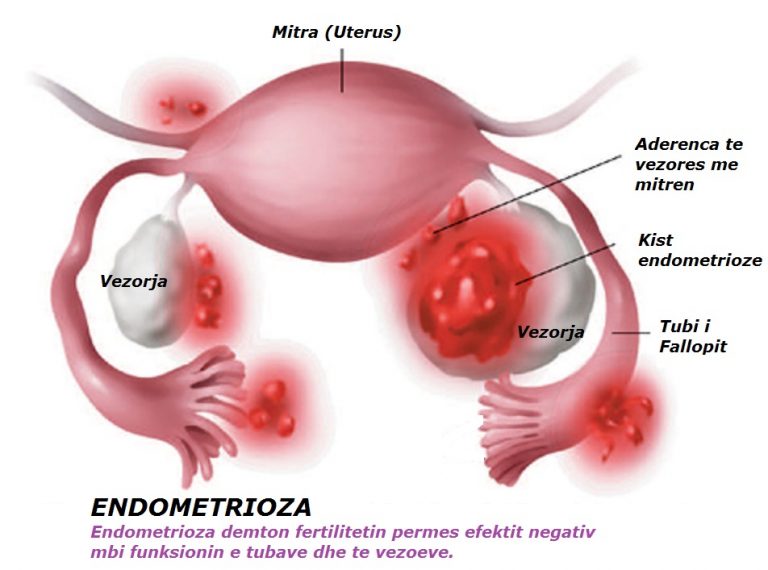 After looking for a way to save both mother and baby, I found a study that showed that a woman can safely receive chemotherapy in the second and third trimesters of pregnancy. The hospital ethics committee agreed, and my patient underwent chemotherapy. I had the honor of supervising the normal growth and development of her son; He just graduated from college!
After looking for a way to save both mother and baby, I found a study that showed that a woman can safely receive chemotherapy in the second and third trimesters of pregnancy. The hospital ethics committee agreed, and my patient underwent chemotherapy. I had the honor of supervising the normal growth and development of her son; He just graduated from college!
Due to little experience in diagnosing and treating pregnant women with cancer, no institution will be able to collect enough cases to truly know the safest way to treat cancer during pregnancy. It was then that I opened the Cancer and Pregnancy Registry, which is now an international collection of cancer cases in women and their children who were diagnosed with cancer during pregnancy. A third career-impacting patient was added to the registry after she was diagnosed with breast cancer. She named her son David because he "wrestled with Goliath", he went through chemotherapy before he was born. He is followed annually in the registry, as is his beautiful mother. Both are healthy and the job is done. David has just become a father and his mother a grandmother. I was told that this is not possible for children who have received chemotherapy in the womb. Women who are diagnosed with cancer during pregnancy can be treated and remain healthy enough to become mothers and even grandmothers!
Both are healthy and the job is done. David has just become a father and his mother a grandmother. I was told that this is not possible for children who have received chemotherapy in the womb. Women who are diagnosed with cancer during pregnancy can be treated and remain healthy enough to become mothers and even grandmothers!
Although it is normal for pregnant women with cancer to focus on the baby and not on themselves, know that the best way to have a healthy baby is to take care of yourself during pregnancy. Consider treating cancer during pregnancy if recommended by your doctor. Also take time for yourself, accept help from others, rest and eat when you can between treatments and during treatment. Know that you are not alone; Approximately 90,007 1 in 1,000 pregnant women 90,008 are diagnosed with cancer each year.
If you are being treated for cancer during pregnancy, be sure to talk to your doctor about how it might affect you and your baby. The most important question for those who are first diagnosed with cancer is: “How would I be treated if I was not pregnant?” The next question to ask should be: “Has this treatment been done before, and what were the risks and outcomes for children?”
Alice Cardonic, MD, is Professor of Obstetrics and Gynecology at the Cooper School of Medicine at Rowan University in Camden, New Jersey. Dr. Kardonik is closely following a cohort study of over 450 pregnant women with 1997 was diagnosed with cancer, including mothers with children beyond the postpartum period.
Dr. Kardonik is closely following a cohort study of over 450 pregnant women with 1997 was diagnosed with cancer, including mothers with children beyond the postpartum period.
https://www.cancer.net/blog/2021-01/what-do-when-you-are-diagnosed-with-cancer-during-pregnancy
diagnosis, safe treatment, pregnancy after cancer
Oncology during pregnancy is very rare - one case per 1000 pregnant women. In recent decades, this figure has begun to increase. More and more women in different countries of the world want to get a good education first, build a career. For this reason, childbearing is planned in 30-40 years, at a time when the risk of most cancers increases. For a long time, it was believed that the only right decision for pregnant women with cancer would be to have an abortion. Then undergo a full-fledged treatment for oncology, and then try to get pregnant again and give birth. Current scientific research refutes the hypothesis that the response to cancer therapy and prognosis in pregnant women is worse than in non-pregnant women. Each such case of detection of oncology should be considered by oncologists together with obstetricians with particular care in order to select the most effective treatment for the expectant mother without harming the fetus.
Each such case of detection of oncology should be considered by oncologists together with obstetricians with particular care in order to select the most effective treatment for the expectant mother without harming the fetus.
Incidence of cancer during pregnancy
Cancer most likely to be detected during pregnancy during pregnancy 1 :
- breast cancer 1:3000,
- cervical cancer 1:2000,
- ovarian cancer 1:10000,
- leukemia 1:75000,
- lymphoma 1:1000,
- melanoma 1:1000,
- colorectal cancer 1:13000.
Other types of oncology (tumors of the brain, stomach, endometrium, thyroid gland) can also be detected, but this happens even less frequently.
Diagnosis of cancer during pregnancy
Due to the high volume of diagnostic examinations, cervical cancer is most easily detected during pregnancy, even at an early stage. When examined in a gynecological chair, the doctor will suspect a disease, prescribe additional examination methods, and refer narrow specialists for consultation. Other malignant neoplasms are more difficult to diagnose by those methods that are included in the list for pregnant women (examination of the vagina in the mirrors, two-handed examination, clinical, biochemical, serological, immunological blood tests, examinations for TORCH infection, ultrasound, ECG, CTG, consultation of narrow specialists - an endocrinologist, genetics , neurologist, ophthalmologist, etc.).
Other malignant neoplasms are more difficult to diagnose by those methods that are included in the list for pregnant women (examination of the vagina in the mirrors, two-handed examination, clinical, biochemical, serological, immunological blood tests, examinations for TORCH infection, ultrasound, ECG, CTG, consultation of narrow specialists - an endocrinologist, genetics , neurologist, ophthalmologist, etc.).
The complexity of diagnosis lies in the fact that the symptoms of oncological diseases are often similar to changes in the state of the body during pregnancy 4 . Women feel that their breasts have become ill, increased in size, its density has changed, but they think that it should be so. Non-core specialists can also miss the symptoms of a tumor at an early stage, attributing everything to changes in the body during pregnancy.
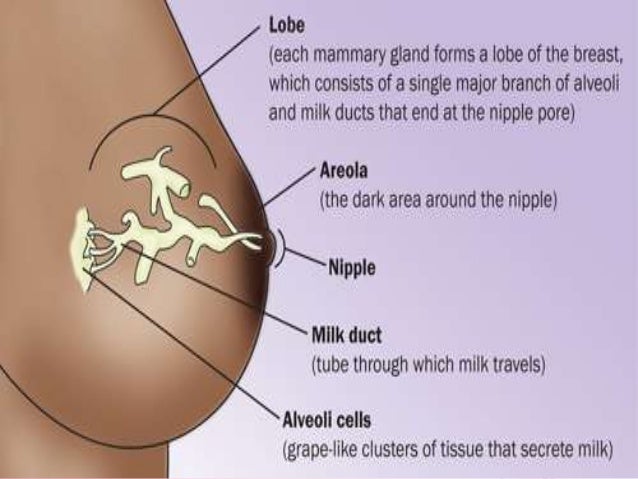
Breast changes during pregnancy. The process is characterized by engorgement, soreness of the mammary glands, changes in density, discharge from the nipples. Characteristic symptoms in oncology: breast enlargement, soreness, change in consistency, fever
Characteristic symptoms in oncology: breast enlargement, soreness, change in consistency, fever
Table comparing signs of oncological diseases with physiological manifestations of pregnancy Conditions of a pregnant woman Amenorrhea, absence or alteration of menstruation due to cancer intoxication Amenorrhea, delayed menstruation due to pregnancy Fatigue, weakness, change in appetite, nausea Toxicosis, nausea, malaise, drowsiness Aches in bones, muscles, joints Pain in joints, lower back Skin discoloration, darkening, redness, peeling Hyperpigmentation of the line from the navel to the pubis, skin of the face, halo, the appearance of stretch marks Breast enlargement, tenderness, change in texture, fever Engorgement, breast tenderness, change in firmness, nipple discharge Bladder dysfunction, stool disorder Urinary frequency, indigestion
Due to the similarity of symptoms, cancer during pregnancy begins to develop insidiously. Cancer affects the health of a pregnant woman, causing miscarriage in the most severe cases. Therefore, if a pregnant woman is concerned about her condition, it is better to consult a doctor, get a consultation, undergo additional examinations than waste time.
Cancer affects the health of a pregnant woman, causing miscarriage in the most severe cases. Therefore, if a pregnant woman is concerned about her condition, it is better to consult a doctor, get a consultation, undergo additional examinations than waste time.
The safety of cancer diagnostic methods for the fetus
The diagnostic arsenal of doctors is reduced: diagnostic methods that can harm the health of the child or mother are excluded. X-ray exposure is dangerous for the health of the baby, its use is associated with the risk of spontaneous miscarriages, the development of malformations of internal organs, mental retardation, microcephaly or leukemia 1 . Such side effects occur as a result of cell trauma. The degree of damage will depend on the radiation dose and trimester: the smaller the fetus, the more serious the consequences can be. Therefore, all methods based on X-ray radiation are excluded (plain radiography, isotope scanning, contrast-enhanced images with barium enemas, computed tomography, intravenous urography, positron emission tomography) 1. 4 .
4 .
Chest X-ray may be used provided the abdomen is protected. Methods of magnetic resonance imaging, ultrasound, mammography are considered relatively safe for a child, even in the first trimester of pregnancy. There are surgical methods that do not pose a danger to the fetus or mother.
MRI during pregnancy
Colposcopy and Pap tests used to diagnose cervical cancer do not cause negative pregnancy outcomes. Targeted biopsy carries the risk of bleeding and preterm birth. Therefore, before carrying out this procedure, an expert commission is assembled to assess the risks, as well as determine the need for a biopsy in each specific case 5 .
Performing a Pap test
The effectiveness of methods for diagnosing cancer during pregnancy
The position of a woman can affect the result of some examinations and tests. So it is necessary to carefully interpret the clinical and biochemical blood tests. The level of some tumor markers may change not only due to the existing tumor, but also due to the growth and differentiation (complication, specialization) of fetal cells 1 . Mammography may become less informative: a decrease in the sensitivity of this method is associated with a change in the radiographic density of breast tissue.
The level of some tumor markers may change not only due to the existing tumor, but also due to the growth and differentiation (complication, specialization) of fetal cells 1 . Mammography may become less informative: a decrease in the sensitivity of this method is associated with a change in the radiographic density of breast tissue.
Cancer in pregnancy, treatment
Pregnancy in cancer significantly influences the choice of treatment tactics. When oncology is detected, the attending physician uses aggressive therapies: radiation, chemotherapy, radical surgery, immunotherapy, and targeted therapy. Most of these methods will adversely affect the health of the child. Women are offered to have an abortion, but there are other options for solving this problem.
Surgery
Surgical removal of the tumor may be done during pregnancy. If the size of the neoplasm is small, then intervention in the mother's body will not affect the condition of the fetus, regardless of the trimester. But doctors try to postpone the operation at least until the beginning of the second trimester, this is due to the risks of spontaneous miscarriage from the administered anesthesia 1,2 . During the operation (especially in the abdomen), additional monitoring of the condition of the fetus and mother is carried out. Surgeons supervise:
But doctors try to postpone the operation at least until the beginning of the second trimester, this is due to the risks of spontaneous miscarriage from the administered anesthesia 1,2 . During the operation (especially in the abdomen), additional monitoring of the condition of the fetus and mother is carried out. Surgeons supervise:
- blood gases (oxygen, carbon dioxide),
- maternal pulse, fetus pulse,
- respiratory rate,
- pressure.
The patient is placed on her side, avoiding the supine position, this prevents blood flow disturbance due to pressure on the inferior vena cava of the enlarged uterine body 1 . Surgery for some types of cancer is delayed and performed after delivery.
Comparison of lateral (right) and supine (left) positions in a pregnant woman. The lateral position prevents blood flow disturbance due to pressure on the inferior vena cava of the enlarged uterine body
Radiation therapy
Radiation therapy can be used after the second trimester in exceptional cases. Irradiation has a teratogenic effect (impairs normal embryonic development), which can greatly harm the baby in the early stages, since the organs are not fully formed. Some doctors believe that with tumors in the supraphrenic segment (cancer of the brain, thyroid gland, breast), it is possible to conduct radiation therapy in the first trimester. During this period, radiation protection will be reliable due to the remote location of the still small uterus 1 .
Irradiation has a teratogenic effect (impairs normal embryonic development), which can greatly harm the baby in the early stages, since the organs are not fully formed. Some doctors believe that with tumors in the supraphrenic segment (cancer of the brain, thyroid gland, breast), it is possible to conduct radiation therapy in the first trimester. During this period, radiation protection will be reliable due to the remote location of the still small uterus 1 .
Chemotherapy
Chemotherapy has an antineoplastic (cytostatic) effect, which stops the growth of tumor cells. But fetal cells exposed to chemotherapy drugs can slow down their growth and reproduction. This will cause a delay in intrauterine development of the child. Therefore, doctors choose high molecular weight drugs that cannot pass through the placental barrier without endangering the baby. Chemotherapy is used no earlier than 14 weeks of gestation 1,2,4 .
- If the tumor is too advanced, we make some compromises with the patient's refusal to terminate the pregnancy and administer chemotherapy during the pregnancy. After 14 weeks and up to 31-32 weeks it is safe, do not be afraid of this method of treatment. 3 weeks before delivery, chemotherapy is stopped. In locally advanced cervical and ovarian cancers, chemotherapy is more commonly used than surgery. But it is important to emphasize that this treatment outside of pregnancy would be considered suboptimal, so it is used only in cases where patients refuse to terminate the pregnancy, says Nosov. Vladimir Borisovich - oncogynecologist, candidate of medical sciences, head of the clinic of obstetrics, gynecology and oncogynecology of EMC (European Medical Center).
After 14 weeks and up to 31-32 weeks it is safe, do not be afraid of this method of treatment. 3 weeks before delivery, chemotherapy is stopped. In locally advanced cervical and ovarian cancers, chemotherapy is more commonly used than surgery. But it is important to emphasize that this treatment outside of pregnancy would be considered suboptimal, so it is used only in cases where patients refuse to terminate the pregnancy, says Nosov. Vladimir Borisovich - oncogynecologist, candidate of medical sciences, head of the clinic of obstetrics, gynecology and oncogynecology of EMC (European Medical Center).
Other methods
Immunotherapy is not considered a treatment for cancer during pregnancy, despite proven efficacy in the treatment of colorectal cancer, ovarian cancer and breast cancer metastases. Monoclonal antibodies cross the placental barrier and can cause severe fetal malformations 1 .
The use of targeted therapy is still being studied, so there is no reliable data on the effect on the fetus.
Features of cancer during pregnancy
Cervical cancer during pregnancy
The management of a patient with oncology during this period will depend on the type of cancer, the size of the tumor, the spread of cancer in the lymphatic system and the duration of the situation. In the long term, at the zero and first stages, doctors choose expectant tactics, since the tumor grows slowly 5 . A few weeks after the birth of the child, treatment can begin. Available methods in this case are conization, trachelectomy and hysterectomy. In the later stages, the patient and the doctor should discuss whether it is advisable to risk the mother's health or whether it is better to have an abortion. If the pregnancy persists, delivery is by caesarean section once the fetus is mature enough to survive outside the uterus. Sometimes doctors may prescribe chemotherapy during the second and third trimester to stop the tumor from growing. Advanced stages of cancer are subject to immediate treatment.
Cervical cancer
Breast cancer during pregnancy
The volume of manipulations in the treatment of breast cancer during pregnancy depends on the stage of the tumor. Surgeons successfully perform radical mastectomy (removal of the breast, pectoral muscles and regional lymph nodes), but treatment cannot be limited to one operation. For a complete recovery with minimal risk of relapse, it is necessary to prescribe chemotherapy, radiation therapy, hormones. But these methods can not always be applied in the presence of a fetus in the womb 2 . Breast cancer is very aggressive, delaying treatment until delivery can be life threatening for the patient 5 . Recent scientific studies have shown that the use of chemotherapy drugs in the second and third trimester does not cause serious disturbances in the development of the child, but can cause premature birth.
Breast Cancer
Ovarian Cancer and Pregnancy
Ovarian tumors may go unnoticed after 12 weeks of gestation, they extend beyond the pelvis and can no longer be palpated. Late-stage ovarian cancer can be fatal before labor begins5. These patients need to start treatment as soon as possible. Therefore, as soon as the child becomes mature enough for extrauterine life, delivery is carried out by caesarean section and the possibility of simultaneous oophorectomy and hysterectomy (radical removal of the uterus, ligaments, appendages) is evaluated.
Late-stage ovarian cancer can be fatal before labor begins5. These patients need to start treatment as soon as possible. Therefore, as soon as the child becomes mature enough for extrauterine life, delivery is carried out by caesarean section and the possibility of simultaneous oophorectomy and hysterectomy (radical removal of the uterus, ligaments, appendages) is evaluated.
Ovarian cancer
Hodgkin's lymphoma and pregnancy
The choice of treatment for lymphoma depends on the stage, rate of growth of the tumor and duration of pregnancy. Treatment of lymphoma try to lead after the end of the first trimester. If a woman decides to keep the embryo, she is given chemotherapy with mandatory monitoring of the fetus and the response of the tumor to therapy. If the disease was diagnosed in the second half of the term, expectant tactics are taken until the birth of the child 3 .
Melanoma during pregnancy
Melanoma treatment will depend on the stage of the cancer. In the first stages, surgical excision is performed. With a widespread process and rapid growth of the tumor, chemotherapy is used. The danger of this type of oncology lies in metastases, tumor cells can spread and grow into the placenta 6 . Five out of six embryos in this case die 7 .
In the first stages, surgical excision is performed. With a widespread process and rapid growth of the tumor, chemotherapy is used. The danger of this type of oncology lies in metastases, tumor cells can spread and grow into the placenta 6 . Five out of six embryos in this case die 7 .
Can late pregnancy cause cancer?
Pregnancy does not provoke the appearance of cancer in the body, and most often does not accelerate tumor growth. The exception is melanoma, the growth of which can provoke changes in the hormonal background 4 .
Pregnancy after cancer
Many women who are diagnosed with cancer at a young age are interested in the possibility of becoming pregnant after cancer treatment. Radical types of surgical intervention (hysterectomy, hysterectomy, oophorectomy) suggest the complete end of fertility, a woman herself will no longer be able to become pregnant and give birth to children. In such cases, consider surrogate motherhood with a donor egg.
Chemotherapy drugs damage the ovaries, reducing their reproductive potential. After such treatment, menopause may occur several years earlier than usual. Radiation therapy of the abdomen or pelvis can lead to scarring on the body of the uterus, depletion of the ovaries, changes in the characteristics of the endometrium. Changes in the work of the pituitary gland, which regulates ovulation, are possible during brain irradiation, which will make attempts to get pregnant useless. The reproductive endocrinologist is engaged in determining the female reproductive function after oncology treatment. A diagnosed cancer does not make pregnancy impossible.
- The possibility of pregnancy can be considered after at least two years from the end of the course of treatment in stable remission. The ideal waiting period is 5 years, but not everyone can wait that long. We do not recommend planning a pregnancy on your own. To decide on a possible pregnancy, a council is convened, which decides whether a break can be made from taking maintenance drugs, such as tamoxifen. After delivery, tamoxifen is resumed immediately, lactation is contraindicated for such women on the background of the drug, - comments Vladimir Borisovich.
After delivery, tamoxifen is resumed immediately, lactation is contraindicated for such women on the background of the drug, - comments Vladimir Borisovich.
To sum it up, cancer and pregnancy are diagnosed together very rarely, it is not always a reason to have an abortion. Modern methods of diagnostics and treatment give a chance to give birth to a healthy child, while curing oncology. Pregnancy imposes restrictions on diagnostic and therapeutic procedures. So it is necessary to almost completely exclude radiographic diagnostic methods and radiation therapy. The use of these methods is associated with a high risk of spontaneous miscarriages, the occurrence of serious malformations. Chemotherapy is given only after the third month to avoid the expected negative effects on the fetus. Surgical operations are possible with a competent approach of the anesthesiologist, monitoring the condition of the mother and fetus. Each type of cancer makes its own changes in the tactics of doctors, but all have similar principles.