Non epidural pain relief labor
Childbirth - pain relief options
Actions for this page
Summary
Read the full fact sheet- Childbirth is usually a painful experience.
- There is a range of options for pain relief in labour including non-medical techniques and medical pain relief options such as nitrous oxide, pethidine and epidural anaesthesia.
- Particularly if you are having your first baby, consider all options and be flexible.
- If you planned to give birth without using pain relief, but find the labour pains are overwhelming, don’t be reluctant to ask the doctor, nurse or midwife for pain relief.
Labour and childbirth is usually a painful experience and women vary in their response to it. Some women are keen to avoid drugs or other medical interventions while others are happy to consider all available options. For a woman having her first baby, the experience of labour (and her reaction to it) is unpredictable.
For this reason, it is a good idea to be aware of the options for pain relief that are available and to know something about the different methods. You may have a plan for how you hope to manage your labour, but it is best to be prepared to be flexible.
Non-medical pain relief options for childbirth
Research suggests that adequate preparation can help to reduce pain or at least modify the perception of pain and reduce anxiety, which can help you to better cope with labour. There are several non-drug pain relief options:
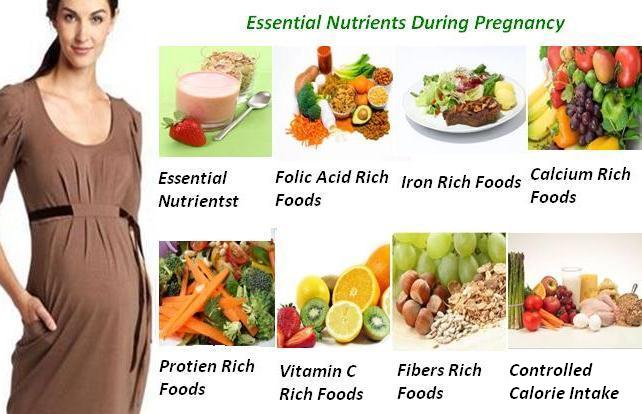
- Being in good physical condition is important. Exercise gently and regularly throughout your pregnancy, avoid cigarettes and alcohol, and eat a healthy, balanced diet.
- Knowing what to expect during the various stages of labour can help reduce anxiety. Antenatal classes are strongly recommended.
- Breathing techniques may help you to ‘ride the waves’ of each contraction.
- Constant, close support from your partner (or a trusted friend or loved one) for the duration of labour can reduce anxiety.

- Using distractions like music can help to take your mind off the pain.
- Hot or cold packs, massage, a warm shower or immersion in a warm bath, and keeping active may all be helpful.
- Hypnosis, acupuncture and acupressure are areas in which there has been little research but these may be considered also.
Transcutaneous electrical nerve stimulation (TENS)
TENS is a technique in which nerves in the lower back are stimulated using a small hand-held device controlled by the woman. It has no known side effects for mother or baby and many women find it helpful either alone or in combination with other methods of pain relief.
Medical pain relief options for childbirth
The three main medical pain-relieving options for labour include:
- Nitrous oxide
- Pethidine
- Epidural anaesthesia.
Nitrous oxide
Nitrous oxide, known as ‘laughing gas’, is mixed with oxygen and administered to the mother through a face mask or a tube held in the mouth. The gas takes a few seconds to work, so it is important to breathe from the mask as soon as a contraction starts.
The gas takes a few seconds to work, so it is important to breathe from the mask as soon as a contraction starts.
Nitrous oxide doesn’t stop the pain entirely, but takes the ‘edge’ off the intensity of each contraction. Many women prefer nitrous oxide because it allows them direct control – you can hold the mask yourself and take deep breaths whenever you feel the need.
Nitrous oxide doesn’t interfere with contractions and it doesn’t linger in either the woman’s or the baby’s body.
Possible problems with using nitrous oxide include:
- Nausea and vomiting
- Confusion and disorientation
- Claustrophobic sensations from the face mask
- Lack of pain relief – in some cases, nitrous oxide doesn’t offer any pain relief at all (this applies to around one-third of women).
Pethidine
Pethidine is a strong pain reliever (related to morphine and heroin), usually injected directly into a muscle in the buttock. It may also be administered intravenously (directly into a vein).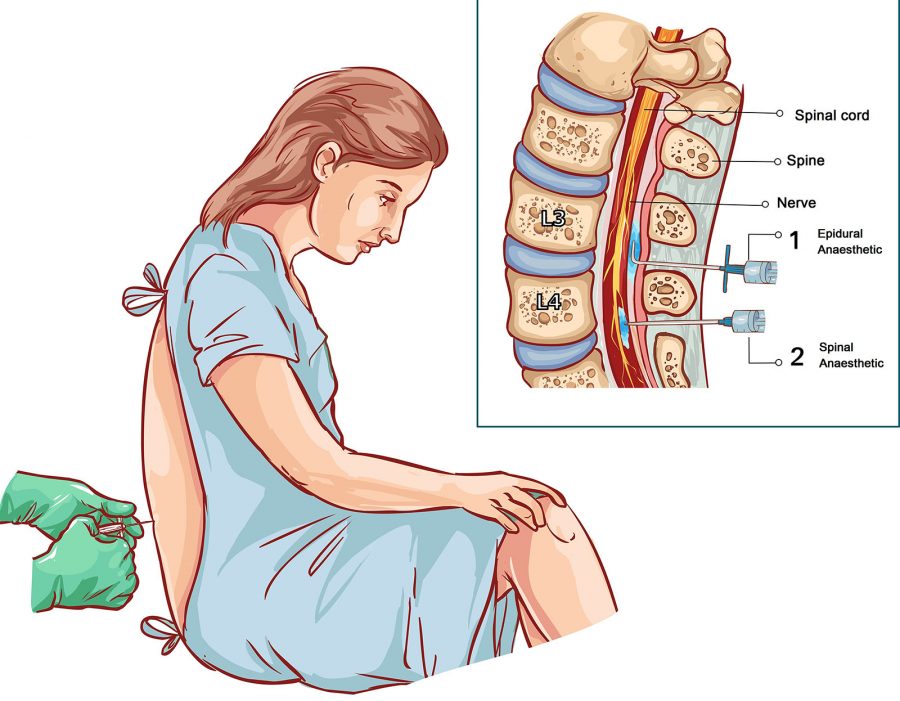 Depending on various factors, the effect of pethidine can last anywhere from two to four hours. Pethidine can make you feel sick, so anti-nausea medications are usually administered at the same time.
Depending on various factors, the effect of pethidine can last anywhere from two to four hours. Pethidine can make you feel sick, so anti-nausea medications are usually administered at the same time.
Possible problems with pethidine for the mother include:
- Giddiness and nausea
- Disorientation and altered perception
- Respiratory depression (reduced breathing)
- Lack of pain relief, in some cases.
Possible problems with pethidine for the baby include:
- The unborn baby is exposed to the drug via the umbilical cord and may experience respiratory depression at birth, particularly if several doses are given or the baby delivers soon after a pethidine injection. This effect can be reversed by an injection given to the baby.
- The baby’s sucking reflex may also be depressed, as well as other normal reflexes. Debate persists over the effects of pethidine on newborns.
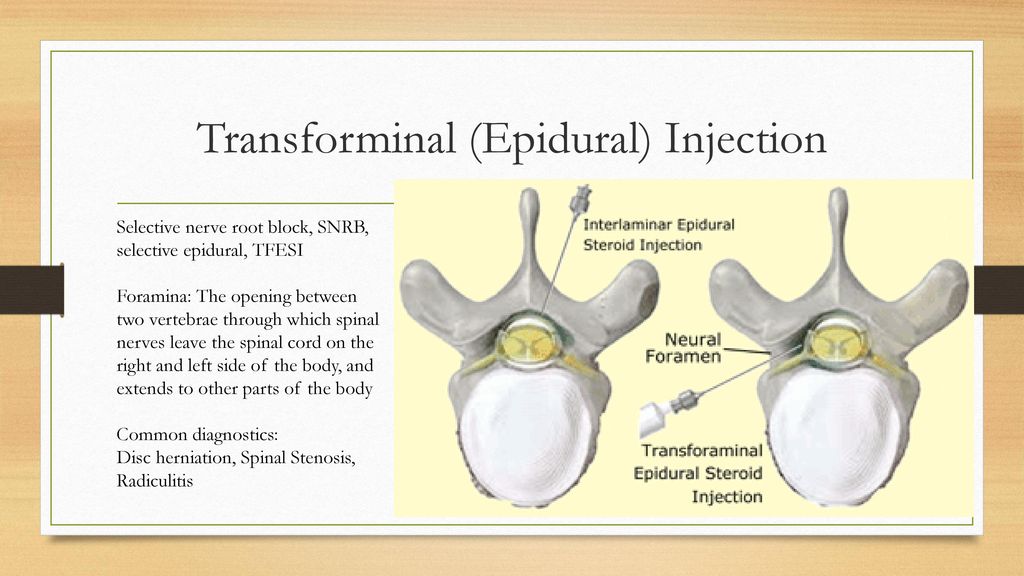
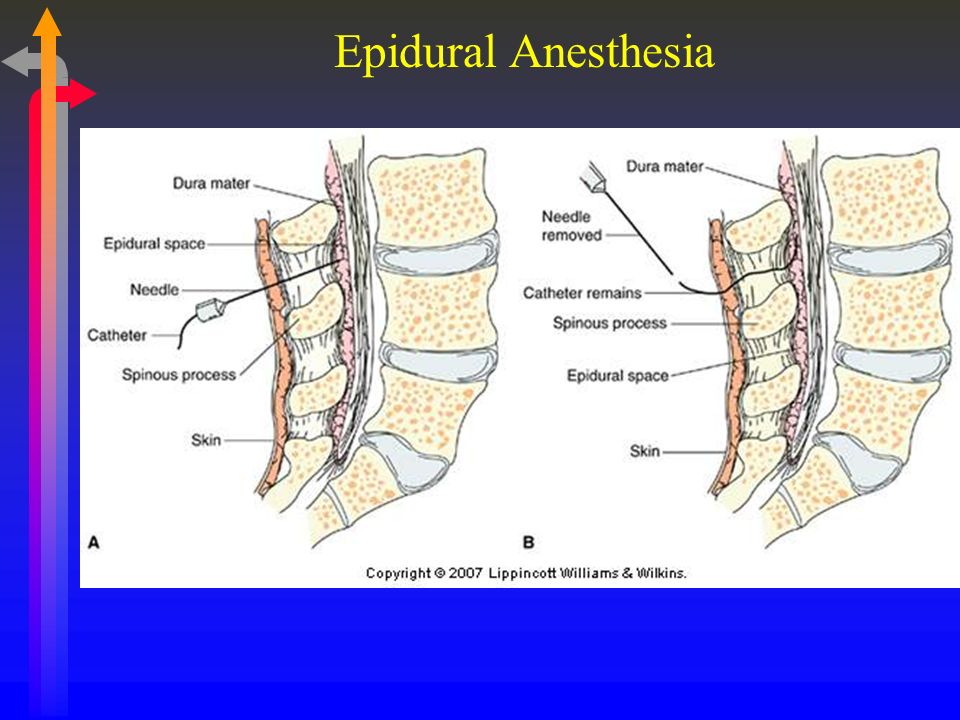
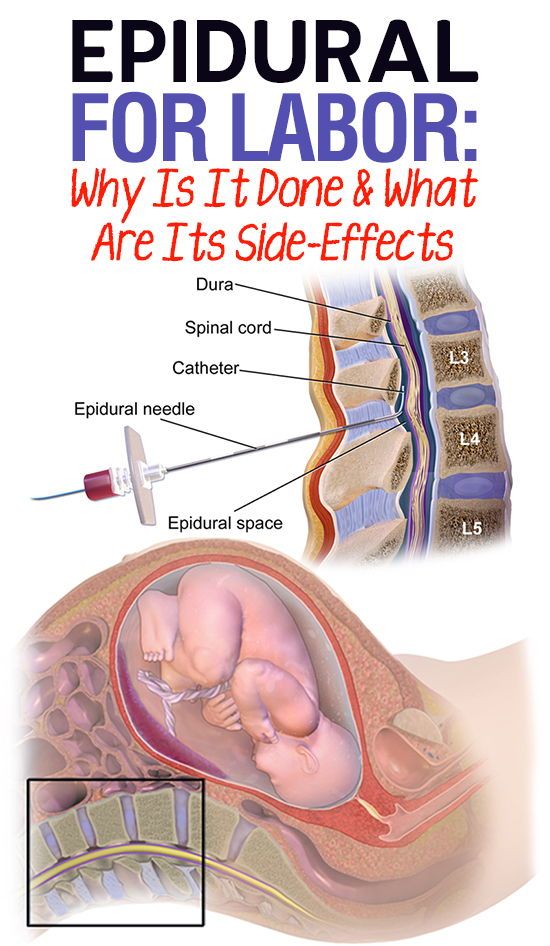
Epidural anaesthesia
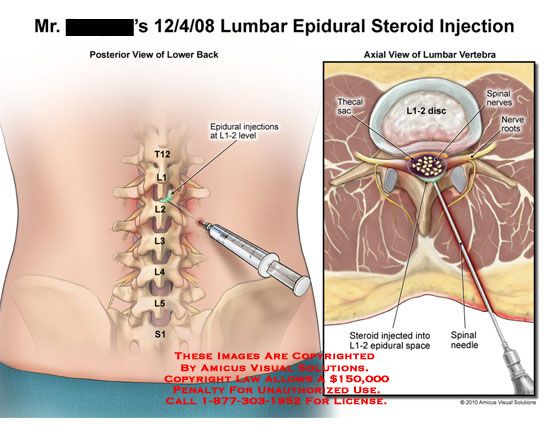
Epidural injections are the most effective pain relief available.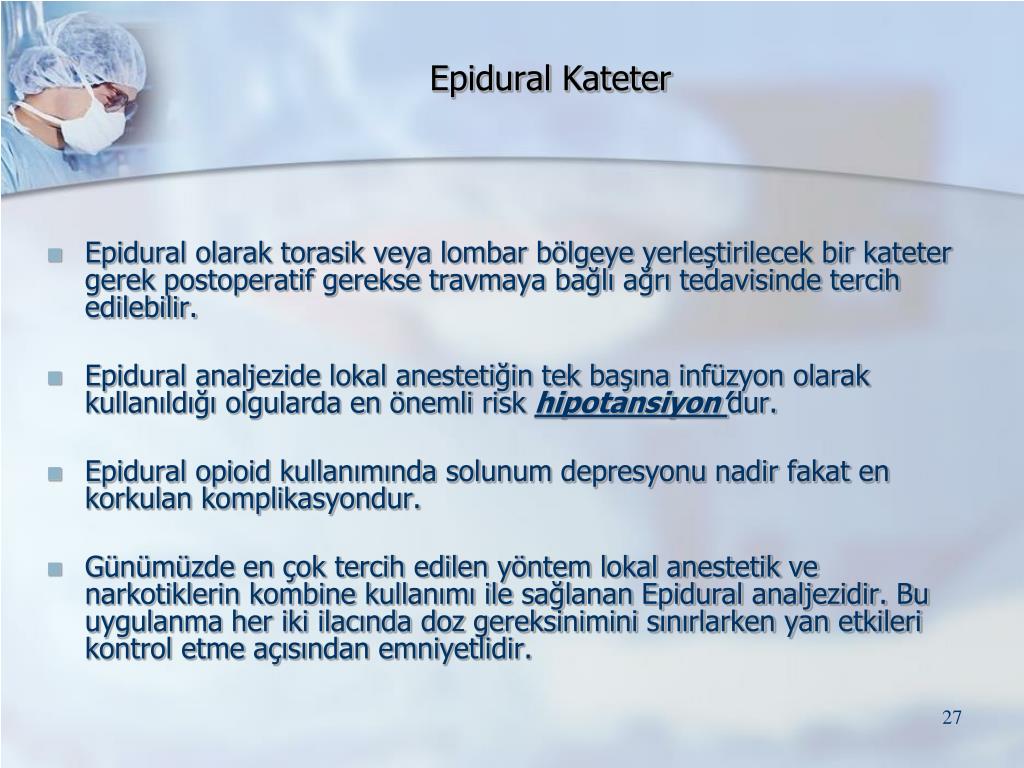 They are used for vaginal births and also for caesarean sections, because they allow the mother to stay awake and alert during the baby’s birth. Anaesthetic is injected into the lining of the spinal cord through the back, which makes the mother feel numb from the waist down. Your baby’s heart rate will be monitored continuously.
They are used for vaginal births and also for caesarean sections, because they allow the mother to stay awake and alert during the baby’s birth. Anaesthetic is injected into the lining of the spinal cord through the back, which makes the mother feel numb from the waist down. Your baby’s heart rate will be monitored continuously.
Possible side effects and complications of epidural anaesthesia include:
- The anaesthesia may not be complete and you may still experience some pain. This may require the procedure to be repeated.
- After the epidural has been inserted, your blood pressure may drop, causing you to feel faint and nauseated. This may also cause stress to your baby. This is treated by giving intravenous fluid.
- An epidural often causes some muscle weakness in the legs, so women who have had an epidural anaesthetic may be confined to bed.
- The lack of sensation in the lower body means that you will not be able to tell when you need to urinate.
 A urinary catheter will be inserted in most cases.
A urinary catheter will be inserted in most cases. - Epidurals can lengthen the second stage of labour.
- The likelihood of having a normal vaginal delivery is reduced.
- If you are unable to push effectively, due to altered sensation and reduced muscle strength, the baby may have to be delivered by forceps or vacuum cup.
- Around one per cent of women experience headache immediately following the procedure.
- Some women experience itchiness after having an epidural. This can usually be effectively treated using antihistamines.
- Some women experience pain or tenderness where the epidural was injected.
- Around one in 550 women experience ongoing patches of numbness on the back near the injection site.
- Very rare complications include infection, blood clots and difficulty breathing.
An epidural does not:
- Increase the length of the first stage of labour
- Increase the likelihood of a caesarean section
- Cause long-term backache.
Where to get help
- Your doctor
- Obstetrician
- Midwife
Things to remember
- Childbirth is usually a painful experience.
- There is a range of options for pain relief in labour including non-medical techniques and medical pain relief options such as nitrous oxide, pethidine and epidural anaesthesia.
- Particularly if you are having your first baby, consider all options and be flexible.
- If you planned to give birth without using pain relief, but find the labour pains are overwhelming, don’t be reluctant to ask the doctor, nurse or midwife for pain relief.
- Continuous support for women during childbirth, 2007, Cochrane Database of Systematic Reviews, Issue 2. More information here.
- Using water for pain relief during labour, 2007, The Royal Women’s Hospital, Melbourne.
- Epidural information, 2013, The Royal Women’s Hospital, Melbourne.
- Pain relief during labour and birth, Women’s and Children’s Health Network, Department of Health, South Australian Government.
 More information here.
More information here. - Epidural anaesthesia – side effects, 2011, NHS Choices, UK. More information here.
- Epidural anaesthesia, NHS, UK. More information here.
This page has been produced in consultation with and approved by:
This page has been produced in consultation with and approved by:
Give feedback about this page
Was this page helpful?
More information
Content disclaimer
Content on this website is provided for information purposes only. Information about a therapy, service, product or treatment does not in any way endorse or support such therapy, service, product or treatment and is not intended to replace advice from your doctor or other registered health professional. The information and materials contained on this website are not intended to constitute a comprehensive guide concerning all aspects of the therapy, product or treatment described on the website.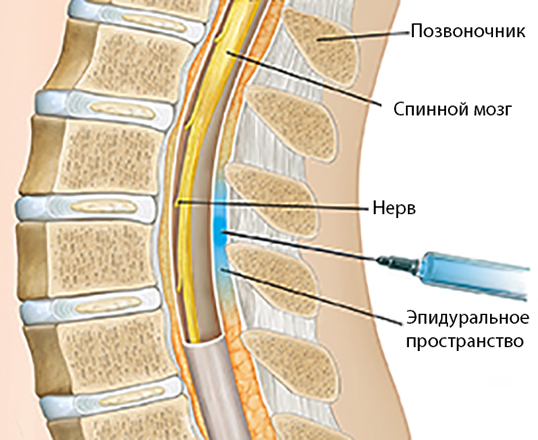 All users are urged to always seek advice from a registered health care professional for diagnosis and answers to their medical questions and to ascertain whether the particular therapy, service, product or treatment described on the website is suitable in their circumstances. The State of Victoria and the Department of Health shall not bear any liability for reliance by any user on the materials contained on this website.
All users are urged to always seek advice from a registered health care professional for diagnosis and answers to their medical questions and to ascertain whether the particular therapy, service, product or treatment described on the website is suitable in their circumstances. The State of Victoria and the Department of Health shall not bear any liability for reliance by any user on the materials contained on this website.
Reviewed on: 31-08-2014
Options for pain management during labor & delivery
As your new baby’s arrival gets closer, you’re doing all you can to prepare. You’re packing your overnight bag. You know the shortest route to the hospital. You know the signs of labor to watch for.
But chances are there’s at least one more big thing on your mind: How you’ll handle pain during labor and delivery.
Some people want to avoid pain medicine unless it becomes absolutely necessary. Others plan for an epidural, and some want to just wait and see how they feel.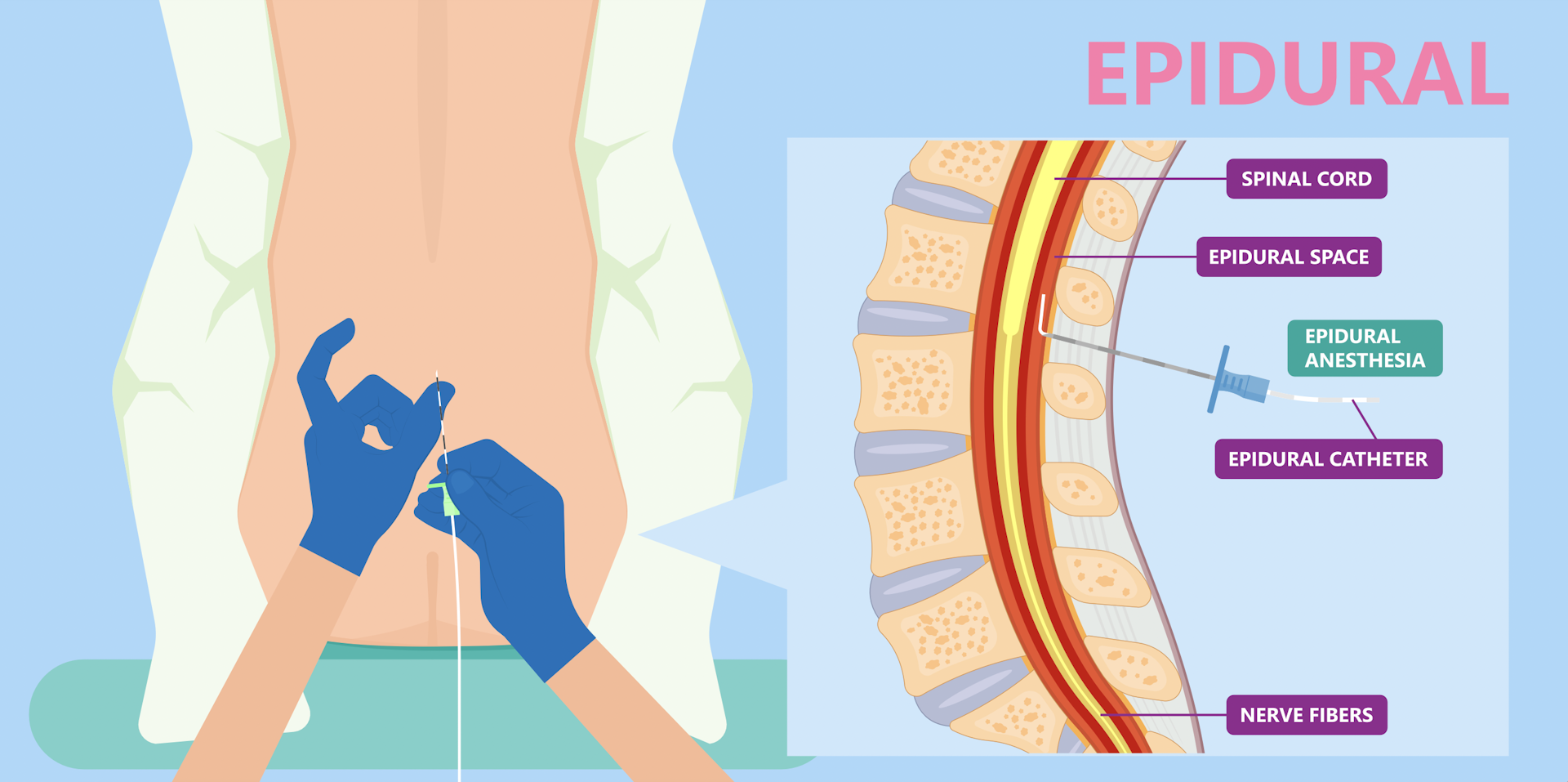
However, even if your birth plan already outlines how you want to deal with labor pains, or you’ve given birth before, you’re still thinking about what this experience will be like. And because every birth is unique, it’s important to know all your pain management options so you feel more comfortable and confident when your contractions begin.
Below, we provide an overview of common ways to manage labor pain, from medications to natural pain relief techniques.
First, how painful is childbirth? (And how much labor pain can you actually handle?)
It’s true. Childbirth is painful. How painful? There isn’t a standard childbirth pain scale because pain is subjective – and it’s also manageable. Your birth experience will be unique, so what you feel will be unique, too.
Braxton-Hicks contractions – those “practice” contractions as your body prepares for the big day – can give you a little taste of what the beginning stages of labor may feel like. You may feel tightening in your lower abdomen that comes and goes, or you may feel something similar to period cramps.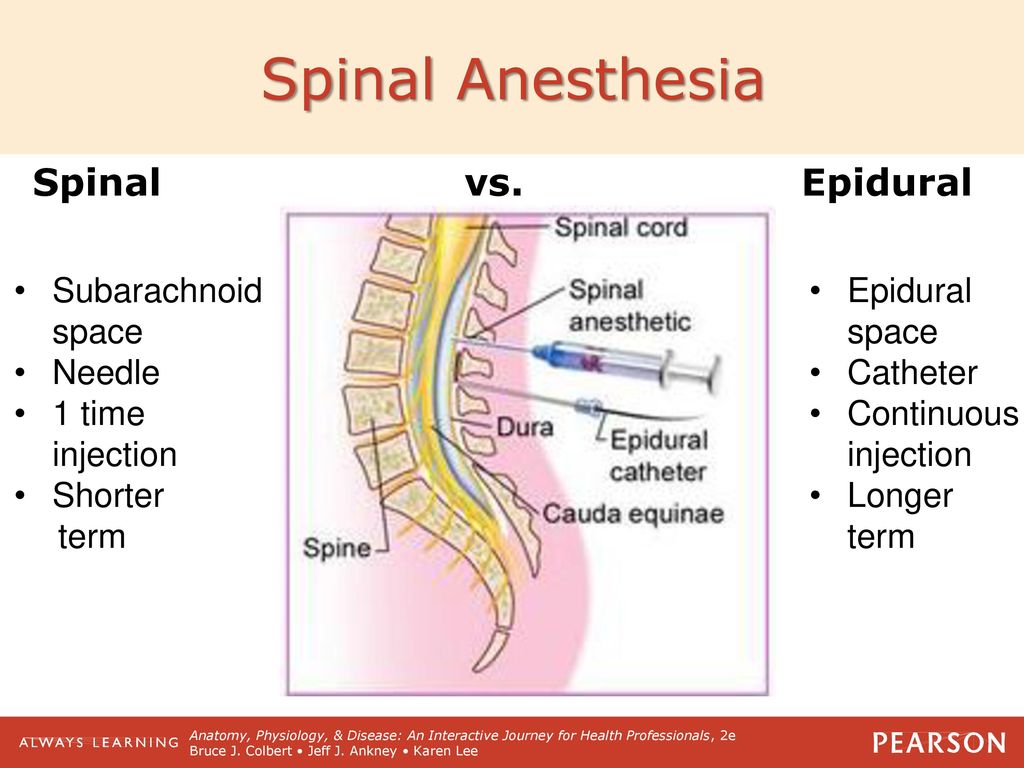 A strong contraction pain may even take your breath away.
A strong contraction pain may even take your breath away.
When real labor contractions start, intensity, frequency and regularity increase – as does the discomfort. And as labor progresses, the sensations you feel can continue to intensify in a range of ways. But the pain you experience (and what you feel like you can handle) on delivery day will greatly depend on how your labor goes and the pain management methods you’ve chosen.
Knowing your pain management options during labor and delivery
You may think your only pain management options are an epidural or natural birth. But there are a range of medical and natural pain relief options today – many that can be used together.
Depending on where you choose to give birth, your options can vary. For example, epidurals are not typically available at freestanding birth centers. But knowing your options can help you finalize your birth wishes and decide on where to have your baby.
Pain medications for labor pains
There are several medical pain management options during labor and delivery. They all work differently, but they’re all designed to provide noticeable pain relief.
They all work differently, but they’re all designed to provide noticeable pain relief.
Epidurals
Epidurals are one of the most common pain medications used during labor and delivery, because they’re usually the most effective way to relieve pain.
An epidural helps numb your lower body. You’ll still feel pressure and some discomfort, but more extreme labor pains are calmed. It’s delivered as a continuous flow or a repeatable dose through a small catheter placed in your lower back, which means the dosage can be adjusted as needed.
But because an epidural numbs your lower body, it’s important to know that your mobility will be limited. Specifically, you won’t be able to safely stand or walk until the medication wears off.
Also, if you arrive at the hospital and you’re already dilated to eight or more centimeters, you might be too far along to receive an epidural. And like any medication, there is a risk of side effects such as a reaction to the medication, headache or a drop in blood pressure.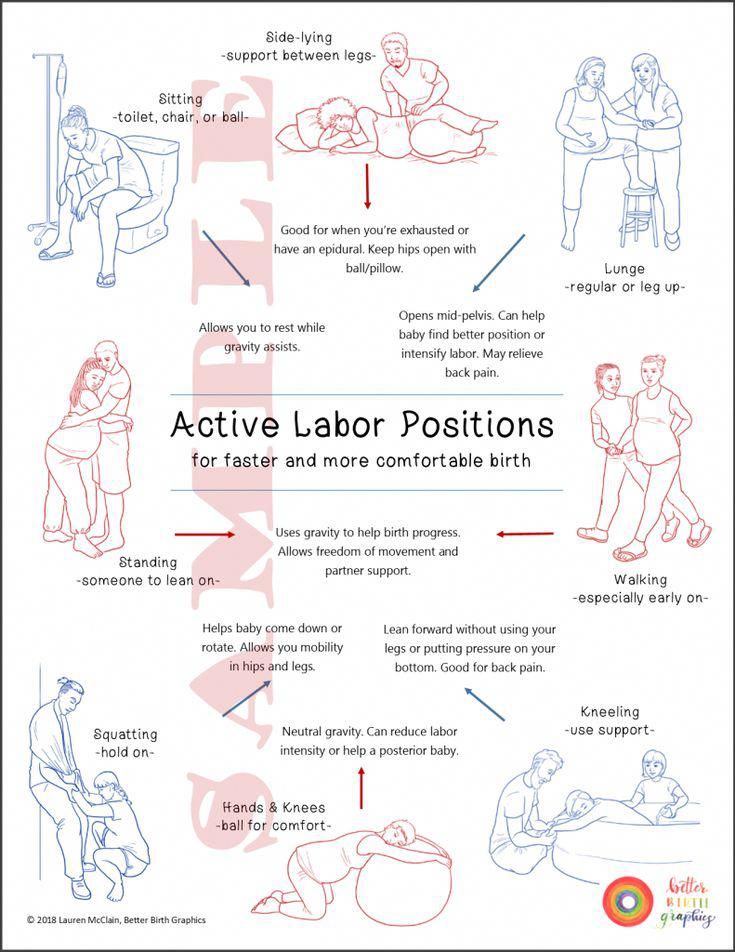 Your care team will be able to answer any questions you have as well as take steps to minimize any potential issues.
Your care team will be able to answer any questions you have as well as take steps to minimize any potential issues.
Nitrous oxide
Nitrous oxide – which is often called laughing gas or nitrous – is a form of mild sedation that you inhale into your lungs through a mask. It’s a popular option for those who hope to use little to no pain medication during childbirth.
Nitrous oxide can help take the edge off pain temporarily as well as help you relax. In fact, many find the gas helps reduce their pain and fear, which can make the entire process less stressful. Plus, nitrous oxide is safe for your baby and has not been shown to affect breastfeeding.
The gas’s effects can come and go quickly, but you’ll be given control of the mask so you can use it as needed. That said, it’s important to know that too much nitrous oxide may make you a little drowsy, dizzy or nauseous at times. Usually taking a break from breathing the gas helps those side effects go away on their own.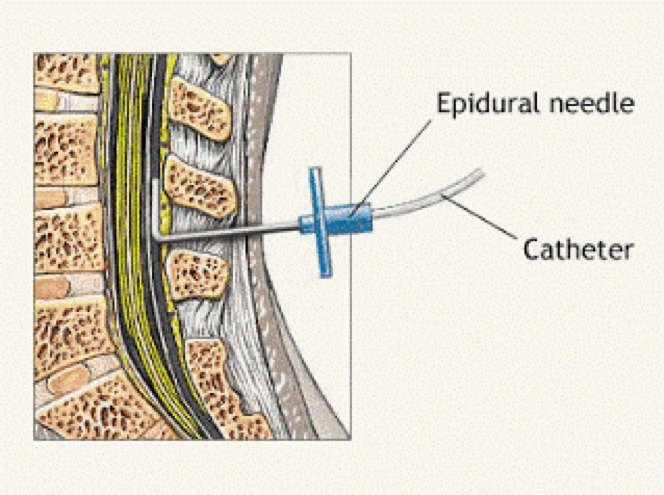
Opioids
Opioids like fentanyl can help you relax and take the edge off your pain. However, opioids aren’t used that often, but when they are, it’s typically only used during early labor. If you’d like more pain relief than opioids provide, you'll likely need another pain relief method. And like other medications, there’s a small chance you could have a reaction like dizziness, nausea or vomiting.
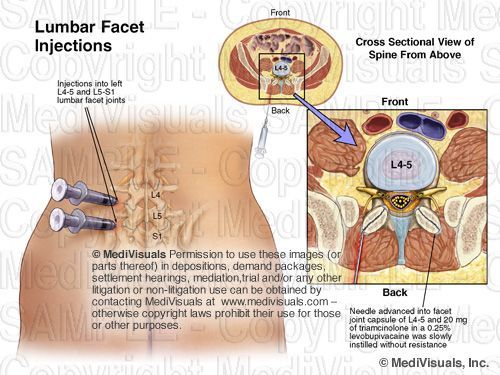
Intrathecal narcotic (ITN)
Intrathecal narcotic – or ITN for short – is a lesser-known and rarely performed medical pain management option during labor. The medication is delivered through a shot in your lower back and is often described as an alternative to an epidural.
However, since it’s delivered as a single shot, pain relief and duration can vary. Also, ITN is most effective when given during the first stage of labor and isn’t recommended for first-time mothers.
Spinal blocks
If you’re planning to deliver vaginally, a spinal block won’t be on your list of pain management options during labor.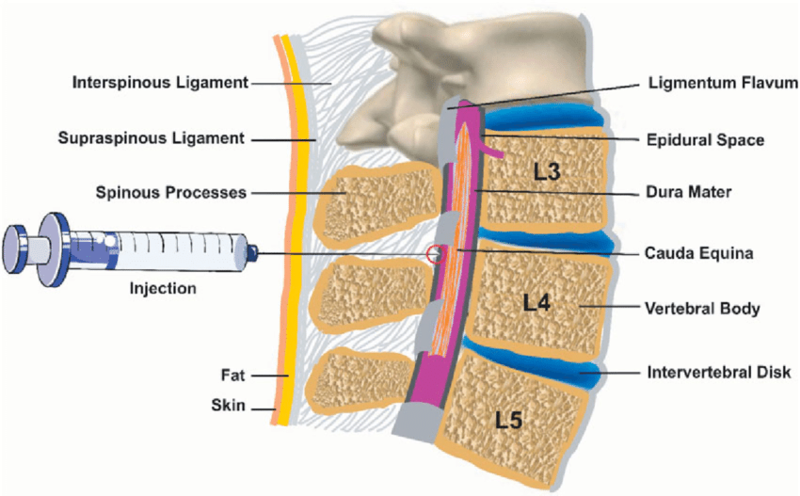 But it’s still important to know about in case an unplanned C-section is needed.
But it’s still important to know about in case an unplanned C-section is needed.
Spinal blocks are sometimes used during non-emergency C-sections to block pain but keep you awake so you can see your baby being born. If an epidural is already in place before an unplanned C-section, the epidural is usually left in and medication is increased. If an emergency C-section is needed, you’ll likely be placed under general anesthesia.
Spinal blocks are also commonly used for planned C-sections. The block is delivered in a single dose, and because of where the injection is placed, the numbing effects are almost immediate. You may not be able to move your legs until it wears off.
Natural pain relief options during labor and delivery
For those who hope to have an unmedicated birth, there are many natural pain relief options that can be mixed and matched based on your preferences.
But natural pain management methods aren’t only for those who hope to have an unmedicated, “natural” birth. They can be used in combination with pain medications so you can have the birth experience you’re hoping for.
They can be used in combination with pain medications so you can have the birth experience you’re hoping for.
Continuous labor support
Having a support person with you from early labor through the birth of your baby has a proven, positive effect on childbirth. This can be your partner, a family member, friend or a doula.
What is a doula? A doula is a birth coach who provides physical and emotional support during the entire pregnancy. During labor, a doula may be with you to give support, but they do not deliver the baby.
Activity and movement
Being active and mobile during your labor is a great way to cope with labor pains. That’s because movement can help reduce pain by stimulating the receptors in your brain for pain perception. Movement also helps labor progression by encouraging baby to move and get into a good position for birth.
Unless you’ve received an epidural or been advised to limit your activity, plan to change positions in bed, walk around, stand up and gently sway from side to side or sit on a rubber birthing ball.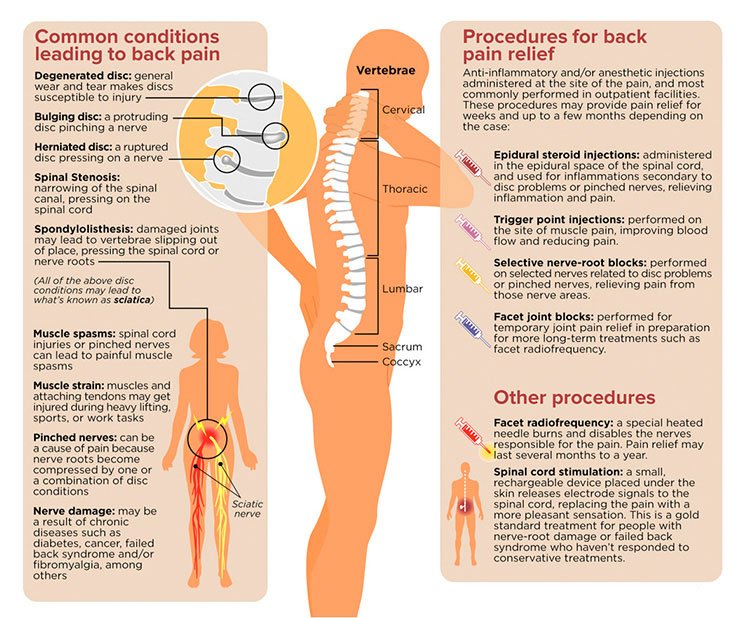 You might also have the option to use telemetry to wirelessly monitor your baby. This makes it easier for you to move freely without the hassle of cords.
You might also have the option to use telemetry to wirelessly monitor your baby. This makes it easier for you to move freely without the hassle of cords.
Distraction
Finding a way to take your mind off the pain of each contraction can go a long way in helping you feel more relaxed and better equipped to handle pain in the moment.
Focused breathing – or organized breathing – is one way to help you focus and distract you from pain during contraction pain. How? It can provide a rhythm and promote oxygen flow so you feel stronger and more in control and relaxed.
Childbirth education classes teach different methods of focused breathing, and many books and resources provide good explanations. But some other ways to distract yourself from pain include:
- Playing cards or a game
- Watching TV
- Listening to music
- Taking a shower
- Visualizing a special place or memory
Massage or counter pressure during labor
Massage techniques are designed to release muscle tension, helping you relax and reducing pain. So it’s no surprise that massage can be a way to relieve pain during labor.
So it’s no surprise that massage can be a way to relieve pain during labor.
Having your support partner massage your back, neck, shoulders, arms or legs throughout the labor process can feel soothing. But a strong massage of your lower back muscles or applying counter pressure during contractions can provide some targeted back pain relief.
Hydrotherapy
Hydrotherapy involves being immersed in warm water during labor. Just like taking a warm bath, hydrotherapy can be comforting, helping you relax and soothing aching muscles.
Being in water can also make it easier to move and reposition. This helps you find the most comfortable position, and movement can help labor progress.
Hydrotherapy is not the same as water birth, so you won’t deliver your baby in water. As long as it’s safe, you can typically get in and out of your hydrotherapy tub until late stage labor. If you choose to have an epidural, tub time will come to an end.
Water birth
Water birth is becoming increasingly popular among those who wish to have an unmedicated birth. Like hydrotherapy, you can labor in the warm water. But the big difference is that you’ll also deliver your baby in water.
Like hydrotherapy, you can labor in the warm water. But the big difference is that you’ll also deliver your baby in water.
However, it’s important to know that water births are only recommended for low-risk pregnancies. There’s also limited research on the risks and benefits of delivering a baby in water.
Aromatherapy and essential oils
While more research needs to be done, there are several studies that suggest aromatherapy and essential oils during labor can have a positive impact on birth experiences. For example, essential oils such as bitter orange, lavender and peppermint helped laboring women with pain, nausea and more.
Acupuncture
Acupuncture is a key part of traditional Chinese medicine that involves strategically inserting very thin needles in your body to relieve stress, aches and pains. But can it really help during labor?
Studies show that acupuncture can be a good supplement to other labor pain relief methods. But it may not be offered at all birth centers and hospitals, and it may or may not be covered by your insurance plan.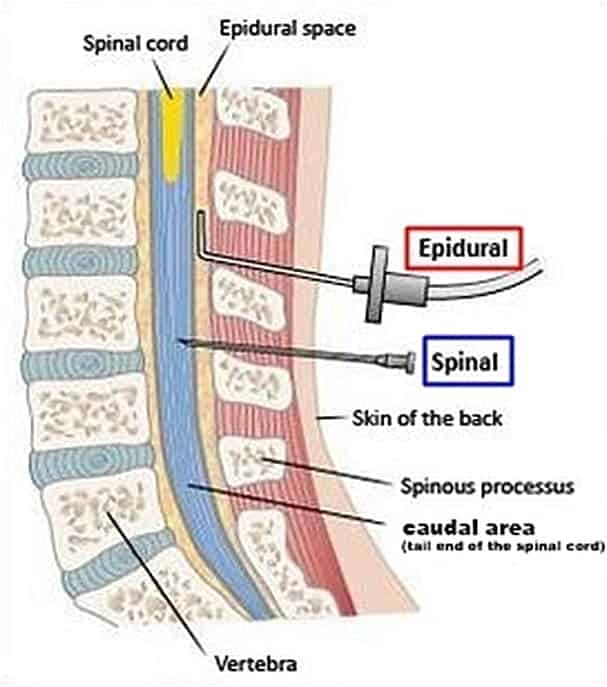 So if you’re interested in acupuncture, make sure to discuss it with your doctor or midwife, and get in touch with the hospital where you plan to deliver and your insurance company.
So if you’re interested in acupuncture, make sure to discuss it with your doctor or midwife, and get in touch with the hospital where you plan to deliver and your insurance company.
Additional FAQs on labor pain management
When do I have to decide which pain relief options I want?
Generally speaking, you don’t need to decide anything until you get to the hospital.
In the excitement of the labor process, you may forget all of your pain relief options, but your health care team will be there to help. We will review the risks and benefits of each option, so you can make a decision that’s right for you.
The one exception here is water birth. If you want to deliver your baby in a birthing tub, talk with your midwife before you’re ready to deliver.
Are all labor pain management options covered by my insurance?
Usually, yes. But you should always check with your insurance provider about what your individual plan covers if you’re concerned.
When you go into labor and start evaluating your pain relief options, the last thing you want to be concerned about is what is or isn’t covered by your insurance. The most important thing is that the hospital you’ve chosen to deliver your baby is in your insurance network.
Don’t hesitate to call your insurance company to learn more about your specific policy details.
What if I’m having a vaginal birth after Cesarean (VBAC)?
If you’ve had a C-section before and you’re planning on a vaginal delivery this time, all pain management options are available to you, with the exception of a water birth.
If you’ve had a C-section before, you can still take advantage of hydrotherapy to labor in water. When it’s time to push, your care team will help you out of the tub and into a birthing bed.
What if I’m having a vaginal birth after Cesarean (VBAC)?
If you’ve had a C-section before and you’re planning on a vaginal delivery this time, all pain management options are available to you, with the exception of a water birth.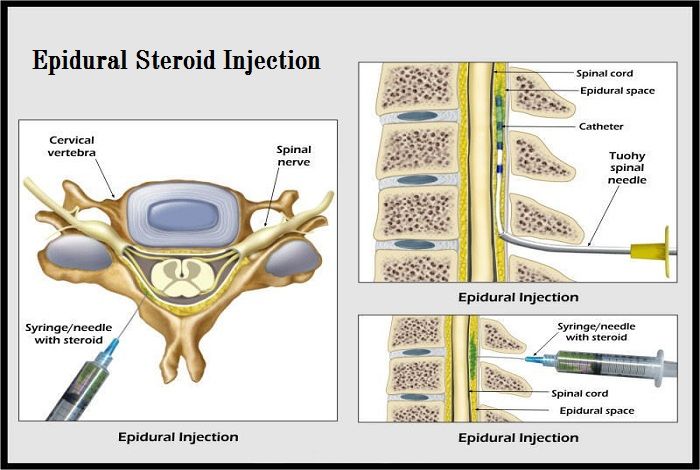
If you’ve had a C-section before, you can still take advantage of hydrotherapy to labor in water. When it’s time to push, your care team will help you out of the tub and into a birthing bed.
Get ready for labor and delivery day
You want the kind of birth experience you hoped for. But flexibility is key – and that’s why it’s so important to know your pain management options. You don’t really know what your pain tolerance is until you start labor – and your unique situation can change rapidly.
Your health care team is there to help you plan for your ideal scenario as well as help you make any adjustments as you go through the labor and delivery process. As always, the ultimate goal is to deliver a healthy baby to a healthy mom, and to make this experience a positive one for you and your family.
Looking for a hospital-based birth center for your delivery?
Not Found (#404)
Paracelsus Medical Center
Page not found.
The above error occurred while the Web server was processing your request.
Please contact us if you think this is a server error. thank you.
Leave feedback Write to management
Please wait, download may take time
Loading...
You know which doctor you want to book
You know the service you want to book
Service selection
A second consultation is considered to be a consultation of one specialist within 30 days from the date of the previous appointment. On the 31st day from the previous visit to a specialist of this profile, the consultation will be primary.
The choice of a specialist
Service selected:
Choosing a specialist service
A second consultation is considered to be a consultation of one specialist within 30 days from the date of the previous appointment. On the 31st day from the previous visit to a specialist of this profile, the consultation will be primary.
Address selection:
st. Vikulova, 33, building 2 st. Bolshakova, d. 68
Date selection:
Time of receipt:
Password
Password
Register Can't login? account activation
To gain access to your personal account, enter the e-mail that was specified during registration, we will send instructions for password recovery
To gain access to your personal account, enter the e-mail that was specified during registration, we will send instructions for reactivating your account
Your application has been accepted, our specialists will answer your question as soon as possible!
Telephone
Commentary
By clicking on the confirmation button, I agree with personal data processing policy
Dear patients!
Multidisciplinary Clinic and Maternity Hospital "Paracelsus" informs you, according to the Letter of the Ministry of Finance of the Russian Federation to the Federal Tax Service dated March 25, 2022. N BS-4-11 / 3605, that subparagraph 3 of paragraph 1 of Article 219 of the Tax Code of the Russian Federation provides for the taxpayer's right to receive a social tax deduction in the amount paid by him in the tax period for medical services provided by medical organizations engaged in medical activities , him, his spouse, parents, children (including adopted children) under the age of 18, wards under the age of 18 (in accordance with the list of medical services approved by the Government of the Russian Federation).
N BS-4-11 / 3605, that subparagraph 3 of paragraph 1 of Article 219 of the Tax Code of the Russian Federation provides for the taxpayer's right to receive a social tax deduction in the amount paid by him in the tax period for medical services provided by medical organizations engaged in medical activities , him, his spouse, parents, children (including adopted children) under the age of 18, wards under the age of 18 (in accordance with the list of medical services approved by the Government of the Russian Federation).
Joint order of the Ministry of Taxation of Russia and the Ministry of Health of Russia of July 25, 2001 N 289 / BG-3-04 / 256 (hereinafter - the order of July 25, 2001) approved the form of the Certificate of payment for medical services for submission to the tax authorities of the Russian Federation (hereinafter - the Certificate payment for medical services).
This certificate certifies the fact of receiving a medical service and its payment through the cash desk of a healthcare institution at the expense of the taxpayer.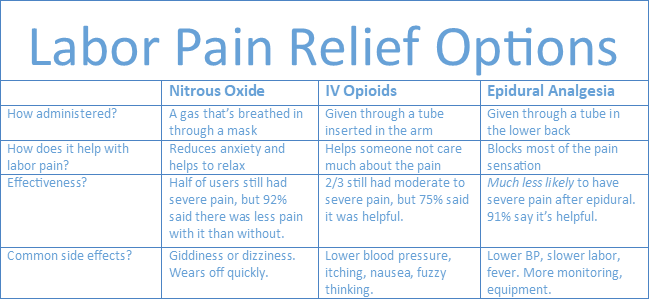
Thus, if the taxpayer submits to the tax authority a Certificate of payment for medical services, the taxpayer's failure to submit the relevant contract for the provision of medical services and (or) documents confirming payment cannot be grounds for refusing to provide such a deduction.
The amounts are based on payment data. Therefore, checks, an agreement and a clinic license are not needed to make a deduction.
Sample certificate attached.
Help Sample
Your application has been accepted, our specialists will contact you shortly!
Telephone
Comment
By clicking on the confirmation button, I agree with personal data processing policy
Deputy Director for Medical Activities of the Multidisciplinary Clinic "Paracelsus"
Makeev Alexander Anatolyevich
Telephone
Comment
By clicking on the confirmation button, I agree with personal data processing policy
media about INVITRO.

Olesya Butuzova
Any pregnant woman is waiting for childbirth - the long-awaited moment of meeting her baby. However, many also experience a contradictory feeling - fear. As a rule, most women who have heard enough stories of "experienced" girlfriends are afraid of pain. That is why a modern pregnant woman thinks not only about the name for the future crumbs, but also about ... pain relief. The most common and, perhaps, the favorite method of pain relief during childbirth is currently epidural anesthesia.
The essence of this method of pain relief is the injection of a local anesthetic under the dura mater of the spinal cord, where the roots of the spinal nerves pass. By "stunning" them, you can save the pregnant woman from pain.
Why is epidural anesthesia good?
Epidural anesthesia is not in vain so popular among both obstetrician-gynecologists and women in labor. It eliminates the pain and gives the woman the opportunity to rest.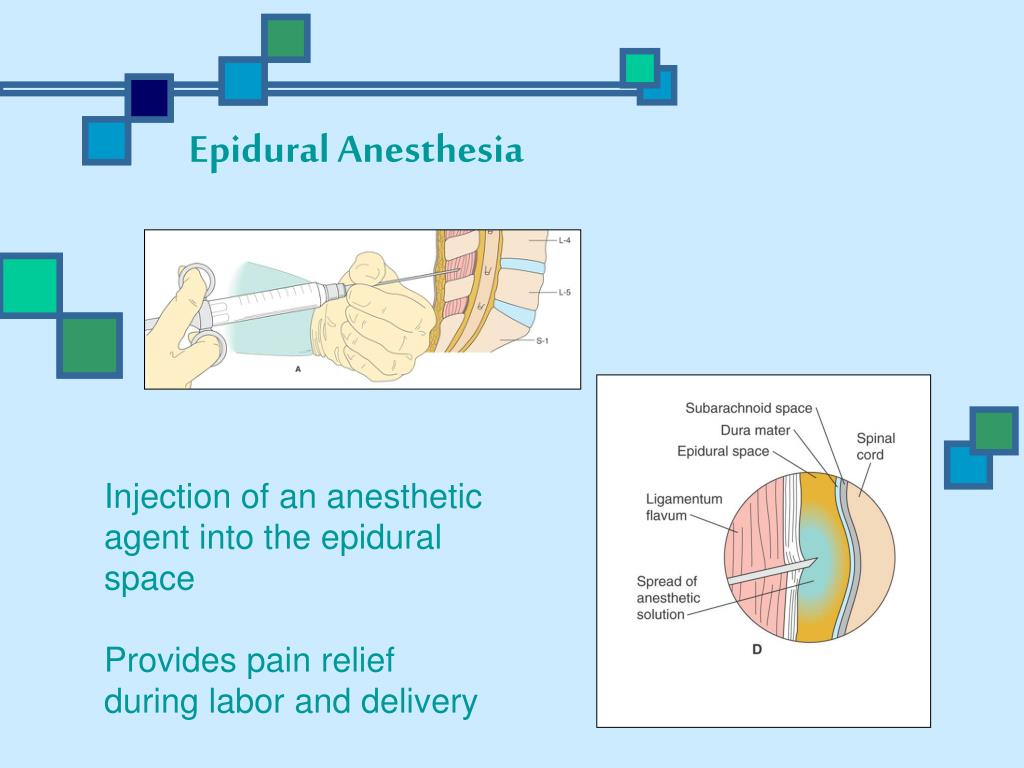 With a small injection of the drug, the woman in labor can move independently without experiencing discomfort. During the caesarean section, the mother is conscious and does not miss the wonderful moment of the first meeting with the baby.
With a small injection of the drug, the woman in labor can move independently without experiencing discomfort. During the caesarean section, the mother is conscious and does not miss the wonderful moment of the first meeting with the baby.
As a rule, the administration of the drug is carried out in doses, it arrives directly for its intended purpose - to the nerve roots, therefore, the dosages are minimal. All this allows the liver to quickly cleanse the blood and dispose of the remnants without missing the medicine to the baby. Thus, epidural anesthesia is practically safe for the baby.
Pain relief only?
Initially, the purpose of epidural anesthesia was not to facilitate the process of childbirth for mothers, but to stop certain threatening conditions.
- Thus, epidural anesthesia has a number of beneficial effects:
- Eases the pain of childbirth and gives the woman the opportunity to rest and gain strength for the important period of attempts.
- Reduces high blood pressure, hyperventilation of the lungs and adrenaline levels, which has a calming effect on the body. Epidural anesthesia facilitates the opening of the cervix and reduces trauma during preterm labor, coordinates contractions and the work of the muscles of the uterus.
- Well, and, most importantly, such pain relief is much safer than the use of intravenous drugs.
How is the procedure performed?
In order to puncture, the doctor must first position the pregnant woman correctly (which can be difficult with painful contractions). It is recommended that the woman in labor sit on a chair, facing the back or lie on her side, curled up.
The puncture site is carefully cleaned with antiseptic solutions to minimize the risk of infection.
The skin and subcutaneous tissue are punctured with a local anesthetic to numb the insertion of a needle under the dura mater of the spinal cord.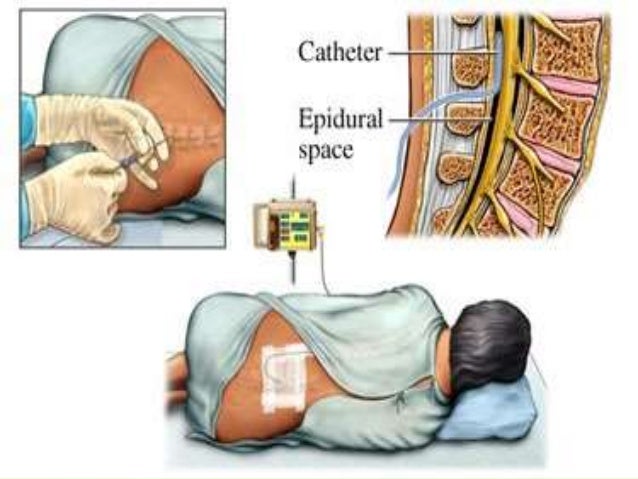
With a special needle, the doctor enters the epidural space and passes a catheter through it, through which the drug is delivered.
Medical indications for epidural anesthesia:
- Caesarean section.
- Diseases of the heart, including defects, - the load on the heart decreases.
- Diseases of the kidneys.
- Diabetes mellitus.
- High blood pressure. Epidural anesthesia helps to reduce it.
- Preterm pregnancy. Epidural anesthesia helps to relax the muscles of the pelvic floor and reduce the resistance exerted by the baby's head. The baby comes out smoothly and gently.
- Discoordination of labor - a condition in which contractions become irregular, frequent, painful and unproductive. They exhaust a woman, but do not contribute to the birth of a child. Epidural anesthesia puts in order the tone of the uterus and muscle contractions, thereby coordinating labor activity.
But epidurals are not for everyone. There is a whole list of contraindications to such anesthesia.
Our expert
Alla Misyutina, doctor of the INVITRO Medical Offices Department
. However, epidural anesthesia is one of the preferred methods of anesthesia in obstetrics. The onset of action of this pain relief is gradual and slow. Pain relief usually develops 10-20 minutes after epidural administration and may be continued until the end of labor as additional doses of drugs can be administered through the epidural catheter. After childbirth, the catheter is removed and after a few hours all sensations return to normal. Anesthesia involves a complete blockage of sensations and movements, it is used more often during a caesarean section.
Epidural analgesia is sometimes performed during childbirth, with the help of which only painful sensations are removed. Then the nerves responsible for motor functions remain partially in working order, and if desired, the woman can move - roll over, sit down, stand.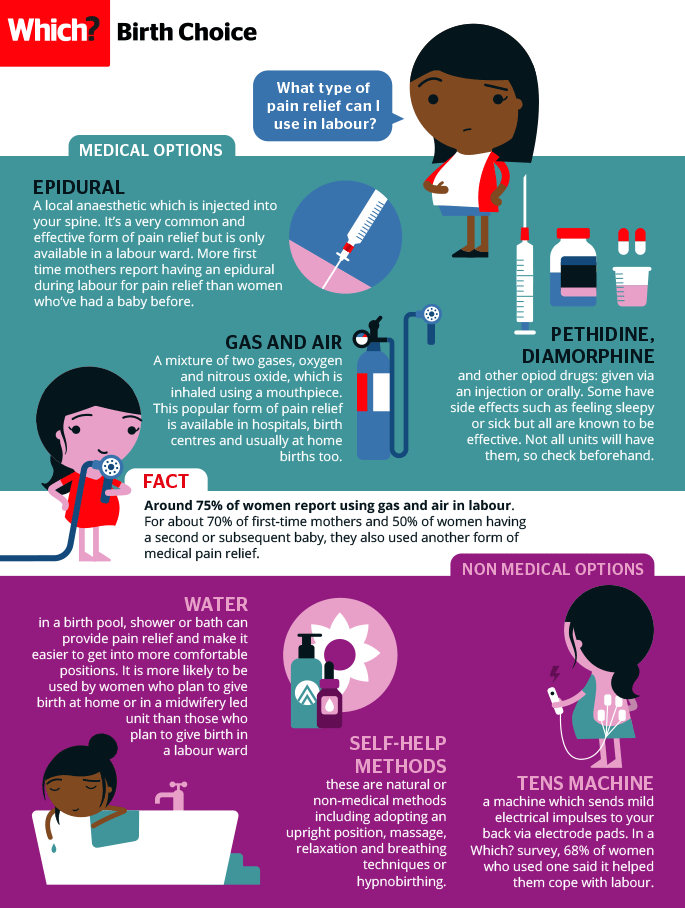 Contractions become painless and are felt by the woman in labor only as pressure below, on the rectum. With a competent approach of doctors - gynecologists and anesthesiologists - the risk is minimal. Obstetrician-gynecologists widely promote this type of pain relief, and many women easily agree to its use.
Contractions become painless and are felt by the woman in labor only as pressure below, on the rectum. With a competent approach of doctors - gynecologists and anesthesiologists - the risk is minimal. Obstetrician-gynecologists widely promote this type of pain relief, and many women easily agree to its use.
About side effects
But, like any other useful medical manipulation, epidural anesthesia is not without side effects.
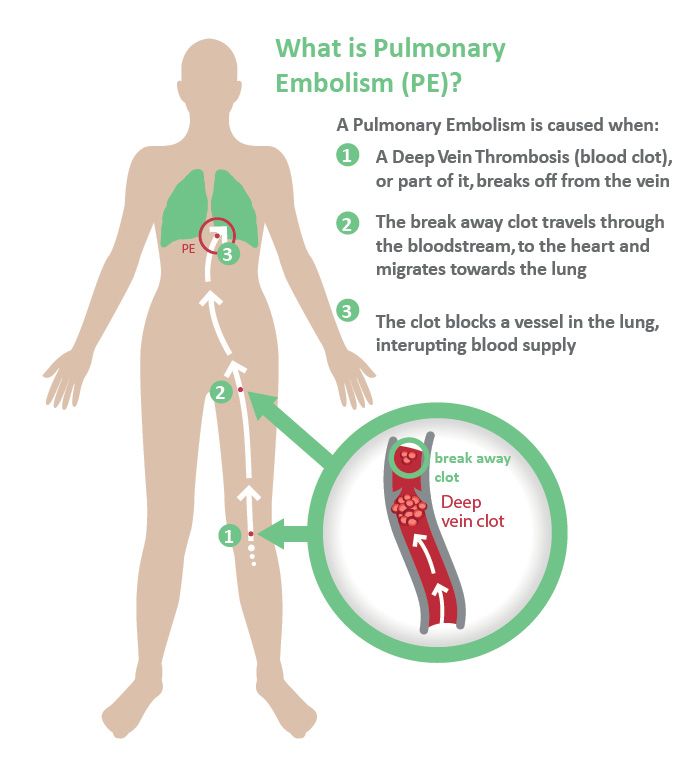
The most common is lowering blood pressure. This is fraught with impaired placental blood flow and hypoxia, that is, oxygen starvation in the baby.
The second serious reaction may be allergic. To prevent anaphylactic shock at the beginning of the procedure, a trial administration of the drug is carried out. If the woman in labor felt pain, burning or itching in the puncture area, then the doctors “cover up” the anesthesia with antiallergic drugs.
When pierced, the drug may enter the spinal canal, which is fraught with difficulty breathing and a drop in blood pressure.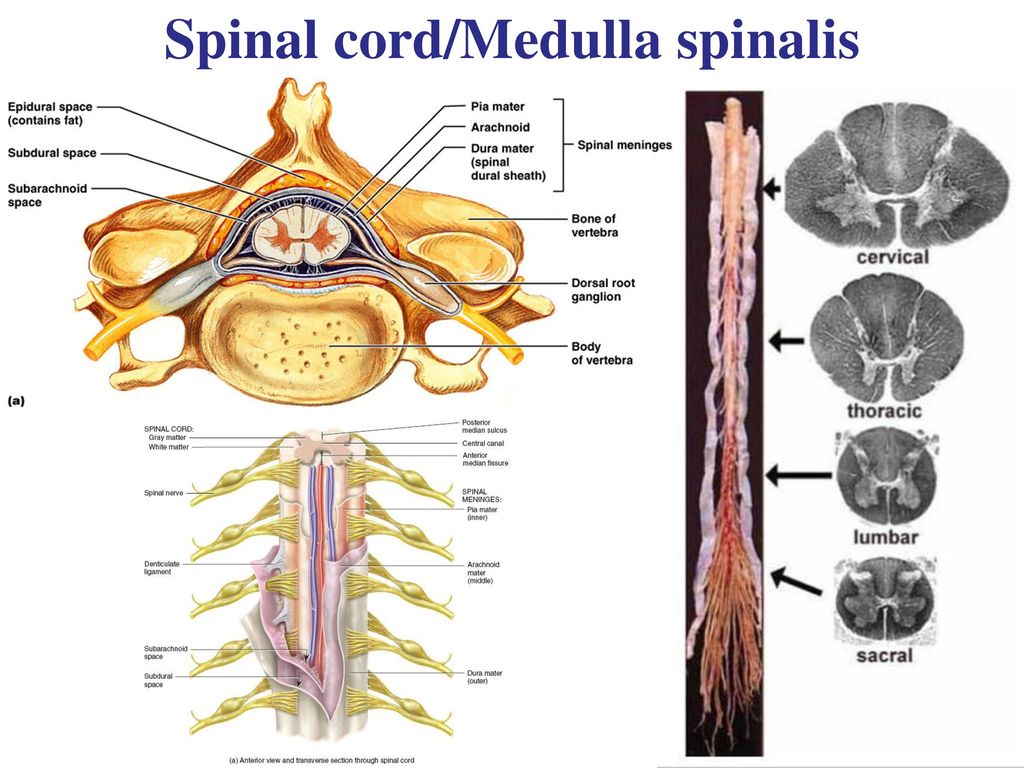 It is also possible to injure the roots of the spinal nerves and pain in the limbs. When the drug is injected under the dura mater of the spinal cord, there is a risk of getting into the epidural veins. In such cases, severe complications develop - a sharp drop in blood pressure, heart rhythm disturbance and dizziness. Often this situation is accompanied by numbness of the tongue.
It is also possible to injure the roots of the spinal nerves and pain in the limbs. When the drug is injected under the dura mater of the spinal cord, there is a risk of getting into the epidural veins. In such cases, severe complications develop - a sharp drop in blood pressure, heart rhythm disturbance and dizziness. Often this situation is accompanied by numbness of the tongue.
Bacteria entering the puncture site can lead to meningitis.
If the dura mater is damaged and, as a result, cerebrospinal fluid enters the epidural space, headache may occur. It appears a few days after childbirth and can last up to a month and a half.
With regard to side effects on the part of the child, this may be respiratory depression, dysmotility, difficulty sucking.
However, I would like to note that according to statistics, all these complications are rare.
Thus, epidural anesthesia is an effective way of pain relief during childbirth, helping the mother to gain strength before meeting the baby.