Is a pap smear safe during pregnancy
Pap smears are safe – before, during and after pregnancy | Women's Health | Your Pregnancy Matters
×
What can we help you find?Refine your search: Find a Doctor Search Conditions & Treatments Find a Location
Appointment New Patient Appointment
or Call214-645-8300
MedBlog
Women's Health; Your Pregnancy Matters
August 3, 2021
Women's Health; Your Pregnancy Matters
Yetunde Awosemusi, M. D. Obstetrics and Gynecology
Pregnancy induces changes in your body and your mind. Many mothers-to-be experience anxiety, which can lead some to second-guess their most routine medical procedures. While this mindset is understandable, one thing you can definitely cross off your “worry list” is the myth that Pap smears are not safe during pregnancy.
It is normal to experience some spotting after a Pap smear, even when you are pregnant. However, this natural response has caused some misconceptions that the Pap smear, a potentially life-saving procedure, isn’t safe during pregnancy.
The truth is that getting a Pap smear is safe for you and your baby; it will not cause a miscarriage.
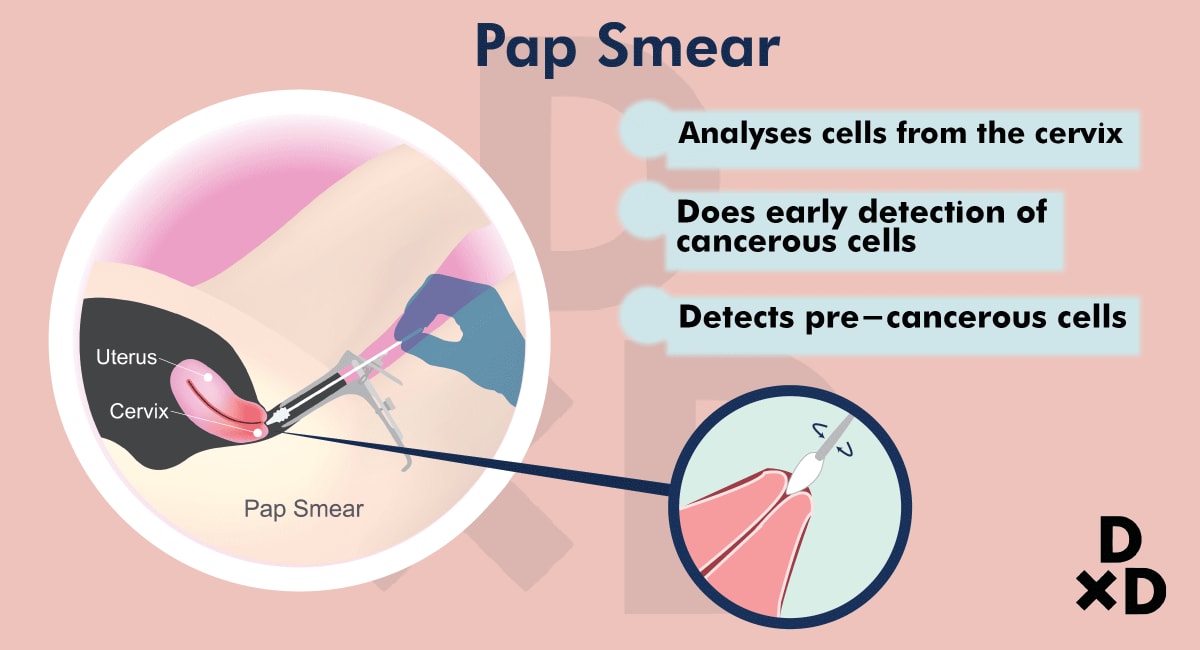
Whether you’re pregnant or not, the Pap smear is the gold standard for screening for cervical cancer. It allows us to collect cells from the surface of the cervix and examine them for abnormalities.
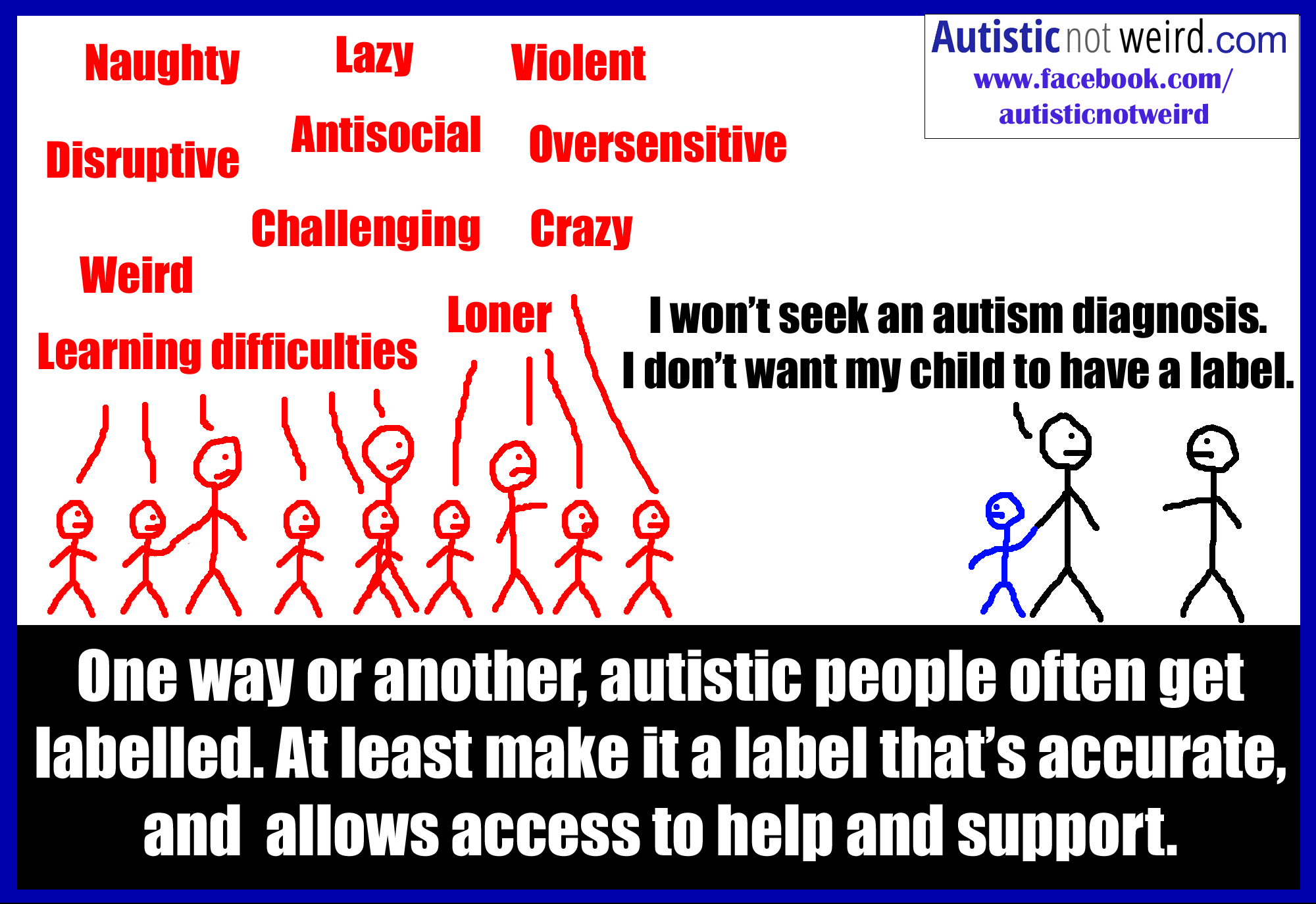
Cervical cancer and abnormal Pap smear results are almost always caused by the human papillomavirus (HPV), a sexually transmitted disease currently infecting around 80 million people in the United States. Though the virus is common, the likelihood of it causing cancer is much less common. In fact, most infections go away on their own. Cancer develops when the infection isn’t detected and managed appropriately, which is why Pap smears are so important.
Data from the Centers for Disease Control and Prevention (CDC) show that cervical cancer deaths have decreased over the last several decades as a result of increased Pap smears. If you follow up on your Pap smear results as recommended by your provider, we almost always will catch the cancer.
What’s even more encouraging is that the HPV vaccine, which the CDC recommends for all children ages 11 or 12, can prevent cervical cancer from developing. We still recommend routine Pap smears for people who receive the vaccine, but we are finding very low rates of abnormal Pap smears within this vaccinated population.
As more people recognize the importance of regular Pap smears, questions about the procedure continue to swirl. We’ve answered the most common ones below.
How often should I get a Pap smear?
We recommend a Pap smear every three years for women between the ages of 21 and 30. If your results are normal and you are negative for HPV, you can extend that to every five years from ages 31 to 65. Higher-risk populations, such as people who have an autoimmune disease, should discuss more frequent testing with their provider.
Do I need a Pap smear when I’m pregnant?
Reviewing your Pap smear history is an early, important step during prenatal care. If you received a normal test result within the last three years, you likely don’t need a Pap smear while pregnant.
If you received a normal test result within the last three years, you likely don’t need a Pap smear while pregnant.
We realize, however, that many newly pregnant people are seeing a doctor for the first time in quite a while – maybe their first time ever as an adult – and haven’t had a Pap smear before, or for several years. To support a healthy pregnancy, we want to rule out the possibility of cervical cancer development as soon as possible.
If I do need one, is it safe?
Pap smears while pregnant are safe for you and your baby. Any suggestion that it might cause a miscarriage is false. It is normal to experience minor bleeding after a Pap smear when you are pregnant because blood flow to the uterus increases, which causes the cervix to bleed more easily when touched.
Any type of bleeding is understandably alarming while pregnant, but in this case the blood is coming from the outside of your cervix – not inside the uterus, where the baby is safe and developing.
What happens if I have an abnormal Pap smear?
The next step may be to perform a colposcopy, which allows us to look more closely at the cervix and take a small tissue sample to test the abnormal cells for cancer. The colposcopy is safe during pregnancy – the only cells we touch are on the outside of the cervix, not the inside near your baby.
Generally, we divide these test results into what we call low-grade or high-grade “dysplasia” – the existence of abnormal cells:
- Low-grade dysplasia doesn’t usually progress to cancer, so we just watch it and will likely encourage you to come back in a year for another Pap smear.
- High-grade dysplasia has an increased chance of progressing to cancer, so we will likely recommend a loop electrosurgical excision procedure (LEEP) after delivery.
LEEP removes the outside portion of the cervix containing the abnormal cells, and it can increase the risk of pregnancy complications like preterm birth or losing the baby in the second trimester. Because cervical cancer is a slow-growing disease, we can usually postpone the procedure until after delivery and watch the area closely, performing a colposcopy every trimester to monitor the dysplasia’s progress.
Because cervical cancer is a slow-growing disease, we can usually postpone the procedure until after delivery and watch the area closely, performing a colposcopy every trimester to monitor the dysplasia’s progress.
Pregnancy weakens the immune system, which can increase the likelihood of abnormal results, so sometimes the high-grade dysplasia resolves itself after pregnancy. If it does progress to cancer, we will work with you to develop a personalized treatment plan that incorporates your specific health conditions and needs. As an academic medical center, we can streamline your access to some of the best oncologists in the U.S., right here at UT Southwestern.
If you need a Pap smear, it is safe to get one during pregnancy. Along with the HPV vaccine, Pap smear is a vital tool that helps make cervical cancer preventable – and it will give you one less thing to worry about as you prepare for the healthy birth of your baby.
To visit with an Ob/Gyn or certified nurse-midwife, call 214-645-8300 or request an appointment online.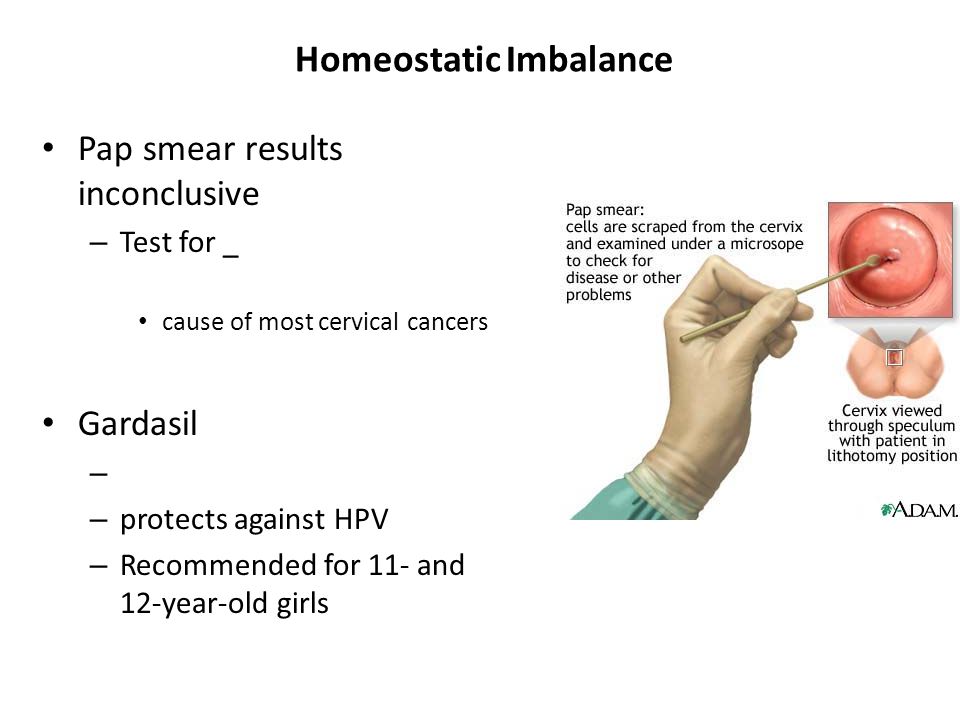
More in: Women's Health, Your Pregnancy Matters
Women's Health
- Maude Carmel, M.D.
October 17, 2022
Men's Health; Women's Health; Your Pregnancy Matters
- Yair Lotan, M.
 D.
D.
September 6, 2022
Pediatrics; Women's Health
- Nirupama DeSilva, M.D.
- Jason Jarin, M.D.
August 31, 2022
Women's Health
- Abey Eapen, M.
 D., Ph.D.
D., Ph.D.
August 18, 2022
Men's Health; Women's Health
July 26, 2022
Prevention; Women's Health
- Andrea Jochim, M.D., Ph.D.
July 25, 2022
Cancer; Discovery; Women's Health
- Kevin Albuquerque, M.
 D.
D. - Chika Nwachukwu, M.D., Ph.D.
May 18, 2022
Diet and Nutrition; Women's Health; Your Pregnancy Matters
- Robyn Horsager-Boehrer, M.D.
- Carrie McAdams, M.D., Ph.D.
May 17, 2022
Patient Stories; Women's Health
May 6, 2022
More Articles
Pap Smear - American Pregnancy Association
A Pap Smear, usually done during your first prenatal visit is a test used to look for changes in the cells of the cervix which indicate cervical cancer or conditions that may develop into cancer.
Pap smears do not diagnose cancer, but they detect 95% of cervical cancers at a stage when they cannot be seen with the naked eye. They can then be treated and are almost always cured. Though Pap smears do not specifically test for other gynecological problems or sexually transmitted diseases, Pap smears will indicate the presence of abnormal cells for which further testing or examination would be required.
What if I am pregnant, and I have an abnormal Pap smear?
A Pap smear is a routine part of your prenatal care and poses no risk to the fetus. If you have an abnormal Pap during pregnancy your physician will discuss treatments which can be done safely during pregnancy, or depending on diagnosis, delay treatment until after your baby is born. If your physician suggests a colposcopy or cervical biopsy, there can be slight bleeding from the external part of the cervix, but this is not a serious complication. If your physician is considering doing an internal biopsy into the endocervical canal, there may be a slight risk of a pregnancy complication.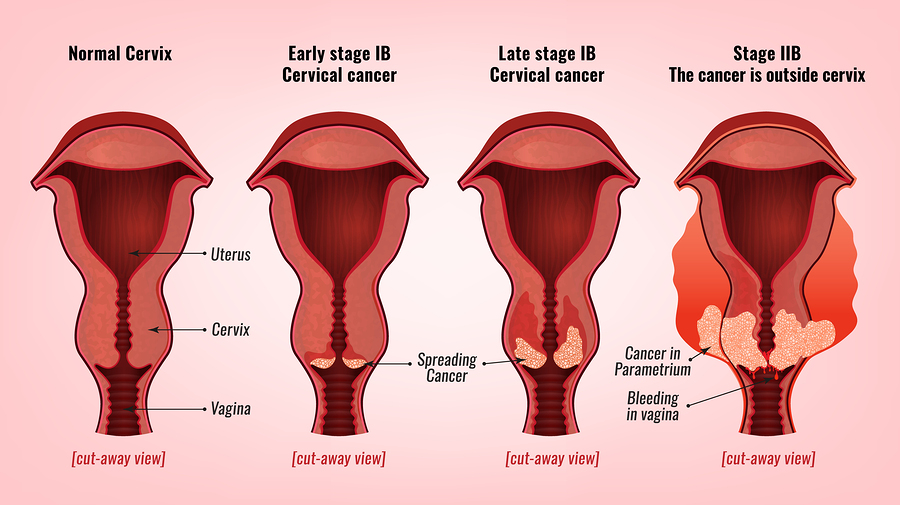 But your health care provider has your best interest in mind and will only do what is medically necessary. Your doctor may perform additional Pap smears during your pregnancy if necessary. Many times the birth of your baby will wash away any abnormal cervical cells.
But your health care provider has your best interest in mind and will only do what is medically necessary. Your doctor may perform additional Pap smears during your pregnancy if necessary. Many times the birth of your baby will wash away any abnormal cervical cells.
What happens during a Pap smear?
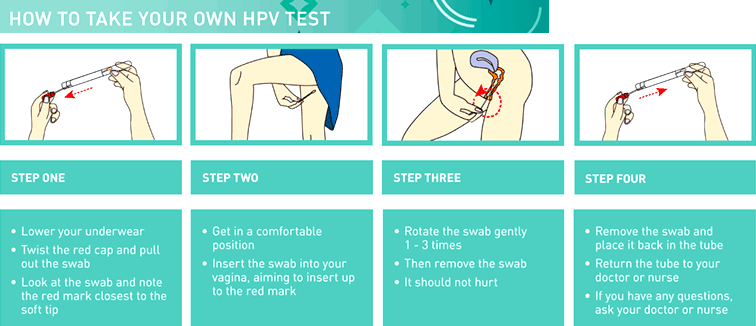
As part of your pelvic exam, your physician will use a small spatula, brush, or swab to remove a few cells from your cervix. You may feel some discomfort, but it is not painful. The cells are placed on a microscope slide and sent to a lab for results. You can help your clinician obtain a good Pap smear by not having intercourse, not douching, or not using any products/medications in the vaginal area for at least two days prior to the examination.
What do the results mean?
A negative result means that your cervix is normal. A positive result indicates the presence of abnormal cells. Your physician may also call this an abnormal Pap. Remember that this is a test, not a diagnosis. A positive result does not prove that you have cancer or even dysplasia (a pre-cancerous condition). However, it usually means you should have further evaluation, such as a colposcopy (microscope used to look into the cervix) or a biopsy (removing a small amount of tissue from the cervix). Your doctor will discuss the results with you. One in ten Pap smears indicates some abnormality, though most are not serious. Further testing will be required to determine if you have an infection, inflammation, a yeast infection, trichomonas, herpes, or the human papillomavirus. Researchers believe that cervical cancer is directly related to human papillomavirus (HPV).
Remember that this is a test, not a diagnosis. A positive result does not prove that you have cancer or even dysplasia (a pre-cancerous condition). However, it usually means you should have further evaluation, such as a colposcopy (microscope used to look into the cervix) or a biopsy (removing a small amount of tissue from the cervix). Your doctor will discuss the results with you. One in ten Pap smears indicates some abnormality, though most are not serious. Further testing will be required to determine if you have an infection, inflammation, a yeast infection, trichomonas, herpes, or the human papillomavirus. Researchers believe that cervical cancer is directly related to human papillomavirus (HPV).
There are over 100 different types of HPV. About 30 types are spread through sexual transmission and can possibly lead to cervical cancer. HPV is the main risk factor for cervical cancer, but most women who receive treatment for abnormal cells caused by HPV, do not develop cervical cancer. In 2003, the FDA approved a screening test that can be done in conjunction with a Pap smear to determine if you have the HPV virus. The HPV DNA test can detect high-risk types of HPV before any abnormal cells can be detected on the cervix. This screening is recommended for women over the age of 30, who are at an increased risk of an HPV infection turning into pre-cancerous cells. Some Pap smears indicate an unsatisfactory sample because of recent sexual activity or use of vaginal creams and douches. Regardless of the reason, an abnormal Pap will require another Pap smear in a few months. With proper screening, cervical cancer is preventable and avoidable.
In 2003, the FDA approved a screening test that can be done in conjunction with a Pap smear to determine if you have the HPV virus. The HPV DNA test can detect high-risk types of HPV before any abnormal cells can be detected on the cervix. This screening is recommended for women over the age of 30, who are at an increased risk of an HPV infection turning into pre-cancerous cells. Some Pap smears indicate an unsatisfactory sample because of recent sexual activity or use of vaginal creams and douches. Regardless of the reason, an abnormal Pap will require another Pap smear in a few months. With proper screening, cervical cancer is preventable and avoidable.
When should I have a Pap smear?
It is recommended that all women get a Pap smear done at age 21. Recent changes to testing guidelines have removed the need for anyone under the age of 21 to be tested, regardless of sexual activity. Pap smears should then be done every 3 years until they are 29. Women between the ages of 30 and 65 can either be Pap-tested every 3 years or every 5 years with a Pap/HPV co-test. Discuss with your health provider what they recommend for a Pap smear schedule as some still encourage that they are done yearly. Even if your health care provider recommends you have a Pap smear every 2-3 years, you still should see your gynecologist every year for pelvic exams, information regarding other women’s health issues, and breast exams. Women should have a Pap smear in the middle of their monthly cycle, or about 10-20 days after the LMP (last menstrual period) began. At least 2 days before the test, women should avoid having anything in the vagina including sexual intercourse, douching, vaginal creams/suppositories, or spermicide. These could interfere with the results of the test and cause an abnormal result.
Discuss with your health provider what they recommend for a Pap smear schedule as some still encourage that they are done yearly. Even if your health care provider recommends you have a Pap smear every 2-3 years, you still should see your gynecologist every year for pelvic exams, information regarding other women’s health issues, and breast exams. Women should have a Pap smear in the middle of their monthly cycle, or about 10-20 days after the LMP (last menstrual period) began. At least 2 days before the test, women should avoid having anything in the vagina including sexual intercourse, douching, vaginal creams/suppositories, or spermicide. These could interfere with the results of the test and cause an abnormal result.
When can a woman stop having this test performed?
According to the National Cancer Institute, women who are over the age of 70 and have a history of normal Pap smears are very unlikely to develop cervical cancer and therefore can discuss the option of not needing any further pap smears. Women who have had a hysterectomy with both the uterus and cervix removed, for reasons not related to cancer, can also discuss the option of not needing any further Pap smears.
Women who have had a hysterectomy with both the uterus and cervix removed, for reasons not related to cancer, can also discuss the option of not needing any further Pap smears.
Who needs pap smears more often?
Women who are taking immunosuppressant medications or have a condition that weakens the immune system should have more frequent Pap smears. These women need to discuss what type of testing schedule they should be on with their health care providers.
Want to Know More?
- Your First Prenatal Visit
- Most Common Pregnancy Complications
- Sex During Pregnancy
Compiled using the following sources:
Danforth’s Obstetrics and Gynecology Ninth Ed. Scott, James R, et al, Ch.26
National Cancer Institute, www.cancer.gov
FDA News Release, March 2003 https://www.fda.gov
Flora smear during pregnancy - when and why to take it
- When to take a flora smear
- What a flora smear shows
- Flora smear preparation rules
The flora smear is the most common test prescribed by an obstetrician-gynecologist. To conduct this study, the doctor, while examining a woman in a gynecological chair, takes the contents of the vagina from the posterior fornix (this is the space that is located between the back wall of the vagina and the cervix), the cervical canal and the discharged urethra, applies the material to the glass slide and directs him to the lab.
Smear examination for flora in the laboratory is carried out by a doctor of laboratory diagnostics under a microscope. This study allows you to determine the nature of the microflora (types of microorganisms) of the vagina, cervical canal and urethra, to identify the inflammatory process in the genitals of a woman, in some cases it also allows you to determine the causative agent of this inflammatory process (for example, gonococcus, Trichomonas).
When to take a smear for flora
It is mandatory for all pregnant women to take a swab twice - at registration and at 30 weeks of pregnancy, often another swab for flora is taken at 36-37 weeks to assess the state of the vaginal microflora before childbirth. During these periods, the analysis is given even in cases where the patient is not bothered by anything. This is carried out in order to identify a hidden inflammatory process that can lead to serious complications during pregnancy. During pregnancy, due to changes in hormonal levels and a decrease in immunity, exacerbation of chronic infections, as well as candidiasis (thrush), is much more likely. Any inflammatory process in the vagina during pregnancy can lead to serious complications of pregnancy - premature rupture of amniotic fluid, premature birth, oligohydramnios or polyhydramnios, intrauterine growth retardation and others.
If a pregnant woman has complaints - the appearance of copious discharge from the genital tract, itching, burning or discomfort in the genital area, a swab for flora is also taken. In some pathological conditions, for example, in the presence of past miscarriages associated with infectious complications of pregnancy, cervical incompetence, a smear for flora is taken once a month, and after 30 weeks once every two weeks.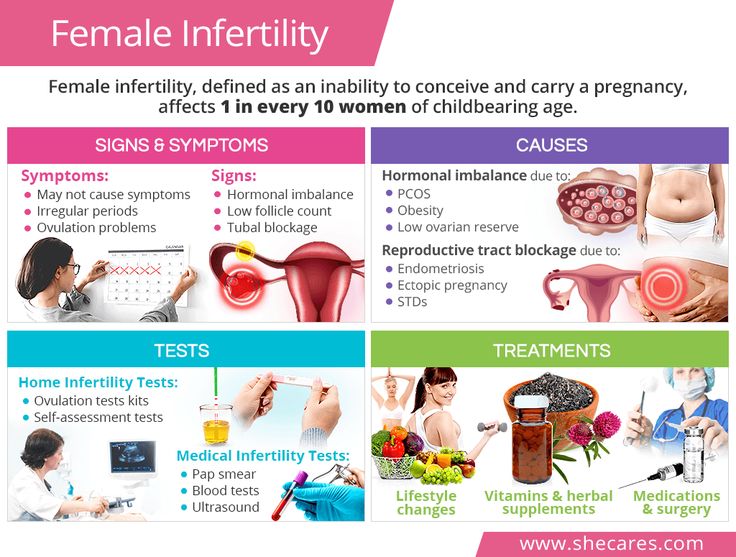 Smear sampling is an absolutely safe procedure and does not lead to any complications, therefore it can be performed at any stage of pregnancy.
Smear sampling is an absolutely safe procedure and does not lead to any complications, therefore it can be performed at any stage of pregnancy.
What a flora smear shows
A flora smear is evaluated according to the following indicators:
Epithelium
Squamous epithelium is the cells of the surface layer of the mucous membrane of the vagina and cervix. The presence of a large amount of squamous epithelium in a smear may indicate an inflammatory process. The absence of epithelium in the smear indicates a violation of the hormonal background.
Leukocytes
These are blood cells involved in the destruction of pathogenic bacteria. Leukocytes are able to actively penetrate through the wall of blood vessels into the tissues of the body and participate in the fight against infectious agents. Normally, no more than 10 leukocytes are present in a smear for flora from the vagina, no more than 15 leukocytes per field of view from the cervical canal, and up to 2 leukocytes per field of view from the urethra.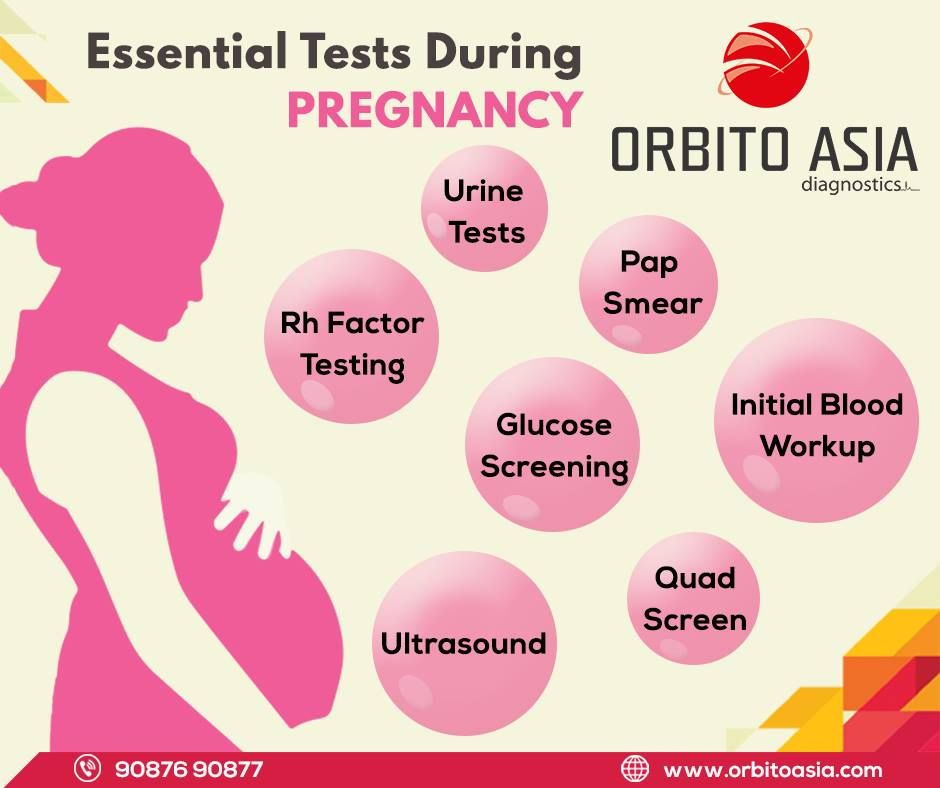 An increase in the content of leukocytes in a smear is a sign of inflammation, while the higher the content of leukocytes in a smear, the more pronounced the inflammatory process.
An increase in the content of leukocytes in a smear is a sign of inflammation, while the higher the content of leukocytes in a smear, the more pronounced the inflammatory process.
Red blood cells
These are red blood cells. Normally, single erythrocytes (1-2 in the field of view) can be found in a flora smear. An increase in the number of red blood cells indicates the presence of a chronic inflammatory process, and also be a sign of injury or occult bleeding, for example, in the presence of cervical ectopia (the so-called erosion, when the vaginal part of the cervix is covered with a cylindrical epithelium normally lining the inside of the cervix).
Slime
Normally, there is no mucus in the urethra, a moderate amount of mucus is detected in the vagina, and there may be a large amount of mucus in the cervix. An increase in the amount of mucus may be a sign of an inflammatory process, but this criterion does not have great diagnostic value, and doctors rarely rely on it when making a diagnosis.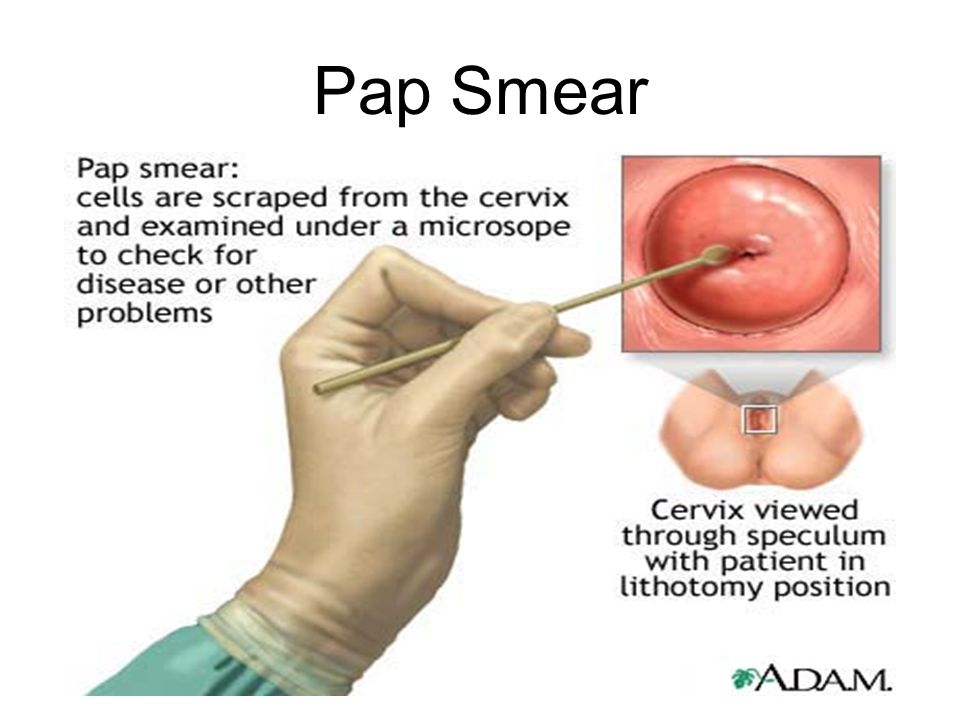
Bacteria
Normally, flora should not be detected in the urethra, rod flora is detected in a moderate amount in the vagina and cervix. Rod flora is most often lactobacilli, which are 95% are normal vaginal biocenosis. Lactobacilli actively colonize the vagina and create an acidic environment in it, thereby preventing the growth and reproduction of pathogenic bacteria.
In addition to lactobacilli, other rod bacteria, such as E. coli, bacteroids, and various cocci, may also be present in the vagina. These are bacteria that, under microscopy, have the shape of balls. This group of bacteria includes streptococci, staphylococci, enterococci. In a small amount, they are normally present in the vagina. If their number increases sharply against the background of the death of normal lactobacilli, this can lead to the development of an inflammatory process. Unfortunately, according to the results of a routine smear on the flora, it is impossible to determine which specific bacteria and in what quantity are present in the vagina. Therefore, with a pronounced inflammatory process, as well as when a large amount of coccal flora is found in a smear on the flora, the doctor prescribes an additional analysis to make the correct diagnosis - sowing on the flora with the determination of sensitivity to antibiotics.
Therefore, with a pronounced inflammatory process, as well as when a large amount of coccal flora is found in a smear on the flora, the doctor prescribes an additional analysis to make the correct diagnosis - sowing on the flora with the determination of sensitivity to antibiotics.
Opportunistic flora
These are micro-organisms that live in the human body in small numbers, without causing harm, but under certain conditions can lead to an inflammatory process. Such microorganisms found in a smear on the flora include fungi of the genus Candida and gardnerella.
Gardnerella ("key cells")
Gardnerella and other bacteria living in anoxic conditions (so-called anaerobic bacteria) normally live in the vagina in small numbers, without causing symptoms of an inflammatory process. With a decrease in local immunity, which is quite common during pregnancy, there is an increase in the proportion of these bacteria in the vaginal microflora, a disease occurs - bacterial vaginosis (vaginal dysbiosis). At the same time, “key” cells are found in a smear on the flora - these are cells of the vaginal mucosa, covered with gardnerella and other anaerobic bacteria. The gardnerella themselves are not visible in a normal unstained smear. They can only be detected by staining smears with special dyes.
At the same time, “key” cells are found in a smear on the flora - these are cells of the vaginal mucosa, covered with gardnerella and other anaerobic bacteria. The gardnerella themselves are not visible in a normal unstained smear. They can only be detected by staining smears with special dyes.
Mushrooms
Microorganisms of the genus Candida are part of the normal microflora of the mouth, vagina and colon of most healthy people. Normally, the number of these microorganisms is small and they do not cause an inflammatory process. Normally, in some women, a small amount of spores of the fungus may be detected in a vaginal smear. In the absence of an inflammatory reaction and complaints of the patient, the treatment of this condition is not carried out. The detection of a large number of spores or mycelium of a yeast-like fungus of the genus Candida in a smear on the flora makes it possible to diagnose candidiasis (or thrush)
Pathogenic flora
There are microorganisms that should not normally be present in the vagina of a healthy woman and the detection of which in a flora smear indicates the presence of a serious sexually transmitted disease.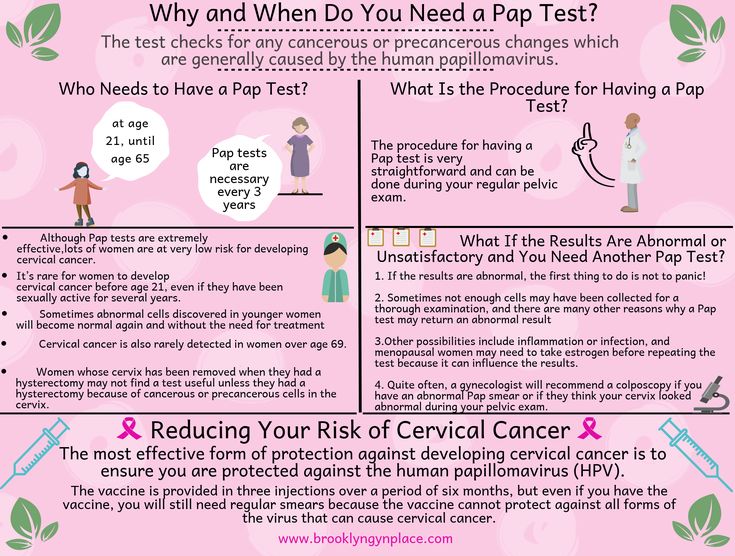 Of these infections in the smear, Trichomonas and gonococci are most often detected.
Of these infections in the smear, Trichomonas and gonococci are most often detected.
Trichomonas
These are the simplest microorganisms that have a flagellum and are capable of movement. Detection in a smear on the flora of Trichomonas indicates the presence of a sexually transmitted disease - trichomoniasis. Trichomoniasis in a pregnant woman increases the risk of preterm birth, premature rupture of amniotic fluid, intrauterine growth retardation. In addition, there is a risk of infection of the baby when passing through the birth canal, therefore, if Trichomonas is found in a smear, antibacterial treatment is mandatory during pregnancy.
Gonococci
These are bacteria that look like double bean-shaped balls in the smear, adjacent to each other with a concave side. Detection of gonococci in a smear allows the doctor to make a diagnosis - gonorrhea. This is a sexually transmitted disease, which must also be cured during pregnancy. The inflammatory process caused by gonococcus significantly complicates the course of pregnancy, can lead to miscarriage, premature birth, premature rupture of amniotic fluid, infection of the placenta and membranes, and in addition, when the baby passes through the birth canal, the eyes of the newborn are affected by gonococcus.
Detection of pathogens of other sexually transmitted infections in a smear on the flora is very difficult. Therefore, in the presence of an inflammatory process according to the smear, the doctor usually recommends testing for sexual infections by another, more sensitive method - a PCR smear.
Rules for preparation for taking a smear for flora
In order for the result of a smear for flora to be reliable, a number of important conditions must be observed before taking this analysis. Within 2-3 days, you can not use any vaginal suppositories or creams, douching with any solutions is contraindicated, since they change the composition of the vaginal microflora, making it difficult to identify the causative agent of inflammation. In addition, within 2 days it is desirable to refrain from sexual intercourse. This is also due to the fact that spermatozoa and residual semen in the vagina can lead to an incorrect smear result for flora.
Cytology smear | KGBUZ "Vladivostok Polyclinic No.
 6"
6" June 29, 2015
[dt_sc_hr_invisible]
[dt_sc_callout_box type="type2" button_text="On Map" target="_blank ]
A smear for cytology can be taken at
st. Borisenko 29 examination room (room 3)
[/dt_sc_callout_box]
[dt_sc_clear]
A cytology smear - (presence of atypical cells) is a laboratory diagnostic method that allows you to detect pathological abnormalities in the cells of the cervix. Other names for this analysis are Pap test and Pap smear. This analysis is assigned not only to pregnant women, but also to every woman who has reached the age of 18 with a frequency of once a year. During pregnancy, it is given when registering for the management of a pregnant woman, and if a woman has erosion (ectopia) of the cervix, it is also repeated at the 30th week of pregnancy.
- In addition to pregnancy, there are other indications for this test:
- menstrual disorder
- infertility
- genital herpes;
- taking hormonal contraceptives;
- human papillomavirus (HPV)
- obesity
- before placing an intrauterine device in a woman
- in the presence of a large number of sexual partners;
- when planning a pregnancy.
Before giving a smear for cytology, a woman is recommended to exclude all sexual contacts for two days, do not douche, do not use vaginal preparations (lubricants, creams, suppositories). Immediately before visiting the doctor for the last time, you need to empty your bladder 2-3 hours before the appointment. If a woman has specific discharge or itching in the vagina, then the smear should be postponed until a complete cure.
The procedure for taking a smear for a cytological examination is the same as for taking a smear for the vaginal microflora. When conducting an internal gynecological examination, cells are taken from the inner and outer surfaces of the cervix using a special brush. The procedure itself is short (about 10 seconds) and practically imperceptible. In some women, as a result of scraping, the site of taking a smear may bleed a little for one to two days, which manifests itself as spotting spotting from the genital tract.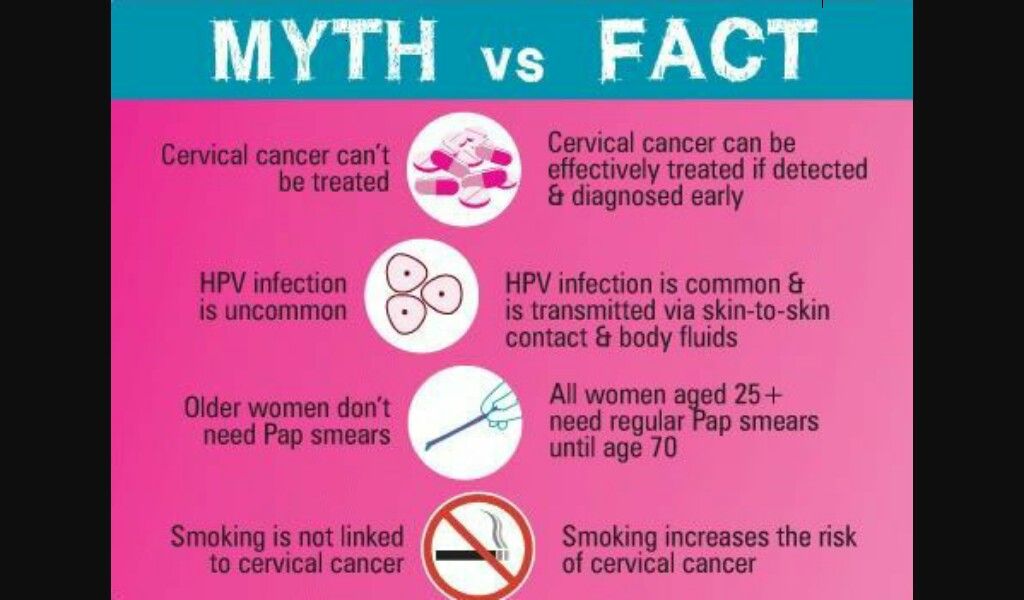 According to the results of a smear for cytology, an assessment of cervical cells is carried out - their number, shape, size, nature of location. All these parameters together give a complete picture of the general condition of the cervix and allow for an accurate diagnosis of background, cancerous and precancerous diseases of the cervix. The results of a smear are considered normal (negative) when absolutely all cells are of the correct shape and size, and no abnormal cells are found. If the results of the smear are bad, then the doctors put one of the following conclusions: “atypia”, “dysplasia of the 1st, 2nd or 3rd degree”. If dysplasia of the first degree is detected, a woman will need to retake the test after five to six months. If atypical (pathological, cancerous) cells are found in a smear for cytology, a woman will need an additional examination, which consists in repeating a cytological examination after a while, as well as in conducting a colposcopic examination with taking cervical tissues for a biopsy.
According to the results of a smear for cytology, an assessment of cervical cells is carried out - their number, shape, size, nature of location. All these parameters together give a complete picture of the general condition of the cervix and allow for an accurate diagnosis of background, cancerous and precancerous diseases of the cervix. The results of a smear are considered normal (negative) when absolutely all cells are of the correct shape and size, and no abnormal cells are found. If the results of the smear are bad, then the doctors put one of the following conclusions: “atypia”, “dysplasia of the 1st, 2nd or 3rd degree”. If dysplasia of the first degree is detected, a woman will need to retake the test after five to six months. If atypical (pathological, cancerous) cells are found in a smear for cytology, a woman will need an additional examination, which consists in repeating a cytological examination after a while, as well as in conducting a colposcopic examination with taking cervical tissues for a biopsy.