Cramping after internal ultrasound pregnant
Pain, Side Effects, and More
What is a sonohysterogram?
A sonohysterogram is an imaging study of the uterus. Your doctor inserts fluid into the uterus via the cervix to examine the uterine lining. This approach allows them to identify more structures than if ultrasound with no fluid was used.
This test is one example of imaging used to diagnose the cause of underlying pelvic pain, infertility, or vaginal bleeding.
Your doctor will recommend a sonohysterogram when they need to examine the structure of your uterus and its lining. Test uses range from testing for infertility to diagnosing the cause of uterine bleeding.
Your doctor may recommend a sonohysterogram for a variety of symptoms and conditions including:
- determining if your fallopian tubes are blocked
- examining the uterus if you’ve had miscarriages or have been unable to get pregnant
- examining scar tissue, such as endometriosis
- identifying abnormal growths, which could include uterine fibroids or polyps
- identifying irregularities in the uterine lining
- visualizing the shape of the uterus
Your OB-GYN typically performs the sonohysterogram at their office.
Before undergoing a sonohysterogram, your doctor will have you take a pregnancy test. You shouldn’t have a sonohysterogram if you’re pregnant or experiencing an inflammatory pelvic disorder.
The sonohysterogram is usually scheduled when you’re not on your period or experiencing vaginal bleeding. Both can affect how well your doctor can see the uterine lining.
The test is usually done one week after you start your period as this reduces infection risk. It’s also when the uterine lining is at its thinnest, which helps doctors identify abnormalities more easily.
You’ll be asked to empty your bladder before the test. You’ll lie down on an examination table or bed. Your doctor may perform a pelvic exam first to check for pain or the possibility of infection.
There are three main parts of a sonohysterogram:
- Performing an initial transvaginal ultrasound. A transvaginal ultrasound involves inserting a special ultrasound probe into the vagina.
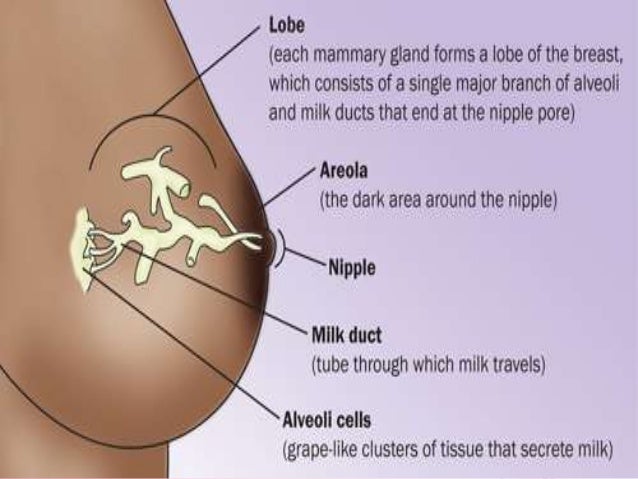
 The probe emits sound waves that recreate an image of the uterine lining. Your doctor will usually take an initial scan without any fluid in the uterus. The images are projected on the ultrasound screen.
The probe emits sound waves that recreate an image of the uterine lining. Your doctor will usually take an initial scan without any fluid in the uterus. The images are projected on the ultrasound screen. - Inserting fluid into the uterus. After your doctor examines the uterus with the ultrasound probe, they’ll insert a speculum in the vagina. This is a special tool designed to keep the vagina open, making it easier to reach the cervix on the way to the uterus. Your doctor will use a special swab to clean the inside of the cervix. They will then insert a tube that can send fluid to the cervical opening. The fluid will cause your uterus to enlarge slightly. It also makes the uterine lining — or endometrium —easier to visualize.
- Performing the ultrasound. Your doctor will once again insert the transvaginal ultrasound probe and use the tube to send more fluid through the vagina and into the uterus. You may experience some cramping when this fluid goes through the uterus.
 Your doctor will use the ultrasound to examine the uterine lining and sometimes note the flow of fluid from the uterus and into the fallopian tubes. They may use a special feature of the ultrasound, known as the Doppler ultrasound. This method allows your doctor to identify blood flow or blood flow blockages. The Doppler is useful in identifying blood clots as well as blood supplies to polyps and tumors.
Your doctor will use the ultrasound to examine the uterine lining and sometimes note the flow of fluid from the uterus and into the fallopian tubes. They may use a special feature of the ultrasound, known as the Doppler ultrasound. This method allows your doctor to identify blood flow or blood flow blockages. The Doppler is useful in identifying blood clots as well as blood supplies to polyps and tumors.
A sonohysterogram usually takes about a half hour, according to the American College of Obstetricians and Gynecologists.
You should be able to return to your usual activities almost immediately after undergoing a sonohysterogram.
The procedure doesn’t usually cause serious side effects that would interfere with work or school. You may wish to abstain from intercourse for a day or so if you have any discomfort. Any light bleeding you experience should stop within a couple of days.
You may experience some light bleeding or cramping following the procedure. This is because the tissues can become irritated from using the transvaginal ultrasound and from having fluid inserted in the uterus.
Most doctors advise taking anti-inflammatory drugs, such as ibuprofen or acetaminophen, to relieve discomfort.
You may experience a pelvic tissue infection after a sonohysterogram. Symptoms of this condition can include fever, pain, and unusual discharge from the vagina. You should call your OB-GYN if you have these symptoms after a sonohysterogram.
Because ultrasound uses sound waves instead of radiation, there’s no radiation exposure during the test.
A sonohysterogram is an alternative or a complementary diagnostic method to a magnetic resonance imaging (MRI) scan, hysteroscopy, or hysterosalpingogram (HSG).
In contrast to the sonohysterogram, an HSG is a radiology test that involves using X-rays. Your doctor performs this procedure by injecting radioactive dye into the uterus. If the fallopian tubes are open, the contrast dye fills the tubes and shows up on an X-ray.
This test is often recommended if your doctor can’t identify if there’s an abnormality of the fallopian tubes by looking at a sonohysterogram or if fertility issues are being investigated.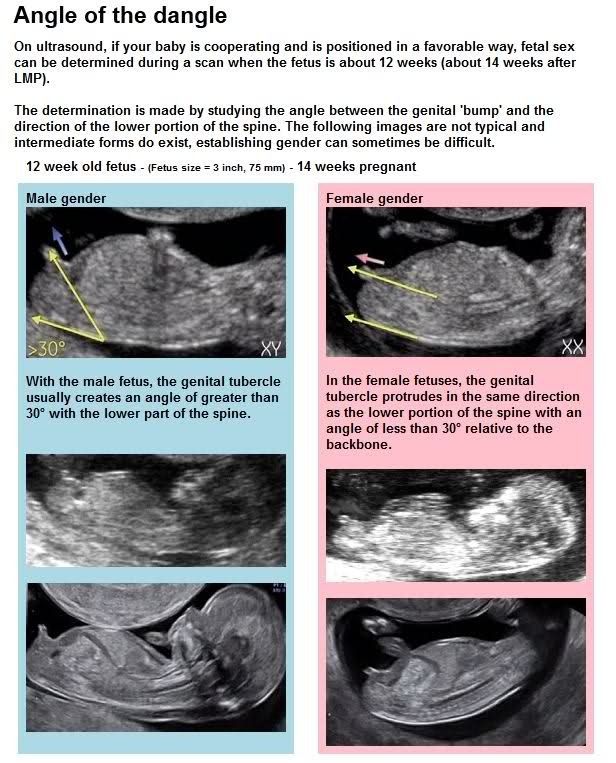
A sonohysterogram is a short, minimally invasive procedure that allows Your doctor to visualize the uterine lining. Your doctor may recommend follow-up testing or treatments depending on what they see during the ultrasound.
If you’ve been having trouble getting pregnant, and your doctor sees that your fallopian tubes are blocked, surgical repair or in vitro fertilization (IVF) might be options to discuss.
Cramps After Ultrasound | Abdominal Pain After Pregnancy Scan
Pregnancy comes with all sorts of new and strange sensations. Some are wonderful, like feeling your baby move for the first time. Some are not so great, like experiencing cramps after an ultrasound.
You’re not alone if you’re experiencing cramps after your ultrasound. Many women experience this after an ultrasound – especially if it is a transvaginal ultrasound. While it can be alarming, there’s usually no need to worry.
Read on to discuss the causes of cramping after an ultrasound and what you can do about it.
What Happens During an Ultrasound Procedure?
An ultrasound is a painless test that uses sound waves to create images of the inside of your body. It’s also called a sonogram. During an abdominal ultrasound, a gel is applied to your stomach area, and a hand-held device called a transducer is moved over your skin to produce the images.
The first ultrasound happens during the first trimester, usually between weeks nine and 12. This ultrasound is also called a dating scan because it helps your healthcare provider figure out how far along you are in your pregnancy. The second ultrasound usually happens during the second trimester, around week 20. It is sometimes called an anatomy scan because it gives a clear picture of the baby’s organs and structures.
Read this article on What exactly is an ultrasound and how does it work. It will help clear your doubts.
Why Do You Experience Cramping After an Ultrasound?
There are a few different reasons you might experience cramping after having an abdominal ultrasound.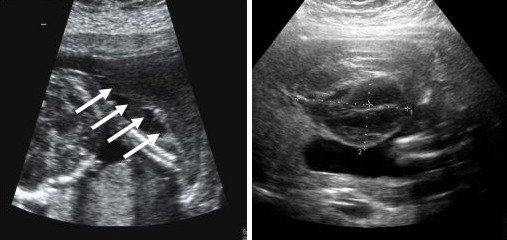 One possibility is that you could be constipated. The gel used during the procedure can sometimes cause constipation, so it’s essential to drink plenty of fluids and eat high-fiber foods in the days following your ultrasound.
One possibility is that you could be constipated. The gel used during the procedure can sometimes cause constipation, so it’s essential to drink plenty of fluids and eat high-fiber foods in the days following your ultrasound.
Another possibility is that you could be experiencing a minor soreness from lying on your back for an extended period. If this is the case, the cramping should subside within a day or two. The level of soreness depends on how much your pregnant belly was moved or prodded during the ultrasound.
You may feel uncomfortable during the ultrasound because you have to lie still on your back. If you’re having severe cramping or pain, it’s essential to call your healthcare provider.
How Can You Prepare for a Pleasant Ultrasound Experience?
If you’re dreading your upcoming ultrasound, there are a few things you can do to try and make the experience comfortable:
-Wear comfortable clothing: You’ll likely be asked to remove any clothing or jewelry that might get in the way of the transducer, but you can leave on anything that makes you feel more comfortable.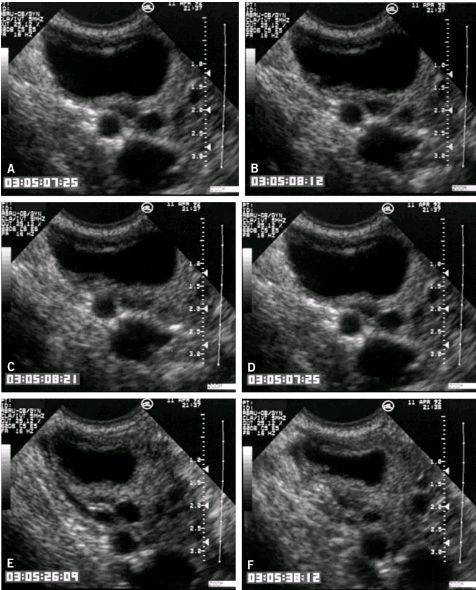
-Drink a Lot of Water: A full bladder is often necessary for certain types of ultrasounds. Drinking plenty of water beforehand will help make sure your bladder is nice and full. A full bladder pushes your intestines out of the way, which makes it easier to get a clear view of your baby.
Baby Dimensions provide the best ultrasounds in Atlanta. Our team is passionate about providing you with the best experience and service possible.
Diastasis of the rectus abdominis muscles and diastasis of the womb. Solvable problems of pregnancy. Interview with Doctor of Medical Sciences, Professor M.A. Chechnevoy
— What is muscle diastasis and what is pubic symphysis diastasis?
— Pregnancy is an amazing and wonderful time, but it is also a period of additional loads, which undoubtedly becomes a test of strength for the female body.
The previously existing everyday point of view that pregnancy rejuvenates and gives strength is not confirmed by anything. During the bearing of a child, significant additional loads are placed on the mother's body, which often lead to the manifestation of problems that were invisible before pregnancy.
During the bearing of a child, significant additional loads are placed on the mother's body, which often lead to the manifestation of problems that were invisible before pregnancy.
Diastasis of the rectus abdominis muscles is a divergence of the inner edges of the muscles along the white line of the abdomen (connective tissue structure) at a distance of more than 27 mm. Pubic diastasis is one of the manifestations of pregnancy-associated pelvic girdle pain. This pathology affects the entire pelvic ring, sacroiliac joints and symphysis. And they certainly have common causes for the appearance.
The formation of such problems is facilitated by a decrease in the strength of connective tissue collagen. One of the reasons is an innate predisposition, the so-called connective tissue dysplasia, when the tissues are very elastic, extensible. During pregnancy, the body of a woman increases the production of the hormone relaxin, which reduces the synthesis of collagen and enhances its breakdown. This is provided by nature to create maximum elasticity of the birth canal. However, other structures, such as the anterior abdominal wall and the pubic symphysis, also fall under the action of relaxin.
This is provided by nature to create maximum elasticity of the birth canal. However, other structures, such as the anterior abdominal wall and the pubic symphysis, also fall under the action of relaxin.
— How does diastasis of the muscles and diastasis of the pubis affect pregnancy and childbirth?
- The divergence of the rectus abdominis muscles is observed in about 40% of pregnant women. During pregnancy, it does not give serious complications that threaten the life of the mother or the condition of the fetus. However, the inferiority of the work of the rectus abdominis muscles forces the redistribution of the load on the back muscles, which can lead to lumbar-pelvic pain and, accordingly, discomfort in the back. During childbirth, the abdominal muscles are involved in attempts, and the violation of their anatomy and function can affect the birth act.
With diastasis of the pubis, things are more complicated. As already mentioned, this is only one of the manifestations of a violation of the structure and function of the pubic joint (symphysiopathy) during pregnancy. It occurs in about 50% of pregnant women in varying degrees of severity: in 25% of cases it leads to restriction of the mobility of the pregnant woman, in 8% - to severe disorders up to disability.
It occurs in about 50% of pregnant women in varying degrees of severity: in 25% of cases it leads to restriction of the mobility of the pregnant woman, in 8% - to severe disorders up to disability.
With symphysiopathy, the ligaments of the pubic articulation and the cartilages that connect the pubic bones are affected. All this leads to severe pain in the pubic joint, pelvic bones, lower back, as well as to a violation of gait and the inability to stand up or lie down without outside help. Women with pelvic girdle pain syndrome experience significant levels of discomfort, disability, and depression, with associated social and economic problems. These include impaired sexual activity during pregnancy, chronic pain syndrome, risk of venous thromboembolism due to prolonged immobility, and even seeking early induction of labor or caesarean section to stop pain.
During childbirth, this patient may experience rupture of the pubic symphysis and may require surgery to repair it.
— How to prevent the development of muscle and pelvic diastasis during pregnancy and childbirth? What factors increase the likelihood of its development?
- There is no recipe that will be one hundred percent. There is a wonderful term in the medical literature called "lifestyle modification". Whatever diseases we study, be it symphysiopathy, diabetes mellitus or preeclampsia, the risk group for pathology is always overweight women. You need to prepare for pregnancy, you need to be in good physical shape. During pregnancy, weight gain should be monitored. The recommendation to "eat for two" is not just wrong, but extremely harmful. Pregnant women should maintain reasonable physical activity. Weak and flabby abdominal muscles, combined with the large size of the fetus, undoubtedly increase the risk of diastasis.
The risk factors for symphysiopathy in numerous studies are hard physical labor and previous injuries of the pelvic bones. Factors such as time elapsed from previous pregnancies, smoking, use of hormonal contraception, epidural anesthesia, mother's ethnicity, number of previous pregnancies, bone density, weight and gestational age of the fetus (post-term fetus) are not associated with an increased risk of symphysiopathy.
— How to diagnose diastasis recti and diastasis pubis?
— In most cases, diastasis rectus abdominis can be diagnosed clinically. It happens that inspection, palpation and simple measurements are enough.
In the standing position, you can see the divergence of the muscles when the woman does not have subcutaneous fat. In this case, diastasis is defined as a vertical defect between the rectus muscles.
With tension of the abdominal press, a longitudinal protrusion is observed in the diastasis zone. Such a protrusion is especially noticeable if the patient in the supine position is asked to raise her head and legs. If necessary, you can measure the width of the defect simply with a ruler.
Ultrasound may be the most accurate diagnostic method. With ultrasound, the inner edges of the rectus muscles are clearly visible and the distance between them at different levels can be measured.
Computed tomography is used in the diagnosis of diastasis extremely rarely, mainly in scientific research.
For the diagnosis of symphysiopathy and diastasis pubis there is no one test as a "gold standard".
The first place, of course, is the questioning and examination of the patient. We pay attention to the gait of the pregnant woman, to how she sits down, lies down and how she gets up. Symphysiopathy is characterized by a “duck gait”, when a pregnant woman rolls from foot to foot. On palpation in the area of the womb, pain and swelling are noted. The so-called pain provocative tests are used, for example, a mat-test (pulling up an imaginary rug, mat with your foot towards you).
The following questionnaires are used to assess quality of life, pain and disability: Health-Related Quality of Life (HRQL), Oswestry Disability Index (ODI), Disability Rating Index (DRI), Edinburgh Postpartum Depression Scale (EPDS), Pregnancy Mobility Index (PMI), and Pelvic Ring Score (PGQ).
Of the instrumental methods, ultrasound is the most widely used, less often computed or magnetic resonance imaging. Ultrasound allows you to assess the condition of the ligaments of the pubic joint and the interpubic disc, the severity of the changes and the risk of natural childbirth.
Ultrasound allows you to assess the condition of the ligaments of the pubic joint and the interpubic disc, the severity of the changes and the risk of natural childbirth.
— What is the treatment for diastasis recti or pubis?
— Primary prevention: when planning and during pregnancy, it is necessary to strengthen all muscle groups of the pelvic girdle, as well as the pelvic diaphragm.
More often, diastasis of the rectus muscles disappears on its own during the first months after childbirth. Special physical exercises to correct the work of muscles, to tone them and restore their basic functions should be performed under the guidance of a competent instructor. There are types of physical exercises that can, on the contrary, worsen the situation with diastasis of the rectus abdominis muscles. In some cases, when there is no effect from physiotherapy exercises, it is necessary to resort to surgical correction of the defect. Currently, both endoscopic and open surgery are practiced. The choice of method depends on the size and localization of the defect.
The choice of method depends on the size and localization of the defect.
With symphysiopathy, therapeutic exercises reduce lumbar and pelvic pain. Acupuncture and wearing a pelvic bandage have a positive effect on symphysiopathy.
Initial treatment of pubic symphysis should be conservative even if symptoms are severe. Treatment includes bed rest and the use of a pelvic brace or corset that tightens the pelvis. Early appointment of physiotherapy with dosed therapeutic exercises will help to avoid complications associated with prolonged immobilization. Walking should be done with assistive devices such as walkers.
In most cases (up to 93%), the symptoms of dysfunction of the pelvic ring, including the pubic joint, progressively subside and completely disappear six months after birth. In other cases, it persists, becoming chronic. However, if the diastasis exceeds 40 mm, then surgical treatment may be required. Most studies recommend surgery only after failure of conservative treatment, inadequate enlargement of diastasis, or its recurrence. Several procedures have been described, including external fixation and open reduction of the pubic bones with internal fixation.
Several procedures have been described, including external fixation and open reduction of the pubic bones with internal fixation.
The best advice for prevention, diagnosis and treatment: ask a competent doctor all the questions that worry you. Only the joint efforts of the doctor and the patient can overcome all problems and find the best solutions.
Leg cramps - symptoms, causes, treatment, first aid, what to do with cramps
Cramping is familiar to most people, it is an unpleasant sensation that is caused by involuntary muscle contraction. It lasts, as a rule, not for long, but it delivers a lot of negative emotions.
What are convulsions?
This is a sharp contraction of the muscles, which is not subject to a simple relaxing effort. The cramp is accompanied by pain, can last from a few seconds to ten minutes. With a strong muscle contraction, a large amount of decay products are released, this is the biological mechanism of convulsions.
What are the causes of seizures
This condition can occur both in patients and in completely healthy people. Muscle contraction can be localized or generalized, when entire muscle groups are affected. In children, such convulsions occur at high temperatures, and in adults, a similar condition is a sign of a serious illness of the nervous system.
Causes of seizures include:
- Deficiency of certain vitamins and minerals, most commonly calcium or magnesium;
- Sedentary lifestyle or too intense exercise;
- Pregnancy and related changes in the female body;
- Taking certain medicines that remove potassium salts from the body;
- Various diseases, including diabetes, varicose veins, overweight and flat feet.
If you are concerned about frequent cramps of the limbs, contact a specialist who will find out the cause of the unpleasant phenomena.
What to do with night cramps?
If a muscle has cramped, it will be impossible to consciously relax it. The only way is to use physical force: straighten your toes with your hands or pull the toe of your foot towards you. After the cramp has passed, the limb can be massaged, this will help restore normal blood circulation.
The only way is to use physical force: straighten your toes with your hands or pull the toe of your foot towards you. After the cramp has passed, the limb can be massaged, this will help restore normal blood circulation.
How to prevent seizures?
Prevention of seizures exists if you understand the risk of their occurrence and the reason that can lead to this. For example, with flat feet, it is important to choose the right shoes and use orthopedic insoles. With varicose veins - avoid excessive physical activity. During pregnancy - observe the regimen and take the necessary vitamins. In any case, if you want to avoid night cramps, you need to adjust your diet to include foods rich in potassium, calcium and magnesium. Instead of sweets, give preference to dried apricots and dates.
Diagnosis of the cause of seizures
In case of an unpleasant condition, it is first of all recommended to contact a therapist who will prescribe a series of tests and conduct the necessary diagnostics.