Bleeding cervix pregnancy
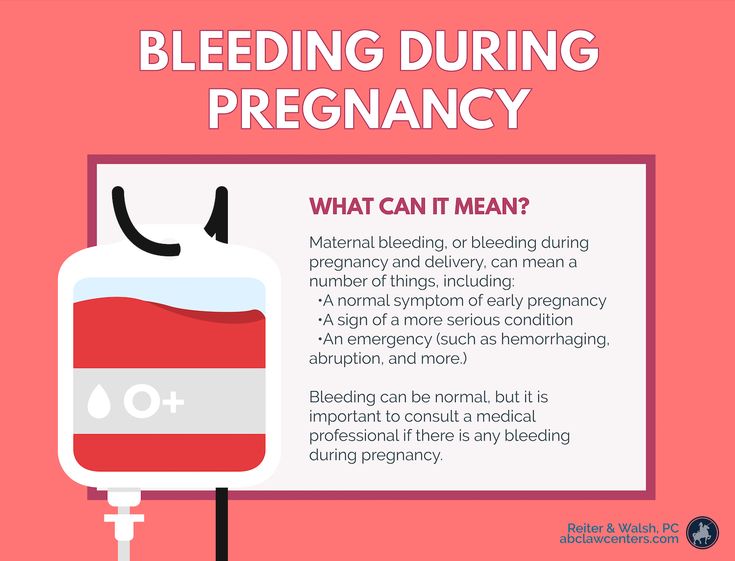
Bleeding and spotting from the vagina during pregnancy
Bleeding and spotting from the vagina during pregnancy are common
If you bleed or spot during pregnancy, it doesn’t always mean there’s a problem but in some cases they may be signs of a problem for you or your baby’s health
If you have heavy bleeding, call your health care provider right away
Tell your provider about any bleeding or spotting you have during pregnancy
Bleeding and spotting from the vagina during pregnancy are common. Up to 1 out of 4 (up to 25%) of all pregnant women have some bleeding or spotting during their pregnancy.
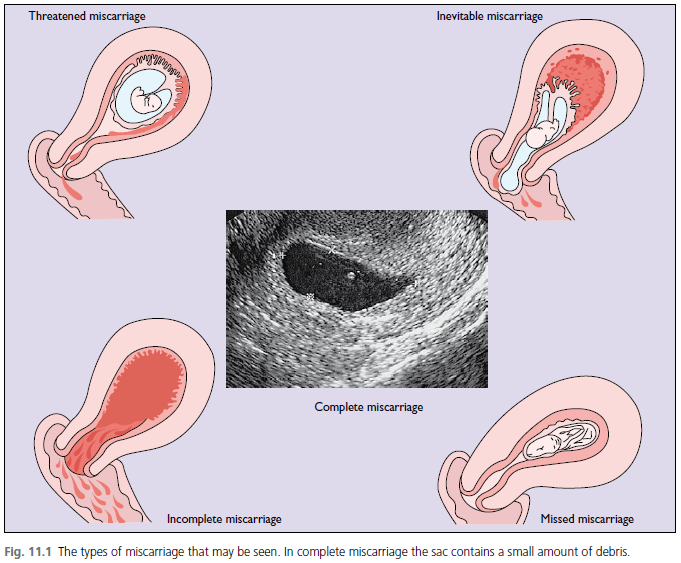
Bleeding and spotting in pregnancy don’t always mean there’s a problem, but they can be a sign of miscarriage or other serious complications. Miscarriage is when a baby dies in the womb before 20 weeks of pregnancy.
Call your health care provider if you have any bleeding or spotting, even if it stops. It may not be caused by anything serious, but your provider needs to find out what’s causing it.
What’s the difference between bleeding and spotting?
Bleeding or spotting can happen anytime, from the time you get pregnant to right before you give birth. Spotting is light bleeding. It happens when you have a few drops of blood on your underwear. Spotting is so light that the blood wouldn’t cover a panty liner. Bleeding is when the blood flow is heavier, enough that you need a panty liner or pad to keep the blood from soaking your underwear and clothes.
What should you do if you have bleeding or spotting during pregnancy?
Call your health care provider if you have any kind of bleeding during pregnancy and do these things:
- Keep track of how heavy your bleeding is, if it gets heavier or lighter, and how many pads you are using.
- Check the color of the blood. Your provider may want to know. It can be different colors, like brown, dark or bright red.
- Don’t use a tampon, douche or have sex when you’re bleeding.
Call your health care provider right away at any time during pregnancy or go to the emergency room if you have:
- Heavy bleeding
- Bleeding with pain or cramping
- Dizziness and bleeding
- Pain in your belly or pelvis
What causes bleeding or spotting early in pregnancy?
It’s normal to have some spotting or bleeding early in pregnancy. Bleeding or spotting in the first trimester may not be a problem. It can be caused by:
- Having sex
- An infection
- Implantation. When a fertilized egg (embryo) attaches to the lining of the uterus (womb) and begins to grow.
- Hormone changes. Hormones are chemicals made by the body.
- Changes in your cervix. The cervix is opening to the uterus that sits at the top of the vagina.
- Certain types of testing during pregnancy like an amniocentesis or Chorionic villus sampling (CVS). These are tests that are done to check for genetic abnormalities in your baby.
 Genetic abnormalities are changes in the genes that are passed down to a baby from mom or dad. These genetic changes can cause health problems for a baby.
Genetic abnormalities are changes in the genes that are passed down to a baby from mom or dad. These genetic changes can cause health problems for a baby. - Problems related to smoking. If you smoke, it’s best to stop before pregnancy or as soon as you know you’re pregnant.
Sometimes bleeding or spotting in the first trimester is a sign of a serious problem, like:
- Miscarriage. Almost all women who miscarry have bleeding or spotting before the miscarriage.
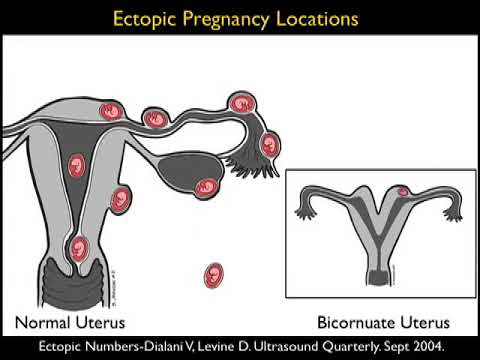
- Ectopic pregnancy. This is when a fertilized egg implants itself outside of the uterus and begins to grow. An ectopic pregnancy cannot result in the birth of a baby. It can cause serious, dangerous problems for the pregnant woman.
- Molar pregnancy. This is when a mass of tissue forms inside the womb, instead of a baby. Molar pregnancy is rare.
What causes bleeding or spotting later in pregnancy?
Bleeding or spotting later in pregnancy may be caused by:
- Labor
- Having sex
- An internal exam by your health care provider
- Problems with the cervix, like an infection, growths, inflammation or cervical insufficiency.
 This is when a woman’s cervix opens too early. Inflammation of the cervix is when it may be painful, swollen, red or irritated.
This is when a woman’s cervix opens too early. Inflammation of the cervix is when it may be painful, swollen, red or irritated.
Bleeding or spotting later in pregnancy may be a sign of a serious problem, like:
- Preterm labor. This is labor that happens too early, before 37 weeks of pregnancy.
- Placenta previa. This is when the placenta lies very low in the uterus and covers all or part of the cervix.
- Placenta accreta. This is when the placenta grows into the wall of the uterus too deeply.
- Placental abruption. This is when the placenta separates from the wall of the uterus before birth.
- Uterine rupture. This is when the uterus tears during labor. This happens very rarely. It can happen if you have a scar in the uterus from a prior cesarean birth (also called c-section) or another kind of surgery on the uterus.
 A c-section is surgery in which your baby is born through a cut that your doctor makes in your belly and uterus.
A c-section is surgery in which your baby is born through a cut that your doctor makes in your belly and uterus.
How are bleeding and spotting treated?
Your treatment depends on what caused your bleeding. You may need a medical exam and tests.
Most of the time, treatment for bleeding or spotting is rest. Your provider may also suggest treatments like:
- Take time off from work and stay off your feet for a little while
- You may need medicine to help protect your baby from Rh disease. Rh disease is when your blood and baby’s blood are incompatible (can’t be together). This disease can cause serious problems — even death — for your baby.
- Don’t have sex, douche or use tampons
- If you have heavy bleeding, you may need a hospital stay or surgery
Last reviewed April 2020
Vaginal bleeding in pregnancy Information | Mount Sinai
Pregnancy - vaginal bleeding; Maternal blood loss - vaginal
Vaginal bleeding in pregnancy is any discharge of blood from the vagina during pregnancy.
The ultrasound has become a standard procedure used during pregnancy. It can demonstrate fetal growth and can detect increasing numbers of conditions in the fetus including meningomyelocele, congenital heart disease, kidney abnormalities, hydrocephalus, anencephaly, club feet, and other deformities. Ultrasound does not produce ionizing radiation and is considered a very safe procedure for both the mother and the fetus.
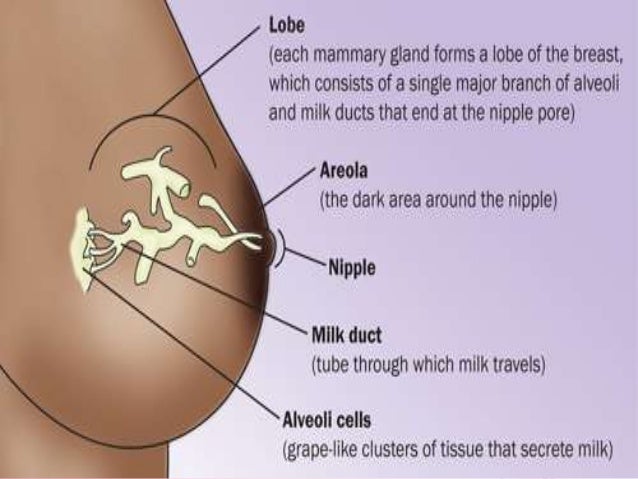
External structures of the female reproductive anatomy include the labium minora and majora, the vagina and the clitoris. Internal structures include the uterus, ovaries, and cervix.
Internal structures include the uterus, ovaries, and cervix.
The placenta provides the fetus with oxygen and nutrients and takes away waste such as carbon dioxide via the umbilical cord.
Placenta previa is a condition of pregnancy when the placenta implants in the lower part of the uterus, partly or completely obstructing the cervical outlet to the vagina (birth canal).
There are many possible causes of bleeding during pregnancy. Bleeding should always be evaluated by a health care provider.
Considerations
Up to 1 in 4 women have vaginal bleeding at some time during their pregnancy. Bleeding is more common in the first 3 months (first trimester), especially with twins.
Causes
A small amount of light spotting or bleeding may be noted 10 to 14 days after conception. This spotting results from the fertilized egg attaching itself to the lining of the uterus. Assuming it is light and does not last very long, this finding is most often nothing to be concerned about.
This spotting results from the fertilized egg attaching itself to the lining of the uterus. Assuming it is light and does not last very long, this finding is most often nothing to be concerned about.
During the first 3 months, vaginal bleeding may be a sign of a miscarriage or ectopic pregnancy. Contact the health care provider right away.
During months 4 to 9, bleeding may be a sign of:
- The placenta separating from the inner wall of the uterus before the baby is born (abruptio placentae)
- Miscarriage
- The placenta covering all or part of the opening to the cervix (placenta previa)
- Vasa previa (baby's blood vessels exposed across or near the internal opening of the uterus)
Other possible causes of vaginal bleeding during pregnancy:
- Cervical polyp or growth
- Early labor (bloody show)
- Ectopic pregnancy
- Infection of the cervix
- Trauma to the cervix from intercourse (small amount of bleeding) or recent pelvic exam
Home Care
Avoid sexual intercourse until your provider tells you that it is safe to start having intercourse again.
Consume only fluids if the bleeding and cramping are severe.
You may need to cut down your activity or be put on bed rest at home. Your provider will talk to you about the specific kinds of activity changes you may need to make.
Medicine is not needed in most cases. DO NOT take any medicine without talking with your provider.
Also, talk to your provider about what to look for, such as the amount of bleeding and color of the blood.
When to Contact a Medical Professional
Contact your provider if:
- You have any vaginal bleeding during pregnancy. Treat this as a potential emergency.
- You have vaginal bleeding and have placenta previa (get to the hospital right away).
- You have cramps or labor pains.
What to Expect at Your Office Visit
Your provider will take a medical history and perform a physical exam.
You will probably have a pelvic exam, or ultrasound as well.
Tests that may be done include:
- Blood tests
- Pregnancy ultrasound
- Ultrasound of the pelvis
You may be referred to a high risk specialist for the duration of the pregnancy.
Francois KE, Foley MR. Antepartum and postpartum hemorrhage.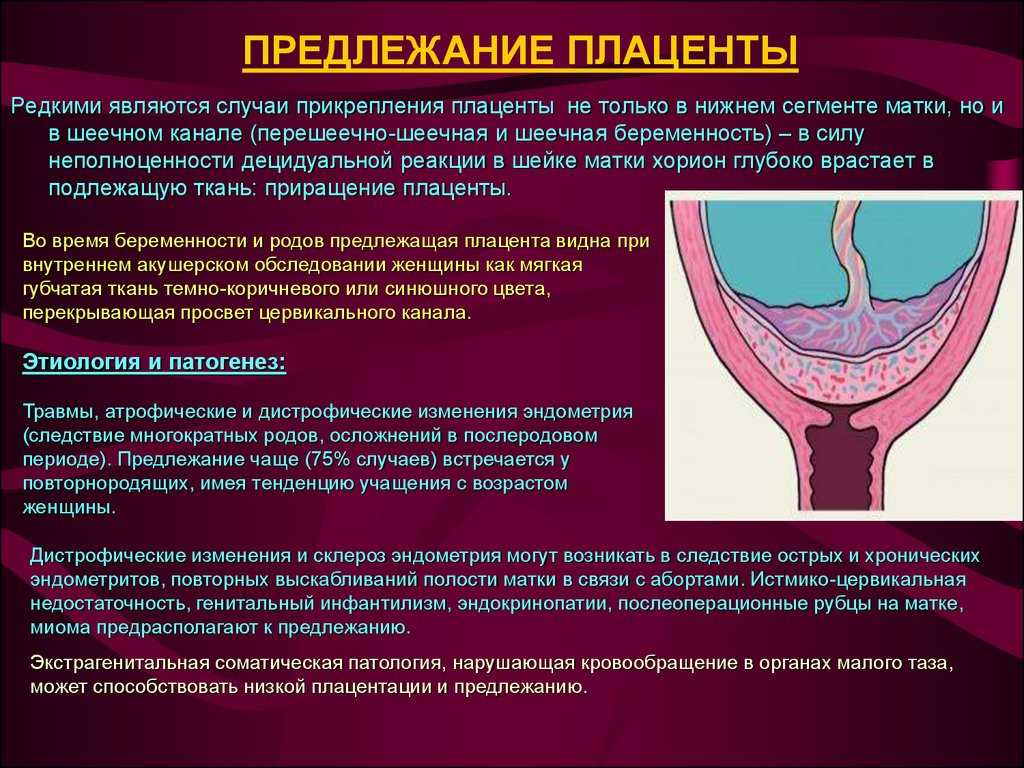 In: Landon MB, Galan HL, Jauniaux ERM, et al, eds. Gabbe's Obstetrics: Normal and Problem Pregnancies. 8th ed. Philadelphia, PA: Elsevier; 2021:chap 18.
In: Landon MB, Galan HL, Jauniaux ERM, et al, eds. Gabbe's Obstetrics: Normal and Problem Pregnancies. 8th ed. Philadelphia, PA: Elsevier; 2021:chap 18.
Salhi BA, Nagrani S. Acute complications in pregnancy. In: Walls RM, Hockberger RS, Gausche-Hill M, eds. Rosen's Emergency Medicine: Concepts and Clinical Practice. 9th ed. Philadelphia, PA: Elsevier; 2018:chap 178.
Turocy J, Williams Z. Early and recurrent pregnancy loss: etiology, diagnosis, treatment. In: Gershenson DM, Lentz GM, Valea FA, Lobo RA, eds. Comprehensive Gynecology. 8th ed. Philadelphia, PA: Elsevier; 2022:chap 16.
Last reviewed on: 1/10/2022
Reviewed by: John D. Jacobson, MD, Department of Obstetrics and Gynecology, Loma Linda University School of Medicine, Loma Linda, CA. Also reviewed by David Zieve, MD, MHA, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
The question is asked by Anya, - a question-answer from the specialists of the clinic "Mother and Child"
10/23/2014
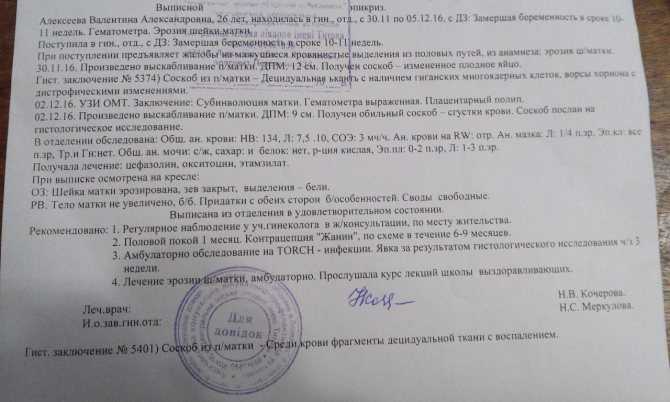
Hello! I have a second pregnancy (my son is 1 year 2 months), the term is 13-14 weeks.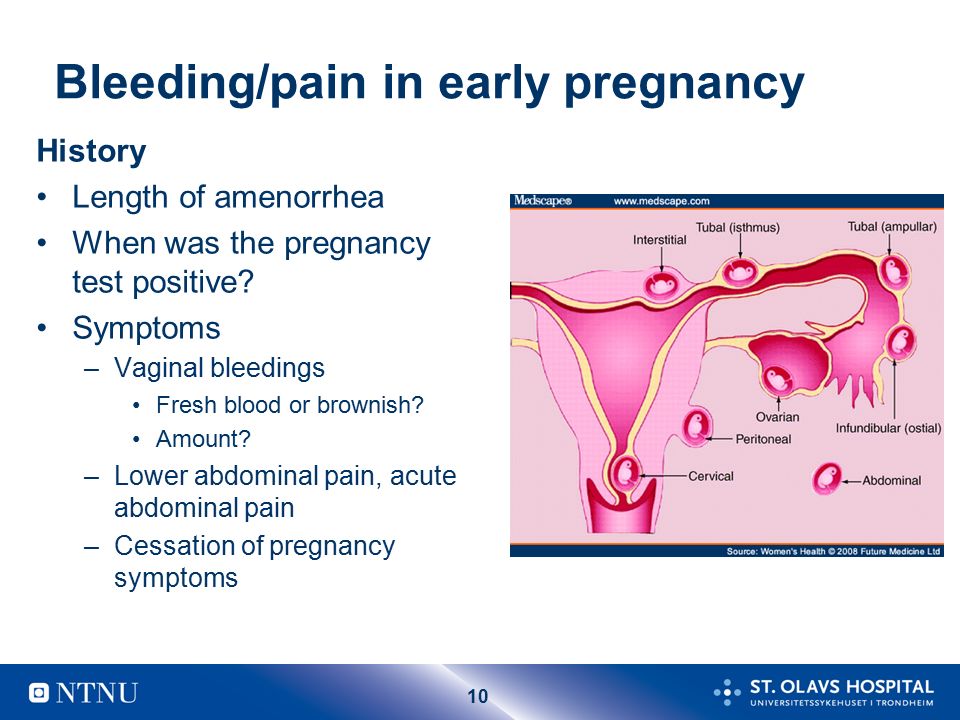 At the 11th week, heavy bleeding began (until that time, nothing bothered) and I was admitted to the hospital with a diagnosis of “beginning miscarriage.” Heavy bleeding lasted from 13.00 to 16.00, then it bled a little all the next day, and on the third day the discharge began to darken and disappeared. The next morning after admission, I had an ultrasound scan (06/04/05), which showed: The uterus in anteflexio, with clear, even contours, rounded, enlarged due to pregnancy and according to its duration. Meometrium of normal structure and echogenicity, without nodules and retrochorial hematomas, in which one live embryo is visualized. The placenta is formed on the right side with the transition to the anterior wall of the uterus, up to 1.2 m thick. The amount of water is normal. The internal os of the uterus is completely closed. The results of the analyzes: Cl. blood test: Er - 4, 15; Hb - 124; Ht - 35, 8; L-9, four; P - 6; C - 73; L - 18; M-3; E-0; ESR - 22. General analysis of urine: Specified weight -1010, PH - Neutral; Protein, Glucose, erythrocytes - neg; L - 1-2-1; epithelium singly.
At the 11th week, heavy bleeding began (until that time, nothing bothered) and I was admitted to the hospital with a diagnosis of “beginning miscarriage.” Heavy bleeding lasted from 13.00 to 16.00, then it bled a little all the next day, and on the third day the discharge began to darken and disappeared. The next morning after admission, I had an ultrasound scan (06/04/05), which showed: The uterus in anteflexio, with clear, even contours, rounded, enlarged due to pregnancy and according to its duration. Meometrium of normal structure and echogenicity, without nodules and retrochorial hematomas, in which one live embryo is visualized. The placenta is formed on the right side with the transition to the anterior wall of the uterus, up to 1.2 m thick. The amount of water is normal. The internal os of the uterus is completely closed. The results of the analyzes: Cl. blood test: Er - 4, 15; Hb - 124; Ht - 35, 8; L-9, four; P - 6; C - 73; L - 18; M-3; E-0; ESR - 22. General analysis of urine: Specified weight -1010, PH - Neutral; Protein, Glucose, erythrocytes - neg; L - 1-2-1; epithelium singly.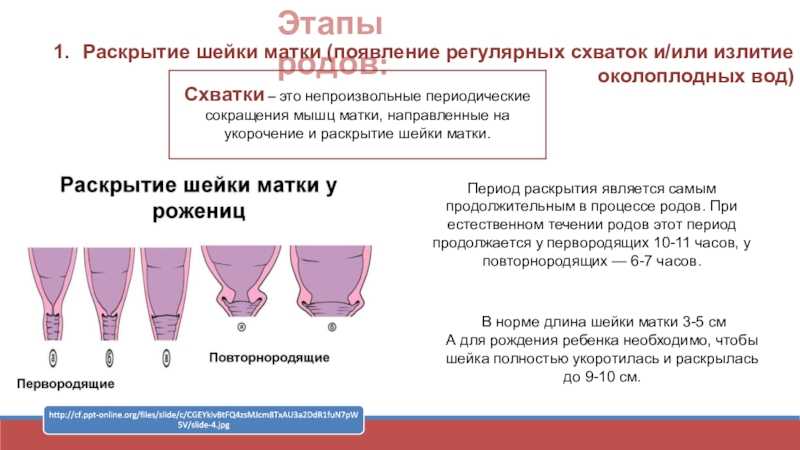 Biochem. blood test: Common. Protein - 65.0; Urea - 3, 2; Creatinine - 76; Bilirubin - 12-0-12; Alat - 23; AsAt - 59; Glucose - 3, 4. Gr. Blood A (II) Rh - factor positive. RW, HIV, HBs Ag - negative, DHA - 1.88. Treatment was prescribed: No-shpa 2, 0-3 times / m, papaverine 2 times, utrozhestan 1 t - 2 times, Vite 1-3 times, dicynone 2, 0 - 2 times / m, valerian 1 - 3 times, dexamethasone ½ tab. H night, magneB6 2-3 times, Materna 1. a day. While I was in the hospital, I bled a little bit a couple of times, and every day there were periodically pulling pains and tingling in the lower abdomen. She was discharged after 2 weeks, the medications were the same (except for decinone). The next day after discharge, dark brown discharge appeared again, on the same day I did a new ultrasound (06/20/05) results: Pregnancy 14 weeks, One live embryo is determined in the uterine cavity, the size of the fetus is proportional and corresponds to a period of 12 weeks. Rhythmic heartbeat 10 beats/min.
Biochem. blood test: Common. Protein - 65.0; Urea - 3, 2; Creatinine - 76; Bilirubin - 12-0-12; Alat - 23; AsAt - 59; Glucose - 3, 4. Gr. Blood A (II) Rh - factor positive. RW, HIV, HBs Ag - negative, DHA - 1.88. Treatment was prescribed: No-shpa 2, 0-3 times / m, papaverine 2 times, utrozhestan 1 t - 2 times, Vite 1-3 times, dicynone 2, 0 - 2 times / m, valerian 1 - 3 times, dexamethasone ½ tab. H night, magneB6 2-3 times, Materna 1. a day. While I was in the hospital, I bled a little bit a couple of times, and every day there were periodically pulling pains and tingling in the lower abdomen. She was discharged after 2 weeks, the medications were the same (except for decinone). The next day after discharge, dark brown discharge appeared again, on the same day I did a new ultrasound (06/20/05) results: Pregnancy 14 weeks, One live embryo is determined in the uterine cavity, the size of the fetus is proportional and corresponds to a period of 12 weeks. Rhythmic heartbeat 10 beats/min.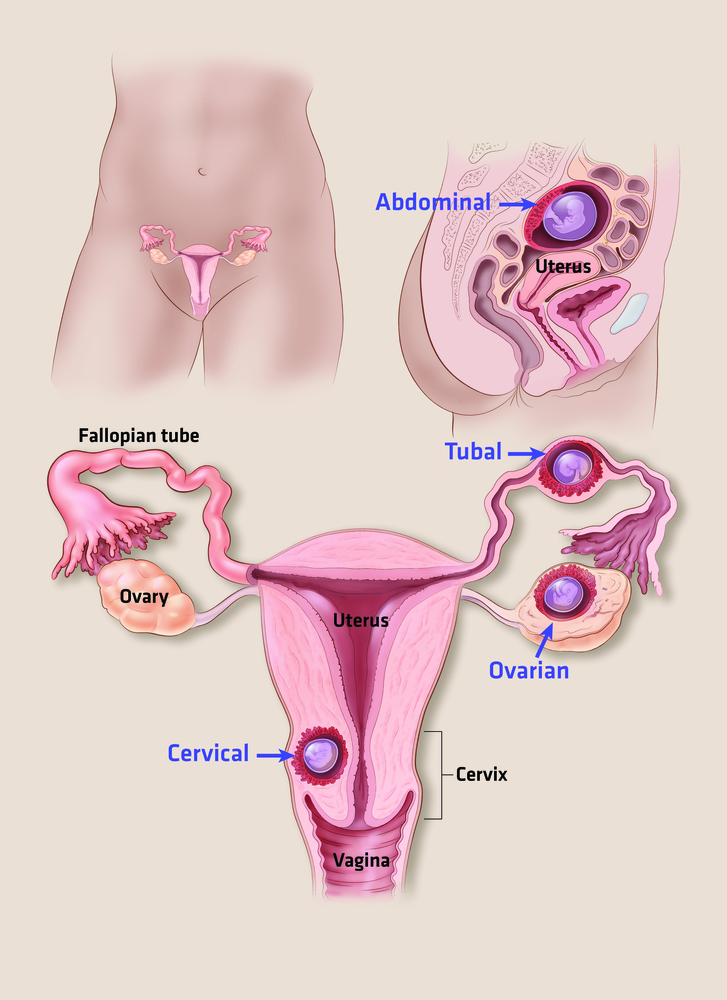 Motor activity is determined by malformations not identified. Chorion along the anterior wall of the uterus On the degree of maturity. The thickness of the placenta is 16 mm. The tone of the myometrium is slightly increased along the anterior wall. The cervix is not shortened. The cervical canal is closed. I have a few questions: How might such a threat affect a child's development? What additional tests should be taken to clarify the cause of the threat? How long to take the prescribed medication in this amount? Could the short period between pregnancies be the cause of the threat? Thank you for your advice
Motor activity is determined by malformations not identified. Chorion along the anterior wall of the uterus On the degree of maturity. The thickness of the placenta is 16 mm. The tone of the myometrium is slightly increased along the anterior wall. The cervix is not shortened. The cervical canal is closed. I have a few questions: How might such a threat affect a child's development? What additional tests should be taken to clarify the cause of the threat? How long to take the prescribed medication in this amount? Could the short period between pregnancies be the cause of the threat? Thank you for your advice
Clinic "Mother and Child" Kuntsevo:
01/27/2021
The presence of short-term bleeding during pregnancy with normal blood tests and ultrasound data (adequate fetal development, absence of detachment of the placenta) does not have a negative effect on the fetus. In such cases, it is necessary to exclude inflammation of the vagina, a decidual polyp of the cervical canal, when spotting does not occur from the uterus, but is external in nature and is not associated with problems of the fetal egg.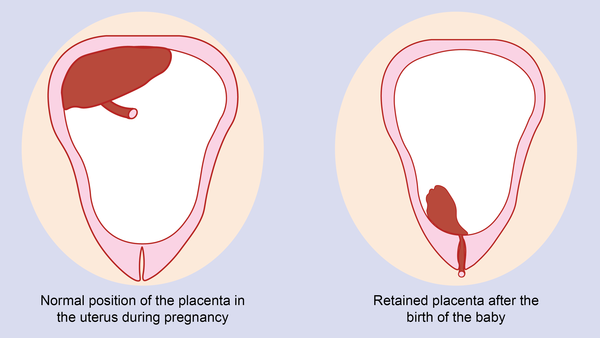 Nevertheless, in your case, it is better to follow a sparing regimen, take antispasmodics (no-shpu, magnesium B6, soothing herbs, continue taking utrogestan until 16 weeks of pregnancy, dexamethasone. With normal health and ultrasound data after 16 weeks, gradually cancel utrogestan, antispasmodics, magnesium B6).
Nevertheless, in your case, it is better to follow a sparing regimen, take antispasmodics (no-shpu, magnesium B6, soothing herbs, continue taking utrogestan until 16 weeks of pregnancy, dexamethasone. With normal health and ultrasound data after 16 weeks, gradually cancel utrogestan, antispasmodics, magnesium B6).
Bleeding early in pregnancy | Mamovedia
It is good when the pregnancy goes smoothly and without complications. However, it often happens that unpleasant moments occur during pregnancy, including uterine or vaginal bleeding.
Experts say that bleeding is most dangerous at the beginning of pregnancy. But at the same time, it is necessary to take into account the fact that not any bleeding at the beginning of pregnancy is dangerous and indicates a pathology.
Most bleeding, but not all, require immediate medical attention.
At the very beginning of pregnancy, minor bleeding can be considered normal, since they do not pose a danger to the normal course of pregnancy. This is due to the fact that the beginning of pregnancy is the time of a global restructuring of the woman's body, both at the hormonal and physiological levels. When the fetal egg is fixed in the wall of the uterus, then small fragments of its mucous membrane can be rejected. This is the cause of minor bleeding from the vagina. Such discharge can be brown, brown or bright red. Normally, they are insignificant and are not accompanied by pain.
This is due to the fact that the beginning of pregnancy is the time of a global restructuring of the woman's body, both at the hormonal and physiological levels. When the fetal egg is fixed in the wall of the uterus, then small fragments of its mucous membrane can be rejected. This is the cause of minor bleeding from the vagina. Such discharge can be brown, brown or bright red. Normally, they are insignificant and are not accompanied by pain.
But, in any case, if you have any bleeding during pregnancy (even the smallest), you should consult a doctor. This is necessary in order to make sure that the condition of the fetus is not disturbed, the pregnancy is proceeding normally, and there is no threat of miscarriage.
One of the most common causes of bleeding in early pregnancy in many women is cervical erosion. The mucous membrane of the cervix at the beginning of pregnancy may bleed, as there is increased blood flow to the uterus. With erosion of the cervix during pregnancy, the inflammatory process is activated.
If a woman has cervical erosion, then bleeding at the beginning of pregnancy may occur due to physical exertion, after sexual contact, or just out of the blue. With such bleeding, there are no painful sensations, and the discharge is insignificant and quickly stops spontaneously.
The presence of cervical canal polyps and decidua polyps can also lead to bleeding at the beginning of pregnancy. Such polyps are considered harmless tumors on the uterus or cervix. Blood discharge is also not plentiful and there is no pain.
More severe complications of the first trimester of pregnancy are vaginal bleeding, which may threaten miscarriage or signal an ectopic pregnancy.
Dangerous bleeding at the beginning of pregnancy is discharge that occurs with pathologies of the cervix, with varicose veins of the external genital organs, as well as with various infections of the vagina.
Precisely because a pregnant woman should know that any bleeding should be a reason for immediate medical attention.