Can gestational diabetes go away
Gestational Diabetes and Pregnancy | CDC
Gestational diabetes is a type of diabetes that is first seen in a pregnant woman who did not have diabetes before she was pregnant. Some women have more than one pregnancy affected by gestational diabetes. Gestational diabetes usually shows up in the middle of pregnancy. Doctors most often test for it between 24 and 28 weeks of pregnancy.
Often gestational diabetes can be managed through eating healthy foods and regular exercise. Sometimes a woman with gestational diabetes must also take insulin.
Learn more about Diabetes Self-Management Education and Support Services
Blood sugar that is not well controlled in a woman with gestational diabetes can lead to problems for the pregnant woman and the baby:
An Extra-Large Baby
Diabetes that is not well controlled causes the baby’s blood sugar to be high. The baby is “overfed” and grows extra-large. Besides causing discomfort to the woman during the last few months of pregnancy, an extra-large baby can lead to problems during delivery for both the mother and the baby. The mother might need a C-Section to deliver the baby. The baby can be born with nerve damage due to pressure on the shoulder during delivery.
C-Section (Cesarean Section)
A C-section is an operation to deliver the baby through the mother’s belly. A woman who has diabetes that is not well controlled has a higher chance of needing a C-section to deliver the baby. When the baby is delivered by a C-section, it takes longer for the woman to recover from childbirth.
High Blood Pressure (Preeclampsia)
When a pregnant woman has high blood pressure, protein in her urine, and often swelling in fingers and toes that doesn’t go away, she might have preeclampsia. It is a serious problem that needs to be watched closely and managed by her doctor. High blood pressure can cause harm to both the woman and her unborn baby. It might lead to the baby being born early and also could cause seizures or a stroke (a blood clot or a bleed in the brain that can lead to brain damage) in the woman during labor and delivery. Women with diabetes have high blood pressure more often than women without diabetes.
Women with diabetes have high blood pressure more often than women without diabetes.
Low Blood Sugar (Hypoglycemia)
People with diabetes who take insulin or other diabetes medications can develop blood sugar that is too low. Low blood sugar can be very serious, and even fatal, if not treated quickly. Seriously low blood sugar can be avoided if women watch their blood sugar closely and treat low blood sugar early.
If a woman’s diabetes was not well controlled during pregnancy, her baby can very quickly develop low blood sugar after birth. The baby’s blood sugar must be watched for several hours after delivery.
5 Tips for Women with Gestational Diabetes
- Eat Healthy Foods
Eat healthy foods from a meal plan made for a person with diabetes. A dietitian can help you create a healthy meal plan. Learn more about diabetes meal planning. - A dietitian can also help you learn how to control your blood sugar while you are pregnant.
 To find a registered dietician near you, please visit The Academy of Nutrition and Dietetics website.
To find a registered dietician near you, please visit The Academy of Nutrition and Dietetics website.
- Exercise Regularly
Exercise is another way to keep blood sugar under control. It helps to balance food intake. After checking with your doctor, you can exercise regularly during and after pregnancy. Get at least 30 minutes of moderate-intensity physical activity at least five days a week. This could be brisk walking, swimming, or actively playing with children.Learn more about physical activity during pregnancy » - Monitor Blood Sugar Often
Because pregnancy causes the body’s need for energy to change, blood sugar levels can change very quickly. Check your blood sugar often, as directed by your doctor. - Take Insulin, If Needed
Sometimes a woman with gestational diabetes must take insulin. If insulin is ordered by your doctor, take it as directed in order to help keep blood sugar under control.
- Get Tested for Diabetes after Pregnancy
Get tested for diabetes 6 to 12 weeks after your baby is born, and then every 1 to 3 years.For most women with gestational diabetes, the diabetes goes away soon after delivery. When it does not go away, the diabetes is called type 2 diabetes. Even if the diabetes does go away after the baby is born, half of all women who had gestational diabetes develop type 2 diabetes later. It’s important for a woman who has had gestational diabetes to continue to exercise and eat a healthy diet after pregnancy to prevent or delay getting type 2 diabetes. She should also remind her doctor to check her blood sugar every 1 to 3 years.
Women who had gestational diabetes or who develop prediabetes can also learn more about the National Diabetes Prevention Program (National DPP), CDC-recognized lifestyle change programs. To find a CDC-recognized lifestyle change class near you, or join one of the online programs.
More Information
Gestational Diabetes and Pregnancy [PDF – 1 MB]
View, download, and print this brochure about gestational diabetes and pregnancy.
For more information on gestational diabetes, visit the American Diabetes Association’s website.
- Diabetes
- Before Pregnancy
- Healthy Pregnancy
- Birth Defects
- CDC’s National Center on Birth Defects and Developmental Disabilities
Gestational Diabetes Facts: Diagnosis, Risks & Effects
CS-Blog Cedars-Sinai Blog
Feb 28, 2019 Cedars-Sinai Staff
Unlike other types of diabetes, gestational diabetes usually goes away soon after delivery.
Gestational diabetes is when a woman without diabetes develops high blood sugar levels during pregnancy.
Why? Like so many things in pregnancy, it comes down to hormones.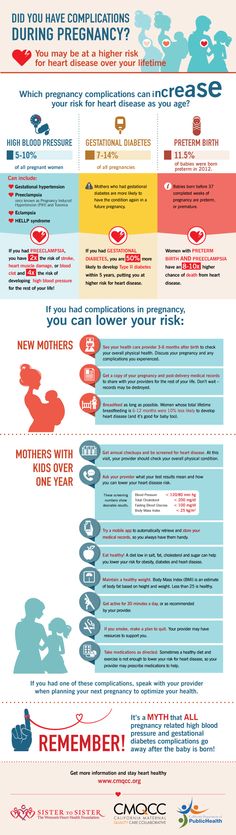
Insulin is a hormone that keeps blood sugar (aka glucose) at healthy levels.
During pregnancy, higher levels of other hormones can interfere with your body's sensitivity to insulin, resulting in elevated blood sugar.
Unlike other types of diabetes, gestational diabetes usually goes away on its own and soon after delivery blood sugar levels return to normal, says Dr. Tania Esakoff, clinical director of the Prenatal Diagnosis Center.
"There is no need for gestational diabetes to take away from the joys of pregnancy."
If gestational diabetes goes away on its own, why is it a problem?
The problem with having too much sugar in your blood is that it bypasses the placenta and goes straight to the unborn baby.
Will the baby be OK?
Most women who get gestational diabetes do well as long as it is adequately managed.
"However, there can be complications for the baby like low blood sugar at birth, breathing issues, low levels of calcium, and jaundice," says Dr. Esakoff.
Esakoff.
High blood sugar levels can also lead to an excessive buildup of amniotic fluid, macrosomia (which is when the baby is much larger than normal), or in rare cases, a stillbirth. Other risks include early delivery, high blood pressure, or preeclampsia.
Most of these complications can be prevented. The key is to get your blood sugar levels under control as soon as you're diagnosed.
Read: What You Should Know About Preeclampsia
How is it diagnosed?
While most women with gestational diabetes have no obvious symptoms, some experience extreme hunger, thirst, or fatigue. Since these symptoms are also common during typical pregnancies, Dr. Esakoff says it's essential to get proper screening.
"We have patients who take care of themselves, are in excellent shape, watch their diet, and they still get it," says Dr. Esakoff. “So you should definitely get tested around 24-28 weeks."
Tests include a 1-hour glucose tolerance test, and if it's positive, a follow-up 3-hour test to confirm the diagnosis.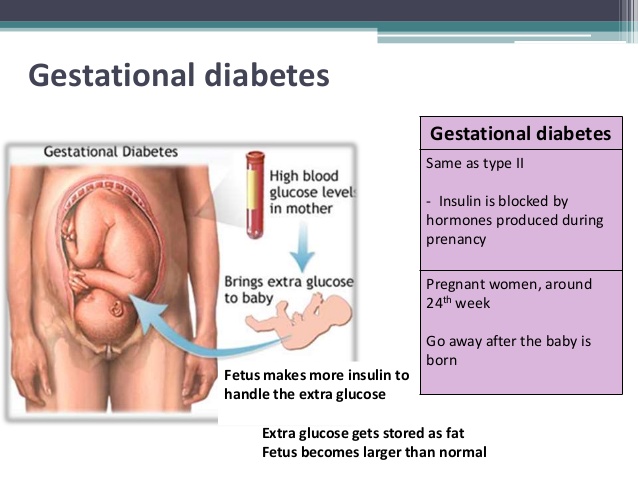
Pregnant women should get tested around 24-28 weeks.
Click To Tweet
What's the best way to manage it?
Unless your doctor has restricted exercising, keeping active is important. It keeps you and the baby healthy and it minimizes weight gain—women who are overweight or obese are more likely to develop gestational diabetes.
Dr. Esakoff also recommends consulting a diabetic nurse educator, dietitian, or doctor to find a way of eating that works for you.
"Controlling gestational diabetes is about finding a correct balance of protein, fats, and carbs," she explains. "A lot of patients assume if they cut carbs, things will be better, but you do need carbs when you're pregnant."
Some women also need medication or insulin injections.
Who's at risk?
Any woman can develop gestational diabetes when she's pregnant, but you're at higher risk if you:
- Are overweight or obese
- Have a family history of diabetes
- Had gestational diabetes in a past pregnancy
- Are over 25
- Are African-American, American Indian, Asian-American, Hispanic or Latina, or Pacific Islander
- Are prediabetic
- Have high blood pressure
Read: Prediabetes: A Tool for Change
Will gestational diabetes go away?
For most women, yes, but half the women who test positive for gestational diabetes have an increased chance of developing type 2 diabetes later in life.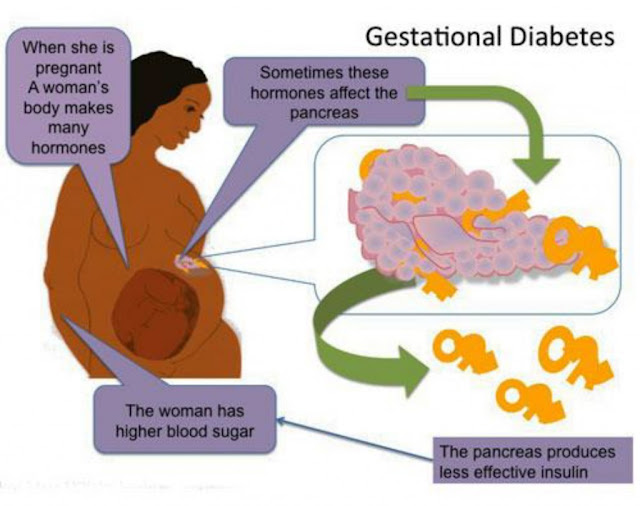
All women with gestational diabetes should be screened at 6 weeks postpartum to determine if they actually have diabetes outside of pregnancy.
"Once a woman has had gestational diabetes, she has to be mindful about diet and exercise for the rest of her life," says Dr. Esakoff.
But that can also be a silver lining.
"Better eating habits will give mom a healthier heart, more energy, and improved self-esteem. That benefits her and the whole family," says Dr. Esakoff.
"There is no need for gestational diabetes to take away from the joys of pregnancy."
Gestational diabetes in pregnancy | OneTouch®
Gestational Diabetes
2What Causes Gestational Diabetes?
Doctors don't know exactly what causes gestational diabetes, but they have some ideas about it.
The placenta supports and nourishes the baby as it grows. Hormones from the placenta help the baby develop. But these same hormones also block the action of insulin, reducing its effectiveness. Gestational diabetes occurs when your body is no longer able to produce and use all the insulin it needs during pregnancy, resulting in high blood glucose levels if left untreated.
Gestational diabetes occurs when your body is no longer able to produce and use all the insulin it needs during pregnancy, resulting in high blood glucose levels if left untreated.
Some women are at higher risk of developing gestational diabetes. The following factors increase the risk of developing gestational diabetes:
- Being overweight before pregnancy
- Too much weight gain during pregnancy (more than the recommended amount)
- Age over 25
- History of gestational diabetes
- Presence of diabetes in close relatives
- African American, Asian, Hispanic or Native American
How is gestational diabetes diagnosed?
Most women who receive good medical care during pregnancy are regularly screened for gestational diabetes between the 24th and 28th weeks of pregnancy. If you are at high risk of developing gestational diabetes, your doctor may test you earlier and/or more than once during your pregnancy.
As part of the Gestational Diabetes Test, your doctor will ask you to drink a sugary drink, and you will have a blood sample taken before and after you drink the drink. If the results show that the blood glucose level at the specified time is above the recommended limits, the diagnosis of gestational diabetes is confirmed. Your doctor will tell you about a plan for treating gestational diabetes.
Why is it important to treat gestational diabetes?
A mother instinctively protects her child. It is important for the health of both mother and child that treatment for gestational diabetes be started as soon as the diagnosis is made. If left untreated, gestational diabetes can cause problems that include the following:
- An increased chance of having a large baby weighing more than 4 kg - this condition is called macrosomia. It increases the likelihood
- complications and injuries during vaginal delivery;
- caesarean section. (K-section)
- Your baby is at high risk for preterm labor and breathing problems (respiratory distress)
- Your baby is at high risk for low blood sugar (hypoglycemia) shortly after birth
- You are more likely to have preeclampsia (high blood pressure and liver or kidney problems)
Following your doctor's instructions and carefully managing your gestational diabetes can greatly reduce your risk of developing these complications.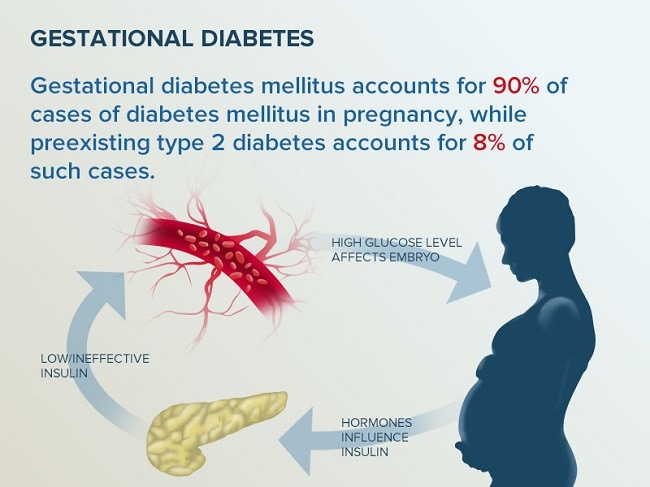
What to expect if you are diagnosed with gestational diabetes?
If you have been diagnosed with gestational diabetes:
- Your doctor will recommend a healthy carbohydrate-controlled diet and exercise. In many cases, these measures will be sufficient to control blood glucose levels throughout pregnancy.
- You may need help from a dietitian in developing a healthy eating plan. A dietitian can teach you how to control the amount and types of carbohydrates in your food to manage your blood glucose levels while still meeting the needs of your growing child. You may also be asked to keep a food journal and monitor your weight.
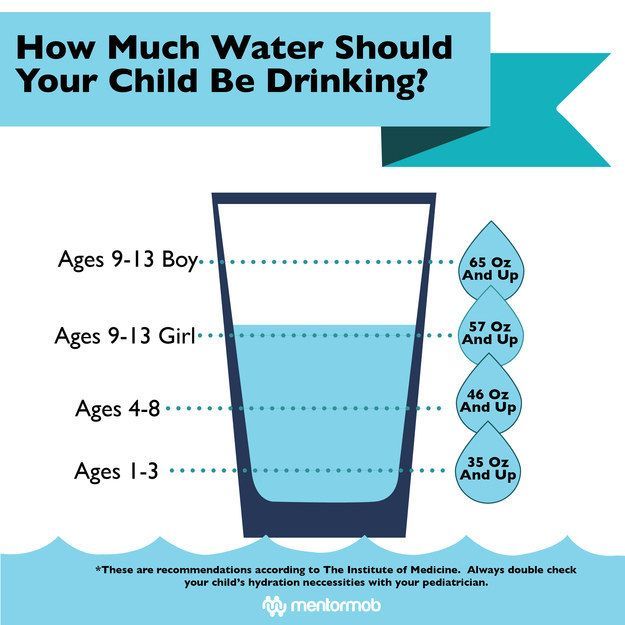
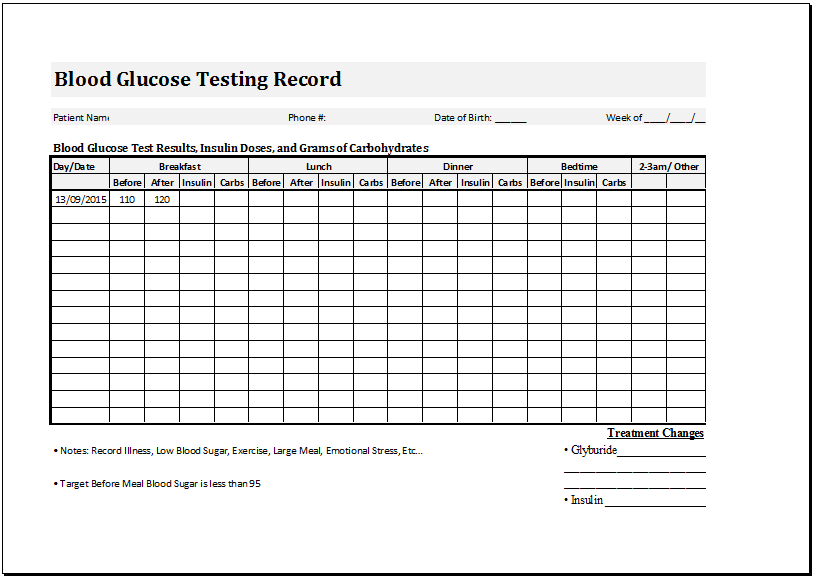
- You may need to check your blood glucose daily with a glucometer. Ask your doctor or diabetes consultant to recommend a glucometer that is right for you. Checking and tracking your blood glucose levels will help you and your doctor manage your gestational diabetes.
As a rule, blood glucose levels should be checked at least 4 times a day, usually on an empty stomach, and then 1-2 hours after a meal. Your doctor or healthcare professional will tell you how often you should test and what your target blood glucose range is. Remember to record your blood glucose measurements, including the time and results of the test, before or after a meal, and how long after a meal the test was taken.
Your doctor or healthcare professional will tell you how often you should test and what your target blood glucose range is. Remember to record your blood glucose measurements, including the time and results of the test, before or after a meal, and how long after a meal the test was taken.
- Light exercise during pregnancy will help your body make better use of its own insulin and help control blood glucose levels. Types of exercise that can be safely performed by pregnant women include brisk walking and swimming. Talk to your doctor for advice on safe exercise during pregnancy.
At your appointment, the midwife can check your blood pressure and take a urine sample. You will also talk to your doctor about your blood glucose test results, how you eat, how much exercise you do, and how much weight you have gained. Your growing child will also be closely monitored. All this will help determine if the prescribed treatment plan for gestational diabetes is working and if it needs to be adjusted.
If dietary changes and exercise don't help control your blood glucose, your doctor may prescribe medication—pills or insulin—for the rest of your pregnancy.
Medication (pills, insulin)
Just because your doctor prescribes pills or insulin doesn't mean you can't manage your gestational diabetes. In some cases, your body may simply not be able to produce enough insulin on its own that your body needs as your baby grows. It is very important to follow your doctor's advice to protect yourself and your baby. You may be able to stop taking antidiabetic drugs after the baby is born.
If your doctor prescribes insulin to treat gestational diabetes, you can get it by injection or by other means, such as an insulin pump. Someone in your family can learn this with you and help you take your insulin as prescribed by your doctor. Fortunately, today, thanks to insulin syringes with small, thin needles, injections are virtually painless. Your doctor will tell you when and how much insulin you should take each time, and may recommend adjusting your insulin intake during your pregnancy.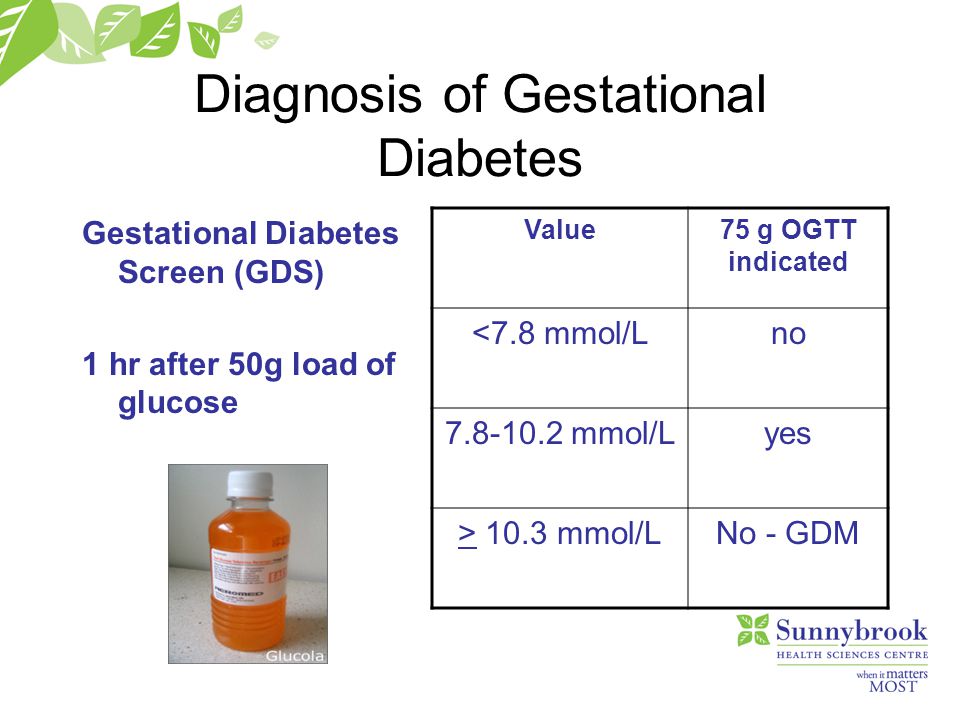
Refs:
2 IDF Diabetes Atlas (Version 8) (2017). International Diabetes Federation: Brussels, Belgium. Online version dated May 5, 2018 at http://diabetesatlas.org/IDF_Diabetes_Atlas_8e_interactive_EN/
You may be interested
What is diabetes?
Gestational diabetes - causes, symptoms, diagnosis, treatment, diet, prevention of diabetes during pregnancy0009
Gestational diabetes is diabetes that occurs during pregnancy. From 1 to 20% (on average - 7%) of expectant mothers face such a problem. For the majority, this pathology after childbirth disappears without a trace, but in 10-15% it turns into type II diabetes mellitus. Half of women who have gestational diabetes during pregnancy acquire type II diabetes within the next 10-15 years after giving birth.
Causes of gestational diabetes
The exact mechanism of the onset of the disease is still not completely clear.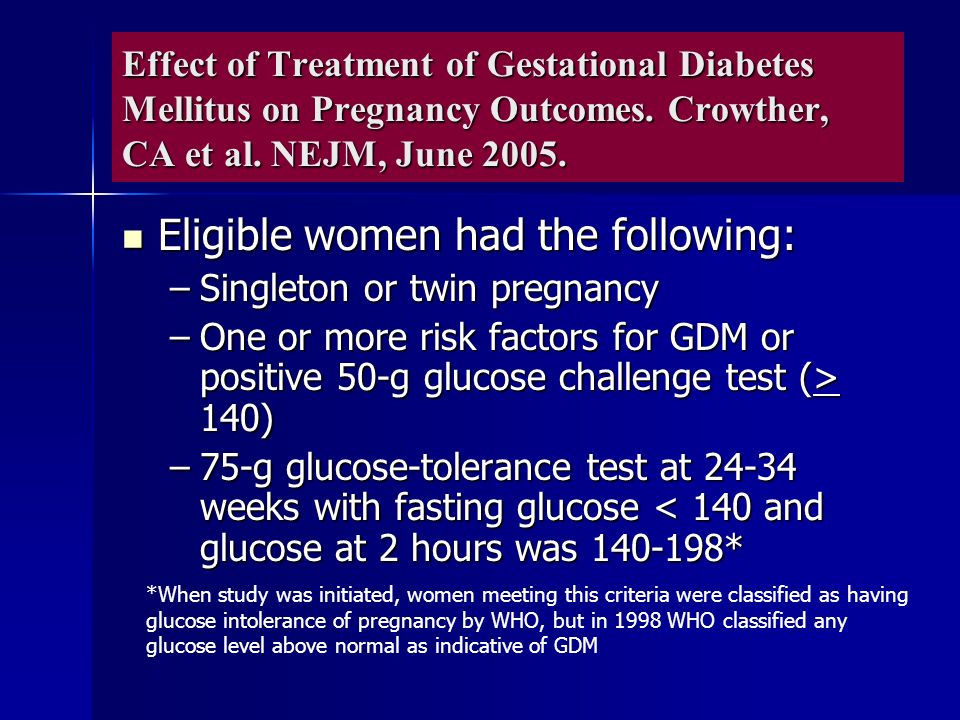 Doctors are inclined to believe that the hormones responsible for the proper development of the fetus block the production of insulin, which leads to a violation of carbohydrate metabolism. During pregnancy, more glucose is required for both the woman and the baby. The body compensates for this need by suppressing the production of insulin.
Doctors are inclined to believe that the hormones responsible for the proper development of the fetus block the production of insulin, which leads to a violation of carbohydrate metabolism. During pregnancy, more glucose is required for both the woman and the baby. The body compensates for this need by suppressing the production of insulin.
There are other possible causes of gestational diabetes, such as autoimmune diseases that destroy the pancreas. In principle, any pathology of the pancreas can increase the risk of diabetes during pregnancy.
Danger of diabetes during pregnancy
This pathological condition threatens the health of both mother and child. Even before birth, the fetus begins to actively produce insulin to compensate for the increased glucose in the mother's blood. Such children are prone to low blood sugar from birth, they have a higher risk of obesity and type II diabetes in adulthood.
Gestational diabetes increases the risk of high blood pressure as well as preeclampsia, a severe form of preeclampsia. It is manifested by headaches, nausea, vomiting, visual disturbances, lethargy, drowsiness or insomnia. This is one of the most severe disorders during pregnancy, affecting the central nervous system.
It is manifested by headaches, nausea, vomiting, visual disturbances, lethargy, drowsiness or insomnia. This is one of the most severe disorders during pregnancy, affecting the central nervous system.
Another worrying factor is that diabetes during pregnancy contributes to rapid weight gain in the baby during the prenatal period (macrosomia). This causes difficulties in childbirth and poses a threat to the mother. A large child is considered to be over 4 kg. These children are at higher risk of birth injury and are more likely to need a caesarean section. Due to the large size of the fetus, an early delivery may be required. At the same time, the risk of preterm birth is high.
Also, high sugar in pregnant women increases the risk of cardiovascular and nervous pathologies of the fetus, increases the risk of respiratory distress syndrome in the baby (a condition that makes breathing difficult), and generally increases the incidence of complications during pregnancy and childbirth.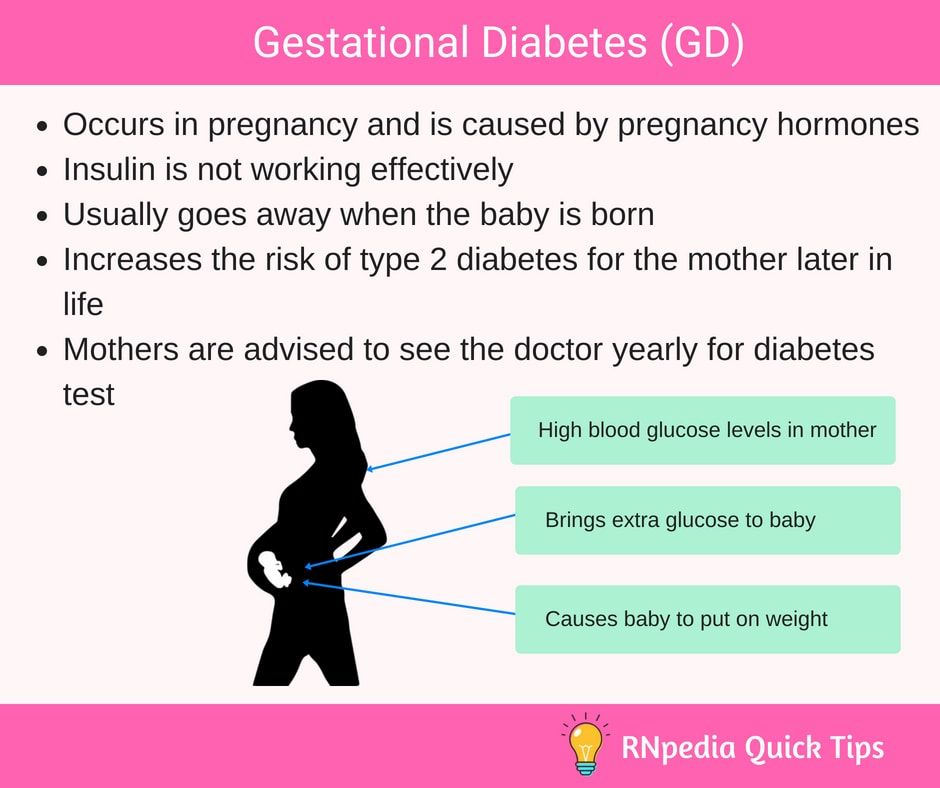
Risk factors for gestational diabetes
- Age under 18 and over 30 years of age.
- Unbalanced diet with a lot of fast carbohydrates.
- Bad habits (smoking, alcohol abuse).
- Overweight and obesity. Excess weight obviously implies a violation of metabolic processes.
- Lack of physical activity.
- Previous gestational diabetes or pre-diabetes. The tendency to diseases of this series does not disappear with time.
- Polycystic ovary syndrome.
- Diabetes in a close relative. The risk of gestational diabetes is doubled or more if close relatives have any form of diabetes.
- Previous birth of a child over 4 kg or a large fetus during the current pregnancy.
- Race. The Caucasian race has the lowest risk of developing gestational diabetes, most often black women suffer from this problem.
Unfortunately, GDM can also develop in a perfectly healthy woman without risk factors, so you need to visit a doctor and not skip the recommended screenings.
Symptoms of gestational diabetes
In most cases, the disease is asymptomatic for a long time, and this is its danger. Usually, the problem is detected after the 20th week of pregnancy through a blood sugar test.
Severe symptoms are rare and all are non-specific: intense thirst, weight gain, increased daily urination. Sometimes patients complain of fatigue and lack of energy.
Diagnosis of gestational diabetes
There is also good news. All pregnant women, when registering, must take a blood test for glucose levels, therefore, if you regularly undergo all the prescribed examinations, you will find a problem at the very initial stage.
The normal value is 3.3-5.1 mmol/l in the analysis of blood from a fasting vein. Patients whose glucose level exceeds 5.1 mmol / l are at risk. In this case, the doctor will order a glucose loading test or a glucose tolerance test to confirm or refute the diagnosis.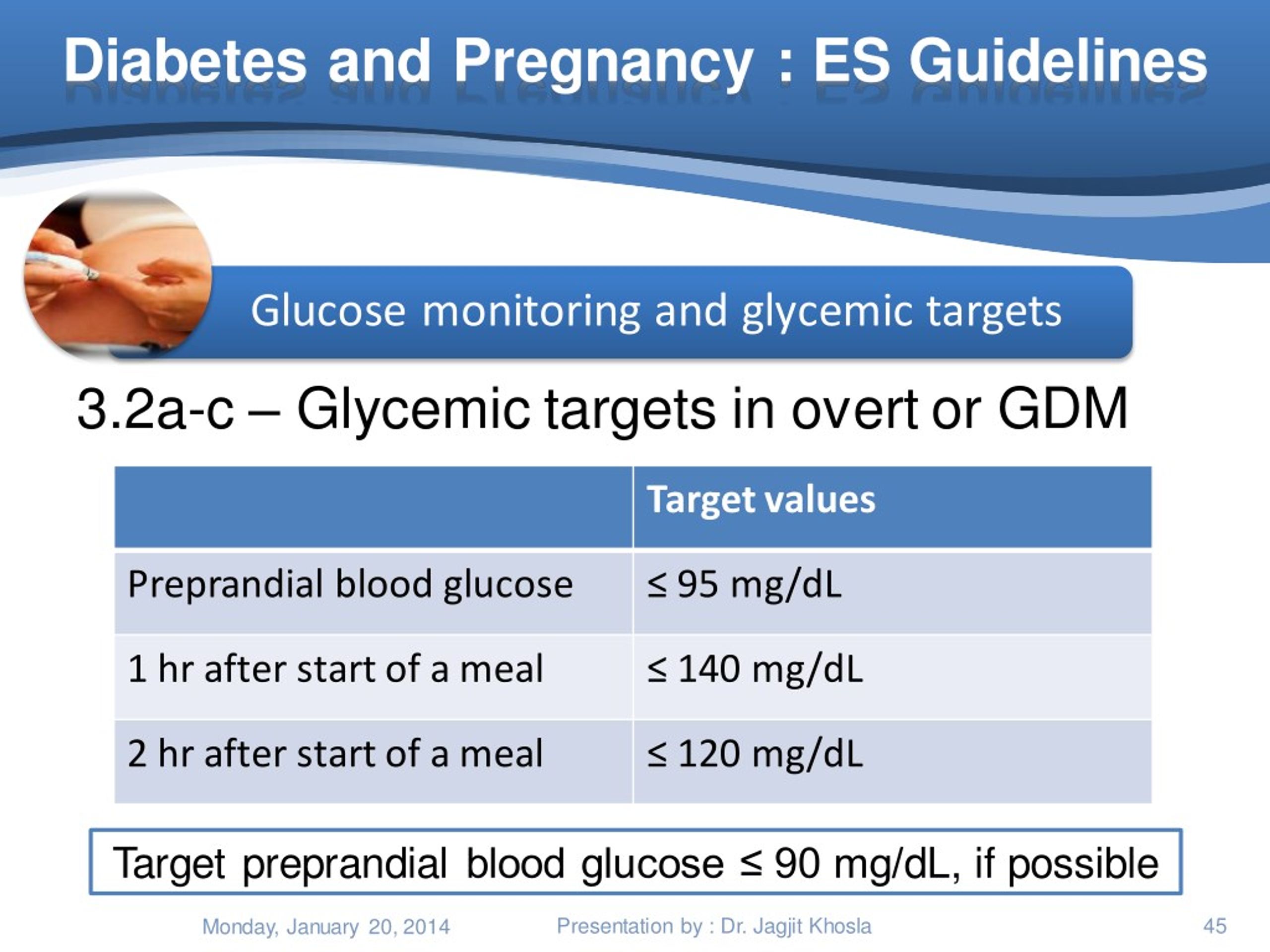 It is carried out at the 24-28th week of pregnancy. Such a study includes two stages: first, a woman takes a regular blood test for fasting glucose, after which she drinks a special solution containing 75 grams of glucose, and takes the test again two hours later. If a disease is suspected, the same analysis is repeated again after a few hours.
It is carried out at the 24-28th week of pregnancy. Such a study includes two stages: first, a woman takes a regular blood test for fasting glucose, after which she drinks a special solution containing 75 grams of glucose, and takes the test again two hours later. If a disease is suspected, the same analysis is repeated again after a few hours.
The diagnosis of gestational diabetes is made if the fasting blood glucose level is less than 7 mmol / l, but above 5.1 mmol / l, and the level of venous blood glucose two hours after 75 g of glucose is above 8.5 mmol / l .
Treatment of gestational diabetes
The first step in treating GDM is a balanced diet and moderate exercise. The main goal of the diet is to reduce sugar to normal values, so the expectant mother will have to give up sweets and fast carbohydrates.
Recommended for pregnant women:
- Eat a little, but often.
- Avoid high glycemic foods (sugar, honey, potatoes, white bread, muffins, bananas, grapes).

- Refuse fast food and fatty sweet pastries.
- Drink plenty of fluids if there are no contraindications from the kidneys.
- Diversify the diet with fresh vegetables, lean meat, cereals.
Like all pregnant women, it is important for patients with GDM to receive the full range of vitamins and minerals that are necessary to maintain their own health and the proper development of the fetus.
Walking, swimming, water gymnastics, physiotherapy for pregnant women - any light activity will benefit.
If diet and exercise fail to lower blood sugar levels, insulin therapy is indicated.
Important: Women with high blood sugar should check their glucose levels daily. Measurements are taken on an empty stomach and an hour after each meal using a home glucometer.
Prevention of gestational diabetes
Unfortunately, there are no 100% effective measures that would protect against this disease.